Strategic Contamination Control in Nested PCR: A Complete Guide for Reliable Molecular Diagnostics
This article provides a comprehensive framework for researchers and drug development professionals to understand, prevent, and troubleshoot contamination in nested Polymerase Chain Reaction (nested PCR) protocols.
Strategic Contamination Control in Nested PCR: A Complete Guide for Reliable Molecular Diagnostics
Abstract
This article provides a comprehensive framework for researchers and drug development professionals to understand, prevent, and troubleshoot contamination in nested Polymerase Chain Reaction (nested PCR) protocols. Nested PCR's exquisite sensitivity, which allows for detection of low-copy pathogens like Acanthamoeba or Fusarium tricinctum, is paradoxically its greatest vulnerability, making it highly susceptible to amplicon carryover contamination and false-positive results. We explore the foundational sources of contamination, detail rigorous methodological controls including physical laboratory separation and enzymatic decontamination, and offer advanced troubleshooting protocols. Furthermore, we present a comparative analysis of nested PCR against alternative molecular techniques like qPCR, validating its specific niche in sensitive diagnostics when performed with stringent contamination controls, ultimately ensuring data integrity in biomedical research and clinical applications.
Understanding the Enemy: Sources and Consequences of Nested PCR Contamination
Nested PCR is a powerful molecular technique renowned for its high sensitivity and specificity. By using two sets of primers and successive rounds of amplification, it significantly enhances the detection of low-abundance targets, making it invaluable in pathogen detection, genetic studies, and cancer research [1] [2]. However, this exceptional sensitivity comes with a significant trade-off: an increased vulnerability to contamination. This guide explores the reasons behind this susceptibility and provides actionable strategies for researchers to mitigate these risks in their experiments.
FAQ: Understanding Contamination in Nested PCR
What makes nested PCR more prone to contamination than standard PCR?
Nested PCR is particularly prone to contamination due to its two-step amplification process. The primary reason is the need to transfer the first-round PCR product to a second tube for the next amplification round [1] [2]. Each time the reaction tube is opened, there is a risk of introducing airborne contaminants or carryover amplicons from previous reactions into the laboratory environment. Furthermore, because the second round of PCR uses the highly amplified product of the first round as its template, even a minuscule, invisible aerosol droplet containing this product can serve as a potent template, leading to false-positive results [1].
Contamination in PCR laboratories typically originates from four main sources [3]:
- Carryover Contamination: Amplified PCR products from previous reactions are the most common source.
- Cloned DNA: Previously handled plasmid or cloned DNA in the lab.
- Sample-to-Sample Contamination: Can occur during extensive sample processing.
- Exogenous DNA: Environmental DNA present on laboratory equipment, in reagents, or introduced during nucleic acid extraction.
How can I tell if my nested PCR reaction is contaminated?
Signs of contamination include [3]:
- False-positive results: Amplification bands appearing in your negative control reactions (e.g., no-template controls).
- Unexpected bands: Presence of amplification products that do not match the expected size or pattern when analyzed by gel electrophoresis.
A critical step in troubleshooting is always to include and check the results of your negative controls. If the negative control shows amplification, the experiment is compromised by contamination [3].
Troubleshooting Guide: Preventing and Managing Contamination
Preventive Best Practices
The most effective strategy for managing contamination is prevention through rigorous laboratory practice.
- Physical Separation of Workspaces: Establish and strictly maintain separate, dedicated areas for [3]:
- Pre-PCR Area: For reaction setup only. This area should contain dedicated pipettes, tips, reagents, and lab coats. No amplified DNA or post-PCR materials should ever enter this space.
- Post-PCR Area: For PCR amplification, gel electrophoresis, and product analysis. Equipment, including pipettes and the thermal cycler, should remain in this area.
- Use of Aerosol-Barrier Tips: Always use pipette tips with filters to prevent aerosol contamination from pipettes [3].
- Aliquot Reagents: Prepare and store reagents in small, single-use aliquots to minimize repeated exposure and cross-contamination [3].
- Implement UV Irradiation: Use UV light in laminar flow hoods and on work surfaces to degrade any contaminating DNA before and after setting up reactions [3].
- Consider Single-Tube Nested PCR: Where possible, adopt single-tube nested PCR protocols where both primer sets are included in the initial reaction mix, eliminating the need for physical transfer and significantly reducing contamination risk [1].
Decontamination Protocols
If contamination is suspected or occurs, take immediate action to decontaminate your workspace and equipment [3]:
- Surface Decontamination: Thoroughly clean workstations, equipment, and pipettes with a 10% bleach solution, followed by wiping with ethanol or RNAse/DNAse-free water [3].
- UV Irradiation: Leave pipettes and other small equipment under a UV light in a cell culture hood overnight [3].
- Replace Reagents: Discard all current aliquots of reagents (buffers, water, master mix) used in the contaminated experiment and prepare fresh ones [4].
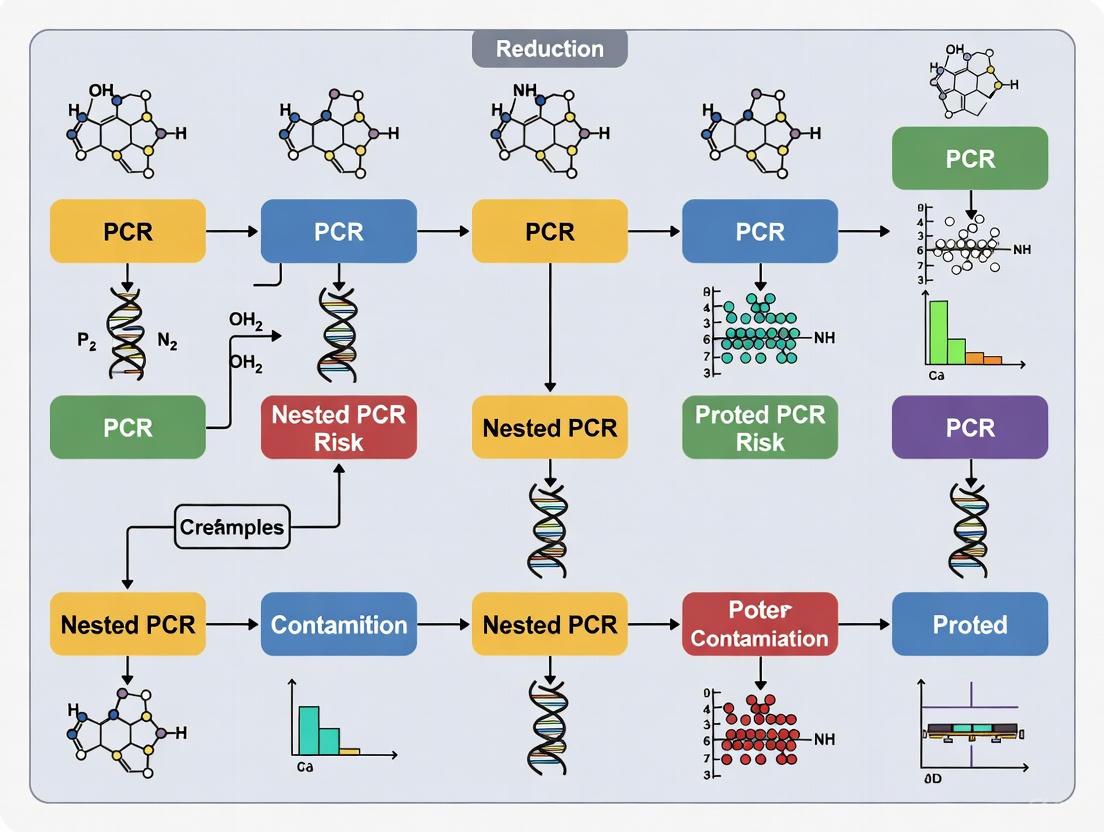
The workflow below illustrates the key contamination risks in the traditional nested PCR process and the primary mitigation strategies.
Quantitative Data on Contamination Risks
The table below summarizes the primary factors that contribute to contamination in nested PCR and their potential impact on experimental results.
Table 1: Factors Contributing to Contamination in Nested PCR
| Factor | Description | Impact on Experiment |
|---|---|---|
| Tube Transfer [1] [2] | Requirement to open tube after first round of amplification to add nested primers or transfer product. | Creates opportunity for aerosol release of highly concentrated amplicons, leading to laboratory-wide contamination and false positives. |
| Extreme Sensitivity [1] [5] | Second round uses product from first round as template, amplifying already amplified material. | Can detect minute levels of contaminating DNA (e.g., from a single aerosol droplet), making false positives likely without stringent controls. |
| Increased Manipulation [1] [2] | Involves more steps and handling than standard PCR. | Prolongs sample exposure to the environment, increasing the probability of introducing contaminants. |
Research Reagent Solutions for Contamination Control
Using the right reagents and materials is fundamental to minimizing contamination risk. The following table lists essential items for a robust nested PCR workflow.
Table 2: Key Reagents and Materials for Contamination Control
| Item | Function | Importance for Contamination Control |
|---|---|---|
| Hot-Start DNA Polymerase [6] | Enzyme activated only at high temperatures, preventing non-specific amplification during reaction setup. | Improves specificity and yield, reducing background that can complicate analysis and be mistaken for contamination [6]. |
| Aerosol-Barrier Pipette Tips [3] | Disposable tips with an internal filter. | Prevents aerosols from contaminating the pipette shaft and subsequent samples, a primary vector for carryover contamination [3]. |
| UV Lamp [3] | Source of ultraviolet light. | Used to irradiate workstations and equipment to degrade contaminating DNA before setting up reactions [3]. |
| Dedicated Pre-PCR Reagents [3] | Buffers, nucleotides, and water aliquoted for PCR setup only. | Stored separately from post-PCR analysis reagents to prevent introduction of amplicons into new reactions [3]. |
| Single-Tube Nested PCR Kits [1] | All reagents and primers for both rounds in one tube. | Eliminates the tube-opening step between amplification rounds, drastically reducing the biggest contamination risk in traditional nested PCR [1]. |
Nested PCR remains a "double-edged sword"—its unparalleled sensitivity is its greatest asset and its most significant vulnerability. The very act of amplifying a target to such a high degree creates a substantial risk of contamination that can compromise experimental integrity. However, by understanding the sources of contamination and rigorously implementing the preventive measures and troubleshooting protocols outlined in this guide—particularly physical workspace separation, meticulous technique, and the adoption of single-tube methods where possible—researchers can confidently wield this powerful technique while safeguarding the validity of their results.
FAQs
The main sources of contamination in nested PCR are:
- PCR Amplicon Carryover: This is the most significant source. A typical PCR can generate up to 10^9 copies of the target sequence. These previously amplified products (amplicons) can aerosolize and contaminate reagents, equipment, and laboratory ventilation systems, leading to false-positive results in subsequent runs [7] [8].
- Cross-Contamination between Samples: This occurs when a sample with a high concentration of the target organism contaminates neighboring samples during handling, nucleic acid extraction, or pipetting [8] [9].
- Environmental Nucleic Acids: Plasmid clones or nucleic acids from previously analyzed organisms can persist in the laboratory environment and be introduced into new reactions [7] [8].
- Contaminated Reagents: Reagents, especially water, can become reservoirs for contaminating DNA if not properly handled and sterilized [9].
Why is nested PCR particularly susceptible to carryover contamination?
Standard nested PCR is highly susceptible because it requires transferring the amplified product from the first PCR reaction to a new tube for the second round of amplification. This process of opening reaction tubes significantly increases the risk of generating aerosols and spilling amplicons, which can then contaminate future experiments [5] [10]. The extreme sensitivity of the technique, designed to detect very low abundance targets, means that even minute amounts of this carryover contamination can be detected and amplified, leading to false positives [11] [8].
What are the most effective strategies to prevent amplicon carryover?
A multi-layered approach is most effective. The core strategies are summarized in the table below.
| Strategy | Description | Key Action |
|---|---|---|
| Physical Segregation | A unidirectional workflow separates pre- and post-PCR activities into different rooms or dedicated spaces to prevent amplicons from entering clean areas [7] [9]. | Move from sample prep → PCR setup → amplification → product analysis without backtracking. |
| UNG/dUTP Treatment | An enzymatic method where dTTP is replaced with dUTP in the PCR master mix. The enzyme Uracil-N-Glycosylase (UNG) is added to new reactions, destroying any contaminating uracil-containing amplicons before amplification begins [7] [8]. | Incorporate UNG enzyme and dUTP in your PCR protocol. |
| Single-Tube Nested PCR | A protocol modification where both amplification rounds occur in the same sealed tube, eliminating the need for transfer and drastically reducing contamination risk [10] [12]. | Adopt single-tube protocols using primers with different melting temperatures or immobilized inner primers. |
| UV Irradiation | Using ultraviolet (UV) light to induce thymidine dimers in contaminating DNA, rendering it unamplifiable [7] [8]. | Expose workstations, instruments, and PCR master mixes (without template) to UV light before use. |
| Chemical Decontamination | Routinely cleaning surfaces and equipment with sodium hypochlorite (bleach), which oxidizes and damages nucleic acids [7] [8]. | Clean work surfaces with 10% bleach followed by 70% ethanol to remove residue. |
How can I decontaminate my laboratory after a contamination event is suspected?
If you suspect a widespread contamination event, take these aggressive steps:
- Discard Reagents: Shut down the laboratory and discard all working solutions, especially water and master mixes [9].
- Thorough Decontamination: Decontaminate all work surfaces, equipment, pipettes, and laboratory coats. Use a 10% bleach solution, followed by ethanol to remove the bleach residue [7] [9].
- Replace Consumables: Autoclave or incinerate contaminated utensils and order new supplies of PCR reagents [9].
- Use Robust Controls: Always include negative controls (No-Template Controls) to monitor for contamination in every run [13] [9].
Experimental Protocols for Contamination Control
Protocol 1: Implementing a Single-Tube Nested PCR
This protocol adapts the traditional two-step nested PCR into a single closed-tube format, dramatically reducing contamination risk by eliminating tube opening between amplification rounds [10] [12].
Workflow Diagram:
Methodology:
- Primer Design and Immobilization: Design two primer sets (outer and inner) targeting the same locus. The inner primers are immobilized on the inside of the PCR tube cap by drying (e.g., with a trace of bromophenol blue) at 37°C [10].
- Reaction Setup: In the bottom of the tube, prepare a standard PCR master mix containing the outer primers, dNTPs, buffer, polymerase, and the DNA template.
- Amplification:
- First Round: Run 15-20 cycles at an annealing temperature high enough to permit binding only for the outer primers. This generates the first amplicon.
- Primer Mixing: Pause the thermocycler at 92°C. Invert the closed tube several times to dissolve the inner primers from the cap into the reaction mixture.
- Second Round: Resume for 30-40 cycles at a lower annealing temperature suitable for the inner primers, which will now amplify the specific product from the first round.
- Detection: Analyze the final product by gel electrophoresis. This method has been shown to achieve a sensitivity of 10-100 target copies [10].
Protocol 2: Pre-Amplification Sterilization with Uracil-N-Glycosylase (UNG)
This method is a widely used pre-amp sterilization technique that can be integrated into any PCR protocol to degrade contaminating amplicons from previous reactions [7] [8].
Workflow Diagram:
Methodology:
- dUTP Incorporation: In all PCR assays, substitute dTTP in the master mix with dUTP. This ensures all newly synthesized amplicons contain uracil instead of thymine [7] [8].
- Sterilization of New Reactions: For a new PCR setup, add the UNG enzyme to the complete master mix (containing dUTP) before adding the new DNA template. Incubate the reaction at room temperature for 10 minutes. During this step, UNG will recognize and hydrolyze the glycosidic bond of uracil in any contaminating, uracil-containing amplicons, breaking the DNA backbone and rendering them unamplifiable [7].
- Enzyme Inactivation and Amplification: Incubate the reaction tube at 95°C for 5 minutes. This heat step inactivates the UNG enzyme so it does not degrade the new uracil-containing products in the upcoming PCR. Proceed with the standard thermal cycling program [8].
Research Reagent Solutions
The following reagents are essential for implementing effective contamination control protocols.
| Reagent/Kit | Function in Contamination Control |
|---|---|
| Uracil-N-Glycosylase (UNG) | Key enzyme in the most widely used method to prevent carryover; cleaves uracil-containing DNA from previous amplifications [7] [8]. |
| dUTP | Used as a substitute for dTTP in PCR master mixes to generate amplicons that are susceptible to cleavage by UNG [7] [8]. |
| Single-Tube Nested PCR Kits | Pre-formulated master mixes optimized for two-round amplifications in a single tube, reducing manipulation and contamination risk. |
| Positive Displacement Pipettes/Tips | Mechanical barriers that prevent aerosol formation during pipetting, reducing sample-to-sample and amplicon cross-contamination [9]. |
| PCR Workstations with UV Light | Dedicated hoods or cabinets equipped with UV lamps to sterilize work surfaces and reaction setups by damaging stray nucleic acids [7] [9]. |
False positives in diagnostic and research PCR protocols represent a critical failure point with consequences that extend far beyond an inconclusive result. In diagnostics, a false positive can lead to unnecessary medical treatments, psychological distress, and substantial healthcare costs. In research, they can invalidate experimental findings, waste precious resources, and derail scientific progress. Within the specific context of nested PCR—a method prized for its high sensitivity in detecting low-abundance targets—the risk of false positives is particularly acute due to the extensive sample manipulation required [1]. This technical support guide provides researchers and drug development professionals with actionable strategies to identify, troubleshoot, and prevent the contamination that leads to false positives.
The first step in mitigating false positives is understanding their origins. Contamination in nested PCR primarily arises from two key sources, each requiring distinct control strategies.
Amplicon Carryover Contamination: This is the single most significant source of false positives [9]. PCR amplicons (the amplified DNA products from previous reactions) are present in extremely high concentrations (up to 10⁹ copies per reaction) and can form aerosols during post-PCR handling steps like tube opening, gel loading, or pipetting [14]. These aerosolized amplicons can contaminate reagents, equipment, and laboratory surfaces, acting as potent templates in subsequent reactions.
Cross-Contamination: This involves the introduction of non-amplified target sequences into the reaction. Sources include cross-contamination between clinical samples during nucleic acid extraction and the use of positive control plasmids or clones [14]. Contamination can be spread by laboratory personnel via hair, skin, clothing, or jewelry and through contaminated equipment like pipettes, vortexers, and lab coats [15] [9].
Physical and Workflow Controls for Contamination Prevention
Implementing rigorous physical barriers and a unidirectional workflow is the cornerstone of an effective contamination control program.
Spatial Separation and Unidirectional Workflow
The most effective strategy is the strict physical separation of laboratory activities into distinct, dedicated areas [15] [14]. Traffic must flow unidirectionally from "clean" to "dirty" areas, with no backtracking.
The following workflow diagram illustrates the recommended unidirectional flow of materials and personnel in a nested PCR laboratory to prevent contamination.
Dedicated Work Areas:
- Pre-PCR Areas (Clean Zones):
- Reagent Preparation Area: A dedicated space for preparing and aliquoting master mixes, primers, and other PCR reagents. This should be the most pristine environment [16] [17].
- Sample Preparation Area: A separate area for nucleic acid extraction and purification from patient samples or research specimens [17].
- Post-PCR Area (Contaminated Zone): A separate room for all activities involving amplified PCR products, including gel electrophoresis, PCR product purification, and sequencing [16] [9]. This area must be located downstream from the clean zones and should contain its own dedicated equipment.
Dedicated Equipment and Consumables
Each designated area must have its own set of equipment and consumables, which must never be moved between areas [9] [14].
- Use dedicated pipettes and pipette tips with aerosol filters for pre-PCR work [16].
- Use color-coded lab coats, gloves, and waste containers for each area to prevent accidental transfer of contaminants [9].
- Aliquot all reagents into single-use volumes to prevent contamination of entire stocks [15] [17].
Biochemical and Technical Strategies
In addition to physical controls, specific biochemical and technical methods can be employed to sterilize potential contaminants and improve reaction specificity.
Key Research Reagent Solutions
The following table details essential reagents and their functions in preventing false positives and enhancing nested PCR reliability.
| Reagent/Material | Function in Contamination Control |
|---|---|
| Uracil-DNA-Glycosylase (UNG) | Enzymatically degrades contaminating uracil-containing amplicons from previous PCRs before amplification begins [15] [14]. |
| dUTP | A nucleotide substitute for dTTP. When used in PCR, it incorporates uracil into new amplicons, making them susceptible to UNG degradation in subsequent runs [14]. |
| Hot-Start DNA Polymerase | Polymerase is inactive at room temperature, preventing non-specific amplification and primer-dimer formation during reaction setup, which reduces background and improves specificity [15] [18]. |
| Aerosol-Barrier Pipette Tips | Prevent aerosols and liquids from entering the pipette shaft, reducing cross-contamination between samples and from pipettes to reagents [9] [17]. |
| 10% Sodium Hypochlorite (Bleach) | Causes oxidative damage to nucleic acids, rendering contaminating DNA unamplifiable. Used for routine decontamination of work surfaces and equipment [15] [14]. |
PCR Technique Modifications for Enhanced Specificity
- Hot-Start PCR: This technique uses a modified DNA polymerase that is inactive until a high-temperature activation step. This prevents non-specific priming and primer-dimer formation that can occur during reaction setup at room temperature, thereby increasing specificity and yield [18].
- Touchdown PCR: This cycling method starts with an annealing temperature higher than the primer's melting temperature (Tm), then gradually reduces it in subsequent cycles. The initial high stringency selectively favors the intended specific primer binding over non-specific binding, reducing false amplification [15] [18].
Detection and Troubleshooting of Contamination
Despite all precautions, contamination can occur. A robust monitoring system is essential for its detection.
Essential Controls for Every Experiment
- No-Template Control (NTC): This is the most critical control for detecting contamination. It contains all PCR reagents except the template DNA, which is replaced with nuclease-free water. A positive signal in the NTC confirms the presence of contaminating DNA in your reagents or master mix [15] [16] [17].
- Positive Control: Contains a known, low-concentration target sequence to verify that the assay is working correctly.
- Negative Control (or Blank): Typically consists of water taken through the nucleic acid extraction process to monitor for contamination during sample preparation.
Troubleshooting Guide: Contamination Incidents
When contamination is detected via your controls, follow this structured troubleshooting guide to identify the source and implement a corrective action.
| Observation | Potential Source | Corrective Action |
|---|---|---|
| No-Template Control (NTC) is positive | Contaminated reagents (water, master mix, primers) or contaminated pipettes used for reagent dispensing. | Discard all aliquots of reagents implicated. Decontaminate pipettes with UV and bleach. Prepare fresh aliquots from clean stocks in a dedicated clean area [17]. |
| Multiple samples and NTC are positive | Widespread amplicon contamination in the laboratory environment or a contaminated piece of shared equipment (e.g., centrifuge, vortexer). | Perform a thorough decontamination of all work surfaces and equipment with 10% bleach [14]. Implement stricter unidirectional workflow and physical separation. Use UNG treatment for all future assays [15]. |
| Only one sample is positive in a run, but it is unexpected | Cross-contamination from another sample during nucleic acid extraction or pipetting. | Use aerosol-barrier tips for all liquid handling. Add template DNA last to the reaction mix. Ensure careful technique to avoid splashing between wells [9]. |
Frequently Asked Questions (FAQs)
Q1: Our lab has a persistent contamination problem that we can't resolve. What is the most drastic but effective action we can take? In a worst-case scenario where contamination is rampant, it may be necessary to perform a "lab reset." This involves discarding all working solutions and reagents, performing a thorough decontamination of all surfaces and equipment with 10% bleach and/or UV irradiation, and ordering new stocks of all PCR reagents. Restart operations with strict adherence to a unidirectional workflow from the outset [9].
Q2: Are there specific risks associated with nested PCR that are different from standard PCR? Yes. The primary added risk in traditional two-tube nested PCR is the requirement to open the reaction tube after the first round of amplification to transfer an aliquot of the product to the second reaction. This step exposes a high concentration of first-round amplicons to the environment, dramatically increasing the risk of carryover contamination. To mitigate this, consider adopting single-tube nested PCR protocols where both primer sets are present but designed to work at different cycling conditions, eliminating the need to open the tube [1].
Q3: How effective is UV light in decontaminating surfaces and reagents? UV light (254 nm) is effective at creating thymidine dimers in DNA, which blocks polymerase extension. However, its efficacy is reduced for short amplicons (<300 bp) and GC-rich sequences. It also cannot penetrate liquids or plastic. Therefore, UV decontamination should be used as an adjunct to bleach cleaning, not as a replacement for it [9] [14].
Q4: What is the role of UNG, and are there any limitations? UNG enzymatically cleaves uracil-containing DNA from previous amplifications. It is highly effective but works best for AT-rich sequences and has reduced activity for GC-rich targets. Furthermore, UNG must be completely inactivated during the initial denaturation step; otherwise, residual activity can degrade your new PCR products. Always store PCR products containing dUTP at -20°C or analyze them immediately after amplification [14].
In molecular diagnostics and research, nested Polymerase Chain Reaction (nested PCR) is a powerful technique used to amplify specific DNA sequences with high specificity. This method involves two successive rounds of PCR amplification using two sets of primers. The second, or "nested," set of primers binds within the product of the first amplification, thereby significantly reducing non-specific binding and amplifying the intended target more reliably [19] [20].
However, the exquisite sensitivity of nested PCR, which is its greatest strength, also makes it particularly vulnerable to contamination. The high number of amplification cycles and the need to transfer first-round PCR products to a second reaction tube dramatically increase the risk of false positives due to amplicon carryover contamination [14] [20]. Contaminating amplification products from previous reactions can build up in the laboratory environment, potentially contaminating reagents, equipment, and ventilation systems. In a clinical setting, the consequences can be very serious, including false test results that lead to inappropriate treatment choices or undue patient stress [21]. Therefore, implementing a robust, multi-layered barrier system is non-negotiable for ensuring the integrity of results in nested PCR protocols.
Mechanical Barriers
Principle and Objective
Mechanical barriers are physical and procedural controls designed to prevent the physical transfer of amplification products from "dirty" post-amplification areas to "clean" pre-amplification areas. The primary objective is to create a unidirectional workflow that eliminates cross-contamination [14].
Implementation Protocols
A strict spatial separation of the laboratory is fundamental. The following workflow must be enforced without exception:
- Reagent Preparation Area: A dedicated, clean room for preparing and aliquoting all master mixes. This area should contain dedicated equipment, laboratory coats, gloves, and aerosol-resistant pipettes. All reagents and disposables must be delivered directly to this area and should never leave and re-enter [14].
- Sample Preparation Area: A separate space for processing clinical or environmental specimens to extract nucleic acids.
- Amplification Area: A designated area for the thermal cyclers where the first and second rounds of PCR are performed.
- Product Analysis Area: A physically separated, contained area where the final amplified products are analyzed, for example, by gel electrophoresis. All traffic must be unidirectional from clean to contaminated areas. Technologists must be alert to the possibility of transferring amplification products on their hair, glasses, jewelry, and clothing from contaminated rooms to clean rooms [14].
Chemical Barriers
Principle and Objective
Chemical barriers involve using chemical agents to degrade or modify contaminating nucleic acids before they can be amplified. These methods target the integrity of the DNA molecule itself, rendering it unsuitable as a template for the DNA polymerase [14].
Implementation Protocols
The most common and effective chemical decontamination agent is sodium hypochlorite (bleach).
- Work Surface Decontamination: Workstations in all areas, but especially in pre-amplification zones, must be routinely cleaned with a 10% sodium hypochlorite solution, followed by ethanol to remove the bleach residue. Bleach causes oxidative damage to nucleic acids, preventing re-amplification [14].
- Equipment and Item Decontamination: Any item that must be transferred from a contaminated area to a clean area (which should be avoided when possible) must be decontaminated. This involves soaking the item in a 2% to 10% bleach solution overnight, followed by extensive washing before transfer [14].
Enzymatic Barriers
Principle and Objective
Enzymatic barriers employ enzymes to selectively destroy contaminating amplicons from previous PCRs before a new round of amplification begins. This is a pre-emptive sterilization step incorporated directly into the PCR mix [14].
Implementation Protocol: The dUTP/UNG System
The most widely used enzymatic contamination control system is the uracil-N-glycosylase (UNG) method.
- Principle: In this system, dTTP in the PCR master mix is partially or fully replaced with dUTP. During amplification, the enzyme incorporates dUTP instead of dTTP, generating amplification products that contain uracil. In subsequent PCR setups, the reaction mix is treated with the UNG enzyme. UNG recognizes and catalyzes the removal of uracil bases from the DNA backbone, generating apyrimidinic sites. When the PCR is initiated and the temperature is raised for the first denaturation step, the DNA backbone fragments at these sites, destroying the contaminating amplicons and rendering them unamplifiable. The subsequent high-temperature step (e.g., 95°C) inactivates the UNG, allowing the new, pristine dUTP-containing amplification products to be synthesized from the natural template [21] [14].
The following diagram illustrates this protective mechanism:
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: Why is contamination control especially critical in nested PCR compared to standard PCR? Nested PCR involves two sequential amplification rounds and requires physical transfer of the first-round product, significantly increasing the risk of carryover contamination. Furthermore, the second set of primers can amplify any contaminating first-round amplicons with extreme efficiency, leading to pervasive false positives [20].
Q2: We use UNG. Can we completely disregard physical separation of work areas? No. UNG is highly effective against dUTP-containing amplicons but is ineffective against contamination from natural DNA templates (e.g., high-target concentration in clinical samples) or amplicons from labs that do not use the dUTP/UNG system. Mechanical separation remains the first and most critical line of defense [14].
Q3: What is a No Template Control (NTC), and how do I interpret its results? An NTC is a well that contains all PCR reaction components (primers, master mix, water) but no sample nucleic acid template. It is essential for detecting contamination in reagent components or the environment [21].
- NTC is negative: No contamination is evident. The experiment is valid.
- NTC is positive: Indicates primer-dimer formation or contamination of one or more reaction components with the target sequence. The experiment's results are compromised, and the source of contamination must be investigated [21].
Troubleshooting Common Contamination Issues
| Problem | Possible Cause | Interpretation | Corrective & Preventive Actions |
|---|---|---|---|
| False Positive Results | Amplicon carryover from previous nested PCR runs [14] | Contamination of reagents, equipment, or environment with specific amplification products. | 1. Enforce strict unidirectional workflow [14].2. Implement the dUTP/UNG system in all PCR mixes [21] [14].3. Decontaminate surfaces and equipment with 10% bleach [14]. |
| Contaminated assay components (enzymes, buffers) [21] | Manufacturing process introduced bacterial nucleic acids or synthetic templates. | 1. Use reagents from reputable suppliers.2. Invalidate and replace suspect reagent batches. | |
| False Negative Results | Carryover of inhibitory materials during sample preparation [21] | PCR reaction is inhibited, leading to amplification failure. | 1. Include an internal positive control (IPC) in each reaction [21].2. Repeat sample processing with cleaner nucleic acid extraction. |
| Bubble Formation (in microfluidic chips) | Water vapor permeation and "respiration" in PDMS-made chips [22] | Bubbles displace solution, cause volume loss, and can lead to cross-contamination between reaction units. | Apply a high-pressure liquid seal (above 109 kPa) to effectively prevent bubble formation in PDMS-based devices [22]. |
The Scientist's Toolkit: Essential Research Reagent Solutions
The following reagents and controls are essential for implementing an effective contamination control strategy in nested PCR.
| Item | Function in Contamination Control |
|---|---|
| Uracil-N-glycosylase (UNG) | The core enzyme in the enzymatic barrier; hydrolyzes contaminating dUTP-containing amplicons before PCR begins [21] [14]. |
| dUTP | Used to substitute dTTP in the PCR master mix, creating "sterilizable" amplification products that are susceptible to UNG digestion [14]. |
| Sodium Hypochlorite (Bleach) | The primary chemical barrier; oxidizes and destroys nucleic acids on work surfaces and equipment [14]. |
| Hot-Start DNA Polymerase | A modified polymerase inactive at room temperature. Prevents non-specific amplification and primer-dimer formation during reaction setup, reducing potential background and aiding in the specificity of the nested reaction [6] [23]. |
| No Template Control (NTC) | A critical quality control to monitor for the presence of contamination in reagents or from environmental sources [21]. |
| Internal Positive Control (IPC) | A control sequence added to each reaction to distinguish true target-negative results from PCR inhibition, a common cause of false negatives [21]. |
Building a Fortified Workflow: Practical Protocols for Contamination Prevention
Frequently Asked Questions
Q1: Why is a unidirectional workflow non-negotiable for nested PCR? Nested PCR involves two rounds of amplification, dramatically increasing the risk of amplicon (PCR product) carryover contamination. A unidirectional workflow ensures that amplified DNA products from the second round of PCR or post-amplification analysis are never introduced into the pre-amplification areas where reagents and first-round reactions are prepared. This physical separation is the most critical step in preventing false positives [8] [24].
Q2: What is the most common sign of contamination in my experiments? The most common and reliable indicator is amplification in your No Template Control (NTC) wells. These wells contain all PCR reaction components (primers, master mix, etc.) but no DNA template. Any amplification signal in the NTC indicates that contaminating DNA has been introduced into your reaction [25].
Q3: Can't I just use UV light to decontaminate my workspace instead of physical separation? While UV irradiation is a useful supplementary decontamination method for surfaces and some consumables, it is not a substitute for physical separation. UV light can inactivate exposed amplicons by inducing thymidine dimers, but it may not reach all surfaces effectively and is unreliable for decontaminating liquid reagents [8]. A unidirectional workflow is a proactive, systems-based approach that prevents contamination from occurring in the first place.
Q4: Our lab space is limited. What is the absolute minimum setup required? At a minimum, you must establish two dedicated and physically separated areas:
- Pre-PCR Area: For reagent preparation, sample preparation, and first-round PCR setup.
- Post-PCR Area: For the second round of nested PCR, amplification, and all analysis of PCR products [25] [24]. These areas must have dedicated equipment (pipettes, centrifuges, lab coats, etc.). Technologists should move from the pre- to post-PCR areas, but not back again on the same day without extensive decontamination [24].
Troubleshooting Guides
Problem: Amplification in No Template Control (NTC) Wells
| Observation | Potential Cause | Corrective Action |
|---|---|---|
| Consistent Ct values across all NTC wells | Contaminated reagent (e.g., master mix, water, primers) | Prepare fresh aliquots of all reagents. Replace contaminated stocks [25]. |
| Random Ct values in only some NTC wells | Aerosol contamination during plate setup | Improve pipetting technique; use aerosol-filter tips; centrifuge tubes before opening; review workflow to ensure no amplicons are present [25]. |
| Contamination persists after corrective actions | Widespread environmental amplicon contamination | Perform a deep clean of all pre-PCR surfaces with 10% fresh bleach, followed by 70% ethanol [25] [8]. Implement stricter unidirectional workflow protocols and use UNG enzyme chemistry [25]. |
Problem: High Background or Non-Specific Amplification in Samples
| Observation | Potential Cause | Corrective Action |
|---|---|---|
| Non-specific bands or high background after gel electrophoresis | Contamination from previous nested PCR products | Ensure the second round of PCR is set up in the post-PCR area. Verify that the inner primers are specific and that annealing temperatures are optimized for the second round [26]. |
| General smearing or multiple bands | Carryover contamination degrading assay specificity | Decontaminate workspaces and equipment. Use dedicated pre-PCR lab coats and gloves. Ensure all personnel are trained in contamination avoidance [26]. |
Experimental Protocols for Contamination Control
1. Protocol for Surface Decontamination
- Purpose: To inactivate amplified DNA fragments on work surfaces, equipment, and pipettes.
- Reagents: 10-15% (v/v) sodium hypochlorite (bleach) solution, 70% ethanol, deionized water.
- Procedure:
- Prepare a fresh bleach solution weekly due to its instability [25].
- Apply the bleach solution to the surface and allow it to sit for 10-15 minutes to ensure complete inactivation of DNA [25] [8].
- Wipe down the surface with a paper towel moistened with deionized water to remove bleach residue.
- Follow with a wipe of 70% ethanol to aid in drying and remove any residual water [24].
- Safety: Wear gloves and eye protection when handling bleach solutions [25].
2. Protocol for Using Uracil-N-Glycosylase (UNG) to Prevent Carryover
- Purpose: To enzymatically destroy carryover contamination from previous PCR amplifications prior to the thermocycling of the current experiment.
- Principle: UNG recognizes and removes uracil bases from DNA strands. In this method, dTTP in the PCR master mix is replaced with dUTP. All newly synthesized PCR products will then contain uracil. In subsequent reactions, UNG is added to the master mix and will degrade any uracil-containing contaminant amplicons before PCR begins [25] [8].
- Procedure:
- Reaction Setup: Incorporate dUTP into your PCR master mix instead of dTTP [8].
- UNG Treatment: Include UNG enzyme in the master mix for your next experiment. Incubate the reaction plate at room temperature for 10 minutes before thermocycling. During this step, UNG will cleave any contaminating uracil-containing DNA [8].
- Enzyme Inactivation: Initiate the PCR thermal profile. A first denaturation step at 95°C for 5 minutes will inactivate the UNG enzyme, preventing it from degrading the new uracil-containing products that will be synthesized in the current amplification [8].
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function |
|---|---|
| Aerosol-Resistant Filtered Pipette Tips | Prevents aerosolized contaminants from entering the pipette shaft and contaminating subsequent samples [25]. |
| UNG (Uracil-N-Glycosylase) | An enzymatic system used to destroy carryover amplification products from previous PCR experiments, as detailed in the protocol above [25] [8]. |
| dUTP (Deoxyuridine Triphosphate) | Used as a substitute for dTTP in PCR mixes to generate uracil-containing amplicons that are susceptible to degradation by UNG [8]. |
| 10-15% Bleach (Sodium Hypochlorite) | A potent chemical decontaminant for inactivating DNA on non-porous surfaces and equipment [25] [8] [24]. |
| Aliquoted Reagents | Storing reagents (primers, master mix, water) in small, single-use volumes to prevent repeated freeze-thaw cycles and contamination of a large stock [25]. |
| No Template Control (NTC) | A critical quality control containing all reaction components except the template DNA; used to monitor for the presence of contamination in reagents or the environment [25]. |
Workflow Diagrams
This guide addresses frequently asked questions on essential personal practices for minimizing contamination in sensitive molecular biology workflows, such as nested PCR.
Frequently Asked Questions
1. Why is changing gloves so frequently necessary, and what are the specific guidelines?
The exquisite sensitivity of PCR means that even minute amounts of DNA on gloves can lead to false-positive results. Contamination can originate from previously handled samples, amplicons from post-PCR areas, or the laboratory environment [24] [27].
- When to Change Gloves: The general rule is to wear fresh gloves when starting work in a pre-PCR area and to change them frequently [24]. Specific triggers include:
- Suspected contamination: Change gloves immediately if you suspect they have become soiled with solutions containing template DNA or amplicons [24].
- Moving between work areas: Always change gloves (and lab coat) when moving from a post-PCR area to a pre-PCR area [24] [27].
- During lengthy procedures: While direct studies on PCR are limited, evidence from related fields like arthroplasty surgery suggests that microbiological contamination of gloves increases with time [28]. As a best practice, change gloves at least once per hour during extended pre-PCR setup and whenever moving between critical pre-PCR stations (e.g., from master mix preparation to sample addition) [24] [28].
2. What constitutes proper pipetting technique to prevent aerosol contamination?
Proper pipetting is critical for assay performance and preventing cross-contamination between samples. Incorrect technique can create aerosols that contaminate reagents, pipettes, and adjacent samples [24] [27].
- Use Filter Tips: Always use aerosol-resistant filter tips to prevent aerosol contamination from entering the pipette shaft [27] [16].
- Avoid Splashing: Ensure proper pipetting technique to avoid splashing when aspirating and dispensing liquids [24].
- Handle Tubes Carefully: Open and close all sample tubes and reaction plates carefully to prevent samples from splashing out. A best practice is to briefly spin down (centrifuge) tubes and plates before opening to prevent aerosols from forming when the cap is opened [24].
- Work Methodically: Maintain a calm, organized workflow to avoid accidental spills or splashes.
3. What are the most effective solutions and protocols for surface decontamination?
A rigorous aseptic cleaning technique is a cornerstone of contamination control. Surfaces must be decontaminated to inactivate any DNA present [24] [27].
- Primary Reagent: Diluted Bleach: Sodium hypochlorite (bleach) is highly effective at degrading DNA. The recommended concentration is 10-15% bleach (equivalent to 0.5-1% sodium hypochlorite) [24] [27].
- Decontamination Protocol:
- Clean: Wipe down all work surfaces, pipettors, and touchpoints (e.g., fridge handles) with the freshly prepared bleach solution. Soak the surface for 10-15 minutes to ensure complete inactivation of nucleic acids [24] [27].
- Rinse: After the contact time, use a de-ionized (DI) water-dampened paper towel to wipe away the bleach residue, which can corrode equipment [24] [27].
- Dry (Optional): The surface can be wiped with a 70% ethanol-dampened paper towel to aid in rapid drying [24].
- Frequency: Perform this decontamination before and after each PCR work session and immediately after any spill [24] [27].
4. What do my No Template Control (NTC) results indicate, and how should I respond?
The No Template Control (NTC) is a critical diagnostic for detecting contamination. It contains all PCR reaction components except the DNA template; therefore, any amplification in the NTC indicates contamination [24] [27].
The table below summarizes how to interpret NTC results and recommended actions.
| Observation | Possible Cause | Corrective Actions |
|---|---|---|
| Amplification in all/some NTCs at similar Ct values | Contaminated reagent (e.g., master mix, water, primers) [27] | Replace all reagents with fresh aliquots. Systematically introduce one new reagent at a time to identify the source [27]. |
| Random amplification in NTCs with variable Ct values | Aerosol contamination during reaction setup (e.g., from amplicons in the environment or cross-talk between samples) [27] | Review and improve technique: use aerosol-filter tips, centrifuge tubes before opening, and decontaminate the workspace and equipment thoroughly [24] [27] [16]. |
Decontamination Setup and Workflow
Effective contamination control requires careful preparation and a disciplined, unidirectional workflow.
Preparation is Key:
- Aliquot Reagents: Divide all primers, dNTPs, and buffers into small, single-use aliquots to prevent repeated freeze-thaw cycles and avoid contaminating stock solutions [27] [16].
- Fresh Bleach: Always prepare diluted bleach solutions fresh daily or at least every week, as it degrades and loses effectiveness over time [27].
Logical Workflow: The entire process must flow from "clean" (pre-PCR) to "dirty" (post-PCR) areas, with no backtracking. The following diagram illustrates this unidirectional workflow to prevent amplicon carryover.
Research Reagent Solutions
The table below details key reagents and materials essential for implementing these decontamination practices.
| Item | Function & Rationale |
|---|---|
| Sodium Hypochlorite (Bleach) [24] [27] | The primary chemical for surface decontamination. It effectively degrades DNA contaminants on benchtops and equipment. |
| 70% Ethanol [24] [27] | Used for general cleaning and rapid drying of surfaces after bleach decontamination and rinsing. |
| Aerosol-Resistant Filter Pipette Tips [27] [16] | Create a physical barrier to prevent aerosols and liquids from contaminating the pipette shaft, a common source of cross-contamination. |
| Uracil-DNA Glycosylase (UNG) [8] [27] | An enzymatic method to prevent carryover contamination from previous PCR amplicons. It is included in some master mixes and degrades uracil-containing DNA from prior runs. |
| Laboratory Bleach | Used for general cleaning and rapid drying of surfaces after bleach decontamination and rinsing. |
The dUTP-UNG system is an enzymatic method widely recognized for preventing false-positive results in PCR by eliminating carryover contamination from previous amplification products [8] [29]. This powerful technique is particularly valuable in sensitive applications like nested PCR and when analyzing limited samples, such as in single-cell analysis or liquid biopsies [30].
The system operates on a simple but effective principle:
- dUTP Incorporation: During PCR amplification, deoxyuridine triphosphate (dUTP) is incorporated into newly synthesized DNA amplicons in place of deoxythymidine triphosphate (dTTP) [30] [29]. These uracil-containing amplicons are functionally equivalent to thymine-containing DNA for most downstream applications but possess a critical distinguishing characteristic [29].
- Enzymatic Degradation: In subsequent PCR setups, the reaction mixture is treated with the enzyme uracil-N-glycosylase (UNG) prior to thermal cycling. UNG recognizes and catalyzes the hydrolysis of uracil residues from the sugar-phosphate backbone in any contaminating dUTP-containing DNA [29]. This cleavage creates apyrimidic sites that fragment under the high temperatures of PCR initiation, rendering the contaminants unamplifiable [8] [29].
- Enzyme Inactivation & New Amplification: The UNG enzyme is then thermally inactivated during the initial denaturation step of the new PCR cycle, protecting the newly synthesized dUTP-containing amplicons generated in the current reaction [29].
Experimental Protocols & Workflows
Standard Protocol for Incorporating dUTP-UNG
The following step-by-step methodology is adapted for a target-specific preamplification or standard PCR workflow [30] [8].
Reagent Setup:
- Prepare a master mix using a dNTP blend where dTTP is fully replaced by dUTP [30]. Standard concentration is 0.2 mM for each dNTP, including dUTP [31].
- Include UNG enzyme at a concentration recommended by the manufacturer (e.g., 0.01 - 0.1 U/µL) [8].
- The master mix should also contain all other standard PCR components: primers (0.25 µM), DNA polymerase, PCR buffer, MgCl2 (1.5 mM), and KCl (50 mM) [31].
Step-by-Step Procedure:
Reaction Assembly
- Combine template DNA, master mix, and nuclease-free water to the final desired volume.
- Gently mix and briefly centrifuge the tubes or plates.
UNG Incubation Phase
Enzyme Inactivation & PCR Amplification
- Initiate the thermal cycling protocol with a 5-minute denaturation step at 95°C [8]. This serves two purposes:
- Irreversibly inactivates the UNG enzyme.
- Fragments the sugar-phosphate backbone of UNG-treated contaminant DNA.
- Proceed with the standard cycling parameters for your assay (Denaturation: 90-96°C, Annealing: 40-68°C, Extension: 70-75°C) [31].
- Initiate the thermal cycling protocol with a 5-minute denaturation step at 95°C [8]. This serves two purposes:
Adaptation for Single-Cell Gene Expression Profiling
For sensitive applications like single-cell analysis, a modified protocol demonstrates the system's utility [30]:
Cell Lysis & Reverse Transcription
- Collect individual cells directly into lysis buffer.
- Perform reverse transcription to generate cDNA.
Contamination Control with Cod UNG
- Treat cDNA with Cod UNG (a heat-labile variant) prior to preamplification.
- Key Advantage: Cod UNG can be completely and irreversibly heat-inactivated, preventing any loss of precious preamplification products [30].
Preamplification with dUTP
- Perform target-specific preamplification using a master mix where dTTP is replaced with dUTP.
- This generates sufficient material for multiple downstream qPCR or dPCR analyses while incorporating uracil into all amplicons.
Downstream Quantification
- Use the preamplified product for quantitative analysis via qPCR.
- The protocol successfully eliminates contaminating uracil-containing DNA, even in the presence of a spike-in contaminant, ensuring accurate quantification of rare targets [30].
Performance Data & Comparative Analysis
Quantitative Performance of dUTP vs. dTTP in Preamplification
A comprehensive study using 96 target assays and qPCR compared the performance of dUTP against standard dTTP in preamplification mixes [30].
Table 1: Performance Metrics of dUTP vs. dTTP in Preamplification
| Performance Metric | dTTP (Standard) | dUTP (Experimental) | Statistical Significance |
|---|---|---|---|
| Average Amplification Efficiency | 102% | 94% | p < 0.0001 |
| Reproducibility | Lower | Significantly improved at 3 of 6 concentrations | p < 0.05 |
| Sensitivity (Positive Replicates at Low Concentration) | No significant difference | No significant difference | p > 0.05 |
| Carryover Contamination Elimination after Cod UNG Treatment | Not Applicable | 97% of uracil-containing template degraded | Highly Effective |
Contamination Removal Efficiency
The dUTP-UNG system demonstrates robust degradation of contaminating amplicons, crucial for maintaining assay integrity [30] [32].
Table 2: Contamination Removal Efficiency of the UNG System
| Parameter | Efficiency | Notes |
|---|---|---|
| Overall Template Degradation | 97% average reduction | Across 45 assays [30] |
| Complete Elimination | 34 of 45 assays (76%) | All replicates showed no contamination [30] |
| High Concentration Contamination | Positive correlation with failure | Assays contaminated with high molecule numbers and containing few uracils may still show some contamination post-UNG [30] |
| Sensitivity Limit | >10,000,000-fold reduction | In amplicon concentration shown in RNA virus detection [32] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for dUTP-UNG Experiments
| Reagent / Material | Function / Purpose | Example Usage & Notes |
|---|---|---|
| dUTP (Deoxyuridine Triphosphate) | Replaces dTTP as a nucleotide base; incorporated into amplicons, making them susceptible to future UNG degradation [30] [29]. | Use at standard dNTP concentration (e.g., 0.2 mM). Full replacement of dTTP is required for the system to work [30]. |
| UNG (Uracil-N-Glycosylase) | Enzymatic core of the system; hydrolyzes uracil bases in contaminating dUTP-containing DNA from previous runs [8] [29]. | Also known as UDG. Incubate with reaction mix prior to PCR (e.g., 25°C for 10 min or 50°C for 2 min) [8] [29]. |
| Cod UNG (Heat-Labile) | A recombinant UNG from Atlantic cod that can be completely and irreversibly inactivated by heat [30]. | Critical for preamplification protocols and any workflow where residual UNG activity could degrade new dUTP-containing products [30]. |
| dUTP-containing Master Mix | A pre-formulated, optimized mix containing dUTP, UNG, polymerase, buffer, and salts [29] [27]. | Simplifies experimental setup and ensures optimal concentration of all components for robust amplification and contamination control. |
| Positive Control Template | Validates that all PCR components are functional and the amplification is successful [3]. | Should be a well-characterized, confirmed positive sample. Its concentration should not be so high as to pose a contamination risk [33]. |
| No Template Control (NTC) | A critical control containing all reaction components except the DNA template; used to monitor for contamination [16] [27]. | Amplification in the NTC indicates contamination of reagents or the environment with target DNA or amplicons [27]. |
Troubleshooting Guide & FAQs
Frequently Asked Questions
Q1: My PCR efficiency decreased after switching to a dUTP-based master mix. Is this normal and how can I address it?
Yes, a slight decrease in average amplification efficiency is a documented characteristic of dUTP incorporation. Studies show efficiency may drop from 102% (with dTTP) to 94% (with dUTP) [30]. To mitigate this:
- Optimize Primer Design: Ensure primers have dA-nucleotides near their 3' ends so that primer-dimers are efficiently degraded by UNG [29].
- Check Mg²⁺ Concentration: MgCl₂ is a divalent cation required by the DNA polymerase and its concentration (typically 1.5 mM) can affect efficiency [31] [3].
- Verify UNG Compatibility: The sequence being amplified should contain dA and dT (now dU) nucleotides to be a substrate for UNG [29].
Q2: I am performing one-step RT-PCR. Can I use the dUTP-UNG system?
Using standard E. coli UNG in one-step RT-PCR is not recommended. The reverse transcription step occurs at a temperature (typically 50-55°C) that is within the active range of UNG. This would cause the enzyme to degrade the newly synthesized dU-containing cDNA [29].
- Solution 1: Perform reverse transcription and PCR in two separate reactions.
- Solution 2: Use a specialized one-step RT-PCR master mix that employs a heat-labile UNG (e.g., Cod UNG). This variant can be inactivated during the reverse transcription step, protecting the cDNA [29].
Q3: After implementing dUTP-UNG, I still see contamination in my no-template controls. What could be wrong?
The dUTP-UNG system only degrades uracil-containing DNA. If you are still seeing contamination, the source is likely natural thymine-containing DNA [29]. Re-evaluate your laboratory practices:
- Physical Separation: Strictly maintain separate pre- and post-PCR areas with dedicated equipment, lab coats, and consumables [16] [27] [33].
- Decontaminate Surfaces: Regularly clean benches and equipment with 10% fresh sodium hypochlorite (bleach) or 70% ethanol followed by UV irradiation [8] [27] [33].
- Review Workflow: Ensure a unidirectional workflow (pre- to post-PCR) and that no items from the post-PCR area are brought back into the pre-PCR area [16] [33].
Q4: For which specific applications is the dUTP-UNG system NOT suitable?
Avoid using the dUTP-UNG system in the following scenarios:
- Nested PCR where the first-round product is dUTP-containing: UNG will degrade the product needed for the second round of amplification [29].
- Amplification of bisulfite-treated DNA: Bisulfite conversion transforms unmethylated cytosine residues into uracil, making the template a target for UNG degradation [29].
- Genotyping with delayed end-point analysis: If you plan to read the PCR product long after the run is complete, residual UNG activity (in non-heat-labile forms) could degrade your amplicons over time [29].
- Amplification of GC-rich targets with few dT sites: UNG efficacy is tied to uracil content; targets with few thymine (and thus uracil) bases may not be degraded efficiently [30] [27].
Nested Polymerase Chain Reaction (nested PCR) is a powerful molecular technique that significantly enhances the sensitivity and specificity of target DNA amplification by using two sets of primers in sequential reactions. While this method is invaluable for detecting low-abundance targets in clinical, environmental, and research applications, its extreme sensitivity also makes it particularly vulnerable to contamination, especially from previous amplification products (amplicons). This guide provides a comprehensive contamination-aware protocol to help researchers implement robust nested PCR procedures that minimize false positives and maintain experimental integrity.
FAQs: Understanding Nested PCR and Contamination Risks
What is nested PCR and why is it so susceptible to contamination?
Nested PCR is a two-stage amplification method where the product of the first PCR (using "outer" primers) serves as the template for a second PCR (using "inner" or "nested" primers). This sequential amplification significantly increases sensitivity—by as much as 100 to 1000-fold compared to single PCR [34]. However, this extreme sensitivity comes with increased vulnerability to contamination because the laboratory environment becomes saturated with amplification products from previous reactions. The multi-step nature of nested PCR requires additional tube openings and reagent transfers, creating more opportunities for amplicon contamination [8] [34].
There are four main contamination sources in nested PCR:
- Carryover contamination: Amplification products from previous PCRs are the most significant source [3] [8].
- Cross-contamination between samples: Occurs during sample handling and processing [8].
- Cloned DNA or control plasmids: Previously handled in the laboratory [3].
- Environmental DNA: Exogenous DNA present on laboratory equipment, in reagents, or introduced via personnel [3].
How can I distinguish true positives from contamination in my results?
Implementing appropriate controls is essential for identifying contamination:
- No-template controls (NTC): Contain all PCR components except template DNA; if positive, indicate contamination [3] [33].
- Positive controls: Should be carefully selected and used sparingly [33].
- Chimeric positive controls: Novel approaches using engineered control DNA that can be distinguished from natural templates via restriction enzyme digestion help identify carryover contamination [35].
Troubleshooting Guides
Common Nested PCR Problems and Solutions
| Problem | Possible Causes | Solutions |
|---|---|---|
| No amplification products | Incorrect annealing temperature, poor primer design, missing reaction components, PCR inhibitors, insufficient cycles | Recaculate primer Tm, test annealing temperature gradient, include positive control, increase cycles (up to 40), purify template to remove inhibitors [3] [36] [37] |
| Non-specific bands/smearing | Low annealing temperature, primer non-specificity, excess template, enzyme activity at room temperature | Increase annealing temperature incrementally (2°C steps), use hot-start polymerase, reduce template amount, use touchdown PCR [3] [18] [36] |
| Contamination (false positives) | Amplicon carryover, contaminated reagents, improper lab workflow | Implement physical separation of pre-and post-PCR areas, use UNG system, aliquot reagents, UV irradiation of equipment [3] [8] [33] |
| Poor yield in second round | Insufficient product from first PCR, suboptimal dilution, inhibitor transfer | Optimize dilution factor of first PCR product (try 1:10 to 1:1000), ensure efficient first amplification, increase cycles slightly [18] [38] |
Quantitative Data for Nested PCR Optimization
| Parameter | Recommended Range | Notes |
|---|---|---|
| First PCR cycles | 25-30 cycles | Avoid overcycling to reduce amplicon accumulation [3] |
| Second PCR cycles | 20-25 cycles | Fewer cycles than first round to reduce non-specific products [38] |
| Template dilution | 1:10 to 1:1000 | 10-fold dilutions typically used between first and second rounds [3] [38] |
| Annealing time | 5-15 seconds | Shorter times enhance specificity, especially for PrimeSTAR polymerases [3] |
| Primer concentration | 0.1-1 μM | Optimize for each primer set; high concentrations promote primer-dimers [36] [37] |
Step-by-Step Contamination-Aware Protocol
Pre-PCR Preparation: Laboratory Setup and Reagent Preparation
Physical Laboratory Separation
- Establish three distinct work areas: (1) reagent preparation, (2) sample preparation/template addition, and (3) amplification product analysis [8] [33].
- Maintain unidirectional workflow—never bring equipment or reagents from post-PCR areas back to pre-PCR areas [3] [33].
- Each area should have dedicated equipment (pipettes, tips, centrifuges, lab coats) [33].
Reagent Preparation
- Aliquot all reagents to avoid multiple freeze-thaw cycles and contamination of master stocks [33].
- Prepare master mixes in a laminar flow cabinet equipped with UV light [3] [33].
- Use aerosol-resistant filter tips for all pipetting steps [33].
- Include appropriate controls: no-template, positive, and negative extraction controls [33].
Nested PCR Procedure with Contamination Controls
First Round PCR
- Prepare master mix on ice in the reagent preparation area: Note: For additional protection, substitute dTTP with dUTP in the master mix to enable subsequent UNG treatment [8].
Add template DNA in the sample preparation area.
Thermal cycling conditions:
- Initial denaturation: 94-95°C for 2-5 minutes
- 25-30 cycles of:
- Denaturation: 94-95°C for 30 seconds
- Annealing: Temperature specific to outer primers for 5-15 seconds [3]
- Extension: 72°C for 1 minute/kb
- Final extension: 72°C for 5-10 minutes
Inter-Round Transfer
- Dilute first-round PCR product (typically 1:10 to 1:100) in the sample preparation area [3] [38].
- Centrifuge tubes before opening to avoid aerosol formation [33].
Second Round PCR
- Prepare master mix in the reagent preparation area using inner primers.
- Add diluted first-round product as template in the sample preparation area.
- Use the same thermal cycling conditions as the first round, but with 20-25 cycles.
Post-Amplification Analysis
- Analyze PCR products in the dedicated post-amplification area.
- Never bring amplification products back to pre-PCR areas.
- Clean work surfaces with 10% sodium hypochlorite (freshly prepared) or commercial DNA-decontaminating solutions after use [8] [33].
- Decontaminate equipment with UV irradiation (254 nm for 5-20 minutes) [8].
Advanced Contamination Control Strategies
Enzymatic Control: Uracil-DNA Glycosylase (UNG) System
The UNG method is one of the most effective techniques for preventing carryover contamination:
- Incorporation: Substitute dTTP with dUTP in all PCR mixes, resulting in uracil-containing amplicons [8].
- Contamination Elimination: Before PCR, treat reactions with UNG at room temperature for 10 minutes to degrade any uracil-containing contaminants from previous reactions [8].
- Enzyme Inactivation: UNG is thermally inactivated at 95°C for 5 minutes prior to the actual PCR cycles [8].
Workflow Visualization
Alternative Approaches to Reduce Contamination Risk
Single-Tube Nested Real-Time PCR
Chimeric Positive Controls
- Engineered control plasmids that generate amplicons distinguishable from natural targets via restriction enzyme digestion [35].
- Allows rapid identification of carryover contamination versus true positive results.
The Scientist's Toolkit: Essential Research Reagent Solutions
| Reagent/Equipment | Function in Contamination Control | Implementation Notes |
|---|---|---|
| Hot-start DNA polymerase | Reduces non-specific amplification and primer-dimer formation by inhibiting enzyme activity until high temperatures are reached [18] | Enables room temperature setup without compromising specificity |
| UNG system | Prevents carryover contamination by degrading uracil-containing amplicons from previous reactions [8] | Requires substitution of dTTP with dUTP in all PCR mixes |
| Aerosol-resistant filter tips | Prevents aerosol contamination of pipettors and cross-contamination between samples [33] | Essential for all pipetting steps; confirm compatibility with your pipettes |
| DNA decontamination solutions | Destroys contaminating DNA on work surfaces and equipment [33] | 10% sodium hypochlorite (freshly made) or commercial DNA-destroying products |
| Dedicated equipment and lab coats | Prevents transfer of amplicons between work areas [3] [33] | Color-coding different areas helps prevent accidental transfer |
| UV irradiation equipment | Damages contaminating DNA through thymidine dimer formation [3] [8] | Effective for decontaminating surfaces, tools, and equipment; 254 nm wavelength |
Implementing a contamination-aware nested PCR protocol requires meticulous attention to laboratory workflow, physical separation of pre-and post-amplification activities, and strategic use of enzymatic controls. By adopting these practices—including the UNG system, proper laboratory zoning, and rigorous use of controls—researchers can leverage the exceptional sensitivity of nested PCR while minimizing the risk of false positives due to contamination. These measures are particularly crucial in diagnostic, clinical, and regulatory settings where result accuracy directly impacts patient care, research validity, and regulatory decisions.
In nested PCR protocols, where the amplification of specific DNA sequences is paramount, the risk of contamination poses a significant threat to experimental integrity. Minute airborne particulates or aerosolized amplicons from previous reactions can lead to false positives, rendering data unreliable. This technical support center outlines the systematic use of laminar flow hoods and ultraviolet (UV) decontamination to establish a controlled, contaminant-free workspace, thereby safeguarding the accuracy of your molecular research and drug development processes.
Laminar Flow Hood Fundamentals and Classification
What is a Laminar Flow Hood?
A laminar flow hood, also known as a clean bench, is a piece of laboratory equipment designed to provide a sterile, particulate-free workspace. It achieves this by drawing air through a High-Efficiency Particulate Air (HEPA) filter and projecting it across the work surface in a smooth, laminar, non-turbulent flow. This constant stream of clean air protects the items placed within the hood from contamination by particulates such as dust, airborne microbes, and aerosol particles [39] [40].
Types of Laminar Flow Hoods
Laminar flow hoods are categorized based on the direction of airflow. The table below summarizes the two main types.
Table: Comparison of Laminar Flow Hood Types
| Feature | Horizontal Laminar Flow (HLF) | Vertical Laminar Flow (VLF) |
|---|---|---|
| Airflow Direction | Air flows horizontally from the back of the hood, across the work surface, and towards the user [41]. | Air flows vertically from the top of the hood, down over the work surface [41]. |
| Product Protection | Excellent; the sample is downstream of the filter and upstream of the user or environment. | Excellent; creates a curtain of clean air between the user and the work surface. |
| User Protection | Does not protect the user; not suitable for hazardous materials [41]. | Offers better operator protection than horizontal flow, but still not designed for hazardous materials [41]. |
| Common Applications | Electronics assembly, media plate preparation, and non-hazardous sample manipulation. | Pharmaceutical preparations, medical device manufacturing, and sensitive microbiological work [41] [39]. |
Cleanroom Classifications and Laminar Flow Hoods
Laminar flow hoods create a micro-environment that typically meets the requirements for an ISO 5 (Class 100) cleanroom, which is significantly cleaner than the ISO 8 (Class 100,000) cleanrooms common in medical device manufacturing areas [39]. The following diagram illustrates the typical workflow for establishing and maintaining this sterile environment.
UV Decontamination: Principles and Safety
How Does UV Sterilization Work?
Ultraviolet (UV) sterilization is a disinfection technique that uses short-wavelength UVC light (in the range of 200 to 280 nanometers) to kill or inactivate microorganisms [42]. The mechanism is biochemical: UVC photons are absorbed by the microorganism's DNA and RNA, causing covalent bonds to form between adjacent thymine (in DNA) and uracil (in RNA) molecules [42]. This creates structural abnormalities (thymine dimers) that disrupt genetic replication and function, rendering the microorganism unable to reproduce and effectively inactivating it [42].
Integrating UV Lamps in Laminar Flow Hoods
Many laminar flow hoods are equipped with an optional UVC lamp as an added layer of protection [41]. This lamp is used to sterilize the interior work surface and the contents within the hood between operational periods, typically before and after work sessions [41] [42]. It is crucial to note that the UV light is intended for surface decontamination when the hood is not in use, as it does not sterilize the air during active airflow.
Critical Safety Protocols for UV Light
UVC light is harmful to both skin and eyes. Strict safety protocols must be followed:
- Never be present when the UV light is on. Some hoods are equipped with safety features, such as motion sensors that automatically switch off the UV light when movement is detected [42].
- If you must handle the UV lamp, wear appropriate Personal Protective Equipment (PPE), including UV-blocking safety glasses and gloves [42].
- Ensure the hood's sash or night door/cover is closed when the UV light is activated to contain radiation [41].
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q: Can I use a laminar flow hood for working with pathogenic agents?
- A: No. Standard laminar flow hoods are designed only for product protection. They direct air toward the user and are not safe for handling hazardous, toxic, or pathogenic materials. For such work, you must use a Biosafety Cabinet (BSC), which is designed to provide both product and personnel protection [41].
Q: Why is my laminar flow hood not maintaining a uniform airflow velocity?
- A: A common cause is a clogged HEPA filter. The filter has a finite lifespan and must be replaced when airflow drops below the required level. Other causes can include a faulty blower motor or an obstruction in the pre-filter or ductwork.
Q: How long should I run the UV light to effectively decontaminate the hood?
- A: A typical sterilization cycle runs for a minimum of 15-30 minutes. However, the required time can vary based on the lamp's intensity and the level of contamination. Consult the manufacturer's instructions for specific guidance.
Q: I see a growth in my negative control during nested PCR. Could hood contamination be the cause?
- A: Yes. While the hood protects your work, the UV lamp does not sterilize the air during use. Aerosolized amplicons from previous nested PCR runs can contaminate the workspace. Ensure you decontaminate all surfaces, pipettes, and equipment with a validated disinfectant (e.g., 10% bleach followed by 70% ethanol) and use dedicated consumables within the UV-sterilized hood.
Q: The UV lamp in my hood has stopped working. What should I check?
- A: First, ensure the lamp has not reached the end of its usable life (typically 8,000-9,000 hours). If it is within its lifespan, check the electrical connections and the lamp starter. Always refer to the manufacturer's troubleshooting guide and de-energize the unit before any inspection.
Troubleshooting Common Issues
Table: Troubleshooting Laminar Flow Hood and UV Lamp Problems
| Problem | Potential Causes | Corrective Actions |
|---|---|---|
| Low or No Airflow | 1. Clogged HEPA filter.2. Faulty blower motor.3. Obstructed pre-filter. | 1. Replace HEPA filter.2. Contact service technician.3. Clean or replace pre-filter. |
| UV Lamp Not Turning On | 1. Lamp has reached end of life.2. Ballast or starter failure.3. Loose electrical connection. | 1. Replace the UV lamp.2. Replace ballast/starter.3. Check and secure connections (with power off). |
| Turbulent Airflow | 1. Large object obstructing airflow.2. Improperly placed equipment.3. Room with strong air currents. | 1. Remove obstruction.2. Rearrange work area to minimize disruption.3. Relocate hood away from vents/doors. |
| PCR Contamination | 1. Inadequate surface decontamination.2. Aerosolized amplicons in the environment.3. UV cycle not run or ineffective. | 1. Clean with 10% bleach and 70% ethanol.2. Use aerosol-resistant tips and dedicated equipment.3. Ensure adequate UV exposure time; verify lamp output. |
The Scientist's Toolkit: Research Reagent Solutions
For researchers conducting sensitive nested PCR protocols, maintaining the integrity of reagents is critical. The following table details essential materials and their functions in contamination control.
Table: Essential Materials for Contamination Control in Nested PCR
| Item | Function | Application Note |
|---|---|---|
| HEPA Filter | Removes 99.97% of airborne particles ≥0.3 µm, creating the sterile work zone [39]. | The core component of a laminar flow hood; requires periodic replacement. |
| UVC Germicidal Lamp | Decontaminates the work surface by damaging microbial DNA/RNA between uses [41] [42]. | Used when the hood is unoccupied; not for real-time air sterilization. |
| Nuclease-Free Water | Free of RNases and DNases, preventing degradation of nucleic acids and reagents. | Essential for preparing PCR master mixes and dilutions. |
| Aerosol-Resistant Barrier Tips | Prevent pipette tip aerosols from contaminating the sample or the pipette shaft. | A first line of defense against cross-contamination between samples. |
| Surface Decontaminants | Inactivates nucleic acids and microbes on work surfaces and equipment. | A 10% sodium hypochlorite (bleach) solution is effective for destroying DNA amplicons. |
| UV-Durable Work Surface | Interior surfaces (e.g., stainless steel) resist degradation from prolonged UV exposure [41]. | Ensures the long-term structural integrity of the laminar flow hood. |
Experimental Protocol: Decontaminating a Nested PCR Workspace
This detailed protocol ensures a sterile environment for setting up nested PCR reactions, minimizing the risk of false positives.
Materials and Equipment
- Laminar flow hood (Vertical or Horizontal) with integrated UVC lamp
- 70% (v/v) Ethanol
- 10% (v/v) Sodium Hypochlorite (freshly diluted bleach)
- Nuclease-free wipes
- Personal Protective Equipment (lab coat, gloves, safety glasses)
Methodology
- Preparation: Turn on the laminar flow hood's blower and allow it to run for at least 15 minutes to purge particulate matter.
- Pre-Cleaning: While the blower is running, wipe down the entire work surface and any equipment (e.g., pipettes, tube racks) with 70% ethanol to remove gross contaminants.
- Nuclease Decontamination: After the ethanol has evaporated, wipe the surface with a fresh 10% bleach solution to hydrolyze any contaminating DNA, particularly persistent PCR amplicons.
- Final Wipe: Perform a final wipe with 70% ethanol to remove any residual bleach, which can corrode stainless steel and interfere with the PCR reaction.
- UV Sterilization: Place all pre-cleaned, non-plastic consumables (e.g., pipettes, tube racks) inside the hood. Close the sash or night cover. Ensure no one is in the room and activate the UVC lamp. Irradiate for a minimum of 30 minutes.
- Post-UV Setup: After the UV cycle is complete, turn off the lamp and allow the hood to ventilate for 2-3 minutes. You can now enter the room and begin setting up your nested PCR reactions aseptically within the clean, sterile environment.
The logical relationship between equipment function and contamination risk is summarized in the following cause-and-effect diagram.
Solving Practical Challenges: Optimization and Decontamination Strategies
A false positive in PCR is like a mirage in the desert—it leads you to believe in something that isn't there. Understanding your NTCs is the first step in distinguishing reality from illusion.
In the highly sensitive world of polymerase chain reaction (PCR) diagnostics, particularly in nested PCR protocols, the no-template control (NTC) serves as an essential sentinel against false positives. An NTC reaction contains all PCR components—master mix, primers, probes, and water—except for the template nucleic acid [43]. This control acts as a critical diagnostic tool, detecting contamination that could compromise experimental integrity and lead to erroneous conclusions in research and drug development.
For scientists working with nested PCR, where amplification products from the first round can easily contaminate the second, proper interpretation of NTCs becomes particularly crucial [26]. This guide will help you diagnose contamination sources through systematic NTC interpretation and implement effective corrective actions.
FAQ: Interpreting NTC Results and Troubleshooting Contamination
What does amplification in my NTC indicate?
Amplification in an NTC signifies that contamination has been introduced into your reaction. The specific pattern of amplification—both in terms of which wells show positivity and their corresponding Ct values—provides vital clues to the contamination source [44] [27].
- Consistent amplification across NTC replicates at similar Ct values typically points to contaminated reagents, as the same contaminated component is present in all reactions [44].
- Random amplification in some but not all NTCs with varying Ct values suggests random contamination events during plate setup, such as aerosol contamination or pipetting errors [44].
How can I distinguish between primer dimer and specific product amplification in an NTC?
Primer dimer formation is a common issue, particularly with SYBR Green chemistry [44]. To distinguish it from specific amplification:
- Analyze the melt curve: Primer dimers typically display a distinct peak at lower melting temperatures compared to the specific product [44].
- Observe amplification plots: Prior to dissociation curve analysis, primer dimers and specific products may appear similar in standard amplification plots [44].
- Optimize primer concentrations: Using suboptimal primer concentrations increases the likelihood of primer dimer formation [44].
Nested PCR presents unique contamination challenges due to the requirement for two separate amplification rounds and physical transfer of first-round products [26]. Key contamination sources include:
- Carryover contamination: From previously amplified PCR products in the laboratory environment [8] [14]
- Cross-contamination: Between samples during nucleic acid extraction or template addition [8]
- Contaminated reagents: One or more reaction components (master mix, water, primers) containing template nucleic acids [44]
- Environmental contamination: From plasmid clones or target organisms present in the laboratory environment [8]
The following table summarizes how to interpret different NTC amplification patterns and identifies likely contamination sources.
| NTC Amplification Pattern | Likely Contamination Source | Characteristics | Corrective Actions |
|---|---|---|---|
| Consistent amplification across replicates with similar Ct values [44] | Contaminated reagent | All NTC wells show amplification with minimal Ct variation | Replace all reagents systematically; use new aliquots |
| Random amplification in some wells with varying Ct values [44] | Random contamination during setup | Irregular amplification pattern; different Ct values | Improve pipetting technique; use aerosol barrier tips; implement clean workspace practices |
| Amplification with low melting temperature peak [44] | Primer-dimer formation | Distinct peak in melt curve at lower Tm | Optimize primer concentrations; improve reaction specificity |
| Amplification in specific workflow areas | Carryover contamination from amplicons | Correlated with personnel, equipment, or location | Implement physical workflow separation; use UNG/dUTP system; enhance decontamination protocols |
Experimental Protocols for Contamination Control
Implementing a Unidirectional Workflow
Establishing distinct physical areas for different PCR stages is fundamental to contamination control [14] [27] [45].
Detailed Methodology:
- Reagent Preparation Area: Dedicated clean space for preparing master mixes and aliquoting reagents. This area should be free of templates and amplified products [45]. Ideally, use a laminar flow cabinet equipped with UV light [45].
- Sample Preparation Area: Separate space for nucleic acid extraction and template addition to reaction mixes [45].
- Amplification Area: Designated location for thermal cyclers [45].
- Product Detection Area: Separate room for analyzing amplified products, ideally at a substantial distance from pre-amplification areas [14].
Critical Considerations:
- Maintain unidirectional workflow—personnel should not return to clean areas after working in post-amplification areas [45].
- Use dedicated equipment, lab coats, and supplies for each area [45].
- Implement separate air handling systems with appropriate pressure differentials (positive pressure in clean areas, negative in post-amplification areas) [45].
UNG Decontamination Protocol
The Uracil-N-Glycosylase (UNG) system provides enzymatic decontamination of carryover PCR products [8] [14] [27].
Procedure:
- Incorporation: Substitute dTTP with dUTP in PCR reactions, resulting in uracil-containing amplification products [14].
- Decontamination: In subsequent reactions, include UNG enzyme and incubate at room temperature for 10 minutes before PCR. UNG will cleave uracil-containing contaminants from previous reactions [14].
- Inactivation: Heat to 95°C for 5 minutes prior to PCR cycling to inactivate UNG and prevent degradation of new amplification products [14].
Limitations:
- Works best with thymine-rich amplification products [27].
- Reduced activity with G+C-rich targets [14].
- May not be completely inactivated in some conditions, potentially degrading new products [14].
Modified Single-Tube Nested PCR Protocol
To address the high contamination risk in conventional nested PCR, consider implementing a modified single-tube approach [46].
Methodology:
- Prepare reaction mix with outer primers and all standard PCR components [46].
- Immobilize inner primers on the inner side of the tube cap using appropriate adhesives [46].
- Perform first round of amplification with outer primers [46].
- Briefly centrifuge tube to dissolve inner primers into reaction mix [46].
- Perform second round of amplification with inner primers [46].
Advantages:
- Eliminates tube opening between amplification rounds [46].
- Reduces cross-contamination risk [46].
- Maintains high sensitivity of nested PCR while improving reliability [46].
The Scientist's Toolkit: Essential Reagents for Contamination Control
| Reagent/Equipment | Function | Application Notes |
|---|---|---|
| Uracil-N-Glycosylase (UNG) | Enzymatic degradation of carryover contamination | Most effective against T-rich amplicons; requires dUTP incorporation in previous PCR [14] [27] |
| Aerosol-resistant pipette tips | Prevent aerosol cross-contamination | Essential for all liquid handling; particularly crucial in sample preparation [45] |
| Sodium hypochlorite (bleach) | Surface decontamination through nucleic acid oxidation | Use 10-15% solution with 10-15 minute contact time; follow with ethanol rinse [14] [45] |
| UV light chamber | Nucleic acid sterilization through thymidine dimer formation | Ineffective for short (<300 bp) and G+C-rich templates; useful for sterilizing surfaces and equipment [8] [14] |
| dUTP nucleotide mix | Substitute for dTTP to create UNG-sensitive amplicons | Enables UNG decontamination system; may require optimization for specific targets [14] |
Effectively interpreting No-Template Controls requires both technical expertise and systematic laboratory practices. In nested PCR protocols, where contamination risks are magnified, implementing the diagnostic and procedural guidelines outlined above can significantly enhance result reliability. Remember that contamination prevention is always more effective than remediation—building robust workflows, maintaining disciplined practices, and systematically investigating NTC anomalies will protect the integrity of your research and development outcomes.
Systematic Decontamination Protocols for Reagents, Workspaces, and Equipment
Within the context of nested PCR protocols, the risk of contamination is exponentially magnified due to the high number of amplification cycles and the use of multiple primer sets. Contaminating DNA molecules, often originating from previous amplifications (amplicons) or the laboratory environment, can co-amplify with the target sequence, leading to false-positive results and a complete compromise of research integrity. This technical support center provides a focused guide to identifying, troubleshooting, and preventing the specific contamination challenges faced by researchers in nested PCR and sensitive molecular applications.
Core Principles of Contamination Control
A robust defense against contamination is built on a foundation of core operational principles. Diligent application of these practices is the most effective strategy for protecting the validity of your nested PCR experiments.
- Physical Separation of Work Areas: Maintain strictly separated pre- and post-PCR areas. These areas should be in different rooms with dedicated equipment, lab coats, and consumables. A one-way workflow must be enforced, meaning personnel should not move from post-PCR to pre-PCR areas on the same day [27].
- Meticulous Laboratory Technique: Always use aerosol-resistant filter pipette tips to prevent aerosol contamination [47] [27]. Change gloves frequently, especially when moving between different workstations or after handling potentially contaminated materials [47]. Open tubes carefully to avoid splashing and keep them capped as much as possible [27].
- Rigorous Use of Controls: Include multiple control reactions in every experiment to monitor for contamination. No Template Controls (NTCs) are essential; amplification in these wells indicates contamination of your reagents [27]. RT-negative controls help identify contamination from genomic DNA [47].
- Systematic Surface Decontamination: Regularly clean all work surfaces and equipment before and after use. A 10-15% fresh bleach (sodium hypochlorite) solution is highly effective for DNA degradation, but requires a 10-15 minute contact time and should be wiped down with de-ionized water afterwards [27]. Commercial DNA-decontaminating sprays are also available for rapid decontamination of surfaces [48].
Troubleshooting Common Contamination Issues
Use this guide to diagnose and address common contamination problems in your laboratory.
FAQ 1: My No Template Controls (NTCs) are showing amplification. What is the source of this contamination and how can I resolve it?
- Problem: Amplification in NTCs signals that one or more of your PCR reagents or the laboratory environment is contaminated with the target DNA sequence.
- Diagnosis: Observe the pattern of amplification in your NTCs. If all NTCs show amplification at a similar Ct value, the contamination is likely in a shared reagent (e.g., master mix, water, or primers). If amplification is random and at variable Ct values, the source is likely aerosol contamination in the lab environment or during pipetting [27].
- Solution:
- Replace Reagents: Discard all suspect reagents, particularly water and master mix. Always prepare and use reagents in small, single-use aliquots to prevent widespread contamination [27].
- Decontaminate Reagents: If the contamination persists, consider treating your reagents. DNase I treatment has been shown to be an effective method for eliminating contaminating DNA from PCR reagents while conserving PCR efficiency [49].
- Deep Clean: Perform a thorough decontamination of all work surfaces, equipment (especially centrifuges and vortexers), and pipettes using a fresh 10% bleach solution [27].
FAQ 2: After a nested PCR run, I get false-positive results even though my NTCs were clean. What could be causing this?
- Problem: False positives in samples with clean NTCs suggest sample-to-sample cross-contamination or contamination introduced during the sample processing stages (e.g., DNA extraction).
- Diagnosis: This is a common issue in nested PCR due to the high concentration of amplicons from the first round of amplification being carried over into the second round.
- Solution:
- Physical Barriers: Use a dedicated PCR workstation or hood with UV light for setting up reactions. UV irradiation can be used to decontaminate surfaces and equipment by damaging any residual DNA [50].
- Workflow Management: Ensure a strict one-way workflow from pre-PCR to post-PCR areas. Never open tubes containing the first-round PCR products in the same area where the second-round PCR is being set up [27].
- Enzymatic Prevention: Incorporate Uracil-N-Glycosylase (UNG) into your PCR protocol. By using dUTP instead of dTTP in the first-round PCR, all amplicons will contain uracil. UNG enzyme, added to the second-round master mix, will then degrade any carryover uracil-containing contaminants before PCR amplification begins, while leaving the natural thymine-containing sample DNA intact [27].
FAQ 3: My PCR efficiency is low, and I suspect my reagents or workspace are contaminated with nucleases. How can I address this?
- Problem: DNases or RNases can degrade your target nucleic acids or primers, leading to reduced sensitivity, false negatives, or complete PCR failure.
- Diagnosis: This is distinct from DNA contamination and is characterized by a gradual loss of signal or complete absence of amplification, even in positive controls.
- Solution:
- Use Nuclease-Inactivating Products: Employ surface decontaminants that are specifically formulated to destroy nucleases in addition to nucleic acids [48].
- Proper Storage and Handling: Always store reagents and enzymes at recommended temperatures. Use nuclease-free water and consumables, and work quickly on ice to minimize nuclease activity.
Experimental Protocols for Decontamination and Validation
Protocol: Surface and Equipment Decontamination
This protocol outlines a systematic method for decontaminating laboratory workspaces to remove DNA and nuclease contaminants [51] [50] [27].
- Materials:
- Personal Protective Equipment (PPE): Safety glasses, impervious gloves, lab coat [51].
- Disinfectant: Freshly diluted 10-15% household bleach (sodium hypochlorite) or EPA-approved disinfectant wipes (e.g., DisCide Ultra) or commercial DNA decontamination spray (e.g., PCR Clean) [51] [48] [27].
- Consumables: Paper towels or delicate wipers (e.g., Kimwipes) [51] [48].
- Hazardous waste bin for disposal [51].
- Methodology:
- Preparation: Put on appropriate PPE. If using a spray, moisten a paper towel with the decontamination solution; do not spray directly onto electronic equipment to avoid damage [51].
- Initial Cleaning: If surfaces are visibly soiled, clean first with soap and water to remove debris [51].
- Application: Wipe down all high-touch surfaces, including benchtops, micropipettes, instrument handles, door knobs, and the exterior of equipment [51] [52].
- Contact Time: Adhere to the manufacturer's recommended contact time for the disinfectant. For bleach, this is typically 10-15 minutes; for some commercial wipes, it can be as short as 30 seconds [51] [27].
- Rinsing (if required): If bleach was used, wipe the surface with de-ionized water after the contact time to prevent corrosion [27].
- Disposal: Dispose of used towels and gloves in a hazardous waste bin [51].
Protocol: Reagent Decontamination with DNase I
For hypersensitive PCR applications where commercial reagents may contain trace bacterial DNA, this method can be employed [49].
- Materials:
- PCR reagents (water, buffers)
- DNase I (RNase-free)
- EDTA or heat-inactivation solution
- Methodology:
- Treatment: Add DNase I to the reagent(s) requiring decontamination according to the enzyme manufacturer's specifications.
- Incubation: Incubate the mixture at a defined temperature (e.g., 37°C) for 30-60 minutes.
- Inactivation: Inactivate the DNase I by adding EDTA and/or heating to 65-75°C for 10-15 minutes. The specific inactivation method depends on the DNase I formulation.
- Validation: The decontaminated reagents must be tested for both the absence of contaminating DNA (via NTCs) and the preservation of PCR efficiency using a positive control with a known, low-copy-number target [49].
Protocol: Environmental Surveillance for Contamination Monitoring
Proactive monitoring of air and surfaces is critical for identifying contamination sources before they impact diagnostic results [50].
- Materials:
- Sterile swabs
- 0.9% sodium chloride solution
- Sterile tubes
- Open plates (for air sampling)
- Real-time PCR instrumentation and assay for a common contaminant (e.g., a 16S rDNA assay) or your specific nested PCR target.
- Methodology:
- Sampling:
- Analysis: Use 200 µL of the collected sample as a template in a real-time PCR reaction designed to detect the contaminant of concern [50].
- Interpretation: A positive PCR signal from an environmental sample confirms the presence and location of contamination, guiding targeted decontamination efforts.
Data Presentation
Comparison of Common DNA Decontamination Methods
The following table summarizes the efficacy and limitations of various methods used to decontaminate PCR reagents, as identified in comparative studies [49] [53].
| Method | Mechanism of Action | Efficacy | Key Limitations |
|---|---|---|---|
| DNase I Treatment | Enzymatic degradation of single- and double-stranded DNA | Effective in eliminating contaminating DNA while conserving PCR efficiency [49] | Requires careful inactivation; time-consuming; potential for reagent contamination during processing [49] |
| Restriction Endonuclease | Cleaves DNA at specific recognition sites | Failed to consistently eliminate contaminating bacterial DNA [49] | Inefficient for short, non-specific DNA fragments; requires specific sites [49] |
| UV Irradiation | Introduces thymine dimers, blocking polymerase | Inconsistent decontamination; fails to eliminate short DNA fragments effectively [49] [50] [53] | Efficiency depends on fragment size and is reduced by reagents; not completely reliable [49] [53] |
| 8-Methoxypsoralen | Intercalates and cross-links DNA upon UV exposure | Resulted in inhibition of the PCR reaction [49] | Can interfere with PCR efficiency; requires long-wave UV light [49] |
| Multi-Strategy (e.g., γ/UV + dsDNase) | Combined physical and enzymatic degradation | Highly effective for hypersensitive PCR, preserves PCR efficiency [53] | Complex, requires optimization of multiple treatment parameters [53] |
Research Reagent Solutions for Decontamination
This table details key reagents and materials essential for implementing an effective decontamination strategy.
| Item | Function | Example Use Case |
|---|---|---|
| Aerosol-Resistant Filter Tips | Prevents aerosolized contaminants from entering pipette shafts and cross-contaminating samples [47] [27] | Used during all pipetting steps, especially when setting up PCR master mixes and adding template DNA. |
| Uracil-N-Glycosylase (UNG) | Enzymatically degrades carryover contamination from previous uracil-containing PCR products [27] | Added to the PCR master mix; incubated prior to thermal cycling to destroy contaminants from earlier runs. |
| DNA Decontamination Spray | Ready-to-use solution for rapid degradation of DNA, RNA, and nucleases from surfaces [48] | Wiping down biosafety cabinets, benchtops, and equipment before and after PCR setup. |
| Sodium Hypochlorite (Bleach) | Chemical oxidation and degradation of nucleic acids [27] | Diluted to 10% for periodic deep-cleaning of non-corrosive surfaces, with a 10-15 minute contact time. |
| Ethanol (70-75%) | General disinfectant and cleaning agent; effective for surface decontamination but less so for DNA removal alone [50] [27] | Routine wiping of surfaces and equipment; used in air sprayers for room decontamination before cleaning [50]. |
Workflow for Systematic Decontamination
The following diagram illustrates the logical workflow for preventing, identifying, and responding to contamination in a nested PCR laboratory, integrating physical, procedural, and enzymatic controls.
Optimizing Primer and Template Volumes to Minimize Aerosol Risks
Core Concepts: Aerosols and Contamination in PCR
What are the primary aerosol risks in nested PCR? The most significant aerosol contamination risk in nested PCR is amplicon carryover contamination [8]. Nested PCR is particularly susceptible because it requires transferring the first-round amplification product to a second reaction tube, creating an opportunity for tiny, aerosolized droplets containing billions of copies of the target DNA to contaminate reagents, equipment, and subsequent reactions [54]. This can lead to false-positive results.
How do primer and template volumes relate to aerosol risk? While primer and template solutions themselves are not the main source of amplicons, improper pipetting techniques when handling these liquids can generate aerosols. Using smaller, optimized volumes reduces the potential liquid surface area and the amount of material that could be aerosolized during pipetting, thereby minimizing risk. Furthermore, optimizing volumes to avoid the need for repeated pipetting or tube opening directly reduces aerosol generation events [27].
Optimization Strategies for Volumes and Workflows
What are the recommended volumes for primer and template in PCR? Optimal volumes depend on the final concentration desired. The following table summarizes standard recommendations for a conventional PCR reaction, which forms the basis for each round of nested PCR [55]:
| Component | Stock Concentration | Typical Volume per 50 µL Reaction | Final Concentration |
|---|---|---|---|
| Template DNA (genomic) | Varies | 1-10 µL (50-250 ng total) | < 250 ng/reaction |
| Template DNA (plasmid) | Varies | 1 µL (1-10 ng total) | 1-10 ng/reaction |
| Forward Primer | 10 µM | 2.5 µL | 0.5 µM |
| Reverse Primer | 10 µM | 2.5 µL | 0.5 µM |
What is the single most effective workflow change to reduce aerosol risks? Adopting a single-tube nested PCR protocol is highly recommended. This advanced technique places both the outer and inner primer pairs in the same tube before amplification begins. The thermal cycler program is designed to use a high annealing temperature for the first round of amplification (with the outer primers) and a lower annealing temperature for the second round (with the inner primers) [56] [54]. This eliminates the need to open the reaction tube for the second round, thereby entirely preventing aerosol-mediated carryover contamination at this critical step [56].
The following workflow diagram contrasts the traditional and optimized single-tube approaches, highlighting the points of aerosol risk:
Frequently Asked Questions (FAQs)
Q1: My no-template control (NTC) shows amplification. What should I do? Amplification in your NTC indicates contamination. First, do not proceed with experiments until the issue is resolved [27]. Follow this systematic checklist:
- Replace all reagents, especially water and master mix components, with fresh aliquots.
- Decontaminate your workspace and equipment with a 10% bleach solution, followed by 70% ethanol, and use UV irradiation where available [8] [27].
- Verify your technique: Ensure you are using aerosol-resistant filter tips and that your pipettes are calibrated and decontaminated.
- Review lab workflow: Confirm that no one has moved from post-PCR areas to pre-PCR areas without changing lab coats and gloves [57].
Q2: Besides volume optimization, what other physical methods prevent aerosol contamination? Implementing strict physical separation of pre- and post-PCR activities is fundamental [8] [27] [57]. The ideal setup uses separate rooms for:
- Reagent Preparation and Reaction Setup
- Template Addition
- Amplification (Thermal Cycling)
- Post-Amplification Analysis
Each area should have dedicated equipment, lab coats, and supplies. A unidirectional workflow (from clean pre-PCR areas to dirty post-PCR areas) must be enforced to prevent amplicons from being carried back into clean spaces [27] [57].
Q3: Are there enzymatic methods to destroy contaminating amplicons? Yes, the Uracil-N-Glycosylase (UNG) system is highly effective. In this method, dTTP in the PCR master mix is replaced with dUTP. During amplification, all newly synthesized amplicons incorporate uracil instead of thymine. In subsequent PCR setups, the UNG enzyme is added to the reaction mix and incubated at room temperature before thermocycling. It will cleave any contaminating uracil-containing amplicons from previous runs. When the PCR starts, the initial denaturation step permanently inactivates UNG, allowing the new (also uracil-containing) target to amplify without interference [8] [27].
The Researcher's Toolkit: Essential Reagents & Equipment
The following table details key materials for implementing contamination-controlled nested PCR.
| Item | Function in Risk Reduction |
|---|---|
| Aerosol-Resistant Filter Pipette Tips | Creates a physical barrier preventing aerosols and liquids from contaminating the pipette shaft, a major source of cross-contamination [27]. |
| Uracil-N-Glycosylase (UNG) | Enzymatically degrades carryover contamination from previous PCR amplifications, as described in the FAQ above [8] [27]. |
| Aliquoted, High-Purity Reagents | Preparing single-use aliquots of water, buffers, dNTPs, and primers minimizes the number of times a stock vial is opened, protecting it from contamination [27]. |
| Laminar Flow Hood / PCR Workstation | Provides an ISO Class 5 (or cleaner) particulate-free work environment with HEPA/ULPA-filtered air for critical reagent mixing and reaction setup [57]. |
| 10% Bleach Solution & 70% Ethanol | Standard chemical decontaminants for work surfaces and equipment. Bleach degrades DNA, while ethanol cleans and evaporates quickly [8] [27]. |
| UV Crosslinker / Light Box | UV irradiation (254 nm) induces thymine dimers in exposed DNA, rendering contaminating nucleic acids unamplifiable. Useful for decontaminating surfaces, plastics, and some reagents [8]. |
| Single-Tube Nested PCR Primers | Specifically designed outer (long, high Tm) and inner (shorter, lower Tm) primer sets that enable the entire nested reaction to be performed in a single, sealed tube [56] [54]. |
Frequently Asked Questions (FAQs)
1. What are the main contamination risks associated with traditional nested PCR? Traditional nested PCR is highly prone to carryover contamination because it requires transferring the amplified product from the first PCR reaction to a second tube for the nested amplification. This tube-opening step can release millions of aerosolized copies of the target DNA into the laboratory environment, which can then contaminate reagents, equipment, and subsequent reactions, leading to false-positive results [27] [58] [5].
2. How do one-tube and semi-nested PCR formats reduce these contamination risks? These formats significantly reduce contamination by minimizing or eliminating physical handling of amplicons between amplification steps.
- One-Tube Nested PCR: All reaction components, including both outer and inner primers, are contained within a single tube. In the described immobilized primer method, the inner primers are physically separated (e.g., dried onto the tube cap) during the first round of amplification and are only mixed in after the first PCR is complete, without opening the tube [10].
- Semi-Nested PCR: This method uses three primers instead of four. One primer is used in both the first and second rounds of amplification, reducing the number of reagent additions and manipulations compared to a full nested protocol, thus lowering contamination opportunities [58].
3. Do these alternative formats compromise on sensitivity or specificity? No, when optimized, these formats can maintain, and sometimes even improve, the high sensitivity and specificity of traditional nested PCR.
- Sensitivity: The one-tube nested PCR was shown to detect as few as 10 copies of Dengue virus serotype 1, demonstrating high sensitivity [10]. The uninterrupted semi-nested PCR for Plasmodium falciparum was reported to maintain the sensitivity of the traditional nested method [58].
- Specificity: The use of two sets of primers that bind to the same genetic locus ensures high specificity. Off-target sequences amplified non-specifically in the first round are unlikely to be re-amplified in the second round because they lack the correct internal priming sites [5].
4. What are the key practical benefits of adopting these formats? The primary benefits are:
- Reduced False Positives: By minimizing carryover contamination, the risk of false-positive results is greatly diminished [10].
- Workflow Efficiency: These methods save time by reducing tube handling and the need for reagent transfers. The semi-nested PCR for malaria detection reduced total assay time to under two hours [58].
- Cost-Effectiveness: Using fewer reaction tubes and consumables lowers the cost per reaction [10].
- Suitability for Field Use: The simplified, closed-tube workflow makes these formats more adaptable for use in field settings or point-of-care devices [58] [10].
5. What are the critical steps for optimizing a one-tube or semi-nested PCR protocol? Optimization is crucial for success. Key parameters to optimize include:
- Primer Design and Concentration: Primers must be highly specific, and the concentration ratio between outer and inner primer sets often requires careful titration. A study on one-tube PCR used a 1:50 ratio of outer to inner primers [10].
- Cycling Conditions: Annealing temperatures and the number of cycles for each round must be adjusted. Some protocols use a "touchdown" approach in initial cycles to enhance specificity [18].
- Reaction Components: Concentrations of MgCl₂, dNTPs, and polymerase may need optimization, as demonstrated in the development of a nested PCR for Hepatitis E virus where only specific reagent combinations yielded successful amplification [38].
Troubleshooting Guides
Problem 1: No Amplification or Weak Band in One-Tube/Semi-Nested PCR
| Possible Cause | Solution |
|---|---|
| Insufficient primer solubilization (One-tube with immobilized primers) | Ensure the thermocycler pause and tube-inversion steps are performed correctly to fully dissolve the inner primers into the reaction mix [10]. |
| Suboptimal primer ratios | Titrate the ratio of outer to inner primers. A common starting point is a 1:50 ratio (e.g., 0.3 pmol outer : 15 pmol inner) [10]. |
| Inhibitors in the sample | Use a DNA polymerase with high processivity that is more tolerant of inhibitors [18], or further purify the template DNA. |
| Non-optimal cycling parameters | Adjust annealing temperatures. Consider a touchdown PCR protocol for the first few cycles to improve initial specificity [18]. |
Problem 2: Non-Specific Amplification or Primer-Dimer Formation
| Possible Cause | Solution |
|---|---|
| Primer-dimer formation during reaction setup | Use a hot-start DNA polymerase. Its activity is inhibited at room temperature, preventing non-specific amplification and primer-dimer formation during sample preparation [18]. |
| Inner primers participating in the first PCR round | For one-tube protocols, verify that the physical separation method (e.g., cap drying) is effective in preventing early access of inner primers. |
| Excessively low annealing temperature | Optimize the annealing temperature for both primer sets. Increase the temperature incrementally by 1-2°C [18]. |
Problem 3: Contamination is Still Observed
| Possible Cause | Solution |
|---|---|
| Laboratory layout and workflow issues | Establish physically separate pre- and post-PCR areas with dedicated equipment, lab coats, and consumables. Maintain a one-way workflow [27] [16]. |
| Contaminated reagents or equipment | Aliquot all reagents to avoid repeated freeze-thaw cycles and exposure to aerosols. Decontaminate work surfaces and equipment regularly with a 10% bleach solution, followed by 70% ethanol and deionized water [27] [59]. |
| Improper technique | Always use aerosol-filter pipette tips. Change gloves frequently. Handle tubes from the bottom or middle to avoid contaminating the cap. Mix contents slowly to prevent aerosol formation [27] [59]. |
Single-Tube Nested PCR for Dengue Virus Detection
This protocol adapts a traditional two-step nested RT-PCR into a single-tube format to reduce contamination [10].
- Primer Immobilization: Inner primers (15 pmol each) are immobilized onto the inner surface of the PCR tube cap by drying at 37°C.
- First-Round Reaction Setup: The PCR mixture is assembled in the tube containing:
- 10 mM Tris-HCl, 50 mM KCl, 1.5 mM MgCl₂, 0.1 mg/ml gelatin
- 0.2 mM each dNTP
- 0.3 pmol of each outer primer
- 2.5 U Taq DNA Polymerase
- Template DNA (1-2 µL)
- Amplification Profile:
- First Round: 15 cycles of: 92°C for 30 sec, 55°C for 1 min, 72°C for 1 min.
- Primer Solubilization: The thermocycler is paused at 92°C. Tubes are inverted several times to mix the inner primers into the reaction.
- Second Round: 45 cycles of: 92°C for 30 sec, 55°C for 1 min, 72°C for 1 min.
- Analysis: Products are analyzed by standard agarose gel electrophoresis.
Uninterrupted Semi-Nested PCR forPlasmodium falciparum
This protocol for malaria detection uses an asymmetric, semi-nested approach in a single tube to reduce assay time and contamination risk [58].
- Primer Design: Two sets of primers target the P. falciparum dihydrofolate reductase (DHFR) gene.
- Reaction Setup: All primers and reagents are added to a single tube at the beginning. The reaction uses a specialized buffer and a hot-start DNA polymerase.
- Amplification Profile: The thermocycling program is uninterrupted, with a first set of cycles for the initial amplification using the outer primer pair, immediately followed by a second set of cycles where the annealing temperature is shifted to favor the binding of the inner, nested primers.
- Detection: The amplicon is detected quantitatively using lateral flow strips with up-converting phosphor (UCP) reporter technology, making it suitable for point-of-care applications.
Quantitative Data Comparison
The table below summarizes performance data for different PCR formats, highlighting the effectiveness of alternative nested methods.
Table 1: Comparative Performance of Standard and Alternative Nested PCR Methods
| PCR Format | Application / Target | Reported Sensitivity | Key Advantage | Reference |
|---|---|---|---|---|
| Traditional Two-Step Nested PCR | Dengue Virus | 100 copies for all serotypes | Established reference method | [10] |
| Single-Tube Nested PCR | Dengue Virus | 10 copies (DENV-1), 100 copies (DENV-2, -3) | Reduced contamination risk; more cost-effective | [10] |
| Uninterrupted Semi-Nested PCR | Plasmodium falciparum | Comparable to traditional nested PCR | Reduced assay time (<2 hours); suitable for point-of-care | [58] |
| Nested PCR | HeLa Cell Contamination (HPV-18) | 1% contamination level (10x higher than STR profiling) | High sensitivity; uses culture supernatant directly | [60] |
Workflow Visualization
The following diagram illustrates the key procedural differences between traditional and single-tube nested PCR workflows, highlighting the steps where contamination risk is highest.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Materials for Contamination-Free Nested PCR
| Item | Function & Importance | Application Note |
|---|---|---|
| Hot-Start DNA Polymerase | Reduces non-specific amplification and primer-dimer formation by remaining inactive until the initial high-temperature denaturation step. | Critical for multiplex and one-tube protocols to prevent mispriming during reaction setup [18]. |
| Aerosol-Resistant Filter Pipette Tips | Creates a barrier against aerosols, preventing contamination of the pipette shaft and subsequent samples. | A first-line defense for all molecular biology work, especially when setting up pre-PCR mixes [27] [16]. |
| dNTPs with Uracil (dUTP) | Enables use of Uracil-N-Glycosylase (UNG) carryover prevention system. UNG degrades uracil-containing prior amplicons before PCR starts. | Most effective for preventing contamination from previous PCR products. Inactivated at high PCR temperatures [27]. |
| Dedicated Pre-PCR Reagents | Reagents (water, buffers, dNTPs) aliquoted for pre-PCR use only and stored separately from post-PCR areas. | Prevents contamination of stock solutions with amplified DNA. Aliquoting avoids repeated freeze-thaw cycles [27] [59]. |
| PCR Additives (e.g., DMSO) | Helps denature templates with high GC-content or complex secondary structure, improving amplification efficiency and specificity. | Often required for robust amplification of difficult targets. Note that it may lower the effective primer annealing temperature [18]. |
Developing a Laboratory-Wide Quality Assurance and Training Program
The exquisite sensitivity of nested Polymerase Chain Reaction (nPCR), capable of detecting a single molecule of DNA, is also its greatest vulnerability [9] [34]. This sensitivity makes it exceptionally prone to contamination, primarily from amplification products (amplicons) generated in previous reactions, which can lead to false-positive results and compromise diagnostic integrity or research conclusions [14] [61]. A single aerosolized droplet, created when opening a post-amplification tube, can contain up to 10^6 copies of amplicons, which can permeate the laboratory environment, contaminating reagents, equipment, and ventilation systems over time [14]. Establishing a robust Quality Assurance (QA) and training program is therefore not merely a best practice but a fundamental requirement for any laboratory relying on this powerful technique. The following guide provides a structured framework of troubleshooting guides, FAQs, and standardized protocols designed to systematically reduce contamination risks in nPCR workflows.
FAQs and Troubleshooting Guides
Frequently Asked Questions (FAQs)
Q1: What are the most common sources of contamination in a nested PCR lab? The most critical source is aerosolized amplicons from post-PCR analysis [9] [61]. Other key sources include: target template from cross-contamination of samples [9], contaminated reagents (especially water) [9], plasmid clones used for positive controls [14], and fomites such as laboratory coats, gloves, vortexers, and pipettes that carry contaminants from post-PCR to pre-PCR areas [9].
Q2: How can I tell if my nPCR assay is contaminated? The primary indicator is amplification in your No-Template Control (NTC) [27] [61]. An NTC contains all PCR reaction components—primers, reagents, enzyme—but uses nuclease-free water instead of a DNA template. The appearance of a PCR product in the NTC on an agarose gel confirms contamination. If the contamination is from a reagent, all NTCs will likely be positive with similar amplification efficiency; if it's random aerosol contamination, only some NTCs may be positive with varying signal strengths [27].
Q3: Our lab is small with only one room. How can we possibly separate pre- and post-PCR areas? While separate rooms are ideal, a single room can be adapted by using designated laminar flow hoods or PCR workstations equipped with UV lights for pre-PCR activities [9]. All pre-PCR setup should occur inside the hood. Establish a strict, unidirectional daily schedule: perform pre-PCR activities (reagent preparation, reaction setup) first, followed by amplification, and finally post-PCR analysis, with thorough cleaning between phases [9].
Q4: What is the most effective method for surface decontamination? A 10% bleach (sodium hypochlorite) solution is highly effective because it causes oxidative damage to nucleic acids, rendering them unamplifiable [27] [14]. Surfaces and equipment should be cleaned with 10% bleach, left for 10-15 minutes for the solution to work, and then wiped down with de-ionized water or ethanol to remove the bleach residue [27]. Note that bleach can corrode metal; for these surfaces, dedicated DNA decontamination solutions like DNA-away are suitable alternatives [61].
Q5: Are there inherent methods to make nPCR more contamination-resistant? Yes. Consider adopting modified single-tube nested PCR (Mo-STNPCR) protocols. In this format, both outer and inner primer pairs are present in the same tube from the start, with the inner primers physically separated (e.g., immobilized on the tube cap) and introduced only after the first round of amplification is complete. This eliminates the need to open the tube to add inner primers, drastically reducing the risk of carryover contamination [46].
Troubleshooting Guide for Common Contamination Issues
Table 1: Troubleshooting Common Nested PCR Contamination Problems
| Problem | Potential Causes | Corrective & Preventive Actions |
|---|---|---|
| Consistent NTC Amplification | Contaminated master mix reagent (water, buffer, primers, polymerase) [61]. | Systematically replace each reagent with a new, unopened aliquot and re-test the NTC to identify the contaminated source. Discard the contaminated reagent [61]. |
| Sporadic NTC Amplification | Aerosol contamination from amplicons in the lab environment; contaminated pipettes or lab coats [27]. | Decontaminate all surfaces and equipment with 10% bleach or DNA-away [27] [61]. Implement strict unidirectional workflow and use aerosol-filter tips for all liquid handling [9] [16]. |
| False Positives in Patient/Sample Controls | Sample-to-sample cross-contamination during DNA extraction or PCR setup [34]. | Use positive displacement tips or aerosol-filter barrier tips when pipetting template DNA. Always add the template last to the reaction mix. Centrifuge tubes briefly before opening [9]. |
| Loss of Sensitivity/Inhibition | Carryover of PCR inhibitors (e.g., residual bleach, phenol, SDS) from cleaning or DNA extraction [34]. | Ensure work surfaces are wiped with water or ethanol after bleach decontamination. Optimize DNA extraction protocols to remove inhibitors completely. Include a positive control to monitor assay sensitivity [34]. |
Standard Operating Procedures (SOPs) for Risk Reduction
Laboratory Workflow and Spatial Separation
The cornerstone of contamination prevention is the physical and temporal separation of the amplification process into discrete stages.
Diagram 1: Unidirectional workflow for contamination control.
Procedure:
- Dedicated Areas: Maintain physically separated rooms or designated zones for pre-PCR, amplification, and post-PCR activities [9] [27]. The post-PCR area must be located away from and downstream of the pre-PCR area.
- Unidirectional Workflow: Personnel and materials must move in one direction only: from pre-PCR to post-PCR. Never move equipment or samples from the post-PCR area back into the pre-PCR area [9] [16].
- Dedicated Equipment: Each area must have its own set of pipettes, tips, centrifuges, vortexers, lab coats, and waste containers. All equipment should be clearly labeled for their designated area [9] [27].
- Personal Protective Equipment (PPE): Wear dedicated lab coats and gloves in each area. Change them completely when moving between areas, especially when moving from a post-PCR to a pre-PCR area [27].
Chemical and Enzymatic Decontamination Protocols
A. Surface Decontamination with Bleach
- Application: Wipe down all work surfaces, pipettes, tube racks, centrifuges, and vortexers before and after PCR setup [27].
- Solution: 10% (v/v) sodium hypochlorite (bleach) in water [27] [14].
- Protocol: Apply the solution, allow it to remain wet on the surface for 10-15 minutes to ensure nucleic acid degradation, then wipe the surface with de-ionized water or 70% ethanol to remove corrosive residue [27]. Prepare fresh bleach solutions weekly as it degrades over time.
B. Pre-PCR Sterilization with Uracil-N-Glycosylase (UNG)
- Principle: This enzymatic method selectively destroys carryover contamination from previous PCRs [27] [14].
- Protocol:
- dUTP Incorporation: In all PCR setups, substitute dTTP in the master mix with dUTP. This results in all newly synthesized amplicons containing uracil instead of thymine [14].
- UNG Treatment: Include the UNG enzyme in the master mix of subsequent PCR reactions. During reaction setup and an initial incubation at room temperature (e.g., 10 minutes), UNG will recognize and catalyze the destruction of any uracil-containing DNA (i.e., carryover amplicons) [9] [14].
- UNG Inactivation: The initial denaturation step at 95°C in the thermal cycler permanently inactivates UNG, allowing the new, uracil-free target DNA to amplify without interference [14].
- Limitations: UNG is most effective on thymine (uracil)-rich sequences and may be less effective for GC-rich amplicons [14].
Modified Single-Tube Nested PCR (Mo-STNPCR) Protocol
This protocol, adapted from studies on leishmaniasis detection, minimizes the primary contamination risk in traditional nPCR [46].
Workflow:
- Primer Design: Design outer and inner primer pairs as for conventional nPCR.
- Reaction Assembly: In a single PCR tube, combine the DNA template, reaction master mix, and the outer primer pair. The inner primer pair is pre-dispensed and physically separated—for example, dried down on the inner wall of the tube or immobilized on the tube cap using a sugar matrix.
- First Amplification Round: Run the first-round PCR cycling program to amplify the target using the outer primers.
- Primer Mixing: Without opening the tube, perform a brief centrifugation step ("spin-down") to mix the inner primers into the main reaction mixture. This can be facilitated by a specialized thermal cycler or manual handling.
- Second Amplification Round: Immediately run the second-round PCR cycling program with the appropriate annealing temperature for the inner primers.
- Analysis: Open the tube only for post-PCR analysis in the designated contaminated area.
Advantages: This method bypasses the requirement for tube handling between amplification rounds, thereby eliminating a major source of carryover contamination and reducing the risk of false positives associated with conventional nPCR [46].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Essential Reagents and Materials for Contamination Control
| Item | Function & Importance in QA |
|---|---|
| Aerosol-Resistant Filter Pipette Tips | Prevents aerosols and liquids from contaminating the shaft of the pipette, a major vector for amplicon carryover. Essential for all pre-PCR pipetting [9] [27]. |
| Aliquoted Reagents | Dividing bulk reagents (water, buffer, dNTPs, enzyme) into single-use volumes prevents the contamination of an entire stock and reduces freeze-thaw cycles, preserving reagent integrity [9] [61]. |
| UNG Enzyme and dUTP | Key components of an enzymatic carryover prevention system. They are used together to selectively degrade PCR products from previous reactions [27] [14]. |
| Hot-Start DNA Polymerase | Remains inactive at room temperature, preventing non-specific amplification and primer-dimer formation during reaction setup. This enhances specificity and reduces potential background that can complicate analysis [18]. |
| 10% Bleach Solution / DNA Decontaminant | The primary chemical agent for surface and equipment decontamination. It irreversibly oxidizes and destroys contaminating nucleic acids [27] [14]. |
| Dedicated Lab Coats & Gloves | Acts as a physical barrier. Separate sets for pre- and post-PCR areas prevent the transfer of amplicons on clothing [9] [27]. |
| UV Light Chamber (UV Crosslinker) | Used to decontaminate surfaces, empty pipettes, and other non-plastic equipment within laminar flow cabinets before use. UV light induces thymine dimers in DNA, blocking polymerase elongation [9] [14]. |
Training Program and Quality Control Implementation
A successful program relies on trained personnel who understand and adhere to the protocols.
Core Training Modules
- Theory of Contamination: Educate all personnel on the sources and consequences of PCR contamination, emphasizing the stability and potency of aerosolized amplicons [14] [61].
- Hands-on SOP Training: Conduct practical sessions on the unidirectional workflow, proper use of dedicated equipment, and correct pipetting techniques to minimize aerosol generation.
- Troubleshooting Drills: Train staff to recognize contamination (e.g., NTC amplification) and execute the systematic troubleshooting guide to identify the source.
- Emergency Decontamination Protocol: Establish and train staff on a "worst-case scenario" protocol for a major contamination event. This includes shutting down the lab, discarding all working solutions, and performing a comprehensive decontamination of all surfaces and equipment before ordering new reagents [9].
Quality Control (QC) Measures
- Mandatory Controls: The use of NTCs and positive amplification controls in every run is non-negotiable for monitoring contamination and assay performance [27] [34].
- QC Logs: Maintain detailed records for reagent aliquoting, equipment maintenance, and surface decontamination.
- Audits: Perform regular audits of laboratory practices and workflow adherence to ensure compliance with the QA program.
Ensuring Assay Fidelity: Validation, Comparison with qPCR, and Case Studies
Core Concepts: Defining the Validation Pillars
What are the fundamental criteria for validating a nested PCR assay, and why are they critical? Establishing rigorous validation criteria is the cornerstone of reliable nested PCR. Three pillars—specificity, sensitivity, and reproducibility—are non-negotiable for ensuring your results are accurate, dependable, and meaningful, particularly in a context focused on contamination risk reduction.
- Specificity refers to the assay's ability to amplify only the intended target sequence without cross-reacting with non-target DNA, which is crucial for avoiding false positives in contaminated environments.
- Sensitivity defines the lowest quantity of the target that can be reliably detected by the assay. Highly sensitive methods can identify low-level contaminants but also risk amplifying contaminating DNA if not properly controlled.
- Reproducibility measures the assay's consistency, both within a single run (intra-assay) and across different runs, days, and operators (inter-assay). A robust, reproducible protocol is your first defense against variable results introduced by procedural errors or environmental contamination.
FAQs and Troubleshooting Guides
FAQ 1: My No-Template Controls (NTCs) are showing amplification. What is the likely cause and how can I resolve this? Amplification in your NTCs is a classic sign of contamination, most likely from amplicon carryover or contaminated reagents [27].
- Immediate Actions:
- Discard Reagents: Immediately discard all open reagents, especially water, primers, and master mix components [62].
- Decontaminate: Thoroughly clean all work surfaces, pipettes, and equipment with a fresh 10% bleach solution, followed by ethanol to remove the bleach residue [14] [27].
- Use Fresh Aliquots: Use new, single-use aliquots of all reagents for your next experiment [16].
- Long-Term Prevention:
- Enforce Physical Separation: Strictly maintain separate pre- and post-PCR laboratories with dedicated equipment, lab coats, and consumables [14] [16] [27]. A unidirectional workflow (from pre-PCR to post-PCR, never the reverse) is essential.
- Implement UNG Treatment: Incorporate Uracil-N-Glycosylase (UNG) into your PCR mix. This enzyme degrades any PCR products from previous reactions that contain dUTP (which you substitute for dTTP), preventing their re-amplification [14] [27].
FAQ 2: My assay's sensitivity is inconsistent between runs. How can I improve it? Inconsistent sensitivity often stems from variations in reaction efficiency or sample quality.
- Check Primer Performance: Verify that your primers are specific and efficient. Use in silico tools like Primer-BLAST for design and generate a standard curve to calculate amplification efficiency, which should ideally be between 90% and 110% [63].
- Optimize Reaction Conditions: Systematically optimize annealing temperatures using a thermal gradient cycler [63]. For nested PCR, ensure the annealing temperatures of the inner and outer primer sets are distinct to enable specific two-stage amplification [64].
- Control Sample Quality: Assess RNA quality spectrophotometrically and via gel electrophoresis. Treat samples with DNase to remove genomic DNA contamination that can interfere with accurate quantification [65] [62].
FAQ 3: How can I best design my experiment to ensure my results are statistically sound and reproducible? A robust experimental design accounts for both technical and biological variability.
- Incorplicate Appropriately: Include at least three biological replicates (samples from different origin) to account for biological variation, and at least two technical replicates (repeat measurements of the same sample) to account for pipetting and plate-based noise [63].
- Use a Dilution-Replicate Design: Consider using a dilution series for each sample instead of just identical replicates. This design allows for simultaneous estimation of PCR efficiency and initial template quantity within a single experiment, improving quantification accuracy and requiring fewer total reactions [66].
- Validate Reference Genes: Do not assume classic reference genes (e.g., GAPDH, ACTB) are stable under your experimental conditions. Use an algorithm like geNorm to validate their stability, selecting genes with an M value below 0.5 for homogeneous sample sets [63].
Detailed Experimental Protocols for Validation
Protocol for Determining Analytical Sensitivity and Specificity
This protocol outlines how to establish the limit of detection (LOD) for your assay and confirm its specificity.
Methodology:
- Standard Curve Preparation: Create a serial dilution of a known target template (e.g., plasmid DNA or synthetic gBlock). A typical 10-fold dilution series should cover a range from 10^6 to 10^0 copies/μL [63] [66].
- Testing for Sensitivity: Run each dilution level in replicates (n≥3) using your nested PCR protocol. The lowest concentration at which all replicates consistently amplify is your provisional LOD. Confirm this LOD in at least three independent runs.
- Testing for Specificity: Challenge your assay with templates from closely related non-target organisms or a panel of clinical samples known to be positive for other pathogens. No amplification should be observed from these non-target samples [64].
Expected Outcomes and Data Analysis:
- The standard curve will allow you to calculate the amplification efficiency (E) using the formula: E = 10^(-1/slope) - 1 [66].
- The LOD should be expressed as copy number per reaction. An example of high sensitivity is an LOD of 5 copies/reaction, as demonstrated in a multiplex one-tube nested RT-PCR for respiratory viruses [64].
Table 1: Example Sensitivity Data from a Validated mOTNRT-PCR Assay
| Target Virus | Correlation Coefficient (R²) | Amplification Efficiency | Limit of Detection (copies/reaction) |
|---|---|---|---|
| RSV | 0.997 | 98.5% | 5 |
| HRV | 0.994 | 95.7% | 5 |
| HMPV | 0.995 | 92.5% | 5 |
Source: Adapted from [64]
Protocol for Determining Reproducibility (Precision)
This protocol assesses the variability of your assay, both within a run and between runs.
Methodology:
- Sample Selection: Prepare three samples with target concentrations at high, medium, and low levels (e.g., near the LOD).
- Intra-assay Variability: Test each of the three samples in multiple replicates (n≥3) within a single PCR run.
- Inter-assay Variability: Test the same three samples in multiple replicates (n≥3) across three different PCR runs, performed on different days by different operators.
Expected Outcomes and Data Analysis:
- Calculate the mean Cq (Quantification Cycle) value and standard deviation (SD) for each sample set.
- Determine the coefficient of variation (CV = SD / mean Cq × 100%) for both intra- and inter-assay experiments. A CV of less than 5% is generally considered acceptable for a robust assay [64].
Table 2: Example Reproducibility Data from a Validated mOTNRT-PCR Assay
| Target | Concentration (copies/μL) | Intra-assay CV (%) | Inter-assay CV (%) |
|---|---|---|---|
| RSV | 10^2 | 1.52 | 2.15 |
| 10^4 | 0.87 | 1.33 | |
| 10^6 | 0.51 | 0.83 | |
| HRV | 10^2 | 2.95 | 3.67 |
| 10^4 | 1.64 | 2.41 | |
| 10^6 | 1.01 | 1.58 | |
| HMPV | 10^2 | 3.66 | 3.45 |
| 10^4 | 2.12 | 2.88 | |
| 10^6 | 1.45 | 1.96 |
Source: Adapted from [64]
Visualization of Workflows and Relationships
Nested PCR Experimental Workflow and Contamination Control
Uracil-N-Glycosylase (UNG) Amplicon Sterilization Mechanism
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents for Contamination-Reducing Nested PCR
| Reagent / Material | Function & Importance | Considerations for Use |
|---|---|---|
| UNG/dUTP System | Critical for carryover prevention; enzymatically destroys PCR amplicons from previous reactions. | Most effective for thymine-rich targets. Requires substitution of dTTP with dUTP in all reactions [14] [27]. |
| LNA-Modified Primers | Increases primer binding affinity (Tm), improving specificity and sensitivity, especially in one-tube nested formats. | Allows for a large Tm difference between outer and inner primers, enabling single-tube nested PCR and reducing contamination risk [64]. |
| Aerosol-Resistant Filter Pipette Tips | Creates a physical barrier preventing aerosols from contaminating the pipette shaft and subsequent samples. | Essential for all pre-PCR pipetting, especially when handling template DNA [16] [62]. |
| Fresh 10% Bleach Solution | Powerful chemical decontaminant; causes oxidative damage to nucleic acids, rendering them unamplifiable. | Must be made fresh frequently as it degrades. Follow with ethanol or water wipe to prevent equipment corrosion [14] [27]. |
| Predesigned & Validated Primers | Saves optimization time and ensures high, known amplification efficiency. | Verify that the validation conditions (species, sample type) match your experimental system [63]. |
| Aliquoted Reagents | Prevents repeated freeze-thaw cycles and cross-contamination of stock solutions. | Prepare single-experiment aliquots of all reagents (water, buffers, enzymes, primers) [16] [62]. |
Polymersse Chain Reaction (PCR) is a cornerstone technique in molecular biology, with nested PCR and quantitative real-time PCR (qPCR) being two pivotal methods for detecting target nucleic acids. While both offer high sensitivity, they present a different balance of benefits and challenges, particularly concerning contamination risk. This technical support center provides a detailed, evidence-based comparison of these two techniques. It offers troubleshooting guides and FAQs to help researchers, scientists, and drug development professionals implement robust protocols that maximize sensitivity while minimizing false positives due to contamination, directly supporting broader thesis research on contamination risk reduction.
Direct Comparison: Sensitivity and Contamination
The core differences between nested PCR and qPCR are summarized in the table below, which synthesizes data from controlled experiments.
Table 1: Head-to-Head Comparison of Nested PCR and qPCR
| Feature | Nested PCR | Quantitative PCR (qPCR) |
|---|---|---|
| Theoretical Sensitivity | Can achieve up to (10^{-6}) [67] | Can achieve up to (10^{-6}) or greater [67] |
| Demonstrated Sensitivity | (10^{-5}) dilution in a controlled cell dilution model [67] | (10^{-6}) dilution in the same controlled model [67] |
| Quantification Capability | No; qualitative (presence/absence) | Yes; absolute or relative quantification [67] |
| Turnaround Time | Longer; requires two amplification rounds and post-PCR gel electrophoresis [67] | Shorter; single-tube, closed-system amplification and detection [67] [27] |
| Major Contamination Risk | High; due to post-PCR handling for second round and gel analysis [67] [68] | Low; closed-tube system prevents amplicon release [67] [8] |
| Primary Contamination Source | Amplicon carryover from first-round product [8] [7] | Contaminated reagents or sample cross-contamination during setup [21] [27] |
| Key Contamination Control | Physical separation of pre- and post-PCR areas, UV irradiation, UNG (if dUTP is used) [7] [57] | UNG enzyme system, strict workflow controls, No Template Controls (NTCs) [21] [27] |
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: My No Template Control (NTC) is positive in my qPCR run. What should I do?
A positive NTC indicates contamination. The pattern of amplification can help identify the source [27]:
- Consistent Ct across all NTCs: Points to a contaminated reagent. You should replace all reagents, starting with the master mix and water.
- Random, variable Ct in NTCs: Suggests aerosol contamination during plate setup. Review your pipetting technique, use aerosol-filter tips, and decontaminate your workspace and equipment with fresh 10% bleach followed by 70% ethanol [21] [27].
- Systematic checking: Implement a "wipe test" to monitor surface contamination and use UV irradiation on consumables and workstations to inactivate contaminating DNA [7].
Q2: Why is my nested PCR sensitivity lower than expected, even though I am using a validated protocol?
Sensitivity in nested PCR is highly dependent on pre-amplification steps. Lower sensitivity can be attributed to:
- Inefficient RNA extraction or reverse transcription: The quality and integrity of your starting template are critical [67].
- Experimental model differences: Diluting cells (as in a "cells-in-cells" model) rather than purified RNA can more closely mimic in vivo conditions and yield a different sensitivity than a pure "RNA-in-RNA" dilution [67].
- Inactivation of critical reagents: Ensure Taq polymerase has not been degraded by repeated freeze-thaw cycles or contaminated.
Q3: How can I effectively prevent carryover contamination in nested PCR?
A multi-pronged "prevent and destroy" strategy is essential [7] [69]:
- Physical Separation: Use separate, dedicated rooms or laminar flow hoods for reagent preparation, sample preparation, the first PCR, the second PCR, and gel electrophoresis. Maintain a unidirectional workflow [7] [57].
- Chemical Decontamination: Routinely clean workspaces and equipment with 10% sodium hypochlorite (bleach), which causes oxidative damage to DNA, followed by 70% ethanol to remove the bleach [7] [27].
- Enzymatic Control (UNG): Incorporate dUTP instead of dTTP in your PCR master mix. Before each new amplification, treat the reaction with Uracil-N-Glycosylase (UNG), which will destroy any uracil-containing carryover amplicons from previous runs. The UNG is then inactivated during the initial denaturation step [7] [27].
Troubleshooting Common Scenarios
Table 2: Troubleshooting Common Problems
| Problem | Possible Causes | Recommended Solutions |
|---|---|---|
| False Positives in Nested PCR | Amplicon carryover from previous runs, contaminated pipettes, or cross-contamination between samples. | Implement strict unidirectional workflow, use dedicated equipment and labs coats for each area, and incorporate the UNG-dUTP system [7] [57]. |
| High Variation in qPCR Replicates | Inconsistent pipetting, poor sample mixing, or partial inhibition of the PCR reaction. | Calibrate pipettes, vortex and centrifuge all reagents before use, and include an internal positive control (IPC) to detect inhibition [21]. |
| Loss of Sensitivity in Nested PCR | Degraded primers or enzymes, suboptimal cycling conditions, or inefficient transfer of first-round product. | Aliquot and properly store enzymes, re-optimize primer annealing temperatures, and minimize dilution when transferring the first PCR product to the second reaction [67]. |
Experimental Protocols for Comparison
To objectively compare the performance of nested PCR and qPCR in your research, the following protocols, adapted from peer-reviewed studies, can be implemented.
Protocol: Sensitivity Comparison Using a Cell Dilution Model
This controlled experiment is designed to empirically determine the sensitivity limit of each method [67].
1. Sample Preparation:
- Create a standard curve via serial 10-fold dilutions of BCR-ABL-positive K562 cells into BCR-ABL-negative NB4 cells. A typical range is from (10^{-3}) to (10^{-7}) [67].
- Include patient samples (e.g., bone marrow or peripheral blood from CML patients) and negative controls.
2. Nucleic Acid Extraction:
- Extract total RNA from all samples and cell line dilutions using a commercial kit (e.g., QIAamp RNA Blood Mini Kit).
- Synthesize cDNA using a reverse transcription kit (e.g., GeneAmp Gold RNA PCR Core Kit) with 1 µg of total RNA as input.
3. Parallel Amplification:
- Nested PCR: Perform the first round of PCR using outer primers (e.g., BCR-b1-A and ABL-a3-B). Then, use a small aliquot (e.g., 1 µL) of the first-round product as a template for the second round with inner primers (e.g., BCR-b2-C and ABL-a3-D). Analyze the final product on a 2% agarose gel [67].
- qPCR: Perform amplification in a real-time PCR system using TaqMan probes and primers specific for the target (e.g., BCR-ABL) and a control gene (e.g., ABL). Use both absolute quantification (with a standard curve) and relative quantification (ΔΔCt method) [67].
4. Analysis:
- The last dilution that yields a reproducible positive signal determines the sensitivity limit for each method.
- Compare the results, noting the dilution factor at which each method fails to detect the target.
Protocol: Assessing Contamination Rates
This protocol helps monitor and quantify contamination in your laboratory setup.
1. No Template Controls (NTCs):
- Include multiple NTCs in every PCR run. For qPCR, distribute them across the plate to detect aerosol contamination [70] [27].
- For nested PCR, include NTCs in both the first and second rounds to pinpoint the stage of contamination.
2. Environmental Monitoring:
- Regularly perform "wipe tests" by swabbing bench surfaces, pipettes, and equipment with a moistened swab and then using the swab as a template in a sensitive PCR assay [69].
- Use UV irradiation (254-300 nm) on PCR workstations, consumables, and reagents for 5-20 minutes before starting reactions to inactivate contaminating DNA [7].
Workflow Visualization
The diagrams below illustrate the procedural steps and inherent contamination risks of each PCR method.
The Scientist's Toolkit: Essential Reagents & Materials
Table 3: Key Research Reagent Solutions for PCR Methods
| Item | Function in Experiment | Example Product/Brand |
|---|---|---|
| RNA Extraction Kit | To isolate high-quality, intact total RNA from cell lines or patient samples. | QIAamp RNA Blood Mini Kit (QIAGEN) [67] |
| Reverse Transcription Kit | To synthesize stable cDNA from RNA templates for subsequent PCR amplification. | GeneAmp Gold RNA PCR Core Kit (Applied Biosystems) [67] |
| Taq DNA Polymerase | The enzyme that catalyzes the synthesis of new DNA strands during PCR. | AmpliTaq Gold (Applied Biosystems) [67] |
| dNTP/dUTP Mix | The building blocks (A, C, G, T/U) for DNA synthesis. dUTP allows for UNG-based carryover prevention. | dUTP-containing dNTP mix [7] [27] |
| Uracil-N-Glycosylase (UNG) | An enzyme used pre-amplification to degrade contaminating uracil-containing amplicons from previous runs. | Heat-labile UNG (often included in master mixes) [7] [27] |
| TaqMan Probe & Primers | For qPCR; a sequence-specific fluorescent probe and primers that enable real-time detection and quantification. | Assays-on-Demand (Applied Biosystems) [67] |
| Laminar Flow Hood / PCR Workstation | Provides a clean, HEPA/ULPA-filtered airflow workspace to protect samples from environmental contamination during setup. | Sentry Air Portable Clean Rooms [57] |
The association between the periodontal pathogen Porphyromonas gingivalis and atherosclerotic cardiovascular disease is a significant area of research. A critical step in establishing this link is the robust detection of the bacterium within complex human atherothrombotic plaques. These plaques present a substantial technical challenge for molecular detection due to their highly calcified nature, the presence of PCR inhibitors, and the typically low bacterial load. This case study examines how the application of a nested PCR protocol significantly enhanced detection sensitivity for P. gingivalis in these challenging samples, and provides a technical support framework for researchers implementing this method.
Experimental Protocol & Workflow
The following protocol is adapted from the methodology that successfully increased the detection rate of P. gingivalis in highly calcified atherothrombotic plaques by 22.2% compared to direct real-time PCR [71] [72].
Sample Preparation and DNA Extraction
- Sample Source: Human carotid, coronary, or aneurysmal atherothrombotic plaques.
- Storage: Samples should be immediately frozen after collection and stored at -70°C or lower until processing [72].
- Homogenization: Mechanically homogenize the plaque tissue to lyse cells and release microbial DNA. This step is critical for calcified tissues [72].
- DNA Extraction: Use a commercial DNA extraction kit suitable for tough tissues (e.g., Qiagen DNeasy Blood & Tissue Kit or equivalent). Ensure the protocol includes steps to remove PCR inhibitors common in vascular tissues.
Nested PCR Amplification
The protocol involves two successive amplification rounds using two sets of primers targeting the P. gingivalis-specific 16S rRNA gene [71].
First Round PCR (External Primers)
- Reaction Mix:
- Template DNA: 1-2 µL
- External Forward and Reverse Primers (each): 0.2 µM final concentration
- dNTP mix: 200 µM of each dNTP
- 10x PCR Buffer: 1x final concentration
- MgCl₂: 1.5-2.0 mM final concentration
- Taq DNA Polymerase: 1.25 U
- Sterile Ultra-Pure Water: to a final volume of 25 µL
- Thermal Cycling Conditions [54]:
- Initial Denaturation: 94°C for 2 minutes
- 30-35 Cycles of:
- Denaturation: 94°C for 30 seconds
- Annealing: 45-60°C (optimize based on primer Tm) for 30 seconds
- Extension: 72°C for 1 minute
- Final Extension: 72°C for 5 minutes
- Hold: 4°C
Second Round PCR (Internal/Nested Primers)
- Template: Dilute the first-round PCR product (e.g., 1:10 to 1:100) and use 1-2 µL.
- Reaction Mix: Identical to the first round, but replace the external primers with the internal primer set.
- Thermal Cycling Conditions: Use the same cycling protocol as the first round.
Analysis of Results
- Analyze PCR products using agarose gel electrophoresis.
- The second round should yield a more intense and specific band of the expected size.
- For absolute confirmation, Sanger sequencing of the amplified product can be performed.
Workflow Diagram
The diagram below illustrates the key stages of the nested PCR protocol and its critical control points for contamination prevention.
Key Research Reagent Solutions
The table below details the essential reagents and materials required for the nested PCR protocol, along with their specific functions.
| Reagent/Material | Function in the Protocol | Specification/Note |
|---|---|---|
| Plaque Sample | Source of target P. gingivalis DNA | Highly calcified; store at -70°C [72] |
| External Primers | First amplification of target 16S rRNA gene | Designed for P. gingivalis specificity [71] |
| Internal Primers | Second, nested amplification | Bind within the first amplicon; enhance specificity [71] [20] |
| Taq DNA Polymerase | Enzymatic DNA amplification | Thermostable; 1.25U per 25 µL reaction [54] |
| dNTP Mixture | Building blocks for new DNA strands | 200 µM of each dNTP in final reaction [54] |
| MgCl₂ Solution | Cofactor for polymerase activity | Optimized concentration of 1.5-2.0 mM [54] |
| PCR Buffer | Provides optimal reaction conditions | Includes KCl and Tris-HCl at pH 8.8 [54] |
Troubleshooting Guides & FAQs
Frequently Asked Questions (FAQs)
Q1: Why is nested PCR particularly advantageous for detecting P. gingivalis in atherothrombotic plaques compared to standard PCR?
A: Nested PCR provides significantly enhanced sensitivity and specificity, which is crucial for challenging samples like calcified plaques where the bacterial load is low and PCR inhibitors are present. The two successive amplification rounds and the use of a second primer set that binds within the first product drastically reduce non-specific amplification and false positives, allowing for the detection of even a few copies of the target DNA [71] [20] [73].
Q2: What is the single greatest contamination risk in nested PCR, and how can it be mitigated?
A: The greatest risk is carryover contamination during the transfer of the first-round PCR product to the second reaction tube. This can be mitigated by:
- Physical Separation: Performing reagent preparation, the first PCR, and the second PCR in different, dedicated rooms or workstations.
- Use of Aerosol-Resistant Filter Tips: For all liquid handling steps.
- Unidirectional Workflow: Moving from "clean" pre-PCR areas to "dirty" post-PCR areas without backtracking [54] [73].
Q3: Are there modifications to the standard nested PCR that can reduce the contamination risk?
A: Yes, single-tube (one-tube) nested PCR is a modification where both amplification rounds are performed in the same sealed tube. The inner primers are designed with a lower annealing temperature than the outer primers. The reaction starts with a high annealing temperature for the outer primers, followed by a lower temperature for the inner primers, eliminating the need for tube opening and transfer [54] [58].
Troubleshooting Guide
| Problem | Potential Cause | Solution |
|---|---|---|
| No PCR product in either round | Inhibitors co-purified with DNA from plaque. | Dilute the template DNA, use a DNA clean-up kit, or add PCR facilitators like BSA. |
| Inefficient cell lysis due to calcification. | Optimize mechanical homogenization of the plaque tissue [72]. | |
| Strong band in first round, no band in second round | Primer dimers or non-specific products in the first round. | Optimize the first-round annealing temperature and cycle number. Dilute the first-round product more (e.g., 1:100) for the second round [54]. |
| Inefficient inner primers. | Re-design and validate the internal primer set. | |
| Non-specific bands or smearing on the gel | Excessive number of cycles leading to non-specific binding. | Reduce the number of cycles in both PCR rounds (e.g., to 25-30) [20]. |
| Too much template or enzyme in the reaction. | Titrate the amount of template DNA and ensure the correct Taq polymerase concentration is used [54]. | |
| High background contamination in negative controls | Contaminated reagents or amplicon carryover. | Prepare fresh reagents, use new aliquots, decontaminate workspaces with UV light, and strictly enforce physical separation of pre- and post-PCR areas [73]. |
The following table quantifies the performance enhancement achieved by the nested PCR protocol for P. gingivalis detection in vascular samples, as reported in the foundational study.
| Detection Method | Key Performance Metric | Outcome in Atherothrombotic Plaques | Application Context |
|---|---|---|---|
| Direct Real-time PCR | Detection Rate | Baseline | Standard method; can be limited by inhibitors and low target concentration [71] [72]. |
| Nested PCR Protocol | Detection Rate | Increased by 22.2% | Superior for complex, inhibitor-rich samples like calcified plaques [71] [72]. |
| Nested PCR Protocol | Specificity | Good Specificity Maintained | Reduced false positives due to two primer sets binding to the correct target [71] [20]. |
Technical Support Center
Frequently Asked Questions (FAQs) and Troubleshooting Guides
1. Question: Our nested PCR for Acanthamoeba detection is producing inconsistent results between replicates. What could be causing this?
Answer: Inconsistent results typically indicate contamination or reagent degradation. Implement these specific measures:
- Spatorial Separation: Establish three physically separated work areas: (1) pre-PCR reagent preparation, (2) sample preparation and DNA addition, and (3) post-PCR analysis [8] [14]. Traffic must flow unidirectionally from clean to contaminated areas.
- UNG Contamination Control: Incorporate uracil-N-glycosylase (UNG) into your PCR master mix. Use dUTP instead of dTTP in all reactions. UNG will degrade any contaminating amplicons from previous reactions (which contain dUTP) but not your native DNA template [8] [14]. Incubate reactions with UNG at room temperature for 10 minutes before the thermal cycling starts.
- Surface Decontamination: Routinely clean all work surfaces, equipment, and pipettes with 10% sodium hypochlorite (bleach), followed by 70% ethanol to remove any residual bleach [8] [14].
- UV Irradiation: Expose reagents (except enzymes, primers, and DNA templates) and plasticware to UV light (254 nm) for 5-20 minutes in a UV crosslinker or light box to degrade contaminating DNA [8] [14].
2. Question: We suspect our negative controls are giving false positives. How can we confirm and resolve amplification product carryover contamination?
Answer: Follow this "Detect and Destroy" strategy:
- Detection: Run a series of negative controls including a no-template control (water instead of DNA) and a sample processing control (all reagents without sample). If these amplify, contamination is confirmed [69] [34].
- Destroy with UNG: The most effective method is using the UNG system described above, which enzymatically destroys carryover contaminants before amplification begins [14].
- Switch to Closed-Tube Systems: Consider migrating to real-time PCR methods that detect amplification products in a closed-tube system, eliminating post-PCR handling and significantly reducing contamination risk [8] [14].
- Laboratory Purge: If contamination is widespread, implement a laboratory shutdown for comprehensive decontamination: discard all open reagents, thoroughly clean all surfaces and equipment with bleach, and use UV irradiation in all work areas [69].
3. Question: Our Acanthamoeba genotyping PCR fails to detect certain known genotypes. Are there primer design limitations we should consider?
Answer: Yes, this is a recognized limitation with standard JDP primers. Research has identified specific genotype detection gaps:
- The commonly used JDP1 and JDP2 primer set cannot successfully align with genotypes T7, T8, T9, T17, and T18 [74].
- Solution - Optimally Modified Primers: Implement the "Optimal Modified Genotyping Nested PCR" method. This uses:
- Outer Primers: Common free-living amoeba (FLA) primer set (ComFLA F/R) that aligns with all Acanthamoeba genotypes [74].
- Inner Primers: A modified primer set (AcanF900 + JDP2-M) where the JDP2-M primer contains a strategic nucleotide change (position 15 from A to R [A/G]) to enable alignment with all genotypes, including T7, T8, T9, T17, and T18 [74].
4. Question: What is the optimal sample processing method for concentrating Acanthamoeba from large volume water samples while minimizing PCR inhibitors?
Answer: Follow this validated protocol for reliable results:
- Filtration: Filter 1L of water sample sequentially through 200μm mesh to remove large debris, then through a 0.22μm pore-size polycarbonate membrane to capture Acanthamoeba cysts and trophozoites [75].
- DNA Extraction: Use a commercial DNA extraction kit (e.g., ZymoBIOMICS DNA Miniprep Kit) for consistent yield and purity. This method is more effective than traditional phenol-chloroform extraction and reduces exposure to inhibitory substances [75].
- Inhibition Check: Include an internal control in your PCR reactions to detect potential inhibition from co-concentrated substances in environmental samples.
Detailed Methodology: Optimal Modified Genotyping Nested PCR for Acanthamoeba
This protocol significantly enhances detection sensitivity and genotype coverage compared to standard JDP-PCR [74].
Primer Sequences and Specifications
| Primer Name | Sequence (5' → 3') | Length (bp) | Undetected Genotypes | Role |
|---|---|---|---|---|
| ComFLA F (Outer) | CGC GGT AAT TCC AGC TCC AAT AGC | 980-1090 | None | Outer forward primer |
| ComFLA R (Outer) | CAG GTT AAG GTC TCG TTC GTT AAC | 980-1090 | None | Outer reverse primer |
| AcanF900 (Inner) | CCC AGA TCG TTT ACC GTG AA | 440-550 | None | Inner forward primer |
| JDP2-M (Inner) | TCT CAC AAG CTG CTR GGG GAG TCA | 440-550 | None | Modified inner reverse primer |
Protocol Steps
- First Round PCR (Outer Amplification)
- Reaction Mix: 1X PCR buffer, 2.5mM MgCl₂, 0.4mM dNTPs, 0.4μM each outer primer (ComFLA F/R), 1.25U DNA polymerase, 2μL template DNA, nuclease-free water to 25μL.
- Cycling Conditions: Initial denaturation 95°C for 5 min; 40 cycles of 95°C for 30s, 55°C for 30s, 72°C for 1min; final extension 72°C for 7min.
Second Round PCR (Nested Amplification)
- Reaction Mix: Same as above but with inner primers (AcanF900/JDP2-M) and 1μL of 1:100 diluted first-round product as template.
- Cycling Conditions: Same as first round.
Product Analysis
- Analyze 5μL of nested PCR product on 1.5% agarose gel stained with ethidium bromide.
- Expected band: 440-550bp fragment.
- For genotyping: Purify PCR product and perform Sanger sequencing.
Comparative Performance of Acanthamoeba Detection Methods
Table 1: Comparison of Six PCR Methods for Acanthamoeba Detection in Aquatic Samples [74]
| Method Name | Primers Used | Detection Length (bp) | Undetected Genotypes | Relative Sensitivity |
|---|---|---|---|---|
| JDP-genotyping PCR (M1) | JDP1 + JDP2 | 440-550 | T9, T17, T18 | Reference standard |
| Optimal Modified Genotyping Nested PCR (M3) | ComFLA F/R (outer) + AcanF900/JDP2-M (inner) | 440-550 | None | Significantly higher |
| Genotyping Nested PCR (M2) | ComFLA F/R (outer) + JDP1/JDP2 (inner) | 440-550 | T7, T8, T9, T17, T18 | Higher than M1 |
| Qvarnstrom Real-time PCR (M6) | AcanF900 + JDP2 | N/A | None | Higher than M1 |
Table 2: Acanthamoeba Prevalence in Different Aquatic Environments
| Environment Type | Location | Detection Rate | Predominant Genotype | Citation |
|---|---|---|---|---|
| Rivers/Reservoirs/River Basin | Taiwan | Variable (underestimated by JDP-PCR) | T4 | [74] |
| Freshwater River Systems | Taichung, Taiwan | Detected at multiple sites | Not specified | [75] |
| Beach Wet Sand | Phuket, Thailand | 100% (21/21 samples) | T5 (83.9%) | [76] |
| Beach Dry Sand | Phuket, Thailand | 52.4% (11/21 samples) | T5 (83.9%) | [76] |
| Beach Seawater | Phuket, Thailand | 14.3% (3/21 samples) | T5 (83.9%) | [76] |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Acanthamoeba Genotyping
| Reagent/Material | Function/Application | Specific Examples/Considerations |
|---|---|---|
| Polycarbonate Filters (0.22μm) | Concentration of Acanthamoeba from large water samples | Compatible with filtration systems for 1L water samples [75] |
| DNA Extraction Kit | Isolation of high-quality genomic DNA | ZymoBIOMICS DNA Miniprep Kit effectively removes PCR inhibitors [75] |
| dUTP/dTTP Mixture | Incorporation into amplicons for UNG-based contamination control | Use dUTP instead of dTTP or in combination; requires optimization [14] |
| Uracil-N-Glycosylase (UNG) | Enzymatic destruction of contaminating amplicons | Add to PCR master mix; incubate at room temperature before thermal cycling [8] [14] |
| Optimally Modified Primers | Comprehensive genotype coverage | JDP2-M with R (A/G) substitution at position 15 enables detection of all genotypes [74] |
| PCR Master Mix with MgCl₂ | Provides optimal buffer conditions and magnesium concentration | 3mM MgCl₂ concentration used in successful protocols [75] |
Workflow Visualization
Nested PCR Laboratory Workflow
UNG Contamination Control Mechanism
Defining the Ideal Application Niche for Nested PCR in Modern Molecular Labs
Core Principles and Applications of Nested PCR
Nested Polymerase Chain Reaction (PCR) is a powerful modification of the standard PCR technique designed to significantly enhance the sensitivity and specificity of nucleic acid amplification. This method involves two successive rounds of amplification using two distinct sets of primers [1].
The foundational principle of nested PCR relies on the use of an initial set of "outer primers" that amplify a larger fragment of the target gene. The product from this first amplification round then serves as the template for a second round of PCR, which uses a set of "inner primers" (or nested primers) that bind to a sequence internal to the first amplicon [1]. This two-step process substantially reduces non-specific amplification because the nested primers are unlikely to find binding sites on any primer dimers or non-specific artifacts generated during the primary PCR [1].
The primary advantage of this approach is a dramatic increase in assay sensitivity and specificity, making it particularly useful for suboptimal nucleic acid samples or when the target organism is present in very low quantities [77] [1]. Consequently, nested PCR has found its ideal application niche in several key areas of modern molecular biology and diagnostics:
- Detection of Low-Abundance Pathogens: It has proven invaluable for detecting microorganisms present in very low concentrations in clinical samples, such as Rickettsia, Bartonella, Mycobacterium tuberculosis, herpesvirus, and enteroviruses [1].
- Analysis of Suboptimal Samples: It is particularly effective for nucleic acids extracted from formalin-fixed, paraffin-embedded (FFPE) tissue, where DNA quality may be compromised [1].
- Cell Line Authentication: It provides a rapid, sensitive method for detecting low-level cell cross-contamination, such as identifying HeLa cell contamination in cell cultures with 10-fold higher sensitivity than Short Tandem Repeat (STR) profiling [60].
- Highly Sensitive Multiplex Detection: Advanced formats like multiplex one-tube nested real-time RT-PCR enable simultaneous detection of multiple respiratory viruses (RSV, HRV, HMPV) with extremely high sensitivity [64].
Troubleshooting Guide: FAQs for Nested PCR Experiments
No or Low Amplification Product
Q: I have followed the nested PCR protocol, but I am not seeing any product or the yield is very low after the second round. What could be wrong?
This common issue can stem from problems in either the first or second round of amplification. The following table summarizes the potential causes and solutions:
| Cause | Solution |
|---|---|
| PCR reagents omitted or inactive | Repeat the reaction, ensuring all components are added. Include a positive control to verify component functionality [3]. |
| Poor primer design or efficiency | Redesign primers following optimal characteristics: length of 15-30 bases, 40-60% GC content, and 3' ends containing a G or C to prevent "breathing" [78]. |
| Insufficient number of PCR cycles | Increase the number of cycles by 3-5 cycles at a time, up to a maximum of 40 cycles, to overcome issues with low-abundance templates [3]. |
| Suboptimal cycling conditions | Lower the annealing temperature in increments of 2°C or increase the extension time [3]. |
| PCR inhibitors in the template | Dilute the template or purify it using a commercial clean-up kit. Alternatively, use a DNA polymerase with higher tolerance to impurities [3]. |
| Insufficient template | Increase the amount of template. For genomic DNA, use 1 ng–1 μg per 50 μL reaction; for plasmid DNA, use 1 pg–10 ng [78] [79]. |
Non-Specific Bands or Smearing
Q: My final nested PCR product shows multiple unexpected bands or a smear on the agarose gel. How can I improve specificity?
Non-specific amplification is a frequent challenge, but the nested PCR format offers inherent advantages in overcoming it. If non-specific products persist, consider these solutions:
| Cause | Solution |
|---|---|
| Primers binding non-specifically | Use BLAST alignment to check primer specificity. Redesign primers if the 3' ends are complementary to non-target sites [3]. |
| PCR conditions not stringent enough | Increase the annealing temperature incrementally by 2°C. Use touchdown PCR or reduce the number of PCR cycles [3]. |
| Excessive template amount | Reduce the amount of starting template by 2- to 5-fold [3]. |
| Primer dimer formation | Utilize a hot-start DNA polymerase to inhibit enzyme activity at room temperature, preventing mispriming and primer-dimer formation during reaction setup [6]. |
| Long annealing time | For certain polymerases, using a short annealing time (5–15 seconds) during three-step PCR is essential for specific amplification [3]. |
PCR Contamination (False Positives)
Q: My negative controls are showing amplification, indicating contamination. How did this happen, and how can I address it?
Contamination is a major risk in nested PCR due to its high sensitivity and the need to transfer first-round products [1]. The most common source is "carryover contamination" from amplified PCR products (amplicons) from previous experiments [3] [8]. A single PCR can generate up to 10^8 copies of the target sequence, creating a significant contamination risk if not properly contained [8].
Decontamination Strategies:
- Chemical Decontamination: Clean work benches and surfaces with a 10% sodium hypochlorite (bleach) solution, followed by 70% ethanol to remove residual bleach. Note that bleach may damage metal and plastic parts of pipettes over time [33] [8].
- UV Irradiation: Expose reagents (except those containing template) and equipment to UV light (254 nm) for 5-20 minutes. UV light induces thymidine dimers in DNA, rendering contaminating amplicons unamplifiable [8].
- Enzymatic Control (UNG System): Incorporate the dUTP/UNG (Uracil-N-Glycosylase) system. In this method, dUTP is used in place of dTTP during PCR, making all amplicons contain uracil. Before the next PCR, treatment with UNG enzyme degrades any contaminating uracil-containing amplicons, which is then inactivated during the initial denaturation step [8].
Contamination Troubleshooting Pathway: This diagram outlines a logical workflow for responding to and resolving suspected PCR contamination, guiding from initial detection to preventive redesign.
Contamination Risk Reduction: Protocols and Best Practices
The extreme sensitivity of nested PCR makes it highly susceptible to contamination, which can lead to false-positive results. A robust contamination risk reduction strategy is foundational to any successful nested PCR protocol.
Unidirectional Workflow and Laboratory Design
The most critical mechanical method for preventing contamination is implementing a unidirectional workflow where materials and personnel move from "clean" pre-PCR areas to "dirty" post-PCR areas, never in reverse [33] [8].
The following workflow diagram visualizes the ideal physical separation of laboratory spaces to minimize the risk of amplicon contamination:
Ideal Unidirectional PCR Workflow: This workflow shows the one-way path from clean (green) to dirty (red) areas, including an intermediate stage (yellow), to prevent amplicon carryover.
Key Protocol Steps:
- Physical Separation: Ideally, four separate rooms should be designated [33] [8]:
- Room 1 (Pre-PCR): Reagent Aliquoting and Mastermix Preparation. This should be the cleanest area, ideally a laminar flow cabinet equipped with a UV light. No samples or amplified DNA should enter this space [33].
- Room 2 (Pre-PCR): Nucleic Acid Extraction and Template Addition. A separate area for extracting and handling sample DNA/RNA. A dedicated set of pipettes and consumables should be used here. Change gloves before handling positive controls [33].
- Room 3 (Post-PCR): Amplification. This room houses the thermal cyclers. The primary PCR product should be opened here if a traditional two-step method is used.
- Room 4 (Post-PCR): Product Analysis. This area is for gel electrophoresis, visualization, and any downstream analysis of the final amplicon [33].
Dedicated Equipment and Supplies: Each area must have a separate set of pipettes, filter tips, tube racks, lab coats, gloves, and waste containers. All items should be clearly labeled and must never be moved from a post-PCR area back to a pre-PCR area [33] [3].
Personal Practice: Personnel should not move from post-PCR to pre-PCR areas on the same day. If unavoidable, they must thoroughly wash hands, change lab coats and gloves, and not bring any equipment (including lab notebooks) from the dirty area to the clean area [33].
Single-Tube Nested PCR Protocols
To mitigate the high contamination risk associated with transferring the first-round product to a new tube for the second round, Single-Tube Nested PCR (STNPCR) protocols have been developed [1] [64]. In this format, both outer and inner primer sets are added to the same reaction vessel at the beginning, and an extended PCR program is run.
Protocol Overview: The success of STNPCR relies on designing outer and inner primers with significantly different annealing temperatures (Tm). A common strategy is to use Locked Nucleic Acid (LNA) modifications on the outer primers to increase their Tm [64].
Example Cycling Conditions for a Multiplex One-Tube Nested Real-Time RT-PCR [64]:
- Reverse Transcription: 50°C for 30 min.
- Initial Denaturation: 95°C for 2 min.
- First-Stage Amplification (10-15 cycles):
- Denature: 95°C for 15 sec.
- Anneal/Extend: 64°C for 1 min. (This higher temperature allows only the LNA-modified outer primers to bind efficiently).
- Second-Stage Amplification (30-40 cycles):
- Denature: 95°C for 15 sec.
- Anneal/Extend: 54°C for 1 min. (This lower temperature allows both the inner primers and the outer primers to bind, but the inner primers now dominate the amplification from the first-round products).
This protocol demonstrated an extreme sensitivity of 5 copies/reaction for detecting respiratory viruses without the risk of carryover contamination associated with open-tube transfers [64].
Advanced Applications and Performance Data
Quantitative Performance of Nested PCR vs. Standard PCR
The enhanced sensitivity of nested PCR formats is quantitatively demonstrated in clinical studies. The table below summarizes the superior performance of a multiplex one-tube nested real-time RT-PCR (mOTNRT-PCR) compared to individual real-time PCR (RT-qPCR) assays for detecting respiratory viruses [64].
| Virus | Detection by RT-qPCR (n=398) | Detection by mOTNRT-PCR (n=398) | Analytical Sensitivity (Copies/Reaction) |
|---|---|---|---|
| RSV | 95 (23.87%) | 109 (27.39%) | 5 |
| HRV | 137 (34.42%) | 150 (37.69%) | 5 |
| HMPV | 38 (9.55%) | 44 (11.06%) | 5 |
Comparison of Assay Performance: mOTNRT-PCR showed higher clinical sensitivity and an excellent limit of detection across multiple targets.
The Scientist's Toolkit: Essential Reagents for Robust Nested PCR
| Reagent / Material | Function in Nested PCR |
|---|---|
| Hot-Start DNA Polymerase | Inhibits polymerase activity at room temperature, preventing non-specific priming and primer-dimer formation during reaction setup, thereby enhancing specificity in both amplification rounds [6]. |
| dNTP Mix (with dUTP) | Provides the building blocks for DNA synthesis. Including dUTP instead of dTTP allows for subsequent degradation of contaminating amplicons by the UNG enzyme [8]. |
| Uracil-N-Glycosylase (UNG) | An enzymatic contamination control that degrades any uracil-containing DNA (i.e., previous PCR products) present in the reaction mix before amplification begins [8]. |
| Primer Sets (Outer & Inner) | Outer primers flank the target region, while inner primers bind within the first amplicon. Careful design is critical for success, including checking for specificity and ensuring Tm compatibility [78] [1]. |
| PCR Buffers with Additives | Buffer components stabilize the reaction. Additives like DMSO, Betaine, or BSA can help overcome challenges such as high GC content or the presence of residual PCR inhibitors in the sample [78] [6]. |
| Aerosol-Barrier Filter Pipette Tips | Prevent the formation of aerosols and cross-contamination of samples and reagents, which is essential for maintaining the integrity of pre-PCR areas [33]. |
Conclusion
Contamination control in nested PCR is not merely a technical step but a fundamental mindset that must be embedded throughout the entire experimental workflow. By integrating foundational knowledge of contamination sources with rigorous methodological practices, proactive troubleshooting, and thorough validation, researchers can harness the full power of nested PCR's superior sensitivity without succumbing to its pitfalls. The future of reliable molecular diagnostics and sensitive pathogen detection, as evidenced by its successful application in challenging fields from cardiovascular microbiology to environmental surveillance, depends on this disciplined approach. Embracing these comprehensive contamination reduction strategies ensures that nested PCR remains a robust, trustworthy, and invaluable tool in the advancement of biomedical and clinical research.
References
- 1. : Principle and Applications • Microbe Online Nested PCR [https://microbeonline.com/nested-pcr-principle-applications/]
- 2. What is Nested ?- Concept, Primers, Protocol, Advantages and... PCR [https://geneticeducation.co.in/what-is-nested-pcr/]
- 3. Troubleshooting your PCR [https://www.takarabio.com/learning-centers/pcr/faq/troubleshooting]
- 4. Troubleshooting PCR Part Three: Solutions for Weak Bands and Smearing | GoldBio [https://goldbio.com/articles/article/troubleshooting-pcr-part-three-solutions-for-weak-bands-and-smearing]
- 5. Advantages & Limits of Nested vs. Standard PCR | AAT Bioquest PCR [https://www.aatbio.com/resources/application-notes/advantages-limits-of-nested-pcr-vs-standard-pcr]
- 6. Methods - Top Ten Strategies | Thermo Fisher Scientific - RU PCR [https://www.thermofisher.com/ru/ru/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/pcr-education/pcr-reagents-enzymes/pcr-methods.html]
- 7. Preventing PCR Amplification Carryover Contamination in a Clinical Laboratory [https://www.annclinlabsci.org/content/34/4/389.full]
- 8. Regulatory Concern of Polymerase Chain Reaction (PCR) Carryover Contamination | IntechOpen [https://www.intechopen.com/chapters/52932]
- 9. | PDF Pcr contamination prevention [https://www.slideshare.net/slideshow/pcr-contamination-prevention/42247326]
- 10. Single-tube nested using immobilized internal primers for the... PCR [https://pmc.ncbi.nlm.nih.gov/articles/PMC1993823/]
- 11. Nested Polymerase Chain Reaction (PCR) - PubMed [https://pubmed.ncbi.nlm.nih.gov/30710024/]
- 12. Development of a Highly Sensitive Nested-PCR Procedure Using a ... [https://ncbi.nlm.nih.gov/pmc/articles/PMC101457]
- 13. & Solutions | Boster Bio PCR Troubleshooting Guide [https://www.bosterbio.com/protocol-and-troubleshooting/pcr-troubleshooting]
- 14. Preventing PCR Amplification Carryover Contamination in a Clinical Laboratory [https://www.annclinlabsci.org/content/34/4/389.long]
- 15. and Preventing Results false Positive false Negative PCR [https://www.clinicallab.com/preventing-false-positive-and-false-negative-pcr-results-26261]
- 16. 7 tips for avoiding DNA contamination in your PCR [https://www.takarabio.com/about/bioview-blog/tips-and-troubleshooting/avoid-dna-contamination-in-pcr]
- 17. How to prevent PCR contamination – miniPCR bio [https://www.minipcr.com/how-to-prevent-pcr-contamination/]
- 18. PCR Methods - Top Ten Strategies | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/pcr-education/pcr-reagents-enzymes/pcr-methods.html]
- 19. Nested Polymerase Chain Reaction - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/neuroscience/nested-polymerase-chain-reaction]
- 20. - Wikipedia Nested polymerase chain reaction [https://en.wikipedia.org/wiki/Nested_polymerase_chain_reaction]
- 21. Controlling for contamination in qPCR testing - LGC [https://blog.biosearchtech.com/how-to-control-for-contamination-in-qpcr-testing]
- 22. Overcoming bubble formation in polydimethylsiloxane-made PCR chips: mechanism and elimination with a high-pressure liquid seal | Microsystems & Nanoengineering [https://www.nature.com/articles/s41378-024-00725-1]
- 23. Optimizing PCR : Proven Tips and Troubleshooting Tricks | The Scientist [https://www.the-scientist.com/optimizing-pcr-proven-tips-and-troubleshooting-tricks-71660]
- 24. 6 Ways to Minimize Contamination during PCR | labclinics.com [https://www.labclinics.com/2019/07/22/six-ways-to-minimize-contamination-during-pcr/?lang=en]
- 25. Avoiding Contamination | Thermo Fisher Scientific - ZA [https://www.thermofisher.com/za/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/good-laboratory-practice-avoid-contamination-qpcr-experiments.html]
- 26. Nested Polymerase Chain Reaction - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/nested-polymerase-chain-reaction]
- 27. Avoiding Contamination | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/good-laboratory-practice-avoid-contamination-qpcr-experiments.html]
- 28. to reduce the Glove of surgical site infection or prosthetic... change risk [https://pubmed.ncbi.nlm.nih.gov/30497094/]
- 29. What is UNG /UDG? | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/what-is-ung-udg.html]
- 30. Preamplification with dUTP and Cod UNG Enables Elimination of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6214100/]
- 31. Molecular Nucleic Acid Amplification Flashcards | Quizlet [https://quizlet.com/ca/377868713/molecular-nucleic-acid-amplification-flash-cards/]
- 32. Use of modified nucleotides and uracil-DNA glycosylase ( UNG ) for the... [https://pubmed.ncbi.nlm.nih.gov/1406734/]
- 33. Dos and don’ts for molecular testing [https://www.who.int/teams/global-malaria-programme/case-management/diagnosis/nucleic-acid-amplification-based-diagnostics/dos-and-don-ts-for-molecular-testing]
- 34. Practical problems with PCR detection in asia: the importance of... [https://www.fao.org/4/x4946e/x4946e0d.htm]
- 35. Development of a rapid method for identifying carryover... [https://pubmed.ncbi.nlm.nih.gov/25320443/]
- 36. PCR Troubleshooting Guide | NEB [https://www.neb.com/tools-and-resources/troubleshooting-guides/pcr-troubleshooting-guide]
- 37. PCR Troubleshooting Guide | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/pcr-education/pcr-reagents-enzymes/pcr-troubleshooting.html]
- 38. MedPharmRes: Nested PCR optimization for detecting hepatitis E virus [https://www.medpharmres.com/archive/view_article?pid=mpr-8-2-104]
- 39. What is ISO 8 Cleanroom Classification ? [https://www.setra.com/blog/what-is-iso-14644-1-cleanroom-classification]
- 40. Repair Help: Learn How to Fix It Yourself. Laminar Flow Hood [https://www.ifixit.com/Device/Laminar_Flow_Hood]
- 41. and Laminar | Air Science Flow Hoods UV Sterilization [https://www.airscience.com/laminar-flow-hoods-and-uv-sterilization]
- 42. What is UV ? How does it work? | Ossila Sterilization [https://www.ossila.com/pages/uv-sterilization]
- 43. PCR controls [https://www.qiagen.com/us/knowledge-and-support/knowledge-hub/bench-guide/pcr/reference-genes-and-controls/pcr-controls]
- 44. Amplification of the No (NTC) Template Control [https://www.thermofisher.com/za/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/real-time-pcr-troubleshooting-tool/gene-expression-quantitation-troubleshooting/amplification-no-template-control.html]
- 45. The Devil in the Details: Contamination in a PCR Lab [https://www.rapidmicrobiology.com/news/the-devil-in-the-details-contamination-in-a-pcr-lab]
- 46. A highly sensitive modified nested PCR to enhance case detection in leishmaniasis | BMC Infectious Diseases | Full Text [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-019-4180-3]
- 47. Basic PCR /qPCR/dPCR protocols for assay quality control and... [https://www.sigmaaldrich.com/JP/en/technical-documents/technical-article/genomics/pcr/pcr-technologies-protocols-introduction]
- 48. PCR Clean™ | Minerva Biolabs [https://minerva-biolabs.com/en/dna-decontamination-reagents/pcr-clean]
- 49. Comparison of different decontamination for methods to... reagents [https://link.springer.com/article/10.1385/MB:22:3:231]
- 50. DNA decontamination methods for internal quality management in clinical PCR laboratories - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6816905/]
- 51. Standard Operating Procedures and Guidelines for Cleaning Laboratory Workspace - Office of Environmental Health and Safety - Wayne State University [https://research.wayne.edu/oehs/cleaninglabsop]
- 52. Laboratory Cleaning Checklist | Pritchard [https://www.pritchardindustries.com/lab-life-science-facility-cleaning-checklist/]
- 53. An efficient multistrategy DNA decontamination procedure of PCR ... [https://pubmed.ncbi.nlm.nih.gov/20927390/]
- 54. Nested PCR: Principle, Protocol and Application - BOC Sciences [https://www.bocsci.com/resources/nested-pcr-principle-protocol-and-applications.html]
- 55. ProtocolsStandardPCR < Lab < TWiki [https://barricklab.org/twiki/bin/view/Lab/ProtocolsStandardPCR]
- 56. Development of a single-tube nested -lateral flow biosensor assay... PCR [https://pmc.ncbi.nlm.nih.gov/articles/PMC6224276/]
- 57. Prevent PCR Contamination with Laminar Flow Hoods | Sentry Air [https://www.sentryair.com/blog/industry-applications/laboratories/help-prevent-pcr-contamination-with-laminar-flow-hoods/]
- 58. Improved assay to detect Plasmodium falciparum using an... [https://malariajournal.biomedcentral.com/articles/10.1186/1475-2875-12-74]
- 59. 10 Handy Tips to Help Keep Your PCRs Contamination Free [https://bitesizebio.com/23625/10-handy-tips-to-help-keep-your-pcrs-contamination-free/]
- 60. Rapid detection of low-level HeLa cell contamination in cell culture... [https://pubmed.ncbi.nlm.nih.gov/30353657/]
- 61. Clean Up Your Act! How To Clean Up PCR Contamination [https://bitesizebio.com/20773/clean-up-your-act-how-to-clean-up-pcr-contamination/]
- 62. Could your PCR be affected by contamination ? | IDT [https://www.idtdna.com/page/support-and-education/decoded-plus/could-your-pcr-be-affected-by-contamination/]
- 63. Designing and Performing Reproducible qPCR Experiments | Bioradiations [https://www.bioradiations.com/key-steps-to-ensure-optimized-and-reproducible-qpcr-experiments/]
- 64. A multiplex one-tube nested real time RT- PCR assay for simultaneous... [https://virologyj.biomedcentral.com/articles/10.1186/s12985-018-1061-0]
- 65. Design and Sampling Plan Optimization for RT-qPCR Experiments in Plants: A Case Study in Blueberry - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4779984/]
- 66. Efficient experimental design and analysis of real-time PCR assays - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3710343/]
- 67. of Comparison of sensitivity and... - Biochemia Medica nested PCR [https://www.biochemia-medica.com/en/journal/17/1/10.11613/BM.2007.012]
- 68. Evaluation of Two Multiplexed qPCR Assays for Malaria Detection and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11879595/]
- 69. False-Positive Results and Contamination in Nucleic Acid Amplification Assays: Suggestions for a Prevent and Destroy Strategy | European Journal of Clinical Microbiology & Infectious Diseases [https://link.springer.com/article/10.1007/s10096-004-1100-1]
- 70. Time to get real with qPCR controls: The frequency of sample contamination and the informative power of negative controls in environmental DNA studies - PubMed [https://pubmed.ncbi.nlm.nih.gov/34752687/]
- 71. Innovative application of nested for PCR of... detection [https://pubmed.ncbi.nlm.nih.gov/32363006/]
- 72. Innovative application of nested PCR for detection of Porphyromonas gingivalis in human highly calcified atherothrombotic plaques - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7178846/]
- 73. Nested Polymerase Chain Reaction - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/immunology-and-microbiology/nested-polymerase-chain-reaction]
- 74. Efficient nested-PCR-based method development for detection and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8571327/]
- 75. Detection and co-occurrence of Acanthamoeba and Klebsiella... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-025-03867-y]
- 76. (PDF) Genotyping and physiological characteristics of Acanthamoeba ... [https://www.academia.edu/143708356/Genotyping_and_physiological_characteristics_of_Acanthamoeba_isolated_from_beaches_in_Phuket_Province_Thailand]
- 77. Development of a Synthetic Positive Control Which Also Detects... [https://link.springer.com/article/10.1007/s11008-005-0112-y]
- 78. Polymerase Chain Reaction: Basic Protocol Plus Troubleshooting and Optimization Strategies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4846334/]
- 79. PCR Basic Troubleshooting Guide [https://www.creative-biogene.com/blog/pcr-basic-troubleshooting-guide]