Strategies to Reduce False Positives in lncRNA Biomarker Detection for Hepatocellular Carcinoma
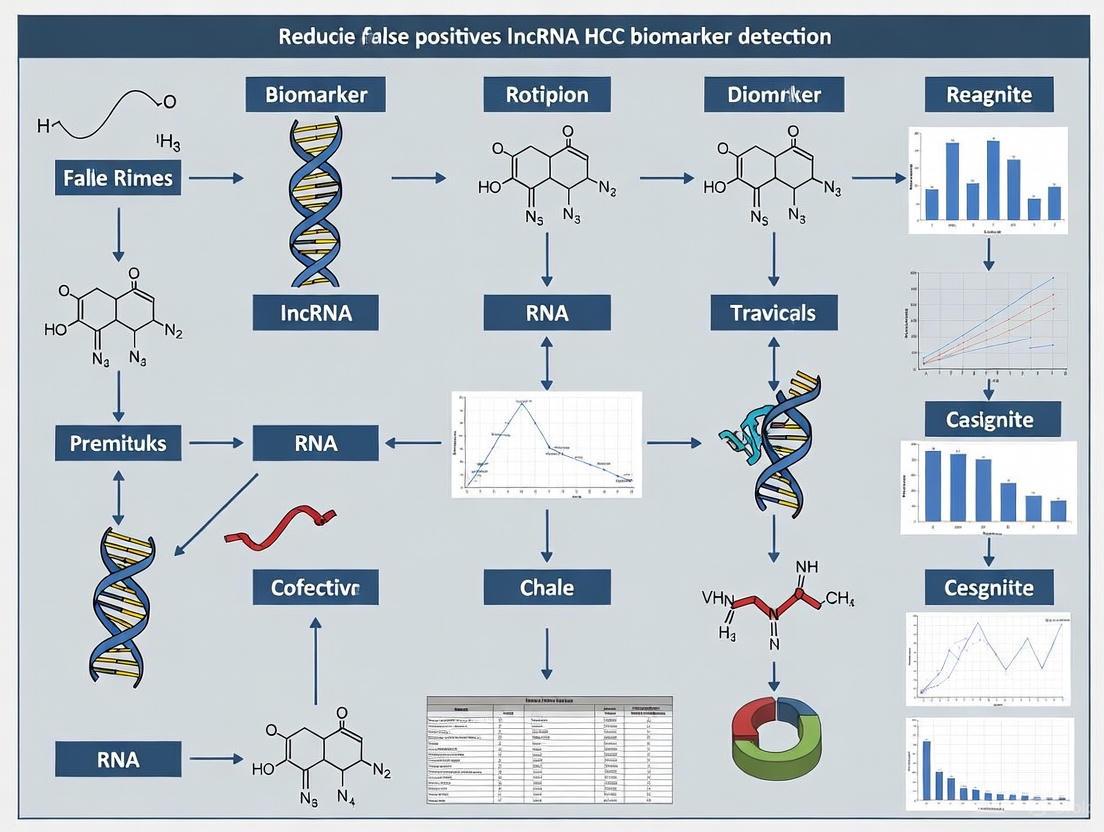
This article addresses the critical challenge of false positives in the detection of long non-coding RNA (lncRNA) biomarkers for Hepatocellular Carcinoma (HCC), a major obstacle to their clinical adoption.
Strategies to Reduce False Positives in lncRNA Biomarker Detection for Hepatocellular Carcinoma
Abstract
This article addresses the critical challenge of false positives in the detection of long non-coding RNA (lncRNA) biomarkers for Hepatocellular Carcinoma (HCC), a major obstacle to their clinical adoption. Aimed at researchers, scientists, and drug development professionals, it provides a comprehensive exploration of the biological and technical sources of inaccuracy. The scope spans from foundational knowledge of lncRNA biology and heterogeneity to advanced methodological solutions involving multi-analyte panels and artificial intelligence. It further delves into troubleshooting experimental variables and outlines rigorous validation frameworks and comparative performance metrics against established standards like AFP, ultimately presenting a pathway towards developing robust, clinically viable lncRNA-based diagnostic tools for precision oncology.
Understanding the Roots of Error: Biological and Technical Sources of False Positives in lncRNA Detection
The investigation of long non-coding RNAs (lncRNAs) as biomarkers for hepatocellular carcinoma (HCC) presents a unique paradox: their remarkable structural integrity in circulation offers tremendous diagnostic potential, yet this very stability can be misleading if degradation artifacts are not properly controlled. LncRNAs are arbitrarily defined as non-coding transcripts longer than 200 nucleotides [1] and can be detected in plasma even under oppressive conditions such as multiple freeze-thaw cycles or prolonged incubation at room temperature [2] [3]. This stability originates from their extensive secondary structures, encapsulation in protective exosomes, and association with RNA-binding proteins [2] [3]. However, pre-analytical variables and improper handling can generate partial degradation products that compromise data integrity and contribute to false positives in biomarker studies. This technical guide addresses this paradox by providing actionable protocols to leverage lncRNA stability while minimizing degradation artifacts in HCC biomarker research.
Frequently Asked Questions: Core Stability Concepts
What gives circulating lncRNAs their unusual stability compared to mRNAs? Circulating lncRNAs exhibit exceptional stability due to multiple protective mechanisms:
- Extensive secondary structures that limit nuclease accessibility [3]
- Encapsulation in membrane vesicles like exosomes and microvesicles, which protect against RNase degradation [2] [3]
- Association with lipoprotein complexes or RNA-binding proteins such as Argonaute (Ago) complexes that provide stabilization [2]
- Stabilizing post-translational modifications that may enhance resistance to degradation [3]
Why is stability both an advantage and a potential source of artifacts in HCC detection? The high stability of lncRNAs enables their detection in archived samples and makes them robust biomarkers [3]. However, this same stability means that partially degraded fragments persist in samples, potentially leading to:
- False positive signals from truncated isoforms that still contain primer binding sites
- Inaccurate quantification if degradation is uneven across sample groups
- Misinterpretation of results if degradation products are amplified instead of full-length transcripts
Which blood collection tubes best preserve lncRNA integrity for HCC studies? Based on comparative studies:
- EDTA plasma and serum both effectively maintain lncRNA stability [2]
- Heparin plasma should be avoided as it causes significant decline in lncRNA levels [2]
- Consistent use of the same collection method across all samples in a study is critical
How can researchers distinguish true lncRNA biomarker signals from degradation artifacts?
- Implement RNA Integrity Number (RIN) assessment even for fragmented RNAs
- Use spike-in controls to monitor extraction efficiency and degradation
- Target multiple regions of the lncRNA transcript to detect fragmentation patterns
- Employ 3'/5' integrity assays to assess degradation bias
Troubleshooting Guides: Solving Common Stability Issues
Pre-Analytical Phase: Sample Collection and Handling
Problem: Inconsistent lncRNA levels between sample batches
| Root Cause | Solution | Quality Indicator |
|---|---|---|
| Improper blood collection tubes | Use EDTA tubes or serum tubes exclusively; avoid heparin | Plasma/serum consistency across ≥95% samples |
| Delayed processing | Process samples within 2 hours of collection; use standardized protocols | Documented processing time <2 hours for all samples |
| Variable freeze-thaw cycles | Aliquot upon first thaw; never refreeze | ≤2 freeze-thaw cycles documented |
| Hemolyzed samples | Implement centrifugation protocols to remove cellular contaminants | Visual inspection and absorbance ratio (A414/A540 <0.2) |
Experimental Protocol: Plasma Processing for lncRNA Analysis
- Collect whole blood in EDTA vacutainer tubes [2]
- Process within 2 hours of collection by centrifugation at 1,200-1,600 × g for 15 minutes at 4°C
- Transfer supernatant to fresh tubes and centrifuge at 16,000 × g for 15 minutes to remove residual cells
- Aliquot plasma into RNase-free tubes in small volumes (100-200 μL) to avoid repeated freeze-thaw cycles
- Store immediately at -80°C until RNA extraction
Analytical Phase: RNA Extraction and Quality Control
Problem: Unreliable lncRNA quantification despite apparent high RNA yield
| Root Cause | Solution | Quality Indicator |
|---|---|---|
| Co-purification of inhibitors | Use silica membrane-based columns with DNase treatment | PCR efficiency between 90-110% |
| Inadequate RNA integrity | Implement fragment analyzer with specific lncRNA integrity score | RINe >7.0 or similar integrity metric |
| Inconsistent reverse transcription | Use gene-specific primers and include controls for genomic DNA | Standard deviation of Cq values <0.5 among replicates |
| Amplification of degraded products | Design assays targeting 5' and 3' ends; avoid single amplicon dependency | <2 Cq difference between 5' and 3' amplicons |
Experimental Protocol: RNA Isolation and Quality Assessment
- Extract RNA using miRNeasy Mini Kit (QIAGEN) or similar silica membrane-based methods [4]
- Include spike-in synthetic RNA controls (e.g., from other species) to monitor extraction efficiency
- Treat with DNase I to remove genomic DNA contamination
- Assess RNA quality using Bioanalyzer or TapeStation systems
- Use consistent input amounts (typically 10-100 ng) across all samples in a study
Post-Analytical Phase: Data Analysis and Validation
Problem: Inconsistent correlation between lncRNA expression and HCC clinical parameters
Experimental Protocol: Machine Learning Integration for HCC Detection Recent studies demonstrate that integrating multiple lncRNAs with conventional biomarkers using machine learning significantly improves HCC detection accuracy [4].
- Quantify lncRNAs of interest (e.g., LINC00152, UCA1, GAS5) by qRT-PCR using PowerTrack SYBR Green Master Mix [4]
- Normalize data using reference genes (GAPDH, β-actin) that show stable expression in your sample set
- Integrate lncRNA data with conventional laboratory parameters (ALT, AST, AFP)
- Apply machine learning algorithms (Python's Scikit-learn platform) to develop diagnostic models
- Validate model performance using independent sample sets and calculate sensitivity/specificity
Quantitative Stability Data for Key HCC-Associated lncRNAs
Table 1: Stability Profiles of HCC-Related lncRNAs Under Various Conditions
| lncRNA | Stability in Plasma | Resistance to Freeze-Thaw | Diagnostic Performance for HCC | Key References |
|---|---|---|---|---|
| MALAT1 | High - stable at room temperature up to 24h | Resistant to multiple cycles | Specificity: 96% for NSCLC [3] | [2] [3] |
| HULC | High - detectable in plasma of HCC patients | Resistant to degradation | Elevated in HCC patients [3] | [5] [3] |
| LINC00152 | Moderate to high | Moderate resistance | Sensitivity: 60-83%, Specificity: 53-67% [4] | [4] |
| UCA1 | High in serum | Stable under storage | Specificity: 82.1% for HCC [3] | [3] [4] |
| GAS5 | Moderate | Moderate resistance | Tumor suppressor function in HCC [4] | [4] |
Table 2: Diagnostic Performance of Individual vs. Combined lncRNA Biomarkers for HCC
| Biomarker Approach | Sensitivity (%) | Specificity (%) | AUC | Reference |
|---|---|---|---|---|
| LINC00152 alone | 60-83 | 53-67 | 0.72 | [4] |
| UCA1 alone | 60-75 | 67-82 | 0.75 | [3] [4] |
| GAS5 alone | 55-70 | 60-75 | 0.68 | [4] |
| Machine learning model combining 4 lncRNAs + lab parameters | 100 | 97 | 0.99 | [4] |
| Three-lncRNA signature (PTENP1, LSINCT-5, CUDR) | 85 | 90 | 0.94 | [3] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for lncRNA Stability Studies
| Reagent/Category | Specific Product Examples | Function in lncRNA Research | Stability Considerations |
|---|---|---|---|
| Blood Collection Tubes | EDTA tubes, Serum tubes | Preserve lncRNAs in circulation | Avoid heparin; process within 2 hours [2] |
| RNA Stabilization | PAXgene Blood RNA tubes, RNAlater | Stabilize RNA at collection | Critical for field studies or delayed processing |
| RNA Extraction Kits | miRNeasy Mini Kit (QIAGEN) | Isolate total RNA including lncRNAs | Silica membrane methods show good recovery [4] |
| DNase Treatment | RNase-Free DNase Set (QIAGEN) | Remove genomic DNA contamination | Essential for accurate qRT-PCR results |
| Reverse Transcription | RevertAid First Strand cDNA Synthesis Kit | Generate cDNA for downstream analysis | Use consistent priming methods [4] |
| qPCR Master Mix | PowerTrack SYBR Green Master Mix | Quantify lncRNA expression | Provides consistent amplification [4] |
| Reference Genes | GAPDH, β-actin, RPLP0 | Normalize expression data | Must validate stability in your sample type [2] [4] |
Advanced Methodologies: Integrating Machine Learning for Improved Specificity
Implementation Protocol:
- Quantify multiple lncRNAs (LINC00152, LINC00853, UCA1, GAS5) from plasma samples [4]
- Measure conventional parameters (AFP, ALT, AST, bilirubin, albumin) from the same samples
- Integrate data into a unified dataset with normalized values
- Apply Random Forest or SVM algorithms to identify optimal biomarker combinations
- Validate model performance using cross-validation and independent cohorts
This approach has demonstrated 100% sensitivity and 97% specificity for HCC detection, significantly outperforming individual biomarkers [4].
The stability of lncRNAs presents both extraordinary opportunities and significant challenges in HCC biomarker development. By implementing rigorous pre-analytical controls, standardized processing protocols, and advanced computational integration, researchers can effectively leverage lncRNA stability while minimizing degradation artifacts. The integration of multiple lncRNA markers with conventional parameters through machine learning approaches represents the most promising path forward for reducing false positives and developing clinically viable HCC diagnostic tools. As the field advances, continued attention to the nuances of lncRNA biology and stability characteristics will be essential for translating these biomarkers into meaningful clinical applications.
Frequently Asked Questions (FAQs)
FAQ 1: How does the molecular heterogeneity of HCC fundamentally challenge lncRNA biomarker discovery? HCC is not a single disease but comprises multiple molecular subtypes with distinct clinical behaviors and molecular profiles. This heterogeneity means that a lncRNA highly expressed in one subtype may be absent in another. If a research cohort over-represents a particular subtype, a detected lncRNA might appear as a general biomarker, leading to false positives when applied to a broader, more heterogeneous patient population [6] [7]. For instance, a study stratified HCC into three subtypes (C1-C3) based on plasma exosomal lncRNA profiles, with the C3 subtype exhibiting a uniquely poor prognosis, advanced stage, and immunosuppressive microenvironment. A lncRNA signature derived predominantly from C3 patients would likely fail to accurately diagnose patients with the C1 or C2 subtypes [6] [8].
FAQ 2: What are the major biological processes driven by HCC subtypes that influence lncRNA expression? Different HCC subtypes are characterized by the hyperactivation of specific biological pathways, which in turn regulate distinct sets of lncRNAs. Relying on a lncRNA panel linked to a single process increases the risk of missing other significant subtypes. Key processes include:
- Hypoxia: A hallmark of the solid tumor microenvironment, hypoxia activates hypoxia-inducible factors (HIFs) that transcriptionally regulate lncRNAs like LINC00674 and NEAT1, promoting proliferation and metastasis [9] [10].
- Metabolic Reprogramming: Subtypes can be defined by specific metabolic pathways. Research has identified subtypes based on fatty-acid-associated lncRNAs and amino-acid-metabolism-related lncRNAs, each showing different prognostic outcomes and tumor microenvironments [11] [12].
- Immune Evasion: Certain subtypes, such as the exosomal lncRNA-defined C3 subtype, exhibit an immunosuppressive microenvironment with increased Treg infiltration and elevated expression of immune checkpoints like PD-L1 and CTLA4. LncRNAs active in this context are often involved in immune suppression [6] [9].
FAQ 3: Beyond tissue samples, what are other clinically relevant sources of lncRNAs for reducing false positives? Liquid biopsies offer a less invasive and potentially more comprehensive view of the tumor's molecular landscape.
- Plasma Exosomal lncRNAs: Exosomes are nanoscale vesicles released by tumors into the circulation. They carry a stable cargo of lncRNAs that reflect the molecular subtype of the originating tumor. Profiling plasma exosomal lncRNAs can provide a systemic view that may better represent intra-tumoral heterogeneity than a single tissue biopsy [6] [8] [7].
- Circulating Tumor Cells (CTCs) and ctDNA: While not the focus of this guide, these are other components of liquid biopsies that can be analyzed alongside lncRNAs for a multi-analyte approach to subclassify tumors [7].
FAQ 4: What computational strategies can be used to control for molecular heterogeneity during biomarker signature development? Employing robust bioinformatic methods during the discovery phase is critical.
- Unsupervised Clustering: Before building a diagnostic model, use algorithms like ConsensusClusterPlus to molecularly subtype your patient cohort based on their overall transcriptomic data. This ensures you are aware of the subtype composition of your dataset [6] [9] [11].
- Multi-Omics Integration: Combine lncRNA data with genomic mutations (e.g., TP53 vs. CTNNB1), metabolic pathway activities, and immune cell infiltration data. This helps in building a composite signature that is specific and resilient across subtypes [11] [7]. For example, the C3 subtype is associated with higher TP53 mutation rates, providing a genomic correlate to the lncRNA signature [11].
Troubleshooting Guides
Problem: High False Positive Rate in an Assay Detecting a Putative Oncogenic lncRNA
| Potential Cause | Diagnostic Experiments | Recommended Solution & Interpretation |
|---|---|---|
| Cohort Bias: The training cohort was enriched for a specific molecular subtype. | 1. Subtype Re-analysis: Use established gene signatures (e.g., from TCGA) to re-classify your cohort into known molecular subtypes (e.g., C1, C2, C3) [6] [11]. 2. Prevalence Check: Compare the prevalence of your lncRNA across the identified subtypes using differential expression analysis (e.g., with the limma R package). |
If the lncRNA is exclusively or highly expressed in one subtype, it is not a pan-HCC biomarker. Report it as a subtype-specific biomarker and validate it in independent, subtype-balanced cohorts. |
| Context-Specific Expression: The lncRNA is only expressed under specific microenvironmental conditions (e.g., hypoxia). | 1. Pathway Correlation: Perform Gene Set Variation Analysis (GSVA) or GSEA to correlate lncRNA expression levels with hallmark pathway activities (e.g., hypoxia, glycolysis) [6] [10]. 2. In vitro Validation: Culture HCC cell lines (e.g., Huh-7, Hep3B) under normoxic and hypoxic (1% O₂) conditions for 24 hours. Measure lncRNA expression via RT-qPCR [9] [10]. | A significant correlation with hypoxia pathways or induction under low oxygen confirms context-dependent expression. This lncRNA's diagnostic value may be limited to advanced, hypoxic tumors. |
| Technical Cross-Reaction: The detection probe or primer set is not specific enough. | 1. BLAST Analysis: Check the primer/probe sequence for specificity against the entire transcriptome. 2. Gel Electrophoresis: Run RT-qPCR products on a gel to confirm a single, correctly sized band. 3. Sanger Sequencing: Sequence the PCR product to verify its identity. | Redesign primers/probes to avoid homologous regions. Use locked nucleic acid (LNA) probes in qPCR to enhance specificity and discrimination of closely related lncRNA family members. |
Key lncRNA Signatures Across HCC Molecular Subtypes
The table below summarizes recently identified lncRNA-based molecular subtypes and their characteristics, highlighting the direct link between subtype and lncRNA expression.
| Molecular Subtype / Signature | Defining LncRNAs or Related Genes | Associated Biological Processes | Clinical & Microenvironment Features |
|---|---|---|---|
| Plasma Exosomal Subtypes [6] [8] | 22 dysregulated exosomal lncRNAs; 6-gene risk score (G6PD, KIF20A, NDRG1, ADH1C, RECQL4, MCM4) | Cell cycle, TGF-β signaling, p53 pathway, ferroptosis, glycolysis, mTORC1 hyperactivation | C3 Subtype: Poorest OS, immunosuppressive (↑Tregs, ↑PD-L1/CTLA4), high TIDE score, ↑TP53 mutations. |
| Hypoxia/Anoikis Signature [9] | 9-lncRNA model (incl. LINC01554, FIRRE, LINC01139, LINC01134, NBAT1) | Hypoxia response, anoikis resistance, tumor metastasis | High-risk group: Poor OS, increased immunosuppressive cells (Tregs, M0 macrophages), limited immunotherapy efficacy. |
| Fatty Acid Metabolism Subtypes [11] | 7-lncRNA signature (TRAF3IP2-AS1, SNHG10, AL157392.2, LINC02641, AL357079.1, AC046134.2, A1BG-AS) | Fatty acid metabolism signaling | C3 Subtype: Worst OS, lower immune scores, distinct immune checkpoint expression, associated with TP53 mutations. |
| Amino Acid Metabolism Signature [12] | 4-lncRNA risk model (incl. key gene AL590681.1) | Amino acid metabolism, BCAA metabolism | High-risk group: Lower OS, more immunosuppressive immune infiltration (↑CD276, CTLA4, TIGIT). |
Experimental Protocols for Validating Subtype-Specific LncRNAs
Protocol 1: Inducing and Validating Hypoxia-Responsive LncRNAsIn Vitro
Principle: To experimentally confirm whether a candidate lncRNA is regulated by hypoxia, a key driver of molecular heterogeneity.
Workflow Diagram:
Key Reagents:
- HCC Cell Lines: Huh-7, Hep3B, MHCC97H, Li-7 [9] [10] [12].
- Hypoxia Chamber/Workstation: To maintain a controlled environment of 1% O₂, 5% CO₂, at 37°C [9] [10].
- RNA Extraction Kit: RNeasy Mini Kit (Magen, China) or equivalent [9].
- Reverse Transcription Kit: PrimeScript TM RT Master Mix (Takara, China) [9].
- qPCR Reagents: TB Green Premix Ex Taq, and gene-specific primers [9].
Procedure:
- Cell Culture: Seed HCC cells in standard 6-well plates and allow them to adhere overnight.
- Hypoxia Induction: Place the experimental group in a hypoxia chamber set to 1% O₂, 5% CO₂, and 37°C for 24 hours. Maintain the control group under standard normoxic conditions (21% O₂).
- RNA Extraction: After 24 hours, immediately lyse cells and extract total RNA using the RNeasy Mini Kit according to the manufacturer's instructions. Include a DNase digestion step to remove genomic DNA contamination.
- cDNA Synthesis: Convert 1 µg of total RNA into cDNA using the PrimeScript RT Master Mix.
- Quantitative PCR (qPCR): Perform qPCR reactions in triplicate using TB Green chemistry and gene-specific primers. Include a housekeeping gene (e.g., GAPDH, β-actin) for normalization.
- Data Analysis: Calculate relative gene expression using the 2^(-ΔΔCt) method. A significant upregulation in the hypoxia group confirms the lncRNA as hypoxia-responsive.
Protocol 2: Functional Validation of Oncogenic LncRNAs via Knockdown
Principle: To determine the functional role of a subtype-specific lncRNA in HCC proliferation and viability.
Workflow Diagram:
Key Reagents:
- siRNA or shRNA: Specific short hairpin RNA (shRNA) or siRNA targeting the lncRNA of interest, and a non-targeting scramble control [12] [13].
- Transfection Reagent: Lipofectamine 3000 (Invitrogen) or HiPerFect (Qiagen) [12] [13].
- Assay Kits: CCK-8 kit for cell viability; Crystal Violet for colony staining; MTT assay reagents [12] [13].
Procedure:
- Knockdown: Transfect HCC cells (e.g., Huh-7) with lncRNA-specific siRNA or shRNA using Lipofectamine 3000, following the manufacturer's protocol. Include a non-targeting scramble siRNA as a negative control.
- Efficiency Check: 48 hours post-transfection, harvest cells and extract RNA. Perform RT-qPCR to confirm significant knockdown of the target lncRNA compared to the control group.
- Functional Assays:
- Cell Viability (CCK-8/MTT): Seed transfected cells in 96-well plates. At 0, 24, 48, and 72 hours, add CCK-8 reagent and measure the absorbance at 450nm to track viability over time.
- Colony Formation: Seed a low density (e.g., 1000 cells/well) of transfected cells in 6-well plates. Culture for 14 days, changing media periodically. Fix colonies with paraformaldehyde, stain with crystal violet, and count the number of visible colonies.
- Interpretation: A significant reduction in cell viability and colony-forming ability upon lncRNA knockdown confirms its functional role in promoting HCC cell growth, supporting its relevance as a subtype-specific oncogene.
The Scientist's Toolkit: Research Reagent Solutions
| Essential Material / Reagent | Function in Experimental Workflow | Specific Examples & Notes |
|---|---|---|
| Hypoxia Chamber | Creates a controlled low-oxygen environment to mimic the tumor microenvironment and study hypoxia-regulated lncRNAs. | Baker's Ruskinn INVIVO2 400, or comparable tri-gas incubators. Critical for validating hypoxia-associated signatures [9] [10]. |
| LNA-based qPCR Probes | Enhance specificity and sensitivity for detecting and discriminating highly homologous lncRNA sequences, reducing technical false positives. | Qiagen miRCURY LNA PCR assays; Exiqon probes. Ideal for quantifying lncRNAs from liquid biopsy samples with low abundance [7]. |
| CIBERSORT / ssGSEA Algorithms | Computational tools for deconvoluting immune cell infiltration from bulk RNA-seq data, linking lncRNA signatures to the immune context of subtypes. | CIBERSORT (using LM22 signature); R package GSVA for ssGSEA. Essential for characterizing immunogenic subtypes [6] [9] [11]. |
| ExoRBase 2.0 Database | A public repository for plasma exosomal transcriptomes, providing a reference for discovering and validating exosomal lncRNA biomarkers. | Contains RNA-seq data from 112 HCC patients and 118 healthy controls. Invaluable for starting liquid biopsy-based projects [8]. |
| ConsensusClusterPlus R Package | Performs unsupervised clustering to robustly define molecular subtypes within a patient cohort, a crucial first step in assessing heterogeneity. | Used in multiple studies to identify 2-3 stable HCC subtypes based on lncRNA expression profiles [6] [9] [11]. |
A major obstacle in the development of reliable liquid biopsies for Hepatocellular Carcinoma (HCC) is the high prevalence of underlying chronic liver diseases (CLD) in the at-risk population. Many long non-coding RNAs (lncRNAs) are dysregulated in response to general hepatic inflammation, fibrosis, and cirrhosis, long before the development of malignancy. This presents a significant risk of false positives in biomarker studies if these CLD-elevated lncRNAs are misattributed as being HCC-specific. This technical guide addresses this confounder by providing clear experimental and bioinformatic strategies to differentiate true HCC-specific lncRNA signals from the background of chronic liver injury.
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: Why is it crucial to distinguish CLD-related lncRNAs from HCC-specific ones? The primary goal is to improve the specificity and positive predictive value of a lncRNA-based biomarker. A lncRNA that is elevated in both cirrhosis and HCC offers limited diagnostic value for the early detection of cancer in a cirrhotic patient, as a positive result may simply reflect the underlying cirrhosis rather than malignant transformation. Identifying lncRNA signals that show a significant step-up specifically at the point of HCC development is key to a clinically useful test [14].
Q2: My candidate lncRNA is elevated in HCC patient plasma compared to healthy controls. Does this confirm it's HCC-specific? Not necessarily. This is a common pitfall. A comparison against healthy controls only confirms the lncRNA is dysregulated in the disease state (HCC), but it does not isolate the cause of dysregulation. The critical control group for establishing HCC-specificity is patients with advanced chronic liver disease or cirrhosis without HCC. You must demonstrate that your lncRNA's expression is significantly higher in the HCC group compared to this non-malignant CLD group [14] [4].
Q3: What are the main biological mechanisms that can cause lncRNA dysregulation in CLD? Chronic liver injury creates a microenvironment that profoundly alters lncRNA expression through several mechanisms:
- Epigenetic Modifications: Changes in DNA methyltransferases (DNMTs) or histone acetylases in CLD can silence or activate lncRNA promoters. For example, promoter hypermethylation by DNMTs in HCC can lead to the downregulation of the tumor suppressor lncRNA MEG3 [15].
- Transcription Factor Activation: Oncogenic transcription factors like Myc, which are activated in stressed and diseased livers, can drive the expression of lncRNAs such as linc00176 [15].
- Metabolic Reprogramming: The liver's central metabolic role means that metabolic substrates like SAM (for methylation) and Acetyl-CoA (for acetylation) can influence the epigenetic landscape and lncRNA expression [15].
Troubleshooting Common Experimental Issues
Problem: High background signal from CLD in cohort studies.
- Solution: Implement rigorous patient stratification. Recruit well-defined cohorts: (1) Healthy controls, (2) Patients with CLD (e.g., HCV, HBV, NAFLD) without fibrosis, (3) Patients with CLD with advanced fibrosis/cirrhosis, and (4) Treatment-naive HCC patients on a background of CLD. Statistical models like logistic regression should include CLD status as a covariate to isolate the independent effect of HCC on lncRNA expression [16] [17].
Problem: Inconsistent results from a single lncRNA biomarker.
- Solution: Develop a multi-lncRNA signature panel. It is unlikely that a single lncRNA will perfectly distinguish HCC from all etiologies of CLD. Combine lncRNAs with complementary profiles—for instance, one that is general to inflammation and one that is highly specific to malignancy. Machine learning approaches are highly effective here. A 2024 study demonstrated that a model integrating four lncRNAs (LINC00152, LINC00853, UCA1, GAS5) with conventional lab data achieved 100% sensitivity and 97% specificity, far outperforming any single lncRNA [4].
Problem: Uncertain biological relevance of a candidate lncRNA.
- Solution: Perform functional validation and mechanistic studies. Determine the lncRNA's subcellular localization and its interaction partners. For example, if a lncRNA acts as a competitive endogenous RNA (ceRNA or "sponge") for a microRNA, this mechanism might be active in both CLD and HCC, contributing to background signal. Techniques like RNA in situ hybridization (e.g., using branched DNA assays) can visualize lncRNA distribution in tissue samples from different disease stages [15] [18].
The table below summarizes the diagnostic performance of several well-studied lncRNAs, highlighting the importance of multi-marker panels.
Table 1: Diagnostic Performance of Select lncRNAs in HCC
| LncRNA | Reported Sensitivity | Reported Specificity | Key Characteristics and Clinical Utility |
|---|---|---|---|
| LRB1 | Not specified | Not specified | Serum levels significantly increased in HCC vs. healthy volunteers. Positively associated with AFP, large tumor size, and venous invasion. Diagnostic accuracy enhanced when combined with AFP and DCP [19]. |
| SNHG1 | 87.3% | 86.0% | Plasma levels show superior sensitivity but slightly lower specificity compared to AFP alone. AUC of 0.92, indicating high diagnostic accuracy [20]. |
| LINC00152 | ~83% | ~67% | Often found elevated in HCC. The LINC00152/GAS5 expression ratio has been reported to significantly correlate with increased mortality risk [4]. |
| GAS5 | ~60% | ~53% | A tumor suppressor lncRNA. Lower expression is often associated with worse prognosis. Its ratio with oncogenic lncRNAs can be informative [4]. |
| Multi-lncRNA Panel (LINC00152, LINC00853, UCA1, GAS5) + Machine Learning | 100% | 97% | A 2024 study demonstrated that integrating multiple lncRNAs with standard lab data into an ML model dramatically outperformed individual biomarkers [4]. |
Detailed Experimental Protocol: A Step-by-Step Guide
This protocol outlines a robust method for quantifying circulating lncRNAs from patient plasma, suitable for differentiating HCC from CLD.
Title: Quantification of Circulating lncRNAs from Plasma via RNA Extraction and qRT-PCR Objective: To isolate, reverse transcribe, and quantify the relative expression levels of target lncRNAs from the plasma of healthy, CLD, and HCC patients.
Materials & Reagents:
- Sample Collection: BD Vacutainer sodium heparin tubes (or other EDTA tubes for plasma) [19].
- RNA Isolation: miRNeasy Mini Kit (Qiagen) or similar [4].
- cDNA Synthesis: RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) [4].
- qPCR: PowerTrack SYBR Green Master Mix (Applied Biosystems); ViiA 7 or StepOne Real-Time PCR system [19] [4].
- Primers: Validated primers for target lncRNAs (e.g., LRB1, GAPDH) [19].
Procedure:
- Plasma Preparation: Collect peripheral blood and centrifuge using a multi-step protocol to prevent nucleic acid contamination: 4°C at 800 × g for 20 min, then 2,000 × g for 10 min, and finally 5,000 × g for 5 min. Aliquot the supernatant (plasma) and store at -80°C [19].
- RNA Isolation: Extract total RNA from plasma samples using the miRNeasy Mini Kit according to the manufacturer's protocol. Include a DNase digestion step to remove genomic DNA contamination [4].
- cDNA Synthesis: Synthesize single-strand cDNA from a fixed amount (e.g., 10 µg) of total RNA using the RevertAid kit and random hexamers/oligo-dT primers [19] [4].
- Quantitative PCR (qPCR):
- Prepare a 20 µl reaction mixture containing: 10 µl SYBR Green Master Mix, 5 pmol each of forward and reverse primer, and 2 µl of cDNA template [19].
- Run the reaction with the following cycling conditions: Initial denaturation at 95°C for 1 min, followed by 35-40 cycles of: 95°C for 1 min (denaturation), 58°C for 1 min (annealing), 72°C for 1 min (extension) [19].
- Perform all reactions in triplicate.
- Data Analysis:
- Use the Quantification Cycle (Cq) for calculations.
- Normalize the Cq values of the target lncRNAs to a stable endogenous control (e.g., GAPDH) to obtain ΔCq.
- Use the 2−ΔΔCq method to calculate the relative expression levels (fold change) between experimental groups (HCC, CLD) and the control group [19] [4].
Signaling Pathways & Molecular Mechanisms
The following diagram illustrates how a single lncRNA, such as NEAT1, can be involved in multiple stages of liver disease progression, from chronic injury to cancer, explaining why it can be a confounder in biomarker studies.
Diagram: LncRNA NEAT1 as a Nexus in Liver Disease Pathogenesis. This figure shows how one lncRNA can be dysregulated by chronic liver disease (CLD) and, in turn, promote HCC progression through multiple condition-specific mechanisms, such as acting as a microRNA sponge [21].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Kits for lncRNA Biomarker Research
| Research Reagent / Kit | Function / Application | Key Consideration |
|---|---|---|
| BD Vacutainer Sodium Heparin Tubes | Plasma collection for cell-free RNA analysis. | Ensures high-quality plasma recovery with minimal cellular RNA contamination [19]. |
| miRNeasy Mini Kit (Qiagen) | Total RNA isolation from plasma/serum. | Efficiently recovers both small and long RNA species, crucial for analyzing diverse lncRNAs [4]. |
| RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) | Reverse transcription of RNA to cDNA. | Provides high-efficiency synthesis, essential for working with low-abundance circulating lncRNAs [4]. |
| Power SYBR Green / PowerTrack SYBR Green Master Mix | Fluorescent detection for qRT-PCR. | Enables sensitive and specific quantification of lncRNA amplicons [19] [4]. |
| Branched DNA (bDNA) In Situ Hybridization Assay | Visualization and quantitation of lncRNAs in FFPE tissue. | Critical for determining the spatial distribution and cellular origin of lncRNAs, helping link circulating levels to tissue pathology [18]. |
| LncRNA-Specific Primers | Amplification of target sequences in qPCR. | Requires careful in-silico design and validation to ensure specificity for the target lncRNA isoform [19]. |
Frequently Asked Questions (FAQs)
Q1: Why focus on exosomal lncRNAs instead of freely circulating lncRNAs for HCC detection? Exosomal lncRNAs offer significant advantages for reducing false positives in hepatocellular carcinoma (HCC) detection. Exosomes provide a protective lipid bilayer that shields lncRNAs from degradation by RNases, greatly enhancing their stability in biofluids [3] [22]. Furthermore, exosomes originating from tumor cells contain molecular cargo specific to their cell of origin, which improves the specificity of the detection signal. By targeting EpCAM-specific exosomes (Epexo), for instance, researchers can preferentially analyze tumor-derived lncRNAs, substantially reducing background noise from healthy cells [22].
Q2: What are the key challenges in isolating high-quality exosomes from plasma for lncRNA analysis? The major challenges include: (1) Efficient recovery of exosomes without co-precipitation of contaminants like lipoproteins; (2) Maintaining RNA integrity during the isolation process; (3) Achieving sufficient yield for downstream lncRNA analysis; and (4) Ensuring reproducibility across samples and batches. The complex cellular origin of plasma exosomes can lead to inconsistent results if tumor-associated exosomes are not specifically enriched [22].
Q3: Which biofluids show most promise for lncRNA-based HCC detection? Plasma and serum are the most extensively studied biofluids for lncRNA detection in HCC research [3] [23] [19]. Plasma is often preferred over serum as it contains fewer clotting-related contaminants. Emerging evidence also suggests that urine and saliva may serve as alternative, less invasive biofluid sources, though research on these for HCC detection remains preliminary [24] [17].
Q4: How can I validate the diagnostic performance of a candidate lncRNA biomarker? Robust validation should include: (1) Measuring expression levels in a sufficiently large, independent cohort of HCC patients and controls using RT-qPCR; (2) Calculating sensitivity, specificity, and area under the ROC curve (AUC) to assess diagnostic accuracy; (3) Comparing performance against established markers like AFP; and (4) Assessing correlation with clinical parameters (tumor stage, size, survival) [25] [19]. The identified lncRNA panel should be tested in both retrospective and prospective cohorts to ensure reliability [22].
Troubleshooting Common Experimental Issues
Low RNA Yield from Plasma Exosomes
Problem: Insufficient lncRNA quantity for downstream RT-qPCR or sequencing analysis.
Solutions:
- Increase starting material: Process larger plasma volumes (3-5 mL recommended) while ensuring proper storage at -80°C to prevent degradation [22].
- Optimize isolation method: Compare efficiency of different exosome isolation kits; affinity-based methods targeting EpCAM can enrich tumor-specific exosomes [22].
- Carrier RNA: Add glycogen or linear acrylamide as carrier during RNA precipitation to improve recovery of low-abundance lncRNAs.
- Quality control: Verify exosome isolation success through transmission electron microscopy, nanoparticle tracking analysis, and Western blot for markers (CD63, EpCAM) before RNA extraction [25] [22].
Inconsistent RT-qPCR Results
Problem: High variability in lncRNA quantification across technical replicates and samples.
Solutions:
- Normalization strategy: Use multiple reference genes (e.g., GAPDH, U6) and validate their stability in your experimental system [19].
- RNA integrity: Check RNA quality using Bioanalyzer; DV200 > 70% is recommended for long RNA species.
- Freeze-thaw cycles: Minimize repeated freeze-thaw cycles of both plasma samples and isolated RNA.
- PCR optimization: Determine optimal primer annealing temperatures and perform standard curves to ensure amplification efficiency between 90-110%.
Poor Specificity in Discriminating HCC from Chronic Liver Disease
Problem: Candidate lncRNAs show elevated levels in both HCC and patients with cirrhosis or hepatitis, leading to false positives.
Solutions:
- Multi-lncRNA panels: Develop biomarker panels combining multiple lncRNAs rather than relying on single markers [22].
- Combination with conventional markers: Integrate lncRNA data with AFP, DCP, or clinical parameters to improve specificity [19].
- Histological stratification: Ensure control groups include patients with benign liver conditions to properly assess specificity.
- Exosomal subpopulations: Isulate exosomes using tumor-specific surface markers (e.g., EpCAM) to enrich for cancer-derived lncRNAs [22].
Diagnostic Performance of Circulating lncRNAs in HCC
Table 1: Diagnostic Performance of Selected lncRNAs for HCC Detection
| lncRNA Name | Biofluid Source | Sensitivity (%) | Specificity (%) | AUC | Key Findings | Reference |
|---|---|---|---|---|---|---|
| LRB1 | Serum | 72.4 | 84.6 | 0.841 | Superior to AFP for early detection; levels decreased post-surgery | [19] |
| MALAT-1 | Plasma | 76.0 | 84.8 | 0.86 | Higher levels in HCC vs. healthy controls; correlates with tumor stage | [3] |
| HULC | Plasma | 75.2 | 79.3 | 0.82 | Significantly elevated in HCC patients | [3] |
| UCA1 | Serum | 68.9 | 82.1 | 0.79 | Discriminates HCC from liver cirrhosis | [3] |
| Combination Panel | Plasma Exosomes | 86.0 | 89.0 | 0.93 | Multi-lncRNA signature shows superior performance | [22] |
Table 2: Comparison of Exosome Isolation Methods for lncRNA Analysis
| Method | Principle | Advantages | Limitations | Recommended Use |
|---|---|---|---|---|
| Ultracentrifugation | Sequential centrifugation based on size/density | Gold standard; no chemical additives; high purity | Time-consuming; requires specialized equipment; low yield | Basic research; when high purity is critical |
| Precipitation (e.g., ExoQuick) | Polymer-based precipitation | Simple protocol; high recovery; suitable for small volumes | Co-precipitation of contaminants; may affect downstream applications | High-throughput studies; when yield is priority |
| Affinity Capture (e.g., EpCAM) | Antibody-based binding to surface markers | Tumor-specific isolation; high specificity | Limited to markers of interest; higher cost | Clinical applications; when specificity is crucial |
| Size-Exclusion Chromatography | Size-based separation in column | Good purity; maintains exosome integrity | Sample dilution; limited processing capacity | When functional studies are planned |
Experimental Protocols
Protocol for Isolation of EpCAM-Specific Exosomes from Plasma
Principle: Immunoaffinity capture using anti-EpCAM magnetic beads to isolate tumor-derived exosomes [22].
Materials:
- Anti-EpCAM magnetic beads (e.g., Dynabeads)
- Plasma samples (collected in heparin or EDTA tubes)
- Magnetic separation rack
- Phosphate-buffered saline (PBS)
- ExoStep Incubation Buffer
- Detachment solution (glycine-HCl, pH 2.5-3.0)
- Neutralization buffer (1M Tris-HCl, pH 8.0-8.5)
Procedure:
- Centrifuge plasma at 3,000 × g for 15 min at 4°C to remove cells and debris.
- Transfer 50 μL of clarified plasma to a tube containing 45 μL Incubation Buffer and 10 μL anti-EpCAM magnetic beads.
- Incubate overnight at 4°C with gentle rotation.
- Place tube in magnetic rack for 2 min, discard supernatant.
- Wash beads twice with 500 μL PBS.
- Add 100 μL detachment solution, incubate at 37°C for 2 hours to release exosomes from beads.
- Centrifuge at 2,500 × g for 5 min, collect supernatant containing Epexo.
- Neutralize with 10 μL neutralization buffer.
- Store isolated exosomes at -80°C or proceed to RNA extraction.
Quality Control:
- Verify exosome isolation by TEM and nanoparticle tracking [25] [22]
- Confirm presence of exosomal markers (CD63, EpCAM) by Western blot
- Check absence of negative markers (e.g., apolipoproteins)
Workflow for lncRNA Biomarker Discovery and Validation
Diagram 1: Comprehensive lncRNA Biomarker Development Workflow
Research Reagent Solutions
Table 3: Essential Research Reagents for Exosomal lncRNA Studies
| Reagent Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Exosome Isolation Kits | ExoQuick (SBI), Total Exosome Isolation (Thermo Fisher), exoRNeasy (Qiagen) | Isolation of exosomes from biofluids | Compare yield and purity; consider downstream applications |
| EpCAM Magnetic Beads | Dynabeads EpCAM (Thermo Fisher), EpCAM Antibody Magnetic Beads (Cell Biolabs) | Immunoaffinity capture of tumor-derived exosomes | Optimize antibody concentration and incubation time |
| RNA Extraction Kits | miRNeasy (Qiagen), Total RNA Purification Kit (Norgen) | Simultaneous isolation of long and small RNAs | Ensure effective lysis of exosomal membranes |
| RT-qPCR Reagents | TaqMan Advanced miRNA cDNA Synthesis Kit, SYBR Green Master Mix | lncRNA quantification | Design primers spanning exon-exon junctions |
| Reference Genes | GAPDH, U6, RNU44, miR-16-5p | Normalization of lncRNA expression | Validate stability across patient samples |
| Quality Control Tools | Bioanalyzer RNA chips, Nanosight NS300, CD63/EpCAM antibodies | Assessment of RNA and exosome quality | Implement standardized QC metrics |
Diagram 2: Experimental Design for Robust lncRNA Biomarker Studies
Advanced Detection Paradigms: Implementing Multi-Marker Panels and AI to Enhance Specificity
Technical Support Center: Troubleshooting lncRNA Panel Development
Frequently Asked Questions (FAQs)
Q1: Our single lncRNA assay (e.g., GAS5) shows promising initial sensitivity but high false positives in non-malignant liver disease controls. How can a multi-lncRNA panel address this? A1: Single lncRNAs can be dysregulated in various benign conditions, such as hepatitis or cirrhosis, leading to false positives. A panel combining lncRNAs with complementary biological roles and expression patterns increases specificity. For instance, while GAS5 might be downregulated in both HCC and cirrhosis, a second marker like UCA1, which is highly specific for malignant transformation, can be included. The concurrent assessment requires both markers to fit the diagnostic signature, effectively filtering out false positives from benign diseases.
Q2: What is the recommended method for validating the diagnostic performance of a proposed lncRNA panel? A2: A rigorous multi-phase approach is critical to minimize overfitting and ensure generalizability.
- Discovery Phase: Use RNA-Seq on a small cohort (e.g., HCC vs. normal/cirrhosis) to identify candidate lncRNAs.
- Training Phase: Develop and optimize RT-qPCR assays for the top candidates on a larger, well-defined cohort. Use statistical models (e.g., Logistic Regression) to build the multi-marker panel and establish a diagnostic score.
- Validation Phase: Blindly test the finalized panel and its score on a large, independent cohort to confirm its accuracy, sensitivity, and specificity.
Q3: We are observing high variability and inconsistent results in our RT-qPCR data for LINC00152. What are the primary sources of this error? A3: Inconsistency in RT-qPCR often stems from pre-analytical and analytical factors.
- Pre-analytical: Source of RNA (tissue vs. plasma), sample collection tubes (use RNase-free), and RNA extraction efficiency. Ensure consistent handling.
- Analytical: Poor primer design for lncRNAs (pseudogenes, low abundance), suboptimal cDNA synthesis, and lack of a stable normalization strategy. Always use a validated, lncRNA-specific primer set and include multiple reference genes (e.g., geometric mean of GAPDH, β-actin, and 18S rRNA) for robust normalization.
Q4: How do we functionally validate that the lncRNAs in our panel are not just correlative but have complementary roles in hepatocarcinogenesis? A4: Functional validation involves in vitro and in vivo experiments to dissect the mechanistic pathways.
- Gain/Loss-of-Function: Transfert HCC cell lines with siRNA/shRNA (knockdown) or overexpression plasmids for each lncRNA.
- Phenotypic Assays: Assess changes in proliferation (CCK-8 assay), apoptosis (Annexin V/PI staining), migration/invasion (Transwell assay).
- Mechanistic Studies: Perform RNA Immunoprecipitation (RIP) to identify protein partners (e.g., GAS5 binding to glucocorticoid receptor) or Chromatin Isolation by RNA Purification (ChIRP) to find DNA binding sites.
Experimental Protocols & Data
Protocol 1: RT-qPCR for Plasma lncRNA Quantification
- RNA Extraction: Isolate total RNA from 200-500 µL of plasma using a miRNeasy Serum/Plasma Kit (Qiagen). Include a spike-in synthetic RNA (e.g., C. elegans miR-39) to control for extraction efficiency.
- cDNA Synthesis: Use a reverse transcription kit with random hexamers and RNase inhibitor. Use a fixed input volume of RNA (e.g., 8 µL) per reaction.
- qPCR: Prepare reactions in triplicate using a SYBR Green master mix. Use lncRNA-specific primers.
- Cycling Conditions: 95°C for 10 min; 40 cycles of 95°C for 15 sec, 60°C for 1 min.
- Data Analysis: Calculate ∆Ct = Ct(lncRNA) - Ct(reference geometric mean). Use the comparative ∆∆Ct method for relative quantification.
Protocol 2: Functional Knockdown using siRNA in HepG2 Cells
- Cell Seeding: Seed HepG2 cells in a 12-well plate to reach 60-70% confluency at transfection.
- Transfection: Complex 50 nM of lncRNA-specific siRNA (or scrambled siRNA control) with Lipofectamine RNAiMAX in Opti-MEM. Add complexes to cells.
- Incubation: Incubate for 48-72 hours.
- Validation: Harvest cells. Extract RNA and perform RT-qPCR to confirm knockdown efficiency (>70% is ideal).
- Downstream Assay: Proceed with functional assays like Transwell invasion.
Table 1: Diagnostic Performance of Single lncRNAs vs. a Combinatorial Panel
| Biomarker | AUC | Sensitivity (%) | Specificity (%) | Cohort Size (HCC/Ctrl) | Key Limitation (False Positive Source) |
|---|---|---|---|---|---|
| LINC00152 | 0.84 | 78.5 | 81.0 | 120/100 | Chronic Hepatitis B |
| UCA1 | 0.88 | 82.0 | 85.5 | 120/100 | Early-stage sensitivity <70% |
| GAS5 | 0.79 | 75.0 | 80.5 | 120/100 | Liver Cirrhosis |
| Three-lncRNA Panel | 0.95 | 90.2 | 92.8 | 120/100 | Significantly reduced false positives |
Table 2: Research Reagent Solutions for lncRNA HCC Panel Studies
| Reagent / Kit | Function | Key Consideration |
|---|---|---|
| miRNeasy Serum/Plasma Kit (Qiagen) | Stabilizes and isolates high-quality cell-free RNA from liquid biopsies. | Critical for preventing RNA degradation in blood samples. |
| TaqMan Advanced lncRNA Assays (Thermo Fisher) | Provides pre-optimized, highly specific primers/probes for difficult lncRNA targets. | Reduces design time and minimizes off-target amplification. |
| Lipofectamine RNAiMAX (Thermo Fisher) | Efficiently delivers siRNA into hard-to-transfect hepatic cell lines for functional studies. | Low cytotoxicity is essential for subsequent viability assays. |
| CCK-8 Assay Kit (Dojindo) | Measures cell proliferation and viability sensitively and safely. | More sensitive and safer than traditional MTT assay. |
| Coriell Biorepository Samples | Provides well-characterized, ethically sourced human HCC and control tissue/RNA. | Ensures experimental reproducibility and ethical compliance. |
Pathway and Workflow Visualizations
Diagram 1: Complementary lncRNA Pathways in HCC
Diagram 2: Diagnostic Panel Development Workflow
Frequently Asked Questions (FAQs)
FAQ 1: What is the fundamental principle behind using lncRNA expression ratios, as opposed to measuring individual lncRNAs, for HCC diagnostics? The core principle is noise reduction and biological context. Individual lncRNA expression levels can be influenced by technical variations (e.g., sample collection, RNA extraction efficiency) and non-specific biological factors. Measuring a ratio between a consistently upregulated oncogenic lncRNA (like LINC00152) and a consistently downregulated tumor-suppressive lncRNA (like GAS5) inherently normalizes for this background noise. This ratio more accurately captures the functional balance within the cancer-related pathway, providing a sharper, more reliable signal of the tumor's biological state. Integrating this ratio with other data using machine learning models has been shown to significantly boost diagnostic performance, achieving up to 100% sensitivity and 97% specificity in distinguishing HCC from controls [26].
FAQ 2: Beyond LINC00152 and GAS5, what other lncRNA pairs show promise as diagnostic or prognostic ratios for HCC? Research indicates that other lncRNA pairs can form powerful diagnostic ratios. A key candidate is the combination involving UCA1 [26] [27]. While the LINC00152/GAS5 ratio has been directly linked to mortality risk, other panels often include UCA1 and LINC00853 to create a multi-marker signature [26]. The combination of LINC00152 and UCA1 has itself been validated for distinguishing HCC from liver cirrhosis and healthy controls, with both lncRNAs showing significant upregulation in HCC patient serum [27]. The future of biomarker development lies in exploring these multi-lncRNA ratio panels to capture the complexity of hepatocarcinogenesis.
FAQ 3: What is the most critical step in the qRT-PCR protocol to ensure the accuracy and reproducibility of my lncRNA expression ratio? The most critical step is rigorous normalization. While calculating a ratio provides some internal control, the integrity of the initial quantification is paramount. This involves:
- Using an Appropriate Housekeeping Gene: The housekeeping gene (e.g., GAPDH) must be validated for stable expression in your specific sample set (e.g., plasma from HCC patients versus controls) [26].
- Technical Replication: Each qRT-PCR reaction must be performed in triplicate to control for pipetting and instrument variability [26].
- Standardized RNA Handling: Use a validated kit (e.g., miRNeasy Mini Kit) for RNA isolation and a robust reverse transcription kit (e.g., RevertAid First Strand cDNA Synthesis Kit) to ensure high-quality cDNA synthesis [26]. Inconsistencies in these preparatory steps are a major source of false positives.
FAQ 4: My LINC00152/GAS5 ratio shows high values in some control samples. What could be causing these false positives? False positives can arise from several sources:
- Underlying Liver Disease: The control group must be carefully selected. Patients with pre-cirrhotic conditions, chronic viral hepatitis (HBV/HCV), or liver cirrhosis can exhibit dysregulated lncRNA expression even before malignant transformation [27]. Ensure your control group is free from significant liver pathology.
- Sample Purity: Hemolyzed blood samples can release cellular RNAs, altering the plasma lncRNA profile and leading to inaccurate ratios.
- Data Analysis Errors: Confirm that the quantification cycle (Cq) values for both lncRNAs are within the linear amplification range. Very high Cq values (low expression) for GAS5 can make the ratio volatile and unreliable. Re-inspecting the raw data and applying a minimum expression threshold for GAS5 may be necessary.
FAQ 5: How can I transition my researched lncRNA ratio from a diagnostic marker to a prognostic one? To establish prognostic value, your study design must shift from a cross-sectional to a longitudinal cohort approach. Instead of just comparing HCC patients to controls, you need to:
- Measure the LINC00152/GAS5 ratio in a cohort of HCC patients at diagnosis.
- Clinically follow these patients over time, tracking outcomes such as overall survival, disease-free survival, tumor recurrence, or metastasis.
- Perform statistical analysis (e.g., Cox regression) to determine if the ratio at diagnosis is an independent predictor of the later outcome. A 2019 meta-analysis confirmed that high LINC00152 expression alone is a significant prognostic factor for poor overall survival and lymph node metastasis in various solid tumors, providing a strong rationale for its use in a ratio [28].
Troubleshooting Guides
Issue 1: High Variability in qRT-PCR Results for GAS5 Quantification
Problem: The expression levels of the tumor suppressor GAS5, which is often lowly expressed in HCC samples, show high variability between technical replicates, making the ratio calculation unstable.
Solution:
- Confirm RNA Integrity: Check the RNA Integrity Number (RIN) using an instrument like a Bioanalyzer. Degraded RNA will disproportionately affect the quantification of less abundant transcripts like GAS5.
- Optimize cDNA Input: Titrate the amount of cDNA template in the qRT-PCR reaction. For low-abundance targets, increasing the cDNA input within the linear range can improve signal consistency.
- Switch Detection Chemistry: If using SYBR Green, design new primers and check for primer-dimer formation or non-specific amplification by analyzing the melt curve. Consider switching to a more specific probe-based assay (e.g., TaqMan) for GAS5.
- Validate in a Larger Cohort: Ensure the observed variability is not a true biological phenomenon by increasing your sample size.
Issue 2: Inconsistent Findings When Validating the LINC00152/GAS5 Ratio in an Independent Patient Cohort
Problem: A ratio that performed well in the initial discovery cohort fails to significantly distinguish HCC patients in a new, independent validation cohort.
Solution:
- Audit Cohort Demographics: Critically compare the clinical characteristics of your discovery and validation cohorts. Differences in etiology (e.g., HCV vs. HBV vs. NAFLD), disease stage (early vs. advanced HCC), or the proportion of patients with cirrhosis can drastically affect biomarker performance [27].
- Re-evaluate Pre-analytical Variables: Standardize sample processing protocols. Differences in plasma preparation, storage time, or freeze-thaw cycles between cohorts can introduce bias.
- Utilize Machine Learning: Instead of relying on a fixed ratio cutoff, use the lncRNA expression data (including the ratio) as features in a machine learning model (e.g., built with Scikit-learn in Python). These models can integrate multiple variables and are often more robust and generalizable to new populations [26] [29].
Issue 3: Poor Separation Between HCC and Cirrhosis Groups Using the Ratio
Problem: The LINC00152/GAS5 ratio is elevated in both HCC and liver cirrhosis groups, limiting its diagnostic specificity for early cancer detection.
Solution:
- Incorporate Additional Biomarkers: The LINC00152/GAS5 ratio is powerful but not infallible. Integrate it with other established biomarkers like Alpha-fetoprotein (AFP) or other lncRNAs (e.g., UCA1) to create a multi-parameter panel [26] [27]. A model combining lncRNAs with conventional lab data has been shown to achieve near-perfect classification [26].
- Refine the Ratio: Explore if a different ratio, such as (LINC00152 + UCA1) / GAS5, provides better discriminatory power for your specific patient population.
- Apply a Staging-Aware Model: Develop different ratio thresholds for patients with different stages of underlying liver disease, as the baseline level of "noise" may vary.
Experimental Protocol: Quantifying the LINC00152/GAS5 Expression Ratio from Plasma
Objective: To reliably extract, reverse transcribe, and quantify the expression of LINC00152 and GAS5 from human plasma samples for the calculation of a diagnostic and prognostic ratio.
Workflow Summary: The entire process, from sample collection to data analysis, is visualized below.
Materials and Reagents:
- Patient Plasma Samples: Collected in EDTA tubes from HCC, cirrhosis, and healthy control groups [26] [27].
- RNA Isolation Kit: miRNeasy Mini Kit (QIAGEN, cat no. 217004) [26].
- Reverse Transcription Kit: RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific, cat no. K1622) [26].
- qRT-PCR Master Mix: PowerTrack SYBR Green Master Mix (Applied Biosystems, cat no. A46012) [26].
- Primers: Validated primers for LINC00152, GAS5, and a housekeeping gene (e.g., GAPDH). Sequences from the literature [26]:
- LINC00152: Sense:
GACTGGATGGTCGCTTT, Antisense:CCCAGGAACTGTGCTGTGAA - GAS5: Sense:
TCCCAGCCTCAGACTCAACA, Antisense:TCGTGTCC...(ensure full sequence is obtained)
- LINC00152: Sense:
- qRT-PCR Instrument: ViiA 7 real-time PCR system or equivalent [26].
Step-by-Step Procedure:
- RNA Isolation: Isolate total RNA from 200-500 µL of plasma using the miRNeasy Mini Kit according to the manufacturer's protocol. Include a DNase digestion step to remove genomic DNA contamination.
- cDNA Synthesis: Reverse transcribe 200 ng-1 µg of total RNA into cDNA using the RevertAid Kit with oligo(dT) or random hexamer primers.
- qRT-PCR Setup and Run:
- Prepare reactions in triplicate for each sample. A 20 µL reaction should contain 10 µL SYBR Green Master Mix, 1 µL of forward and reverse primer mix, 2 µL of cDNA template, and 7 µL of nuclease-free water.
- Run on the real-time PCR system with the following cycling conditions: 95°C for 5 min, followed by 40 cycles of 95°C for 15 sec and 60°C for 1 min [26].
- Data Analysis:
- Calculate the average Cq value for each lncRNA and GAPDH from the triplicates.
- Normalize the Cq values using the ΔΔCq method:
ΔCq(target) = Cq(target) - Cq(GAPDH). - Calculate the relative expression:
2^(-ΔCq). - Compute the final ratio:
LINC00152/GAS5 Ratio = 2^(-ΔCq_LINC00152) / 2^(-ΔCq_GAS5).
Research Reagent Solutions
| Item | Function/Application in Research | Example Product/Catalog Number |
|---|---|---|
| Total RNA Purification Kit | Isolation of high-quality total RNA (including lncRNAs) from plasma/serum samples. | miRNeasy Mini Kit (QIAGEN, 217004) [26] |
| Reverse Transcription Kit | Synthesis of first-strand cDNA from RNA templates for subsequent PCR amplification. | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific, K1622) [26] |
| qRT-PCR Master Mix | Sensitive detection and quantification of lncRNA transcripts via fluorescence. | PowerTrack SYBR Green Master Mix (Applied Biosystems, A46012) [26] |
| Validated Primer Sets | Specific amplification of LINC00152, GAS5, and other target lncRNAs. | Custom oligonucleotides based on published sequences [26] |
| Housekeeping Gene Assay | Endogenous control for normalization of RNA input and loading variations. | GAPDH primer assay [26] |
The table below consolidates key performance metrics for the LINC00152/GAS5 ratio and related biomarkers from recent studies.
Table 1: Performance Metrics of lncRNA Biomarkers in Hepatocellular Carcinoma (HCC)
| Biomarker / Model | Diagnostic Accuracy (vs. Controls) | Prognostic Value | Key Clinical Association |
|---|---|---|---|
| LINC00152/GAS5 Ratio | N/A (Specific data not provided in search) | Significant correlation with increased mortality risk [26] | Serves as a functional indicator of oncogenic vs. tumor-suppressive balance [26] |
| Individual LINC00152 | Sensitivity: 60-83%, Specificity: 53-67% [26] | Independent predictor of poor outcome (HR=2.23) [27]; Linked to poor OS/DFS in solid tumors [28] | Lesions in both liver lobes [27] |
| Individual UCA1 | Data not provided | Not an independent prognostic factor in multivariate analysis [27] | Vascular invasion, late cancer stage [27] |
| Machine Learning Model | 100% Sensitivity, 97% Specificity [26] | Data not provided | Integrates lncRNA data with conventional lab parameters for superior diagnosis [26] |
Signaling Pathway Context
The prognostic power of the LINC00152/GAS5 ratio stems from its reflection of competing pathways in hepatocellular carcinoma. The following diagram illustrates the core mechanisms and how the ratio provides a functional readout.
Frequently Asked Questions (FAQs)
Q1: Our multi-lncRNA model is performing well on training data but generalizes poorly to independent validation cohorts. What could be the cause? A1: Poor generalization often stems from overfitting, especially with high-dimensional lncRNA data. A key strategy is to employ a machine learning-based integrative procedure. One established method involves testing numerous algorithm combinations (e.g., Lasso, Ridge, stepwise Cox) within a leave-one-out cross-validation (LOOCV) framework to identify the most robust model. The model with the highest average C-index across multiple validation datasets should be selected for its stability and generalizability [30] [31].
Q2: What is the best way to select immune-related lncRNAs for a prognostic model in cancer research? A2: We recommend a two-step process for selecting immune-related lncRNAs with high biological relevance:
- Use the ImmLnc Algorithm: This pipeline identifies lncRNAs significantly associated with immune-related pathways by calculating partial correlation coefficients and performing gene set enrichment analysis (GSEA). A standard threshold is an lncRES score >0.995 and FDR <0.05 [30] [31].
- Validate with WGCNA: Perform a consensus cluster analysis of tumor immune infiltration patterns. Then, use Weighted Gene Co-expression Network Analysis (WGCNA) to identify modules of lncRNAs highly correlated with these immune clusters. The overlap between ImmLnc results and hub lncRNAs from relevant WGCNA modules provides a high-confidence candidate list [31].
Q3: How can we functionally validate that a specific lncRNA from our model is involved in immune regulation? A3: While bioinformatics identifies candidates, functional validation is crucial. If your model and analyses like ssGSEA indicate that the low-risk group has enriched immune cell infiltration (e.g., CD8+ T cells), this provides indirect validation that the lncRNAs defining that group are associated with a favorable immune microenvironment [30] [31]. For direct validation, experimental workflows are required.
Q4: Our multi-omics data integration is complex. How can AI help improve the classification accuracy for HCC subtypes? A4: AI, particularly machine learning, excels at finding patterns in complex, multi-layered data. You can train models that integrate multi-omics data (e.g., lncRNA expression, mutational data, clinical variables) to identify distinct HCC subtypes with unique molecular signatures. These models can achieve high accuracy (AUC up to 0.85) in aiding early diagnosis and predicting responses to therapies like immune checkpoint blockade [7] [32].
Troubleshooting Guides
Issue: Model Performance is Highly Variable Across Different Algorithm Choices This occurs when a model is too reliant on the specificities of one algorithm or training dataset.
| Troubleshooting Step | Action | Expected Outcome |
|---|---|---|
| Algorithm Integration | Integrate multiple machine learning algorithms (e.g., Random Survival Forest, Lasso, SVM, CoxBoost) and compare their performance using the C-index [30] [31]. | Identification of a stable, high-performing algorithm combination that is robust across datasets. |
| Rigorous Validation | Validate the final model in multiple independent cohorts (e.g., from GEO or in-house cohorts) [30] [31]. | Confidence in the model's generalizability and clinical applicability. |
| Benchmarking | Compare your model's predictive power against traditional clinical variables and existing published signatures [31]. | Demonstrated superior accuracy and added value of your multi-lncRNA model. |
Issue: High False Positive Rate in Biomarker Discovery from High-Throughput Data False positives arise from analyzing thousands of lncRNAs without proper statistical correction.
| Troubleshooting Step | Action | Expected Outcome |
|---|---|---|
| Multiple Testing Correction | Apply strict False Discovery Rate (FDR) correction during initial differential expression and univariate Cox analysis [30]. | Reduction in false positives from random noise. |
| Consensus Clustering | Use consensus clustering to define robust molecular subtypes before identifying subtype-specific biomarkers [31]. | Identification of biomarkers tied to stable biological patterns, not cohort-specific noise. |
| Multi-Omics Corroboration | Cross-reference significant lncRNAs with other data types (e.g., mutations, immune cell infiltration scores) to ensure biological plausibility [7]. | A refined, high-confidence list of lncRNA biomarkers with supporting evidence. |
Experimental Protocols for Key Workflows
Protocol 1: Constructing a Robust Immune-Related lncRNA Prognostic Model
This protocol details the steps for building and validating a prognostic signature, a common application in the field [30] [31].
- Data Collection and Preprocessing:
- Obtain RNA-seq raw read count and clinical data from public databases like TCGA (training set) and GEO (validation sets).
- Filter samples to retain only those with complete essential clinical information (e.g., survival time, status, AJCC stage).
- Identify Prognostic Immune-Related lncRNAs:
- Immune Correlation: Use the
RpackageImmLncto identify lncRNAs significantly associated with immune pathways (lncRES score >0.995, FDR <0.05). - Survival Analysis: Perform univariate Cox regression analysis on the immune-related lncRNAs to identify those with significant prognostic value (p < 0.05).
- Immune Correlation: Use the
- Model Building and Integration:
- Subject the prognostic lncRNAs to a machine learning-based integrative procedure.
- Fit numerous models (e.g., Lasso, Enet, RSF, survival-SVM) using a LOOCV framework in the training set.
- Calculate the C-index for each model in all validation datasets.
- Select the optimal model based on the highest average C-index across all validation cohorts.
- Risk Score Calculation and Validation:
- Calculate a risk score for each patient using the formula:
Risk Score = Σ (LncRNA_Expression_i * Coefficient_i). - Divide patients into high- and low-risk groups based on the optimal cut-off value (e.g., median risk score).
- Validate the model's performance by assessing the survival difference between risk groups in the training and all validation sets using Kaplan-Meier analysis and log-rank tests.
- Calculate a risk score for each patient using the formula:
Protocol 2: Functional Characterization of Risk Groups
This protocol outlines analyses to biologically interpret the risk groups defined by your model [30].
- Tumor Immune Microenvironment (TIME) Analysis:
- Use algorithms like CIBERSORT or ssGSEA to estimate the proportions of various immune cells (e.g., T cells, B cells, macrophages) in each sample.
- Compare the immune cell infiltration scores between the high- and low-risk groups. Typically, the low-risk group displays abundant lymphocyte infiltration and higher expression of immune markers like CD8A and PD-L1.
- Genomic Mutation Analysis:
- Utilize the R package
maftoolsto analyze and visualize somatic mutation data (e.g., from TCGA). - Compare the tumor mutation burden (TMB) and the frequency of specific genomic mutations (e.g., in TP53, TTN) between the risk groups.
- Utilize the R package
- Drug Sensitivity Prediction:
- Use the R package
pRRopheticto predict the IC50 values of common chemotherapeutic and targeted drugs for each sample. - Analyze differences in predicted drug sensitivity between risk groups. Often, high-risk groups show sensitivity to certain chemotherapies, while low-risk groups may benefit more from immunotherapy.
- Use the R package
- Pathway Enrichment Analysis:
- Identify differentially expressed genes (DEGs) between the risk groups.
- Perform functional enrichment analysis (e.g., GO, KEGG) on the DEGs using the
clusterProfilerR package to identify biological pathways dysregulated in high-risk patients.
The following table details key materials and tools used in the development of multi-lncRNA classification models.
| Item Name | Function / Application | Relevance to Reducing False Positives |
|---|---|---|
| ImmLnc R Package | Identifies immune-related lncRNAs by correlating their expression with immune pathway activity [30] [31]. | Provides a biologically grounded starting point, filtering out lncRNAs with no immune context. |
| CIBERSORT/ssGSEA | Computational algorithms to deconvolute immune cell fractions from bulk tumor RNA-seq data [30] [31]. | Enables validation that the lncRNA signature is associated with a tangible immune phenotype. |
| maftools R Package | Analyzes, summarizes, and visualizes mutation annotation format (.maf) files from large-scale sequencing studies [30]. | Helps correlate lncRNA risk groups with genomic features, adding a layer of biological validation. |
| pRRophetic R Package | Predicts clinical chemotherapeutic response from tumor gene expression profiles [30]. | Tests the clinical utility of the model, a key step in moving from association to actionable insight. |
| The Cancer Genome Atlas (TCGA) | A public database containing genomic, epigenomic, and clinical data for over 20,000 primary cancers [30]. | Serves as a primary source for model training and discovery. |
| Gene Expression Omnibus (GEO) | A public functional genomics data repository supporting MIAME-compliant data submissions [30]. | Provides independent datasets essential for rigorous external validation of models. |
Technical Troubleshooting Guide: Addressing False Positives in lncRNA Detection
FAQ: What are the primary sources of false positives when detecting lncRNA biomarkers for HCC, and how can I mitigate them?
False positive results in lncRNA detection can arise from multiple sources in the experimental workflow, from sample collection to data analysis. The table below summarizes common issues and evidence-based solutions.
Table 1: Troubleshooting False Positives in lncRNA Liquid Biopsy for HCC
| Problem Source | Specific Issue | Recommended Solution | Supporting Evidence/Principle |
|---|---|---|---|
| Sample Purity | Contamination by genomic DNA in cfRNA prep. | Treat samples with DNase I. Include a no-reverse-transcriptase control in qPCR assays. | Ensures signal is from transcribed RNA, not genomic contamination [33]. |
| Assay Specificity | Cross-reactivity with homologous sequences or other lncRNAs. | Use locked nucleic acid (LNA) probes to increase binding specificity. In silico validate probes for unique regions. | Enhances hybridization stringency, reducing off-target binding [34]. |
| Sample Collection & Handling | Hemolysis; release of non-tumor-derived nucleic acids. | Use EDTA or specialized cfDNA/RNA blood collection tubes. Process plasma within 2-6 hours of draw. | Preserves sample integrity and reduces background noise from blood cell lysis [35] [36]. |
| Low Analytical Specificity | Inability to distinguish tumor-derived lncRNA from background. | Employ a multi-analyte approach. Use ctDNA mutations (e.g., CTNNB1) or CTC counts to corroborate lncRNA findings. | A signal confirmed by multiple independent analytes is less likely to be a false positive [37] [33]. |
| Data Analysis | Inadequate normalization to reference genes. | Identify and use stable reference genes (e.g., GAPDH, ACTB) validated for plasma/serum in HCC cohorts. | Corrects for technical variations in RNA extraction and reverse transcription [38]. |
FAQ: How can a multi-analyte approach specifically help reduce false positives in early HCC detection?
A multi-analyte approach leverages the orthogonal strengths of different biomarkers, where one analyte validates the findings of another. For instance, a positive signal from a specific lncRNA can be considered more reliable if it is accompanied by a confirmed ctDNA mutation or an abnormal cfDNA fragmentation profile (e.g., as detected by the DELFI method) [33]. This convergence of evidence from independent biological signals significantly increases the positive predictive value of the test. In the context of HCC, where the current standard biomarker Alpha-fetoprotein (AFP) has a sensitivity of only 47-64% [38], combining it with more specific molecular markers like lncRNAs, ctDNA, and CTCs can dramatically improve diagnostic accuracy and minimize false alarms that lead to unnecessary invasive procedures [36].
Experimental Protocols for a Multi-Analyte Workflow
The following protocol outlines a coordinated method for the simultaneous extraction and analysis of key liquid biopsy analytes, which is crucial for ensuring analyte compatibility and minimizing inter-assay variability.
Coordinated Multi-Analyte Extraction from Blood Plasma
Principle: This protocol is designed to process a single blood plasma sample to sequentially isolate cell-free nucleic acids (containing ctDNA and cfRNA/lncRNAs) and extracellular vesicles (EVs), from which additional RNA (including lncRNAs) can be extracted. The cellular pellet is used for Circulating Tumor Cell (CTC) enrichment [39] [34].
Reagents and Materials:
- Collection Tubes: K2EDTA blood collection tubes or specialized cell-free DNA blood collection tubes (e.g., Streck, Roche).
- PBS: Phosphate-buffered saline, RNase/DNase-free.
- cfDNA/RNA Extraction Kit: Commercially available kits for co-purification or sequential purification of cfDNA and cfRNA (e.g., QIAamp Circulating Nucleic Acid Kit, Norgen's Cell-Free RNA/DNA Purification Kit).
- EV Isolation Reagent: Commercially available polymer-based precipitation solution (e.g., from System Biosciences, Thermo Fisher).
- CTC Enrichment Kit: Immunomagnetic beads (positive or negative selection) or a microfluidic platform (e.g., Parsortix, ClearCell FX).
Procedure:
- Blood Collection and Plasma Separation: Draw blood into K2EDTA tubes. Process within 2-4 hours of collection.
- Centrifuge at 800-1,600 x g for 10-20 minutes at 4°C to separate plasma from blood cells.
- Carefully transfer the supernatant (plasma) to a new microcentrifuge tube without disturbing the buffy coat.
- Perform a second, high-speed centrifugation at 16,000 x g for 10 minutes at 4°C to remove any remaining cells and debris. Transfer the clarified plasma to a new tube. Aliquot as needed.
cfDNA and cfRNA Co-Extraction:
- Use 1-4 mL of clarified plasma as input for a commercial cfDNA/cfRNA extraction kit, following the manufacturer's instructions. This fraction will be used for ctDNA analysis and lncRNA quantification.
Extracellular Vesicle (EV) Isolation from Depleted Plasma:
- To the plasma supernatant remaining after cfDNA/RNA extraction (or a fresh aliquot), add an equal volume of EV Precipitation Reagent.
- Incubate overnight at 4°C.
- Centrifuge at 12,000 x g for 30-60 minutes at 4°C to pellet the EVs.
- Resuspend the EV pellet in PBS. Proceed to RNA extraction using a standard RNA isolation kit (e.g., miRNeasy Mini Kit) to obtain EV-derived RNA, which is enriched for lncRNAs.
CTC Enrichment from Cellular Pellet:
- Use the initial cellular pellet (buffy coat) obtained in step 1.
- Resuspend the cells in PBS and perform RBC lysis if necessary.
- Proceed with CTC enrichment using an immunomagnetic system (e.g., anti-EpCAM beads for positive selection) or a label-free microfluidic device based on cell size and deformability.
- The enriched CTCs can be used for downstream applications like RNA sequencing (for lncRNA expression), culture, or immunostaining.
Key lncRNA Detection and Quantification Protocol (Using RT-qPCR)
Principle: To accurately detect and quantify low-abundance lncRNAs from the cfRNA and EV-RNA extracts.
Reagents:
- Reverse Transcription Kit (e.g., High-Capacity cDNA Reverse Transcription Kit).
- LNA-enhanced qPCR Assays: Specifically designed for target lncRNAs.
- qPCR Master Mix (e.g., SYBR Green or TaqMan).
Procedure:
- Reverse Transcription: Convert the isolated total RNA (from cfRNA and EV fractions) into cDNA using a reverse transcription kit with random hexamers and/or oligo-dT primers.
- qPCR Setup:
- Design LNA-enhanced primers and probes for specific lncRNAs of interest (e.g., HOTAIR, MALAT1, HULC) and reference genes.
- Perform qPCR reactions in triplicate for each sample.
- Include negative controls (no-template control and no-RT control).
- Data Analysis: Use the comparative Cq (ΔΔCq) method to calculate relative expression levels of target lncRNAs, normalized to stable reference genes.
Visualizing the Multi-Analyte Workflow and Its Rationale
The following diagram illustrates the integrated experimental workflow and the synergistic relationship between different analytes in reducing false positives.
Integrated Multi-Analyte Workflow for HCC Detection
The Scientist's Toolkit: Essential Research Reagents & Materials
The successful implementation of a Liquid Biopsy 2.0 approach relies on a suite of specialized reagents and platforms. The table below details key solutions for this research.
Table 2: Research Reagent Solutions for Multi-Analyte Liquid Biopsy
| Item Name | Function / Application | Key Characteristics |
|---|---|---|
| Cell-Free DNA Blood Collection Tubes | Sample Collection & Stabilization | Contains preservatives to stabilize nucleated blood cells, preventing lysis and release of genomic DNA for up to 14 days, crucial for accurate cfDNA/RNA analysis [35]. |
| Microfluidic CTC Enrichment Platform | CTC Isolation | Label-free, size-based enrichment of CTCs; preserves cell viability for downstream functional studies and RNA analysis (e.g., Parsortix, ClearCell FX) [39]. |
| LNA-enhanced qPCR Probes | lncRNA Detection & Quantification | Significantly increases the thermal stability of probe:target duplexes, improving hybridization specificity and discrimination of single-nucleotide differences, reducing off-target signals [34]. |
| Targeted Sequencing Panels | ctDNA Mutation Profiling | Designed to detect hot-spot mutations in HCC (e.g., in TERT, TP53, CTNNB1) with high sensitivity (down to 0.1% variant allele frequency) from limited cfDNA input [37] [33]. |
| EV Isolation/Precipitation Reagent | Extracellular Vesicle Isolation | Polymer-based solution that efficiently precipitates EVs from large-volume plasma samples, enabling the study of the EV-enriched lncRNA subpopulation [34]. |
Optimizing the Workflow: From Pre-Analytical Sample Handling to Data Normalization
Standardized Protocols for Blood Collection and RNA Processing
Q: What are the best practices for collecting blood for lncRNA studies?
A standardized workflow for blood collection and processing is fundamental for reliable lncRNA analysis. The following diagram outlines the critical steps to ensure sample integrity.
Detailed Methodologies:
Blood Collection Tube Selection: Collect blood into tubes designed to stabilize cell-free RNA. A 2025 study systematically evaluated ten blood collection tubes and found that classic tubes (like EDTA) can outperform some manufacturer-designated preservation tubes for extracellular mRNA and miRNA analysis [40]. Consistency in tube type across a study is critical.
Sample Processing Timeline: Define and strictly adhere to time intervals between blood draw and processing. The same 2025 study assessed three processing time intervals, identifying that delays can critically interact with tube type and affect exRNA profiles [40]. Process samples within a pre-determined, consistent window (e.g., within 2 hours).
Plasma/Serum Isolation: Centrifuge blood samples using a standardized, double-spin protocol.
- First Spin: Lower speed (e.g., 2,000 × g for 10-20 minutes at 4°C) to separate plasma from cells.
- Second Spin: Higher speed (e.g., 16,000 × g for 10 minutes at 4°C) of the supernatant to remove any remaining platelets and debris.
- Always use a refrigerated centrifuge to minimize RNA degradation.
Q: Which RNA isolation methods are recommended for optimal lncRNA recovery?
The choice of RNA purification method significantly impacts the concentration, number of genes detected, and replicability of results [40].
Methodology for Evaluation: A comprehensive 2025 study evaluated eight RNA purification methods using robust z-score transformation of multiple performance metrics, including:
- Sensitivity: Absolute number of mRNAs and miRNAs detected.
- RNA Concentration: Determined via sequencing data and Femto Pulse electropherogram analysis.
- Replicability: Variability between technical replicates.
- Transcriptome Coverage: Diversity in mRNA capture sequencing reads [40].
Recommendations:
- For a given method, using the maximal allowable plasma input volume consistently resulted in higher RNA concentration, more detected genes, and better reproducibility [40].
- Methods that allow for a smaller eluate volume (or condensing the eluate post-purification) generally yield higher RNA concentrations, which is beneficial for downstream applications [40].
- Performance can vary significantly between methods, and critical interactions exist between the collection tube, purification method, and processing time. Pilot studies are recommended to determine the optimal combination for your specific research context [40].
Troubleshooting Common RNA Extraction Issues
Q: My extracted RNA is degraded. What could be the cause and how can I fix it?
RNA degradation is a common issue that can severely impact the detection of long RNA species like lncRNAs.
| Potential Cause | Solution |
|---|---|
| RNase Contamination | Ensure all centrifuge tubes, tips, and solutions are RNase-free. Wear gloves and use a dedicated clean area [41]. |
| Improper Sample Storage | Use fresh samples or store them stably at -80°C. Avoid repeated freezing and thawing by storing samples in single-use aliquots [41]. |
| Prolonged Processing Time | Reduce the time between blood collection and RNA stabilization/isolation. Follow a standardized processing timeline [42]. |
Q: My RNA sample has genomic DNA contamination. How do I remove it?
| Potential Cause | Solution |
|---|---|
| High Sample Input | Reduce the starting sample volume or increase the volume of the lysis reagent [41]. |
| Inefficient DNase Treatment | Use RNA purification kits that include a DNase digestion step. Alternatively, use reverse transcription reagents that contain a genomic DNA removal module [41]. |
| Primer Design | When designing qPCR primers for lncRNAs, use trans-intron primers that span an exon-exon junction to avoid amplification from genomic DNA [41]. |
Q: My RNA yield is low. What can I do to improve it?
| Potential Cause | Solution |
|---|---|
| Incomplete Homogenization | Optimize homogenization conditions to ensure complete disruption of cells and release of RNA [41]. |
| Too Much Starting Sample | Excessive sample can lead to incomplete homogenization and inefficient RNA release. Adjust sample amount to the recommended protocol input [41]. |
| Incomplete RNA Precipitation | For small tissue or cell quantities, ensure the volume of TRIzol or similar reagent is proportionally reduced to prevent excessive dilution. For low-concentration samples, add glycogen as a carrier to aid precipitation [41]. |
| RNAase Contamination | As above, stringent measures to prevent RNAase contamination are essential to preserve yield [41]. |
Specific Solutions for lncRNA HCC Biomarker Detection
Q: How can pre-analytical variability lead to false positives in lncRNA-based HCC detection?
Reducing variability is crucial to ensure that observed changes in lncRNA levels are due to the disease state (HCC) and not pre-analytical artifacts. The relationship between pre-analytical factors and false results is summarized below.
Mechanisms Leading to False Results:
- Inconsistent RNA Stabilization: If blood samples are not processed or stabilized uniformly, degradation of lncRNAs can occur at different rates. A partially degraded sample might show artificially low levels of a tumor-suppressor lncRNA (e.g., GAS5), mimicking the profile of an HCC patient and leading to a false positive interpretation [4] [42].
- Hemolysis and Cellular Contamination: Improper blood handling or centrifugation can cause hemolysis or release of cellular RNA from blood cells. This releases abundant cellular RNAs that can mask the signal from low-abundance, disease-specific circulating lncRNAs (like LINC00152 or UCA1), or introduce background noise that varies between samples [42] [40].
- Variable Extraction Efficiency: Using different RNA purification methods or protocols across a study can lead to significant variations in the yield and purity of lncRNAs. A method with poor efficiency might fail to recover a key lncRNA biomarker, resulting in a false negative [40].
Q: What integrative strategies can enhance the specificity of HCC detection?
Beyond standardizing pre-analytical steps, the following strategies can help minimize false positives:
- Utilize Machine Learning (ML) Models: Relying on a single lncRNA biomarker can be error-prone. A 2024 study on HCC screening achieved 100% sensitivity and 97% specificity by using a machine learning model that integrated the expression of four lncRNAs (LINC00152, LINC00853, UCA1, GAS5) with conventional laboratory biomarkers (like AFP, ALT, AST) [4]. This multi-parameter approach is more robust to pre-analytical noise.
- Employ lncRNA Ratios: The same study found that the expression ratio of two lncRNAs (e.g., a higher LINC00152 to GAS5 ratio) was a more reliable prognostic indicator than the level of either lncRNA alone [4]. Using internal ratios can help control for technical variations.
Frequently Asked Questions (FAQs)
Q: What is the difference between accuracy and precision in the context of this research?
- Accuracy refers to how close a measured value (e.g., lncRNA concentration) is to the true or accepted value. It is affected by systematic errors, which are consistent, reproducible biases (e.g., from an uncalibrated pipette) [43] [44].
- Precision refers to the repeatability of measurements—how close repeated measurements are to each other. It is affected by random errors, which are unpredictable fluctuations (e.g., minor variations in tube inversion during mixing) [43] [44]. High pre-analytical vigilance improves both accuracy and precision.
Q: Why is the pre-analytical phase particularly critical for multicenter clinical trials?
In multicenter trials, laboratory analyses are often centralized to reduce analytical variability. However, this dramatically magnifies the impact of pre-analytical variables (collection, processing, storage, and shipment of samples from multiple sites). Inconsistent pre-analytical practices across different clinical centers can introduce significant bias, potentially leading to the misinterpretation of a drug's efficacy or the performance of a biomarker [42].
Q: Can I use PAXgene and RNAlater tubes interchangeably for lncRNA studies?
No, the choice of stabilization system should be consistent and validated for your specific application. A 2010 study comparing PAXgene and RNAlater for RNA stabilization in blood found that while both were appropriate, RNAlater provided superior RNA yield and integrity values [45]. Furthermore, a 2025 study highlighted critical interactions between collection tubes and downstream RNA purification methods [40]. Switching tubes mid-study introduces a major variable that can compromise data integrity.
Research Reagent Solutions
The following table details key materials and their functions for standardizing pre-analytical workflows in lncRNA research.
| Item | Function/Benefit |
|---|---|
| EDTA Blood Collection Tubes | Classic anticoagulant tubes; a 2025 study found they can perform well for exRNA analysis when processing is timely [40]. |
| Cell-Free RNA Stabilization Tubes | Specialized tubes (e.g., Streck cfRNA BCT) designed to stabilize extracellular RNA in whole blood for longer periods before processing. |
| RNA Purification Kits (Plasma/Serum) | Kits specifically designed for low-abundance RNA in biofluids (e.g., miRNeasy Advanced, Norgen, others). Performance varies, so select based on metrics like sensitivity and replicability [40]. |
| RNase Inhibitors | Additives used in lysis buffers or during sample preparation to protect RNA from degradation by ubiquitous RNases. |
| Synthetic Spike-In RNAs | Added to samples at the start of RNA extraction to monitor purification efficiency, quantify recovery, and control for technical variation during library preparation and sequencing [40]. |
| DNase I Enzyme | Critical for removing contaminating genomic DNA during RNA purification, preventing false positive signals in qPCR or sequencing. |
In the pursuit of reliable hepatocellular carcinoma (HCC) biomarkers, the accurate detection of long non-coding RNAs (lncRNAs) using quantitative real-time PCR (qRT-PCR) is paramount. The inherent challenges of lncRNA biology—including low abundance, overlapping transcripts, and multiple isoforms—can significantly contribute to false-positive results if not meticulously addressed. This technical guide provides detailed protocols and troubleshooting advice to ensure primer specificity, optimize reaction conditions, and implement robust validation workflows. By adhering to these guidelines, researchers can enhance the reproducibility and accuracy of their data, thereby strengthening the validation of lncRNAs as clinical biomarkers for HCC.
The Scientist's Toolkit: Essential Reagents for lncRNA qRT-PCR
The table below lists key reagents and their critical functions for successful lncRNA quantification.
Table 1: Key Research Reagent Solutions for lncRNA qRT-PCR
| Reagent / Kit | Function in lncRNA qRT-PCR | Key Considerations |
|---|---|---|
| High Pure miRNA Isolation Kit (Roche) | Isolation of total RNA, including the lncRNA fraction, from tissue and cell lines [46]. | Ensures high-quality RNA input; critical for downstream accuracy. |
| PrimeScript RT Reagent Kit with gDNA Eraser (Takara) | Genomic DNA (gDNA) removal and subsequent cDNA synthesis [47]. | A dedicated gDNA removal step is non-negotiable for eliminating false positives from genomic contamination. |
| SYBR Premix Ex Taq II (Takara) | SYBR Green dye-based master mix for qPCR amplification [47]. | Provides high sensitivity and allows for melt curve analysis to verify amplicon specificity. |
| LncProfiler qPCR Array Kit (SBI) | A commercial system for quantifying 90 lncRNAs in a single run [46]. | Useful for screening; includes a optimized cDNA synthesis method with polyA-tailing and adaptor-anchoring. |
Optimized Experimental Workflow for lncRNA Detection
The following diagram outlines a standardized workflow, from sample preparation to data analysis, designed to minimize variability and false positives.
Core Methodology: Detailed qRT-PCR Protocol for lncRNA Validation
This section provides a step-by-step protocol for validating lncRNA expression, adapted from established methods [48] [47].
Step 1: RNA Isolation and Quality Control
- Isolate total RNA using a kit that guarantees high recovery of long RNA fragments, such as the High Pure miRNA isolation kit [46].
- Quantify RNA using a spectrophotometer (e.g., NanoDrop) and assess integrity via native agarose gel electrophoresis to confirm the presence of sharp 28S and 18S rRNA bands. High-quality RNA is a prerequisite for reliable lncRNA quantification [46].
Step 2: Genomic DNA Removal and cDNA Synthesis
- Treat 1 µg of total RNA with a gDNA Eraser to eliminate contaminating genomic DNA [47].
- Perform reverse transcription using a robust cDNA synthesis kit. For lncRNAs, kits that use random hexamer primers preceded by polyA-tailing and an adaptor-anchoring step have been shown to provide lower Ct values (indicating higher sensitivity) for 67.78% of lncRNAs compared to simpler methods [46].
- Critical Note: Using only oligo(dT) primers is not recommended for many lncRNAs, as they may lack poly-A tails [46] [49].
Step 3: Quantitative PCR Amplification
- Prepare the reaction mix using a SYBR Green master mix.
- Use the following thermocycling conditions on an instrument such as an ABI7500 [47]:
- Initial Denaturation: 95°C for 30 seconds.
- 40 Cycles:
- Denaturation: 95°C for 5 seconds.
- Annealing/Extension: 60°C for 30 seconds.
- Immediately perform a melt curve analysis to verify amplification of a single, specific product:
- 94°C for 60 seconds.
- 37°C for 60 seconds.
- 72°C for 120 seconds (with continuous fluorescence acquisition).
Step 4: Data Analysis
- Calculate the relative expression levels (fold change) using the comparative 2−ΔΔCt method.
- Use at least two validated reference genes (e.g., Actin (Act) and Tubulin (Tua)) for normalization to ensure accurate results [48].
Technical FAQs and Troubleshooting Guide
Q1: Why is my amplification plot irregular, and how can I improve primer specificity for lncRNAs?
- Cause: Non-specific amplification or primer-dimer formation, often due to the complex secondary structures of lncRNAs or primers designed to non-unique regions.
- Solutions:
- Design Primers Across Exon-Exon Junctions: For multi-exon lncRNAs, design primers that span a splice junction. This prevents amplification from any contaminating genomic DNA that might have escaped digestion [50].
- Target a Unique Region: Use tools like Primer3 or IDT PrimerQuest to design primers that target a unique exon or a specific splice junction site of the lncRNA transcript, distinguishing it from other isoforms or overlapping genes [48] [50].
- Check for Secondary Structures: Analyze the predicted secondary structure of your lncRNA and use in-silico tools to ensure your primers are not binding to highly structured regions. Also, check primers themselves for self-complementarity (hairpins) or heterodimer formation [48].
Q2: My cDNA synthesis seems inefficient, leading to high Ct values. How can I optimize it for lncRNAs?
- Cause: Standard cDNA synthesis kits using only oligo(dT) primers are inefficient for lncRNAs that lack a poly-A tail.
- Solutions:
- Use a Superior cDNA Synthesis Method: A study comparing kits found that using random hexamer primers preceded by polyA-tailing and an adaptor-anchoring step yielded lower Ct values (higher sensitivity) for the majority (67.78%) of lncRNAs tested [46].
- Use a Blend of Primers: Kits that employ a blend of random hexamer and oligo(dT) primers can also be effective, offering a balance for quantifying both polyadenylated and non-polyadenylated RNAs [50].
Q3: How does RNA degradation impact lncRNA quantification, and how should I handle my samples?
- Cause: RNA degradation is a common issue during sample collection and storage.
- Solutions:
- Do Not Assume Stability: While one study found that for 83% of lncRNAs tested, degradation did not strongly influence quantification, a significant portion (70%) still showed statistically different Ct values in degraded samples [46].
- Prioritize RNA Quality: Always start with high-quality RNA (with clear 28S and 18S bands on a gel) for the most accurate and reproducible results. The stability of lncRNAs can be sequence-dependent, so it should not be generalized [46].
Q4: What is the critical control experiment I must include to rule out false positives from genomic DNA?
- Solution: Always include a "No-Reverse Transcriptase" control (-RT control) in your experiment. This reaction contains all PCR components except the reverse transcriptase enzyme. A signal in the -RT control indicates amplification from contaminating genomic DNA, which will lead to false-positive results. The gDNA Eraser step is designed to prevent this [47].
Molecular Context: The Role of lncRNAs in HCC
Understanding the biological function of your target lncRNA is crucial for interpreting qRT-PCR results. In HCC, lncRNAs often function as competitive endogenous RNAs (ceRNAs), acting as molecular sponges for miRNAs. The following diagram illustrates this common mechanism, disruption of which can be a key event in hepatocarcinogenesis.
For example, the lncRNA SNHG1 is upregulated in HCC and acts as a ceRNA, sponging miR-195-5p to increase the expression of the oncogenic protein PDCD4, thereby promoting tumorigenesis [20]. Accurate quantification of SNHG1 levels via qRT-PCR is therefore critical for understanding its role in HCC progression.
In the pursuit of reliable hepatocellular carcinoma (HCC) biomarkers, long non-coding RNAs (lncRNAs) have emerged as promising candidates due to their tissue-specific expression and roles in tumorigenesis. However, the accurate quantification of these molecules is hampered by their characteristically low abundance and high tissue specificity, which predisposes detection assays to false positives when normalization is suboptimal. Proper normalization against stable reference genes is not merely a technical step but a fundamental prerequisite for generating clinically translatable data in HCC biomarker research.
The challenge is particularly acute in HCC studies, where sample heterogeneity, varying etiologies (viral, alcoholic, metabolic), and complex tumor microenvironments can significantly influence gene expression patterns. Without robust normalization strategies, technically driven variations can be misinterpreted as biological signals, leading to erroneous conclusions and failed biomarker validation. This guide provides troubleshooting resources and methodological frameworks to overcome these challenges, with a specific focus on reducing false positives in lncRNA-based HCC detection.
Understanding lncRNA Characteristics and Associated Technical Challenges
Long non-coding RNAs are defined as functional RNA molecules longer than 200 nucleotides that lack significant protein-coding potential [51]. Unlike messenger RNAs, lncRNAs exhibit distinctive characteristics that pose unique challenges for accurate quantification:
- Low Abundance: Most lncRNAs are expressed at significantly lower levels than mRNAs, making them more susceptible to technical noise and detection limits [52].
- Tissue-Specific Expression: lncRNAs demonstrate highly restricted expression patterns, with the mammalian brain alone expressing approximately 40% of known lncRNAs [53]. This specificity is valuable for biomarker development but complicates reference gene selection.
- Subcellular Localization: Many lncRNAs are retained in the nucleus or localized to specific cellular compartments, creating potential fractionation biases during RNA extraction [53].
- Less Evolutionary Conservation: lncRNAs show lower sequence conservation across species compared to protein-coding genes, limiting the transferability of normalization strategies from model organisms [51].
Table 1: Technical Challenges in lncRNA Quantification and Their Consequences
| Challenge | Impact on Quantification | Risk of False Positives/Negatives |
|---|---|---|
| Low Abundance | Increased technical variation, lower signal-to-noise ratio | High risk of both false positives and negatives |
| Tissue Specificity | Reference gene stability varies across tissue types | False positives when using pan-tissue reference genes |
| Complex Isoforms | Multiple transcript variants may not be equally detected | Underestimation or overestimation of total expression |
| Nuclear Enrichment | Differential recovery during RNA extraction | Biased quantification if reference genes are cytoplasmic |
Frequently Asked Questions (FAQs): Troubleshooting Normalization Issues
Q1: Why can't I use GAPDH and β-actin as reference genes for lncRNA quantification in HCC studies?
While GAPDH and β-actin are commonly used as reference genes, their expression can vary significantly in HCC due to the metabolic reprogramming of tumor cells and changes in cytoskeletal architecture. For example, studies analyzing m6A RNA modification in HCC have utilized normalization against traditional housekeeping genes but complemented this with extensive stability validation [54]. The high metabolic activity in HCC tumors particularly affects GAPDH expression, making it unstable across different tumor stages and etiologies.
Q2: How many reference genes should I include for reliable lncRNA normalization?
Current evidence suggests that using a minimum of three validated reference genes provides significantly more reliable normalization than single reference genes. Research on migrasome-related lncRNAs in HCC has employed computational algorithms to select multiple stable reference genes based on large HCC datasets [55]. The precise number should be determined through stability analysis using algorithms like geNorm or NormFinder, with stability values (M-values) below 0.5 being generally acceptable for most applications.
Q3: My candidate lncRNA shows significant expression in cell lines but not in patient tissues. Is this a normalization artifact?
This pattern commonly indicates normalization issues. Cell lines often have different growth conditions and lack the complex microenvironment of primary tissues, which can affect reference gene stability. Troubleshoot this by:
- Validating your reference genes in both cell lines and primary tissues
- Ensuring RNA quality is consistent between samples (RIN >7)
- Testing multiple reference genes specifically validated for HCC tissue
- Using spike-in controls to account for extraction efficiency differences
Q4: How does RNA quality specifically affect lncRNA quantification and normalization?
RNA quality significantly impacts lncRNA quantification because longer transcripts (including many lncRNAs) degrade more rapidly than shorter reference genes. This differential degradation creates a bias where lncRNA expression appears lower in partially degraded samples even after normalization. Always document RNA Integrity Numbers (RIN) and establish a minimum quality threshold (typically RIN >7) for all samples in your analysis.
Experimental Protocols for Reference Gene Validation
Comprehensive Workflow for Reference Gene Selection
The following diagram illustrates the systematic approach to selecting and validating reference genes for lncRNA quantification in HCC research:
Candidate Gene Selection and Experimental Design
Step 1: Candidate Reference Gene Selection Select 10-15 candidate reference genes from diverse functional classes to minimize co-regulation:
- Traditional housekeeping: GAPDH, ACTB, B2M
- Ribosomal proteins: RPLP0, RPS18, RPS29
- Transcriptional factors: POLR2A, TBP
- Cytoskeletal: TUBA1B, TUBB
- Metabolic: HPRT1, PGK1
Step 2: Experimental Design Include biological replicates that represent the entire scope of your study:
- For HCC studies: include normal liver, cirrhotic tissue, early HCC, and advanced HCC
- Account for different etiologies (HBV, HCV, NAFLD)
- Include technical replicates to assess assay variability
- Balance samples by age, sex, and tissue quality where possible
Step 3: RNA Extraction and Quality Control
- Use standardized RNA extraction protocols across all samples
- Document RNA concentration, purity (A260/280 ratio >1.8), and integrity (RIN >7)
- Use the same RNA input amount for all reverse transcription reactions
- Perform reverse transcription under identical conditions using random hexamers
qPCR Analysis and Stability Validation
Step 4: qPCR Analysis
- Design primers with similar annealing temperatures (60°C ± 2°C)
- Ensure amplification efficiencies between 90-110% with R² > 0.98
- Include no-template controls for each primer pair
- Use uniform cycling conditions across all plates
- Implement inter-run calibrators for multi-plate experiments
Step 5: Stability Analysis Utilize algorithm-based approaches to determine the most stable reference genes:
Table 2: Stability Analysis Algorithms for Reference Gene Selection
| Algorithm | Primary Metric | Interpretation | Advantages |
|---|---|---|---|
| geNorm | M-value (average pairwise variation) | Lower M-value indicates higher stability | Identifies optimal number of reference genes |
| NormFinder | Stability value based on intra- and inter-group variation | Accounts for sample subgroups | Robust against co-regulated genes |
| BestKeeper | Pearson correlation coefficient | Higher correlation indicates better stability | Works with raw Ct values |
| ΔCt method | Pairwise variability | Compares candidates against each other | Simple implementation |
Step 6: Final Validation Validate your selected reference genes by measuring the expression of a well-characterized target across your sample set using both single and multiple reference genes for normalization. The variation should decrease significantly with the optimized reference gene panel.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Research Reagent Solutions for Robust lncRNA Quantification
| Reagent/Platform | Function | Application Notes |
|---|---|---|
| RNA Spike-in Controls | Normalization for extraction efficiency | Particularly crucial for low-abundance lncRNAs; use synthetic RNA sequences not found in humans |
| High-Quality Reverse Transcriptase | cDNA synthesis | Use enzymes with high processivity for long transcripts; maintain consistent reaction conditions |
| qPCR Master Mix with High Specificity | Amplification detection | Select mixes designed to minimize primer-dimer formation; include SYBR Green or probe-based options |
| Pre-Designed Reference Gene Panels | Stability assessment | Commercial panels include multiple validated reference genes with optimized primer sets |
| RNA Integrity Analyzer | Quality control | Essential for documenting RIN values; critical for interpreting quantification results |
| Cross-Platform Validation Tools | Data harmonization | Tools like SurvivalML help normalize data across different platforms and cohorts [56] |
Advanced Normalization Strategies for Multi-Platform Studies
Contemporary lncRNA biomarker discovery often requires integration of data across multiple platforms and studies. The SurvivalML platform addresses this need by implementing comprehensive preprocessing pipelines that include re-annotation, normalization, and data cleaning to improve consistency across datasets and technologies [56]. This approach is particularly valuable for HCC lncRNA studies aiming to validate findings across independent cohorts.
For projects involving single-cell RNA sequencing, additional normalization considerations apply. The Seurat package provides specialized functions for normalizing single-cell data, including approaches that account for the unique characteristics of lncRNA expression patterns at single-cell resolution [54].
Diagram: Housekeeping Gene Validation Workflow
The following workflow outlines the critical steps for validating reference genes specifically for lncRNA studies in HCC research:
Reducing false positives in lncRNA HCC biomarker detection requires meticulous attention to normalization strategies. By implementing the troubleshooting guides, experimental protocols, and validation workflows outlined in this technical support center, researchers can significantly enhance the reliability of their lncRNA quantification data. The key principles include: (1) always validating reference genes in your specific experimental system, (2) using multiple reference genes rather than relying on a single one, (3) documenting and controlling for RNA quality, and (4) utilizing computational tools to harmonize data across platforms. Through these rigorous approaches, the HCC research community can advance more reliable biomarkers toward clinical application.
The discovery of long non-coding RNA (lncRNA) biomarkers for hepatocellular carcinoma (HCC) represents a promising frontier in cancer diagnostics and personalized medicine. However, the high-dimensional nature of transcriptomic data, where thousands of lncRNAs are measured across relatively few patient samples, creates substantial challenges in distinguishing true biological signals from background noise. Establishing statistically validated clinical cut-offs is therefore essential to ensure that biomarker signatures are reliable, reproducible, and clinically actionable.
Statistical false discovery occurs when biomarkers are incorrectly identified as associated with a disease or clinical outcome due to random chance rather than true biological relationship. In the context of lncRNA biomarker development for HCC, this can lead to wasted resources in validation studies, incorrect biological conclusions, and ultimately, failed clinical applications. The False Discovery Rate (FDR) has emerged as a preferred framework for addressing this challenge, as it offers greater statistical power than traditional family-wise error rate controls while providing interpretable guarantees about the reliability of discovered biomarkers [57] [58].
This technical support guide provides researchers with practical methodologies for establishing statistically validated thresholds in lncRNA-HCC biomarker research, with particular emphasis on controlling false positives throughout the discovery and validation pipeline.
Understanding False Discovery Rate (FDR) in Biomarker Research
Core Concepts and Definitions
False Discovery Rate (FDR) is defined as the expected proportion of false discoveries among all features called significant. An FDR of 5% means that among all biomarkers identified as significant, approximately 5% are expected to be truly null (false positives) [57]. This contrasts with the Family-Wise Error Rate (FWER), which represents the probability of making at least one false discovery among all hypothesis tests. In genomic studies where thousands of lncRNAs are tested simultaneously, controlling FWER using traditional methods like Bonferroni correction is often overly conservative, leading to many missed findings [57] [58].
The q-value is the FDR analog of the p-value. While a p-value threshold of 0.05 yields a false positive rate of 5% among all truly null features, a q-value threshold of 0.05 yields an FDR of 5% among all features called significant. This distinction is crucial for proper interpretation in high-dimensional biomarker studies [57].
FDR Control Methods Comparison
Table 1: Comparison of Multiple Testing Correction Methods
| Method | Error Controlled | Approach | Best Use Case | Limitations |
|---|---|---|---|---|
| Bonferroni | FWER | Divides significance threshold (α) by number of tests | Small number of hypotheses; confirmatory studies | Overly conservative for genomic studies; low power |
| Benjamini-Hochberg | FDR | Orders p-values and uses step-up procedure | Large-scale exploratory studies | Assumes independent or positively dependent tests |
| Knockoff Framework | FDR | Creates "fake" knockoff variables as controls | High-dimensional data with correlated features | Computationally intensive; requires specialized implementation |
| Bootstrap/Resampling | FDR | Uses resampling to estimate null distribution | Complex dependency structures | May require smoothness assumptions for validity |
Troubleshooting Guide: Common FDR Challenges in lncRNA Biomarker Studies
FAQ 1: Why do my lncRNA biomarkers fail to validate in independent cohorts despite strong initial p-values?
Issue: This commonly occurs when false discovery control is inadequate during the discovery phase. With thousands of lncRNAs tested simultaneously, even stringent p-value thresholds (e.g., p < 0.001) may still yield numerous false positives due to multiple testing burden.
Solution:
- Implement FDR control rather than relying solely on p-values. Use q-values to select biomarkers, with a threshold typically set at q < 0.05 or q < 0.10 depending on the exploratory nature of the study [57].
- Apply the knockoff framework, which creates "fake" knockoff variables that mimic the correlation structure of real lncRNAs but are known to be null. The selection frequency of knockoff variables provides a robust benchmark for FDR control [58].
- For studies using machine learning approaches, incorporate embedded FDR control methods rather than relying solely on cross-validation, which does not directly control false discoveries [58].
Experimental Protocol: When analyzing RNA-Seq data from 50 HCC tissues and 50 matched controls:
- Perform differential expression analysis using DESeq2 or edgeR to obtain p-values for each lncRNA [59] [60].
- Calculate q-values using the Benjamini-Hochberg procedure or more robust empirical methods.
- Construct knockoff variables using the model-free knockoff framework to account for the complex correlation structure among lncRNAs.
- Select lncRNAs with q < 0.05 and that significantly outperform their knockoff counterparts.
FAQ 2: How can I determine the optimal sample size for adequate power while controlling FDR in lncRNA biomarker discovery?
Issue: Underpowered studies either detect only the strongest signals (missing true biomarkers) or generate an unacceptably high proportion of false discoveries when liberal thresholds are applied.
Solution:
- Perform power analysis specifically designed for FDR control settings rather than traditional power calculations based on individual hypothesis tests.
- Use pilot data to estimate the proportion of truly alternative lncRNAs (π1 = 1 - π0) and effect sizes to inform sample size planning.
- Consider the dependency structure among lncRNAs, as independent assumption-based calculations may be inaccurate.
Experimental Protocol: For planning an lncRNA biomarker study targeting FDR < 0.10:
- Conduct a pilot study with 20-30 samples per group to estimate effect sizes and correlation structure.
- Use the
pwrpackage in R or specialized FDR power analysis tools to determine sample size needed to detect the anticipated effect sizes with adequate power. - For high-dimensional settings, consider simulation-based power calculations that incorporate the estimated correlation structure from pilot data.
- Allocate sufficient samples for an independent validation cohort (typically 30-50% of discovery sample size).
FAQ 3: How should I handle highly correlated lncRNAs when establishing clinical cut-offs?
Issue: Co-expressed lncRNAs can lead to spurious correlations with clinical outcomes, where multiple lncRNAs in the same regulatory network are all selected as biomarkers, inflating false discoveries.
Solution:
- Implement the knockoff framework, which specifically accounts for correlation structure among features [58].
- Use clustering or network-based methods to group correlated lncRNAs prior to biomarker selection.
- Apply penalized regression methods (e.g., elastic net) that naturally handle correlated features, coupled with FDR control procedures validated for such methods.
Experimental Protocol: When dealing with correlated lncRNA clusters in HCC data:
- Perform weighted gene co-expression network analysis (WGCNA) to identify modules of correlated lncRNAs [61].
- Within each module, select representative lncRNAs based on connectivity or biological relevance.
- Apply the knockoff filter with group feature importance statistics to control FDR at the group level.
- Validate that selected lncRNAs maintain significance after adjusting for correlated features.
Diagram 1: FDR-Controlled Biomarker Discovery Workflow
Experimental Protocols for FDR-Controlled lncRNA Biomarker Discovery
Knockoff Framework Implementation for lncRNA Biomarker Selection
The knockoff framework provides a powerful approach for FDR-controlled variable selection in high-dimensional settings. This method creates "knockoff" variables that mimic the correlation structure of original lncRNAs but are known to be null with respect to the outcome [58].
Materials and Reagents:
- RNA-Seq or microarray data from HCC patients and appropriate controls
- Clinical outcome data (overall survival, recurrence-free survival, treatment response)
- Computational resources (R statistical environment, Python for machine learning implementations)
Methodology:
- Data Preprocessing: Normalize lncRNA expression data using TPM (transcripts per million) or similar normalized metrics. Adjust for potential batch effects and technical covariates [55].
- Knockoff Variable Construction: Generate model-free knockoff variables using the approximate algorithm for multivariate Gaussian distributions, which has demonstrated robustness to deviations from Gaussian assumptions [58].
- Feature Importance Statistics: Compute importance measures for both original and knockoff lncRNAs. For continuous outcomes, use the Difference in R-Squared (DRS) statistic. For survival outcomes, use Cox model coefficients or random forest variable importance measures.
- Feature Selection: Calculate the difference between original and knockoff feature importance statistics. Select lncRNAs whose importance significantly exceeds their knockoff counterparts.
- FDR Control: Use the knockoff+ filter to guarantee FDR control at the desired level (e.g., 10%).
Troubleshooting Notes:
- If computational resources are limited, consider the fixed-X knockoff framework which is less computationally intensive.
- For small sample sizes (n < 100), supplement with bootstrap stability selection to improve reproducibility.
- When applying to survival outcomes, ensure proportional hazards assumptions are met or use appropriate non-linear survival models.
Machine Learning Integration with FDR Control
Machine learning approaches can enhance lncRNA biomarker discovery by capturing complex nonlinear relationships, but require special consideration for FDR control [29] [4].
Protocol for ML-Based Biomarker Discovery:
- Data Partitioning: Split data into discovery (60%), tuning (20%), and validation (20%) sets.
- Model Training: Train multiple models (random forest, SVM, neural networks) using lncRNA expression data to predict clinical outcomes.
- Feature Importance: Calculate permutation importance or SHAP values for each lncRNA across models.
- FDR Estimation: Use the stability selection procedure with knockoffs to estimate and control FDR.
- Biomarker Signature Development: Combine selected lncRNAs into a multimodal signature, potentially integrating with established biomarkers like AFP [4].
Validation:
- Apply the signature to the held-out validation set
- Assess performance using time-dependent ROC curves for survival outcomes
- Calculate clinical utility measures (net reclassification improvement, decision curve analysis)
Table 2: Key Research Reagent Solutions for lncRNA Biomarker Studies
| Reagent/Resource | Function | Example Implementation | Considerations |
|---|---|---|---|
| RNA-Seq Platforms | lncRNA quantification | Illumina, PacBio | Ensure adequate sequencing depth for low-abundance lncRNAs |
| qRT-PCR Assays | Technical validation | TaqMan assays, SYBR Green | Design primers spanning exon-exon junctions |
| Bioinformatic Tools | Differential expression | DESeq2, edgeR, limma | Use appropriate parameters for lncRNA-specific characteristics |
| FDR Control Software | Statistical validation | knockoff package (R), statsmodels (Python) | Match method to data structure and sample size |
| Public Databases | Independent validation | TCGA, GEO, ArrayExpress | Check platform compatibility and clinical annotation quality |
Advanced Statistical Approaches for Clinical Cut-off Definition
Time-Dependent ROC Analysis for Survival Outcomes
In HCC research, many important clinical outcomes are time-to-event endpoints such as overall survival (OS) and recurrence-free survival (RFS). Standard ROC analysis must be adapted for these censored outcomes [5] [55].
Implementation Protocol:
- Calculate time-dependent sensitivity and specificity using cumulative sensitivity and dynamic specificity definitions.
- Plot time-dependent ROC curves at clinically relevant timepoints (1, 3, and 5 years).
- Determine optimal cut-offs that maximize the area under the curve (AUC) or according to clinical utility considerations.
- Validate cut-offs using bootstrap resampling to account for overoptimism.
Example from HCC Literature: A meta-analysis of 40 studies found that lncRNA overexpression was associated with poor OS (pooled HR 1.25, 95% CI 1.03-1.52) and RFS (pooled HR 1.66, 95% CI 1.26-2.17) in HCC patients [5]. These effect sizes can inform power calculations for future studies.
Multimodal Signature Integration
Single biomarkers rarely provide sufficient discrimination for clinical use. Integrating multiple lncRNAs with established clinical variables improves prognostic performance [4] [55] [60].
Protocol for Signature Development:
- Select candidate lncRNAs through FDR-controlled discovery as described above.
- Combine lncRNAs with clinical variables (age, liver function tests, AFP) using multivariable regression or machine learning models.
- Calculate risk scores using the formula: Risk Score = Σ(βi × Expressioni) for each lncRNA in the signature.
- Determine optimal risk score cut-offs using maximally selected rank statistics or clinical outcome-oriented approaches.
Diagram 2: Multimodal Signature Development with FDR Control
Validation Frameworks for lncRNA Biomarker Signatures
FAQ 4: What validation steps are essential before progressing to clinical implementation of lncRNA biomarkers?
Issue: Inadequate validation leads to irreproducible biomarkers that fail in clinical translation.
Solution: Implement a comprehensive validation framework encompassing technical, biological, and clinical dimensions.
Technical Validation Protocol:
- Analytical Specificity: Verify that detection assays specifically measure target lncRNAs without cross-reactivity.
- Sensitivity and Linearity: Establish limit of detection (LOD) and limit of quantification (LOQ) using serial dilutions of synthetic standards.
- Precision: Assess intra-assay and inter-assay coefficients of variation (CV < 15% typically acceptable).
- Reproducibility: Demonstrate consistent performance across operators, instruments, and reagent lots.
Biological Validation Protocol:
- Independent Cohort Validation: Test the biomarker signature in at least one independent patient cohort with similar inclusion criteria [4] [55].
- Cross-Population Validation: Assess performance across diverse demographic and clinical subgroups.
- Stability Assessment: Evaluate biomarker stability under various pre-analytical conditions (sample collection, processing delays, storage conditions).
Clinical Validation Protocol:
- Clinical Utility: Demonstrate that the biomarker provides information beyond standard clinical parameters using net reclassification improvement (NRI) or decision curve analysis.
- Clinical Scenarios: Validate performance in specific clinical contexts (early detection, prognosis, treatment selection) [62].
- Regulatory Considerations: Document analytical and clinical performance according to relevant regulatory guidelines (FDA, EMA).
FAQ 5: How can I address batch effects and platform differences when validating lncRNA biomarkers across multiple sites?
Issue: Technical variability introduced by different processing batches or measurement platforms can obscure biological signals and increase false discoveries.
Solution:
- Implement robust normalization methods that mitigate batch effects while preserving biological signal.
- Use combat or removeBatchEffect methods for known batch effects.
- For multi-platform studies, include reference samples to enable cross-platform calibration.
- Consider using ratio-based biomarkers (e.g., LINC00152 to GAS5 ratio) which may be more robust to technical variation [4].
Experimental Protocol for Multi-Site Validation:
- Distribute standardized reference samples across all participating sites.
- Implement standardized RNA extraction, quantification, and detection protocols.
- Use mixed models that include site as a random effect during validation.
- Assess measurement concordance using intraclass correlation coefficients (ICC > 0.8 typically indicates excellent agreement).
Establishing statistically validated clinical cut-offs for lncRNA biomarkers in HCC requires a comprehensive approach that integrates rigorous statistical FDR control with biological and clinical considerations. The knockoff framework provides a powerful methodology for false discovery control in high-dimensional settings, while machine learning approaches enable the development of multimodal signatures with enhanced predictive performance. Through systematic implementation of the troubleshooting guides and experimental protocols outlined in this technical support document, researchers can significantly improve the reliability and clinical translatability of lncRNA biomarkers for hepatocellular carcinoma.
Successful biomarker development requires balancing statistical rigor with practical considerations, ensuring that discovered signatures not only achieve statistical significance but also provide clinically meaningful improvements in patient management. By adhering to these principles and methodologies, the research community can accelerate the translation of lncRNA discoveries into clinically useful tools for HCC diagnosis, prognosis, and treatment selection.
Benchmarking for Clinical Translation: Validation Frameworks and Performance Against Current Standards
Robust validation of a long non-coding RNA (lncRNA) signature is critical for translating research findings into clinically applicable biomarkers for Hepatocellular Carcinoma (HCC). The following strategies, demonstrated in recent studies, provide a framework for confirming panel performance across diverse populations.
Table 1: Key Metrics from Published lncRNA Validation Studies
| Study Focus | Validation Strategy | Cohort Details | Key Performance Metrics |
|---|---|---|---|
| 10-lncRNA Prognostic Signature for HNSCC [63] | TCGA data split into Training (n=213) and Testing (n=212) cohorts. | Head and Neck Squamous Cell Carcinoma patients from TCGA. | Testing cohort: Median OS 1.65 vs. 13.04 years (high vs. low risk; P<0.0001). |
| 4-lncRNA Diagnostic Panel for HCC [4] | Independent clinical cohort with machine learning integration. | 52 HCC patients vs. 30 age-matched controls. | Individual lncRNAs: 60-83% sensitivity, 53-67% specificity. ML model: 100% sensitivity, 97% specificity. |
| 29-lncRNA Panel for Ovarian Cancer HRD [52] | Train/Validation/Test split (60/20/20) with stratified sampling. | TCGA ovarian cancer dataset. | Random Forest model on test set: R²=0.52, Pearson correlation=0.72 for HRD score. |
The diagram below illustrates the logical workflow for a multi-cohort validation strategy, integrating the methods from these studies.
Detailed Experimental Protocols
Protocol 1: Building a Prognostic Signature from TCGA Data
This protocol is adapted from a study identifying a 10-lncRNA signature for head and neck cancer prognosis [63].
- Data Acquisition: Download lncRNA expression data (e.g., from TANRIC database) and corresponding clinical data for HCC patients from The Cancer Genome Atlas (TCGA).
- Cohort Splitting: Randomly divide the patient cohort into a training set (e.g., 50%) and an independent testing set (e.g., 50%).
- Univariate Cox Regression: In the training cohort, perform univariate Cox regression analysis to identify lncRNAs significantly associated with overall survival (P<0.01).
- Multivariate Cox Regression: Subject the significant candidate lncRNAs from step 3 to a multivariate Cox regression analysis to identify independent prognostic factors.
- Risk Score Calculation: Construct a risk-score formula using the final lncRNA panel. The formula is a linear combination of each lncRNA's expression level weighted by its regression coefficient from the multivariate analysis.
- Example: Risk score = (CoefficientlncRNA1 × ExpressionlncRNA1) + (CoefficientlncRNA2 × ExpressionlncRNA2) + ...
- Validation: Apply the risk-score formula to the testing cohort. Use the median risk score from the training cohort as a cut-off to stratify patients into high-risk and low-risk groups. Compare survival between groups using Kaplan-Meier analysis and the log-rank test.
Protocol 2: Independent Clinical Validation via qRT-PCR
This protocol is based on a study that validated a 4-lncRNA panel for HCC screening [4].
- Cohort Selection: Recruit a well-characterized, independent cohort of patients (e.g., 52 HCC patients) and age-matched controls (e.g., 30 individuals). Adhere to strict inclusion/exclusion criteria (e.g., treatment-naive patients, confirmed diagnosis via LI-RADS imaging or histopathology).
- Sample Collection and RNA Isolation: Collect plasma samples. Isolate total RNA using a commercial kit (e.g., miRNeasy Mini Kit).
- cDNA Synthesis: Perform reverse transcription using a dedicated kit (e.g., RevertAid First Strand cDNA Synthesis Kit).
- Quantitative Real-Time PCR (qRT-PCR):
- Use PowerTrack SYBR Green Master Mix on a real-time PCR system.
- Design specific primers for each target lncRNA (e.g., LINC00152, GAS5).
- Run all reactions in triplicate.
- Use a housekeeping gene (e.g., GAPDH) for normalization.
- Calculate relative expression using the ΔΔCT method.
- Statistical and Machine Learning Analysis:
- Assess individual lncRNA performance using Receiver Operating Characteristic (ROC) curve analysis.
- For enhanced accuracy, integrate lncRNA expression data with clinical variables (e.g., AFP, ALT, AST) into a machine learning model (e.g., using Python's Scikit-learn library). Use techniques like cross-validation to train and test the model's diagnostic power.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Kits for lncRNA Validation
| Item | Function | Example Product & Specification |
|---|---|---|
| RNA Isolation Kit | Extracts high-quality total RNA from plasma or tissue. | miRNeasy Mini Kit (QIAGEN, cat no. 217004) [4]. |
| cDNA Synthesis Kit | Reverse transcribes RNA into stable cDNA for qRT-PCR. | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific, cat no. K1622) [4]. |
| qRT-PCR Master Mix | Enables sensitive and specific quantification of lncRNA targets. | PowerTrack SYBR Green Master Mix (Applied Biosystems, cat no. A46012) [4]. |
| Bioinformatics Tools | For coding potential assessment during lncRNA discovery. | CPC, CNCI, Pfam, CPAT, and PhyloCSF [52] [64]. |
| Analysis Software | For differential expression and statistical analysis. | R/Bioconductor packages (DESeq2, survival, timeROC) [63] [65]. |
The following workflow diagram outlines the key experimental steps for the qRT-PCR validation protocol.
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: Our lncRNA signature performs well in the initial cohort but fails in an independent validation cohort. What are the most common reasons for this? A1: This often stems from overfitting during the discovery phase or cohort-specific biases. To mitigate this:
- Ensure your discovery cohort is sufficiently large and use data-splitting methods (training/test/validation sets) [63] [52].
- Apply regularization techniques (e.g., LASSO regression) during feature selection to penalize model complexity and select the most robust lncRNAs [65].
- Critically assess the clinical and demographic characteristics (e.g., etiology of liver disease, stage distribution) of your validation cohort to ensure it is truly representative of the target population [66].
Q2: How can we improve the sensitivity and specificity of a single lncRNA biomarker? A2: Combining multiple lncRNAs into a panel or integrating them with established clinical biomarkers is highly effective. For instance, while individual lncRNAs showed moderate accuracy (Sens: 60-83%, Spec: 53-67%), a machine learning model that integrated four lncRNAs with standard lab tests (AFP, ALT, AST) achieved nearly perfect performance (Sens: 100%, Spec: 97%) [4]. This approach leverages the synergistic power of multiple markers.
Q3: What is the advantage of using a risk-scoring method over simple expression level cut-offs for prognostic signatures? A3: A risk score incorporates the relative contribution (weight) of each lncRNA in the panel, based on its regression coefficient. This provides a more powerful and integrated measure of patient risk than individual expression levels. Studies have successfully used this method to stratify patients into groups with significantly different overall survival (e.g., 1.65 vs. 13.04 years) [63].
Common Experimental Pitfalls and Solutions
Problem: High background noise and inconsistent qRT-PCR results.
- Solution: Always run reactions in triplicate and use a well-validated housekeeping gene (e.g., GAPDH) for normalization [4]. Ensure RNA quality is high by using instruments like a Bioanalyzer to check RNA Integrity Number (RIN) before proceeding.
Problem: Low RNA yield from plasma samples, hindering detection.
- Solution: Use specialized kits designed for isolating RNA from biofluids, which are optimized for low-concentration samples. Concentrate the RNA during the elution step if necessary and use a sufficient volume of starting plasma.
Problem: The diagnostic model works well in one patient population but not in another.
- Solution: This underscores the need for validation in diverse, multi-center cohorts. Factors like different prevalent hepatitis viruses (HBV vs. HCV) or ethnic genetic backgrounds can influence lncRNA expression. Actively seek out collaborative opportunities to test your panel in geographically and ethnically distinct populations [66] [4].
Diagnostic Performance: lncRNA Signatures vs. Traditional AFP
FAQ: How does the diagnostic performance of novel lncRNA signatures compare directly with Alpha-fetoprotein (AFP) for hepatocellular carcinoma (HCC) detection?
The quantitative comparison of diagnostic accuracy between emerging long non-coding RNA (lncRNA) signatures and the conventional AFP biomarker is crucial for evaluating their clinical potential. The table below summarizes key performance metrics from recent studies.
Table 1: Diagnostic Performance of lncRNA Signatures vs. AFP in HCC
| Biomarker / Signature | Sensitivity (%) | Specificity (%) | AUC | Sample Type | Reference/Model |
|---|---|---|---|---|---|
| Individual lncRNAs (Range) | 60 - 83 | 53 - 67 | Moderate | Plasma | [4] |
| 4-lncRNA Panel + ML Model | 100 | 97 | Near Perfect | Plasma | [4] |
| 3-DRL Signature (1-year) | - | - | 0.756 | Tissue (TCGA) | [67] |
| 3-DRL Signature (3-year) | - | - | 0.695 | Tissue (TCGA) | [67] |
| 3-DRL Signature (5-year) | - | - | 0.701 | Tissue (TCGA) | [67] |
| Traditional AFP | ~60-70 (Limited in early stages) | Variable | <0.8 (Often reported as moderate) | Serum | [4] [68] |
Key Interpretation: While individual lncRNAs may show only moderate performance, combining them into a multi-lncRNA signature, especially when integrated with machine learning (ML) models that include standard laboratory parameters, can significantly outperform AFP, achieving sensitivity and specificity over 95% [4]. Furthermore, lncRNA signatures show strong prognostic value, maintaining predictive power for patient survival over 1, 3, and 5 years [67].
Core Experimental Protocol for lncRNA Biomarker Evaluation
FAQ: What is a standard experimental workflow for validating the diagnostic efficacy of an lncRNA signature against AFP?
The following detailed protocol is synthesized from methodologies used in recent studies comparing lncRNA biomarkers with AFP [4] [68].
Phase 1: Study Population and Sample Collection
- Participant Recruitment: Enroll cohorts of confirmed HCC patients, patients with chronic liver disease (e.g., Hepatitis B/C, cirrhosis) as a high-risk control group, and healthy controls. Matching for age and gender is critical.
- Inclusion/Exclusion Criteria:
- HCC Patients: Diagnosis confirmed via LI-RADS imaging criteria or histopathology; treatment-naive before sample collection.
- Controls: No history of liver disease, cancer, or chronic inflammatory disorders.
- Exclusion: Patients on immunosuppressants, with other malignancies, or non-HCC liver tumors.
- Sample Collection: Collect fasting venous blood. For serum, use vacuum tubes with separation gel and procoagulant. For plasma, use EDTA anticoagulant tubes. Centrifuge samples within 2 hours of collection, aliquot the supernatant (serum/plasma), and store at -80°C.
Phase 2: RNA Isolation and cDNA Synthesis
- RNA Extraction: Isolate total RNA from 200 μL of serum/plasma using a commercial kit (e.g., miRNeasy Mini Kit or TRIzol reagent). Include DNase treatment to remove genomic DNA contamination.
- Quality Control: Measure RNA concentration and purity with a spectrophotometer. Accept A260/A280 ratios between 1.8 and 2.1.
- cDNA Synthesis: Reverse transcribe 1-2 μg of total RNA into complementary DNA (cDNA) using a kit with oligo(dT) and random hexamer primers (e.g., RevertAid First Strand cDNA Synthesis Kit).
Phase 3: Quantitative Real-Time PCR (qRT-PCR)
- Primer Design: Use exon-spanning, specific primers for the target lncRNAs and reference genes (e.g., GAPDH, β-actin, B2M, TBP).
- Reaction Setup: Perform qRT-PCR in triplicate for each sample using a SYBR Green Master Mix on a real-time PCR system.
- Data Analysis: Calculate relative expression levels using the ΔΔCt method with normalization to reference genes.
Phase 4: AFP Measurement and Data Integration
- AFP Quantification: Measure serum AFP levels for all participants using standard clinical immunoassay techniques (e.g., ELISA, chemiluminescence).
- Machine Learning Integration: Use a platform like Python's Scikit-learn to build a predictive model. Input variables include the expression levels of the target lncRNAs, AFP, and other relevant clinical laboratory parameters (e.g., ALT, AST, Albumin).
Phase 5: Statistical and Diagnostic Analysis
- ROC Curve Analysis: Generate Receiver Operating Characteristic (ROC) curves for individual lncRNAs, the lncRNA signature, AFP, and the combined ML model.
- Metric Calculation: From the ROC curves, calculate and compare the Area Under the Curve (AUC), sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV).
- Survival Analysis: For prognostic signatures, use Kaplan-Meier analysis to assess the correlation between lncRNA risk scores and overall survival.
The following workflow diagram visualizes this multi-phase experimental protocol:
The Scientist's Toolkit: Key Research Reagent Solutions
FAQ: What are the essential reagents and kits required to set up this lncRNA vs. AFP validation experiment?
This table lists critical reagents, their functions, and examples cited in recent publications.
Table 2: Essential Research Reagents for lncRNA/AFP Biomarker Studies
| Reagent / Kit | Function / Application | Specific Example (from literature) |
|---|---|---|
| RNA Extraction Kit | Isolation of high-quality total RNA from liquid biopsies. | miRNeasy Mini Kit (QIAGEN) [4], TRIzol Reagent [69] |
| cDNA Synthesis Kit | Reverse transcription of RNA into stable cDNA for qPCR. | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) [4] |
| qPCR Master Mix | Sensitive and specific detection of lncRNA targets via fluorescence. | PowerTrack SYBR Green Master Mix (Applied Biosystems) [4], TB Green Master Mix (Takara Bio) [69] |
| LncRNA-specific Primers | Exon-spanning primers for accurate amplification of target lncRNAs. | Custom-designed primers (e.g., for LINC00152, UCA1, GAS5) [4] |
| Reference Gene Primers | Primers for housekeeping genes for data normalization. | Primers for GAPDH [4], β-actin (ACTB) [69], B2M, TBP [70] |
| AFP Detection Kit | Quantitative measurement of AFP levels in serum. | Standard clinical immunoassay (e.g., ELISA) [4] |
| EV Isolation Kit/Reagents | Isolation of extracellular vesicles from serum/plasma for EV-derived lncRNA analysis. | Size-exclusion chromatography columns (e.g., ES911) [68] |
Troubleshooting Common Experimental Challenges
FAQ: What are the common sources of false positives and low reproducibility in lncRNA biomarker studies, and how can they be mitigated?
Issue 1: Inconsistent RNA Quality and Purity
- Problem: Degraded RNA or contaminants from the isolation process can lead to unreliable qPCR results and inflated Ct values.
- Solution:
- Strictly adhere to the 2-hour processing window for blood samples.
- Use a spectrophotometer to check A260/A280 and A260/A230 ratios. Only proceed with samples having ratios >1.8 and >2.0, respectively.
- Include an RNA integrity check (e.g., using a Bioanalyzer) for sequencing-based studies.
Issue 2: Lack of Assay Standardization
- Problem: Inconsistent primer specificity and amplification efficiency between batches can cause non-reproducible results.
- Solution:
- Design and validate exon-spanning primers to avoid amplification of genomic DNA [69].
- Perform efficiency tests for all primer sets. Only use primers with efficiency between 90-110%.
- Include a positive control (synthetic oligo or known positive sample) and a no-template control (NTC) in every qPCR run.
Issue 3: Inappropriate Data Normalization
- Problem: Using an unstable reference gene can skew relative expression data, leading to false positives or negatives.
- Solution:
- Validate reference gene stability across all sample groups (HCC, disease controls, healthy) using algorithms like geNorm or NormFinder before the main study. Do not assume a gene is stable.
- Consider using a panel of multiple reference genes (e.g., GAPDH, β-actin, B2M) for more robust normalization [4] [70].
Issue 4: Overfitting of Machine Learning Models
- Problem: A model performs perfectly on a small initial dataset but fails in external validation, a hallmark of overfitting.
- Solution:
- Ensure a sufficient sample size. Use power analysis during the study design phase [4].
- Apply regularization techniques like LASSO-Cox regression, which helps select the most relevant biomarkers and reduces model complexity [67] [55].
- Validate the model in an independent cohort from a different clinical center to prove its generalizability [55].
Issue 5: Confounding from Underlying Liver Disease
- Problem: lncRNA expression can be altered by non-malignant conditions like hepatitis or cirrhosis, causing false positives for HCC.
- Solution:
- Include relevant disease control groups (e.g., patients with chronic hepatitis B, liver cirrhosis) in the study design [68].
- In the ML model, incorporate standard liver function tests (ALT, AST, Bilirubin) as variables to help the model adjust for and distinguish background liver inflammation from HCC-specific signals [4].
The following diagram illustrates the critical checkpoints in the experimental workflow to minimize these issues:
Troubleshooting Guide: FAQs on lncRNA Biomarker Research
FAQ 1: My lncRNA signature shows strong correlation with survival in training data but fails in validation. What are potential causes?
This is often caused by false positive associations from the initial discovery phase. Key solutions include:
- Pre-filter with Disease Association: Integrate disease-associated Single Nucleotide Polymorphisms (SNPs) to filter lncRNAs before signature development. This links candidates directly to disease biology, reducing noise [71].
- Incorporate Cis-Regulatory Analysis: Prioritize lncRNAs that are co-expressed with their neighboring protein-coding genes (cis-regulation) within your specific disease context, as this often indicates functional relevance [71].
- Ensure Adequate Sample Sizing: For the validation phase, ensure your cohort size is calculated based on the sensitivity and specificity observed in your discovery set. A statistically powered validation is crucial for reliability [72].
FAQ 2: How can I improve the specificity of a circulating lncRNA biomarker to distinguish HCC from other liver diseases?
To enhance specificity for Hepatocellular Carcinoma (HCC):
- Develop Multi-lncRNA Panels: Relying on a single lncRNA is often insufficient. Combine multiple lncRNAs into a signature. For example, a panel of PTENP1, LSINCT-5, and CUDR (UCA1) outperformed conventional markers CEA and CA19-9 in gastric cancer [3].
- Combine with Classical Biomarkers: Use your lncRNA signature in conjunction with standard biomarkers like Alpha-fetoprotein (AFP). For instance, the lncRNA LRB1 showed increased diagnostic accuracy for HCC when combined with AFP and Des-gamma-carboxy prothrombin (DCP) [19].
- Focus on Stable Circulating lncRNAs: Leverage the inherent stability of blood-derived lncRNAs, which are protected by exosomes and their secondary structures, making them more reliable analytes [3].
FAQ 3: My lncRNA signature correlates with tumor stage but not with treatment response. How can I investigate its predictive utility?
A signature correlating with stage indicates a role in tumor burden or progression, but not necessarily in therapy resistance mechanisms.
- Interrogate Relevant Pathways: Conduct gene set enrichment analysis (GSEA) to see if your signature is associated with known drug resistance pathways. For example, a Notch signaling-related lncRNA signature in renal cell carcinoma was correlated with sensitivity to specific targeted therapies and chemotherapeutics [73].
- Link to Functional Mechanisms: Investigate if the lncRNAs in your signature have known roles in therapy resistance. For instance, SNHG1 activates the Akt pathway to confer sorafenib resistance in HCC, making it a strong predictive candidate [20].
- Analyze by Molecular Subtype: Ensure that the predictive power is not confined to a specific molecular subgroup. Validate the signature within homogeneous patient cohorts defined by tumor stage, genetic drivers, or previous treatments [72].
Quantitative Data on lncRNA Diagnostic and Prognostic Performance
Table 1: Diagnostic Performance of Select Circulating lncRNAs in HCC
| lncRNA | Sample Type | Sensitivity | Specificity | AUC | Comparison to AFP | Key Reference |
|---|---|---|---|---|---|---|
| SNHG1 | Plasma | 87.3% | 86.0% | 0.92 | Superior sensitivity (87.3% vs 64.6%) | [20] |
| LRB1 | Serum | Information Not Specified | Information Not Specified | Information Not Specified | Improved accuracy when combined with AFP & DCP | [19] |
| MALAT-1 | Plasma | Information Not Specified | 84.8% | Information Not Specified | Studied in prostate cancer | [3] |
| HULC | Blood | Information Not Specified | Information Not Specified | Information Not Specified | Reported as elevated in HCC patients | [3] |
Table 2: Prognostic Value of lncRNA Signatures in Various Cancers
| Cancer Type | lncRNA Signature | Prognostic Value (High-Risk Group) | Independent Prognostic Factor? | Key Reference |
|---|---|---|---|---|
| Ovarian Cancer | 8-lncRNA signature | Shorter median OS (2.81 vs 4.85 years) | Yes | [74] |
| Clear Cell Renal Cell Carcinoma | 5 Notch-related lncRNAs | Shorter Overall Survival | Yes | [73] |
| HCC (Meta-analysis) | Multiple lncRNAs | Shorter OS (HR=1.25) & RFS (HR=1.66) | Yes | [75] |
Detailed Experimental Protocols
Protocol 1: Developing a Reduced False-Positive lncRNA Signature using the DAnet Strategy
This protocol uses a novel strategy that integrates disease associations to lower the false discovery rate (FDR) in functional annotation [71].
Sample Collection & Data Preparation:
- Collect transcriptomic data (RNA-seq or microarray) from patient and control groups. A minimum of 3 biological replicates per condition is recommended for discovery, though larger cohorts are needed for validation [72].
- Annotate transcripts into lncRNAs and mRNAs using a reference database like GENCODE.
Identify Disease-Associated lncRNAs:
- SNP Integration: Screen lncRNAs for the presence of disease-associated SNPs from relevant genome-wide association studies (GWAS).
- Condition-Specific Expression: Calculate the coefficient of variation (CV) for lncRNA expression across samples. Filter for lncRNAs with high condition-specific expression variability.
Construct Cis-Regulatory Network:
- For the disease-associated lncRNAs from Step 2, identify their neighboring protein-coding genes (e.g., within a 1 Mb genomic window).
- Perform Weighted Gene Co-expression Network Analysis (WGCNA) to build a co-expression network between these lncRNAs and their neighboring genes.
Functional Enrichment & Signature Building:
- Conduct pathway enrichment analysis (e.g., KEGG) on the co-expressed neighboring genes to infer the potential biological functions of the linked lncRNAs.
- Use machine learning (e.g., LASSO Cox regression) on the filtered, functionally-informed lncRNA list to build a compact prognostic signature and calculate a risk score for each patient [73].
The workflow for this strategy is outlined below:
Protocol 2: Validating a Circulating lncRNA Biomarker in HCC Serum/Plasma
This protocol details the steps for quantifying a candidate lncRNA in blood, as used in clinical studies [19].
Sample Acquisition and Processing:
- Collect peripheral blood from patients (e.g., HCC patients and healthy controls) using tubes containing anticoagulants like sodium heparin.
- Process blood promptly through sequential centrifugation to obtain pure serum/plasma (e.g., 800 × g for 20 min, then 2,000 × g for 10 min at 4°C). Aliquot and store at -80°C.
RNA Extraction:
- Isolate total RNA from serum/plasma using a specialized commercial kit designed for low-abundance nucleic acids. Include a DNase digestion step to remove genomic DNA contamination.
Reverse Transcription Quantitative PCR (RT-qPCR):
- Synthesize cDNA from a fixed amount of total RNA (e.g., 10 µg) using a reverse transcription kit.
- Perform qPCR in triplicate for each sample. Use a reaction mix containing SYBR Green Master Mix, specific forward and reverse primers for your target lncRNA, and the cDNA template.
- Primer Example for LRB1: Forward: 5′-TCATGCGATAGCTGAACGCTA-3′, Reverse: 5′-GAGGCCGGTAGTCGTAACT-3′ [19].
- Normalize the expression of your target lncRNA to an internal control (e.g., GAPDH) using the 2^–ΔΔCq method.
Statistical and Diagnostic Analysis:
- Correlate lncRNA expression levels with clinical parameters (tumor stage, grade, survival).
- Perform Receiver Operating Characteristic (ROC) curve analysis to evaluate the diagnostic accuracy (sensitivity, specificity, and Area Under the Curve - AUC) of the lncRNA, both alone and in combination with standard markers like AFP.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Kits for lncRNA Biomarker Studies
| Reagent / Kit | Function | Example Use Case in Research |
|---|---|---|
| RNA Isolation Kit (for serum/plasma) | Extracts total RNA, including small and fragmented RNAs, from low-volume/ low-concentration biofluids. | Used to isolate circulating lncRNAs from patient serum samples for downstream RT-qPCR analysis [19]. |
| ReverTra Ace qPCR RT Kit | Synthesizes first-strand cDNA from total RNA templates. | Converts extracted RNA into stable cDNA for subsequent quantitative PCR amplification [19]. |
| Power SYBR Green PCR Master Mix | Provides all components (except primers/template) for real-time PCR detection using SYBR Green chemistry. | Used in the qPCR step to detect and quantify the amplified lncRNA product [19]. |
| LncRNA Microarray | High-throughput profiling of lncRNA expression across thousands of targets. | Used for discovery-phase screening to identify differentially expressed lncRNAs between case and control groups [19]. |
| Human α-Fetoprotein Quantikine ELISA Kit | Quantifies protein levels of AFP in serum. | Used as a standard biomarker to compare and combine with novel lncRNA biomarkers for improved diagnostic performance [19]. |
Frequently Asked Questions (FAQs) for lncRNA Biomarker Development
FAQ 1: What is the single most critical factor to define early in biomarker development? The most critical factor is establishing a clear Context of Use (COU). The COU is a concise description of the biomarker's specified purpose, which includes its biomarker category (e.g., diagnostic, prognostic, monitoring) and its intended application in drug development or clinical practice [76]. A clearly defined COU dictates the entire study design, including the statistical analysis plan, choice of study populations, and the acceptable parameters for measuring the biomarker, ensuring that the collected data accurately evaluates its reliability for the proposed use [76].
FAQ 2: How do regulatory pathways differ for a high-risk diagnostic test versus a low-risk test? Regulatory pathways and evidence requirements vary significantly based on the device's risk classification [77] [78].
- High-Risk Devices (Class III in the U.S., Class IIb/III under EU MDR): Typically require a Premarket Approval (PMA) in the U.S., which demands comprehensive clinical data proving safety and efficacy. The mean decision time for Breakthrough Device Program designations through the PMA pathway is 230 days [77].
- Moderate/Low-Risk Devices: May follow the de novo (mean 262 days) or 510(k) (mean 152 days) pathways, which often have less stringent evidence requirements, potentially relying on predicate devices or existing data [77]. For all classes, engagement with regulators like the FDA early in the process is essential to align on evidence requirements [78].
FAQ 3: What are the key technical challenges in lncRNA investigation that lead to variable results? Key technical challenges include [79] [80]:
- Low Abundance and Detection: Many lncRNAs are expressed at very low levels, with cycle threshold (Ct) values often ≥35 in qRT-PCR, making accurate quantification difficult [80].
- Complex Genomic Architecture: LncRNAs can overlap with other genes, be transcribed from bidirectional promoters, or have isoforms, making targeted manipulation without affecting neighboring genes highly challenging [79].
- Cellular Localization: Determining the precise nuclear or cytoplasmic localization of a lncRNA is crucial for inferring its function but can be difficult with standard assays [80].
- Sample Degradation: RNA is inherently unstable, and improper sample collection, handling, or storage can lead to degradation, directly causing false positives or negatives [81].
FAQ 4: How can I demonstrate clinical utility for a prognostic lncRNA biomarker? For a prognostic biomarker, clinical validation must demonstrate the biomarker's accuracy in predicting the likelihood of a clinical event within a defined period in individuals with the disease [76]. The study design should:
- Use a clearly defined clinical endpoint or accepted standard (e.g., overall survival, radiographically confirmed progression) [76].
- Be sufficiently powered and include a longitudinal analysis to establish the relationship between the biomarker and the clinical outcome [76].
- Statistically evaluate the added value of the lncRNA biomarker to improve the accuracy of prediction models beyond existing clinical parameters [76] [4].
FAQ 5: What is the difference between analytical validation and clinical validation? These are two distinct, sequential stages of biomarker development [76]:
- Analytical Validation: This process establishes that the test or assay itself is technically reliable. It evaluates performance characteristics like sensitivity, specificity, accuracy, and precision using a specified technical protocol. It validates the test's technical performance, not its clinical usefulness [76].
- Clinical Validation: This process establishes that the test results acceptably identify, measure, or predict the clinical concept of interest (e.g., the presence of a disease, the prediction of a future event). It validates the biomarker's usefulness for the specified COU [76].
Troubleshooting Common Experimental Issues
Issue 1: High Variability and False Positives in lncRNA Quantification
Problem: Inconsistent results and high background noise during qRT-PCR or RNA-seq analysis of lncRNAs.
Solution:
- Conduct Analytical Validation: Before clinical validation, rigorously test your assay's performance. The table below outlines key parameters to assess.
Table 1: Key Parameters for Analytical Validation of a lncRNA Assay
| Parameter | Description | Target Performance |
|---|---|---|
| Sensitivity | The lowest concentration of the lncRNA that can be reliably detected. | Should be established based on biological relevance [76]. |
| Specificity | The ability to detect only the target lncRNA and not cross-react with similar sequences. | Use BLAST and secondary structure prediction to check for off-target binding [80]. |
| Accuracy | The closeness of the measured value to the true value. | Evaluate using spike-in controls or standardized samples [76]. |
| Precision | The reproducibility of the measurement (repeatability and reproducibility). | Determine coefficients of variation (CV) within and between runs [76]. |
- Standardize Sample Preparation: Implement automated homogenization systems to minimize cross-contamination and variability introduced by manual processing [81]. Use single-use consumables and consistent disruption parameters.
- Control for Contamination: Implement strict contamination prevention strategies, including dedicated clean areas, routine equipment decontamination, and proper handling procedures [81].
- Ensure RNA Integrity: Maintain a consistent cold chain from sample collection to analysis. Use immediate flash-freezing (e.g., in liquid nitrogen) and careful thawing on ice to preserve RNA integrity [81].
Issue 2: Functionally Characterizing a Low-Abundance lncRNA
Problem: A candidate lncRNA shows significant differential expression but is lowly abundant, making functional studies difficult.
Solution:
- Define the Full-Length Transcript: Use 5' and 3' RACE (Rapid Amplification of cDNA Ends) to define the complete transcript sequence, as many lncRNAs are incompletely annotated. This is critical for designing functional assays [80].
- Determine Subcellular Localization: Perform cell fractionation followed by qRT-PCR as a first step to determine if the lncRNA is primarily nuclear or cytoplasmic. This provides critical clues about its potential function [80].
- Use Advanced Genome Editing: For loss-of-function studies, utilize the CRISPR/Cas9 system. To avoid affecting overlapping genes, target the lncRNA's promoter or use CRISPR interference (CRISPRi) to block transcription without altering the DNA sequence [79] [80].
- Investigate Modular Function: Since lncRNAs often have a modular structure, design experiments to test individual domains or repeats for their specific roles in RNA-protein interactions or nucleic acid binding [1] [79].
The following diagram illustrates a generalized workflow for tackling a novel lncRNA, from identification to initial functional characterization, incorporating strategies to mitigate false positives.
Issue 3: Integrating lncRNA Biomarkers with Machine Learning Models
Problem: How to build a robust diagnostic model using multiple lncRNAs and clinical variables.
Solution:
- Combine Biomarkers: Individual lncRNAs may have moderate diagnostic accuracy on their own (e.g., 60-83% sensitivity). Combining them into a panel, potentially with traditional biomarkers like AFP, can significantly improve performance [4].
- Apply Machine Learning (ML): Use ML algorithms like Random Forest, XGBoost, or Multi-layer Perceptron (MLP) to integrate the expression levels of multiple lncRNAs with conventional laboratory data (e.g., ALT, AST, AFP) [4] [32]. One study achieved 100% sensitivity and 97% specificity using this approach, far exceeding the performance of any single lncRNA [4].
- Ensure Robust Validation: Validate the ML model on large, independent, and multi-site cohorts to ensure its performance generalizes across different patient populations and comorbidities [76] [32].
Table 2: Example Diagnostic Performance of Individual lncRNAs vs. a Machine Learning Model in HCC [4]
| Biomarker / Model | Sensitivity | Specificity |
|---|---|---|
| LINC00152 | 83% | 53% |
| UCA1 | 60% | 67% |
| GAS5 | 67% | 60% |
| LINC00853 | 63% | 63% |
| Machine Learning Model\n(Combining lncRNAs & clinical data) | 100% | 97% |
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagent Solutions for lncRNA Biomarker Development
| Item | Function / Application | Examples / Notes |
|---|---|---|
| Automated Homogenizer | Standardizes sample disruption, reduces cross-contamination, and improves throughput for nucleic acid extraction. | Omni LH 96; uses single-use tips to eliminate cross-sample exposure [81]. |
| RNA Isolation Kit | Extracts high-quality, intact total RNA from plasma, serum, or tissue samples. | miRNeasy Mini Kit (QIAGEN); designed for efficient recovery of small and large RNAs [4]. |
| cDNA Synthesis Kit | Reverse transcribes RNA into stable cDNA for subsequent qRT-PCR analysis. | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) [4]. |
| qRT-PCR Master Mix | Enables sensitive and specific quantification of lncRNA expression levels. | PowerTrack SYBR Green Master Mix (Applied Biosystems); ensure it is optimized for long RNA targets [4]. |
| CRISPR/Cas9 System | Provides precision genome editing for functional loss-of-function studies on lncRNA loci. | Can be used to target the lncRNA promoter or use CRISPRi to block transcription [79] [80]. |
| Antisense Oligonucleotides (ASOs) | Used for post-transcriptional knockdown of lncRNAs, useful for functional validation. | Chemically modified ASOs can be designed to target and degrade specific lncRNAs [79]. |
| Bioinformatics Databases | Provide annotation, conservation, and potential functional insights for lncRNAs. | Lncipedia, NONCODE, lncRNAdb, UCSC Genome Browser, Ensembl [1] [80]. |
The following diagram maps out the key stages and decision points on the path from discovery to clinical adoption, highlighting the critical role of regulatory strategy and clinical validation.
Conclusion
The journey toward clinically reliable lncRNA biomarkers for HCC hinges on a multi-faceted strategy to minimize false positives. Key takeaways confirm that moving beyond single markers to integrated, AI-powered multi-lncRNA panels dramatically enhances diagnostic specificity. Meticulous attention to pre-analytical and analytical workflows is non-negotiable for data integrity. Future progress depends on large-scale, multi-center validation studies that solidify the link between specific lncRNA signatures and clinical outcomes. The successful reduction of false positives will not only unlock the potential of lncRNAs for early HCC detection but also pave the way for their application in personalized treatment stratification and monitoring, fundamentally advancing precision oncology.
References
- 1. Long non-coding RNAs: definitions, functions, challenges ... [https://www.nature.com/articles/s41580-022-00566-8]
- 2. Long Noncoding RNAs as Novel Biomarkers Have a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4842029/]
- 3. Blood-derived lncRNAs as biomarkers for cancer diagnosis [https://www.nature.com/articles/s41698-022-00283-7]
- 4. Analysis of four long non-coding RNAs for hepatocellular ... [https://www.nature.com/articles/s41598-024-80926-w]
- 5. lncRNAs as prognostic molecular biomarkers in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5601763/]
- 6. Plasma exosomal lncRNA-related signatures define ... [https://pubmed.ncbi.nlm.nih.gov/41169384/]
- 7. Innovative Approaches to Hepatocellular Carcinoma [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561740/]
- 8. Plasma exosomal lncRNA-related signatures define ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1663943/full]
- 9. Hypoxia- and Anoikis-Related lncRNA Signature Defines ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12533731/]
- 10. The regulation of hypoxia-related lncRNAs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11076439/]
- 11. A novel classification of HCC basing on fatty-acid- ... [https://www.nature.com/articles/s41598-022-23681-0]
- 12. Amino acid metabolism-related LncRNAs as prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12545943/]
- 13. MIAT, HEIH, and HOTAIR: A novel LncRNA signature in ... [https://www.sciencedirect.com/science/article/pii/S1874467225000169]
- 14. LncRNAs Act as a Link between Chronic Liver Disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7216144/]
- 15. Dynamic role of long noncoding RNA in liver diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC12078412/]
- 16. Surveillance for Hepatocellular Carcinoma: Current Best ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6636644/]
- 17. Biomarkers for diagnosis and therapeutic options in ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02101-z]
- 18. Non-isotopic Method for In Situ LncRNA Visualization and ... [https://pubmed.ncbi.nlm.nih.gov/26721490/]
- 19. Serum long noncoding RNA LRB1 as a potential biomarker for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6036462/]
- 20. LncRNA SNHG1: A novel biomarker and therapeutic target ... [https://www.sciencedirect.com/science/article/abs/pii/S0378111925002501]
- 21. Review Molecular mechanisms of lncRNA NEAT1 in the ... [https://www.sciencedirect.com/science/article/abs/pii/S0344033825000597]
- 22. A LncRNA panel within EpCAM-specific exosomes for ... [https://respiratory-research.biomedcentral.com/articles/10.1186/s12931-025-03220-x]
- 23. Novel Biomarkers for Early Detection of Hepatocellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11507329/]
- 24. Value of Non-Coding RNA Expression in Biofluids to ... [https://www.mdpi.com/2075-4418/14/7/729]
- 25. Identification of plasma exosomal lncRNA as a biomarker ... [https://pubmed.ncbi.nlm.nih.gov/39440243/]
- 26. Analysis of four long non-coding RNAs for hepatocellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11604705/]
- 27. Serum LINC00152 and UCA1 in HCC | BTT [https://www.dovepress.com/serum-linc00152-and-uca1-in-hcv-induced-hepatocellular-carcinoma-clini-peer-reviewed-fulltext-article-BTT]
- 28. Prognostic Values of Long Noncoding RNA linc00152 in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6964117/]
- 29. Integrating AI and RNA biomarkers in cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512311/]
- 30. Integrating multiple machine learning algorithms for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10111190/]
- 31. Machine learning-based integration develops an immune ... [https://www.nature.com/articles/s41467-022-28421-6]
- 32. Integrating AI and RNA biomarkers in cancer: advances in ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-025-02434-2]
- 33. Liquid biopsy for early detection and therapeutic ... [https://www.e-jlc.org/journal/view.php?number=509]
- 34. Liquid Biopsy: An Evolving Paradigm for Non-invasive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10772356/]
- 35. The Liquid Biopsy Consortium: Challenges and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10591039/]
- 36. Liquid biopsies: the future of cancer early detection [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-023-03960-8]
- 37. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 38. Novel biomarkers for monitoring and management of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11668010/]
- 39. Enhancing detection and monitoring of circulating tumor cells [https://www.sciencedirect.com/science/article/pii/S295019542500013X]
- 40. Blood collection tube and RNA purification method recommendations for extracellular RNA transcriptome profiling | Nature Communications [https://www.nature.com/articles/s41467-025-58607-7]
- 41. Troubleshooting Guide: RNA Extraction for Sequencing [https://rna.cd-genomics.com/resource/troubleshooting-rna-extraction.html]
- 42. The impact of preanalytical variability in clinical trials: are we underestimating the issue? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4740010/]
- 43. Experimental Error: Videos & Practice Problems - Pearson [https://www.pearson.com/channels/general-chemistry/learn/jules/bonus-lab-techniques-and-procedures/experimental-error]
- 44. Experimental Error [https://courses.cit.cornell.edu/virtual_lab/LabZero/Experimental_Error.shtml]
- 45. Assessment of mRNA and microRNA Stabilization in Peripheral Human Blood for Multicenter Studies and Biobanks - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2956623/]
- 46. Quantification of long non-coding RNAs using qRT-PCR [https://pmc.ncbi.nlm.nih.gov/articles/PMC8314425/]
- 47. qRT-PCR Validation of lncRNAs in Plasma [https://bio-protocol.org/exchange/minidetail?id=5822246&type=30]
- 48. 4.6. Quantitative Real-Time PCR (QRT-PCR) Validation of ... [https://bio-protocol.org/exchange/minidetail?id=10396006&type=30]
- 49. Deciphering the nexus between long non-coding RNAs ... [https://www.nature.com/articles/s41420-024-02200-2]
- 50. Long Non-coding RNA qPCR | LncRNA qPCR Assays [https://www.arraystar.com/lncrna-qpcr-service/]
- 51. A Comprehensive Review of Long Non-Coding RNAs in Plants [https://pmc.ncbi.nlm.nih.gov/articles/PMC12294436/]
- 52. Long non-coding RNAs as a biomarker for homologous ... [https://www.nature.com/articles/s42003-025-08836-9]
- 53. Techniques for investigating lncRNA transcript functions in ... [https://www.nature.com/articles/s41380-023-02377-5]
- 54. Identification of prognostic biomarkers for hepatocellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12476503/]
- 55. A migrasome-related lncRNA signature predicts prognosis ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1581122/full]
- 56. Efficient discovery of robust prognostic biomarkers and ... [https://www.sciencedirect.com/science/article/abs/pii/S0304383525000667]
- 57. False Discovery Rate [https://www.publichealth.columbia.edu/research/population-health-methods/false-discovery-rate]
- 58. False Discovery Rate Control in Cancer Biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6628039/]
- 59. Longitudinal dysregulation of long non-coding RNAs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10792423/]
- 60. Identification of lncRNA biomarkers in hepatocellular ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2022.832952/full]
- 61. RNA-Seq analysis reveals the long noncoding RNAs ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-11485-1]
- 62. Biomarker Discovery and Validation: Statistical Considerations [https://pmc.ncbi.nlm.nih.gov/articles/PMC8012218/]
- 63. Identification and validation of potential long non-coding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6507327/]
- 64. Workflow of LncRNA Sequencing and Its Data Analysis [https://www.cd-genomics.com/workflow-of-lncrna-sequencing-and-its-data-analysis.html]
- 65. Identification of diagnostic long non-coding RNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6625424/]
- 66. The role of long non-coding RNA in hepatocellular carcinoma [https://pmc.ncbi.nlm.nih.gov/articles/PMC10929815/]
- 67. A novel disulfidptosis-related lncRNA signature for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12582836/]
- 68. Characteristics of extracellular vesicle-derived lncRNAs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12619285/]
- 69. Use of serum long non-coding RNA expression panel as a ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1523997/full]
- 70. MAPK14 and its associated lncRNAs are up-regulated in ... [https://www.nature.com/articles/s41598-025-20689-0]
- 71. LncRNA functional annotation with improved false ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8724965/]
- 72. The Clinical Utility of lncRNAs and Their Application as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10138835/]
- 73. A Notch signaling-related lncRNA signature for predicting ... [https://www.nature.com/articles/s41598-023-48596-2]
- 74. Comprehensive analysis of lncRNA expression profiles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5078024/]
- 75. lncRNAs as prognostic molecular biomarkers in ... [https://www.oncotarget.com/article/19559/text/]
- 76. Biomarker Program FAQs [https://www.ninds.nih.gov/current-research/focus-tools-topics/biomarkers-research/biomarker-program-faqs]
- 77. Regulatory landscape of accelerated approval pathways for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12119601/]
- 78. Optimize Approval: Essential Regulatory Strategies for… [https://www.nsf.org/knowledge-library/optimize-approval-essential-regulatory-strategies-high-risk-medical-devices]
- 79. Techniques for investigating lncRNA transcript functions in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11176085/]
- 80. Challenges and Opportunities in Linking Long Noncoding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5222717/]
- 81. Common Lab Issues That Impact Biomarker Data [https://blog.omni-inc.com/blog/common-lab-issues-that-impact-biomarker-data]