Targeting SOX9 in Tumor-Associated Macrophages: A Comprehensive Protocol for Knockdown and Functional Analysis in the Tumor Microenvironment
This article provides a detailed methodological and conceptual framework for researchers aiming to investigate the role of SOX9 in tumor-associated macrophages (TAMs).
Targeting SOX9 in Tumor-Associated Macrophages: A Comprehensive Protocol for Knockdown and Functional Analysis in the Tumor Microenvironment
Abstract
This article provides a detailed methodological and conceptual framework for researchers aiming to investigate the role of SOX9 in tumor-associated macrophages (TAMs). It covers the foundational biology of the TGF-β/SOX9 axis in promoting tumor metastasis and immune suppression, establishes robust protocols for SOX9 knockdown in macrophage models using siRNA and CRISPR/Cas9, outlines common troubleshooting scenarios, and defines key validation assays. By integrating current research, this guide supports the development of novel therapeutic strategies targeting the TAM-fueled tumor microenvironment.
Understanding the SOX9 Axis: Why Target This Pathway in Tumor-Associated Macrophages?
SOX9 as a Master Regulator in the Tumor Microenvironment
The SRY-Box Transcription Factor 9 (SOX9) is a crucial transcription factor that extends its function beyond embryonic development and stem cell regulation to become a pivotal orchestrator of the tumor microenvironment (TME) [1]. As a key mediator of tumor-stroma interactions, SOX9 influences critical cancer hallmarks including immune evasion, metastatic progression, and therapy resistance [1] [2]. This Application Note examines the multifaceted role of SOX9 within the TME and provides detailed protocols for investigating SOX9 knockdown in tumor-associated macrophages (TAMs), framing this within the broader context of targeting SOX9 to disrupt pro-tumorigenic signaling pathways for therapeutic benefit.
SOX9 Structure and Function
The SOX9 protein contains several functionally critical domains that enable its role as a master transcriptional regulator. The N-terminal dimerization domain (DIM) facilitates protein-protein interactions, while the central High Mobility Group (HMG) box domain mediates DNA binding to specific consensus sequences (e.g., CCTTGAG) and contains nuclear localization and export signals that control its cellular trafficking [1] [3] [4]. The protein also contains two transcriptional activation domains - a central domain (TAM) and a C-terminal domain (TAC) - along with a proline-glutamine-alanine (PQA)-rich motif that enhances transactivation potency [3] [4]. The TAC domain is particularly significant as it competitively binds to the ARM repeats of β-catenin, thereby inhibiting the formation of β-catenin-TCF/LEF complexes and modulating Wnt signaling output [3].
SOX9 as a Central Regulator in the Tumor Microenvironment
SOX9 in Tumor-Associated Macrophage Signaling
The crosstalk between tumor cells and TAMs represents a critical axis in tumor progression, with SOX9 serving as a key mediator. Research in non-small cell lung cancer (NSCLC) demonstrates that TAMs secrete TGF-β, which activates the C-jun/SMAD3 pathway in cancer cells, leading to increased SOX9 expression [5] [6]. This SOX9 upregulation promotes epithelial-to-mesenchymal transition (EMT), characterized by reduced E-cadherin and increased vimentin expression, enhancing tumor cell migration and invasion capabilities [5]. This TGF-β/SOX9 axis establishes a feed-forward loop wherein tumor cells educated by TAMs become more aggressive, while simultaneously promoting M2 polarization of macrophages, further reinforcing the immunosuppressive TME [5].
SOX9 in Cancer Stem Cell Maintenance and Chemoresistance
Beyond its role in TAM signaling, SOX9 functions as a critical regulator of cancer stem cell (CSC) properties and therapy resistance. In high-grade serous ovarian cancer (HGSOC), SOX9 expression is epigenetically upregulated following platinum-based chemotherapy, where it drives a stem-like transcriptional state associated with chemoresistance [7]. SOX9 promotes transcriptional divergence - a metric of cellular plasticity - enabling cancer cells to adapt to therapeutic stress [7]. This reprogramming capacity allows SOX9 to regulate multiple resistance mechanisms, including the maintenance of CSC populations, enhancement of DNA damage repair, and activation of drug efflux transporters, positioning SOX9 as a central node in the therapeutic resistance network across multiple cancer types [2] [7].
SOX9 Interactions with Key Signaling Pathways
SOX9 engages in complex cross-regulation with several fundamental signaling pathways, particularly the canonical Wnt pathway. SOX9 can antagonize Wnt signaling through multiple mechanisms: promoting β-catenin degradation via ubiquitination/proteasome-dependent pathways, facilitating lysosomal breakdown of β-catenin, activating β-catenin antagonists like MAML2, and inhibiting β-catenin nuclear translocation [3]. Furthermore, the TAC domain of SOX9 competitively binds to the ARM repeats of β-catenin, preventing the formation of β-catenin-TCF/LEF transcriptional complexes and subsequently modulating the expression of Wnt target genes [3]. This intricate regulatory relationship creates a balance that influences cell fate decisions, stemness maintenance, and tumor progression within the TME.
Quantitative Analysis of SOX9 in Cancer
Table 1: SOX9 Expression and Clinical Correlations Across Cancers
| Cancer Type | SOX9 Expression Pattern | Correlation with Clinical Features | Prognostic Value | Reference |
|---|---|---|---|---|
| Breast Cancer | Frequently overexpressed | Associated with basal-like subtype, proliferation, and chemotherapy resistance | Shorter survival in ER-negative patients | [1] |
| Non-Small Cell Lung Cancer | Positively correlated with TAM density | Associated with EMT and metastasis | Co-expression with CD163 predicts poorer survival | [5] [6] |
| High-Grade Serous Ovarian Cancer | Chemotherapy-induced upregulation | Drives stem-like state and platinum resistance | Top quartile SOX9 expression associated with shorter overall survival | [7] |
| Malignant Bone Tumors | Overexpressed in tumor tissue and peripheral blood | Correlates with high grade, metastasis, and poor therapy response | Higher expression predicts recurrence and worse outcomes | [8] |
| Glioblastoma | Highly expressed in tumor tissue | Associated with IDH-mutant status and immune infiltration | Prognostic value varies by molecular context | [9] |
Table 2: SOX9-Associated Functional Phenotypes in the Tumor Microenvironment
| Functional Domain | Key Mechanisms | Experimental Evidence | Therapeutic Implications | |
|---|---|---|---|---|
| Immunomodulation | Promotes immune evasion by sustaining cancer cell stemness; regulates immune cell infiltration | SOX9 maintains latent cancer cell dormancy and avoids immune surveillance; correlates with altered T-cell and macrophage populations | Potential for combination with immune checkpoint inhibitors | [1] [4] |
| TME Crosstalk | Mediates cancer cell-fibroblast, macrophage, and endothelial cell interactions; responds to TGF-β from TAMs | Cell-cell interaction analysis reveals SOX9-dependent communication networks in TME | Targeting SOX9 may disrupt pro-tumorigenic stromal signaling | [1] [5] |
| Therapy Resistance | Drives transcriptional reprogramming to stem-like state; regulates drug efflux and DNA repair | SOX9 knockdown increases platinum sensitivity in ovarian cancer; overexpression induces chemoresistance | SOX9 inhibition may reverse acquired resistance to multiple agents | [2] [7] |
| Metastatic Progression | Promotes EMT through TGF-β/SOX9 axis; enhances migratory and invasive capabilities | SOX9 knockdown inhibits TGF-β-mediated EMT in lung cancer cells | Metastasis prevention through SOX9 pathway modulation | [5] [6] |
Experimental Protocols
Protocol: Investigating SOX9 Knockdown in Tumor-Associated Macrophages
Objective: To evaluate the functional consequences of SOX9 knockdown in TAMs on tumor cell behavior and TME dynamics.
Materials and Reagents:
- Human monocytic THP-1 cell line or primary human monocytes
- Phorbol 12-myristate 13-acetate (PMA) for macrophage differentiation
- IL-4 and IL-13 for M2 polarization
- SOX9-targeting siRNA or CRISPR/Cas9 constructs
- TGF-β receptor inhibitor (LY364947)
- Transwell co-culture systems
- ELISA kits for TGF-β, IL-10 quantification
- Antibodies for flow cytometry (CD163, CD206)
- Western blot reagents (SOX9, E-cadherin, vimentin antibodies)
Procedure:
Macrophage Differentiation and Polarization:
- Culture THP-1 cells in RPMI-1640 with 10% FBS.
- Differentiate into macrophages using 100 nM PMA for 48 hours.
- Polarize to M2 phenotype using 20 ng/mL IL-4 and 20 ng/mL IL-13 for 24 hours.
- Verify polarization by flow cytometry for CD163 and CD206 expression.
SOX9 Knockdown in TAMs:
- Transfert polarized TAMs with SOX9-targeting siRNA using lipid-based transfection reagent.
- Use scrambled siRNA as negative control.
- Confirm knockdown efficiency at 48-72 hours post-transfection by western blot and qRT-PCR.
Conditioned Media Collection and Co-culture:
- Collect conditioned media from SOX9-knockdown TAMs and control TAMs.
- Alternatively, establish direct co-culture systems using Transwell inserts.
- Treat cancer cells (A549, H1299 for NSCLC or other appropriate lines) with TAM-conditioned media or co-culture for 24-48 hours.
Functional Assays:
- Migration and Invasion: Perform Transwell migration and Matrigel invasion assays with cancer cells exposed to TAM-conditioned media.
- EMT Marker Analysis: Evaluate E-cadherin (epithelial) and vimentin (mesenchymal) expression in cancer cells by western blot.
- Cytokine Profiling: Quantify TGF-β, IL-10, and other cytokine levels in conditioned media using ELISA.
TGF-β/SOX9 Axis Validation:
- Treat cancer cells with recombinant TGF-β (5 ng/mL) with or without TGF-β receptor inhibitor.
- Assess SOX9 expression changes in cancer cells by western blot.
- Perform SOX9 knockdown in cancer cells to confirm necessity for TGF-β-mediated effects.
Expected Outcomes: SOX9 knockdown in TAMs should reduce TGF-β secretion, decrease cancer cell migration and invasion, and reverse EMT markers in cancer cells, demonstrating the critical role of TAM-expressed SOX9 in promoting tumor progression.
Protocol: Assessing SOX9-Mediated Chemoresistance
Objective: To determine the role of SOX9 in promoting chemotherapy resistance and stem-like properties.
Materials and Reagents:
- Appropriate cancer cell lines (e.g., OVCAR4, Kuramochi for HGSOC)
- Platinum drugs (carboplatin, cisplatin)
- SOX9 overexpression constructs
- SOX9-targeting sgRNA and CRISPR/Cas9 components
- Colony formation assay reagents
- Cancer stem cell markers (CD44, CD133) antibodies
- Aldefluor assay kit
Procedure:
Chemotherapy-Induced SOX9 Expression:
- Treat cancer cells with IC50 concentrations of carboplatin for 72 hours.
- Monitor SOX9 expression at RNA and protein levels by qRT-PCR and western blot.
SOX9 Modulation and Chemosensitivity:
- Establish SOX9 knockout cells using CRISPR/Cas9 and SOX9-overexpressing cells using lentiviral transduction.
- Treat modified cells with gradient concentrations of chemotherapy drugs.
- Assess cell viability using MTT assay and clonogenic survival using colony formation assays.
Cancer Stem Cell Enrichment Analysis:
- Evaluate cancer stem cell populations in SOX9-modified cells by flow cytometry for CD44/CD133.
- Perform Aldefluor assay to measure aldehyde dehydrogenase activity.
- Conduct sphere formation assays in ultra-low attachment plates.
Transcriptional Divergence Assessment:
- Perform single-cell RNA sequencing on SOX9-modified cells with and without chemotherapy.
- Calculate transcriptional divergence using P50/P50 ratio as described [7].
The Scientist's Toolkit
Table 3: Essential Research Reagents for SOX9-TME Studies
| Reagent/Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| SOX9 Modulation Tools | SOX9-targeting siRNA, shRNA, CRISPR/Cas9 constructs; SOX9 overexpression plasmids | Gain- and loss-of-function studies to establish causality | Verify efficiency by multiple methods; consider inducible systems for temporal control |
| TAM Modeling Systems | THP-1 cell line, primary human monocytes, PMA, IL-4/IL-13 polarization cytokines | Establish physiologically relevant TAM models in vitro | Validate polarization status with surface markers (CD163, CD206) and cytokine secretion |
| Signaling Modulators | Recombinant TGF-β, TGF-β receptor inhibitors (LY364947), Wnt pathway activators/inhibitors | Pathway-specific manipulation to dissect molecular mechanisms | Use multiple inhibitors with different mechanisms to confirm specificity |
| Analysis Tools | SOX9 antibodies (IHC, WB, flow cytometry), EMT antibody panels, cytokine ELISA kits | Phenotypic and molecular characterization | Validate antibodies in multiple applications; use multiplex assays for comprehensive profiling |
| Functional Assays | Transwell migration/invasion systems, colony formation assays, 3D spheroid co-culture models | Assess functional consequences of SOX9 manipulation | Implement appropriate controls for assay-specific artifacts; use multiple complementary assays |
SOX9 emerges as a master regulator within the tumor microenvironment, integrating signals from multiple cellular compartments to drive tumor progression, therapy resistance, and immune evasion. The experimental protocols outlined provide a framework for investigating SOX9 function in TAMs and its broader role in modulating TME dynamics. Targeting the SOX9 pathway represents a promising therapeutic strategy worthy of further investigation, particularly in combination with conventional chemotherapy and emerging immunotherapies. Future studies should focus on developing selective SOX9 inhibitors and evaluating their efficacy in disrupting the pro-tumorigenic networks orchestrated by SOX9 within the complex ecosystem of the tumor microenvironment.
Linking TAM-Secreted TGF-β to SOX9 Upregulation and Metastasis
Within the tumor microenvironment (TME), tumor-associated macrophages (TAMs) are a major stromal component that profoundly influences cancer progression. Most TAMs exhibit an immunosuppressive M2 phenotype, which affects the TME and promotes metastasis [5]. A key mechanism underlying this pro-tumoral activity is the secretion of cytokines, among which Transforming Growth Factor-beta (TGF-β) plays a pivotal role [5] [10]. This application note delineates the mechanistic pathway linking TAM-secreted TGF-β to the upregulation of the transcription factor SOX9 in cancer cells, a critical event driving epithelial-to-mesenchymal transition (EMT), tumor invasion, and metastasis. Furthermore, it provides detailed protocols for investigating this axis, framing the research within the broader context of therapeutic SOX9 knockdown strategies.
Key Quantitative Findings: The TGF-β/SOX9 Axis
Research consistently demonstrates that the TGF-β/SOX9 pathway is a powerful driver of tumor aggression and poor patient outcomes. The tables below summarize key clinical and experimental data.
Table 1: Clinical Correlations of TAM Density and SOX9 Expression in Human Cancers
| Cancer Type | Correlation Finding | Prognostic Impact | Study Reference |
|---|---|---|---|
| Non-Small Cell Lung Cancer (NSCLC) | Positive correlation between CD163+ TAM density and SOX9+ staining [5] | High co-expression of CD163 and SOX9 associated with shorter overall and disease-free survival [5] | [5] |
| Various Solid Tumors (Meta-Analysis) | --- | High SOX9 expression predicts poor overall survival (HR: 1.66) and disease-free survival (HR: 3.54) [11] | [11] |
| Pancreatic Cancer | SOX9 demethylation and overexpression in invasive Cancer Stem Cells (CSCs) [12] | Contributes to invasiveness and stem cell-like properties [12] | [12] |
Table 2: Experimental Evidence of TAM/Cancer Cell Crosstalk
| Experimental Setup | Key Outcome | Signaling Pathway Implicated | Study Reference |
|---|---|---|---|
| Co-culture of macrophages with A549/H1299 lung cancer cells | Induction of EMT-like phenotype; Increased SOX9 protein and mRNA levels [5] | TGF-β / SOX9 [5] | [5] |
| Treatment of lung cancer cells with recombinant TGF-β | Increased SOX9 expression and EMT; Effects blocked by TGF-β receptor inhibitor [5] | TGF-β / C-jun / SMAD3 [5] | [5] |
| SOX9 knockdown in cancer cells co-cultured with macrophages | Inhibition of EMT; Reduced tumor cell migration and invasion [5] | SOX9-dependent EMT [5] | [5] |
| Analysis of pancreatic CSCs | NF-κB p65 subunit directly binds SOX9 promoter to regulate its expression [12] | NF-κB / SOX9 [12] | [12] |
Detailed Experimental Protocols
Protocol 1: In Vitro TAM-Cancer Cell Co-culture and SOX9 Expression Analysis
This protocol assesses the direct effect of TAM-secreted factors on SOX9 upregulation in cancer cells.
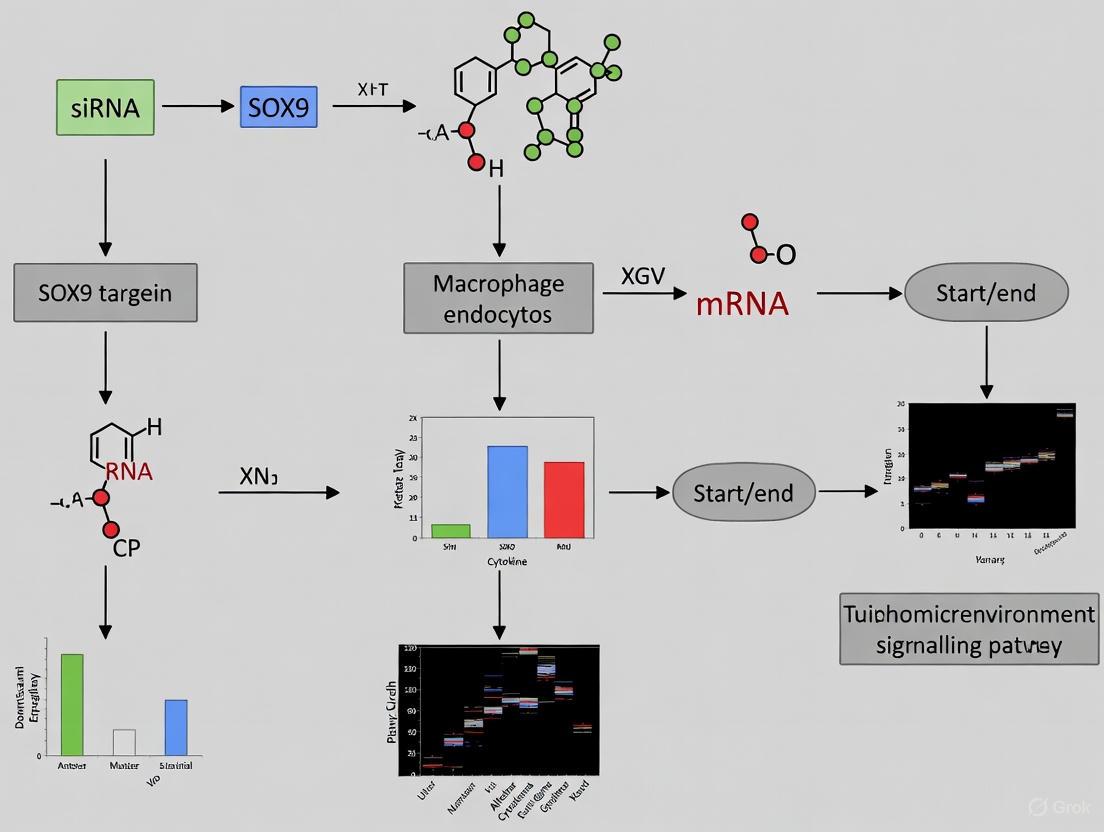
Workflow Diagram: Co-culture and Analysis
Methodology:
- TAM Generation: Differentiate human monocytic THP-1 cells into M2 macrophages using Phorbol 12-myristate 13-acetate (PMA, 100 nM for 24-48 hours), followed by polarization with IL-4 (20 ng/mL) and IL-13 (20 ng/mL) for an additional 48 hours [5] [10].
- Conditioned Medium (CM) Collection: Culture the differentiated M2 macrophages in serum-free medium for 24-48 hours. Centrifuge the collected supernatant to remove cells and debris. Aliquot and store at -80°C.
- Cancer Cell Treatment: Seed target cancer cells (e.g., A549, H1299). At 60-70% confluency, replace the medium with the TAM-conditioned medium. Include control groups with normal medium and medium with recombinant TGF-β (e.g., 5-10 ng/mL). To confirm TGF-β dependency, pre-treat cells with a TGF-β receptor inhibitor (e.g., SB431542, 10 µM) for 1 hour before CM application [5].
- Downstream Analysis: After 24-72 hours of treatment, harvest cells for:
- SOX9 mRNA: Extract RNA, perform reverse transcription, and analyze SOX9 levels via qPCR.
- SOX9 Protein: Lyse cells for Western Blotting or fix for Immunofluorescence staining using anti-SOX9 antibodies.
- Functional Assays: Perform transwell migration and invasion assays to assess phenotypic changes [5].
Protocol 2: Validating the TGF-β/SOX9 Axis via SOX9 Knockdown
This protocol determines the necessity of SOX9 in TGF-β-mediated EMT and metastasis.
Methodology:
- SOX9 Knockdown: Generate stable SOX9-knockdown cell lines using lentiviral transduction with shRNAs targeting SOX9. A non-targeting shRNA should be used as a negative control.
- Rescue Experiments: For rescue experiments, transfer a SOX9 overexpression plasmid into the knockdown cells using a suitable transfection reagent.
- TGF-β Stimulation: Treat the SOX9-knockdown and control cells with recombinant TGF-β (5-10 ng/mL) for 48 hours [5].
- EMT and Functional Analysis:
- EMT Marker Analysis: Analyze EMT markers (E-cadherin, Vimentin, N-cadherin) by Western Blot to confirm the mesenchymal phenotype is blocked upon SOX9 knockdown.
- Proliferation/Migration/Invasion Assays:
- Proliferation: Use MTT or CCK-8 assays.
- Migration/Invasion: Use transwell assays with (invasion) or without (migration) Matrigel coating. Seed cells in the upper chamber and quantify cells that migrate/invade to the lower chamber after 24-48 hours [5].
Signaling Pathways: From TAMs to Metastasis
The diagram below illustrates the core signaling pathway and the experimental strategy for its inhibition.
Signaling Pathway and Therapeutic Targeting
As shown, TAM-secreted TGF-β binds to its receptor on cancer cells, initiating both canonical (SMAD3/SMAD4) and non-canonical (C-jun) signaling pathways that converge to activate SOX9 transcription [5]. In certain contexts, such as pancreatic cancer, the NF-κB pathway can also directly bind the SOX9 promoter and drive its expression [12] [13]. Elevated SOX9 then orchestrates the EMT program, leading to enhanced cell migration, invasion, and ultimately, metastasis.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Investigating the TAM TGF-β/SOX9 Axis
| Reagent / Tool | Function / Application | Example Products / Assays |
|---|---|---|
| TGF-β Receptor Inhibitor | Blocks TGF-β signaling to confirm pathway specificity in experiments. | SB431542, Galunisertib [5] |
| Recombinant Human TGF-β | Positive control for stimulating the TGF-β/SOX9 pathway in cancer cells. | PeproTech, R&D Systems [5] |
| SOX9 shRNA/siRNA | Knocks down SOX9 expression to validate its functional necessity in metastasis. | Lentiviral sh particles, siRNA oligos [5] |
| SOX9 Antibodies | Detects SOX9 expression and localization in cells and tissues (IHC, IF, WB). | Santa Cruz (sc-166505), Millipore (AB5535) [11] |
| EMT Antibody Sampler Kit | Simultaneously analyzes key EMT markers (E-cadherin, Vimentin, N-cadherin). | Cell Signaling Technology (#97872) [5] |
| Transwell / Boyden Chambers | Quantifies cancer cell migration and invasion capabilities after experimental manipulation. | Corning Costar inserts, with Matrigel for invasion assays [5] |
| NF-κB Pathway Inhibitor | Inhibits the NF-κB pathway to investigate its role in SOX9 regulation. | JSH-23, SM-7368 [12] |
Concluding Remarks
The TGF-β/SOX9 axis is a critical signaling node driven by TAMs to promote tumor metastasis. The protocols and tools detailed herein provide a robust framework for researchers to dissect this pathway, from initial ligand-receptor interaction to downstream functional outcomes. Given the strong association between SOX9 overexpression and poor patient prognosis, targeting SOX9—either directly or through its upstream regulators like TGF-β—represents a promising therapeutic strategy. Future work should focus on developing specific SOX9 inhibitors and evaluating their efficacy, particularly in combination with TAM-depleting or reprogramming therapies, to combat advanced and metastatic cancers.
SOX9 (SRY-related HMG-box 9) is an established transcription factor with critical functions in development and stem cell maintenance. Recent research has solidified its dual role as a master regulator of both epithelial-mesenchymal transition (EMT) and tumor immune suppression, making it a high-value target for therapeutic intervention [14] [4]. Its activity is particularly relevant in the context of the tumor microenvironment (TME), where it is influenced by and, in turn, influences key stromal components like tumor-associated macrophages (TAMs) [5] [15]. This Application Note details the mechanistic insights into SOX9's functions and provides standardized protocols for investigating its role, with a specific focus on SOX9 knockdown in TAM-co-culture models.
Key Mechanisms of SOX9 in Cancer Progression
SOX9 as a Central Mediator of EMT
SOX9 is a potent inducer of EMT, a process crucial for tumor metastasis, by regulating key signaling pathways.
- TGF-β/SOX9 Axis: In non-small cell lung cancer (NSCLC), TAMs secrete TGF-β, which upregulates SOX9 expression via the C-jun/SMAD3 pathway. This SOX9 upregulation is necessary and sufficient to drive EMT, as evidenced by decreased E-cadherin and increased vimentin expression [5].
- Functional Validation: Knockdown of SOX9 in lung cancer cells (e.g., A549, H1299) co-cultured with TAMs almost completely inhibits the TGF-β-mediated EMT phenotype, confirming its pivotal role in this process [5].
SOX9 as a Potent Suppressor of Anti-Tumor Immunity
SOX9 facilitates tumor immune evasion through multiple distinct mechanisms, effectively creating an immunosuppressive TME.
- Inhibition of Immune Cell Infiltration: Bioinformatics analyses across cancers reveal that high SOX9 expression negatively correlates with the infiltration levels of cytotoxic lymphocytes, including CD8+ T cells and NK cells [14] [4].
- Promotion of Immunosuppressive Cells: SOX9 activity is associated with increased infiltration of regulatory immune cells. It promotes the accumulation of T-regulatory cells (Tregs) and M2-like TAMs in the TME [14] [4].
- Regulation of Immune Checkpoints: SOX9 can transactivate the expression of PD-L1 (programmed death-ligand 1) on tumor and other cells in the TME, directly engaging with the PD-1 checkpoint to inhibit T-cell function [14] [4].
- Impairment of Antigen Presentation: SOX9 expression is linked to the downregulation of genes involved in antigen processing and presentation, blunting the ability of the adaptive immune system to recognize tumor cells [14].
Table 1: SOX9-Mediated Mechanisms of Immune Suppression
| Mechanism | Functional Outcome | Evidence |
|---|---|---|
| Reduced CD8+ T cell Infiltration | Diminished cytotoxic T-cell activity in tumor core | Correlation analysis in liver, breast cancer [14] |
| Increased Treg & M2-TAM Accumulation | Immunosuppressive microenvironment | Positive correlation with Treg/TAM markers [14] [4] |
| PD-L1 Transactivation | T-cell exhaustion and anergy | Direct transcriptional regulation [14] [4] |
| Downregulation of Antigen Presentation | Avoidance of immune detection | Down-regulation of antigen processing pathway genes [14] |
Visualizing the TAM-SOX9-EMT Signaling Axis
The diagram below illustrates the core signaling pathway by which Tumor-Associated Macrophages (TAMs) activate the SOX9 program to drive EMT and immune suppression in cancer cells.
Experimental Protocol: SOX9 Knockdown in a TAM-Tumor Co-culture Model
This protocol outlines a methodology to investigate the functional consequences of SOX9 knockdown in tumor cells on TAM-induced EMT and immune suppression.
Protocol Workflow
Detailed Experimental Procedures
Part 1: Generation of Tumor-Associated Macrophages (TAMs)
- Human Monocyte Isolation: Isolate peripheral blood mononuclear cells (PBMCs) from healthy donor buffy coats using density gradient centrifugation (e.g., Ficoll-Paque).
- Monocyte Differentiation: Adhere monocytes to tissue culture plates for 2 hours. Remove non-adherent cells. Differentiate adherent monocytes into macrophages by culturing for 6-7 days in RPMI-1640 medium supplemented with 100 ng/mL M-CSF.
- M2 Polarization (TAM-like): Polarize the resulting macrophages towards an M2-like, TAM phenotype by treating for 48 hours with 20 ng/mL IL-4 and 20 ng/mL IL-13 [5] [15]. Confirm polarization by assessing surface markers (e.g., CD206, CD163) via flow cytometry.
Part 2: Tumor Cell Culture and SOX9 Knockdown
- Cell Line Selection: Culture relevant cancer cell lines (e.g., A549 or H1299 for lung cancer, MDA-MB-231 for breast cancer) in their recommended media.
- SOX9 Knockdown:
- Transfection: Transfect tumor cells at 60-70% confluency with SOX9-specific siRNA or a non-targeting scrambled siRNA control using a suitable transfection reagent.
- Lentiviral Transduction (Alternative): For stable knockdown, transduce tumor cells with lentiviral particles carrying shRNA against SOX9 (sh-SOX9) or a non-targeting control (sh-NC). Apply appropriate selection antibiotics (e.g., Puromycin) for 3-5 days to generate a polyclonal knockdown population [5].
- Validation: 48-72 hours post-transfection/selection, validate knockdown efficiency by:
- qRT-PCR: Analyze SOX9 mRNA levels.
- Western Blot: Confirm reduction in SOX9 protein expression.
Part 3: Co-culture Establishment
- Setup: Seed SOX9-knockdown or control tumor cells in the lower chamber of a transwell system.
- TAM Addition: Plate the generated TAMs in the upper chamber insert (e.g., 0.4 µm pore size for factor exchange). Alternatively, to collect TAM-conditioned media (TCM), culture TAMs alone for 48 hours, collect the supernatant, filter it, and apply it to the tumor cells [5].
- Incubation: Maintain the co-culture for 48-72 hours to allow for paracrine signaling.
Part 4: Phenotypic Analysis
- Migration & Invasion Assay: After co-culture, harvest tumor cells and seed them into Matrigel-coated (invasion) or uncoated (migration) transwell inserts. Allow cells to migrate/invade for 24-48 hours. Fix, stain (e.g., with Crystal Violet), and count the cells that have traversed the membrane [5].
- Proliferation Assay: Perform assays like CCK-8 or EdU incorporation at 0, 24, 48, and 72 hours post-co-culture to assess changes in tumor cell proliferation.
Part 5: Molecular Analysis
- Western Blotting: Analyze protein lysates from co-cultured tumor cells for:
- EMT Markers: E-cadherin (epithelial, downregulated in EMT), Vimentin, N-cadherin (mesenchymal, upregulated in EMT) [5].
- Pathway Analysis: Phospho-SMAD3, total SMAD3, C-jun.
- qRT-PCR: Quantify mRNA expression of EMT markers and SOX9 target genes.
- Immunofluorescence: Stain co-cultured tumor cells for E-cadherin and Vimentin to visualize the morphological and molecular shifts associated with EMT.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for SOX9 and TAM Research
| Reagent / Tool | Function / Specificity | Application in Protocol |
|---|---|---|
| M-CSF (Human) | Differentiates monocytes into macrophages | Generation of primary human macrophages from PBMCs [15] |
| IL-4 & IL-13 | Cytokines for M2 macrophage polarization | Induction of TAM-like phenotype [5] [15] |
| SOX9 siRNA/shRNA | Targets SOX9 mRNA for degradation | Knockdown of SOX9 in tumor cell lines [5] |
| TGF-β Receptor Inhibitor | Selective kinase inhibitor (e.g., SB431542) | Inhibition of TGF-β signaling to validate pathway specificity [5] |
| Anti-CD206 (MMR) | Antibody against M2 macrophage surface marker | Confirmation of TAM polarization via flow cytometry [15] |
| Anti-E-cadherin Antibody | Binds epithelial adhesion protein | Detection of EMT status by Western Blot/IF [5] |
| Anti-Vimentin Antibody | Binds intermediate filament protein in mesenchymal cells | Detection of EMT status by Western Blot/IF [5] |
| Cordycepin | Natural adenosine analog, SOX9 inhibitor | Small-molecule inhibition of SOX9 for therapeutic validation [16] [17] |
The experimental evidence solidifies SOX9's position as a critical node linking the pro-tumorigenic processes of EMT and immune evasion. The TGF-β/SOX9 axis, strongly influenced by TAMs, is a key driver of this malignant phenotype [5]. The protocols detailed herein provide a framework to dissect this axis.
From a therapeutic perspective, targeting SOX9 holds significant promise. Strategies include direct inhibition with small molecules like cordycepin, which has been shown to downregulate SOX9 expression in a dose-dependent manner [16] [17], or indirect targeting via upstream pathways such as TGF-β signaling. Combining SOX9-targeted approaches with existing immunotherapies (e.g., anti-PD-1/PD-L1) could potentially overcome mechanisms of immune escape and provide more durable anti-tumor responses. The reagents and methods outlined in this Application Note provide a foundational toolkit for researchers aiming to validate SOX9 as a therapeutic target and develop novel anti-cancer strategies.
Non-small cell lung cancer (NSCLC) remains a leading cause of cancer-related mortality worldwide, with tumor metastasis representing a primary cause of treatment failure and poor prognosis. The tumor microenvironment (TME) plays a crucial role in cancer progression, with tumor-associated macrophages (TAMs) being a key component. Most TAMs exhibit an M2 immunosuppressive phenotype characterized by expression of the scavenger receptor CD163, which promotes tumor progression through various mechanisms [5] [18] [19]. Simultaneously, the transcription factor SOX9 has emerged as an important regulator of tumor metastasis in NSCLC [20].
This Application Note explores the clinical correlation between SOX9 and CD163 as prognostic markers in NSCLC, framed within the context of a broader thesis investigating SOX9 knockdown in TAMs. We summarize quantitative clinical data, detail experimental methodologies for studying this relationship, and visualize the underlying signaling pathways.
Clinical Data Correlation
Association with Patient Survival
Analysis of clinical NSCLC specimens reveals significant prognostic implications for both CD163-positive TAMs and SOX9 expression:
Table 1: Prognostic Significance of CD163 and SOX9 in NSCLC
| Marker | Expression Level | Overall Survival | Disease-Free Survival | Statistical Significance |
|---|---|---|---|---|
| CD163+ TAMs | High density | Shorter | Shorter | p < 0.01 [5] |
| SOX9 | High expression | Shorter | Shorter | p < 0.01 [5] |
| CD163 & SOX9 combined | Co-expression | Shortest | Shortest | p < 0.01 [5] |
Immunohistochemical analysis of 164 NSCLC patient specimens demonstrated that high densities of CD163+ TAMs were significantly associated with poor prognosis [5]. Similarly, SOX9 overexpression correlated with advanced TNM stage (p=0.03 for T stage, p=0.000 for N stage, p=0.032 for M stage) and poorer survival outcomes [20]. Most notably, patients exhibiting co-expression of both markers experienced the shortest overall and disease-free survival, suggesting a potential synergistic effect [5].
Correlation in Tumor Tissues
Table 2: Correlation Analysis Between CD163+ TAM Density and SOX9 Expression
| Parameter | Correlation | Experimental Method | Biological Significance |
|---|---|---|---|
| TAM density vs. SOX9 expression | Positive correlation | Immunofluorescent staining [5] | TAMs may promote SOX9 expression in tumor cells |
| SOX9+ staining pattern | Co-localization with TAM-rich areas | Immunohistochemistry [5] | Spatial relationship in tumor microenvironment |
| TAM secretion | TGF-β production | Cytokine analysis [5] | Mechanism for SOX9 induction |
Immunofluorescent staining of human NSCLC tissues revealed a positive correlation between the density of CD163+ TAMs and SOX9 expression in cancer cells [5]. This correlation was particularly evident in the invasive front of tumors where TAMs abundantly infiltrate [5]. Further investigation identified that TAMs secrete transforming growth factor-β (TGF-β), which promotes SOX9 expression in cancer cells [5].
Molecular Mechanisms
TAM-Induced SOX9 Expression and EMT
TAMs promote tumor progression through SOX9-mediated epithelial-mesenchymal transition (EMT):
Figure 1: TAM-Driven SOX9 Signaling Pathway in NSCLC Metastasis. Tumor-associated macrophages (TAMs) secrete TGF-β, which activates the C-jun/SMAD3 pathway to induce SOX9 expression, promoting epithelial-mesenchymal transition (EMT) and metastasis [5].
The molecular pathway involves TAMs secreting TGF-β, which activates the C-jun/SMAD3 pathway in cancer cells, leading to increased SOX9 expression [5]. Elevated SOX9 then drives the EMT process, characterized by decreased epithelial markers (E-cadherin, γ-catenin) and increased mesenchymal markers (N-cadherin, vimentin) [5] [20]. This transition enhances tumor cell migration, invasion, and metastatic potential [5].
SOX9 in Cancer Stem-Like Properties
Beyond EMT, SOX9 also regulates cancer stem-like cells (CSCs) in NSCLC. SOX9 knockdown experiments demonstrated reduced tumor sphere formation, decreased ALDH activity (a marker for CSCs), and suppressed expression of the stem cell marker ALDH1A1 [21]. This suggests SOX9 contributes to the maintenance of stem-like properties in tumor cells, further enhancing their metastatic potential and treatment resistance.
Experimental Protocols
Co-culture Protocol for TAM-Cancer Cell Interactions
Objective: To investigate the functional crosstalk between TAMs and NSCLC cells and its effect on SOX9 expression and EMT.
Table 3: Research Reagent Solutions for Co-culture Experiments
| Reagent | Function | Application Notes |
|---|---|---|
| THP-1 human monocytic cell line | Source for macrophage differentiation | Culture in RPMI-1640 with 10% FBS [5] |
| Phorbol 12-myristate 13-acetate (PMA) | Induces macrophage differentiation | 100 nM for 24 hours [5] |
| A549 and H1299 NSCLC cells | Model cancer cell lines | Culture in DMEM with 10% FBS [5] |
| Recombinant TGF-β | Positive control for SOX9 induction | 10 ng/mL for 48 hours [5] |
| TGF-β receptor inhibitor | Pathway inhibition control | Confirm TGF-β dependency [5] |
Methodology:
- Macrophage Differentiation: Differentiate THP-1 monocytes into macrophages using 100 nM PMA for 24 hours [5].
- Conditioned Media Collection: Collect supernatant from differentiated macrophages by centrifugation at 1,000 × g for 10 minutes [5].
- Co-culture Setup:
- Direct co-culture: Seed macrophages and NSCLC cells together in appropriate ratio
- Indirect co-culture: Treat NSCLC cells with macrophage-conditioned media
- Incubation: Maintain co-cultures for 24-48 hours [5].
- Analysis:
- Western blot: Analyze SOX9, E-cadherin, vimentin protein levels
- qRT-PCR: Quantify SOX9 mRNA expression
- Immunofluorescence: Assess cellular morphology and marker localization
SOX9 Knockdown and Functional Assays
Objective: To determine the functional necessity of SOX9 in TAM-mediated NSCLC progression.
Methodology:
- SOX9 Knockdown:
Functional Assays:
In Vivo Metastasis:
Immunohistochemical Staining and Scoring
Objective: To correlate CD163 and SOX9 expression patterns in clinical NSCLC specimens.
Methodology:
- Tissue Preparation: Obtain 142-164 formalin-fixed, paraffin-embedded NSCLC specimens [5] [20].
- Sectioning: Cut 4-5μm sections and mount on charged slides.
- Antigen Retrieval: Perform heat-induced epitope retrieval in citrate buffer (pH 6.0).
- Antibody Incubation:
- Primary antibodies: Anti-CD163 (1:200) and anti-SOX9 (1:150)
- Secondary antibodies: HRP-conjugated appropriate species-specific antibodies
- Detection: DAB chromogen development and hematoxylin counterstaining.
- Scoring:
- CD163+ TAM density: Count positive cells in 5 high-power fields (400×)
- SOX9 expression: Score based on intensity (0-3) and percentage of positive tumor cells
- Statistical analysis: Correlate with clinicopathological parameters using χ² test and Spearman's analysis
Therapeutic Implications
The SOX9/CD163 axis represents a promising therapeutic target in NSCLC. Several strategic approaches emerge:
Figure 2: Therapeutic Targeting Strategies for the SOX9/CD163 Axis in NSCLC. Multiple approaches include inhibiting TAM recruitment, depleting existing TAMs, repolarizing TAMs to anti-tumor M1 phenotype, direct SOX9 inhibition, and TGF-β pathway blockade [22] [19].
Small molecule drugs targeting TAMs are being developed that:
- Block monocyte recruitment (CCL2/CCR2, CSF-1/CSF-1R inhibitors) [22]
- Deplete existing TAMs in tumor tissue [22]
- Reprogram TAMs toward pro-inflammatory M1 phenotype (STAT3, STAT6 inhibitors) [22]
- Interrupt TAM-tumor cell interactions (CD47/SIRPα targeting) [22]
Simultaneously, targeting SOX9 downstream of TAM signaling may provide an alternative strategy to inhibit metastasis without directly affecting immune cells.
The clinical correlation between SOX9 and CD163 in NSCLC provides valuable insights into tumor biology and represents a promising prognostic biomarker signature. The mechanistic link involving TAM-derived TGF-β driving SOX9-mediated EMT and cancer stem-like properties offers multiple therapeutic intervention points. Further research, particularly investigating SOX9 knockdown in TAMs themselves, may reveal additional layers of complexity in this clinically relevant pathway. The experimental protocols outlined herein provide a framework for such investigations, with potential to identify novel therapeutic strategies for advanced NSCLC.
The Rationale for SOX9 Knockdown as an Anti-Cancer Strategy
The SRY-Box Transcription Factor 9 (SOX9) is an embryonic transcription factor that regulates critical developmental processes, including cell differentiation, proliferation, and stem cell maintenance [1]. In recent years, compelling evidence has established SOX9 as a significant oncoprotein across multiple cancer types. Its aberrant overexpression is frequently observed in malignancies such as cervical cancer, non-small cell lung cancer (NSCLC), breast cancer, pancreatic ductal adenocarcinoma (PDAC), and intrahepatic cholangiocarcinoma (iCCA) [23] [5] [1]. SOX9 drives tumorigenesis by modulating key cancer hallmarks, including sustained proliferation, metastasis, chemoresistance, and stemness. Consequently, targeted knockdown of SOX9 has emerged as a promising therapeutic strategy to disrupt multiple oncogenic pathways simultaneously.
Molecular Rationale for SOX9 Targeting
SOX9 in Tumor Progression and Metastasis
SOX9 promotes tumor metastasis primarily by regulating the epithelial-to-mesenchymal transition (EMT), a key process enabling cancer cell invasion and dissemination. In the tumor microenvironment, SOX9 expression in cancer cells can be induced by external signals, such as TGF-β secreted by tumor-associated macrophages (TAMs) [5] [6]. This TGF-β/SOX9 axis activation leads to characteristic EMT changes: loss of epithelial markers like E-cadherin and gain of mesenchymal markers like vimentin, resulting in enhanced migratory and invasive capabilities [5]. Furthermore, SOX9 contributes to metastasis by activating the PLOD3/IL-6/JAK/STAT3 signaling cascade. Research in cervical cancer demonstrates that SOX9 directly binds to the PLOD3 promoter to activate its transcription, which in turn promotes cancer progression via the IL-6/JAK/STAT3 pathway [23] [24].
Table 1: SOX9-Driven Molecular Axes in Cancer Progression
| Molecular Axis | Cancer Type Studied | Key Downstream Effects |
|---|---|---|
| TGF-β/SOX9 [5] [6] | Non-Small Cell Lung Cancer (NSCLC) | Induction of EMT, increased migration and invasion |
| SOX9/PLOD3/IL-6/JAK/STAT3 [23] [24] | Cervical Cancer | Enhanced cell proliferation, clone formation, migration, invasion, and angiogenesis |
| SOX9/ALDH1A1 [25] | NSCLC | Increased chemoresistance and cancer stem-like properties |
| SOX9/EpCAM [26] | Pancreatic Ductal Adenocarcinoma (PDAC) | Maintenance of cancer stem cell features and ciliary repression |
SOX9 in Chemoresistance and Cancer Stemness
A major challenge in oncology is overcoming resistance to chemotherapy, and SOX9 has been identified as a key regulator of chemoresistance in multiple cancers. In intrahepatic cholangiocarcinoma (iCCA), patients with high SOX9 expression had a significantly shorter median survival time (22 months) compared to those with low expression (62 months) after chemotherapy [27]. Mechanistically, gemcitabine treatment itself upregulates SOX9 expression, creating a therapeutic feedback loop that promotes survival. SOX9 knockdown markedly increases chemotherapy-induced apoptosis and suppresses the expression of multidrug resistance genes [27].
SOX9 also confers treatment resistance by enriching and maintaining cancer stem-like cells (CSCs), a subpopulation notorious for being refractory to conventional therapies. SOX9 promotes the self-renewal capacity of CSCs, as evidenced by enhanced tumor sphere formation in vitro [25]. This function is partly mediated through the direct transcriptional activation of ALDH1A1, a universal CSC marker and enzyme that detoxifies chemotherapeutic agents [25]. The SOX9-ALDH1A1 axis is therefore a critical mechanism for chemoresistance.
SOX9 in the Tumor Microenvironment and Immune Evasion
The oncogenic role of SOX9 extends beyond cancer cells into the tumor microenvironment (TME). SOX9 expression in cancer cells is influenced by crosstalk with tumor-associated macrophages (TAMs). TAMs secrete TGF-β, which upregulates SOX9 in cancer cells via the C-jun/SMAD3 pathway, thereby promoting metastasis [5] [6]. Furthermore, SOX9 is crucial for immune evasion, enabling latent cancer cells to persist in secondary sites by avoiding immune surveillance [1].
Experimental Evidence Supporting SOX9 Knockdown
Knockdown of SOX9, primarily via RNA interference (RNAi), consistently produces potent anti-tumor effects across diverse in vitro and in vivo models.
Table 2: Anti-Cancer Effects of SOX9 Knockdown in Experimental Models
| Experimental Context | Key Findings Post-SOX9 Knockdown | Citation |
|---|---|---|
| Cervical Cancer (HeLa cells) | Suppressed cell proliferation, clone formation, migration, invasion, and angiogenesis; induced apoptosis. | [23] [24] |
| Non-Small Cell Lung Cancer (NSCLC) | Inhibition of TGF-β-mediated EMT; reduced migration and invasion; increased sensitivity to cisplatin, paclitaxel, and etoposide. | [5] [25] |
| Pancreatic Cancer (PANC-1 cells) | 93 differentially expressed genes; downregulation of stem cell marker EpCAM; upregulation of cilia-associated genes. | [26] |
| Intrahepatic Cholangiocarcinoma (iCCA) | Increased gemcitabine-induced apoptosis; inhibited phosphorylation of checkpoint kinase 1 (CHK1); suppressed multidrug resistance genes. | [27] |
| In Vivo Nude Mouse Models | SOX9 knockdown suppressed tumor growth and metastasis in cervical cancer models. | [23] [24] |
Application Notes & Protocols: Implementing SOX9 Knockdown
siRNA Design and Validation Guidelines
Effective SOX9 knockdown hinges on the careful design and selection of small interfering RNAs (siRNAs). The following guidelines, synthesized from established literature and technical resources, are critical for success [28] [29].
- Design Principles:
- Target Sequence Selection: Identify 21 nucleotide (nt) sequences within the SOX9 mRNA (NM_000346.3) that begin with an AA dinucleotide. The target site should be located within the coding region, starting from the AUG start codon.
- Sequence Composition: Select sequences with 30-50% GC content. Avoid sequences with stretches of more than four consecutive T's or A's, as these can act as premature termination signals for RNA polymerase III.
- Specificity Check: Perform a BLAST search against the relevant genome database to ensure the siRNA has less than 16-17 contiguous base pairs of homology with other coding sequences to minimize off-target effects.
- Empirical Validation:
- Test Multiple Sequences: Given that siRNA efficacy is variable, it is essential to design and experimentally test 2-4 different siRNA sequences targeting distinct regions of the SOX9 transcript.
- Positive Control: Include a well-validated, commercially available SOX9 siRNA in initial experiments. For example, Dharmacon's ON-TARGETplus SMARTpool against human SOX9 (Catalog # M-021507-00) has been successfully used in research [27].
- Negative Control: Use a non-targeting scrambled siRNA sequence with the same nucleotide composition as your specific siRNA but lacking significant sequence homology to any gene in the target genome.
Detailed Protocol: SOX9 Knockdown in Vitro
This protocol outlines the steps for transient SOX9 knockdown in adherent cancer cell lines (e.g., HeLa, A549, PANC-1) using lipid-based transfection of siRNA, followed by functional validation.
Materials Required:
- Cells: Target cancer cell line (e.g., HeLa, ATCC CCL-2).
- SOX9 siRNA: Validated SOX9-specific siRNA and non-targeting control siRNA.
- Transfection Reagent: Lipofectamine RNAiMAX (Invitrogen, cat. no. 13778) or equivalent.
- Media: Appropriate cell culture medium and Opti-MEM Reduced Serum Medium.
- Assay Kits: RNA extraction kit, reverse transcription kit, SYBR Green qPCR master mix, MTT or CellTiter-Glo viability assay kit.
Procedure:
Day 1: Cell Seeding
- Harvest and count cells. Seed cells in a 6-well plate at a density of 1.5 x 10^5 cells per well in 2 mL of complete growth medium without antibiotics. Gently swirl the plate to ensure even distribution. Incubate the cells at 37°C with 5% CO₂ for 18-24 hours, until they are 60-70% confluent at the time of transfection.
Day 2: siRNA Transfection Complex Preparation
- For each transfection sample, prepare two sterile tubes:
- Tube A (siRNA Dilution): Dilute 20 pmol of SOX9 siRNA or control siRNA in 200 µL of Opti-MEM medium. Mix gently.
- Tube B (Reagent Dilution): Dilute 2 µL of Lipofectamine RNAiMAX in 200 µL of Opti-MEM medium. Mix gently and incubate for 5 minutes at room temperature.
- Combine the contents of Tube A and Tube B (total volume ~400 µL). Mix gently by inversion or slow pipetting. Do not vortex. Incubate the complex at room temperature for 20 minutes to allow lipid-siRNA nanoparticle formation.
- For each transfection sample, prepare two sterile tubes:
Day 2: Transfection
- Add the 400 µL of siRNA-lipid complex dropwise to each well containing the cells and 2 mL of medium. Gently rock the plate back and forth to ensure even distribution.
- Return the plate to the 37°C, 5% CO₂ incubator.
Day 4: Harvesting for Validation (48-72 hours post-transfection)
- mRNA Level Analysis (qRT-PCR):
- Extract total RNA from the transfected cells using an appropriate kit.
- Synthesize cDNA via reverse transcription.
- Perform qPCR using primers specific for SOX9 and a housekeeping gene (e.g., GAPDH). Calculate knockdown efficiency using the 2^(-ΔΔCt) method. Aim for >70% knockdown to proceed with functional assays.
- Protein Level Analysis (Western Blot):
- Lyse cells in RIPA buffer supplemented with protease inhibitors.
- Separate proteins by SDS-PAGE, transfer to a PVDF membrane, and immunoblot with anti-SOX9 antibody. Use an anti-GAPDH or anti-β-Actin antibody as a loading control.
- mRNA Level Analysis (qRT-PCR):
Day 4-6: Functional Assays
- Proliferation/Viability (MTT Assay):
- Seed siRNA-transfected cells in a 96-well plate at a low density.
- After 48-72 hours, add MTT reagent (0.5 mg/mL final concentration) and incubate for 3-4 hours at 37°C.
- Carefully remove the medium, dissolve the formed formazan crystals in DMSO, and measure the absorbance at 570 nm with a reference wavelength of 630 nm [27].
- Invasion/Migration (Boyden Chamber Assay):
- 48 hours post-transfection, seed serum-starved cells into the upper chamber of a Matrigel-coated (for invasion) or uncoated (for migration) insert in a 24-well plate. Add medium with 10% FBS to the lower chamber as a chemoattractant.
- After 24-48 hours of incubation, fix the cells that have traversed the membrane, stain with crystal violet, and count under a microscope.
- Proliferation/Viability (MTT Assay):
The Scientist's Toolkit: Key Reagents for SOX9 Research
Table 3: Essential Research Reagents for SOX9 Knockdown Studies
| Reagent / Assay | Function/Principle | Example Product / Citation |
|---|---|---|
| SOX9 siRNA | Induces sequence-specific degradation of SOX9 mRNA. | Dharmacon ON-TARGETplus SOX9 siRNA (M-021507-00) [27] |
| Lipofectamine RNAiMAX | Lipid-based transfection reagent for high-efficiency siRNA delivery into adherent cells. | Invitrogen, cat. no. 13778 [27] |
| Anti-SOX9 Antibody | Detects SOX9 protein levels via Western Blot or Immunohistochemistry. | Sigma-Aldrich, polyclonal rabbit anti-SOX9 (HPA001758) [27] |
| Aldefluor Assay | Measures ALDH enzymatic activity, a marker of cancer stem-like cells regulated by SOX9. | StemCell Technologies, kit #01700 [25] |
| MTT Cell Viability Assay | Colorimetric assay to measure cell proliferation and metabolic activity after SOX9 knockdown. | Sigma-Aldrich, M5655 [27] |
SOX9 operates as a master oncogenic regulator across a spectrum of cancers, integrally involved in metastasis, chemoresistance, and the maintenance of cancer stemness. The strategic knockdown of SOX9 presents a compelling and rational therapeutic approach, demonstrated by consistent in vitro and in vivo evidence showing profound suppression of malignant phenotypes. The provided application notes and detailed protocols for siRNA design, transfection, and functional validation offer a robust framework for researchers to implement and investigate SOX9-targeting strategies in their specific models. Future work should focus on translating these findings into clinically viable targeted therapies, potentially through the development of SOX9-specific small-molecule inhibitors or advanced RNAi delivery systems.
A Step-by-Step Protocol for Efficient SOX9 Knockdown in Macrophage Models
The selection of an appropriate macrophage model is a fundamental decision in immunology and cancer research, directly influencing the physiological relevance, reproducibility, and translational potential of experimental findings. Macrophages, phagocytic innate immune cells, maintain homeostasis by interacting with various tissues, modulating immunological responses, and secreting cytokines [30] [31]. In the specific context of tumor-associated macrophage (TAM) research, this choice becomes particularly critical when investigating molecular targets like SOX9, a transcription factor implicated in promoting tumor progression and immune escape [5] [4]. Researchers are typically faced with two principal pathways: primary human monocyte-derived macrophages (MDMs) or immortalized macrophage cell lines, each possessing distinct advantages, limitations, and technical considerations.
This application note provides a structured comparison of these model systems, with a specific focus on their application in studying SOX9 signaling in TAMs. We summarize key quantitative data in comparative tables, detail essential methodologies, and visualize core signaling pathways to support informed experimental design.
Model System Comparison
Primary Human Monocyte-Derived Macrophages (MDMs)
Origin and Definition: Primary MDMs are differentiated directly from CD14+ monocytes isolated from human peripheral blood mononuclear cells (PBMCs). They are not genetically altered or immortalized, which helps maintain biological activity and population characteristics that more closely resemble the in vivo state [30] [31]. PBMCs themselves constitute a mixed population, with monocytes typically comprising 10–30% of the total cells [31].
Advantages and Disadvantages: The primary advantage of using MDMs is their high physiological relevance. They exhibit considerable functional heterogeneity, closely mirroring the diversity found in native tissue macrophages, and are considered the gold standard for modeling human macrophage biology [30]. This is crucial for studying complex processes like polarization into M1 (pro-inflammatory) or M2 (immunosuppressive, pro-tumoral) phenotypes, a key aspect of TAM function [30] [5].
The most significant drawbacks are their limited proliferative capability and finite lifespan, preventing long-term subculture. Their isolation and culture are technically demanding, require a fresh supply of human blood products, and can be complicated by donor-to-donor variability, necessitating careful control of experimental conditions [30] [31].
Immortalized Macrophage Cell Lines
Origin and Definition: Immortalized cell lines, such as THP-1 and U-937, are stable, proliferative populations created through repeated subculturing, often from malignant sources or via genetic manipulation (e.g., viral transformation) to bypass senescence [30] [31].
Advantages and Disadvantages: The chief advantages of cell lines are their practicality. They offer rapid growth, ease of culture and passage, high stability, reproducibility, and independence from conditioned media or donor variability. This makes them ideal for large-scale screening studies, genetic manipulation, and experiments requiring large cell numbers [30] [32].
The major limitation is their reduced physiological fidelity. Created from malignant single cells or tumors, they often exhibit genotypic and phenotypic drift during long-term culture. Consequently, they may develop molecular phenotypes and functional properties (in polarization, cytokine secretion, and phagocytosis) that differ significantly from primary cells, potentially leading to misleading conclusions in disease modeling [30] [33]. For instance, one transcriptomic study demonstrated that the response of a J774 macrophage cell line to Mycobacterium tuberculosis infection was delayed and less intense compared to primary bone marrow-derived macrophages (BMDMs) [33].
Table 1: Quantitative Comparison of Macrophage Model Systems
| Feature | Primary Human MDMs | THP-1 Cell Line |
|---|---|---|
| Physiological Relevance | High, closely mimics in vivo state [30] | Reduced, exhibits phenotypic drift [30] [33] |
| Proliferation Capacity | Non-proliferative, terminally differentiated [30] | Unlimited, rapid growth [30] |
| Experimental Timeline | 5–7 days differentiation post-monocyte isolation [30] | 3–5 days differentiation from monocytic state [32] |
| Donor Variability | Present, reflects human genetic diversity | Minimal, homogenous population |
| Polarization Plasticity | Pronounced, high functional heterogeneity [30] | Retains plasticity but may have biased responses [30] |
| Cost & Technical Demand | High (donor recruitment, isolation) | Low (easy maintenance) |
| Ideal Use Case | Validation studies, disease modeling, translational research | High-throughput screens, mechanistic studies, genetic manipulation |
Application in SOX9 and TAM Research
The SOX9 Signaling Axis in TAMs
In the tumor microenvironment (TME), crosstalk between cancer cells and immune cells is critical. Research has shown that TAMs, which often display an M2-like phenotype, secrete transforming growth factor-beta (TGF-β) [5]. This cytokine increases SOX9 expression in cancer cells by upregulating the C-jun/SMAD3 pathway, thereby promoting epithelial-to-mesenchymal transition (EMT), tumor proliferation, migration, and invasion [5]. Furthermore, a feedback loop exists wherein cancer cells can promote M2 polarization of macrophages, increasing their secretion of TGF-β and IL-10 [5]. SOX9 knockdown in lung cancer cells has been shown to inhibit this TAM-mediated EMT and reduce tumor cell migration and invasion, highlighting its potential as a therapeutic target [5].
The following diagram illustrates this key signaling pathway in TAMs.
Selecting a Model for SOX9 Knockdown Studies
The choice between primary MDMs and cell lines for SOX9-focused TAM research depends heavily on the experimental goals.
Primary MDMs are superior for validation studies and investigating the human-specific pathophysiology of the TGF-β/SOX9 axis. Their authentic expression of receptors (e.g., TLRs, scavenger receptors) and secretory activity (e.g., IL-1β, lysozyme) ensures that findings on SOX9's role in macrophage polarization and its subsequent effect on tumor cells are physiologically relevant [30] [5]. This is paramount for preclinical therapeutic development.
THP-1 Cells are highly practical for initial mechanistic screening and genetic manipulation. Their ease of use makes them ideal for performing high-throughput SOX9 knockdown or knockout experiments to map its downstream targets and interactions in a human macrophage context [5] [32]. However, confirmatory studies in primary cells are strongly recommended.
Detailed Experimental Protocols
Protocol 1: Differentiation and SOX9 Knockdown in Primary Human MDMs
Workflow Overview:
Step-by-Step Procedure:
Isolation of CD14+ Monocytes:
- Collect heparinized blood from healthy donors with informed consent under ethical approval [34].
- Separate PBMCs via Ficoll-Paque Plus density gradient centrifugation.
- Isolate CD14+ monocytes from PBMCs using immunomagnetic anti-CD14-conjugated microbeads according to the manufacturer's protocol. Purity of 96–99% is typically achievable [34].
Differentiation into Macrophages:
- Plate the isolated CD14+ monocytes in culture plates at a density of (1.5 \times 10^6) cells/mL in RPMI-1640 medium supplemented with 10% Fetal Bovine Serum (FBS) and 1% antibiotic/antimycotic solution.
- Differentiate into macrophages by adding 100 ng/mL Granulocyte-Macrophage Colony-Stimulating Factor (GM-CSF) for M1-like or Macrophage Colony-Stimulating Factor (M-CSF) for M2-like bias. Incubate for 5–7 days [30] [34].
SOX9 Knockdown via Lentiviral Transduction:
- On day 5 of differentiation, transduce MDMs with lentiviral particles carrying shRNA targeting SOX9 or a non-targeting scrambled control. Use a suitable Multiplicity of Infection (MOI) and enhance transduction with polybrene (e.g., 8 µg/mL).
- After 24 hours, replace the virus-containing medium with fresh differentiation medium.
- Allow 48–72 hours for knockdown efficiency before proceeding to functional assays. Validate knockdown via qRT-PCR and Western Blot [5] [35].
Protocol 2: Differentiation and NFκB Profiling in THP-1 Reporter Cells
Workflow Overview:
Step-by-Step Procedure:
Cell Culture and Differentiation:
- Maintain THP-1 monocytes in suspension in RPMI-1640 medium with 10% FBS.
- To differentiate into macrophage-like cells, plate THP-1 cells and treat with 50–100 ng/mL Phorbol 12-myristate 13-acetate (PMA) for 48 hours [32].
- After differentiation, wash cells and rest in fresh medium without PMA for at least 24 hours before experiments.
Using NFκB Reporter Assays for Functional Readout:
- THP-1 NFκB reporter cells, transduced with a firefly luciferase gene under the control of an NFκB response element, can be used to monitor macrophage activation in real-time [32].
- Differentiate THP-1 NFκB FLuc cells as described above.
- Co-culture differentiated THP-1 macrophages with cancer cells (e.g., at a 1:1 ratio) or treat with TAM-conditioned medium in the presence of D-luciferin.
- Measure bioluminescence kinetically over several days using a spectrophotometer. Features like Area Under the Curve (AUC) and peak timing can be extracted to characterize the NFκB activation profile induced by tumor signals [32].
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for Macrophage and SOX9 Research
| Reagent/Catalog | Function/Application | Example Usage in Protocol |
|---|---|---|
| Immunomagnetic CD14+ Microbeads | Positive selection of monocytes from human PBMCs | Isolation of primary human monocytes for MDM differentiation [34]. |
| Recombinant Human M-CSF/GM-CSF | Drives differentiation of monocytes into macrophages | Added to culture medium for 5–7 days to generate primary MDMs [30] [34]. |
| Phorbol 12-Myristate 13-Acetate (PMA) | Protein kinase C activator; induces differentiation of THP-1 cells | Used at 50-100 ng/mL for 48 hours to differentiate THP-1 monocytes into adherent macrophages [32]. |
| shSOX9 Lentiviral Particles | Knocks down SOX9 expression in target cells | Used to transduce macrophages to study the functional role of SOX9 in TAMs [5] [35]. |
| Recombinant TGF-β | Key cytokine for inducing M2 polarization and studying SOX9 upregulation | Used to treat cancer cells or macrophages to activate the TGF-β/SOX9 axis in vitro [5]. |
| D-Luciferin | Substrate for firefly luciferase enzyme | Added to culture medium of THP-1 NFκB FLuc reporter cells to measure NFκB activity via bioluminescence [32]. |
The decision to use primary human monocyte-derived macrophages or an immortalized cell line like THP-1 is not a matter of identifying a universally superior option, but rather of aligning the model system with the specific research question. For research focused on the SOX9 pathway in TAMs, primary MDMs offer unparalleled physiological fidelity for validating findings, while THP-1 cells provide a robust and scalable platform for initial mechanistic and high-throughput studies. A strategic approach often involves using cell lines for discovery and primary cells for validation, thereby balancing practical constraints with the imperative for biologically relevant insights.
Inducing M2-Polarization to Mimic the TAM Phenotype
Tumor-associated macrophages (TAMs) are a major component of the tumor immune microenvironment and predominantly exhibit an M2-like, pro-tumoral phenotype [36] [37]. These cells are pivotal in promoting tumor progression, angiogenesis, metastasis, and immunosuppression [38] [37]. For research aimed at understanding TAM biology and developing therapeutic strategies, such as investigating the impact of SOX9 knockdown, reliably generating macrophage cultures that mimic the TAM phenotype in vitro is an essential first step. This application note provides detailed protocols for polarizing primary macrophages toward an M2 state, which serves as a representative model for TAMs, and outlines subsequent experimental workflows for functional analysis.
Principles of Macrophage Polarization
Macrophages are highly plastic cells whose activation state is dictated by signals in their local microenvironment. The classical M1/M2 dichotomy represents two extremes of this activation spectrum [38].
- M1 Macrophages (Anti-tumor): Induced by IFN-γ and bacterial products like LPS [39] [40]. They are characterized by high production of pro-inflammatory cytokines (e.g., IL-12, IL-23, TNF-α) and express high levels of iNOS, contributing to pathogen killing and anti-tumor immunity [36] [40].
- M2 Macrophages (Pro-tumor/TAM-like): Induced by Th2 cytokines such as IL-4 and IL-13 [39] [40]. They express markers like CD206, CD163, and Arg-1, and produce anti-inflammatory cytokines (e.g., IL-10, TGF-β) that facilitate tissue repair, angiogenesis, and tumor progression [39] [41]. This M2 phenotype closely resembles the majority of TAMs found in solid tumors [37].
It is critical to note that the in vivo TAM population is a complex and heterogeneous mix of cells that may co-express both M1 and M2 genes and do not rigidly conform to this binary classification [40] [41]. However, polarization with IL-4 and IL-13 remains a standard and validated method to generate macrophages with key functional and phenotypic properties of pro-tumoral TAMs for in vitro study.
Key Signaling Pathways in M2 Polarization
The following diagram illustrates the core signaling pathways involved in driving macrophage polarization towards the M2 phenotype.
Experimental Protocols
Protocol 1: Generation and M2 Polarization of Bone Marrow-Derived Macrophages (BMDMs)
This protocol describes the isolation and differentiation of macrophages from mouse bone marrow, followed by polarization to an M2 phenotype [42].
Materials and Reagents
- Mice: 8-12 week old female BALB/c or C57BL/6 mice.
- L929 Cell Conditioned Medium (LCCM): Serves as a source of Macrophage Colony-Stimulating Factor (M-CSF). Culture L929 cells for 7 days, collect supernatant, clarify by centrifugation, and store at -20°C [42].
- Culture Medium: RPMI-1640 supplemented with 10% Fetal Bovine Serum (FBS), 1% Penicillin/Streptomycin (P/S), and 2 mM L-glutamine.
- Complete BMDM Medium: Culture Medium + 30% LCCM [42].
- Polarization Cytokines: Recombinant murine IL-4 (20 ng/mL) and IL-13 (20 ng/mL).
- Sterile PBS, Cell dissociation buffer/enzyme.
Step-by-Step Procedure
- Euthanize the mouse according to institutional ethical guidelines.
- Isolate Bone Marrow: Aseptically remove femurs and tibias. Flush the bone marrow cavities with cold, sterile PBS using a syringe and 25G needle. Create a single-cell suspension by passing through a 70 µm cell strainer.
- Differentiate BMDMs: Seed the bone marrow cells in culture dishes with Complete BMDM Medium. Incubate at 37°C in a 5% CO₂ humidified incubator for 7 days, refreshing the medium on day 3.
- Harvest BMDMs: On day 7, wash adherent cells with PBS and detach using a cell scraper or gentle enzymatic treatment. Seed the mature BMDMs for subsequent experiments.
- M2 Polarization: Treat the BMDMs with Culture Medium containing IL-4 (20 ng/mL) and IL-13 (20 ng/mL) for 24-48 hours to induce M2 polarization.
- Validation: Proceed to Section 4.0 to validate polarization success before initiating functional assays.
Protocol 2: SOX9 Knockdown in M2-Polarized Macrophages
This protocol is designed to be integrated into the workflow following successful M2 polarization (Step 5 of Protocol 1.1.2) to investigate the role of SOX9 in TAM function [5].
Materials and Reagents
- SOX9-specific siRNA or non-targeting scrambled siRNA control.
- Transfection reagent compatible with primary macrophages.
- Opti-MEM or similar serum-free reduced medium.
Step-by-Step Procedure
- Seed Cells: Seed M2-polarized BMDMs in an appropriate multi-well plate to achieve 60-80% confluency at the time of transfection.
- Prepare Transfection Complexes:
- Dilute the required amount of SOX9 siRNA or scrambled control in Opti-MEM.
- Dilute the transfection reagent in a separate tube of Opti-MEM.
- Incubate for 5 minutes at room temperature.
- Combine the diluted siRNA with the diluted transfection reagent. Mix gently and incubate for 20 minutes to allow complex formation.
- Transfect Cells: Add the transfection complexes dropwise to the cells. Gently swirl the plate to ensure even distribution.
- Incubate: Incubate the cells for 6-24 hours, then replace the transfection medium with fresh Culture Medium (with or without IL-4/IL-13 to maintain polarization).
- Validate Knockdown: After 48-72 hours, harvest cells and analyze SOX9 knockdown efficiency via qRT-PCR and/or Western Blot.
The overall experimental workflow, integrating both polarization and genetic manipulation, is outlined below.
Phenotypic and Functional Validation of M2-TAMs
After polarization and/or SOX9 knockdown, it is essential to confirm the macrophage phenotype using a combination of techniques. The table below summarizes key validation methods and the expected outcomes for successfully polarized M2-TAMs.
Table 1: Validation Strategies for M2-Polarized TAMs
| Method | Target/Analyte | M2/TAM Signature | Technical Notes |
|---|---|---|---|
| Flow Cytometry | Surface: CD206, CD163 [38] [41] | Increased expression | Standard for protein-level detection; allows quantification of heterogeneous populations. |
| qRT-PCR | mRNA: Arg1, Ym1, Fizz1 [38] | Increased expression | Sensitive method for transcriptional profiling. |
| Western Blot / ELISA | Cytokines: IL-10, TGF-β [39] [40] | Increased secretion/production | Confirms functional protein output. |
| Immunofluorescence | Surface/Intracellular: CD206, CD163 [38] | Increased expression | Provides spatial distribution and visualization in cultured cells. |
| Functional Assay | Phagocytosis, Co-culture | Altered tumor cell interaction | Assesses downstream biological effect. |
The Scientist's Toolkit: Essential Research Reagents
The following table catalogues critical reagents required for the protocols described in this note.
Table 2: Key Research Reagent Solutions for TAM Polarization and Analysis
| Reagent / Tool | Function / Purpose | Example Application in Protocol |
|---|---|---|
| Recombinant Murine M-CSF | Differentiation and survival of macrophages from bone marrow precursors. | Generated in-house via L929 cell-conditioned medium or purchased commercially [42]. |
| Recombinant Murine IL-4 & IL-13 | Key polarizing cytokines for inducing the M2-like TAM phenotype. | Used at 20 ng/mL each to treat BMDMs for 24-48 hours [39] [40]. |
| SOX9-specific siRNA | Genetic knockdown to investigate the role of SOX9 in TAM function. | Transfected into M2-polarized BMDMs to study effects on phenotype and tumor-promoting functions [5]. |
| Anti-CD206 & Anti-CD163 Antibodies | Primary biomarkers for identifying M2-polarized macrophages via flow cytometry or IF. | Used for validation of successful M2 polarization (See Table 1) [38] [41]. |
| TGF-β & IL-10 ELISA Kits | Quantification of characteristic M2/TAM-secreted anti-inflammatory cytokines. | Used in supernatant collection to functionally validate M2 polarization (See Table 1) [39] [37]. |
Troubleshooting and Technical Notes
- Polarization Efficiency: If M2 marker expression is low, confirm cytokine activity and titrate concentrations (e.g., test 10-50 ng/mL for IL-4/IL-13). Ensure cells are healthy and not over-confluent during polarization.
- SOX9 Knockdown Validation: Always include a non-targeting siRNA control. Optimize transfection conditions for primary macrophages, as they can be resistant to standard transfection methods. Lipofection or electroporation are common approaches.
- Defining TAMs: Remember that in vitro M2 polarization is a model. Where possible, correlate findings with macrophages isolated from tumor samples or more complex co-culture systems.
- Metabolic Profiling: Consider integrating mass spectrometry-based metabolomics to gain deeper insights, as M2 macrophages rely heavily on oxidative phosphorylation and fatty acid oxidation, distinct from the glycolytic profile of M1 cells [36].
SOX9 (SRY-related high-mobility group box gene 9) is a transcription factor that plays a critical role in multiple biological processes, including cell differentiation, proliferation, and reprogramming [43] [4]. In the context of cancer and the tumor microenvironment, SOX9 has emerged as a significant regulator of tumor progression and immune modulation. Research has demonstrated that SOX9 is frequently overexpressed in various solid malignancies, where its expression levels positively correlate with tumor occurrence and progression [4]. In the specific context of tumor-associated macrophages (TAMs), studies have revealed a positive correlation between TAM density and SOX9 expression in non-small cell lung cancer (NSCLC) tissues [5]. TAMs secrete TGF-β, which increases SOX9 expression and promotes epithelial-to-mesenchymal transition (EMT) in lung cancer cells, thereby driving tumor proliferation, migration, and invasion [5]. This TGF-β-mediated EMT has been shown to be SOX9-dependent, establishing SOX9 as a promising therapeutic target in tumor microenvironment research [5].
The functional significance of SOX9 extends beyond epithelial tumor cells to the immune compartment within tumors. SOX9 plays a complex dual role in immunology, acting as a "double-edged sword" [4]. On one hand, it promotes immune escape by impairing immune cell function, making it a potential therapeutic target in cancer. On the other hand, SOX9 helps maintain macrophage function and contributes to tissue regeneration and repair [4]. This dual functionality necessitates precise experimental approaches for studying SOX9 function in specific cellular contexts, particularly in TAMs where its modulation could significantly impact tumor progression.
SOX9 Biology and Significance in TAMs
Molecular Structure and Functional Domains
SOX9 encodes a 509 amino acid polypeptide containing several functionally critical domains [4]. These domains are organized from N- to C-terminus as follows:
- Dimerization domain (DIM): Facilitates protein-protein interactions
- High Mobility Group (HMG) box domain: Responsible for DNA binding and nuclear localization
- Central transcriptional activation domain (TAM): Works synergistically with TAC
- C-terminal transcriptional activation domain (TAC): Interacts with cofactors to enhance transcriptional activity
- Proline/glutamine/alanine (PQA)-rich domain: Essential for transcriptional activation
The HMG domain enables sequence-specific DNA binding, while the transcriptional activation domains (TAM and TAC) mediate interactions with various transcriptional co-regulators, allowing SOX9 to control diverse genetic programs in different cellular contexts [4].
SOX9 in Tumor-Associated Macrophages and Immune Evasion
In the tumor microenvironment, SOX9 expression in cancer cells is influenced by TAMs through paracrine signaling. Research has demonstrated that TAMs secrete TGF-β, which increases SOX9 expression in tumor cells [5]. This TAM-driven SOX9 upregulation promotes several pro-tumorigenic processes:
- Epithelial-to-mesenchymal transition (EMT): SOX9 knockdown inhibits TGF-β-mediated EMT, indicating that this process is SOX9-dependent [5]
- Immune suppression: SOX9 suppresses immune cell infiltration and functionally inhibits tumor-associated CD8+ T cells, natural killer cells, and dendritic cells [44]
- Matrix remodeling: SOX9 significantly elevates collagen-related gene expression and increases collagen fibers, potentially creating a physical barrier to immune cell infiltration [44]
The relationship between TAMs and SOX9 creates a feed-forward loop wherein TAMs promote SOX9 expression in tumor cells, and SOX9 in turn modifies the tumor microenvironment to further support immunosuppressive characteristics [5] [44].
Table 1: Key Evidence Supporting SOX9 as a Therapeutic Target in Tumor Microenvironment
| Evidence Type | Finding | Experimental System | Citation |
|---|---|---|---|
| Clinical correlation | High TAM density correlates with SOX9+ staining in lung cancer cells | Human NSCLC tissues | [5] |
| Functional mechanism | TGF-β secreted by TAMs increases SOX9 expression via C-jun/SMAD3 pathway | In vitro co-culture systems | [5] |
| Therapeutic validation | SOX9 knockdown inhibited EMT and reduced tumor cell migration and invasion | A549 and H1299 lung cancer cells | [5] |
| Immune modulation | SOX9 suppresses immune cell infiltration and increases collagen fibers | KrasG12D mouse LUAD model | [44] |
| Prognostic significance | Co-expression of CD163 (TAM marker) and SOX9 correlated with worse patient outcomes | 164 lung cancer patients | [5] |
siRNA Design and Selection for SOX9 Knockdown
Principles of Effective siRNA Design
Small interfering RNA (siRNA) is a class of short, double-stranded RNA molecules, typically consisting of 21 to 23 nucleotides in length [45]. siRNA induces gene silencing through the RNA-induced silencing complex (RISC) by perfectly pairing with target mRNA, guiding its cleavage, and ultimately leading to mRNA degradation [45] [46]. For successful SOX9 knockdown, careful attention to siRNA design principles is essential:
Sequence Selection Criteria: Optimal siRNA sequences should maximize target specificity and knockdown efficiency while minimizing off-target effects. Based on established parameters from companies like Alnylam, effective siRNAs generally exhibit these characteristics [47]:
- The first position at 5′ is usually a GC base
- The 13th and 14th positions in 5' are usually not G
- There are 3 or more U and A bases in the seed sequence (positions 2-8 of the guide strand)
Computational Validation: Advanced computational approaches, including molecular dynamics simulations and structural docking against Argonaute 2 (the catalytic engine of RISC), can predict silencing efficacy and reduce off-target potential [45]. These methods assess thermodynamic stability, secondary structure, and precise conformational fit within the RISC complex.
SOX9-Specific siRNA Design Considerations
When designing siRNAs specifically targeting SOX9, researchers should consider:
- Isoform specificity: Ensure siRNA sequences target all relevant SOX9 transcript variants
- Conserved regions: Focus on sequences with high conservation across relevant species if translational research is planned
- Accessibility: Target regions with minimal secondary structure to enhance binding efficiency
- Off-target minimization: Perform BLAST analysis against the transcriptome to ensure specificity for SOX9
Table 2: Recommended siRNA Sequences for SOX9 Knockdown
| Target Region | Sequence (5' to 3') | GC Content | Predicted Efficiency | Validation Status |
|---|---|---|---|---|
| SOX9 CDS 1 | Custom design required | ~40-55% | High | See protocol section |
| SOX9 CDS 2 | Custom design required | ~40-55% | Medium-High | See protocol section |
| SOX9 3'UTR | Custom design required | ~40-55% | Medium | See protocol section |
Note: Specific nucleotide sequences should be designed using current bioinformatic tools and validated experimentally. The parameters above serve as guidelines for selection.
siRNA Delivery Methods for Macrophage Systems
Delivery Challenges and Strategies
Efficient siRNA delivery to target cells remains a significant challenge in RNAi therapeutics. siRNAs are inherently unstable in serum and susceptible to degradation by nucleases. Additionally, their negative charge and hydrophilicity limit cellular uptake [45] [46]. For macrophage-targeted delivery, several strategies can be employed:
Lipid-Based Nanoparticles (LNPs): LNP systems typically consist of four components: cationic lipids, cholesterol, auxiliary lipids, and PEG-lipids [47]. These formulations protect siRNA from nuclease degradation, enhance cellular uptake, and promote endosomal escape. The LNP composition can be tuned to preferentially target macrophage populations.
GalNAc Conjugation: N-acetylgalactosamine (GalNAc) is a ligand for the asialoglycoprotein receptor (ASGPR), which is highly expressed on hepatocytes but has limited expression on macrophages [46] [47]. While primarily used for liver targeting, modified GalNAc approaches may have applications in specific macrophage subsets.
Non-Cationic Delivery Systems: To mitigate the cytotoxicity associated with cationic carriers, non-cationic systems including polymeric nanoparticles, gold nanoparticles, and biomimetic vectors offer enhanced biocompatibility [46]. These systems utilize alternative siRNA loading strategies through chemical bonding, hydrogen bonding, hydrophobic interactions, or physical cross-linking.
Experimental Delivery Workflow for TAM Studies
The following diagram illustrates the complete experimental workflow for SOX9 siRNA delivery in TAM studies:
Step-by-Step Experimental Protocol
Pre-Experimental Setup
Materials and Reagents:
- SOX9-specific siRNA and scrambled control siRNA
- Transfection reagent (lipofection-based or polymer-based)
- Cell culture medium appropriate for macrophage cells
- Serum-free Opti-MEM reduced serum medium
- Phosphate-buffered saline (PBS)
- Macrophage colony-stimulating factor (M-CSF) for human macrophage differentiation
- IL-4 and IL-13 for M2 polarization
Equipment:
- Tissue culture hood (Class II biological safety cabinet)
- CO2 incubator (37°C, 5% CO2)
- Inverted phase-contrast microscope
- Centrifuge
- Vortex mixer
- Water bath (37°C)
- Cell counter or hemocytometer
siRNA Transfection Protocol
Day 1: Cell Seeding
- Differentiate monocytes to macrophages using M-CSF (50 ng/mL) for 6-7 days
- Polarize macrophages to M2 phenotype using IL-4 (20 ng/mL) and IL-13 (20 ng/mL) for 48 hours
- Harvest macrophages and seed in appropriate multi-well plates at 60-70% confluence
- Incubate cells overnight at 37°C in a CO2 incubator
Day 2: Transfection Complex Preparation
- Dilute SOX9 siRNA in serum-free medium to a concentration of 20-50 nM in a sterile tube
- In a separate tube, dilute transfection reagent in serum-free medium
- Incubate both solutions for 5 minutes at room temperature
- Combine the diluted siRNA with the diluted transfection reagent
- Mix gently and incubate for 20-30 minutes at room temperature to allow complex formation
Day 2: Transfection
- Remove culture medium from cells and wash once with PBS
- Add the siRNA-transfection complex mixture to cells dropwise while gently swirling the plate
- Incubate cells at 37°C in a CO2 incubator for 6-8 hours
- Replace transfection medium with fresh complete medium
- Continue incubation for 24-72 hours depending on downstream applications
Optimization and Troubleshooting
Critical Parameters for Optimization:
- siRNA concentration: Test a range of 10-100 nM to determine optimal concentration
- Cell density: 60-80% confluence typically yields best results
- Transfection reagent to siRNA ratio: Follow manufacturer recommendations but test ±20%
- Incubation time: 6-8 hours is standard, but can be adjusted based on cytotoxicity
Common Issues and Solutions:
- Low transfection efficiency: Optimize cell density, increase transfection reagent concentration, or try alternative transfection reagents
- High cytotoxicity: Reduce transfection reagent amount, shorten transfection incubation time, or use lower siRNA concentrations
- Inconsistent results: Ensure consistent cell passage number, maintain sterile technique, and prepare fresh solutions
Validation and Functional Assessment
Knockdown Efficiency Validation
mRNA Level Analysis (qRT-PCR):
- Extract total RNA 24-48 hours post-transfection using appropriate RNA isolation kits
- Synthesize cDNA using reverse transcriptase
- Perform quantitative PCR with SOX9-specific primers
- Normalize SOX9 expression to housekeeping genes (GAPDH, β-actin)
- Calculate knockdown efficiency relative to scrambled control
Protein Level Analysis (Western Blot):
- Harvest cells 48-72 hours post-transfection for protein extraction
- Separate proteins by SDS-PAGE and transfer to PVDF membrane
- Probe with anti-SOX9 antibody and appropriate secondary antibody
- Detect using chemiluminescence and quantify band intensity
- Normalize to loading control (β-actin, GAPDH)
Functional Assays in TAM Models
Migration and Invasion Assays:
- Perform Transwell migration and invasion assays using appropriate matrices
- Count migrated cells after 12-24 hours incubation
- Compare migration/invasion capacity between SOX9-knockdown and control macrophages
Cytokine Secretion Profiling:
- Collect conditioned media from transfected macrophages
- Analyze cytokine secretion using ELISA or multiplex assays
- Focus on TAM-relevant cytokines: TGF-β, IL-10, CCL17, CCL22
Co-culture Systems with Cancer Cells:
- Establish direct or indirect co-culture systems with relevant cancer cell lines
- Assess cancer cell proliferation, migration, and invasion
- Evaluate stemness markers in cancer cells after co-culture with SOX9-knockdown TAMs
Table 3: Expected Outcomes from SOX9 Knockdown in TAMs
| Functional Assay | Expected Result with SOX9 Knockdown | Biological Significance |
|---|---|---|
| Migration assay | Reduced macrophage migration | Impaired recruitment to tumor sites |
| Invasion assay | Decreased invasive capacity | Limited tissue infiltration |
| Cytokine profiling | Reduced TGF-β secretion | Disrupted pro-tumorigenic signaling |
| Co-culture with cancer cells | Decreased cancer cell proliferation | Reduced tumor-promoting function |
| EMT marker analysis | Increased E-cadherin, decreased vimentin | Inhibition of EMT in cancer cells |
The Scientist's Toolkit
Table 4: Essential Research Reagents for SOX9 Knockdown Studies
| Reagent Category | Specific Product/Type | Function/Application | Key Considerations |
|---|---|---|---|
| SOX9 siRNA | Custom-designed sequences | Target gene knockdown | Validate specificity and efficiency |
| Control siRNA | Scrambled sequence | Negative control | Ensure no sequence similarity to known genes |
| Transfection reagent | Lipofectamine RNAiMAX, DharmaFECT | siRNA delivery | Optimize for macrophage cell types |
| Macrophage markers | CD68, CD163, CD206 | Cell identification and sorting | Confirm polarization status |
| Polarization cytokines | M-CSF, IL-4, IL-13 | M2 macrophage differentiation | Standardize concentration and timing |
| SOX9 antibodies | Anti-SOX9 for Western blot, IHC | Knockdown validation | Verify specificity for SOX9 isoforms |
| Cell culture media | RPMI-1640, DMEM | Macrophage maintenance | Include appropriate supplements |
| RNA isolation kit | TRIzol, column-based kits | RNA extraction for qPCR | Ensure RNA integrity and purity |
| qPCR reagents | SYBR Green master mix, primers | Knockdown efficiency assessment | Design primers spanning exon junctions |
| Functional assay kits | Transwell plates, ECM matrices | Migration/invasion assessment | Optimize for macrophage characteristics |
Pathway Mapping and Mechanism
The molecular pathway below illustrates how SOX9 knockdown in TAMs influences the tumor microenvironment:
This application note provides a comprehensive framework for implementing transient SOX9 suppression in tumor-associated macrophages using siRNA transfection. The protocols outlined enable researchers to probe SOX9 function in TAMs and evaluate its role in modulating the tumor microenvironment. Successful SOX9 knockdown in TAMs is expected to disrupt key pro-tumorigenic pathways, particularly those mediated through TGF-β signaling and STAT3 activation [43] [5].
The experimental strategies described here can be integrated into broader research programs investigating SOX9 as a therapeutic target in cancer. The transient nature of siRNA-mediated knockdown allows for flexible experimental designs and assessment of acute SOX9 depletion effects. For translational applications, the insights gained from these studies could inform the development of RNAi-based therapeutics targeting the SOX9 pathway in tumor microenvironments [48] [46].
As RNAi technologies continue to advance, with improvements in delivery systems, chemical modifications, and targeting specificity, the approaches outlined in this protocol will likely evolve accordingly. Researchers should stay abreast of developments in nanoparticle design, particularly those enabling cell-type-specific delivery to macrophage populations in vivo, to translate these in vitro findings into preclinical and ultimately clinical applications.
The transcription factor SOX9 (SRY-related high mobility group box 9) plays a critical role in tumor progression and metastasis, particularly in non-small cell lung cancer (NSCLC) where its expression is associated with poor patient prognosis [5]. Research has demonstrated that tumor-associated macrophages (TAMs) promote tumor metastasis via the TGF-β/SOX9 axis, where TAM-secreted TGF-β increases SOX9 expression and promotes epithelial-to-mesenchymal transition (EMT) in lung cancer cells [5] [49]. CRISPR/Cas9 technology provides a powerful approach for generating stable SOX9 knockout cell lines to investigate this pathway and develop potential therapeutic strategies. This application note details a optimized protocol for achieving efficient and stable SOX9 knockout using CRISPR/Cas9, specifically designed for research applications in cancer biology and drug development.
Research Reagent Solutions
The following table summarizes key reagents commercially available for SOX9 CRISPR/Cas9 experiments:
Table 1: Commercial CRISPR/Cas9 Reagents for SOX9 Manipulation
| Product Name | Catalog Number | Key Features | Application |
|---|---|---|---|
| Sox9 CRISPR/Cas9 KO Plasmid (h2) | sc-400143-KO-2 | Pool of 3 plasmids with Cas9 + SOX9-specific gRNAs; transfection-ready | Initial knockout screening |
| Sox9 HDR Plasmid (h2) | sc-400143-HDR-2 | Homology-directed repair template with puromycin-RFP cassette | Selection of stable knockout cells |
| Sox9 Double Nickase Plasmid (h) | sc-400143-NIC | D10A mutated Cas9 for enhanced specificity | Reduced off-target effects |
| Sox9 CRISPR Activation Plasmid (h) | sc-400143-ACT | Synergistic activation mediator (SAM) system | SOX9 overexpression studies |
| Sox9 Lentiviral Activation Particles (h) | sc-400143-LAC | High-titer lentiviral particles | Hard-to-transfect cells |
For researchers requiring complete gene deletion rather than indel mutations, the SUCCESS (Single-strand oligodeoxynucleotides, Universal Cassette, and CRISPR/Cas9 produce Easy Simple knock-out System) method provides an alternative approach. This system utilizes two pX330 plasmids encoding Cas9 and gRNA, two 80mer single strand oligodeoxynucleotides (ssODN), and a blunt-ended universal selection maker sequence to remove large genomic regions of the target gene without constructing targeting vectors [50].
Experimental Design and Workflow
gRNA Design and Validation
Effective SOX9 targeting requires careful gRNA selection and validation. The gRNA sequences in commercial plasmids are derived from the GeCKO (v2) library and are designed for maximum knockout efficiency [51]. For custom designs, follow these principles:
- Target exons encoding critical functional domains
- Verify specificity using CRISPR design tools (e.g., CRISPOR, ChopChop)
- Select gRNAs with minimal off-target potential
- Design two gRNAs for large deletions when appropriate
gRNA efficiency can be validated using surrogate reporter systems such as the LacI-reporter, which quantifies cleavage efficiency by measuring luciferase or EGFP expression upon successful CRISPR-Cas9 cleavage [52]. This system demonstrates strong correlation between measured cleavage efficiency and actual mutation frequency detected by surveyor assays and deep sequencing.
Strategic Approach for Stable Knockout
The complete workflow for generating stable SOX9 knockout cells involves multiple critical steps as illustrated below:
Detailed Experimental Protocols
Cell Transfection and Selection
Materials:
- SOX9 CRISPR/Cas9 KO Plasmid (h2) (Santa Cruz Biotechnology, sc-400143-KO-2)
- SOX9 HDR Plasmid (h2) (Santa Cruz Biotechnology, sc-400143-HDR-2)
- Appropriate cell line (e.g., A549 or H1299 for NSCLC studies)
- Transfection reagent (e.g., Lipofectamine 3000)
- Cell culture media and supplements
- Puromycin (for selection) and blasticidin S (for activation systems)
Procedure:
- Seed cells in 12-well plates at 2.5×10⁵ cells per well one day before transfection [52]
- Co-transfect with SOX9 CRISPR/Cas9 KO Plasmid and SOX9 HDR Plasmid at 1:1 mass ratio
- For lentiviral transduction, use 200 μl of transduction-ready particles (sc-400143-LAC) per well
- 48 hours post-transfection, begin selection with appropriate antibiotic:
- Puromycin: 0.75-5 μg/mL (concentration depends on cell line)
- Blasticidin S: 5-100 μg/mL (for activation systems)
- Hygromycin: 400 μg/mL (alternative selection)
- Maintain selection for 5-7 days, replacing antibiotic-containing media every 2-3 days
- Isolate single-cell clones by limiting dilution or colony picking
Table 2: Antibiotic Selection Parameters for Different CRISPR Systems
| CRISPR System | Selection Marker | Effective Concentration Range | Selection Duration |
|---|---|---|---|
| KO Plasmid + HDR | Puromycin-RFP | 0.75-5 μg/mL | 5-7 days |
| Double Nickase | Puromycin-GFP | 0.75-5 μg/mL | 5-7 days |
| Activation System | Blasticidin, Hygromycin, Puromycin | 5-100 μg/mL blasticidin S | 5-7 days |
| SUCCESS Method | Blasticidin S | 100 μg/mL | 5 days [50] |
Validation of SOX9 Knockout
Molecular Validation:
- Genomic DNA Analysis: Extract genomic DNA from putative knockout clones
- PCR Amplification: Amplify target regions using primers flanking the CRISPR cut sites
- Sequence Verification: Confirm indels via Sanger sequencing or next-generation sequencing
- Surveyor Assay: Detect mutation efficiency in mixed populations [52]
Protein Validation:
- Western Blotting: Confirm SOX9 knockdown using Sox9 Antibody (E-9): sc-166505 [51]
- Immunofluorescence: Visualize SOX9 expression and cellular localization
- Functional Assays: Assess EMT markers (E-cadherin, vimentin) to confirm functional knockout [5]
Troubleshooting and Optimization
Enhancing Knockout Efficiency
Research indicates that several factors significantly impact CRISPR knockout efficiency:
- Antibiotic Concentration: High antibiotic doses (e.g., 100 μg/mL blasticidin S) dramatically improve homozygotic knock-in efficiency compared to lower doses [50]
- DNA End Configuration: Blunt-ended cassettes show superior correct ligation efficiency compared to sticky ends [50]
- ssODN Design: 80mer single strand oligodeoxynucleotides significantly enhance proper cassette integration [50]
- Homology Arms: Incorporating 250 bp homology arms increases knock-in efficiency by facilitating homologous recombination [50]
Addressing Technical Challenges
- Low Transfection Efficiency: Use lentiviral particles (sc-400143-LAC) for hard-to-transfect cells [51]
- Incomplete Knockout: Employ double nickase plasmids (sc-400143-NIC) for enhanced specificity [51]
- Off-target Effects: Validate with multiple gRNAs and use computational prediction tools
- Selection Issues: Titrate antibiotics for each cell line and use appropriate controls
Application in Tumor-Associated Macrophage Research
The TGF-β/SOX9 axis represents a critical mechanism in tumor microenvironment signaling. Research has demonstrated that TAMs secrete TGF-β, which increases SOX9 expression and promotes EMT in lung cancer cells [5]. The molecular mechanism of this pathway can be visualized as follows:
CRISPR-mediated SOX9 knockout provides a powerful tool for investigating this pathway, as SOX9 knockdown has been shown to inhibit TGF-β-mediated EMT, indicating that this process is SOX9-dependent [5]. Utilizing the protocols described herein, researchers can generate stable SOX9 knockout cell lines to study:
- TAM-tumor cell interactions in co-culture systems
- EMT marker expression (E-cadherin loss, vimentin gain)
- Tumor cell migration and invasion capabilities
- Potential therapeutic targets within the TGF-β/SOX9 axis
Table 3: Key Experimental Findings Supporting the TGF-β/SOX9 Axis in NSCLC
| Experimental Approach | Key Finding | Significance |
|---|---|---|
| Clinical sample analysis | High TAM density correlates with SOX9 expression | Prognostic value in NSCLC patients |
| Co-culture experiments | Macrophages promote SOX9 expression and EMT | Direct evidence of TAM-tumor cell crosstalk |
| TGF-β treatment studies | TGF-β increases SOX9 via C-jun/SMAD3 pathway | Mechanism of SOX9 regulation |
| SOX9 knockdown | Inhibits TGF-β-mediated EMT | Establishes SOX9 dependence |
| Survival analysis | Co-expression of CD163+ TAMs and SOX9 predicts poor outcome | Clinical relevance |
CRISPR/Cas9-mediated SOX9 knockout represents a robust method for investigating the role of SOX9 in cancer biology and TAM-tumor cell interactions. The protocols outlined in this application note provide a comprehensive framework for generating stable SOX9 knockout cell lines, with specific utility for studying the TGF-β/SOX9 axis in NSCLC. Through proper gRNA design, optimized transfection and selection parameters, and thorough validation, researchers can effectively utilize this approach to advance understanding of tumor metastasis and identify novel therapeutic targets.
Verifying the efficiency of gene knockdown is a critical step in functional genomics research, particularly in complex biological systems like the tumor microenvironment. This document provides detailed application notes and protocols for confirming SOX9 knockdown efficiency in studies focused on tumor-associated macrophages (TAMs). We outline a rigorous methodology combining quantitative real-time PCR (qRT-PCR) for transcriptional assessment and Western blot (WB) for protein-level validation, emphasizing the technical considerations essential for generating reliable, publication-quality data in the context of macrophage biology and cancer research.
The critical importance of this verification step is highlighted by the frequent discrepancies observed between mRNA and protein measurements. These inconsistencies often arise from biological factors including temporal expression delays, translational regulation, and post-translational modifications, as well as technical pitfalls in experimental execution [53]. Within the TAM research context, where SOX9 has been identified as a key transcription factor promoting tumor metastasis through mechanisms like epithelial-mesenchymal transition (EMT), robust knockdown verification becomes paramount for accurate biological interpretation [5].
Technical Principles and Potential Discrepancies
Understanding the fundamental principles and limitations of each technique is crucial for interpreting verification data. qRT-PCR and Western blot measure different stages of the central dogma and are subject to distinct regulatory mechanisms.
Biological Causes of Discrepancy
- Temporal Delays in Expression: Gene expression is a dynamic process characterized by significant time delays between transcription (mRNA synthesis) and translation (protein synthesis). An mRNA peak detected by qRT-PCR at 6 hours post-stimulation may not correspond to detectable protein levels until 24 hours later [53].
- Protein Stability and Degradation: Protein half-lives vary dramatically. Short-lived proteins targeted by systems like the ubiquitin-proteasome pathway (e.g., p53, cyclins) may degrade rapidly, resulting in high mRNA levels but low detectable protein. Conversely, structural proteins with long half-lives can persist long after their mRNA has diminished [53].
- Translational Regulation: mRNA abundance does not always guarantee proportional protein synthesis. Mechanisms such as miRNA-mediated repression, translational suppression under stress conditions (e.g., hypoxia, heat shock), and variations in mRNA stability can decouple mRNA levels from protein output [53].
- Post-Translational Modifications (PTMs): Western blot detects protein presence but not necessarily functional state. Processes like phosphorylation, glycosylation, and ubiquitination can alter protein function, activity, and antibody recognition without affecting transcription levels [53].
Technical Causes of Discrepancy
- Internal Reference Selection: Using inappropriate reference genes for normalization is a common source of error. Many traditional "housekeeping" genes like GAPDH and β-actin can vary significantly under experimental conditions, leading to normalization artifacts [53] [54].
- Antibody and Primer Specificity: Cross-reactive antibodies in Western blot can produce false-positive bands, while inefficient qRT-PCR primer design (e.g., failure to span exon-exon junctions) can cause false negatives [53].
- Sample Handling and Linearity: Improper sample storage, repeated freeze-thaw cycles, and operating outside the linear dynamic range of detection for both assays can severely compromise quantification accuracy [53] [55].
Table 1: Common Scenarios of Discordant qRT-PCR and Western Blot Results
| qRT-PCR Result | Western Blot Result | Potential Causes |
|---|---|---|
| Increased | Unchanged | Translational repression, long protein half-life |
| Unchanged | Increased | Enhanced translation, reduced protein degradation |
| Increased | Decreased | Accelerated protein degradation (e.g., ubiquitination) |
| Unchanged | Unchanged (but activity altered) | Post-translational modifications affecting protein function |
Detailed Experimental Protocols
Sample Preparation from TAM Cultures
This protocol assumes SOX9 knockdown has been performed in TAMs or a co-culture system using methods like siRNA, shRNA, or CRISPR-Cas13d [56].
Materials:
- TAM culture (e.g., primary macrophages or cell lines like THP-1-derived macrophages)
- RNA extraction kit (e.g., TRIzol)
- Protein lysis buffer (containing protease and phosphatase inhibitors)
Procedure:
- Culture and Transfect: Plate and transfert TAMs according to established protocols. For TAM studies, this may involve co-culture with cancer cells (e.g., A549, H1299) to maintain M2-like polarization [5].
- Harvest Cells: At the appropriate post-transfection timepoint (e.g., 48-72 hours), harvest cells.
- Split Sample: Divide the cell pellet into two equal aliquots for parallel RNA and protein extraction. Critical: This ensures the same population is analyzed by both techniques.
- RNA Extraction: Extract total RNA using your preferred method. Treat with DNase I to remove genomic DNA contamination. Assess RNA purity and integrity (A260/A280 ratio ~2.0, clear ribosomal bands on agarose gel).
- Protein Extraction: Lyse the cell pellet in appropriate RIPA buffer. Centrifuge to remove insoluble debris. Determine protein concentration using a compatible assay (e.g., BCA or Bradford assay) [55].
Verification by Quantitative RT-PCR (qRT-PCR)
This protocol verifies knockdown at the mRNA level.
Materials:
- High-Capacity cDNA Reverse Transcription Kit
- SYBR Green or TaqMan qPCR Master Mix
- Validated primers for SOX9 and reference genes
Procedure:
- cDNA Synthesis: Convert 1 µg of total RNA into cDNA using a reverse transcription kit.
- Primer Design & Validation:
- Design primers that span an exon-exon junction to avoid genomic DNA amplification.
- Validate primer efficiency using a standard curve (efficiency of 90-110% with R² > 0.99).
- qPCR Reaction:
- Prepare reactions in triplicate containing: 1x SYBR Green Master Mix, forward and reverse primers (e.g., 200 nM each), cDNA template (~10 ng equivalent).
- Run on a real-time PCR instrument using a standard two-step cycling protocol.
- Data Analysis:
- Calculate Cq values for SOX9 and reference genes.
- Use the comparative ΔΔCq method to calculate fold-change in gene expression.
- Normalize SOX9 Cq values to the geometric mean of multiple stable reference genes [54].
Table 2: Essential Reagents for qRT-PCR Verification
| Reagent / Equipment | Function / Role | Example Product / Note |
|---|---|---|
| RNA Extraction Kit | Isolates high-purity, intact total RNA | TRIzol, column-based kits |
| Reverse Transcriptase | Synthesizes cDNA from RNA template | M-MLV, AMV-RT |
| qPCR Master Mix | Contains enzymes, dNTPs, buffer, and fluorescent dye | SYBR Green, TaqMan assays |
| Validated Primers | Gene-specific amplification | SOX9, reference genes (Gapdh, Mapk1) |
| Real-Time PCR Instrument | Amplifies and detects DNA in real-time | Applied Biosystems, Bio-Rad, Roche |
Verification by Western Blot
This protocol confirms the knockdown at the protein level.
Materials:
- Pre-cast polyacrylamide gels
- PVDF or nitrocellulose membrane
- Electrophoresis and transfer apparatus
- Primary antibody against SOX9 and loading control
- Species-appropriate HRP-conjugated secondary antibody
- Chemiluminescent substrate
Procedure:
- Protein Electrophoresis:
- Dilute 10-30 µg of total protein lysate in 1x Laemmli buffer.
- Heat denature at 95°C for 5 minutes.
- Load samples and pre-stained protein ladder onto a pre-cast gel (e.g., 4-12% Bis-Tris Plus gel).
- Run gel at constant voltage (e.g., 200V for 20-30 minutes) until the dye front reaches the bottom [55].
- Protein Transfer:
- Transfer proteins from the gel to a PVDF membrane using a wet or semi-dry transfer system.
- Blocking and Antibody Incubation:
- Block the membrane with 5% non-fat milk or BSA in TBST for 1 hour at room temperature.
- Incubate with primary antibody (e.g., anti-SOX9) diluted in blocking buffer overnight at 4°C.
- Wash membrane 3 x 5 minutes with TBST.
- Incubate with HRP-conjugated secondary antibody (optimally diluted, e.g., 1:50,000 to 1:250,000) for 1 hour at room temperature [55].
- Wash membrane 3 x 5 minutes with TBST.
- Signal Detection and Quantification:
- Develop the blot with a high-quality, linear-range chemiluminescent substrate (e.g., SuperSignal West Dura) [55].
- Image the blot using a digital imaging system capable of capturing images without pixel saturation.
- Quantify band intensity using image analysis software (e.g., ImageJ, iBright Analysis Software).
- Normalization:
- Strip and re-probe the membrane for a loading control.
- Normalize the SOX9 band intensity to the loading control. For the most reliable quantification, consider using Total Protein Normalization (TPN) with stains like No-Stain Protein Labeling Reagent, which provides a superior linear dynamic range compared to traditional housekeeping proteins [55].
Table 3: Essential Reagents for Western Blot Verification
| Reagent / Equipment | Function / Role | Example Product / Note | |
|---|---|---|---|
| Pre-cast Gels | Separates proteins by molecular weight | Bolt Bis-Tris Plus Gels | |
| Transfer Apparatus | Transfers proteins from gel to membrane | iBlot 2 Gel Transfer Device | |
| PVDF Membrane | Binds proteins for antibody probing | 0.45 µm PVDF | |
| - | Primary Antibody | Binds specifically to target protein | Anti-SOX9, Anti-β-actin |
| Chemiluminescent Substrate | Generates light signal for detection | SuperSignal West Dura |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Key Research Reagent Solutions for Knockdown Verification
| Category | Specific Item | Function & Importance |
|---|---|---|
| Knockdown Tools | CRISPR-Cas13d System | Provides highly specific RNA knockdown with minimal off-target effects, superior to siRNA for some circRNAs and mRNAs [56]. |
| qRT-PCR | No-Stain Protein Labeling Reagent | Fluorescently labels total protein for superior normalization in Western blot, offering a wider linear dynamic range than traditional housekeeping proteins [55]. |
| Western Blot | High-Linearity Chemiluminescent Substrate | Enables accurate quantification by providing a sensitive, linear signal over a broad protein concentration range (e.g., SuperSignal West Dura) [55]. |
| Reference Genes | Validated Primer Sets (e.g., Gapdh, Mapk1) | Stable internal controls for qRT-PCR data normalization; must be validated for specific cell types and conditions [54]. |
| Cell Culture | Cytokines (e.g., TGF-β) | Used to polarize macrophages towards an M2-like, TAM-associated phenotype for functionally relevant experiments [5]. |
Data Interpretation and Troubleshooting
Successful Knockdown Verification
Successful verification is demonstrated by a significant reduction in both SOX9 mRNA (via qRT-PCR) and SOX9 protein (via Western blot) in the knockdown group compared to the control. Densitometric analysis should show a consistent percentage of knockdown across both techniques. In the context of TAM research, successful SOX9 knockdown should subsequently impair TAM-driven tumor cell invasion and EMT, validating the functional consequence of the knockdown [5].
Addressing Discrepant Results
When qRT-PCR and Western blot results conflict, a systematic troubleshooting approach is required.
- mRNA Down, Protein Unchanged: This suggests efficient transcriptional knockdown but the persistence of a long-lived SOX9 protein. Solution: Extend the time between transfection and analysis to allow for natural protein turnover, or consider treatments that accelerate degradation.
- mRNA Unchanged, Protein Down: This indicates the knockdown mechanism may be acting primarily at the translational level, which is a known advantage of systems like CRISPR-Cas13d [56]. It can also suggest off-target effects. Solution: Verify the specificity of your knockdown tool and check for compensatory transcriptional upregulation.
- Unexpected Banding Patterns in Western Blot: SOX9 may undergo PTMs that shift its molecular weight. Solution: Use modification-specific antibodies and ensure your lysis buffer contains appropriate phosphatase/protease inhibitors.
Visualizing the Workflow and Biological Context
The following diagrams illustrate the core experimental workflow for knockdown verification and the key biological role of SOX9 in TAMs that underpins the necessity of this protocol.
Diagram 1: Knockdown Verification Workflow. This flowchart outlines the parallel pathways for qRT-PCR and Western blot analysis, highlighting critical quality control (QC) checkpoints for robust data generation.
Diagram 2: SOX9 Role in TAM-Promoted Metastasis. This diagram illustrates the key biological pathway in which TAM-derived TGF-β upregulates SOX9 in cancer cells, driving EMT and metastasis—a process that can be inhibited by successful SOX9 knockdown [5].
A meticulously executed and critically analyzed combination of qRT-PCR and Western blot is the cornerstone for reliably verifying gene knockdown. This is especially true in therapeutically relevant contexts like SOX9 function in TAMs, where confirming target engagement at both the transcriptional and protein levels is a prerequisite for meaningful functional studies. By adhering to the detailed protocols, optimization strategies, and troubleshooting guidelines outlined in this document, researchers can confidently validate their knockdown models and generate robust, interpretable data to advance our understanding of cancer biology and therapeutic discovery.
Co-culture systems, which facilitate the growth and interaction of two or more distinct cell types, have become indispensable tools in cancer research. These models enable scientists to move beyond simplistic monoculture studies and better recapitulate the complex cellular interactions within the tumor microenvironment (TME). By modeling the dynamic crosstalk between cancer cells and their surrounding stromal and immune cells, particularly tumor-associated macrophages (TAMs), co-culture systems provide critical insights into the mechanisms driving tumor progression, metastasis, and therapeutic resistance [5] [37]. This application note details the implementation of co-culture systems to investigate cancer cell behavior, with a specific focus on the molecular mechanisms impacted by SOX9 knockdown in TAMs, a key area in contemporary cancer biology research [5].
Quantitative Impact of Co-culture on Cancer Phenotypes
Co-culture models have been instrumental in quantifying the functional effects of stromal cells on cancer cell behavior. The tables below summarize key phenotypic changes observed in cancer cells when co-cultured with TAMs.
Table 1: Documented Phenotypic Changes in Cancer Cells Co-cultured with Tumor-Associated Macrophages (TAMs)
| Cancer Cell Phenotype | Observed Change | Proposed Mechanism | Experimental Evidence |
|---|---|---|---|
| Proliferation | Increased | Secretion of growth factors (e.g., TGF-β, IL-6) by TAMs [37] | Enhanced tumor growth in vivo; increased cell count in vitro [5] |
| Migration & Invasion | Significantly Enhanced | TAM-secreted TGF-β inducing EMT; SOX9 upregulation [5] | Transwell and Matrigel invasion assays showing 2-5 fold increase [5] |
| Therapeutic Resistance | Induced | TAM-secreted IL-6, IL-10, and IL-34 activating survival pathways (e.g., STAT3) [37] | Reduced apoptosis in response to chemo/radiotherapy [37] |
| Stem-like Properties | Promoted | Reciprocal interaction with Tumor Stem Cells (TSC) via WNT and STAT3 pathways [37] | Increased spheroid formation capacity; upregulation of stemness markers [37] |
Table 2: Comparison of Static vs. Perfused Co-culture Systems
| Parameter | Static Co-culture | Perfused (Organ-on-a-Chip) Co-culture | Impact on Data Fidelity |
|---|---|---|---|
| Shear Stress | Absent or minimal | Physiologically relevant levels present [57] | Improved endothelial and epithelial cell differentiation and function [57] |
| Mass Transport | Diffusion-limited | Convective flow improves nutrient/waste exchange [57] | Enhanced cell viability in 3D cultures; enables long-term (>1 week) experiments [57] |
| Biomarker Expression | Baseline | Specific biomarkers (e.g., CYP3A4 in Caco-2) show >2-fold induction [57] | Models in vivo-like metabolic and signaling activities more closely [57] |
| Model Reproducibility | High (standardized) | Variable between systems; lower in 2D, slight improvement in 3D [57] | Requires careful system characterization and protocol standardization [57] |
Experimental Protocols
Protocol 1: Establishing a Direct Co-culture Model to Study TAM-Cancer Cell Interactions
This protocol outlines a method for directly co-culturing TAMs and cancer cells to investigate their physical and paracrine interactions.
Materials:
- Cancer cell line (e.g., A549 or H1299 lung adenocarcinoma cells [5])
- Monocytic cell line (e.g., THP-1 cells) for differentiation into macrophages [5]
- Cell culture medium (e.g., DMEM supplemented with 10% FBS [58])
- Phorbol 12-myristate 13-acetate (PMA) for THP-1 differentiation [5]
- Recombinant human TGF-β (optional, for stimulation) [5]
- TGF-β receptor inhibitor (e.g., SB431542) (optional, for inhibition) [5]
Procedure:
- Macrophage Differentiation: Seed THP-1 monocytes in culture vessels and induce differentiation into macrophages by treating with 100 ng/mL PMA for 24-48 hours [5].
- M2 Polarization: Differentiated macrophages can be polarized toward an M2-like (TAM) phenotype by incubating with IL-4 (20 ng/mL) and IL-13 (20 ng/mL) for an additional 24 hours [37].
- Co-culture Setup: Seed cancer cells (e.g., A549) directly onto the layer of differentiated TAMs at a desired ratio (e.g., 1:1 or 1:5 macrophage-to-cancer cell ratio). Use appropriate mono-cultures of each cell type as controls.
- Incubation and Analysis: Co-culture cells for 24-72 hours in a standard CO₂ incubator (37°C, 5% CO₂). The duration depends on the experimental endpoint.
- Sample Harvesting: After incubation, harvest cells for downstream analysis.
- For protein/mRNA analysis: Wash with PBS and lyse cells directly for Western blot or RT-qPCR to analyze markers like SOX9, E-cadherin, and vimentin [5].
- For functional assays: Use the co-cultured cells in migration, invasion, or proliferation assays.
Protocol 2: Conditioned Medium-Based Indirect Co-culture
This method uses conditioned medium to study paracrine signaling without direct cell contact.
Procedure:
- Generate Conditioned Medium (CM):
- Culture TAMs (as described in Protocol 1) in serum-free medium for 24-48 hours.
- Collect the supernatant and centrifuge (e.g., 200 × g for 5 minutes) to remove cell debris. Filter-sterilize (0.22 µm pore size) [5].
- Stimulate Cancer Cells:
- Culture cancer cells (e.g., A549) to 70-80% confluence.
- Replace the standard medium with the TAM-conditioned medium (or a 1:1 mix with fresh medium as a control).
- Incubate for 24-72 hours [5].
- Validation and Analysis:
Protocol 3: Flow Cytometry Analysis of Co-cultured Cells
This protocol enables the identification and phenotypic analysis of specific cell populations within a mixed co-culture.
Materials:
- Single-cell suspension from co-culture
- Flow cytometry staining buffer (PBS with 5-10% FCS) [59]
- Fc receptor blocking solution (e.g., human IgG or anti-CD16/CD32) [59]
- Fluorescently conjugated antibodies (e.g., anti-CD163 for TAMs, anti-EpCAM for cancer cells)
- Viability dye (e.g., 7-AAD, DAPI) [59]
- Fixation/Permeabilization reagents (if staining intracellular markers like SOX9) [59]
Procedure:
- Cell Harvest and Viability Staining:
- Cell Surface Staining:
- Wash cells to remove unbound dye.
- Block Fc receptors by incubating with blocking buffer for 10-15 minutes on ice [59].
- Without washing, add a cocktail of fluorescently conjugated surface marker antibodies. Incubate for 30 minutes in the dark on ice.
- Wash cells twice to remove unbound antibodies.
- Intracellular Staining (e.g., for SOX9):
- Fix cells using 1-4% paraformaldehyde for 15-20 minutes on ice [59].
- Wash cells and permeabilize using a mild detergent like saponin (0.1-0.5%) or a commercial permeabilization buffer for 10-15 minutes at room temperature [59].
- Stain cells with an antibody against the intracellular target (e.g., anti-SOX9) in permeabilization buffer for 30-60 minutes.
- Wash cells twice and resuspend in staining buffer for acquisition on a flow cytometer [59].
- Data Acquisition and Analysis:
- Use flow cytometry to collect data, gating on single, live cells.
- Further subdivide populations based on surface markers (e.g., CD163+ TAMs vs. EpCAM+ cancer cells) and analyze the expression of intracellular targets (e.g., SOX9) within each gate.
Signaling Pathways and Experimental Workflows
The TGF-β/SOX9 Signaling Axis in TAM-Induced Cancer Progression
Experimental Workflow for SOX9 Knockdown in Co-culture Studies
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Co-culture Studies in Cancer Research
| Reagent / Material | Function / Purpose | Example Product / Target |
|---|---|---|
| Monocytic Cell Lines | Source for generating human macrophages in vitro | THP-1 cells [5] |
| Polarization Cytokines | To differentiate macrophages into M2-like TAM phenotype | IL-4, IL-13 [37] |
| Recombinant Growth Factors | To stimulate specific signaling pathways in co-culture | Recombinant Human TGF-β [5] |
| Pathway Inhibitors | To inhibit and test the necessity of specific signaling | TGF-β Receptor Inhibitor (SB431542) [5] |
| Gene Knockdown Tools | To investigate gene function (e.g., SOX9) | SOX9-targeting siRNA/shRNA [5] |
| Antibodies for Flow Cytometry | To identify and isolate specific cell populations | Anti-CD163 (TAMs), Anti-EpCAM (Cancer Cells) [5] [59] |
| Viability Dyes | To distinguish live from dead cells in analysis | 7-AAD, DAPI [59] |
| Fixation/Permeabilization Kits | For intracellular staining of markers like SOX9 | Commercial kits (e.g., ab185917) [59] |
Troubleshooting SOX9 Knockdown: Overcoming Low Efficiency and Off-Target Effects
Addressing Low Transfection Efficiency in Hard-to-Transfect Macrophages
The genetic manipulation of tumor-associated macrophages (TAMs) represents a promising therapeutic strategy in oncology, with SRY-related high-mobility group box gene 9 (SOX9) emerging as a transcription factor of significant interest. However, macrophages are notoriously difficult to transfect due to their intrinsic biological characteristics, including their proficiency in recognizing and degrading foreign nucleic acids through pattern recognition receptors and their robust endocytic and phagocytic activities that often sequester or degrade transfection complexes before reaching the cytosol [60] [61]. This challenge is particularly pronounced in primary macrophages and those within the tumor microenvironment (TME), where their immunosuppressive M2-polarized state further complicates efficient gene delivery. The development of reliable protocols for SOX9 knockdown in TAMs is therefore contingent upon overcoming these fundamental biological barriers through advanced transfection technologies and optimized methodologies.
Current Transfection Technologies: A Comparative Analysis
Several non-viral transfection platforms have been developed to address the unique challenges of macrophage transfection. The table below summarizes the key performance characteristics of leading technologies based on current research findings:
Table 1: Comparison of Transfection Technologies for Macrophages
| Technology | Mechanism of Action | Reported Efficiency (RAW 264.7) | Cytotoxicity Profile | Key Advantages |
|---|---|---|---|---|
| QDP/siRNA [60] | Clathrin/caveolin-mediated endocytosis | ~90% (2x higher than commercial reagents) | Minimal at ≤120 nM | High delivery efficiency, endosomal escape |
| Tyrosine-modified PPI-G4 [62] | Nanoparticle complexation | High efficacy in hard-to-transfect MSCs | Favorable biocompatibility | Effective for primary cells |
| Nanostraw Electro-actuated Transfection (NExT) [63] | Nanostraw penetration with localized electric fields | High throughput (14M cells) | Minimal cellular disruption | Preserves cell viability and function |
| Lipid Nanoparticles (LNPs) [61] | Endosomal fusion and release | Varies by formulation | Generally biocompatible | Clinical validation, scalable production |
Quantitative Assessment of Transfection Performance
Recent studies provide quantitative data supporting the efficacy of these platforms in macrophage-like cell lines and primary cells:
Table 2: Quantitative Performance Metrics of Transfection Systems
| Parameter | QDP/FAM-small RNA [60] | Commercial Reagents [60] | Nanostraw Technology [63] |
|---|---|---|---|
| Delivery Efficiency | 90% at 80-120 nM | <50% in RAW 264.7 cells | High across multiple immune cell types |
| Silencing Efficiency | Significant GAPDH knockdown | Lower silencing efficiency | CRISPR/Cas9 knockout demonstrated |
| Cell Viability | >95% at 120 nM | Variable | Minimal perturbation |
| Therapeutic Effect | Effective M1-to-M2 conversion | Not specifically reported | CAR transgene delivery successful |
Experimental Protocol for SOX9 Knockdown in TAMs
QDP/siRNA Complex Preparation and Transfection
This protocol details the use of polyethyleneimine-modified carboxyl quantum dots (QDP) for SOX9 siRNA delivery to TAMs, adapted from established methodologies with modifications specific to SOX9 targeting [60].
Day 1: Macrophage Culture Preparation
- Isolate primary human monocytes from peripheral blood using Ficoll density gradient centrifugation.
- Differentiate monocytes into macrophages by culturing in RPMI-1640 medium supplemented with 10% FBS and 50 ng/mL M-CSF for 7 days.
- Polarize macrophages to M2 phenotype (TAM-like) by treating with 20 ng/mL IL-4 and 20 ng/mL IL-13 for 48 hours.
- Plate M2-polarized macrophages in 24-well plates at a density of 2×10^5 cells/well in antibiotic-free medium and incubate overnight at 37°C, 5% CO₂.
Day 2: QDP/siSOX9 Complex Formation
- Prepare SOX9 siRNA targeting the following sequence: 5'-GGAUCAAGCACGACGUCAATT-3' (sense) with validated silencing efficacy.
- Dilute 5 μL of carboxyl-QDs (C-QDs, 15 nm) in 50 μL of serum-free medium.
- Prepare tyrosine-modified polymer solution by diluting 2.5 μg in 50 μL serum-free medium.
- Combine QDs and polymer solutions, incubate for 15 minutes at room temperature to form QDP complexes.
- Add 5 μL of 20 μM SOX9 siRNA to the QDP solution, mix gently, and incubate for 30 minutes at room temperature to form QDP/siSOX9 complexes.
- Add 100 μL of serum-free medium to achieve final volume of 200 μL.
Day 2: Transfection Procedure
- Remove culture medium from macrophages and wash once with PBS.
- Add 200 μL of QDP/siSOX9 complexes to cells (final siRNA concentration: 80 nM).
- Incubate cells at 37°C, 5% CO₂ for 6 hours.
- Replace transfection medium with complete growth medium containing 10% FBS.
- Continue incubation for 24-72 hours based on experimental requirements for downstream analysis.
Validation and Functional Assessment
Efficiency Validation
- After 48 hours post-transfection, harvest cells for RNA extraction and quantify SOX9 knockdown using qRT-PCR with the following primers: SOX9 forward 5'-AGGAAGCTGGCAGACCAGTA-3', reverse 5'-ACGAAGGGTCTCTTCTCGCT-3'.
- At 72 hours post-transfection, analyze SOX9 protein expression by western blot using anti-SOX9 antibody (1:1000 dilution).
- Confirm successful transfection efficiency using fluorescence microscopy or flow cytometry for FAM-labeled siRNA (typically >90% expected).
Functional Phenotype Assessment
- Evaluate TAM repolarization by measuring M1/M2 marker expression 72 hours post-transfection.
- Quantify M1 markers (iNOS, IL-12, TNF-α) and M2 markers (Arg-1, CD206, IL-10) using qRT-PCR and ELISA.
- Assess functional changes through migration assays (Transwell system) and phagocytosis assays (pHrodo-labeled E. coli bioparticles).
Flowchart 1: SOX9 Knockdown Experimental Workflow
Mechanism of Action and Intracellular Trafficking
Cellular Uptake and Endosomal Escape
The QDP/siRNA platform leverages specific endocytic pathways for efficient intracellular delivery. Studies demonstrate that QDP/siRNA complexes enter macrophages primarily through clathrin- and caveolin-mediated endocytosis, as evidenced by significant uptake inhibition when treated with chlorpromazine (clathrin inhibitor) and methyl-β-cyclodextrin (caveolin inhibitor) [60]. This targeted entry mechanism distinguishes it from other nanoparticle systems that may utilize less efficient pathways. Following cellular internalization, the intracellular trafficking follows a defined temporal sequence: QDP/siRNA complexes localize to early endosomes (EEA1-positive) within 5 minutes, escape predominantly at 10-30 minutes, traffic to late endosomes/lysosomes (LAMP1-positive) at 2-4 hours, and release siRNA into the cytoplasm by 4 hours post-transfection [60]. This efficient endosomal escape is critical for productive siRNA delivery and represents a significant advantage over conventional transfection reagents that often exhibit extensive endo-lysosomal sequestration.
SOX9 Biology in Macrophage Function and Signaling
SOX9 has emerged as a pivotal regulator in various disease contexts, though its specific role in TAM biology requires further elucidation. In vascular smooth muscle cells, SOX9 drives phenotypic transformation through direct binding to the STAT3 promoter, enhancing proliferation and migration – processes relevant to TAM functionality in tumor progression [64]. Furthermore, in neuropathic pain models, SOX9 transcriptionally regulates hexokinase 1 (HK1), driving glycolytic flux and promoting pro-inflammatory astrocyte subsets through lactate-mediated histone lactylation [65]. This immunometabolic regulatory function may parallel potential mechanisms in TAMs, where metabolic reprogramming is a hallmark of polarization states. Successful SOX9 knockdown in TAMs may therefore disrupt critical transcriptional networks governing both inflammatory signaling and metabolic pathways central to their pro-tumoral functions.
Flowchart 2: Intracellular Trafficking and Mechanism of SOX9 Knockdown
Troubleshooting and Optimization Guide
Common Challenges and Solutions
Table 3: Troubleshooting Guide for Macrophage Transfection
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Low Transfection Efficiency | Incomplete complex formation; suboptimal QD:siRNA ratio; insufficient cellular uptake | Optimize QD:siRNA ratio (test 1:1 to 1:5); verify complex size (115.5 nm expected); confirm serum-free conditions during transfection [60] |
| High Cytotoxicity | Excessive QDP concentration; serum presence during transfection; inadequate polymer modification | Titrate QDP concentration (test 40-120 nM range); ensure serum-free conditions during transfection; extend recovery period post-transfection [60] [62] |
| Inconsistent SOX9 Knockdown | Inefficient siRNA design; poor endosomal escape; rapid siRNA degradation | Validate multiple SOX9 siRNA sequences; incorporate endosomolytic agents; confirm siRNA integrity and complex stability [60] [61] |
| Variable Repolarization Effects | Heterogeneous macrophage populations; incomplete polarization; TME-mimicking conditions insufficient | Standardize M2 polarization protocol (validate with CD206+ staining); incorporate TME-conditioned medium; use primary macrophages rather than cell lines when possible |
Critical Optimization Parameters
Several key parameters require systematic optimization to maximize SOX9 knockdown efficacy while maintaining macrophage viability:
Polymer Modification and Formulation Tyrosine-modified polymers demonstrate enhanced stability and transfection efficiency compared to unmodified counterparts. The tyrosine modification of low molecular weight PEIs (2-25 kDa) and PPI dendrimers significantly improves siRNA complexation while reducing cytotoxicity [62]. Optimal results have been achieved with tyrosine-modified PPI-G4, which shows particular efficacy in hard-to-transfect primary cells. The polymer-to-siRNA ratio should be systematically titrated, with mass ratios between 10:1 and 30:1 typically providing optimal balance between complex stability and cytotoxicity.
Cell Culture and Handling Considerations Primary macrophages demonstrate substantial donor-dependent variability in transfection efficiency. Pre-screening donors or using pooled macrophage populations can improve experimental consistency. Maintaining macrophage polarization status throughout the transfection process is critical, as dedifferentiation can confound results. Including polarization cytokines (IL-4, IL-13) during recovery periods post-transfection helps maintain phenotype integrity. Furthermore, the use of specialized culture surfaces (e.g., low-attachment plates) can improve macrophage viability and functionality during transfection procedures.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Macrophage Transfection and SOX9 Studies
| Reagent/Category | Specific Examples | Function/Application | Notes for Macrophage Research |
|---|---|---|---|
| Nanocarrier Platforms | Carboxyl quantum dots (C-QDs); Tyrosine-modified PPI/PEI; LNPs | siRNA complexation and delivery | QDP shows >90% efficiency in RAW 264.7; Tyrosine-modification enhances efficacy in primary cells [60] [62] |
| Polarization Cytokines | M-CSF; IL-4; IL-13; IFN-γ; LPS | Directional polarization to M1/M2 phenotypes | Validate polarization state pre-transfection via surface markers (CD206 for M2) |
| SOX9 Targeting Reagents | Validated SOX9 siRNA; Anti-SOX9 antibodies; SOX9 luciferase reporters | Knockdown validation and functional assessment | Confirm species specificity; multiple siRNA sequences recommended |
| Analytical Tools | qPCR primers for M1/M2 markers; Flow cytometry antibodies; Phagocytosis assay kits | Phenotypic and functional validation | Include both transcriptomic and functional endpoints |
| Critical Assay Kits | Cell viability assays (MTT/WST-1); ELISA kits for cytokine profiling; Metabolic assay kits | Assessment of cytotoxicity and functional consequences | Avoid LDH assays due to inherent macrophage secretion |
The protocol described herein provides a validated framework for efficient SOX9 knockdown in hard-to-transfect TAMs using advanced nanocarrier systems. The QDP platform demonstrates particular promise, achieving approximately 90% delivery efficiency in macrophage cell lines with minimal cytotoxicity at optimized concentrations. The successful implementation of this technology enables researchers to probe SOX9 function in TAM biology and assess its therapeutic relevance as a target for reprogramming the tumor microenvironment. As the field advances, the integration of these transfection methodologies with single-cell analytics and in vivo delivery systems will be essential for translating basic research findings into clinically viable TAM-targeted therapies. The continued refinement of nanoparticle design, with particular emphasis on cell-type specificity and enhanced endosomal escape, will further accelerate progress in this critical area of cancer immunotherapy research.
Optimizing siRNA Concentration and Reagent Formulations
Within the tumor microenvironment, tumor-associated macrophages (TAMs) play a critical role in promoting cancer progression and metastasis. Research has established that TAMs secrete factors such as TGF-β, which increases SOX9 expression and promotes epithelial-to-mesenchymal transition (EMT) in lung cancer cells, thereby driving tumor proliferation, migration, and invasion [5]. Knockdown of SOX9 has been shown to inhibit this TAM-mediated EMT process, indicating that the TGF-β-mediated EMT is SOX9-dependent [5]. This application note provides detailed methodologies for optimizing siRNA delivery to effectively silence SOX9 in TAMs, a strategy that holds significant promise for disrupting this pro-metastatic pathway.
Key Challenges in siRNA Delivery to TAMs
Delivering siRNA to TAMs presents unique challenges that necessitate careful optimization. siRNAs are inherently vulnerable to degradation in biological environments and require protective delivery systems [66]. Furthermore, achieving targeted delivery is critical for optimal efficacy and minimal off-target effects [66]. The primary obstacles include ensuring stability of siRNA in culture, achieving high transfection efficiency in often difficult-to-transfect primary immune cells, and minimizing non-specific immune activation and cytotoxicity.
Systematic Optimization of siRNA Formulations
Transfection Reagent and siRNA Concentration
The cornerstone of successful gene silencing is identifying the optimal combination of transfection reagent and siRNA concentration that maximizes knockdown while maintaining cell viability. The table below summarizes a recommended optimization matrix for a 24-well plate format, using Lipofectamine RNAiMAX as a starting point due to its superior efficiency for siRNA delivery in a wide range of cell types, including difficult-to-transfect cells [67] [68].
Table 1: siRNA and Transfection Reagent Optimization Matrix for a 24-well Plate
| siRNA Concentration (nM) | Lipofectamine RNAiMAX (µL) | Expected Knockdown Efficiency | Expected Cell Viability |
|---|---|---|---|
| 1 | 1.0 | Low (>50%) | High (>90%) |
| 5 | 1.5 | Moderate (50-70%) | High (>85%) |
| 10 | 2.0 | High (70-90%) | Good (>80%) |
| 25 | 2.5 | Very High (>90%) | Moderate (70-80%) |
| 50 | 3.0 | Very High (>90%) | Potential Cytotoxicity |
Protocol:
- Complex Formation: Dilute the SOX9 siRNA (e.g., 5 µL of a 10 µM stock) in 50 µL of serum-free medium. In a separate tube, dilute the recommended amount of Lipofectamine RNAiMAX (see table) in 50 µL of the same serum-free medium. Incubate for 5 minutes at room temperature.
- Complexation: Combine the diluted siRNA with the diluted transfection reagent (total volume: 100 µL). Mix gently and incubate for 20 minutes at room temperature to allow complex formation.
- Transfection: Add the 100 µL complex dropwise to the cells in the well. Gently swirl the plate to ensure even distribution.
- Incubation: Incubate cells for 6-24 hours before replacing the transfection medium with fresh complete growth media to reduce cytotoxicity [68].
Cell-Specific Parameters
Cell health and density at the time of transfection are critical for reproducibility. The following parameters must be optimized:
- Cell Density: Plate cells so they are 40-80% confluent at the time of transfection [68]. For primary BMDMs, a confluence of 60-80% is recommended [69].
- Cell Passage: Use cells at a low passage number (e.g., less than 50) to ensure genetic stability and high transfection efficiency [67] [68].
- Antibiotic-Free Medium: Transfect in medium without antibiotics, as they can accumulate in permeabilized cells and cause toxicity [67] [68].
Controls for Experimental Validation
Including the correct controls is mandatory for interpreting results.
- Positive Control: An siRNA targeting a housekeeping gene (e.g., GAPDH) to confirm transfection efficiency is working, with an expected ≥70% knockdown of the target mRNA [68].
- Negative Control: A scrambled sequence siRNA with no significant homology to the genome to distinguish sequence-specific effects from non-specific effects [67] [68].
- Fluorescently Labeled siRNA: Can be used to visually optimize transfection efficiency and study siRNA subcellular localization [67].
Diagram 1: SOX9 knockdown strategy to inhibit TAM-driven metastasis.
Advanced Delivery Strategies for Challenging Cells
While lipid-based transfection is effective for many cell types, primary macrophages and other immune cells can be challenging. Recent advances highlight alternative strategies:
- Lipid-Conjugate-Mediated Delivery: A systematic study showed that lipid-conjugate-mediated delivery outperformed lipid-nanoparticle-mediated and extracellular-vesicle-mediated delivery in activated T cells ex vivo. This method was also the first robust report of productive siRNA uptake into resting primary immune cells [70], which is highly relevant for TAM research.
- Electroporation: For cell lines that are notoriously difficult to transfect with standard reagents, electroporation may be the only viable alternative. This method uses electrical pulses to create transient pores in the cell membrane. Note that a balance must be struck between gene knockdown and cell mortality by optimizing voltage, pulse length, and pulse number [68].
Validation and Analysis
Assessing Knockdown Efficacy
To ensure the success of your SOX9 knockdown experiment, efficacy and specificity must be monitored at the appropriate timepoints.
- mRNA Analysis: Use qRT-PCR to quantify target mRNA levels 24-48 hours after siRNA transfection [68] [71]. Calculate the percentage of gene silencing using the formula: [ \text{Percentage gene silencing} = \left(1 - \frac{\text{Treated sample expression level}}{\text{Control sample expression level}}\right) \times 100 ] [71]
- Protein Analysis: Assess SOX9 protein knockdown by Western blot 48-72 hours after transfection, as protein turnover rates affect the optimal time for observation [68]. The correlation between SOX9 expression and TAM density can be further analyzed via immunofluorescent staining for SOX9 and the macrophage marker CD163 [5].
Functional Assays
Given the role of the TGF-β/SOX9 axis in metastasis, functional validation is crucial.
- Migration and Invasion Assays: Perform assays (e.g., Boyden chamber) after SOX9 knockdown in lung cancer cells co-cultured with TAMs or treated with TGF-β. SOX9 knockdown should significantly reduce TAM-induced migration and invasion [5].
- Phenotypic Observation: Monitor cells for a reversal of the EMT-like phenotype (e.g., morphological changes from mesenchymal to epithelial) following SOX9 knockdown [5].
Diagram 2: Experimental workflow for optimizing siRNA transfection.
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for siRNA-Mediated SOX9 Knockdown
| Item | Function/Purpose | Example Products & Notes |
|---|---|---|
| SOX9-Targeting siRNA | Sequence-specific silencing of the target gene. | Design 2-4 different sequences; use online tools (e.g., siDirect, Dharmacon siDESIGN) for specificity and efficacy [71]. |
| Transfection Reagent | Forms complexes with siRNA for cellular delivery. | Lipofectamine RNAiMAX (superior for wide range of cells) [67]. Test multiple reagents for challenging cells [68]. |
| Positive Control siRNA | Validates transfection protocol is working. | siRNA targeting a constitutively expressed gene (e.g., GAPDH). Expect ≥70% knockdown [68]. |
| Negative Control siRNA | Rules out non-specific effects. | Scrambled sequence siRNA with no significant homology to the genome [67]. |
| Fluorescently Labeled siRNA | Visual optimization of transfection efficiency and uptake. | e.g., Cy3- or FAM-labeled siRNA [67]. |
| qRT-PCR Reagents | Quantitative assessment of mRNA knockdown. | TaqMan or SYBR Green assays for SOX9 and normalizing housekeeping genes. |
| Western Blot Reagents | Confirmation of protein-level knockdown. | Antibodies against SOX9 and a loading control (e.g., β-Actin). |
| Cell Culture Media | Maintaining healthy, transferable cells. | Use serum-free or reduced-serum medium for transfection if required by the reagent protocol [68]. |
Troubleshooting Common Pitfalls
- High Cytotoxicity with Good Knockdown: Reduce the amount of transfection reagent and/or shorten the exposure time to complexes before replacing the media [68].
- Poor Knockdown Efficiency: Ensure cells are healthy and not over-confluent. Re-optimize the siRNA concentration and transfection reagent volume. Consider using a different transfection reagent or switching to electroporation [68].
- Off-Target Effects: Use multiple siRNA sequences targeting different regions of the SOX9 gene and confirm findings with consistent phenotypic results across all sequences [71]. Always include a scrambled siRNA control.
The transcription factor SOX9 has been identified as a pivotal regulator in the tumor microenvironment (TME), where it exhibits a complex, "Janus-faced" role in tumor immunity [4]. It promotes tumor immune escape by impairing the function of cytotoxic immune cells and is frequently overexpressed in various solid malignancies, including lung adenocarcinoma (LUAD) [4] [44]. In the context of tumor-associated macrophages (TAMs), a key interaction has been elucidated: TAMs secrete Transforming Growth Factor-beta (TGF-β), which upregulates SOX9 expression in cancer cells via the C-jun/SMAD3 pathway. This SOX9 induction promotes epithelial-to-mesenchymal transition (EMT), tumor proliferation, migration, and invasion [5]. Consequently, SOX9 knockdown in TAM-focused research represents a promising therapeutic strategy. However, such approaches, particularly those utilizing CRISPR-Cas9, necessitate rigorous validation to control for off-target genomic effects and unintended immune consequences. This application note provides a detailed protocol for this essential validation process.
Key Signaling Pathways and Workflows
SOX9 in the Tumor Immune Microenvironment
The following diagram illustrates the central role of SOX9 in the interplay between tumor cells and the immune microenvironment, highlighting key pathways relevant to knockdown strategies.
Specificity Validation Workflow for SOX9 Knockdown
A multi-tiered experimental workflow is essential to confidently attribute phenotypic changes to on-target SOX9 knockdown. The recommended strategy integrates computational prediction, in vitro and in-cellulo off-target detection, and in vivo immune profiling, as outlined below.
Experimental Protocols
Protocol: In Silico gRNA Design and Off-Target Prediction
This initial protocol is critical for selecting a specific gRNA before any wet-lab experiments begin.
1. gRNA Selection:
- Design 3-5 gRNAs targeting exonic regions of the SOX9 gene using established design tools.
- Priority should be given to gRNAs with a high on-target efficiency score and low off-target potential. Truncated gRNAs (tru-gRNAs) with 17-18 nucleotides of specificity instead of 20 can be considered to enhance specificity [72].
2. Off-Target Prediction:
- Input the candidate gRNA sequences into multiple in silico prediction tools.
- Cas-OFFinder: Use this alignment-based tool to identify potential off-target sites with up to 5 nucleotide mismatches across the reference genome. It allows for the specification of the protospacer-adjacent motif (PAM) sequence relevant to the Cas nuclease used (e.g., 5'-NGG-3' for SpCas9) [73] [72].
- Cutting Frequency Determination (CFD) Score: Utilize this scoring-based model to rank and score the potential off-target sites identified by Cas-OFFinder. A higher CFD score indicates a greater likelihood of cleavage [73] [72].
- Cross-referencing: Select the final gRNA candidate based on the lowest number of predicted off-target sites, especially those with high CFD scores and located within protein-coding genes or regulatory regions.
Protocol: Experimental Detection of Off-Target Edits
Following in silico prediction, unbiased genome-wide methods are required to empirically identify off-target sites.
1. Sample Preparation:
- Transfert the chosen CRISPR-Cas9 construct (e.g., as a ribonucleoprotein complex, RNP) into the target macrophage or co-culture model.
- Culture cells for 72 hours to allow for genome editing.
- Extract high-quality, high-molecular-weight genomic DNA (gDNA) using a silica-column or magnetic bead-based method.
2. Off-Target Screening with GUIDE-seq:
- This is a cell-based, unbiased method that captures genome-wide double-strand breaks [72].
- Procedure: Co-transfect cells with the Cas9/gRNA complex and a proprietary, end-protected double-stranded oligodeoxynucleotide (dsODN) tag.
- After 72 hours, harvest cells and extract gDNA.
- Shear the gDNA and prepare a sequencing library. Using PCR, amplify fragments that have integrated the dsODN tag.
- Perform high-throughput sequencing (e.g., Illumina MiSeq) on the amplified products.
- Data Analysis: Map the sequenced reads to the reference genome. Sites of Cas9 cleavage are identified by the presence of the integrated dsODN tag and microhomology sequences. Compare the list of detected off-target sites to the in silico predictions.
3. Alternative: Cell-Free CIRCLE-seq:
- This is a highly sensitive, in vitro method that uses purified genomic DNA [72].
- Procedure: Isolate gDNA from control cells and shear it into fragments.
- The DNA is then circularized and treated with Cas9-gRNA complex in a test tube.
- Cas9 cleaves its target sites, linearizing the circular DNA at those positions.
- The linearized fragments are purified and sequenced.
- Data Analysis: Map the sequenced fragments to the reference genome to identify all sites cleaved by Cas9-gRNA. This provides a highly sensitive, albeit potentially over-inclusive, list of potential off-target sites without the constraints of cellular chromatin.
Protocol: Validating On-Target Knockdown and Immune Profiling
This protocol confirms successful SOX9 knockdown and assesses its functional impact on the immune microenvironment.
1. On-Target Efficiency Validation:
- Quantitative PCR (qPCR): 72 hours post-transfection, extract total RNA from control and treated cells, synthesize cDNA, and perform qPCR using primers specific for SOX9. Normalize expression to a housekeeping gene (e.g., GAPDH, ACTB). Expect >70% knockdown of SOX9 mRNA.
- Western Blotting: Lyse cells and quantify protein concentration. Separate proteins by SDS-PAGE, transfer to a membrane, and probe with anti-SOX9 and anti-β-Actin (loading control) antibodies. Confirm knockdown at the protein level.
2. Immune Profiling via Flow Cytometry:
- Cell Surface Staining: For in vivo studies, harvest tumors from a syngeneic mouse model after therapeutic intervention. Create a single-cell suspension and stain with a panel of fluorescently conjugated antibodies.
- Key Immune Panel:
- Myeloid Cells: CD11b, F4/80, CD206 (M2-like TAMs), MHC-II (antigen presentation).
- Lymphoid Cells: CD3, CD8 (Cytotoxic T cells), CD4, FoxP3 (Regulatory T cells), NK1.1 (Natural Killer cells).
- Analysis: Acquire data on a flow cytometer and analyze the frequency and, if possible, the activation state (e.g., cytokine production) of each immune population. Successful SOX9 knockdown should correlate with a decrease in immunosuppressive cells (Tregs, M2-TAMs) and an increase in cytotoxic cells (CD8+ T cells, NK cells) [44] [14].
The Scientist's Toolkit: Research Reagent Solutions
Table 1: Essential reagents and tools for validating SOX9 knockdown specificity and immune activation.
| Item | Function/Description | Example/Note |
|---|---|---|
| High-Fidelity Cas9 | Engineered Cas9 variants with reduced off-target activity while maintaining high on-target efficiency. | HiFi Cas9, eSpCas9, SpCas9-HF1 [72]. |
| Cas9 Nickase | A Cas9 that cuts only one DNA strand; using two paired nickases increases specificity. | Requires two adjacent gRNAs for a double-strand break [72]. |
| Ribonucleoprotein (RNP) | Pre-complexed Cas9 protein and gRNA. Reduces off-target effects by shortening exposure time. | Therapeutically relevant formulation; preferred over plasmid DNA delivery [73] [72]. |
| Truncated gRNA (tru-gRNA) | gRNA with shortened guide sequence (17-18 nt). Increases specificity by tolerating fewer mismatches. | Can reduce off-target effects but may also lower on-target efficiency [72]. |
| GUIDE-seq Kit | An unbiased, cell-based method for genome-wide detection of off-target double-strand breaks. | Integrated DNA Technologies (commercial source available) [72]. |
| CIRCLE-seq | A highly sensitive, cell-free, biochemical method for comprehensive off-target identification. | Protocol detailed in [72]. |
| Anti-SOX9 Antibody | For validation of SOX9 protein knockdown via Western Blot or Immunohistochemistry. | Multiple commercial suppliers (e.g., Cell Signaling Technology, Abcam). |
| Immune Cell Staining Panel | Fluorescently labeled antibodies for flow cytometry analysis of tumor immune infiltration. | Should include markers for T cells (CD3, CD8), TAMs (CD11b, F4/80, CD206), and NK cells [44] [14]. |
Table 2: Comparison of Major Off-Target Detection Methods. This table summarizes the core techniques for identifying unintended CRISPR edits, aiding in the selection of an appropriate experimental strategy [72].
| Method | Principle | Detection Type | Key Advantage | Key Limitation |
|---|---|---|---|---|
| In Silico (e.g., Cas-OFFinder) | Computational alignment of gRNA to a reference genome. | Biased/Predictive | Fast, inexpensive, guides initial gRNA design. | Does not account for cellular context (e.g., chromatin state). |
| GUIDE-seq | Captures double-strand breaks via integration of a dsODN tag in living cells. | Unbiased/Cell-Based | Genome-wide, works in a cellular context. | Requires efficient delivery of the dsODN tag; lower sensitivity than cell-free methods. |
| CIRCLE-seq | Cas9 cleavage of circularized genomic DNA in a test tube. | Unbiased/In Vitro | Extremely high sensitivity, no delivery barriers. | Lacks cellular context (e.g., chromatin, nuclear transport), may yield false positives. |
| SITE-seq | Cas9 cleavage of sheared genomic DNA followed by sequencing of cleavage sites. | Unbiased/In Vitro | Sensitive, uses biotinylated gRNA for complex purification. | Lacks cellular context. |
Table 3: Key Immune Cell Correlates of SOX9 Activity in Lung Adenocarcinoma. This table outlines expected changes in tumor immune infiltration upon successful SOX9 knockdown, based on findings from murine and human studies [4] [44] [14].
| Immune Cell Type | Change with High SOX9 | Functional Consequence | Validation Method |
|---|---|---|---|
| CD8+ T Cells | ↓ Infiltration & Function | Reduced tumor cell killing, immune escape. | Flow Cytometry, IF/IHC |
| Natural Killer (NK) Cells | ↓ Infiltration & Activity | Diminished innate immune surveillance. | Flow Cytometry, Functional Assay |
| M2-like TAMs | ↑ Infiltration & Activity | Increased TGF-β secretion, promotes EMT and metastasis. | Flow Cytometry (CD206), IF/IHC |
| Regulatory T Cells (Tregs) | ↑ Infiltration | Enhanced immunosuppressive microenvironment. | Flow Cytometry (FoxP3+) |
| Dendritic Cells (DCs) | ↓ Infiltration & Function | Impaired antigen presentation and T cell priming. | Flow Cytometry, scRNA-seq |
Assessing Cell Viability and Phenotypic Stability Post-Knockdown
The SRY-related high-mobility group box gene 9 (SOX9) is a transcription factor increasingly recognized for its pivotal role in cancer progression and therapy resistance. While its functions have been studied in various cancer cell types, emerging evidence indicates that SOX9 also plays a critical role in mediating the behavior of immune cells within the tumor microenvironment, particularly tumor-associated macrophages (TAMs). TAMs constitute essential components of the tumor microenvironment, with M2-like TAMs being particularly important in facilitating tumor metastasis and augmenting tumor drug resistance [74]. Assessing cellular responses following SOX9 knockdown requires robust methodologies for evaluating both viability and phenotypic markers, which provides critical insights into the molecular mechanisms driving cancer progression and therapeutic resistance.
This application note provides a standardized framework for evaluating the functional consequences of SOX9 knockdown, with particular emphasis on protocols relevant to TAM research. The procedures outlined herein enable researchers to quantitatively assess how SOX9 suppression impacts fundamental cellular processes including viability, proliferation, and phenotypic stability—methodologies that are directly applicable to investigations of TAM polarization and function within the tumor microenvironment.
Key Assays for Post-Knockdown Assessment
Quantitative Assessment of Cellular Responses
Comprehensive evaluation of SOX9 knockdown effects requires multiple complementary assays that capture different aspects of cellular behavior. The table below summarizes the core quantitative measurements essential for characterizing post-knockdown phenotypes:
Table 1: Core Assays for Assessing Cellular Responses Post-SOX9 Knockdown
| Assessment Type | Specific Assay | Measured Parameters | Key Findings from Literature |
|---|---|---|---|
| Viability & Proliferation | MTT Assay [27] | Absorbance at 570nm with 630nm reference; IC50 values | SOX9 knockdown increased cellular sensitivity to chemotherapeutics (gemcitabine, cisplatin, paclitaxel, etoposide) [25] [27] |
| EdU Incorporation Assay [35] | Percentage of EdU-positive nuclei; fluorescence intensity | USP18/SOX9 axis knockdown significantly reduced nuclear EdU incorporation in glioma cells [35] | |
| Clonogenic Potential | Colony Formation Assay [25] | Number of colonies formed; colony size distribution | SOX9 knockdown significantly reduced colony formation after chemotherapeutic exposure [25] |
| Stemness Properties | Tumor Sphere Formation [25] [35] | Primary and secondary sphere numbers; sphere diameter | SOX9 knockdown substantially reduced tumor sphere formation capacity and self-renewal [25] |
| Limiting Dilution Assay [35] | Stem cell frequency; confidence intervals | USP18/SOX9 silencing dramatically reduced tumorsphere formation frequency [35] | |
| Phenotypic Markers | Western Blot Analysis [25] [35] | Protein levels of stemness biomarkers (CD133, Nestin, SOX2, NANOG) | SOX9 knockdown downregulated cancer stem cell markers [35] and ALDH1A1 expression [25] |
| Aldefluor Assay [25] | ALDH enzymatic activity by flow cytometry | SOX9 overexpression elevated ALDH activity, a key cancer stem cell mechanism [25] |
Phenotypic Stability Assessment
Beyond basic viability metrics, evaluating the stability of specific cellular phenotypes following SOX9 knockdown is particularly crucial in TAM research. The polarization state of macrophages significantly influences their function within the tumor microenvironment. The following table outlines key phenotypic markers for characterizing macrophage polarization states:
Table 2: Essential Markers for Assessing Macrophage Phenotypic Stability
| Phenotype | Surface Markers | Secreted Factors/Cytokines | Functional Characteristics |
|---|---|---|---|
| M1-like TAMs [75] [74] | CD86, CD60, CD80, MHC II | TNF-α, IL-1β, IL-6, IL-12, IL-23, CXCL9, CXCL10 | Pro-inflammatory; antitumor effects; strong antigen presentation; promotes Th1-type immune responses |
| M2-like TAMs [75] [74] | CD163, CD206, CD200R, CD209, CD301 | CCL17, CCL18, CCL22, IL-10, TGF-β | Anti-inflammatory; pro-tumoral; promotes tissue repair, angiogenesis, and Th2-type immune responses |
The M1/M2 ratio has emerged as a biologically relevant indicator for prognosticating cancer outcomes, with a higher ratio generally signifying a more favorable prognosis [75]. This metric can be applied to assess how SOX9 knockdown in TAMs influences the overall polarization balance within the tumor microenvironment.
Detailed Experimental Protocols
Cell Viability Assessment via MTT Assay
Purpose: To quantitatively measure metabolic activity as an indicator of cell viability following SOX9 knockdown, particularly in the context of chemotherapeutic challenge.
Materials:
- Cell lines (primary macrophages or relevant macrophage cell models)
- SOX9 knockdown constructs (siRNA or shRNA)
- Chemotherapeutic agents (e.g., gemcitabine, cisplatin)
- MTT reagent (5 mg/mL in PBS)
- Solvent solution (10% SDS, DMSO, acetate acid)
- 96-well tissue culture plates
- Microplate reader
Procedure:
- Seed cells in 96-well plates at a density of 1.5×10⁵ cells per well in complete growth medium.
- Transfert cells with SOX9-targeting siRNA using RNAiMAX transfection reagent according to manufacturer's protocol.
- For controls, use non-targeting scramble siRNA.
- At 48 hours post-transfection, treat cells with a concentration gradient of chemotherapeutic agents.
- Incubate for an additional 48 hours under standard culture conditions.
- Add 10 μL of MTT reagent (5 mg/mL) to each well and incubate for 5 hours at 37°C.
- Carefully remove supernatant and add 100 μL of solvent solution (40 μL 10% SDS, 40 μL DMSO, 20 μL 1.2% acetate acid in PBS).
- Incubate overnight in the dark and measure absorbance at 570 nm with a reference wavelength of 630 nm.
- Calculate cell viability as percentage relative to untreated controls and determine IC50 values using appropriate software.
Technical Notes: The MTT assay provides a quantitative measure of metabolic activity that correlates with viable cell number. For TAM studies, ensure polarization is induced and maintained throughout the assay duration using appropriate cytokines (IFN-γ + LPS for M1; IL-4 + IL-13 for M2) [75] [74].
Clonogenic Survival Assay
Purpose: To evaluate long-term cell survival and reproductive potential after SOX9 knockdown and chemotherapeutic exposure.
Materials:
- 6-well tissue culture plates
- Crystal violet staining solution (0.5% w/v in methanol)
- Methanol
- Acetic acid
Procedure:
- After SOX9 knockdown and chemotherapeutic exposure (e.g., 2-day cisplatin treatment), allow cells to recover in drug-free medium for 4 days.
- Trypsinize, count, and plate cells at very low density (200-1000 cells/well depending on cell type) in 6-well plates.
- Incubate for 10-14 days to allow colony formation, refreshing medium every 3-4 days.
- Once visible colonies form, remove medium, wash with PBS, and fix cells with methanol for 10 minutes.
- Stain with crystal violet solution for 30 minutes, then gently rinse with tap water.
- Air dry plates and count colonies manually or using automated colony counting software.
- Normalize colony counts from treated cells to untreated controls to account for any initial differences in colony formation caused by SOX9 knockdown.
Technical Notes: This assay is particularly valuable for assessing the effect of SOX9 on cancer stem cell populations, as only cells with retained self-renewal capacity will form colonies [25].
Tumor Sphere Formation Assay
Purpose: To evaluate self-renewal and stemness properties after SOX9 manipulation under stem cell-selective conditions.
Materials:
- Ultra-low attachment plates
- Serum-free sphere formation medium (DMEM/F12 supplemented with B27, EGF, bFGF)
- Accutase or trypsin for sphere dissociation
Procedure:
- After SOX9 knockdown, harvest cells and plate as single cells in serum-free sphere formation medium in ultra-low attachment plates.
- Plate at densities ranging from 1,000 to 10,000 cells/mL depending on cell type.
- Culture for 7-14 days, monitoring sphere formation regularly.
- Count primary spheres >50 μm in diameter using an inverted microscope.
- For secondary sphere formation, collect primary spheres, centrifuge gently, and dissociate to single cells using Accutase.
- Replate dissociated cells at the same densities and repeat the counting process.
- For drug sensitivity assessment under stem cell conditions, include chemotherapeutic agents in the sphere formation medium and normalize results to untreated controls.
Technical Notes: The sphere formation assay directly evaluates self-renewal capacity, a key property of cancer stem cells. SOX9 has been demonstrated to positively regulate sphere formation in multiple cancer types, including non-small cell lung cancer and glioblastoma [25] [35].
Flow Cytometric Analysis of Macrophage Polarization
Purpose: To quantitatively assess the impact of SOX9 knockdown on macrophage polarization states using surface marker expression.
Materials:
- Fluorescently conjugated antibodies against CD86 (M1 marker) and CD206 (M2 marker)
- Flow cytometry staining buffer (PBS with 1% BSA)
- Fixation buffer
- Flow cytometer with appropriate lasers and filters
Procedure:
- Differentiate primary human monocytes to macrophages using M-CSF (50 ng/mL) for 6 days.
- Polarize macrophages to M1 phenotype (IFN-γ 20 ng/mL + LPS 100 ng/mL) or M2 phenotype (IL-4 20 ng/mL + IL-13 20 ng/mL) for 48 hours.
- Perform SOX9 knockdown during polarization using appropriate siRNA or shRNA approaches.
- Harvest macrophages using gentle scraping and wash with cold flow cytometry buffer.
- Incubate cells with Fc receptor blocking solution for 10 minutes to prevent non-specific binding.
- Stain with fluorescently conjugated antibodies against CD86 and CD206 for 30 minutes at 4°C in the dark.
- Include appropriate isotype controls for compensation and gating.
- Wash cells twice, resuspend in staining buffer, and analyze using a flow cytometer.
- Calculate M1/M2 ratio based on percentage of CD86+ (M1) versus CD206+ (M2) cells.
Technical Notes: The M1/M2 ratio serves as a clinically relevant parameter, with higher ratios generally associated with better prognosis in multiple cancer types [75]. SOX9 knockdown effects on this ratio can provide insights into its role in modulating the tumor immune microenvironment.
Signaling Mechanisms and Workflow
SOX9-Associated Signaling Pathways
The diagram below illustrates the key molecular mechanisms through which SOX9 influences cell viability and phenotypic stability, particularly in the context of therapy resistance:
Figure 1: SOX9 Signaling in Cell Survival and Therapy Resistance. SOX9 activation occurs through AMPK signaling leading to nuclear translocation, where it transcriptionally regulates STAT3 and ALDH1A1 to promote stemness, viability, and chemoresistance [64] [25].
Experimental Workflow for Post-Knockdown Assessment
The following diagram outlines a comprehensive workflow for assessing cell viability and phenotypic stability following SOX9 knockdown:
Figure 2: Experimental Workflow for Post-Knockdown Assessment. Comprehensive workflow integrating SOX9 knockdown with functional assessments of viability, phenotype, and stemness properties.
Research Reagent Solutions
Table 3: Essential Research Reagents for SOX9 Knockdown Studies
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| SOX9 Targeting | SOX9 siRNA (Dharmacon M-021507-00) [27] | Transient SOX9 knockdown; mechanistic studies | Transfert with RNAiMAX; assess knockdown 48-60 hours post-transfection |
| LV-shSOX9 lentivirus [64] | Stable SOX9 knockdown; long-term studies | Use at 1×10¹² TU/mL; apply in 30% F127 Pluronic gel for in vivo approaches | |
| Polarization Inducers | IFN-γ (20 ng/mL) + LPS (100 ng/mL) [74] | M1 macrophage polarization | 48-hour treatment typically sufficient for polarization |
| IL-4 (20 ng/mL) + IL-13 (20 ng/mL) [74] | M2 macrophage polarization | Confirm with CD206 and CD163 expression | |
| Viability Assays | MTT reagent [27] | Metabolic activity measurement | 5-hour incubation required for formazan crystal formation |
| EdU incorporation kit [35] | DNA synthesis and proliferation | More precise than MTT for proliferation-specific assessment | |
| Phenotypic Markers | Anti-CD86, Anti-CD80 antibodies [74] | M1 macrophage characterization | Use with flow cytometry or immunofluorescence |
| Anti-CD163, Anti-CD206 antibodies [75] [74] | M2 macrophage characterization | IHC preferred for spatial context in tissue sections | |
| Stemness Assays | Aldefluor assay kit [25] | ALDH enzymatic activity measurement | Flow cytometry-based; requires specific inhibitor controls |
| Ultra-low attachment plates [25] | Tumor sphere formation | Prevents cell adhesion forcing growth in suspension |
The methodologies outlined in this application note provide a comprehensive framework for assessing cell viability and phenotypic stability following SOX9 knockdown. The integrated approach combining viability assays, clonogenic assessment, and phenotypic characterization enables researchers to obtain a multidimensional understanding of SOX9 function in relevant cellular models, including tumor-associated macrophages.
The central role of SOX9 in mediating therapy resistance through multiple mechanisms—including STAT3 activation [64], ALDH1A1 regulation [25], and stemness maintenance [35]—makes it a compelling target for investigative studies and potential therapeutic development. The consistent association between SOX9 expression and poor patient outcomes across multiple cancer types [76] [27] further underscores the importance of robust experimental approaches for studying its function.
By implementing these standardized protocols, researchers can generate comparable, reproducible data that advances our understanding of SOX9 in the tumor microenvironment and contributes to the development of novel therapeutic strategies targeting this key transcriptional regulator.
Ensuring Consistent M2-Polarization During Experimental Workflow
Within the context of tumor immunology and SOX9 knockdown research, achieving consistent and reproducible polarization of tumor-associated macrophages (TAMs) toward the M2-like phenotype is a critical methodological cornerstone. M2 TAMs, typically characterized as anti-inflammatory and pro-tumorigenic, play a significant role in shaping the tumor microenvironment (TME) by promoting tumor progression, metastasis, and immune suppression [5] [77]. Their high plasticity allows them to alter their phenotype in response to microenvironmental cues, making standardized induction protocols essential for reliable research outcomes, particularly when investigating the functional consequences of specific gene knockdowns like SOX9 [78] [77]. This application note provides a detailed, standardized protocol for the induction of M2-like macrophages from bone marrow precursors and outlines its integration into studies focusing on the TGF-β/SOX9 axis in cancer metastasis.
The Critical Role of M2 TAMs and SOX9 in Cancer
TAMs are among the most abundant immune cells in the TME. They exist on a dynamic spectrum, with M1-like (pro-inflammatory) and M2-like (immunosuppressive) phenotypes representing two ends of this continuum [77]. In advanced cancer stages, M2 TAMs predominate and are associated with poor prognosis in multiple cancer types, including non-small cell lung cancer (NSCLC) [5]. These cells facilitate tumor growth and metastasis through various mechanisms, including the secretion of factors like Transforming Growth Factor-beta (TGF-β) [5].
The transcription factor SOX9 has been identified as a key mediator in TAM-driven tumor metastasis. Clinical evidence shows a positive correlation between high densities of CD163+ M2 TAMs and elevated SOX9 expression in human NSCLC tissues, a combination linked to significantly shorter overall and disease-free survival in patients [5]. Mechanistically, TGF-β secreted by M2 TAMs upregulates SOX9 expression in lung cancer cells via the C-jun/SMAD3 pathway, which in turn promotes an Epithelial-to-Mesenchymal Transition (EMT)-like phenotype, enhancing tumor cell migration and invasion [5]. Consequently, the TGF-β/SOX9 axis represents a promising therapeutic target, the study of which relies on robust and consistent models of M2 macrophage polarization.
A Generalized Protocol for High-Efficiency M2-like Macrophage Induction
This section details a validated, high-yield protocol for generating M2-like macrophages from the bone marrow mononuclear cells (BMNCs) of mice and rats, optimized for reliability and cross-species applicability [78].
Research Reagent Solutions
Table 1: Essential reagents for BMNC isolation and M2 polarization.
| Item | Manufacturer (Example) | Catalog Number (Example) | Function |
|---|---|---|---|
| Recombinant Murine M-CSF | Peprotech | 315-02 | Drives differentiation of BMNCs into naive M0 macrophages. |
| Recombinant Murine IL-4 | Peprotech | 214-14 | Key cytokine for polarizing M0 macrophages toward the M2 phenotype. |
| Histopaque-1083 | Sigma-Aldrich | 10831 | Density gradient medium for isolating mononuclear cells from bone marrow. |
| DMEM (High Glucose) | Nacalai Tesque | 08458-45 | Base cell culture medium. |
| Fetal Calf Serum (FCS) | - | - | Supplement for cell culture medium. |
| Antibiotics (e.g., Penicillin/Streptomycin) | - | - | Prevents bacterial contamination in culture. |
| Trypan Blue | - | - | Dye for assessing cell viability and counting. |
Step-by-Step Workflow
Step 1: Bone Excision (20-30 minutes) Euthanize a 6-10 week-old mouse (e.g., C57BL/6J) following institutional guidelines [78] [79]. Immerse the body in 70% ethanol for 5 minutes for sterilization. In a biosafety cabinet, secure the animal in a supine position and make a precise skin incision from the ankle to the hip joint to expose and carefully detach the femur and tibia from both hind legs. Remove all soft tissue using sterile forceps and scissors. Sequentially place the cleaned bones in 70% ethanol (5 min), cold PBS (cPBS, 5 min), and cold DMEM (5 min) to ensure sterility. Store bones on ice if not processed immediately [78].
Step 2: BMNCs Isolation (60-90 minutes) Transfer bones to a Petri dish with cPBS. Cut off the bone epiphyses and flush the marrow from the shafts using a syringe filled with culture medium or PBS and a 23G needle [79]. Flush until the bone turns white. Pool the marrow from all bones and use a needle to break up any clumps. Strain the cell suspension through a 70 μm cell strainer into a 50 mL tube. Centrifuge the suspension at 190 x g for 10 minutes. Aspirate the supernatant and resuspend the pellet in 4 mL of ACK lysis buffer for 5 minutes at room temperature to lyse red blood cells. Add 4 mL of culture medium to neutralize and centrifuge at 1300 x g for 10 minutes. Aspirate the supernatant, resuspend the pellet in a small volume of medium, and count the cells using a cell counter with Trypan Blue to assess viability [78].
Step 3: M0 Macrophage Differentiation Plate the isolated BMNCs at a density of 1 x 10^6 cells per 10 cm culture dish in RPMI-1640 medium supplemented with 10% FCS, 1% antibiotics, and 10 ng/mL Macrophage Colony-Stimulating Factor (M-CSF) [78] [79]. Place the plates in a 37°C, 5% CO2 incubator. On day 3, gently add 5 mL of fresh medium containing 10 ng/mL M-CSF. By day 7, the BMNCs will have differentiated into naive, non-activated M0 macrophages, which are ready for polarization [79]. The resulting cells should be >95% positive for the macrophage markers CD11b and F4/80, as determined by flow cytometry [79].
Step 4: M2 Polarization To polarize the M0 macrophages towards an M2-like phenotype, stimulate the cells with recombinant Interleukin-4 (IL-4) for 48-72 hours [78] [79]. The typical concentration range for murine IL-4 is 10-20 ng/mL. This stimulation induces the expression of characteristic M2 markers.
Phenotypic Validation of M2-like Macrophages
Table 2: Key markers for validating M2-like macrophage polarization.
| Marker Category | Marker | Expression in M2 | Method of Detection |
|---|---|---|---|
| Surface Receptor | CD206 (MMR) | Upregulated | Flow Cytometry [78] |
| Surface Receptor | CD163 | Upregulated | Flow Cytometry, IHC [5] |
| Secreted Cytokine | IL-10 | Upregulated | ELISA, RT-qPCR [5] |
| Secreted Cytokine | TGF-β | Upregulated | ELISA, RT-qPCR [5] |
| Metabolic Enzyme | Argınase-1 (Arg-1) | Upregulated | RT-qPCR, Western Blot [78] |
Integrating M2 Polarization with SOX9 Knockdown Research
The standardized M2 polarization protocol serves as a critical foundation for investigating the TAM-driven TGF-β/SOX9 axis in cancer. The experimental logic for integrating these components is outlined below.
Application Workflow:
- Generate Conditioned Medium: Culture polarized M2 macrophages (as per Section 3) and collect the supernatant (conditioned medium), which is rich in secreted factors like TGF-β [5].
- Stimulate Cancer Cells: Treat human lung adenocarcinoma cells (e.g., A549, H1299) with this M2-conditioned medium or co-culture them directly with the M2 macrophages.
- Induce SOX9 and EMT: The TGF-β secreted by M2 TAMs will activate the C-jun/SMAD3 pathway in the cancer cells, leading to upregulated SOX9 expression. This, in turn, induces an EMT-like phenotype, characterized by decreased E-cadherin and increased vimentin expression, resulting in enhanced tumor cell migration and invasion [5].
- Functional Validation with Knockdown: To confirm the specific role of SOX9, perform SOX9 knockdown in cancer cells using RNA interference (RNAi) prior to co-culture. SOX9 knockdown has been shown to inhibit the TGF-β-mediated EMT phenotype and significantly reduce tumor cell migration and invasion, even in the presence of M2 macrophages [5].
Troubleshooting and Key Considerations for Consistency
Table 3: Common challenges and solutions for consistent M2 polarization.
| Challenge | Potential Cause | Solution |
|---|---|---|
| Low M2 Marker Expression | Inadequate IL-4 concentration or duration. | Titrate IL-4 concentration (e.g., 10-20 ng/mL) and extend polarization time up to 72 hours. |
| Contamination | Non-sterile technique during bone isolation. | Ensure adequate ethanol sterilization steps and work in a certified biosafety cabinet. |
| Low Cell Yield | Inefficient bone marrow flushing or RBC lysis. | Flush bones thoroughly until white. Ensure correct ACK lysis buffer incubation time. |
| Unpolarized or Mixed Phenotype | Inconsistent M-CSF lot or serum quality. | Use high-quality, validated cytokine lots and test new serum batches for differentiation efficiency. |
| Cancer Cells Not Undergoing EMT | Low TGF-β secretion by M2 TAMs. | Validate TGF-β levels in conditioned medium via ELISA and ensure M2 polarization was successful. |
Additional Critical Factors:
- Cell Source and Species: This protocol is validated for mouse and rat BMNCs. Be aware that species-specific differences in cytokine responses exist [78].
- Cytokine Quality: Use high-purity, carrier-protein-free recombinant cytokines to ensure batch-to-batch consistency.
- 3R Principles: The protocol is designed to be efficient, obtaining high cell yields (up to 200% as reported) from a single animal to reduce the total number of animals used, aligning with the Replace, Reduce, Refine principles [78].
Validating Functional Outcomes: From Molecular Assays to Phenotypic Confirmation
Epithelial-mesenchymal transition (EMT) is a critical biological process that confers migratory and invasive properties to carcinoma cells, facilitating cancer metastasis [80]. During EMT, cells undergo a profound phenotypic shift, characterized by the downregulation of epithelial markers like E-cadherin and the upregulation of mesenchymal markers such as Vimentin [81]. The transcription factor SOX9 has been identified as a key regulator of this process within the tumor microenvironment, particularly in response to signals from tumor-associated macrophages (TAMs) [5] [6] [49]. These application notes detail the molecular validation protocols for assessing the downstream effects of SOX9 modulation on core EMT markers, providing a standardized framework for researchers investigating this prometastatic axis.
Molecular Mechanisms of SOX9 in EMT Regulation
TAMs, which often exhibit an M2-like, immunosuppressive phenotype, secrete a plethora of factors that shape the tumor microenvironment. Among these, Transforming Growth Factor-Beta (TGF-β) is a potent inducer of EMT [5] [81]. Research indicates that TGF-β secreted by TAMs upregulates SOX9 expression in cancer cells through the C-jun/SMAD3 signaling pathway [5]. Once expressed, SOX9 acts as a pivotal driver of the mesenchymal phenotype.
The functional role of SOX9 in EMT was conclusively demonstrated through knockdown experiments. In non-small cell lung cancer (NSCLC) cells, SOX9 knockdown inhibited the TGF-β-mediated EMT phenotype, preventing the characteristic changes in E-cadherin and Vimentin expression and reducing tumor cell migration and invasion [5]. Similar results were found in papillary thyroid cancer, where SOX9 knockdown inhibited the EMT process and suppressed cell invasion via the Wnt/β-catenin pathway [82]. Furthermore, in oral squamous cell carcinoma, TGF-β1 was shown to promote the nuclear translocation of SOX9, leading to increased N-cadherin expression, a key event in the "cadherin switch" during EMT [83].
Table 1: Key Experimental Findings Linking SOX9 to EMT Regulation
| Cancer Type | Experimental Manipulation | Effect on E-cadherin | Effect on Vimentin | Functional Outcome | Source |
|---|---|---|---|---|---|
| Non-Small Cell Lung Cancer (NSCLC) | SOX9 Knockdown | Increased | Decreased | Inhibition of EMT; reduced migration and invasion | [5] |
| Lung Squamous Cell Carcinoma (LUSC) | Co-culture with M2 TAMs | Decreased | Increased | Enhanced migration, invasion, and proliferation | [81] |
| Papillary Thyroid Cancer | SOX9 Knockdown | Increased | Decreased | Inhibition of EMT and cell invasion | [82] |
| Oral Squamous Cell Carcinoma | TGF-β1 Stimulation (SOX9-dependent) | Decreased | Not Reported | Promoted migratory activity via N-cadherin upregulation | [83] |
Knockdown of SOX9 consistently produces antitumor effects across multiple cancer models. The table below summarizes quantitative data from key functional assays performed after SOX9 inhibition, demonstrating its crucial role in driving proliferation, invasion, and EMT.
Table 2: Summary of Quantitative Functional Data from SOX9 Knockdown Experiments
| Assay Type | Cancer Cell Line | Key Quantitative Finding Post-SOX9 Knockdown | Implied Biological Function | |
|---|---|---|---|---|
| MTT Proliferation Assay | TPC-1 (Thyroid) | Significant inhibition of cell proliferation at 72h | SOX9 is pro-proliferative | [82] |
| MTT Proliferation Assay | BCPAP (Thyroid) | Significant inhibition of cell proliferation at 72h | SOX9 is pro-proliferative | [82] |
| Soft Agar Colony Formation | TPC-1 (Thyroid) | Number of colonies significantly reduced | SOX9 supports anchorage-independent growth | [82] |
| Soft Agar Colony Formation | BCPAP (Thyroid) | Number of colonies significantly reduced | SOX9 supports anchorage-independent growth | [82] |
| Transwell Migration Assay | TPC-1 (Thyroid) | Number of migrated cells significantly reduced | SOX9 promotes cell motility | [82] |
| Transwell Migration Assay | BCPAP (Thyroid) | Number of migrated cells significantly reduced | SOX9 promotes cell motility | [82] |
| Matrigel Invasion Assay | TPC-1 (Thyroid) | Number of invaded cells significantly reduced | SOX9 promotes invasive capacity | [82] |
| Matrigel Invasion Assay | BCPAP (Thyroid) | Number of invaded cells significantly reduced | SOX9 promotes invasive capacity | [82] |
Detailed Experimental Protocols
Protocol 1: Validating EMT Marker Expression via Western Blotting
This protocol is designed to detect protein-level changes in E-cadherin and Vimentin expression following SOX9 knockdown or stimulation with TAM-conditioned media.
Materials:
- RIPA Lysis Buffer (supplemented with protease and phosphatase inhibitors)
- Primary Antibodies: Mouse monoclonal anti-E-cadherin, anti-Vimentin, anti-N-cadherin, anti-SOX9, and anti-β-actin (loading control)
- Secondary Antibody: Peroxidase-conjugated goat anti-mouse IgG
- Precast SDS-PAGE Gels (4-20% gradient)
- Nitrocellulose or PVDF Membranes
- Chemiluminescence Detection Kit
Methodology:
- Cell Treatment and Lysis: Culture cancer cells (e.g., A549, H1299 for NSCLC [5] or H226 for LUSC [81]). Perform SOX9 knockdown via siRNA transfection or treat cells with TAM-conditioned media/TGF-β1 (10 ng/mL) for 24-48 hours. Harvest cells and lyse in RIPA buffer on ice.
- Protein Quantification and Separation: Determine protein concentration using a BCA assay. Load 20-30 µg of total protein per lane and separate by SDS-PAGE electrophoresis.
- Protein Transfer and Blocking: Transfer proteins from the gel to a nitrocellulose membrane. Block the membrane with 5% non-fat dry milk in TBST for 1 hour at room temperature.
- Antibody Incubation: Incubate the membrane with primary antibodies diluted in blocking buffer (1:1000) overnight at 4°C. Wash the membrane with TBST and incubate with the HRP-conjugated secondary antibody (1:3000) for 1 hour at room temperature.
- Detection and Analysis: Develop the membrane using a chemiluminescence substrate. Image the blots and quantify band intensities using densitometry software (e.g., ImageJ). Normalize E-cadherin and Vimentin levels to the β-actin loading control.
Protocol 2: Functional Analysis of Cell Invasion using Matrigel Transwell Assay
This protocol assesses the functional consequence of SOX9-mediated EMT on the invasive potential of cancer cells.
Materials:
- 24-well Transwell plates with 8.0 µm pore size inserts
- Matrigel Basement Membrane Matrix
- Serum-free medium and medium supplemented with 10% FBS as a chemoattractant
- Cell culture incubator maintained at 37°C and 5% CO₂
- Crystal Violet staining solution (0.1% w/v)
Methodology:
- Matrigel Coating: Thaw Matrigel on ice overnight. Dilute it in cold serum-free medium and coat the upper chamber of the Transwell insert with 50-100 µL of the solution (typically 1 mg/mL). Allow it to polymerize for 2 hours in a 37°C incubator.
- Cell Preparation: Harvest SOX9-knockdown or control cells. Resuspend 5.0 × 10⁴ to 1.0 × 10⁵ cells in 200 µL of serum-free medium and seed them into the upper chamber of the Matrigel-coated insert.
- Invasion Assay: Add 500 µL of medium containing 10% FBS to the lower chamber as a chemoattractant. Incubate the plate for 24-48 hours at 37°C with 5% CO₂.
- Staining and Quantification: After incubation, carefully remove non-invaded cells from the upper surface of the membrane with a cotton swab. Fix the cells that have invaded through the Matrigel and membrane by immersing the insert in 4% paraformaldehyde for 10 minutes. Stain with 0.1% crystal violet for 20 minutes, wash gently, and air dry.
- Image Acquisition and Analysis: Capture images of the stained membrane under a light microscope. Count the number of invaded cells in at least four random fields per insert. Perform experiments in triplicate for statistical analysis.
Signaling Pathway Visualization
The following diagram illustrates the primary signaling pathway by which TAMs promote EMT in cancer cells via the TGF-β/SOX9 axis, integrating key findings from the cited research.
Diagram Title: The TGF-β/SOX9 Axis in TAM-Induced EMT
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Investigating the TAM/SOX9/EMT Axis
| Reagent / Assay | Specific Example / Catalog Number | Primary Function in Protocol |
|---|---|---|
| SOX9 siRNA | Sequence: 5′-GCAGCGACGUCAUCUCCAAdTdT-3′ [82] | Knocking down SOX9 gene expression to validate its functional role. |
| TGF-β1 Recombinant Protein | Human TGF-β1 (PeproTech) [83] | Stimulating the TGF-β signaling pathway to induce SOX9 and EMT in vitro. |
| Anti-E-cadherin Antibody | Mouse monoclonal (e.g., Leica Biosystems #PA0387) [81] | Detecting loss of epithelial marker via Western Blot or IHC. |
| Anti-Vimentin Antibody | Mouse monoclonal (e.g., Leica Biosystems #NCL‐L‐VIM‐572) [81] | Detecting gain of mesenchymal marker via Western Blot or IHC. |
| Anti-SOX9 Antibody | Rabbit or mouse polyclonal (e.g., Santa Cruz Biotechnology) [82] | Confirming SOX9 protein expression and nuclear localization. |
| Matrigel Invasion Assay | Corning BioCoat Matrigel Invasion Chamber | Quantifying the invasive potential of cells following experimental manipulation. |
| TGF-β Receptor Inhibitor | Small molecule inhibitor (e.g., SB431542) | Blocking TGF-β signaling to confirm pathway specificity [5]. |
The molecular validation protocols outlined herein establish a clear and reproducible link between SOX9 activity and the regulation of core EMT markers. The consistent finding that SOX9 knockdown reverses the EMT phenotype—elevating E-cadherin, reducing Vimentin, and suppressing invasion—across multiple cancer types underscores its central role in TAM-facilitated metastasis [5] [82]. The TGF-β/SOX9 axis, therefore, represents a promising therapeutic target. The standardized methodologies for molecular and functional analysis presented in these application notes provide a critical toolkit for researchers aiming to dissect this pathway further and develop novel anti-metastatic strategies.
Functional assays that quantify cell migration and invasion are fundamental to cancer research, particularly in studies investigating potential therapeutic targets. This application note details standardized protocols for measuring changes in these critical phenotypic behaviors, framed within the context of research on SOX9 knockdown in tumor-associated macrophages (TAMs). The transcription factor SOX9 is increasingly recognized as a key regulator of tumor progression and metastasis. Recent studies demonstrate that TAMs secrete factors like TGF-β, which upregulates SOX9 expression in cancer cells, promoting epithelial-to-mesenchymal transition (EMT) and enhancing migratory and invasive capabilities [5]. This document provides detailed methodologies and data analysis techniques to consistently quantify these phenotypic changes, enabling the evaluation of therapeutic strategies targeting the TAM-SOX9 axis.
Background and Significance
The TAM-SOX9 Axis in Cancer Progression
The tumor microenvironment (TME) is a critical regulator of cancer metastasis. Within the TME, tumor-associated macrophages (TAMs), which predominantly exhibit an M2 immunosuppressive phenotype, facilitate cancer progression by secreting various cytokines and growth factors [5]. Notably, TAM-derived transforming growth factor-beta (TGF-β) has been identified as a key molecular driver that increases SOX9 expression in cancer cells through the C-jun/SMAD3 pathway [5].
SOX9, a transcription factor, subsequently induces EMT—a fundamental process in metastasis where cells lose epithelial characteristics and gain mesenchymal properties, leading to enhanced motility and invasiveness [5] [84]. Clinical evidence strongly supports this relationship; in non-small cell lung cancer (NSCLC) tissues, a positive correlation exists between TAM density and SOX9 expression, and patients with high co-expression of both markers experience significantly shorter overall and disease-free survival [5]. SOX9's pro-metastatic role extends beyond lung cancer, with documented involvement in glioblastoma stem cell maintenance and colorectal cancer progression [35] [85].
Functional Assays as Readouts for Molecular Interventions
Functional assays provide direct, quantitative measurements of metastatic potential. Knockdown of SOX9 in cancer cells co-cultured with macrophages results in almost complete inhibition of EMT, reduced migration, and decreased invasion, demonstrating that TGF-β-mediated effects are SOX9-dependent [5]. Therefore, assays measuring migration and invasion serve as crucial functional readouts for evaluating the efficacy of targeting the TAM-SOX9 axis. This note standardizes these assays to ensure consistent, reliable data generation across different research settings.
Quantitative Profiling of Cancer Cell Aggression
Different functional metrics capture complementary aspects of metastatic potential. Research comparing three pairs of epithelial cancer cell lines (breast, endometrial, tongue) has quantified two key functional metrics: wound closure migration velocity (relating to local invasion) and cell detachment (relating to intravasation potential) [86].
Table 1: Functional Metrics of Cancer Cell Aggression Across Cell Lines
| Cell Line | Tissue Origin | Metastatic Potential | Wound Closure Migration Velocity | Cell Detachment (at 6 dynes/cm²) |
|---|---|---|---|---|
| MCF-7 | Breast | Low | Higher relative to its detachment | Low ( ~20%) |
| MDA-MB-231 | Breast | High | High | High ( ~80%) |
| Ishikawa | Endometrium | Low | Higher relative to its detachment | Low |
| KLE | Endometrium | High | Lower relative to its detachment | High |
| Cal-27 | Tongue | Low | Higher relative to its detachment | Low |
| SCC-25 | Tongue | High | Lower relative to its detachment | High |
Data adapted from Mehanna et al., 2025 [86].
The data reveals that relying on a single functional metric can be insufficient for characterizing metastatic potential. For instance, while highly metastatic MDA-MB-231 cells exhibit high migration velocity, other highly metastatic lines (KLE, SCC-25) show a phenotype where detachment is the dominant characteristic over migration [86]. This underscores the importance of a multi-assay approach for a comprehensive functional assessment.
Experimental Protocols
This section provides detailed, step-by-step protocols for key functional assays.
Impedance-Based Real-Time Cell Migration Assay
The impedance-based assay uses systems like the Maestro Z Live-cell Analysis System (Axion Biosystems) to monitor cell migration in real-time without labels. This method is highly sensitive and can also measure cell proliferation and barrier integrity in the same experiment [87].
Table 2: Key Research Reagents for Impedance-Based Assays
| Item | Function/Description | Example |
|---|---|---|
| Live-cell Analysis System | Instrument applying AC current & measuring impedance to monitor cell behaviors in real-time. | Maestro Z System (Axion Biosystems) [87] |
| Electrode-Integrated Plates | Specialized multi-well plates with embedded electrodes for impedance measurement. | Axion Biosystems 96-well plates [87] |
| Leptin | Pro-inflammatory cytokine used as a stimulant to enhance cell migration and model TAM-like signaling. | Recombinant Human Leptin (Sigma-Aldrich) [87] |
Procedure:
- Cell Preparation: Seed appropriate cancer cells (e.g., MCF-7, HCC1806, MDA-MB-231) in a 96-well electrode plate at an optimized density (e.g., ( 5 \times 10^4 ) cells/well) to form a confluent monolayer [87].
- Baseline Measurement: Place the plate in the Maestro Z system and record the baseline impedance signal for several hours until stable.
- Wound Induction: Use the system's wound induction tool to create a uniform, cell-free zone in the monolayer. For manual systems, a sterile pipette tip can be used for scratching.
- Experimental Treatment: Add treatments or stimulants. For TAM/SOX9 studies, this could include:
- Real-Time Monitoring: Continuously monitor impedance for 24-48 hours. The system quantifies the increasing impedance as cells migrate and cover the electrodes.
- Data Analysis: Calculate the impedance-based migration rate or the time to 50% wound closure using the system's software.
Scratch (Wound Healing) Assay Protocol
A classic, accessible method to quantify 2D migration.
Procedure:
- Cell Seeding: Seed cells in a 12- or 24-well plate to reach 100% confluence within 24-48 hours.
- Scratching: Use a sterile 200 µL pipette tip to create a straight, uniform "scratch" through the cell monolayer. Gently wash the well with PBS to remove dislodged cells.
- Treatment & Imaging: Add fresh medium containing desired treatments. Immediately capture images at the 0-hour timepoint using a microscope with a marked stage for consistent location finding.
- Time-Lapse Imaging: Capture images at regular intervals (e.g., every 4-6 hours) for 24-48 hours.
- Data Analysis: Measure the cell-free area at each time point using image analysis software (e.g., ImageJ). Calculate the percentage of wound closure or migration velocity (e.g., µm/hour) [86].
Transwell Invasion Assay Protocol
This assay measures the ability of cells to degrade and invade through a basement membrane matrix, a closer mimic of in vivo invasion [84] [35].
Procedure:
- Matrix Coating: Thaw Matrigel on ice. Dilute with cold serum-free medium and coat the membrane of the upper chamber of a Transwell insert. Incubate at 37°C for 1-2 hours to allow gelling.
- Cell Preparation: Serum-starve cells for 24 hours. Harvest and resuspend in serum-free medium. Seed ( 5 \times 10^4 ) to ( 2.5 \times 10^5 ) cells into the Matrigel-coated upper chamber.
- Chemoattractant: Add medium containing 10% FBS or other chemoattractants to the lower chamber.
- Incubation: Incubate the plate for 24-48 hours at 37°C to allow cells to invade through the Matrigel.
- Staining and Counting: Remove non-invading cells from the upper chamber with a cotton swab. Fix the invaded cells on the lower membrane with 4% paraformaldehyde and stain with 0.1% crystal violet. Image multiple fields and count the number of invaded cells [84].
Signaling Pathways in SOX9-Mediated Metastasis
The following diagram illustrates the key molecular pathways connecting TAMs, SOX9, and increased cancer cell migration and invasion, as detailed in the protocols.
Figure 1: Signaling pathways in SOX9-mediated metastasis. This diagram synthesizes mechanisms by which Tumor-Associated Macrophages (TAMs) promote cancer cell migration and invasion via SOX9. TAM-secreted TGF-β activates the C-jun/SMAD3 pathway, which transcriptionally upregulates SOX9 expression [5]. Separately, the deubiquitinase USP18 stabilizes the SOX9 protein by preventing its degradation [35]. Elevated SOX9 levels drive metastasis by inducing Epithelial-to-Mesenchymal Transition (EMT) and activating the RAP1 signaling pathway, which collectively enhance cell motility and invasiveness [5] [84].
Data Analysis and Interpretation
Quantification and Normalization
- Impedance/Scratch Assay Data: Report results as Mean ± SEM from at least three independent experiments. Normalize migration rates to the control group (set at 100%).
- Transwell Invasion Data: Present as the mean number of invaded cells per field or normalized as a percentage of control. Statistical significance is typically determined using a Student's t-test (for two groups) or one-way ANOVA (for multiple groups) with ( p < 0.05 ) considered significant [84] [35].
Troubleshooting Common Issues
- High Variability in Scratch Assays: Ensure wound width is uniform across replicates by using specialized scratching tools.
- Low Invasion in Transwell Assays: Optimize Matrigel concentration and cell seeding number. Verify the activity of the matrix lot.
- Inconsistent Impedance Readings: Ensure electrodes are not scratched and cells are properly seeded to cover the electrode surface evenly.
The functional assays detailed herein—scratch/wound healing, Transwell invasion, and real-time impedance-based monitoring—provide robust, quantifiable methods for assessing the migratory and invasive phenotypes of cancer cells. When applied within the context of the TAM-SOX9 axis, these protocols enable researchers to rigorously validate the functional consequences of SOX9 knockdown and its role as a critical mediator of TAM-driven cancer progression. The consistent application of these standardized protocols will facilitate the comparison of findings across studies and accelerate the development of therapeutics targeting the tumor microenvironment and SOX9 signaling.
The tumor immune microenvironment (TIME) is a critical determinant of cancer progression and therapeutic response, with tumor-associated macrophages (TAMs) representing a major component that supports tumor growth, immune evasion, and metastasis [88] [89]. The transcription factor SOX9 (SRY-related HMG-box 9) has emerged as a significant regulator within this microenvironment, exhibiting context-dependent functions in tumor development and immunity [4]. In non-small cell lung cancer (NSCLC), TAM-secreted TGF-β has been shown to upregulate SOX9 expression in cancer cells through the C-jun/SMAD3 pathway, subsequently promoting epithelial-to-mesenchymal transition (EMT) and metastasis [5]. This protocol details a comprehensive methodology for analyzing changes in the secretome, specifically cytokine profiling, following SOX9 knockdown in TAMs. This approach enables researchers to identify SOX9-regulated secretory pathways in TAMs, potentially revealing novel mechanisms of tumor-stroma crosstalk and identifying therapeutic targets for disrupting protumorigenic signaling networks.
Biological Rationale and Significance
SOX9 in Tumor Immunology
SOX9 plays a complex, "double-edged sword" role in immunology, acting as both an oncogene and a regulator of immune function [4]. It demonstrates a strong association with immune cell infiltration across various cancers, showing negative correlation with anti-tumor immune cells like CD8+ T cells and NK cells, while positively correlating with protumorigenic elements including macrophages and neutrophils [4]. In glioblastoma, SOX9 expression correlates significantly with immune infiltration and checkpoint expression, indicating its involvement in the immunosuppressive tumor microenvironment [9].
TAM-Derived Factors and SOX9 Regulation
The interaction between TAMs and SOX9 represents a clinically relevant signaling axis. In the TME, TAMs often adopt an M2-like, immunosuppressive phenotype that supports tumor progression [89] [90]. Clinical evidence from NSCLC reveals a positive correlation between TAM density (CD163+ macrophages) and SOX9 expression in tumor cells, with co-expression associated with significantly worse patient outcomes [5]. This TAM-mediated SOX9 upregulation occurs primarily through TGF-β secretion, which activates the C-jun/SMAD3 pathway, establishing a feed-forward loop that promotes tumor malignancy [5].
Table 1: Key Cytokine Pathways in TAM-SOX9 Crosstalk
| Cytokine/Factor | Source | Target | Functional Outcome | Therapeutic Implications |
|---|---|---|---|---|
| TGF-β | M2 TAMs [5] | SOX9 in tumor cells | Promotes EMT, metastasis [5] | TGF-β inhibitors may disrupt SOX9 signaling |
| CCL2 | CSCs → TAMs [90] | CCR2 on monocytes | Recruits monocytes to TME [90] | CCR2 antagonists block TAM recruitment |
| IL-6 | TAMs → CSCs [90] | STAT3 in CSCs | Maintains cancer stemness [90] | IL-6/JAK/STAT3 inhibitors |
| CSF-1 | CSCs → TAMs [90] | CSF-1R on macrophages | Promotes TAM survival, polarization [90] | CSF-1R inhibitors deplete TAMs |
Figure 1: TAM-SOX9 Signaling Network in Tumor Progression. This diagram illustrates the feed-forward loop between TAM-derived TGF-β and SOX9 expression in tumor cells, driving EMT and cancer stemness while promoting further TAM recruitment.
Experimental Protocol
SOX9 Knockdown in Tumor-Associated Macrophages
Primary Human Macrophage Isolation and Polarization
- Monocyte Isolation: Isolate peripheral blood mononuclear cells (PBMCs) from healthy donor buffy coats using density gradient centrifugation with Histopaque-1077 [91]. Isolate CD14+ monocytes using magnetic-activated cell sorting (MACS) with anti-CD14 microbeads.
- Macrophage Differentiation: Culture CD14+ monocytes in RPMI-1640 medium supplemented with 10% FBS, 1% penicillin-streptomycin, and 50 ng/mL recombinant human M-CSF for 7 days to generate monocyte-derived macrophages.
- M2 Polarization: Polarize macrophages toward an M2-like TAM phenotype by treating with 20 ng/mL IL-4 and 20 ng/mL IL-13 for 48 hours [92]. Validate polarization by assessing CD206 and CD163 surface expression via flow cytometry.
SOX9 Knockdown Using RNA Interference
- siRNA Design: Design and validate at least three different SOX9-specific siRNA sequences targeting distinct regions of the SOX9 mRNA transcript. Include a non-targeting scrambled siRNA as a negative control.
- Transfection Protocol: Transfect M2-polarized macrophages using lipofectamine RNAiMAX transfection reagent. Use 50 nM siRNA concentration. Optimize transfection efficiency using a fluorescently-labeled control siRNA.
- Knockdown Validation:
- qRT-PCR: Harvest cells 48 hours post-transfection for RNA isolation. Analyze SOX9 mRNA expression using quantitative RT-PCR with the following primers: SOX9-F: 5'-AGTACCCGCATCTGCACAAC-3', SOX9-R: 5'-TACTCGTAATCGGGGTGGTC-3'. Normalize to GAPDH expression.
- Western Blotting: Harvest cells 72 hours post-transfection for protein analysis. Probe with anti-SOX9 antibody (1:1000 dilution) and anti-β-actin (1:5000) as loading control.
Table 2: SOX9 Knockdown Experimental Parameters
| Parameter | Specifications | Quality Control Measures |
|---|---|---|
| Macrophage Source | Primary human CD14+ monocytes | >95% CD14+ purity by flow cytometry |
| Polarization | 50 ng/mL M-CSF (7d) → 20 ng/mL IL-4 + IL-13 (48h) | Verify CD206+/CD163+ phenotype |
| siRNA Concentration | 50 nM SOX9-targeting siRNA | Include fluorescent control for efficiency |
| Transfection Reagent | Lipofectamine RNAiMAX | Optimize lipid:RNA ratio |
| Knockdown Timeline | 48h (mRNA), 72h (protein) | Include scrambled siRNA control |
| Validation | qRT-PCR, Western Blot | >70% knockdown efficiency required |
Secretome Collection and Cytokine Profiling
Conditioned Media Collection
- Serum-Free Conditioning: 72 hours post-transfection, wash SOX9-knockdown and control macrophages with PBS and culture in serum-free medium for 24 hours to eliminate serum protein contamination.
- Conditioned Media Collection: Collect conditioned media and centrifuge at 2000 × g for 10 minutes to remove cells and debris. Aliquot supernatant and store at -80°C until analysis.
Multiplex Cytokine Profiling
- Platform Selection: Utilize Luminex multiplex bead-based technology with a 15-plex human cytokine panel [91]. Recommended analytes: IL-1α, IL-1β, IL-2, IL-4, IL-6, IL-10, IL-12, IL-13, IL-17, IL-18, IL-23, TNF-α, IFN-γ, GM-CSF, and TGF-β.
- Assay Procedure:
- Prepare standards and quality controls following manufacturer specifications.
- Incubate conditioned media samples with antibody-conjugated magnetic beads for 2 hours at room temperature with shaking.
- Wash beads and incubate with biotinylated detection antibody for 1 hour.
- Add streptavidin-PE and incubate for 30 minutes.
- Resuspend beads in wash buffer and analyze on Luminex analyzer.
- Calculate cytokine concentrations from standard curves using xPONENT software.
- Data Normalization: Normalize cytokine concentrations to total cellular protein content from corresponding cell lysates, measured by BCA assay.
Figure 2: Experimental Workflow for Cytokine Profiling Post-SOX9 Knockdown. This diagram outlines the comprehensive protocol from macrophage differentiation and polarization through SOX9 knockdown, secretome collection, and cytokine analysis.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for SOX9-TAM Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Cell Isolation | CD14 MicroBeads, human | Positive selection of monocytes from PBMCs |
| Histopaque-1077 | Density gradient medium for PBMC isolation | |
| Macrophage Polarization | Recombinant Human M-CSF | Differentiation of monocytes to macrophages |
| Recombinant Human IL-4 & IL-13 | M2 polarization cytokines [92] | |
| Gene Knockdown | SOX9-specific siRNA | Target SOX9 expression in TAMs |
| Lipofectamine RNAiMAX | siRNA delivery into primary macrophages | |
| Cytokine Profiling | Luminex Discovery Assay | Multiplex cytokine quantification [91] |
| Luminex FlexMap 3D | Multiplex analysis instrument platform [91] | |
| Validation Assays | CD163, CD206 antibodies | M2 macrophage marker validation |
| SOX9 antibodies | Knockdown efficiency verification | |
| Pathway Inhibition TGF-β Receptor Inhibitor | Blocks TGF-β-mediated SOX9 upregulation [5] | |
| STAT3 Inhibitor | Disrupts IL-6-mediated signaling [90] |
Data Analysis and Interpretation
Statistical Analysis and Bioinformatics
- Differential Expression Analysis: Identify significantly altered cytokines in SOX9-knockdown conditioned media compared to controls using paired t-tests with Benjamini-Hochberg correction for multiple comparisons (FDR < 0.05).
- Pathway Analysis: Perform functional enrichment analysis of altered cytokine pathways using KEGG and Reactome databases. Utilize Metascape for integrated bioinformatics analysis of cytokine networks [9].
- Correlation with Clinical Data: Compare identified SOX9-regulated cytokines with clinical outcomes using publicly available datasets (e.g., TCGA) to assess prognostic significance.
Expected Outcomes and Interpretation
Based on existing literature, SOX9 knockdown in TAMs is anticipated to significantly alter secretion of key cytokines:
- Expected Downregulation: TGF-β, IL-10, CCL2, and CSF-1, consistent with disruption of protumorigenic signaling [5] [90].
- Expected Upregulation: potentially IL-12 and TNF-α, indicating possible shift toward M1-like phenotype [89].
- Validation Experiments: Confirm functional significance of altered secretome through migration/invasion assays with tumor cells cultured in SOX9-knockdown TAM conditioned media.
Technical Notes and Troubleshooting
Critical Optimization Parameters
- Primary Macrophage Viability: Maintain cell viability >90% throughout polarization and transfection procedures. Reduce siRNA concentration to 25 nM if cytotoxicity is observed.
- Serum-Free Conditioning: Limit serum-free conditioning period to 24 hours to prevent cellular stress while minimizing serum protein interference.
- Cytokine Stability: Process samples promptly and maintain consistent freeze-thaw cycles to preserve cytokine integrity.
Technical Validation
- Knockdown Efficiency: Include rescue experiments with SOX9 overexpression constructs to confirm specificity of observed effects.
- Multiplex Assay Quality Control: Ensure standard curve R-values >0.99 and recoveries of quality controls within 80-120%.
- Biological Replicates: Perform minimum of three independent experiments using macrophages from different donors to account for biological variability.
This detailed protocol provides a standardized methodology for investigating SOX9-regulated secretome changes in TAMs, enabling researchers to elucidate novel mechanisms of tumor-stroma crosstalk and identify potential therapeutic targets for cancer immunotherapy.
Within the context of oncology research, particularly in manipulating gene expression within the tumor microenvironment (TME), the selection of an appropriate gene-silencing technique is paramount. The knockdown of the SOX9 transcription factor, a key regulator in cancer progression and metastasis, serves as a critical objective, especially in studies focusing on its role in tumor-associated macrophages (TAMs) [5]. This application note provides a comparative analysis of two principal gene-silencing technologies—small interfering RNA (siRNA) and CRISPR/Cas9—evaluating their efficacy, durability, and practical application for SOX9 knockdown in TAM-related protocols. We summarize key quantitative data, provide detailed experimental methodologies, and outline essential reagents to guide researchers in selecting and implementing the optimal approach for their specific experimental needs in cancer biology and drug development.
The fundamental difference between these technologies lies in their operational level: siRNA mediates gene knockdown at the mRNA level, while CRISPR/Cas9 facilitates a permanent gene knockout at the DNA level [93]. Table 1 summarizes the core characteristics, advantages, and limitations of each system, providing a high-level guide for selection.
Table 1: Core Characteristics of siRNA and CRISPR/Cas9 Gene Silencing Technologies
| Feature | siRNA (Knockdown) | CRISPR/Cas9 (Knockout) |
|---|---|---|
| Mechanism of Action | Degrades target mRNA or stalls its translation via the RNA-induced silencing complex (RISC) [93] [94] | Creates double-strand breaks in DNA, leading to frameshift mutations and gene disruption via error-prone non-homologous end joining (NHEJ) [93] [95] |
| Target Level | Post-transcriptional (mRNA) [93] | Genomic (DNA) [93] |
| Durability | Transient (days to a week), dependent on cell division and siRNA stability [93] | Permanent, heritable to daughter cells [93] |
| Key Advantage | Studies essential genes without lethality; reversible effect; rapid onset [93] | Complete, permanent protein ablation; superior specificity with well-designed guides; versatile platform (KO, KI, editing) [93] [96] |
| Primary Challenge | High off-target effects due to seed-sequence interactions; transient nature requires re-dosing [93] | Off-target cleavage at similar DNA sites; delivery complexity, especially in vivo; lower efficiency in non-dividing cells [96] [95] |
| Therapeutic Delivery | Lipid nanoparticles (LNPs); advanced, bioengineered nanovesicles [97] [98] | Viral vectors (AAV, lentivirus); non-viral vectors (LNPs, extracellular vesicles) [99] [95] |
Quantitative Comparison of Efficacy and Durability
The practical implications of the mechanistic differences are evident in key performance metrics. Table 2 provides a structured comparison of efficacy, durability, and specificity, crucial for experimental planning.
Table 2: Quantitative and Functional Comparison for Experimental Design
| Parameter | siRNA | CRISPR/Cas9 |
|---|---|---|
| Onset of Action | Rapid (hours to 1-2 days) [93] | Slower (days to weeks); dependent on DSB repair and protein turnover [96] |
| Gene Silencing Efficiency | High (>70-90% protein reduction achievable) but can be variable [97] | Can be highly efficient, but varies by cell type, target locus, and delivery method [100] |
| Duration of Effect | Typically 3-7 days in dividing cells [93] | Permanent and stable; allows for creation of clonal knockout cell lines [100] |
| Specificity (Off-Target Effects) | Historically high; sequence-independent immune activation and seed-sequence-based off-targeting are concerns [93] | Generally higher; off-target effects are primarily sequence-dependent and can be minimized with optimized gRNA design [93] |
| Ideal Application | Functional studies of essential genes; acute/temporary inhibition; target validation [93] [5] | Generating stable knockout cell lines; investigating long-term consequences of gene loss; gene correction [100] |
A critical consideration is the cellular context. A 2025 study highlighted that CRISPR repair outcomes differ dramatically in nondividing cells, such as neurons and cardiomyocytes, compared to dividing cells [96]. In these postmitotic cells, indel accumulation from Cas9-induced breaks can take up to two weeks, significantly longer than in dividing cells, and the distribution of repair pathways favors nonhomologous end joining (NHEJ) over other mechanisms [96]. This is a vital consideration when working with primary TAMs, which are often non-dividing.
Application Note: SOX9 Knockdown in Tumor-Associated Macrophages
The TGF-β/SOX9 axis has been identified as a key pathway in TAM-driven tumor metastasis, particularly in non-small cell lung cancer (NSCLC) [5]. TAMs secrete TGF-β, which upregulates SOX9 expression in cancer cells, inducing an epithelial-to-mesenchymal transition (EMT)-like phenotype and promoting migration and invasion [5]. Silencing SOX9 is therefore a promising therapeutic strategy. Research has demonstrated that SOX9 knockdown via RNAi can inhibit this TGF-β-mediated EMT, reducing tumor cell migration and invasion [5]. Alternatively, CRISPR/Cas9-mediated SOX9 knockout in chondrosarcoma cells has been shown to reduce proliferation, clonogenicity, and migration while increasing apoptosis [100]. The choice between siRNA (for transient, acute inhibition) and CRISPR/Cas9 (for permanent, stable knockout) in TAM models depends on the specific biological question and experimental timeline.
Experimental Protocol 1: siRNA-Mediated SOX9 Knockdown
This protocol is adapted from established RNAi methodologies and reflects the use of advanced delivery systems [97].
- Objective: To achieve transient knockdown of SOX9 expression in macrophage or co-culture models.
- Key Reagents:
- SOX9-specific siRNA: A pool of synthetic siRNAs targeting human SOX9 mRNA and non-targeting (scrambled) siRNA control.
- Delivery Vehicle: Bioengineered nanovesicles (e.g., S-protein functionalized BNVs) [97] or commercial lipid nanoparticles (LNPs).
- Cell Model: Human monocyte-derived macrophages (e.g., THP-1 derived) or primary TAMs in co-culture with cancer cell lines (e.g., A549, H1299).
- Workflow:
- siRNA Preparation: Resuspend lyophilized SOX9 siRNA and control siRNA in nuclease-free buffer to a stock concentration of 100 µM.
- Complexation with Delivery Vehicle: Incubate siRNA (at working concentration) with the chosen nanovesicle or LNP formulation according to optimized protocols (e.g., 30 minutes at room temperature) [97] [98].
- Cell Transfection: Add the siRNA-vesicle complexes to the culture medium of target cells. For co-culture models, this can be added directly to the medium.
- Incubation and Analysis:
- Incubate cells for 24-72 hours.
- Harvest cells and analyze knockdown efficiency via:
- Quantitative RT-PCR: To measure SOX9 mRNA levels.
- Western Blotting: To measure SOX9 protein levels.
- Functional Assays: Conduct migration (e.g., Transwell) and invasion (e.g., Matrigel) assays to assess phenotypic consequences [5].
The following workflow diagram illustrates this siRNA-mediated knockdown protocol:
Experimental Protocol 2: CRISPR/Cas9-Mediated SOX9 Knockout
This protocol leverages CRISPR/Cas9 for permanent SOX9 inactivation, suitable for generating stable knockout models [100].
- Objective: To generate a stable SOX9 knockout in a cell line model for long-term functional studies.
- Key Reagents:
- Cas9 Protein: Purified S. pyogenes Cas9 nuclease.
- SOX9-specific gRNA: Chemically synthesized single-guide RNA (sgRNA) targeting an early exon of the SOX9 gene.
- Delivery Vehicle: For in vitro use, electroporation or commercial transfection reagents for ribonucleoprotein (RNP) delivery. For in vivo or hard-to-transfect cells, virus-like particles (VLPs) [96] or extracellular vesicle (EV)-based systems can be used [95].
- Workflow:
- RNP Complex Formation: Pre-complex the Cas9 protein and SOX9 sgRNA at a molar ratio of 1:2 to form the RNP complex. Incubate for 10-20 minutes at room temperature.
- Cell Delivery: Deliver the RNP complex into the target cells using an optimized method (e.g., electroporation).
- Recovery and Expansion: Allow cells to recover for 48-72 hours, then expand them under normal culture conditions.
- Validation and Clonal Selection:
- Efficiency Check: Analyze a portion of the bulk edited population using a T7 Endonuclease I assay or ICE analysis to assess editing efficiency.
- Single-Cell Cloning: Dilute the edited cell population to isolate single-cell clones.
- Genotypic Validation: Sequence the targeted SOX9 locus in expanded clones to confirm frameshift indels.
- Phenotypic Validation: Confirm SOX9 knockout via Western blot and functional assays (proliferation, colony formation) [100].
The following workflow diagram illustrates this CRISPR/Cas9-mediated knockout protocol:
The Scientist's Toolkit: Key Research Reagent Solutions
Successful implementation of gene-silencing experiments relies on critical reagents. The table below lists essential materials and their functions.
Table 3: Essential Reagents for Gene Silencing Experiments
| Reagent / Solution | Function / Application | Examples / Notes |
|---|---|---|
| SOX9-specific siRNA | Targets SOX9 mRNA for degradation by RISC. | Commercially available as pools from multiple vendors; requires validation. |
| Non-targeting siRNA Control | Critical control for non-sequence-specific effects. | Scrambled sequence with no known homology to the human genome. |
| SOX9-specific gRNA | Guides Cas9 nuclease to the target genomic locus. | Chemically synthesized, modified sgRNAs offer higher stability and reduced off-targets [93]. |
| Cas9 Nuclease | Effector enzyme that creates double-strand breaks in DNA. | High-purity, recombinant SpCas9 protein for RNP delivery. |
| Delivery Vectors | Enables intracellular delivery of silencing machinery. | For siRNA: Bioinspired nanovesicles, LNPs [97] [98]. For CRISPR: VLPs, EVs, electroporation systems [96] [95]. |
| Efficiency Assay Kits | Validates the success and efficiency of gene silencing. | For siRNA: qRT-PCR, Western Blot. For CRISPR: T7E1 assay, ICE Analysis, Sanger Sequencing. |
The choice between siRNA and CRISPR/Cas9 for SOX9 knockdown is not a matter of superiority, but of strategic alignment with experimental goals. For acute, transient studies—such as probing the immediate role of SOX9 in TAM-induced EMT over a few days—siRNA offers a rapid and effective solution. For long-term, stable genetic ablation—such as generating stable cell lines to study the chronic effects of SOX9 loss or for therapeutic development—CRISPR/Cas9 is the unequivocal choice. By leveraging the comparative data, detailed protocols, and reagent guidance provided herein, researchers can make an informed decision to effectively silence SOX9 and advance our understanding of its role in cancer and the tumor microenvironment.
Biological Rationale: SOX9 as a Pivotal Node in the Tumor Microenvironment
The transcription factor SOX9 (SRY-related HMG-box 9) has emerged as a critical regulator of tumor progression and a promising therapeutic target. Its function, however, is highly context-dependent, acting as an oncogene in most cancer types while displaying tumor-suppressor properties in others, such as melanoma and specific intestinal tumor contexts [16] [101]. This duality underscores the importance of precise preclinical modeling.
A key mechanism of SOX9-driven oncogenesis is its central role in mediating crosstalk within the tumor microenvironment (TME). Notably, Tumor-Associated Macrophages (TAMs) secrete cytokines like Transforming Growth Factor-beta (TGF-β), which upregulates SOX9 expression in cancer cells via the C-jun/SMAD3 signaling pathway [5]. Elevated SOX9, in turn, promotes Epithelial-to-Mesenchymal Transition (EMT), a process crucial for metastasis, characterized by loss of E-cadherin and gain of vimentin expression [5] [102]. Furthermore, SOX9 contributes to therapeutic resistance by maintaining cancer stem cell (CSC) populations, which are associated with tumor heterogeneity, relapse, and chemoresistance [103] [104].
The diagram below illustrates this core SOX9-mediated pathway in the TME.
Quantitative Evidence: Correlating SOX9 with Disease Progression
The prognostic significance of SOX9 and its relationship with TAMs are supported by clinical data. The following tables summarize key correlative findings from human tissue analyses and in vivo studies.
Table 1: Clinical Correlation of SOX9 and TAM Density in Human Non-Small Cell Lung Cancer (NSCLC) [5]
| Parameter | Correlation Finding | Clinical Impact |
|---|---|---|
| TAM Density (CD163+) | Positively correlated with SOX9 expression in tumor cells. | High density associated with poor prognosis. |
| SOX9 Expression | Positively correlated with TGF-β signaling. | High expression associated with shorter overall survival. |
| Co-expression (CD163+/SOX9+) | Strong positive correlation in patient specimens. | Patients with high co-expression had shortest OS and DFS. |
Abbreviations: OS (Overall Survival), DFS (Disease-Free Survival).
Table 2: Pan-Cancer Analysis of SOX9 mRNA Expression and Prognostic Value [16]
| Cancer Type | SOX9 Expression vs. Normal | Correlation with Overall Survival (OS) |
|---|---|---|
| LGG (Low-grade Glioma) | Significantly Increased | Shorter OS with high SOX9 expression |
| CESC (Cervical Cancer) | Significantly Increased | Shorter OS with high SOX9 expression |
| THYM (Thymoma) | Significantly Increased | Shorter OS with high SOX9 expression |
| SKCM (Skin Melanoma) | Significantly Decreased | (Context-dependent tumor suppressor) |
| TGCT (Testicular Cancer) | Significantly Decreased | (Context-dependent tumor suppressor) |
Experimental Workflow for Evaluating SOX9 Knockdown In Vivo
A robust preclinical protocol is essential for validating the therapeutic potential of targeting SOX9. The following workflow outlines the key steps from model establishment to endpoint analysis, with a focus on assessing TAM interaction and tumor progression.
Detailed Methodologies for Key Experimental Procedures
This protocol is used to generate stable SOX9-knockout cell lines for in vivo transplantation.
Materials:
- SOX9-floxed or wild-type cancer cells (e.g., HCT116, PANC-1).
- sgRNAs targeting SOX9 exons (e.g., Exon 1:
5'-CAGGAGAACACGTTCCCCAA-3'). - TrueCut Cas9 Protein v2.
- Lipofectamine CRISPRMAX Cas9 Transfection Reagent.
- Opti-MEM Reduced-Serum Medium.
- 6-well and 96-well tissue culture plates.
Procedure:
- Seed Cells: Plate 3x10^5 cells per well in a 6-well plate and culture until 60-80% confluent.
- Prepare Complexes:
- Mixture A: Dilute 100 pg of each sgRNA and 2.6 µL Cas9 Plus Reagent in 26.9 µL Opti-MEM. Add 6,250 ng Cas9 protein.
- Mixture B: Dilute 3 µL Lipofectamine CRISPRMAX in 29.3 µL Opti-MEM.
- Incubate both separately for 5 minutes at room temperature, then combine and incubate for another 10-20 minutes.
- Transfect: Add the complete mixture to the cells and incubate for 48 hours.
- Clone: Harvest cells and seed by limiting dilution into 96-well plates to isolate single-cell clones.
- Validate: Expand clones and confirm SOX9 knockout via genomic PCR (e.g., primers F:
5'-CCCGCGTATGAATCTCCTG-3', R:5'-TGCTTGGACATCCACACG-3') and Sanger sequencing, followed by Western blot analysis.
This protocol assesses the functional consequences of SOX9 knockdown on tumor progression.
Materials:
- Immunocompromised mice (e.g., NOD/SCID) or syngeneic mouse models.
- SOX9-knockdown and control cancer cells.
- Calipers, in vivo imaging system (IVIS).
- Tissue processing equipment for formalin-fixed and OCT-embedded samples.
Procedure:
- Inoculation: Subcutaneously inject 1-2x10^6 SOX9-knockdown or control cells into the flanks of mice (n=6-10 per group). For metastasis models, use intravenous or orthotopic injection.
- Monitor: Measure tumor dimensions with calipers twice weekly. Calculate volume using the formula: Volume = (Length x Width²) / 2.
- Terminate: Euthanize mice when control tumors reach a predetermined volume (e.g., 1500 mm³) or at a set time point for metastasis studies.
- Harvest: Excise and weigh tumors. Preserve portions in 10% neutral buffered formalin for histology, snap-freeze for RNA/protein analysis, and embed in OCT for frozen sections. For metastasis, harvest lungs, liver, and other organs for analysis.
Immunohistochemical and Immunofluorescent Analysis of Tumor Sections
This protocol is used to analyze SOX9 expression, TAM infiltration, and EMT markers in tumor tissues.
Materials:
- Formalin-fixed, paraffin-embedded (FFPE) tumor sections.
- Primary antibodies: anti-SOX9, anti-CD163 (for TAMs), anti-E-cadherin, anti-Vimentin, anti-Ki-67.
- HRP or fluorescent-conjugated secondary antibodies.
- Antigen retrieval solution (e.g., citrate buffer), blocking serum, DAPI.
Procedure:
- Dewax and Rehydrate: Bake slides, deparaffinize in xylene, and rehydrate through a graded ethanol series to water.
- Antigen Retrieval: Perform heat-induced epitope retrieval in appropriate buffer (e.g., citrate, pH 6.0) for 20 minutes.
- Block and Incubate: Block endogenous peroxidase and non-specific sites. Incubate with primary antibodies overnight at 4°C.
- Detect: For IHC, incubate with HRP-conjugated secondary antibody, develop with DAB, and counterstain with hematoxylin. For IF, incubate with fluorophore-conjugated secondary antibodies and counterstain with DAPI.
- Image and Quantify: Capture images using a brightfield or fluorescence microscope. Quantify staining intensity (SOX9) and positive cell counts (CD163+ TAMs) using image analysis software (e.g., ImageJ).
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for SOX9 and TAM-Focused Preclinical Research
| Reagent / Tool | Function / Application | Example & Notes |
|---|---|---|
| CRISPR-Cas9 System | Generation of stable SOX9-knockout cell lines. | TrueCut Cas9 Protein with exon-specific sgRNAs [103]. |
| siRNA/shRNA | Transient or stable SOX9 knockdown. | Used for in vitro validation and inducible in vivo models [102]. |
| Anti-CD163 Antibody | Marker for M2-like TAMs in IHC/IF. | Critical for correlating TAM density with SOX9 expression [5]. |
| Anti-SOX9 Antibody | Detection of SOX9 protein in cells and tissues. | Validate knockdown efficiency and localization [105]. |
| Recombinant TGF-β | Activate TGF-β/SOX9 pathway in vitro. | Used to rescue EMT phenotype in SOX9-knockdown cells [5]. |
| TGF-β Receptor Inhibitor | Chemically inhibit the SOX9 upstream pathway. | Tool for mechanistic validation (e.g., SB-431542) [5]. |
| Cordycepin | Small molecule inhibitor of SOX9 expression. | Adenosine analog; shows dose-dependent SOX9 downregulation [16]. |
Conclusion
Knockdown of SOX9 in TAMs presents a promising strategy to disrupt a key oncogenic axis in the tumor microenvironment. Successful implementation requires a solid understanding of SOX9 biology, a robust knockdown protocol, careful troubleshooting, and comprehensive validation of functional outcomes. The evidence suggests that targeting this pathway can inhibit critical pro-tumoral processes, including EMT, metastasis, and potentially, chemoresistance. Future work should focus on developing targeted delivery systems for TAM-specific SOX9 inhibition and exploring its synergistic potential with existing immunotherapies, paving the way for novel combination treatments in oncology.
References
- 1. SOX9: an important factor in regulating breast cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360010/]
- 2. SOX9 as an emerging target for anticancer drugs and a ... [https://pubmed.ncbi.nlm.nih.gov/35636723/]
- 3. Cross-regulation between SOX9 and the canonical Wnt ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10469848/]
- 4. SOX9: a novel janus-faced regulator in immunity and its ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1700812/full]
- 5. Tumor-associated macrophages promote tumor metastasis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5725132/]
- 6. Tumor-associated macrophages promote tumor metastasis ... [https://www.oncotarget.com/article/21068/]
- 7. SOX9 drives a stem-like transcriptional state and platinum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483608/]
- 8. The local and circulating SOX9 as a potential biomarker for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7292907/]
- 9. High expression of SOX9 is a diagnostic and prognostic ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1531937/full]
- 10. The Crosstalk Between Tumor-Associated Macrophages ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2020.590941/full]
- 11. Upregulated SOX9 expression indicates worse prognosis ... [https://www.oncotarget.com/article/22635/text/]
- 12. Epigenetic Regulation of SOX9 by the NF-κB Signaling ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3775871/]
- 13. NF-κB: Governing Macrophages in Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10888451/]
- 14. Role of the SOX family in cancer immune evasion [https://pmc.ncbi.nlm.nih.gov/articles/PMC11789896/]
- 15. Tumor-associated macrophages: an effective player of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10687432/]
- 16. Comprehensive analysis, immune, and cordycepin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10067558/]
- 17. Comprehensive analysis, immune, and cordycepin ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1149986/full]
- 18. Tumor‐Associated Macrophages: Key Players in the Non ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11808749/]
- 19. Tumor‑associated macrophages in lung cancer [https://www.spandidos-publications.com/10.3892/mmr.2020.11518]
- 20. SOX9 drives the epithelial–mesenchymal transition in non ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-019-1895-2]
- 21. SOX9 Regulates Cancer Stem-Like Properties and ... [https://www.nature.com/articles/s41598-017-12037-8]
- 22. The role of tumor-associated macrophages in lung cancer [https://www.sciencedirect.com/science/article/pii/S0753332223018127]
- 23. Oncogenic role of PLOD3 mediated by SOX9 through IL-6/ ... [https://pubmed.ncbi.nlm.nih.gov/41242365/]
- 24. Oncogenic role of PLOD3 mediated by SOX9 through IL-6/ ... [https://www.sciencedirect.com/science/article/abs/pii/S0898656825006655]
- 25. The SOX9-Aldehyde Dehydrogenase Axis Determines ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6944474/]
- 26. SOX9 modulates cancer biomarker and cilia genes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8101357/]
- 27. SOX9 expression decreases survival of patients with ... [https://www.nature.com/articles/s41416-018-0338-9]
- 28. Guidelines for the selection of highly effective siRNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC373388/]
- 29. siRNA Design Guidelines | Technical Bulletin #506 [https://www.thermofisher.com/us/en/home/references/ambion-tech-support/rnai-sirna/general-articles/-sirna-design-guidelines.html]
- 30. Comprehensive review of macrophage models [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1640935/full]
- 31. Comprehensive review of macrophage models: primary cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12404969/]
- 32. Quantitative Analysis of Monocyte-Derived Macrophage NFκB ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579604/]
- 33. Primary macrophages and J774 cells respond differently to ... [https://www.nature.com/articles/srep42225]
- 34. Comprehensive analysis of different tumor cell-line produced ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0274056]
- 35. USP18 deubiquitinates and stabilizes SOX9 to promote the ... [https://www.nature.com/articles/s41420-025-02522-9]
- 36. Implication of metabolism in the polarization of tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10368868/]
- 37. Tumor-associated macrophages: an accomplice in solid ... [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-019-0568-z]
- 38. Evaluating the Polarization of Tumor-Associated ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2019.01512/full]
- 39. Orchestration of Tumor-Associated Macrophages in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12210125/]
- 40. Crosstalk between exosomes and tumor-associated ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1512480/full]
- 41. Targeting of TAMs: can we be more clever than cancer cells? [https://www.nature.com/articles/s41423-024-01232-z]
- 42. Macrophage Transcriptomic Alterations Driven by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12181664/]
- 43. SOX9 mediates the phenotypic transformation of vascular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12213809/]
- 44. SOX9 drives KRAS-induced lung adenocarcinoma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11809655/]
- 45. Molecular dynamics simulations based siRNA design ... [https://www.nature.com/articles/s41598-025-16936-z]
- 46. Non-cationic carriers for siRNA delivery: Current progress ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925009769]
- 47. Optimization of siRNA Design [https://www.bocsci.com/blog/optimization-of-sirna-design/?srsltid=AfmBOopbmjimH7bVjFsaY4ktUrMdz48sAcD4MLr-_t5gmTjHDDrnw2TY]
- 48. Advances in RNA-based therapeutics: current breakthroughs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12592931/]
- 49. Tumor-associated macrophages promote tumor metastasis ... [https://pubmed.ncbi.nlm.nih.gov/29245941/]
- 50. A simple method using CRISPR-Cas9 to knock-out genes in murine cancerous cell lines | Scientific Reports [https://www.nature.com/articles/s41598-020-79303-0]
- 51. Sox9 CRISPR Knockout and Activation Products (h) | SCBT - Santa Cruz Biotechnology [https://www.scbt.com/p/sox-9-crispr-knockout-and-activation-products-h]
- 52. A cleavage-based surrogate reporter for the evaluation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8421217/]
- 53. Why qPCR and WB results are not consistent 2025- ... [https://www.antibodysystem.com/archive/380.html]
- 54. validation of reference genes for analysis by qRT-PCR and ... [https://pubmed.ncbi.nlm.nih.gov/22916200/]
- 55. Quantitative Western Blot Analysis [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/quantitative-western-blot-analysis.html]
- 56. Establishment and evaluation of a circAdpgk-0001 knockdown ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495950/]
- 57. A quantitative meta-analysis comparing cell models in ... [https://www.nature.com/articles/s41598-023-35043-5]
- 58. Development of a Co-culture Model for Assessing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12151291/]
- 59. Flow Cytometry Protocol | Abcam [https://www.abcam.com/en-us/technical-resources/protocols/flow-cytometry-for-intracellular-and-extracellular-targets]
- 60. Quantum dots as biocompatible small RNA nanocarriers ... [https://www.nature.com/articles/s41536-025-00403-4]
- 61. a game-changer in cancer immunotherapy [https://link.springer.com/article/10.1007/s13346-025-01970-1]
- 62. Non-viral siRNA transfection of primary mesenchymal ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517321011650]
- 63. Non-viral, high throughput genetic engineering of primary ... [https://pubmed.ncbi.nlm.nih.gov/39842078/]
- 64. SOX9 mediates the phenotypic transformation of vascular ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1592594/full]
- 65. Sox9 regulation of hexokinase 1 controls ... [https://www.nature.com/articles/s41467-025-65092-5]
- 66. Recent advances in optimizing siRNA delivery to ... [https://pubmed.ncbi.nlm.nih.gov/40126051/]
- 67. Optimizing siRNA Transfection [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/transfection-basics/guidelines-for-rna-transfection/optimizing-sirna-transfection.html]
- 68. Top Ten Ways to Optimize siRNA in Cultured Cells Delivery [https://www.thermofisher.com/tw/zt/home/references/ambion-tech-support/rnai-sirna/general-articles/top-ten-ways-to-optimize-sirna-delivery-in-cultured-cells.html]
- 69. Principles, methods, and reagents of siRNA transfection [https://www.bocsci.com/resources/principles-methods-and-reagents-of-sirna-transfection.html?srsltid=AfmBOoqxJt2KNcxn-RJwNiF5-1x-V0n4qZ3uJIdPOgA-cVOtWxCmPYGX]
- 70. Systematic optimization of siRNA productive uptake into ... [https://www.sciencedirect.com/science/article/pii/S0753332224001665]
- 71. Mastering siRNA Techniques for Quantitative Genetics [https://www.numberanalytics.com/blog/mastering-sirna-techniques-for-quantitative-genetics]
- 72. evaluating and mitigating off-target effects in CRISPR gene ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2023.1339189/full]
- 73. Latest Developed Strategies to Minimize the Off-Target ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7407193/]
- 74. Targeting M2-like tumor-associated macrophages is a ... [https://www.nature.com/articles/s41698-024-00522-z]
- 75. Evaluating the Polarization of Tumor-Associated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6992653/]
- 76. SOX9 as an emerging target for anticancer drugs and a ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644622002136]
- 77. Orchestration of Tumor-Associated Macrophages in the ... [https://www.ijbs.com/v21p4098.htm]
- 78. A generalized protocol for the induction of M2-like ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11964487/]
- 79. A Comprehensive High-Efficiency Protocol for Isolation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8118145/]
- 80. Progress of tumor-associated macrophages in the ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2022.911410/full]
- 81. M2‐like tumor‐associated macrophages promote epithelial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10728010/]
- 82. Knockdown of SOX9 Inhibits the Proliferation, Invasion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7840816/]
- 83. TGF‑β1 induces N‑cadherin expression by upregulating ... [https://www.spandidos-publications.com/10.3892/ol.2020.11582]
- 84. SOX9 promotes the invasion and migration of lung ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10623714/]
- 85. Promotion of colorectal cancer progression by immune- ... [https://www.sciencedirect.com/science/article/pii/S0898656823002681]
- 86. Functional assessment of migration and adhesion to quantify ... [https://pubs.rsc.org/en/content/articlehtml/2025/sm/d4sm01351d]
- 87. Quantitative impedance-based characterization of breast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512568/]
- 88. Exploring tumor-associated macrophages in glioblastoma [https://www.nature.com/articles/s41698-025-00920-x]
- 89. Dual roles and therapeutic targeting of tumor-associated ... [https://www.nature.com/articles/s41392-025-02325-5]
- 90. Macrophages Are a Double-Edged Sword [https://www.mdpi.com/2218-273X/12/6/850]
- 91. Cytokine profiling identifies circulating IL-2, IL23 and sPD ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12279494/]
- 92. SOCS molecules: the growing players in macrophage ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5601173/]
- 93. RNAi vs. CRISPR: Guide to Selecting the Best Gene ... [https://www.synthego.com/blog/rnai-vs-crispr-guide/]
- 94. siRNAs, saRNAs, miRNAs, CRISPR/Cas System [https://nhsjs.com/2025/revolutionizing-gene-editing-techniques-in-medicine-sirnas-sarnas-mirnas-crispr-cas-system/]
- 95. Overcoming the Delivery Challenges in CRISPR/Cas9 Gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12434829/]
- 96. Characterizing and controlling CRISPR repair outcomes in ... [https://www.nature.com/articles/s41467-025-66058-3]
- 97. Bioengineered nanovesicles for efficient siRNA delivery ... [https://www.nature.com/articles/s41467-025-61230-1]
- 98. Bioinspired Extracellular Vesicles for Enhanced Delivery of ... [https://pubmed.ncbi.nlm.nih.gov/40877516/]
- 99. Nanotechnology-Based Delivery of CRISPR/Cas9 for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346122/]
- 100. SOX9 Knockout Induces Polyploidy and Changes Sensitivity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7589851/]
- 101. SOX9 suppresses colon cancer via inhibiting epithelial ... [https://www.jci.org/articles/view/184115]
- 102. Deciphering of SOX9 Functions in Pancreatic Cancer Cells [https://www.mdpi.com/1422-0067/26/6/2652]
- 103. SOX9 knockout decreases stemness properties in colorectal ... [https://jgo.amegroups.org/article/view/76436/html]
- 104. Embryonic transcription factor SOX9 drives breast cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5465894/]
- 105. Sox9 inhibits Activin A to promote biliary maturation and ... [https://www.nature.com/articles/s41467-025-56813-x]