Targeting SOX9 to Overcome Resistance to PD-1/PD-L1 Blockade in Cancer
Combining SOX9 inhibition with PD-1/PD-L1 blockade represents a promising strategy to overcome immunotherapy resistance in solid tumors.
Targeting SOX9 to Overcome Resistance to PD-1/PD-L1 Blockade in Cancer
Abstract
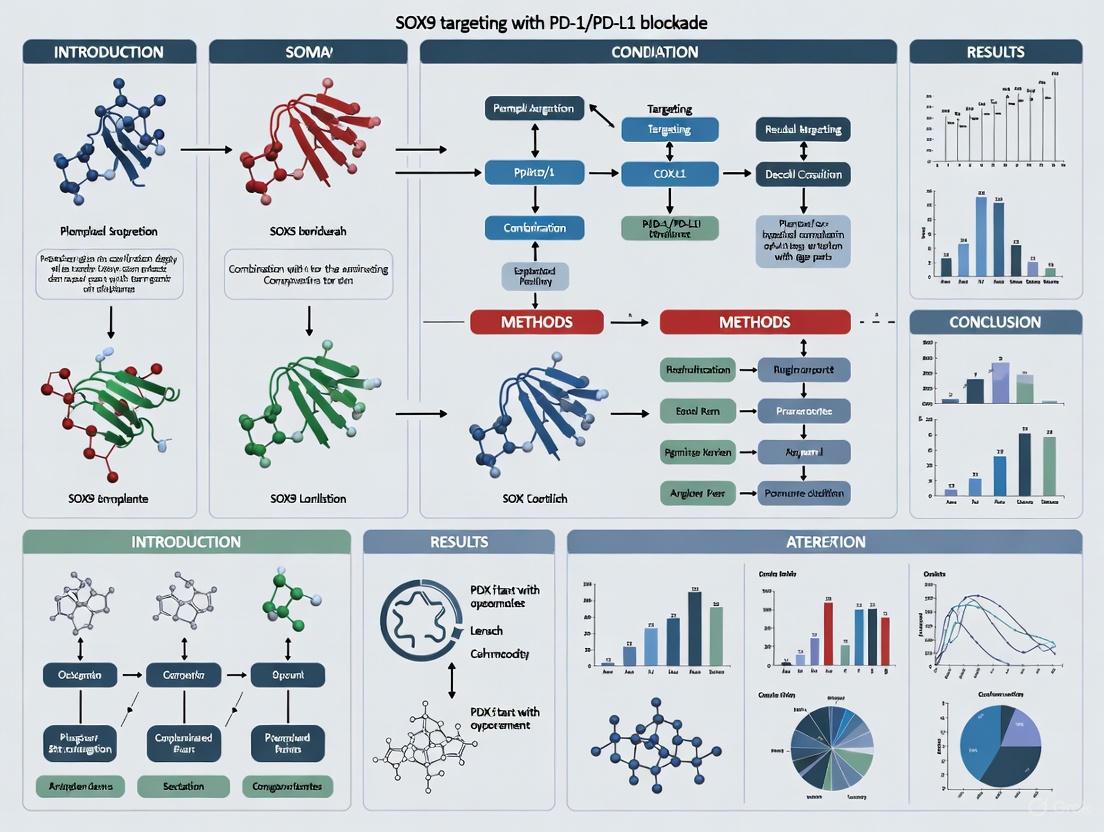
Combining SOX9 inhibition with PD-1/PD-L1 blockade represents a promising strategy to overcome immunotherapy resistance in solid tumors. This article synthesizes recent evidence establishing SOX9 as a key regulator of the immunosuppressive tumor microenvironment, detailing its role in driving resistance to immune checkpoint inhibitors. We explore foundational molecular mechanisms, advanced methodological approaches for targeting SOX9, strategies for troubleshooting and optimizing combination therapies, and comparative validation of therapeutic efficacy across cancer types. For researchers and drug development professionals, this review provides a comprehensive framework for developing SOX9-directed combination immunotherapies to achieve more durable anti-tumor responses.
SOX9 as a Master Regulator of the Immunosuppressive Tumor Microenvironment
SOX9 Structure, Functional Domains, and Transcriptional Regulation
The transcription factor SOX9 (SRY-related HMG box 9) is a master regulator of numerous developmental processes and continues to play critical roles in adult tissue maintenance and disease. As a member of the SOXE subgroup of SOX proteins, SOX9 functions as a key transcriptional switch in cell fate determination, differentiation, and stem cell biology [1] [2]. Its dysregulation contributes to various pathological conditions, including congenital disorders, fibrosis, and cancer, while its emerging role in immunomodulation positions it as a potential target for combination therapies with immune checkpoint blockade [3] [4]. This application note provides a comprehensive overview of SOX9 protein architecture, functional domains, and regulatory mechanisms, with specific methodological protocols for researchers investigating SOX9 targeting in the context of PD-1/PD-L1 blockade research.
SOX9 Protein Structure and Functional Domains
The human SOX9 protein comprises 509 amino acids with several evolutionarily conserved functional domains that confer its DNA-binding capability, dimerization potential, and transcriptional activation functions [1] [4] [5].
Structural Domain Organization
Table 1: SOX9 Functional Domains and Characteristics
| Domain | Position | Key Functions | Interacting Partners |
|---|---|---|---|
| Dimerization Domain (DIM) | N-terminal | Facilitates homo- and heterodimerization with SOXE proteins | SOX8, SOX10 via DIM-HMG interactions |
| HMG Box | Central | Sequence-specific DNA binding (consensus: AGAACAATGG); DNA bending; Nuclear localization | DNA minor groove; Contains NLS/NES signals |
| Transactivation Domain Middle (TAM) | Central | Synergizes with TAC; Transcriptional activation | Transcriptional co-activators |
| PQA-rich Domain | C-terminal | Enhances transactivation; Stabilizes protein | Protein stabilizers |
| Transactivation Domain C-terminal (TAC) | C-terminal | Primary transcriptional activation; Inhibits β-catenin | MED12, CBP/p300, TIP60, WWP2 |
The HMG (High Mobility Group) box represents the defining characteristic of SOX family proteins, facilitating sequence-specific DNA binding to the consensus motif AGAACAATGG (with AACAAT as the core binding element) and inducing structural bends in DNA by forming an L-shaped complex [1] [5]. This domain contains embedded nuclear localization signals (NLS) and a nuclear export signal (NES) that enable nucleocytoplasmic shuttling [4].
The DIM (dimerization) domain, located upstream of the HMG box, facilitates the formation of both homodimers and heterodimers with other SOXE family members (SOX8 and SOX10). Notably, dimerization occurs through interactions between the DIM domain of one molecule and the HMG box of another, rather than through DIM-DIM interactions [5]. This dimerization capability is crucial for SOX9's function in chondrogenesis but appears dispensable in testicular Sertoli cells where SOX9 functions as a monomer [1].
The transactivation domains TAM and TAC work synergistically to activate target gene expression. The TAC domain at the extreme C-terminus physically interacts with key transcriptional co-activators including MED12 (mediator complex subunit 12), CBP/p300, TIP60, and WWP2 [1]. This domain is also essential for SOX9's inhibition of β-catenin during chondrocyte differentiation [4].
The unique PQA-rich domain (abundant in proline, glutamine, and alanine) enhances transactivation capability in vitro, though it lacks autonomous transactivation function [1] [5].
Diagram 1: SOX9 domain structure showing organizational arrangement
Transcriptional and Post-translational Regulation of SOX9
SOX9 expression and activity are regulated through multiple mechanisms including enhancer/promoter elements, epigenetic modifications, and post-translational modifications that fine-tune its transcriptional output in different tissue contexts.
Enhancer and Promoter Regulation
The SOX9 gene locus encompasses an extensive regulatory landscape with multiple long-range enhancers that control its spatiotemporal expression [1] [5]. Key regulatory elements include:
- TES/TESCO: A 3.2 kb testis-specific enhancer located 13 kb upstream of Sox9, with a 1.4 kb core element (TESCO) that binds SRY and steroidogenic factor 1 (SF1) to drive Sertoli cell-specific expression [5].
- SOM: An enhancer located 70 kb upstream that works cooperatively with SOX9 dimers to activate Sox9 expression through a positive feedback loop [5].
- Promoter elements: The proximal promoter region binds transcription factors including CREB1 and CEBPB in Sertoli cells, while FOXO4 transcriptionally activates SOX9 by binding to its promoter [5].
Table 2: SOX9 Regulatory Mechanisms and Modifications
| Regulatory Mechanism | Regulatory Elements/Modifications | Functional Consequences |
|---|---|---|
| Enhancer Elements | TES/TESCO, SOM | Tissue-specific expression; Feed-forward regulation |
| Promoter Binding Factors | FOXO4, CREB1, CEBPB, IL-1β | Transcriptional activation (FOXO4, CREB1, CEBPB) or repression (IL-1β) |
| Epigenetic Modifications | DNA methylation, H3K9/K27 trimethylation, H3 acetylation | Repression via promoter methylation (cancer) or histone modifications (OA) |
| Post-translational Modifications | Serine phosphorylation (S64, S181, S211), SUMOylation, ubiquitination | Modulates protein stability, DNA binding, and transcriptional activity |
Epigenetic Regulation
DNA methylation and histone modifications significantly impact SOX9 expression in a tissue and disease-specific manner [5]. During testicular development, the Sox9 promoter remains unmethylated throughout fetal, neonatal, and adult periods, while specific CpG sites become methylated in mature ovaries [5]. In cancer contexts, promoter methylation patterns vary significantly—the SOX9 promoter is completely methylated in breast cancer but unmethylated in healthy cervical tissue [5]. Similarly, gastric cancer progression associates with increased SOX9 promoter methylation, potentially suppressing SOX9 in advanced stages [5].
The histone methyltransferase EZH2 contributes to SOX9 repression by binding to the Sox9 promoter and promoting chromatin compaction [5]. In osteoarthritis, increased trimethylation of H3K9 and H3K27, along with reduced acetylation of multiple H3 residues (K9, K15, K18, K23, K27), has been observed at SOX9 promoters [5].
Post-translational Modifications
SOX9 undergoes various post-translational modifications that regulate its activity, stability, and subcellular localization [5]:
- Phosphorylation: Serine residues S64, S181, and S211 are phosphorylated, potentially by PKA, affecting SOX9 transcriptional activity.
- SUMOylation: Addition of SUMO moieties modulates SOX9 function.
- Ubiquitination: Regulates SOX9 protein stability and degradation.
These modifications allow precise, context-dependent control of SOX9 activity in response to cellular signals.
Diagram 2: SOX9 regulatory network from gene to functional protein
Experimental Protocols for SOX9 Functional Analysis
Protocol 1: SOX9-DNA Binding Analysis Using Chromatin Immunoprecipitation (ChIP)
Purpose: To identify direct genomic binding sites of SOX9 and assess its transcriptional targets in different cellular contexts.
Reagents and Solutions:
- Crosslinking Solution: 1% formaldehyde in PBS
- Cell Lysis Buffer: 50 mM HEPES-KOH (pH 7.5), 140 mM NaCl, 1 mM EDTA, 10% glycerol, 0.5% NP-40, 0.25% Triton X-100
- Nuclear Lysis Buffer: 10 mM Tris-HCl (pH 8.0), 1% SDS, 10 mM EDTA
- ChIP Dilution Buffer: 0.01% SDS, 1.1% Triton X-100, 1.2 mM EDTA, 16.7 mM Tris-HCl (pH 8.1), 167 mM NaCl
- Protein A/G Magnetic Beads
- SOX9-specific antibody (validated for ChIP)
- Elution Buffer: 1% SDS, 0.1 M NaHCO3
- DNA Recovery Kit
Procedure:
- Crosslink protein-DNA complexes with 1% formaldehyde for 10 min at room temperature. Quench with 125 mM glycine for 5 min.
- Harvest cells and wash twice with ice-cold PBS. Resuspend pellet in Cell Lysis Buffer and incubate for 10 min on ice.
- Centrifuge at 2,000 × g for 5 min at 4°C. Resuspend nuclei in Nuclear Lysis Buffer and incubate for 10 min on ice.
- Sonicate chromatin to fragment size of 200-500 bp. Confirm fragmentation by agarose gel electrophoresis.
- Dilute lysate 10-fold with ChIP Dilution Buffer. Pre-clear with Protein A/G beads for 1 hr at 4°C.
- Incubate supernatant with SOX9 antibody (2-5 μg) overnight at 4°C with rotation.
- Add Protein A/G beads and incubate for 2 hr at 4°C.
- Wash beads sequentially with:
- Low Salt Wash Buffer: 0.1% SDS, 1% Triton X-100, 2 mM EDTA, 20 mM Tris-HCl (pH 8.1), 150 mM NaCl
- High Salt Wash Buffer: 0.1% SDS, 1% Triton X-100, 2 mM EDTA, 20 mM Tris-HCl (pH 8.1), 500 mM NaCl
- LiCl Wash Buffer: 0.25 M LiCl, 1% NP-40, 1% deoxycholate, 1 mM EDTA, 10 mM Tris-HCl (pH 8.1)
- TE Buffer: 10 mM Tris-HCl (pH 8.0), 1 mM EDTA
- Elute complexes with Elution Buffer at 65°C for 15 min with vortexing.
- Reverse crosslinks at 65°C overnight with 200 mM NaCl.
- Purify DNA using DNA Recovery Kit and analyze by qPCR or sequencing.
Technical Notes: Include positive control regions (known SOX9 targets like COL2A1 enhancer) and negative control regions (non-target genes). Optimize sonication conditions for each cell type to ensure appropriate chromatin fragmentation.
Protocol 2: Assessing SOX9-Dependent Alternative Splicing in Beta Cells
Purpose: To evaluate SOX9's non-canonical role in regulating alternative splicing in pancreatic beta cells, relevant to its function in mature tissues [6].
Reagents and Solutions:
- SOX9-depleted beta cell lines (rodent or human stem cell-derived)
- Control beta cell lines
- RNA extraction kit (guanidine thiocyanate-phenol-chloroform based)
- DNase I (RNase-free)
- Reverse transcription kit with random hexamers
- Quantitative PCR reagents
- Alternative splicing PCR primers flanking variable exons
- Capillary electrophoresis system or agarose gel equipment
Procedure:
- Culture control and SOX9-depleted beta cells under standard conditions (RPMI-1640 with 10% FBS, 11 mM glucose).
- Extract total RNA using guanidine thiocyanate-phenol-chloroform method. Treat with DNase I to remove genomic DNA contamination.
- Synthesize cDNA using reverse transcriptase with random hexamers.
- Design PCR primers flanking alternatively spliced exons of key beta cell genes (e.g., SRSF5, insulin secretion pathway genes).
- Perform PCR amplification with high-fidelity DNA polymerase using the following conditions:
- 94°C for 2 min (initial denaturation)
- 35 cycles of: 94°C for 30 sec, 60°C for 30 sec, 72°C for 45 sec
- 72°C for 5 min (final extension)
- Separate PCR products by capillary electrophoresis or 3% agarose gel electrophoresis.
- Quantify splice isoform ratios using image analysis software.
- Validate significant splicing changes by RT-qPCR with isoform-specific probes or Sanger sequencing.
Technical Notes: Include internal splicing controls. Perform triplicate biological replicates. Confirm SOX9 knockdown efficiency by western blot or qPCR. This protocol can be adapted to immune cells when investigating SOX9 in PD-1/PD-L1 contexts.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for SOX9 Investigation
| Reagent Category | Specific Examples | Application Notes |
|---|---|---|
| SOX9 Antibodies | ChIP-validated SOX9 antibodies (e.g., Millipore AB5535) | Validation essential for specific applications; performance varies by technique |
| Cell Models | SOX9-deficient beta cells [6], Chondrocyte cell lines, Cancer cell lines with SOX9 modulation | Choose model relevant to biological context; inducible systems preferred for functional studies |
| Animal Models | Ins-Cre;Sox9fl/fl (pancreatic beta cell knockout) [6], Neural crest-specific Sox9 knockout [7] | Tissue-specific knockout critical for studying SOX9 in development and disease |
| Reporters | SOX9-responsive luciferase reporters (e.g., with COL2A1 enhancer) | Monitor SOX9 transcriptional activity; include mutated binding sites as controls |
| SOX9 Expression Constructs | Wild-type SOX9, Domain mutants (ΔDIM, ΔTAC), Phosphorylation mutants (S64A, S181A, S211A) | Structure-function studies; assess contribution of specific domains |
| Splicing Analysis Tools | Alternative splicing PCR primers, SRSF5 expression constructs [6] | Critical for studying non-canonical SOX9 functions in mature cells |
SOX9 in Cancer-Immunity Cycle and Combination Therapy Potential
SOX9 exhibits complex, context-dependent roles in tumor biology and immunomodulation, presenting both challenges and opportunities for therapeutic targeting [4]. In the tumor microenvironment, SOX9 expression correlates with specific immune cell infiltration patterns—negatively correlating with B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while showing positive correlation with neutrophils, macrophages, activated mast cells, and naive/activated T cells [4].
SOX9 contributes to tumor immune escape through multiple mechanisms: it impairs CD8+ T cell and NK cell function, promotes M2 macrophage polarization, and facilitates the establishment of an "immune desert" microenvironment [4]. These immunomodulatory functions position SOX9 as a potential target for combination therapies with PD-1/PD-L1 blockade, particularly in SOX9-high tumors that may rely on its activity for immune evasion.
The dual nature of SOX9—acting as both an oncogene and regeneration promoter—necessitates careful therapeutic strategy. Potential approaches include:
- Small molecule inhibitors targeting SOX9-DNA binding or protein-protein interactions
- Epigenetic modulators to normalize SOX9 expression in pathological contexts
- SOX9 pathway inhibition in combination with α-PD-1/PD-L1 antibodies to address multiple immune resistance mechanisms
- Context-specific modulation that considers SOX9's tissue-repair functions
SOX9 represents a multifaceted transcription factor with complex regulatory mechanisms governing its diverse functions in development, homeostasis, and disease. Its modular domain architecture, extensive regulatory landscape, and post-translational modifications enable precise context-dependent control of its transcriptional output. The emerging role of SOX9 in immunomodulation and its non-canonical functions in processes like alternative splicing expand its potential relevance as a therapeutic target. The experimental protocols and research tools outlined here provide a foundation for investigating SOX9 in the context of PD-1/PD-L1 blockade research, with particular attention to its complex dual roles in both promoting disease and maintaining tissue homeostasis. As combination immunotherapy approaches advance, understanding and strategically targeting multifaceted regulators like SOX9 will be essential for developing effective cancer treatments that overcome resistance mechanisms while preserving physiological functions.
Pan-Cancer SOX9 Overexpression and Correlation with Poor Prognosis
The SOX9 (SRY-related HMG-box 9) transcription factor is an evolutionarily conserved regulator of developmental processes, including chondrogenesis, bone formation, and organogenesis [8] [9]. Recent molecular and functional analyses have elucidated its crucial role in stem cell biology across mesoderm-, ectoderm-, and endoderm-derived tissues and organs [9]. In oncology, SOX9 has emerged as a critical regulatory node with dualistic functions—acting primarily as an oncogene while demonstrating tumor suppressor activity in specific contexts such as cervical cancer, endometrial carcinoma, and melanomas [8] [9].
This Application Note examines the pan-cancer overexpression of SOX9 and its correlation with poor prognosis, framing these findings within the developing therapeutic paradigm of combining SOX9 pathway targeting with PD-1/PD-L1 blockade strategies. We provide structured quantitative data, experimental protocols for key investigations, pathway visualizations, and essential research reagent solutions to facilitate translational research in this emerging field.
Pan-Cancer SOX9 Expression and Clinical Prognosis
Table 1: SOX9 Overexpression and Prognostic Correlation Across Cancers
| Cancer Type | Expression Status | Prognostic Correlation | Functional Roles | References |
|---|---|---|---|---|
| Pancreatic Ductal Adenocarcinoma | Upregulated in majority of cases | Poor overall survival, associated with tumor stage | Promotes proliferation, metastasis, chemoresistance, regulates TSPAN8-mediated metastasis | [8] [10] [9] |
| Hepatocellular Carcinoma | Overexpression | Poor disease-free survival, poor overall survival | Promotes invasiveness and migration, activates Wnt/β-catenin signaling | [9] |
| Breast Cancer | Overexpression | Poor overall survival | Promotes proliferation, tumorigenesis, and metastasis | [9] |
| Prostate Cancer | Overexpression | Poor relapse-free survival, poor overall survival | Promotes cell proliferation and apoptosis resistance | [9] |
| Glioblastoma | High expression | Better prognosis in lymphoid invasion subgroups | Correlated with immune infiltration and checkpoint expression | [11] |
| Colorectal Cancer | Overexpression | N/A | Promotes cell proliferation, senescence inhibition, and chemoresistance | [9] |
| Bladder Cancer | Overexpression | Poor overall survival | Promotes tumorigenesis | [9] |
| Gastric Cancer | Overexpression | Poor disease-free survival | Promotes chemoresistance | [9] |
| Ovarian Cancer | Overexpression | Poor overall survival (when co-expressed with HIF-2α) | Induces TUBB3 expression | [9] |
The pan-cancer analysis reveals SOX9 overexpression as a recurrent theme across diverse malignancies, with particularly strong associations with aggressive disease phenotypes in pancreatic ductal adenocarcinoma (PDAC). In PDAC, SOX9 upregulation is observed in the majority of cases and is hypothesized to be necessary for the formation and maintenance of tumor phenotypes [8]. SOX9 maintains stemness and facilitates epithelial-mesenchymal transition (EMT), driving proliferation, metastasis, and therapy resistance [12]. The association between high SOX9 expression and poor survival outcomes underscores its potential value as both a prognostic biomarker and therapeutic target.
SOX9 and Immune Checkpoint Interplay in the Tumor Microenvironment
Emerging evidence positions SOX9 within the complex network of tumor-immune interactions, suggesting potential synergy with immune checkpoint blockade approaches.
Table 2: SOX9-Immune System Interactions in Cancer
| Aspect of Interaction | Observation/Effect | Cancer Context | References |
|---|---|---|---|
| Correlation with Immune Checkpoints | Expression correlated with immune checkpoint molecules | Glioblastoma | [11] |
| Immune Cell Infiltration | Correlated with specific immune cell infiltration patterns | Glioblastoma, Pancreatic Cancer | [11] [13] |
| Circulating Tumor Cells (CTCs) | SOX9+ PDX1+ ductal stem cells identified as CTCs | Pancreatic Cancer | [13] |
| PD-L1 Regulation | Potential indirect regulation through inflammatory pathways | Multiple Cancers | [12] |
| Response to Combination Therapy | LIF blockade (affecting SOX9-related pathways) + anti-PD-L1 enhances chemotherapy | Pancreatic Cancer | [14] |
In glioblastoma, SOX9 expression demonstrates significant correlation with immune checkpoint expression and distinct immune infiltration patterns, suggesting its involvement in shaping the immunosuppressive tumor microenvironment [11]. Similarly, in pancreatic cancer models, SOX9-positive circulating tumor cells have been identified, indicating their potential role in metastasis and immune evasion [13]. Preclinical studies demonstrate that targeting pathways upstream of SOX9 (e.g., LIF blockade) in combination with anti-PD-L1 therapy significantly enhances antitumor efficacy in PDAC models, providing compelling rationale for SOX9-focused combination immunotherapy strategies [14].
Experimental Protocols for SOX9 Functional Analysis
Protocol: SOX9 Knockdown via RNA Interference in Pancreatic Cancer Cells
Principle: This protocol describes SOX9 knockdown using small interfering RNA (siRNA) to investigate its functional roles in pancreatic cancer cells, based on established methodologies [8] [12].
Materials:
- Pancreatic cancer cell lines (e.g., PANC-1, COLO357, AsPC-1, BxPC-3)
- SOX9-specific siRNA duplexes (pooled recommended) and negative control siRNA
- Lipofectamine RNAiMAX transfection reagent
- Complete cell culture media (DMEM/F12 or RPMI-1640 with 10% FBS)
- 6-well tissue culture plates
Procedure:
- Cell Seeding: Seed pancreatic cancer cells in 6-well plates at 30-50% confluence 24 hours before transfection.
- Transfection Complex Preparation:
- Dilute 10 nM pooled SOX9 siRNA or negative control siRNA in serum-free medium.
- Dilute Lipofectamine RNAiMAX in serum-free medium.
- Combine diluted siRNA with diluted transfection reagent (1:1 ratio) and incubate 5-20 minutes at room temperature.
- First Transfection: Add siRNA-lipid complexes to cells and incubate 24-48 hours at 37°C, 5% CO₂.
- Second Transfection: Repeat transfection 48 hours after the first transfection to enhance knockdown efficiency.
- Harvesting: Harvest cells 72 hours after the first transfection for downstream analysis (Western blot, RNA-seq, functional assays).
Validation:
- Confirm SOX9 knockdown at protein level via Western blotting.
- Assess phenotypic effects: proliferation assays (MTT, BrdU), apoptosis (caspase activation, Annexin V), migration/invasion (Transwell assays).
Protocol: Assessing SOX9 Expression in Circulating Tumor Cells
Principle: This protocol detects SOX9-positive circulating tumor cells in blood and lymphoid tissues using flow cytometry, applicable to preclinical pancreatic cancer models [13].
Materials:
- Single-cell suspensions from blood, lymph nodes, or spleen
- Red blood cell lysis buffer
- Fluorochrome-conjugated antibodies: anti-CD45, anti-CD11b, anti-SOX9, anti-PDX1
- Live/dead cell marker
- Flow cytometry buffer (PBS with 2% FBS)
- BD FACSCalibur flow cytometer or equivalent
Procedure:
- Sample Preparation: Collect blood, lymph nodes, and spleen from experimental models. Generate single-cell suspensions using mechanical dissociation and filtration through 40μm strainers.
- RBC Lysis: Lyse red blood cells using ammonium-chloride-potassium lysis buffer.
- Cell Staining:
- Resuspend cells in flow cytometry buffer.
- Incubate with live/dead marker for 15 minutes.
- Block Fc receptors with specific blocking solution.
- Stain with surface antibodies (anti-CD45, anti-CD11b) for 30 minutes at 4°C.
- Fix and permeabilize cells using commercial fixation/permeabilization kit.
- Stain intracellular antigens (anti-SOX9, anti-PDX1) for 30 minutes at 4°C.
- Data Acquisition and Analysis:
- Acquire data using flow cytometer.
- Analyze using FlowJo software.
- Identify CTCs as CD45-negative, SOX9-positive, and/or PDX1-positive populations.
Applications: Detection of early metastasis, monitoring treatment response, and isolation of CTCs for molecular characterization.
Signaling Pathways and Experimental Workflows
SOX9-Related Signaling Pathways in Pancreatic Cancer
Figure 1: SOX9 Signaling and Therapeutic Targeting in Pancreatic Cancer. This diagram illustrates key pathways regulating SOX9 expression (EGF/EGFR, KRAS, LIF) and downstream oncogenic processes. Dashed line indicates potential indirect regulation. Therapeutic interventions (blue) target multiple pathway components.
Experimental Workflow for SOX9 Functional Studies
Figure 2: Experimental Workflow for SOX9 Functional Studies. This workflow outlines key steps from initial cell culture through in vivo validation, highlighting parallel molecular and functional analysis pathways.
Research Reagent Solutions
Table 3: Essential Research Reagents for SOX9 and Immune Checkpoint Studies
| Reagent Category | Specific Examples | Application/Function | Key Considerations |
|---|---|---|---|
| SOX9 Modulation | SOX9-specific siRNA, shRNA | Knockdown studies, functional validation | Use pooled siRNA for enhanced efficiency; multiple transfections recommended [8] |
| SOX9 Detection | Anti-SOX9 antibodies (e.g., clone D8G8H) | Western blot, IHC, immunofluorescence, flow cytometry | Validate specificity; different clones may have varying affinities [13] |
| Immune Checkpoint Reagents | Anti-PD-1, Anti-PD-L1 antibodies | Blockade studies, immune profiling | Consider species compatibility (humanized vs. murine) [14] |
| Cell Line Models | PANC-1, COLO357, AsPC-1, BxPC-3 | In vitro studies | Select lines based on genetic background and SOX9 expression levels [8] [12] |
| Animal Models | Orthotopic PDAC, KPC (LSL-KrasG12D; Tp53L/L), spontaneous models | In vivo validation, therapy testing | Orthotopic models better recapitulate tumor microenvironment [14] |
| Flow Cytometry Panels | CD45, CD11b, PD-1, PD-L1, SOX9, PDX1 | Immune profiling, CTC detection | Include live/dead marker for viability assessment [13] |
SOX9 emerges as a master regulatory node in multiple cancers, with overexpression consistently correlating with poor prognosis across diverse malignancies. Its involvement in critical oncogenic processes—including proliferation, EMT, metastasis, and chemoresistance—combined with its emerging role in modulating the tumor immune microenvironment, positions SOX9 as a compelling therapeutic target. The experimental protocols, reagent solutions, and pathway analyses provided in this Application Note offer a framework for investigating SOX9 biology within the context of combination therapies with immune checkpoint blockade. Future research should prioritize the development of direct SOX9 inhibitors and optimize their integration with existing immunotherapeutic regimens to potentially overcome current limitations in cancer treatment, particularly for aggressive malignancies like pancreatic ductal adenocarcinoma.
The transcription factor SOX9 (SRY-related HMG-box 9) is increasingly recognized as a pivotal regulator in the tumor microenvironment (TME), orchestrating complex mechanisms of immune evasion that extend beyond its established role in cell-intrinsic oncogenesis. [4] [15] While SOX9 is well-known for its contributions to tumor progression, chemoresistance, and maintenance of cancer stem-like states, recent research has illuminated its function in modulating anti-tumor immunity, particularly in the context of immune checkpoint blockade therapies. [4] [16] This application note delineates the mechanisms through which SOX9 facilitates immune escape and provides detailed protocols for investigating SOX9-mediated resistance, with specific emphasis on its implications for combination therapies targeting the PD-1/PD-L1 axis. [16]
Table 1: Correlation Between SOX9 Expression and Immune Cell Infiltration in Human Cancers
| Cancer Type | Immune Population | Correlation with SOX9 | Functional Consequence | Experimental Model |
|---|---|---|---|---|
| Colorectal Cancer [4] | B cells, Resting Mast Cells, Monocytes | Negative | Reduced anti-tumor immunity | Bioinformatics analysis of TCGA data |
| Colorectal Cancer [4] | Neutrophils, Macrophages, Activated Mast Cells | Positive | Immunosuppressive TME | Bioinformatics analysis of TCGA data |
| HNSCC [16] | Fpr1+ Neutrophils | Negative (via ANXA1) | Impaired neutrophil accumulation & cytotoxic cell function | Mouse HNSCC model (4NQO-induced) |
| HNSCC [16] | CD8+ T cells, γδ T cells | Negative | Reduced infiltration and killing capacity | Mouse HNSCC model (4NQO-induced) |
| Pan-Cancer Analysis [4] | CD8+ T cells, NK cells, M1 Macrophages | Negative | Impaired effector function | Integrated bioinformatics |
| Pan-Cancer Analysis [4] | Memory CD4+ T cells | Positive | Potential role in immune regulation | Integrated bioinformatics |
Table 2: Experimental Models for Studying SOX9 in Immunotherapy Resistance
| Model System | Key Findings | Therapeutic Context | Measurement Outcomes |
|---|---|---|---|
| 4NQO-induced HNSCC mouse model [16] | SOX9+ tumor cells mediate resistance via ANXA1-FPR1 axis on neutrophils | Anti-LAG-3 + Anti-PD-1 combination therapy | Tumor volume, immune cell infiltration (scRNA-seq), survival |
| Transgenic mouse models (various) [16] | SOX9 regulates ANXA1 transcription, inducing Fpr1+ neutrophil apoptosis | Immunotherapy resistance studies | Neutrophil apoptosis assays, mitochondrial fission markers |
| Triple-Negative Breast Cancer model [17] | SOX9 identified as target for multi-epitope peptide vaccine | Vaccine development | Epitope antigenicity, immune simulation profiling |
| Glioblastoma clinical samples [11] | SOX9 expression correlates with immune infiltration and checkpoints | Prognostic biomarker identification | RNA-seq, immune cell infiltration analysis, survival correlation |
Key Mechanisms and Signaling Pathways
The SOX9-ANXA1-FPR1 Axis in Neutrophil Regulation
Recent research has elucidated a novel mechanism by which SOX9-expressing tumor cells mediate immunotherapy resistance through modulation of neutrophil function. [16] In head and neck squamous cell carcinoma (HNSCC) models resistant to anti-LAG-3 plus anti-PD-1 combination therapy, SOX9 directly regulates the expression of annexin A1 (ANXA1), which mediates apoptosis of formyl peptide receptor 1 (Fpr1)+ neutrophils through the ANXA1-FPR1 axis. [16] This interaction promotes mitochondrial fission and inhibits mitophagy by downregulating BCL2/adenovirus E1B interacting protein 3 (BNIP3) expression, ultimately preventing neutrophil accumulation in tumor tissues. [16] The reduction of Fpr1+ neutrophils impairs the infiltration and tumor cell-killing ability of cytotoxic CD8+ T and γδT cells within the tumor microenvironment, thereby leading to resistance. [16]
Diagram 1: SOX9-ANXA1-FPR1 Axis in Immunotherapy Resistance. This pathway illustrates how SOX9-expressing tumor cells mediate resistance to anti-LAG-3 plus anti-PD-1 therapy through neutrophil modulation. [16]
SOX9-Mediated Modulation of Immune Cell Infiltration
Beyond the ANXA1-FPR1 axis, SOX9 exhibits broader influence on the tumor immune microenvironment through regulation of diverse immune cell populations. Bioinformatics analyses of clinical datasets reveal that SOX9 expression negatively correlates with infiltration levels of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils in colorectal cancer, while showing positive correlation with neutrophils, macrophages, activated mast cells, and naive/activated T cells. [4] Additionally, SOX9 overexpression negatively correlates with genes associated with the function of CD8+ T cells, NK cells, and M1 macrophages, creating an "immune desert" microenvironment that promotes tumor immune escape. [4]
Experimental Protocols
Protocol: Evaluating SOX9-Mediated Therapy Resistance in HNSCC Models
Application: Investigation of SOX9 role in resistance to anti-PD-1/LAG-3 combination therapy.
Background: This protocol establishes a mouse model of HNSCC to study SOX9-mediated resistance mechanisms, particularly focusing on the SOX9-ANXA1-FPR1 axis and its impact on neutrophil function and cytotoxic cell activity. [16]
Materials:
- C57BL/6 wild-type mice
- 4-nitroquinoline 1-oxide (4NQO)
- Anti-PD-1 and anti-LAG-3 antibodies
- Tissue digestion enzymes (collagenase, hyaluronidase)
- Single-cell RNA sequencing reagents
- Antibodies for flow cytometry (CD45, CD3, CD8, Ly6G, etc.)
- Mitochondrial fission markers
Procedure:
Tumor Induction:
- Administer 4NQO (100 µg/mL) in drinking water to 8-week-old C57BL/6 mice for 16 weeks.
- Replace with normal water for additional 8 weeks to allow HNSCC development.
- Monitor weekly for lesion formation.
Therapy Administration:
- Randomize mice with similar tumor sizes into four treatment groups:
- Control IgG
- Anti-PD-1 monotherapy
- Anti-LAG-3 monotherapy
- Anti-LAG-3 plus anti-PD-1 combination therapy
- Administer treatments via intraperitoneal injection every 4 days.
- Measure tumor dimensions every 4 days using calipers.
- Randomize mice with similar tumor sizes into four treatment groups:
Resistance Classification:
- 14 days post-initial treatment, classify response based on RECIST criteria:
- Resistant: Tumor growth >20% compared to original size
- Sensitive: Tumor reduction or stable disease
- 14 days post-initial treatment, classify response based on RECIST criteria:
Tissue Collection and Processing:
- Euthanize mice at endpoint and dissect tongue tumors.
- Divide each tumor for multiple analyses:
- Flash-freeze portion in liquid nitrogen for RNA/protein
- Fix portion in formalin for histology
- Digest remaining tissue for single-cell suspension
Single-Cell RNA Sequencing:
- Process tumor tissues from three mice per group.
- Digest tissues into single-cell suspensions using collagenase/hyaluronidase.
- Perform scRNA-seq library construction following 10X Genomics protocol.
- Sequence libraries and analyze data for cell type identification and differential expression.
Immune Cell Analysis:
- Analyze immune cell infiltration by flow cytometry.
- Stain single-cell suspensions with antibodies against CD45, CD3, CD8, CD4, Ly6G, and other markers.
- Assess neutrophil apoptosis using Annexin V staining.
- Evaluate mitochondrial fission through mitoTracker and BNIP3 expression.
Molecular Validation:
- Validate SOX9 and ANXA1 expression by qRT-PCR and Western blot.
- Perform immunohistochemistry for Ki67 and cleaved-Caspase3.
- Use transgenic models to confirm SOX9-ANXA1 regulatory relationship.
Expected Outcomes: Resistant tumors should show significant enrichment of SOX9+ tumor cells, increased ANXA1 expression, reduced Fpr1+ neutrophil accumulation, and impaired cytotoxic T cell infiltration compared to sensitive tumors. [16]
Protocol: Assessing SOX9 Expression Patterns in Human GBM Samples
Application: Correlation of SOX9 expression with immune infiltration and checkpoint expression in glioblastoma.
Background: This bioinformatics protocol analyzes SOX9 expression in relation to immune cell infiltration and checkpoint markers using publicly available datasets, providing insights into SOX9's role in the immunosuppressive tumor microenvironment. [11]
Materials:
- RNA sequencing data from TCGA and GTEx databases
- R statistical software with appropriate packages (DESeq2, ggplot2, GSVA)
- LinkedOmics database access
- Metascape platform for enrichment analysis
- Human Protein Atlas database access
Procedure:
Data Acquisition:
- Download HTSeq-FPKM and HTSeq-Count data for GBM samples from TCGA.
- Obtain normal brain tissue expression data from GTEx.
- Retrieve protein-level expression data from Human Protein Atlas.
Differential Expression Analysis:
- Compare SOX9 expression between tumor and normal tissues using DESeq2.
- Generate volcano plots with ggplot2 to visualize significant DEGs.
- Set thresholds at |logFC| >2 and adjusted p-value <0.05.
Immune Infiltration Analysis:
- Use ssGSEA and ESTIMATE algorithms to quantify immune cell infiltration.
- Apply GSVA package to calculate enrichment scores for immune cell signatures.
- Correlate SOX9 expression with immune cell scores using Spearman's test.
Immune Checkpoint Correlation:
- Extract expression data for known immune checkpoints (PD-1, PD-L1, CTLA-4, etc.).
- Perform Wilcoxon rank sum test to analyze correlation with SOX9 expression.
- Generate heatmaps of top correlated genes.
Functional Enrichment Analysis:
- Perform GO and KEGG pathway analysis on SOX9-correlated genes.
- Use Metascape for visualization of enriched terms.
- Conduct GSEA to elucidate functional differences between high/low SOX9 groups.
Survival and Prognostic Analysis:
- Perform Kaplan-Meier analysis for overall survival based on SOX9 expression.
- Use univariate and multivariate Cox regression for prognosis analysis.
- Generate nomogram prognostic model incorporating SOX9 and clinical variables.
Expected Outcomes: High SOX9 expression in GBM correlates with specific immune infiltration patterns and checkpoint expression, particularly in IDH-mutant cases, and serves as an independent prognostic factor. [11]
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating SOX9 in Immune Evasion
| Reagent/Category | Specific Examples | Function/Application | Research Context |
|---|---|---|---|
| Animal Models | 4NQO-induced HNSCC mouse model [16] | Studies of SOX9 in therapy resistance | In vivo evaluation of anti-PD-1/LAG-3 resistance mechanisms |
| Animal Models | Various transgenic mouse models [16] | Validation of SOX9-ANXA1-FPR1 axis | Confirmation of molecular mechanisms in neutrophil regulation |
| Therapeutic Antibodies | Anti-PD-1, Anti-LAG-3 [16] | Immune checkpoint blockade studies | Modeling combination immunotherapy and resistance |
| Bioinformatics Tools | TCGA, GTEx databases [11] | Analysis of SOX9 expression patterns | Correlation with immune infiltration across cancer types |
| Bioinformatics Tools | Single-cell RNA sequencing [16] | Tumor microenvironment deconvolution | Identification of SOX9+ tumor cell subpopulations |
| Cell Type Markers | Fpr1, Ly6G (neutrophils) [16] | Identification of specific immune subsets | Tracking neutrophil accumulation and apoptosis |
| Cell Type Markers | CD8, CD3 (T cells) [16] | Cytotoxic lymphocyte quantification | Assessment of T cell infiltration and function |
| Molecular Tools | SOX9-specific antibodies [4] [11] | Protein expression detection | IHC, Western blot for SOX9 validation |
| Molecular Tools | ANXA1, BNIP3 detection reagents [16] | Pathway component analysis | Validation of mitochondrial fission and mitophagy markers |
| Vaccine Components | SOX9 multi-epitope peptides [17] | Immunotherapy development | TNBC vaccine design targeting SOX9 |
Therapeutic Implications and Future Directions
The investigation of SOX9-mediated immune evasion mechanisms reveals promising therapeutic avenues, particularly in the context of combination strategies with PD-1/PD-L1 blockade. The development of a multi-epitope peptide vaccine targeting SOX9 for triple-negative breast cancer demonstrates the feasibility of directly targeting this transcription factor. [17] This vaccine design incorporated B-cell, helper T lymphocyte, and cytotoxic T lymphocyte epitopes with high antigenicity, non-toxicity, and non-allergenicity, linked with appropriate spacers and fused to the 50S ribosomal protein L7/L12 adjuvant. [17] Computational analyses predicted favorable interactions with TLR2 and TLR4 receptors and strong cellular and humoral immune responses. [17]
For researchers exploring SOX9 targeting in combination with PD-1/PD-L1 blockade, several strategic considerations emerge. First, assessment of SOX9 expression and its correlation with neutrophil infiltration may identify patient populations most likely to benefit from combination approaches. Second, simultaneous targeting of the ANXA1-FPR1 axis may overcome SOX9-mediated resistance mechanisms. Finally, the context-dependent dual functions of SOX9—potentially beneficial in some tissue regeneration contexts while detrimental in cancer—necessitate careful therapeutic window evaluation. [4] [18]
Diagram 2: Therapeutic Strategy for SOX9 Targeting in Combination Immunotherapy. This workflow outlines a precision medicine approach for integrating SOX9 assessment and targeting with PD-1/PD-L1 blockade. [16] [17]
SOX9 Correlations with Immune Cell Infiltration and Checkpoint Molecule Expression
The transcription factor SOX9 (SRY-related HMG-box 9) has emerged as a critical regulator in both development and disease, particularly in cancer. Recent evidence has established that beyond its known roles in tumor progression, SOX9 significantly influences the tumor immune microenvironment [4]. This application note details the complex correlations between SOX9 expression, immune cell infiltration, and immune checkpoint molecule expression, providing essential methodological protocols for researchers investigating SOX9 in the context of PD-1/PD-L1 blockade combination therapies. Understanding these relationships is paramount for developing novel therapeutic strategies that simultaneously target cancer cells and modulate immunosuppressive microenvironments.
SOX9 Expression Patterns in Pan-Cancer Analyses
Comprehensive pan-cancer analyses reveal that SOX9 expression is significantly upregulated in the majority of cancer types compared to matched healthy tissues. Studies utilizing data from The Cancer Genome Atlas (TCGA) and Genotype-Tissue Expression (GTEx) databases demonstrate that among 33 cancer types, SOX9 expression is significantly increased in fifteen cancers, including Glioblastoma (GBM), colorectal cancer (COAD), liver cancer (LIHC), lung squamous cell carcinoma (LUSC), and pancreatic cancer (PAAD). Conversely, SOX9 expression is decreased in only two cancer types: skin cutaneous melanoma (SKCM) and testicular germ cell tumors (TGCT) [19].
Table 1: SOX9 Expression and Prognostic Significance Across Selected Cancers
| Cancer Type | SOX9 Expression vs. Normal | Correlation with Overall Survival | Key Immune Correlations |
|---|---|---|---|
| Glioblastoma (GBM) | Significantly Increased [11] [20] | Better prognosis in lymphoid invasion subgroups [11] | Correlated with immune infiltration & checkpoints [11] |
| Thymic Epithelial Tumors (TET) | Highly expressed in tumor cell nuclei [21] | High expression indicates unfavorable outcomes [21] | Associated with M2 macrophage dominance [21] |
| Lung Adenocarcinoma | Upregulated [11] | Correlates with poorer survival [11] | Mutually exclusive with various immune checkpoints [11] |
| Colorectal Cancer (CRC) | Significantly Increased [19] [22] | Overexpression associated with poor survival [22] | Negative correlation with B cells, resting mast cells; positive with neutrophils, macrophages [4] |
| Head and Neck SCC | Enriched in therapy-resistant cells [16] | N/A (Associated with therapy resistance) | Mediates reduction of Fpr1+ neutrophils [16] |
The prognostic significance of SOX9 varies by cancer type. For instance, high SOX9 expression is positively correlated with the worst overall survival in LGG, CESC, and THYM, suggesting its potential utility as a prognostic biomarker [19]. Surprisingly, in glioblastoma, high SOX9 expression was remarkably associated with better prognosis in specific patient subgroups, such as those with lymphoid invasion, highlighting the context-dependent nature of its function [11] [20].
Correlations with Immune Cell Infiltration
SOX9 expression demonstrates consistent and significant correlations with the composition of immune cell infiltrates in the tumor microenvironment, which has profound implications for immunotherapy response.
Innate Immune Cell Populations
- Macrophages: A strong positive correlation exists between SOX9 expression and M2 macrophage infiltration in thymic epithelial tumors [21]. M2 macrophages are generally considered immunosuppressive and pro-tumorigenic, contributing to an immune-evasive microenvironment.
- Neutrophils: In colorectal cancer, SOX9 expression shows a positive correlation with neutrophil infiltration [4]. Recent research in head and neck squamous cell carcinoma (HNSCC) has identified a novel mechanism where SOX9+ tumor cells mediate apoptosis of Fpr1+ neutrophils via the ANXA1-FPR1 axis, thereby preventing neutrophil accumulation and contributing to resistance against anti-LAG-3 plus anti-PD-1 combination therapy [16].
- Dendritic Cells (DCs): The relationship appears to be cancer-type specific. In colorectal cancer, SOX9 shows variable correlations with different DC subsets [4].
Adaptive Immune Cell Populations
- T Lymphocytes: SOX9 expression negatively correlates with genes associated with the function of CD8+ T cells [4]. In HNSCC, the reduction of Fpr1+ neutrophils mediated by SOX9+ tumor cells subsequently impairs the infiltration and tumor-killing ability of cytotoxic CD8+ T cells [16]. The correlation with Tregs and CD4+ T cells varies across cancer types [4].
- B Lymphocytes: In colorectal cancer, SOX9 expression negatively correlates with B cell infiltration [4]. SOX9 is also overexpressed in certain B-cell lymphomas, such as Diffuse Large B-cell Lymphoma (DLBCL), where it acts as an oncogene [4].
Table 2: Summary of SOX9 Correlations with Tumor-Infiltrating Immune Cells
| Immune Cell Type | Correlation with SOX9 Expression | Functional Consequences |
|---|---|---|
| M2 Macrophages | Positive (e.g., in TETs) [21] | Promotes immunosuppressive TME |
| Neutrophils | Positive (e.g., in CRC) [4]; Mediates Fpr1+ neutrophil apoptosis (HNSCC) [16] | Contributes to immune evasion and therapy resistance |
| CD8+ T Cells | Negative correlation with function [4] | Reduces cytotoxic anti-tumor immunity |
| B Cells | Negative (e.g., in CRC) [4] | Diminishes humoral anti-tumor response |
| Plasma Cells | Negative (e.g., in CRC) [4] | May reduce antibody production |
| Mast Cells | Variable (Negative for resting, Positive for activated) [4] | Context-dependent immunomodulation |
Relationships with Immune Checkpoint Molecules
SOX9 expression is intricately linked to the expression of various immune checkpoint molecules, which are critical targets for cancer immunotherapy. In glioblastoma, correlation analysis indicated that SOX9 expression was significantly correlated with the expression of multiple immune checkpoints [11]. Bioinformatic analyses of thymoma revealed that genes negatively associated with SOX9 expression were mapped to pathways involved in PD-L1 expression and the PD-1 checkpoint pathway in cancer [21]. This inverse relationship suggests that high SOX9 expression may suppress certain immune checkpoint pathways, potentially contributing to an immunosuppressive landscape that differs from the classical PD-1/PD-L1 axis.
Furthermore, research in lung adenocarcinoma has found that SOX9 suppresses the tumor microenvironment and is mutually exclusive with various tumor immune checkpoints [11]. This complex interplay indicates that SOX9 activity creates a distinct immunological context that must be understood when designing combination therapies involving checkpoint blockade.
Experimental Protocols for Investigating SOX9-Immune Correlations
Bioinformatics Analysis of SOX9 Expression and Immune Infiltration
Purpose: To analyze SOX9 expression patterns and their correlation with immune cell infiltration across cancer types using public databases.
Materials and Reagents:
- Computer with R statistical environment
- TCGA and GTEx datasets (available via UCSC Xena Browser)
- R packages:
limma,DESeq2,ggplot2,GSVA,ESTIMATE
Procedure:
- Data Acquisition: Download RNA-seq data (HTSeq-FPKM/Counts) for your cancer of interest from TCGA and normal tissue data from GTEx.
- Differential Expression Analysis: Use the
DESeq2R package to compare SOX9 expression between tumor and normal samples. Set significance thresholds at |logFC| > 1 and adjusted p-value < 0.05. - Immune Infiltration Estimation: Utilize the
GSVApackage with ssGSEA algorithm to estimate immune cell infiltration scores based on established gene signatures. - Correlation Analysis: Perform Spearman correlation between SOX9 expression and immune cell infiltration scores.
- Immune Checkpoint Correlation: Extract expression data for key checkpoint genes (PD-1, PD-L1, CTLA-4, LAG-3) and correlate with SOX9 expression using Wilcoxon rank sum test.
- Visualization: Generate heatmaps, volcano plots, and correlation scatter plots using
ggplot2.
Validation: Confirm protein-level expression using immunohistochemistry on patient tissue sections with anti-SOX9 antibodies [21].
Functional Validation in Therapy Resistance Models
Purpose: To investigate the functional role of SOX9 in mediating resistance to combination immunotherapy.
Materials and Reagents:
- C57BL/6 wild-type mice
- 4-nitroquinoline 1-oxide (4NQO) for HNSCC induction
- Anti-PD-1 and anti-LAG-3 blocking antibodies
- Single-cell RNA sequencing platform
- Transgenic mouse models for Sox9 manipulation
Procedure:
- Tumor Model Establishment: Induce HNSCC in mice by administering 4NQO in drinking water for 16 weeks, followed by normal water for 8 weeks [16].
- Therapy Administration: Randomize tumor-bearing mice into treatment groups: control IgG, anti-PD-1 monotherapy, anti-LAG-3 monotherapy, and anti-LAG-3 plus anti-PD-1 combination therapy.
- Resistance Identification: Monitor tumor size every 4 days. Classify tumors as resistant if they grow >20% larger than original size post-treatment [16].
- Single-Cell RNA Sequencing: Pool resistant and sensitive tumor tissues (n=3 per group), digest into single-cell suspensions, and perform scRNA-seq.
- Data Analysis: Use CopyKAT to distinguish malignant cells, then cluster epithelial cells to identify Sox9+ subpopulations.
- Mechanistic Validation: Employ various transgenic mouse models to validate the SOX9-ANXA1-FPR1 axis in mediating neutrophil apoptosis and therapy resistance.
Key Applications: This protocol is essential for investigating SOX9-mediated resistance mechanisms to immune checkpoint inhibitors and identifying potential therapeutic targets to overcome resistance.
Signaling Pathways and Mechanisms
SOX9-ANXA1-FPR1 Axis in Therapy Resistance
Diagram 1: SOX9-Mediated Resistance to Combination Immunotherapy. This pathway illustrates how SOX9+ tumor cells drive resistance to anti-LAG-3 plus anti-PD-1 therapy through the ANXA1-FPR1 axis, leading to neutrophil apoptosis and impaired cytotoxic immune cell function [16].
SOX9 in Immune Microenvironment Remodeling
Diagram 2: SOX9 in Tumor Immune Microenvironment Remodeling. This diagram summarizes how high SOX9 expression orchestrates broad changes in immune cell composition and checkpoint molecule expression to create an immunosuppressive microenvironment [11] [4] [21].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating SOX9-Immune Correlations
| Reagent / Tool | Function/Application | Examples/Specifications |
|---|---|---|
| Anti-SOX9 Antibodies | Detection and quantification of SOX9 protein expression | Polyclonal rabbit anti-SOX9 (e.g., AB5535; Sigma-Aldrich) for IHC [21] |
| Immune Checkpoint Inhibitors | Functional studies of SOX9 in therapy resistance | Anti-PD-1 (Nivolumab), Anti-LAG-3 (Relatlimab) for in vivo models [16] |
| TCGA & GTEx Datasets | Bioinformatics analysis of SOX9 expression | RNA-seq data accessible via UCSC Xena Browser [11] [19] |
| Single-Cell RNA Seq Platform | Characterization of SOX9+ cell populations in TME | 10X Genomics platform for identifying Sox9+ subpopulations [16] |
| R Bioinformatics Packages | Computational analysis of SOX9-immune correlations | limma, DESeq2, GSVA, ESTIMATE packages [11] [19] |
| Cordycepin | Small molecule inhibitor of SOX9 expression | Adenosine analog; inhibits SOX9 mRNA and protein in dose-dependent manner [19] |
| 4NQO-Induced HNSCC Model | In vivo study of SOX9 in therapy resistance | C57BL/6 mice treated with 4NQO in drinking water for 16 weeks [16] |
| Transgenic Mouse Models | Functional validation of SOX9 mechanisms | Sox9 manipulation in epithelial cells to assess impact on immune cells [16] |
SOX9 represents a pivotal regulator at the intersection of tumor biology and immunology, with demonstrated correlations to immune cell infiltration and checkpoint molecule expression. The experimental protocols and analytical frameworks provided in this application note equip researchers with standardized methodologies to investigate SOX9 in the context of combination therapies with PD-1/PD-L1 blockade. As research progresses, targeting SOX9 may emerge as a viable strategy to overcome resistance to immune checkpoint inhibitors and restore anti-tumor immunity across multiple cancer types.
The Dual Role of SOX9 in Tumor Immunity and Tissue Repair
The transcription factor SOX9 (SRY-related HMG-box 9) exemplifies the complexity of biological systems, functioning as a dual-regulatory molecule with context-dependent roles in both pathological and physiological processes [4]. Within the framework of PD-1/PD-L1 blockade research, understanding SOX9's paradoxical functions becomes critical for developing effective combination therapies. This application note synthesizes current evidence on SOX9's mechanisms in suppressing anti-tumor immunity while promoting tissue repair, providing structured experimental data, validated protocols, and strategic insights for researchers and drug development professionals targeting this multifaceted protein in immuno-oncology.
SOX9 in Tumor Immunity: Mechanisms and Therapeutic Implications
SOX9 as a Master Regulator of Immunosuppression
SOX9 drives tumor immune evasion through multiple interconnected mechanisms that create an immunosuppressive tumor microenvironment (TME). In KrasG12D-driven lung adenocarcinoma (LUAD), SOX9 knockout via CRISPR/Cas9 or Cre-LoxP approaches significantly reduced tumor development, burden, and progression, contributing to markedly improved overall survival in murine models [23]. The pro-tumorigenic effects of SOX9 were substantially attenuated in immunocompromised mice compared to syngeneic counterparts, indicating its immunosuppressive functions depend heavily on interactions with the immune system [23].
Mechanistically, SOX9 suppresses immune cell infiltration and functionally impairs tumor-associated CD8+ T cells, natural killer (NK) cells, and dendritic cells [23]. This creates an "immune desert" microenvironment conducive to tumor progression. Additionally, SOX9 significantly elevates collagen-related gene expression and increases collagen fiber deposition, potentially increasing tumor stiffness and physically impeding immune cell penetration [23].
Table 1: SOX9-Mediated Correlations with Immune Cell Infiltration Across Cancers
| Cancer Type | Positive Correlation With | Negative Correlation With | Experimental Model | Citation |
|---|---|---|---|---|
| Colorectal Cancer | Neutrophils, Macrophages, Activated mast cells, Naive/activated T cells | B cells, Resting mast cells, Resting T cells, Monocytes, Plasma cells, Eosinophils | Bioinformatics analysis of TCGA data | [4] |
| Lung Adenocarcinoma | Collagen deposition, M2 macrophages | CD8+ T cells, NK cells, Dendritic cells | KrasG12D mouse model, CRISPR/Cas9 knockout | [23] |
| Glioblastoma | Better prognosis in IDH-mutant subgroups | CD8+ T cell function, NK cell function | TCGA/GTEx database analysis | [11] [20] |
| Multiple Cancers | Memory CD4+ T cells | CD8+ T cells, NK cells, M1 macrophages | Pan-cancer bioinformatics analysis | [4] |
SOX9 in Immunotherapy Resistance
Emerging evidence positions SOX9 as a key mediator of resistance to combination immunotherapy. In head and neck squamous cell carcinoma (HNSCC) models, SOX9+ tumor cells were significantly enriched in tumors resistant to anti-LAG-3 plus anti-PD-1 therapy [16]. These resistant SOX9+ cells directly regulate annexin A1 (Anxa1) expression, mediating apoptosis of formyl peptide receptor 1 (Fpr1)+ neutrophils through the Anxa1-Fpr1 axis [16].
This pathway promotes mitochondrial fission and inhibits mitophagy by downregulating BCL2/adenovirus E1B interacting protein 3 (Bnip3) expression, ultimately preventing neutrophil accumulation in tumor tissues [16]. The reduction of Fpr1+ neutrophils subsequently impairs the infiltration and tumor-killing capacity of cytotoxic CD8+ T and γδT cells within the TME, establishing a mechanistic basis for resistance to combination immune checkpoint blockade [16].
In breast cancer, SOX9 facilitates immune evasion through a SOX9-B7x (B7-H4/VTCN1) axis that safeguards dedifferentiated tumor cells from immune surveillance, driving cancer progression by protecting against tumor-infiltrating lymphocytes [24].
Figure 1: SOX9-Mediated Mechanisms of Immune Suppression and Therapy Resistance. SOX9 drives immunosuppression through multiple pathways including collagen deposition, Anxa1-mediated neutrophil apoptosis, and B7x immune checkpoint expression.
SOX9 in Tissue Repair: Protective Functions and Therapeutic Applications
Central Nervous System Protection
Contrasting its pro-tumorigenic role in cancer, SOX9 demonstrates protective functions in tissue homeostasis and repair, particularly in neurodegenerative contexts. In Alzheimer's disease models, boosting SOX9 expression in astrocytes enhanced clearance of amyloid-β plaques, with higher SOX9 levels improving cognitive performance in mice that had already developed memory deficits [18] [25]. The mechanism involves SOX9 enhancing astrocyte phagocytic activity, effectively enabling these support cells to remove toxic plaque buildup "like a vacuum cleaner" [18].
Experimentally, lowering SOX9 led to accelerated plaque buildup, reduced structural complexity in astrocytes, and diminished plaque-clearing capacity [18]. Conversely, elevating SOX9 increased astrocyte activity, supported plaque removal, and preserved cognitive function, suggesting astrocyte engagement via SOX9 may help slow cognitive decline in neurodegenerative disorders [18] [25].
Context-Dependent Tumor Suppressor Activity
Paradoxically, SOX9 can also function as a tumor suppressor in specific contexts. In colorectal cancer (CRC), SOX9 inactivation occurs frequently through mutations or expression of MiniSOX9, a dominant-negative inhibitor [26]. Restoring wild-type SOX9 activity in DLD-1 CRC cells inhibited cell growth, clonal capacity, and colonosphere formation while decreasing oncogenic Wnt/β-catenin signaling and c-myc expression [26]. This tumor-suppressive activity required physical interaction with nuclear β-catenin rather than SOX9's transcriptional function, demonstrating a non-canonical mechanism of action [26].
Table 2: Dual Roles of SOX9 in Tissue Homeostasis and Disease
| Biological Context | SOX9 Role | Mechanism | Therapeutic Implication | Citation |
|---|---|---|---|---|
| Alzheimer's Disease | Protective | Enhances astrocyte phagocytosis of amyloid plaques | Potential neurodegenerative therapy | [18] [25] |
| Colorectal Cancer | Context-dependent tumor suppressor | Inhibits Wnt/β-catenin signaling, reduces c-myc | Restoration of SOX9 activity | [26] |
| Cartilage Formation & Osteoarthritis | Protective | Maintains macrophage function, promotes cartilage formation | Tissue regeneration and repair | [4] |
| Lung Adenocarcinoma | Oncogenic driver | Suppresses CD8+ T, NK, and dendritic cell infiltration | SOX9 inhibition therapy | [23] |
| Breast Cancer | Promoter of immune evasion | Upregulates B7x immune checkpoint | Combination targeting with PD-1/PD-L1 | [24] |
Experimental Protocols for Investigating SOX9 in Immuno-Oncology
Protocol: Evaluating SOX9 in Immunotherapy Resistance Models
Objective: Establish SOX9-mediated resistance to anti-PD-1/anti-LAG-3 combination therapy in HNSCC models.
Materials and Methods:
- Animal Model: C57BL/6 wild-type mice with 4-nitroquinoline 1-oxide (4NQO)-induced HNSCC
- Treatment Groups: Control IgG, anti-PD-1 monotherapy, anti-LAG-3 monotherapy, anti-LAG-3 + anti-PD-1 combination
- Resistance Criteria: Tumors growing >20% larger than original size 14 days post-treatment (RECIST criteria)
- Single-cell RNA Sequencing: Pool tumor tissues from 3 mice per group; digest into single-cell suspensions; target >30,000 cells total across conditions
- Epithelial Cell Subclustering: Use CopyKAT to distinguish malignant from non-malignant cells; identify SOX9+ subpopulations
- Validation: Employ various transgenic mouse models to confirm SOX9-Anxa1-Fpr1 axis mechanism [16]
Key Parameters:
- Monitor tumor progression every 4 days from initial treatment
- Assess survival rates across treatment groups
- Evaluate immune cell proportions via scRNA-seq cell type identification (epithelial cells: Krt14, Krt5, Krt6a; fibroblasts: Col1a1, Col3a1, Apod; endothelial cells: Flt1, Pecam1, Eng; immune cells: Ptprc, Cd74, Cd3g)
- Measure neutrophil apoptosis and mitophagy markers (BNIP3)
Protocol: Assessing SOX9 in Astrocyte-Mediated Clearance
Objective: Determine how SOX9 enhancement promotes amyloid plaque clearance in Alzheimer's models.
Materials and Methods:
- Animal Models: Alzheimer's mouse models with pre-existing cognitive impairment and amyloid plaques
- Sox9 Manipulation: Either increase or remove Sox9 expression; monitor cognitive performance for 6 months
- Behavioral Tests: Object recognition and location memory assays
- Tissue Analysis: Post-behavioral brain examination for plaque accumulation and astrocyte structural complexity
- Experimental Timeline: Conduct experiments in symptomatic models more relevant to human Alzheimer's presentation [18]
Key Parameters:
- Quantitative plaque measurements pre- and post-intervention
- Astrocyte morphological complexity analysis
- Cognitive performance metrics across intervention groups
- Correlation between SOX9 levels, plaque clearance, and cognitive preservation
Research Reagent Solutions for SOX9 Studies
Table 3: Essential Research Reagents for SOX9 Investigation
| Reagent/Cell Line | Application | Key Features/Function | Citation |
|---|---|---|---|
| DLD-1 CRC Cell Line | SOX9 tumor suppressor studies | Heterozygous L142P inactivating SOX9 mutation; suitable for restoration studies | [26] |
| KrasG12D LUAD Mouse Model | SOX9 oncogenic function studies | CRISPR/Cas9 or Cre-LoxP Sox9 knockout; assesses tumor development and immune infiltration | [23] |
| 4NQO-induced HNSCC Mouse Model | Immunotherapy resistance studies | Develops resistance to anti-LAG-3 + anti-PD-1; enables SOX9+ tumor cell identification | [16] |
| Alzheimer's Mouse Models | Tissue repair studies | Pre-existing cognitive impairment and amyloid plaques; tests SOX9 enhancement effects | [18] [25] |
| Anti-LAG-3 + Anti-PD-1 Antibodies | Combination therapy resistance | Induces resistance enriched in SOX9+ tumor cells; enables mechanism studies | [16] |
Strategic Integration with PD-1/PD-L1 Blockade Research
The dual nature of SOX9 presents both challenges and opportunities for combination with PD-1/PD-L1 blockade strategies. For therapeutic development, several key considerations emerge:
First, context-specific targeting is essential - SOX9 inhibition may enhance anti-tumor immunity in LUAD and HNSCC, while SOX9 activation could be beneficial in neurodegenerative conditions or specific cancer subtypes like IDH-mutant glioblastoma [11] [20].
Second, temporal regulation of SOX9 targeting must be carefully considered, as evidenced by the Alzheimer's models where SOX9 enhancement after symptom onset still provided benefit [18].
Third, combinatorial approaches that simultaneously target SOX9-mediated immunosuppressive mechanisms (e.g., collagen deposition, neutrophil apoptosis) while enhancing immune activation through PD-1/PD-L1 blockade may yield synergistic effects.
Figure 2: Strategic Integration of SOX9 Targeting with PD-1/PD-L1 Blockade. Combination approaches must consider context-specific SOX9 modulation to simultaneously enhance T-cell activation while reducing SOX9-mediated immunosuppression.
Future research directions should prioritize developing conditional SOX9 modulation strategies that can be spatially and temporally controlled, tissue-specific delivery systems to minimize off-target effects on SOX9's protective functions, and biomarkers for identifying patients most likely to benefit from SOX9-targeting combinations with PD-1/PD-L1 blockade.
Advanced Approaches for Targeting SOX9 in Combination Immunotherapy
The transcription factor SOX9 is a pivotal regulator of embryonic development, cell differentiation, and stem cell maintenance. In oncology, SOX9 has emerged as a compelling therapeutic target due to its frequent overexpression in diverse malignancies and its association with key oncogenic processes, including tumor proliferation, metastasis, chemoresistance, and immune evasion [4] [27]. Within the context of cancer immunotherapy, SOX9 exhibits a "double-edged sword" functionality in immunobiology; it can promote tumor immune escape by impairing immune cell function, yet in certain contexts, it helps maintain macrophage function and tissue repair [4]. This complex role makes SOX9 an intriguing target for combination strategies with immune checkpoint blockers. The following application note details current experimental strategies for direct and indirect SOX9 targeting, providing methodologies and resources to support research in this evolving field.
SOX9-Targeting Agent Profiles
Table 1: Direct and Indirect SOX9-Targeting Agents
| Agent Name | Target | Mechanism Related to SOX9 | Experimental Context | Key Quantitative Findings |
|---|---|---|---|---|
| THZ2 [28] | CDK7 | Covalent inhibitor of super-enhancer component; suppresses expression of SE-associated gene SOX9. | Glioblastoma (GBM) cells and TMZ-resistant lines. | Synergistic effect with TMZ (Combination Index calculated); reversed TMZ resistance. |
| JQ1 [28] | BRD4 | Inhibits super-enhancer activity; suppresses SOX9 expression. | Glioblastoma (GBM) cells. | Exhibits synergistic antitumor effects with temozolomide (TMZ). |
| AZ1 [29] | USP28 | Specific inhibitor that disrupts USP28-SOX9 interaction, promoting SOX9 ubiquitination and degradation. | Ovarian cancer cells and PARPi-resistant models. | Reduced SOX9 protein stability; increased sensitivity to PARP inhibitor Olaparib. |
Detailed Experimental Protocols
Protocol: Targeting SOX9-Mediated Chemoresistance with Super-Enhancer Inhibitors
This protocol outlines the use of super-enhancer inhibitors to counteract SOX9-dependent chemoresistance in glioblastoma, based on the work of Wang et al. [28].
Materials and Reagents
- Human GBM cell lines (e.g., A172, U118MG, U87MG, U251).
- THZ2 (CDK7 inhibitor) and JQ1 (BET inhibitor).
- Temozolomide (TMZ).
- Cell culture reagents: DMEM/high-glucose medium, fetal bovine serum (FBS), penicillin/streptomycin.
- Assay kits: CCK-8 kit for cell viability, Transwell chambers for migration/invasion, flow cytometry reagents for cell cycle and apoptosis.
- Antibodies for CUT&RUN: anti-CDK7, anti-BRD4, anti-H3K27ac, anti-SOX9.
Step-by-Step Procedure
Establishment of TMZ-Resistant Cell Lines:
- Culture log-phase GBM cells (e.g., U87MG) and determine the IC50 of TMZ using a CCK-8 assay.
- Expose cells to stepwise increasing concentrations of TMZ, starting from 1/100 of the IC50.
- Maintain each concentration for 14 days before escalating to allow for cellular adaptation.
Assessment of Combinatorial Effects:
- Seed GBM cells (5×10³ cells/well for standard assays, 2×10³ for time-course) in 96-well plates.
- Treat cells with gradient concentrations of THZ2, JQ1, and/or TMZ, both individually and in combination.
- Incubate with CCK-8 solution for 1 hour at 37°C after the desired treatment period (e.g., 24-72 hours).
- Measure absorbance at 450 nm. Calculate the Combination Index (CI) using appropriate software (e.g., CompuSyn) to quantify synergy.
Functional Analysis of SOX9 Suppression:
- Migration/Invasion Assay: Seed serum-starved cells into the upper chamber of a Transwell insert (uncoated for migration, Matrigel-coated for invasion). Treat with inhibitors. After 48 hours, fix, stain with crystal violet, and count migrated/invaded cells.
- Cell Cycle Analysis: After treatment, fix cells in ice-cold 70% ethanol, stain with Propidium Iodide (PI)/RNase A buffer, and analyze DNA content by flow cytometry.
- Apoptosis Assay: Use Annexin V/PI staining followed by flow cytometry to quantify apoptotic cells.
Mechanistic Validation via CUT&RUN Assay:
- Harvest approximately 500,000 cells per condition.
- Permeabilize cells and incubate with concanavalin A-coated magnetic beads.
- Incubate bead-bound chromatin with target-specific primary antibodies (e.g., anti-CDK7, anti-BRD4, anti-SOX9, anti-H3K27ac) overnight at 4°C.
- Add protein A-MNase fusion protein to cleave antibody-bound chromatin fragments.
- Release and purify the cleaved DNA fragments. Proceed with library construction and sequencing to map protein-DNA interactions and histone modifications at the SOX9 locus.
Protocol: Disrupting SOX9 Protein Stability to Overcome PARPi Resistance
This protocol describes targeting the USP28-SOX9 axis to sensitize ovarian cancer cells to PARP inhibitors [29].
Materials and Reagents
- Ovarian cancer cell lines (e.g., SKOV3, UWB1.289), including PARPi-resistant variants.
- AZ1 (USP28-specific inhibitor), Olaparib (PARPi), MG132 (proteasome inhibitor), Cycloheximide (CHX).
- Co-immunoprecipitation (Co-IP) reagents: Lysis buffer, protein A/G magnetic beads, primary antibodies (anti-USP28, anti-SOX9, anti-FBXW7, anti-Ubiquitin).
- Western blot reagents and antibodies for SOX9, γH2AX, RAD51, etc.
- ChIP-Seq kit for SOX9 DNA-binding analysis.
Step-by-Step Procedure
Protein Stability and Degradation Assay:
- Treat cells with the protein synthesis inhibitor Cycloheximide (CHX, e.g., 100 µg/mL) in the presence or absence of AZ1.
- Harvest cells at different time points (e.g., 0, 1, 2, 4, 8 hours).
- Perform Western blotting to detect SOX9 protein levels. Calculate the half-life of SOX9 by densitometric analysis.
Co-Immunoprecipitation (Co-IP) to Validate Protein Interaction:
- Lyse cells from different treatment groups (e.g., control, Olaparib-treated).
- Incubate 800 µg of total protein lysate with anti-SOX9 antibody or normal IgG (control) overnight at 4°C.
- Add protein A/G magnetic beads and incubate for 2 hours.
- Wash beads, boil in SDS loading buffer, and analyze the immunoprecipitates by Western blotting using antibodies against USP28 and FBXW7.
Analysis of DNA Damage Repair (DDR):
- Treat cells with AZ1 and/or Olaparib.
- Monitor DDR by Western blotting for key markers such as γH2AX (DNA double-strand breaks) and RAD51 (homologous recombination).
- Perform immunofluorescence staining for γH2AX foci and quantify foci per nucleus.
Identification of SOX9 Transcriptional Targets via ChIP-Seq:
- Crosslink proteins to DNA in cells using formaldehyde.
- Sonicate chromatin to fragment DNA to 200-500 bp.
- Immunoprecipitate with an anti-SOX9 antibody.
- Reverse crosslinks, purify DNA, and construct sequencing libraries. Bioinformatic analysis will reveal SOX9 binding sites on promoters of DDR genes (e.g., SMARCA4, UIMC1, SLX4).
The Scientist's Toolkit
Table 2: Essential Research Reagents for SOX9-Targeting Studies
| Reagent / Tool | Category | Primary Function in SOX9 Research | Example Application |
|---|---|---|---|
| THZ2 [28] | Small Molecule Inhibitor | Covalent CDK7 inhibitor; disrupts super-enhancer networks, downregulating SOX9 transcription. | Reverses chemoresistance in glioblastoma. |
| AZ1 [29] | Small Molecule Inhibitor | Selective USP28 inhibitor; blocks USP28-mediated deubiquitination, promoting SOX9 degradation. | Sensitizes ovarian cancer to PARP inhibitors. |
| JQ1 [28] | Small Molecule Inhibitor | BET bromodomain inhibitor; displaces BRD4 from super-enhancers, suppressing SOX9 expression. | Synergizes with standard chemotherapy. |
| Anti-SOX9 Antibody | Biological Reagent | Detects SOX9 protein expression and localization (IHC, IF, WB); used for immunoprecipitation (IP, ChIP). | Measuring SOX9 levels, identifying direct transcriptional targets. |
| siRNA/shSOX9 | Genetic Tool | Knocks down SOX9 gene expression; validates oncogenic functions and identifies phenotypic consequences. | In vitro and in vivo loss-of-function studies. |
Signaling Pathway Visualizations
USP28-SOX9 Regulatory Axis in Chemoresistance
Figure 1: USP28-SOX9 axis promotes PARPi resistance. In ovarian cancer, PARPi treatment induces USP28, which competes with the E3 ligase FBXW7 to stabilize SOX9. SOX9 then transactivates key DNA damage repair (DDR) genes, driving therapy resistance. The inhibitor AZ1 targets USP28, restoring SOX9 degradation and sensitizing cells to PARPi [29].
Super-Enhancer-Driven SOX9 Expression in GBM
Figure 2: Targeting super-enhancer complex to suppress SOX9. In glioblastoma, super-enhancers enriched with H3K27ac, CDK7, and BRD4 drive aberrant SOX9 transcription. The inhibitors THZ2 (targeting CDK7) and JQ1 (targeting BRD4) disrupt this complex, downregulating SOX9 and countering chemoresistance [28].
The transcription factor SOX9 (SRY-related HMG-box 9) has emerged as a pivotal regulator in cancer biology, playing complex, context-dependent roles in tumor progression, immune regulation, and therapy resistance [4]. Recent research has illuminated its function as a "double-edged sword" in immunology, contributing to both anti-tumor immunity and mechanisms of immune escape [4]. This application note focuses on the SOX9-ANXA1-FPR1 signaling axis, a critical downstream pathway identified as a key mediator of resistance to combined immune checkpoint blockade therapy targeting PD-1 and LAG-3 [30]. We provide comprehensive experimental protocols and analytical frameworks for investigating this pathway, with particular emphasis on its role in modulating the tumor immune microenvironment and impairing cytotoxic lymphocyte function.
Background and Significance
SOX9 in Cancer and Immunity
SOX9, a member of the SOX family of transcription factors, contains several functionally critical domains: a dimerization domain (DIM), the HMG box DNA-binding domain, and transcriptional activation domains (TAM and TAC) [4]. While traditionally recognized for its roles in development and chondrogenesis, SOX9 is frequently overexpressed in diverse malignancies including liver cancer, lung cancer, breast cancer, and gastric cancer [4] [19]. Its expression correlates strongly with poor prognosis, making it a potential diagnostic and prognostic biomarker [19] [11].
In the immunological context, SOX9 demonstrates dual functionality. It promotes immune escape by impairing immune cell function, yet also maintains macrophage function supporting tissue regeneration and repair [4]. SOX9 expression correlates significantly with altered patterns of tumor immune cell infiltration, showing negative correlations with B cells, resting mast cells, monocytes, and plasma cells, while positively correlating with neutrophils, macrophages, and specific T cell subsets [4]. These immunomodulatory properties position SOX9 as a promising therapeutic target, particularly in combination with existing immunotherapies.
The ANXA1-FPR1 Axis in Therapy Resistance
Recent investigation has revealed that SOX9 directly regulates the expression of annexin A1 (ANXA1), which mediates apoptosis of formyl peptide receptor 1 (FPR1)+ neutrophils through the ANXA1-FPR1 axis [30]. This interaction promotes mitochondrial fission and inhibits mitophagy by downregulating BCL2/adenovirus E1B interacting protein 3 (Bnip3) expression, ultimately preventing neutrophil accumulation in tumor tissues [30]. The consequent reduction of Fpr1+ neutrophils impairs the infiltration and tumor cell-killing capacity of cytotoxic CD8+ T and γδT cells within the tumor microenvironment, establishing an "immune desert" phenotype that facilitates resistance to combination immunotherapy [30].
Key Experimental Findings and Data Synthesis
SOX9-ANXA1-FPR1 Axis in Immunotherapy Resistance
Table 1: Experimental Evidence of SOX9-ANXA1-FPR1 Axis in Therapy Resistance
| Experimental Finding | Model System | Key Result | Citation |
|---|---|---|---|
| SOX9+ tumor cell enrichment in resistant samples | HNSCC mouse model, scRNA-seq | Significant enrichment of SOX9+ tumor cells in anti-LAG-3 + anti-PD-1 resistant tumors | [30] |
| ANXA1 regulation by SOX9 | Transgenic mouse models | SOX9 directly initiates ANXA1 transcription in epithelial cells | [30] |
| Neutrophil apoptosis mechanism | In vitro and in vivo analysis | ANXA1-FPR1 axis promotes mitochondrial fission and inhibits mitophagy via Bnip3 downregulation | [30] |
| Impact on cytotoxic immunity | Immune cell profiling | Reduction of Fpr1+ neutrophils impairs Cd8+ T and γδT cell infiltration and function | [30] |
| Therapy response rates | HNSCC mouse model | 42.9% (6/14) animals resistant to anti-LAG-3 + anti-PD-1 combination therapy | [30] |
SOX9 Expression Patterns in Human Cancers
Table 2: SOX9 Expression Profiles Across Human Cancers
| Cancer Type | SOX9 Expression vs. Normal Tissue | Prognostic Association | Immunological Correlations | |
|---|---|---|---|---|
| Glioblastoma (GBM) | Significantly increased | Better prognosis in lymphoid invasion subgroups; independent prognostic factor for IDH-mutant cases | Correlated with immune infiltration and checkpoint expression | [11] |
| Thymoma (THYM) | Significantly increased | Short overall survival | Negative correlation with Th17 differentiation, PD-L1 expression, and TCR signaling pathways | [19] |
| Skin Cutaneous Melanoma (SKCM) | Significantly decreased | Tumor suppressor activity | SOX9 upregulation inhibits tumorigenicity in melanoma models | [19] |
| Testicular Germ Cell Tumors (TGCT) | Significantly decreased | Not specified | Not specified | [19] |
| Multiple Cancers (15 types) | Significantly increased | Poor prognosis in LGG, CESC, THYM | Correlation with immune cell infiltration patterns | [19] |
Experimental Protocols
Protocol 1: Establishing Therapy Resistance Mouse Models
Purpose: To generate in vivo models for investigating SOX9-mediated resistance to combination immune checkpoint blockade.
Materials:
- C57BL/6 wild-type mice
- 4-nitroquinoline 1-oxide (4NQO)
- Anti-PD-1 and anti-LAG-3 blocking antibodies
- Control IgG
- MRI imaging system
Methodology:
- Induce HNSCC by administering 4NQO in drinking water to mice for 16 weeks, followed by normal water for 8 weeks.
- Select mice with similar tumor lesion sizes and randomize into four treatment groups:
- Control IgG
- Anti-PD-1 monotherapy
- Anti-LAG-3 monotherapy
- Anti-LAG-3 plus anti-PD-1 combination therapy
- Administer treatments and assess tumor size every 4 days from initial treatment.
- Classify response 14 days after initial treatment:
- Resistant tumors: >20% increase in size compared to original
- Sensitive tumors: partial reduction or complete tumor eradication
- Monitor tumor progression using magnetic resonance imaging (MRI).
- Perform histopathological examination of tongue tissue and analyze proliferation (Ki67) and apoptosis (cleaved-Caspase3) markers.
- Process tissues for single-cell RNA sequencing as described in Protocol 2.
Validation Parameters:
- Survival rates across treatment groups
- Tumor growth kinetics
- Immune cell infiltration patterns via scRNA-seq
- Proliferation and apoptosis indices [30]
Protocol 2: Single-Cell RNA Sequencing Analysis
Purpose: To characterize the tumor microenvironment and identify SOX9-mediated transcriptional programs in therapy resistance.
Materials:
- Fresh tumor tissues from resistant and sensitive models
- Single-cell suspension preparation reagents
- 10X Genomics platform
- Cell Ranger software pipeline
- R package "Seurat" for data analysis
- CopyKAT algorithm for malignant cell identification
Methodology:
- Pool tumor tissues from three mice per group (control, resistant, sensitive) and digest into single-cell suspensions.
- Split suspensions into two parts for library construction to ensure technical replication.
- Perform scRNA-seq using 10X Genomics platform following manufacturer's protocols.
- Process raw data through Cell Ranger pipeline with STAR alignment to reference genome.
- Apply quality control filters:
- Minimum 200 genes expressed per cell
- UMI count > 1000 per cell
- Mitochondrial UMI ratio < 20%
- Red blood cell gene ratio < 5%
- Integrate datasets and remove batch effects using CCA method in Seurat.
- Identify cell clusters through dimension reduction and clustering.
- Annotate cell types using canonical markers:
- Epithelial cells: Krt14, Krt5, Krt6a
- Fibroblasts: Col1a1, Col3a1, Apod
- Endothelial cells: Flt1, Pecam1, Eng
- Immune cells: Ptprc, Cd74, Cd3g
- Extract epithelial cells and use CopyKAT to distinguish malignant from non-malignant subpopulations.
- Identify differentially expressed genes and signaling pathways across resistant and sensitive groups.
Downstream Analysis:
- Cell-cell communication analysis using CellChat R package
- InferCNV for copy number variation assessment
- Transcription factor regulatory network analysis with SCENIC [30] [31]
Protocol 3: Validating SOX9-ANXA1-FPR1 Functional Interactions
Purpose: To experimentally verify the functional relationship between SOX9, ANXA1, and FPR1+ neutrophils.
Materials:
- Various transgenic mouse models
- Sox9 overexpression and knockout constructs
- ANXA1 and FPR1 detection antibodies
- Neutrophil isolation kits
- Mitochondrial function assays
- Bnip3 expression analysis tools
Methodology:
- Manipulate SOX9 expression in epithelial cells using transgenic approaches:
- Sox9 overexpression constructs
- Sox9 knockout/knockdown models
- Assess ANXA1 expression changes via:
- qRT-PCR for transcriptional regulation
- Western blot for protein expression
- Immunofluorescence for spatial localization
- Isolate Fpr1+ neutrophils from tumor tissues and co-culture with SOX9-modified tumor cells.
- Evaluate neutrophil apoptosis through:
- Annexin V/propidium iodide staining
- Caspase activation assays
- Analyze mitochondrial dynamics in Fpr1+ neutrophils:
- Mitochondrial fission/fusion markers
- Mitophagy assessment (Bnip3 expression, LC3 puncta formation)
- Examine cytotoxic immune cell function:
- CD8+ T and γδT cell infiltration assays
- Tumor cell killing capacity in co-culture systems
- Validate findings through rescue experiments with:
- ANXA1 inhibitors
- FPR1 antagonists
- Bnip3 overexpression
Key Readouts:
- SOX9-dependent ANXA1 transcription
- Neutrophil apoptosis rates
- Mitochondrial function parameters
- Cytotoxic lymphocyte-mediated killing efficiency [30]
Signaling Pathway Visualization
Figure 1: SOX9-ANXA1-FPR1 Signaling Axis in Immunotherapy Resistance. This diagram illustrates the molecular pathway through which SOX9-expressing tumor cells mediate resistance to combination immune checkpoint blockade. SOX9 directly transcriptionally regulates ANXA1, which engages FPR1 on neutrophils, triggering mitochondrial dysfunction and apoptosis via BNIP3 downregulation and impaired mitophagy. The consequent reduction in neutrophil accumulation impairs cytotoxic lymphocyte function, ultimately leading to therapy resistance.
Experimental Workflow Visualization
Figure 2: Experimental Workflow for Investigating SOX9-Mediated Therapy Resistance. This workflow outlines the key methodological stages for identifying and validating the SOX9-ANXA1-FPR1 axis, from initial model establishment through molecular validation and functional assays.
Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating the SOX9-ANXA1-FPR1 Axis
| Reagent Category | Specific Examples | Research Application | Key Features | |
|---|---|---|---|---|
| Animal Models | C57BL/6 wild-type mice; Various transgenic models (Sox9 manipulation) | In vivo therapy resistance modeling; Mechanistic validation | 4NQO-induced HNSCC; Controlled genetic background | [30] |
| Therapeutic Antibodies | Anti-PD-1; Anti-LAG-3 (Relatlimab) | Combination immunotherapy studies; Resistance modeling | Immune checkpoint blockade; Clinical relevance | [30] |
| scRNA-Seq Platform | 10X Genomics; Cell Ranger; Seurat R package | Tumor microenvironment characterization; Cellular heterogeneity analysis | Single-cell resolution; Comprehensive transcriptomic data | [30] [31] |
| Bioinformatics Tools | CopyKAT; CellChat; InferCNV; SCENIC | Malignant cell identification; Cell-cell communication; Copy number variation; TF network analysis | Specialized algorithms for cancer scRNA-seq data | [30] [31] |
| Detection Reagents | Anti-Ki67; Cleaved-Caspase3; Cell type-specific markers (Krt14, Col1a1, Ptprc) | Proliferation/apoptosis assessment; Cell type identification | Standardized immunohistochemistry; Well-characterized specificity | [30] |
| SOX9 Modulators | Cordycepin (CD); Sox9 overexpression/knockout constructs | SOX9 pathway manipulation; Therapeutic targeting | Dose-dependent SOX9 inhibition; Genetic validation | [19] |
Discussion and Future Directions
The SOX9-ANXA1-FPR1 axis represents a clinically relevant mechanism of resistance to combination immune checkpoint blockade, particularly in the context of anti-PD-1 plus anti-LAG-3 therapy [30]. The experimental protocols outlined herein provide a comprehensive framework for investigating this pathway and its implications for tumor-immune interactions. Several critical considerations emerge for therapeutic translation:
First, the context-dependent nature of SOX9 function necessitates careful patient stratification strategies. While SOX9 generally acts as an oncogene across multiple cancer types, it demonstrates tumor-suppressive activity in specific contexts such as melanoma [19]. Additionally, in glioblastoma, high SOX9 expression unexpectedly correlates with better prognosis in lymphoid invasion subgroups, highlighting tissue-specific immunological functions [11].
Second, the temporal regulation of SOX9 expression and activity presents both challenges and opportunities for therapeutic intervention. In bronchopulmonary dysplasia, SOX9 demonstrates stage-specific functions, with increased expression in early disease stages promoting beneficial differentiation of alveolar epithelial cells [32]. Similar temporal dynamics may operate in cancer contexts, requiring precise therapeutic timing.
Third, the upstream regulation of SOX9 involves multiple layers of control, including epigenetic modifications, post-transcriptional regulation by miRNAs and lncRNAs, and protein-protein interactions [4] [32]. The long noncoding RNA GAS5 has been identified as an upstream regulator of SOX9 in some pathological contexts, suggesting additional nodes for therapeutic intervention [32].
Finally, the potential for targeting downstream effectors of SOX9, particularly the ANXA1-FPR1 interaction, offers promising alternatives to direct SOX9 inhibition. Small molecule inhibitors disrupting this axis could potentially reverse the immunosuppressive microenvironment and restore sensitivity to immune checkpoint blockade [30] [31].
The experimental approaches detailed in this application note provide a roadmap for validating these therapeutic strategies and advancing our understanding of SOX9-mediated immunomodulation in cancer therapy resistance.
Disrupting the SOX9-B7x (B7-H4) Immune Checkpoint Axis
The SOX9-B7x axis represents a novel and critical immunosuppressive pathway in cancer, particularly relevant for immune-cold tumors resistant to conventional immunotherapies. The transcription factor SOX9, a key regulator of cell fate and dedifferentiation, has been identified as a direct transcriptional regulator of B7x (B7-H4, VTCN1), an immune checkpoint molecule with limited expression in normal tissues but significant overexpression in numerous solid cancers [33] [34]. This axis safeguards dedifferentiated, stem-like tumor cells from immune surveillance, facilitating tumor progression and conferring resistance to anti-PD-1/PD-L1 therapy [33] [16]. Disrupting this pathway presents a promising strategy to overcome resistance to existing immune checkpoint blockade, potentially converting immunologically inert tumors into ones susceptible to immune attack.
Key Quantitative Evidence
The following tables summarize core quantitative findings from foundational studies establishing the SOX9-B7x axis as a therapeutic target.
Table 1: Functional Consequences of SOX9 Manipulation In Vivo
| Experimental Model | Genetic/Intervention | Key Phenotypic Outcome | Reported Effect | Citation |
|---|---|---|---|---|
| C3-TAg BLBC Mouse Model | Mammary epithelium Sox9 conditional knockout (cKO) | T cell infiltration in premalignant lesions (MIN) | Massive accumulation of CD3+ T cells; Increased CD8+ & CD4+ T cells [34] | |
| C3-TAg BLBC Mouse Model | Sox9 cKO + T cell depletion | Restoration of tumor progression | Accelerated invasive tumor onset; >50% of tumors developed from Sox9-null cells [34] | |
| HNSCC Mouse Model | Enrichment of Sox9+ tumor cells | Resistance to anti-LAG-3 + anti-PD-1 therapy | Mediated via Anxa1-Fpr1 axis, reducing cytotoxic T and γδT cell infiltration [16] |
Table 2: Mechanistic Insights into the SOX9-B7x Pathway
| Experimental System | Finding | Mechanistic Insight | Citation |
|---|---|---|---|
| Mouse & Human Breast Cancer Models | SOX9 induces B7x expression | 1. Direct transcriptional regulation of B7x2. STAT3 pathway activation [33] [34] | |
| Human Breast Cancer (Patient Samples) | SOX9 and B7x correlation | SOX9 and B7x expression are correlated and associated with reduced CD8+ T cell infiltration [33] [34] | |
| Coculture with SOX9-OE Breast Cancer Cells | Suppression of human T cell function | Significant suppression of proliferation in both CD8+ and CD4+ T cells; Reduced antigen-specific T cell killing [34] | |
| Advanced Tumor Models | B7x targeting | Inhibits tumor growth and overcomes resistance to anti-PD-L1 immunotherapy [33] |
Experimental Protocols
Protocol: Evaluating the SOX9-B7x Axis in a Murine Breast Cancer Model
This protocol is adapted from studies using the C3-TAg basal-like breast cancer (BLBC) model [34].
I. Materials
- Mice: C3-TAg transgenic mice (on C57BL/6 background).
- Reagents: MMTV-iCre transgenic, Sox9Fl/Fl alleles, anti-CD4 (clone GK1.5), anti-CD8 (clone 2.43) depleting antibodies, isotype control antibodies.
II. Methods
- Animal Model Generation:
- Cross MMTV-iCre;Sox9Fl/Fl mice with C3-TAg mice to generate experimental (MMTV-iCre;Sox9Fl/Fl;C3-TAg) and control (Sox9Fl/Fl;C3-TAg) cohorts.
- Monitor mice for mammary intraepithelial neoplasia (MIN) development at ~4 months of age.
Immune Cell Profiling via Flow Cytometry:
- Tissue Processing: Harvest MIN lesions or tumors, mince with a scalpel, and digest in RPMI-1640 media containing collagenase/hyaluronidase. Grind tissue through a 70-μm cell strainer to create a single-cell suspension.
- Cell Staining:
- Resuspend cells in FACS buffer (PBS + 2% FBS).
- Incubate with Fc block (anti-CD16/32) for 10 minutes on ice.
- Stain with fluorescently conjugated antibodies against CD45, CD3, CD4, and CD8 for 30 minutes on ice in the dark.
- Wash cells and resuspend in FACS buffer containing a viability dye.
- Data Acquisition & Analysis: Acquire data on a flow cytometer (e.g., BD FACSCelesta) and analyze using software such as FlowJo. Gate on live, CD45+ leukocytes to quantify CD3+, CD4+, and CD8+ T cell populations.
T Cell Depletion Studies:
- Administer a combination of anti-CD4 (200 μg) and anti-CD8 (200 μg) antibodies intraperitoneally to Sox9-cKO;C3-TAg mice every 5 days for 2 months, starting at 3 months of age.
- Control groups receive equivalent doses of isotype control antibodies.
- Monitor tumor onset and growth by palpation and caliper measurements. Confirm T cell depletion (>90%) in peripheral blood via flow cytometry.
III. Readouts & Analysis
- Primary: Time to invasive tumor onset, tumor-free survival.
- Secondary: Immunophenotyping of tumor-infiltrating lymphocytes (TILs) by flow cytometry and immunohistochemistry (IHC) for CD3/GZMB.
- Validation: Genotype tumors to confirm SOX9 status in "escapee" tumors.
Protocol:In VitroHuman T Cell Suppression Assay
This protocol assesses the functional impact of tumor-cell SOX9 on human T cells [34].
I. Materials
- Cells: SOX9-negative human breast cancer cell line (e.g., MCF7ras) or TNBC line (e.g., HCC1937). Human Peripheral Blood Mononuclear Cells (PBMCs) from healthy donors.
- Reagents: Lentiviral vectors for SOX9 overexpression and control, anti-CD3/CD28 activation beads, human IL-2, CellTrace Violet or CFSE proliferation dye.
II. Methods
- Generation of SOX9-Expressing Tumor Cells:
- Transduce target cancer cells with SOX9-overexpressing (SOX9-OE) or empty vector control (CTRL) lentivirus.
- Select with appropriate antibiotic (e.g., puromycin) for 7-14 days to generate stable pools. Validate SOX9 and B7x protein expression by western blot or flow cytometry.
T Cell Isolation and Staining:
- Isolate PBMCs from donor blood via Ficoll density gradient centrifugation.
- Isolate CD4+ and CD8+ T cells from PBMCs using magnetic negative selection kits.
- Label isolated T cells with CellTrace Violet per manufacturer's instructions to track proliferation.
Coculture and Stimulation:
- Plate irradiated (50 Gy) CTRL or SOX9-OE tumor cells in a 96-well plate.
- Add stained T cells at a T cell:tumor cell ratio of 5:1 to 10:1.
- Stimulate T cells with soluble anti-CD3 (1 μg/mL) and anti-CD28 (1 μg/mL) antibodies or with anti-CD3/CD28 activation beads.
- Include recombinant human IL-2 (50 U/mL) in the culture medium.
- Maintain coculture for 4-5 days.
III. Readouts & Analysis
- T Cell Proliferation: Analyze by flow cytometry, measuring the dilution of CellTrace Violet in CD4+ and CD8+ T cell gates.
- Cytokine Production: After 1-2 days of coculture, restimulate T cells with PMA/ionomycin in the presence of GolgiPlug for 4-6 hours. Perform intracellular staining for IFN-γ and TNF-α, and analyze by flow cytometry.
- Cytotoxicity (Alternative): For antigen-specific killing, engineer T cells with a known TCR (e.g., NY-ESO-1-specific) and coculture with HLA-matched, antigen-positive tumor cells. Measure target cell death via real-time cell analysis or lactate dehydrogenase (LDH) release assay.
Signaling Pathway & Workflow Visualizations
Diagram 1: The core SOX9-B7x immunosuppressive signaling pathway. SOX9 drives B7x expression via STAT3 activation and direct transcriptional regulation. B7x on tumor cells then engages its putative receptor on T cells, inhibiting their proliferation and effector functions, ultimately fostering an immune-cold tumor microenvironment.
Diagram 2: Overcoming PD-1/PD-L1 resistance. Disrupting the SOX9-B7x axis enhances baseline T cell activation. When combined with PD-1/PD-L1 blockade, this creates a synergistic effect that can overcome the resistance mechanisms in immune-cold tumors, leading to effective tumor cell killing.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating the SOX9-B7x Axis
| Reagent / Tool | Function / Application | Example Specifications / Clones | Key Use-Case |
|---|---|---|---|
| Anti-B7x (B7-H4) Antibodies | Blocking/neutralizing; IHC/Flow Cytometry | Clone MIH43 (blocking); Polyclonal for IHC | Functional studies (T cell coculture); Biomarker validation [34] [35] |
| SOX9 Expression Modulators | Genetic manipulation of SOX9 | Lentiviral shRNA (knockdown); Lentiviral ORF (overexpression) | Establishing causal role in vitro and in vivo [34] |
| C3-TAg Transgenic Mice | In vivo BLBC model | MMTV-iCre;Sox9Fl/Fl;C3-TAg | Studying axis in tumor initiation, progression, and therapy [34] |
| Anti-CD3/CD28 Beads | Polyclonal T cell activation | Dynabeads Human T-Activator | In vitro T cell suppression assays [34] |
| Recombinant B7x Protein | Ligand binding studies | Fc-tagged recombinant B7x | Identifying/characterizing the B7x receptor [35] |
| Phospho-STAT3 Antibodies | Detecting pathway activation | Flow cytometry (intracellular); Western Blot | Validating STAT3 as a downstream mediator of SOX9 [33] |
Synthetic Biology and Logic-Gated CAR-T Designs for SOX9+ Tumors
The transcription factor SOX9 (SRY-related HMG-box 9) is increasingly recognized as a pivotal regulator in multiple solid malignancies, where it promotes tumor progression, stemness, and therapy resistance [4] [36]. Recent investigations have revealed its significant role in shaping an immunosuppressive tumor microenvironment (TME), particularly through the regulation of myeloid cell populations and suppression of cytotoxic T-cell infiltration [37] [4]. This application note explores the integration of synthetic biology and logic-gated CAR-T designs to target SOX9-positive tumors, framed within the context of combination strategies with PD-1/PD-L1 blockade research.
Emerging evidence demonstrates that SOX9-positive tumor cells drive resistance to combination immunotherapy (anti-PD-1 plus anti-LAG-3) in head and neck squamous cell carcinoma (HNSCC) models through a novel mechanism involving the ANXA1-FPR1 axis [37]. SOX9 directly regulates annexin A1 (ANXA1) expression, which mediates apoptosis of formyl peptide receptor 1-positive (FPR1+) neutrophils, ultimately preventing neutrophil accumulation and impairing the infiltration and tumor-killing capacity of cytotoxic CD8+ T cells and γδT cells within the TME [37]. This mechanistic insight provides a strong rationale for developing sophisticated cellular therapies specifically engineered to recognize and eliminate SOX9-expressing tumors while overcoming their immunosuppressive strategies.
SOX9 Biology and Role in Therapy Resistance
Molecular Characterization of SOX9
SOX9 is a member of the SOX family of transcription factors, characterized by a highly conserved high-mobility group (HMG) DNA-binding domain [38] [36]. The protein contains several functional domains organized from N- to C-terminus: a dimerization domain (DIM), the HMG box domain, a central transcriptional activation domain (TAM), a C-terminal transcriptional activation domain (TAC), and a proline/glutamine/alanine (PQA)-rich domain [4]. The HMG domain facilitates DNA binding and nuclear localization, while the transcriptional activation domains interact with various cofactors to regulate gene expression programs driving tumor progression and immune evasion [4].
SOX9-Mediated Resistance to Immunotherapy
Recent research has elucidated specific mechanisms through which SOX9 contributes to resistance against immune checkpoint blockade. In HNSCC mouse models, SOX9+ tumor cells were significantly enriched in samples resistant to anti-LAG-3 plus anti-PD-1 combination therapy [37]. The molecular pathway involves:
- Direct transcriptional regulation of ANXA1 by SOX9
- ANXA1-FPR1 axis activation leading to neutrophil apoptosis
- Mitochondrial fission promotion and mitophagy inhibition via BNP3 downregulation
- Reduced neutrophil accumulation in tumor tissues
- Impaired infiltration and function of cytotoxic CD8+ T cells and γδT cells [37]
Table 1: SOX9 Expression Correlations with Immune Parameters in Human Cancers
| Cancer Type | Correlation with Immune Features | Prognostic Significance |
|---|---|---|
| Colorectal Cancer | Negative correlation with B cells, resting mast cells, resting T cells, monocytes; Positive correlation with neutrophils, macrophages, activated mast cells [4] | Associated with poor prognosis [4] |
| Glioblastoma | Correlation with immune cell infiltration and checkpoint expression [20] | Prognostic indicator, particularly in IDH-mutant cases [20] |
| Various Solid Tumors | Negative correlation with CD8+ T cells, NK cells, M1 macrophages; Positive correlation with memory CD4+ T cells [4] | Promotes tumor occurrence and development [36] |
Logic-Gated CAR-T Designs for Precision Targeting of SOX9+ Tumors
SynNotch Receptors for Combinatorial Antigen Recognition
Synthetic Notch (SynNotch) receptors represent a breakthrough technology enabling precision targeting of tumor cells based on combinatorial antigen recognition [39]. These engineered receptors can be programmed to recognize SOX9-associated surface markers and subsequently activate therapeutic transgenes in a spatially and temporally controlled manner.
The fundamental architecture of a SynNotch receptor includes:
- Extracellular domain: SOX9-associated tumor antigen-binding scFv
- Core Notch regulatory domain: Synthetic mechanical regulation module
- Intracellular domain: Custom transcriptional activator
- Response element: Regulated therapeutic transgene (e.g., CAR, cytokine) [39]
In practice, a SOX9-targeting SynNotch receptor can be designed to drive expression of a second-stage CAR upon recognition of a tumor-specific surface antigen. This two-step activation system ensures that full T-cell effector function is only unleashed upon encountering tumor cells expressing both antigens, significantly reducing the risk of on-target, off-tumor toxicity [39].
Co-LOCKR System for Sophisticated Logic Gating
The Colocalization-Dependent Latching Orthogonal Cage-Key pRoteins (Co-LOCKR) system provides an advanced platform for cell-extrinsic logic gating capable of OR, AND, and NOT operations [39]. This fully synthetic protein switch system consists of:
- Cage protein: Structural protein with a "Latch" domain that holds a functional peptide inactive
- Key protein: Separate protein that binds Cage, inducing conformational change
- Universal CAR: Engineered to recognize the exposed functional peptide [39]
For SOX9+ tumors, Co-LOCKR components can be designed with binders specific to SOX9-associated surface antigens (e.g., EpCAM, EGFR, Her2). T-cell activation only occurs when Cage and Key proteins are colocalized on the target cell surface, providing exceptional specificity. The system can be further refined with "Decoy Keys" to implement NOT logic, preventing activation against cells expressing specific healthy tissue markers [39].
Diagram 1: SynNotch-mediated AND-gated recognition of SOX9+ tumor cells. Short title: Logic-gated CAR-T cell activation.
Experimental Models and Validation Protocols
In Vivo Modeling of SOX9-Mediated Resistance
The HNSCC mouse model provides a validated platform for studying SOX9-mediated resistance to combination immunotherapy and evaluating novel logic-gated CAR-T approaches [37].
Protocol 1: Establishment of Therapy-Resistant HNSCC Model
- Animal Model: C57BL/6 wild-type mice
- Tumor Induction: 4-nitroquinoline 1-oxide (4NQO) in drinking water for 16 weeks, followed by normal water for 8 weeks
- Treatment Groups:
- Control IgG
- Anti-PD-1 monotherapy
- Anti-LAG-3 monotherapy
- Anti-LAG-3 + anti-PD-1 combination therapy
- Resistance Criteria: Tumors growing >20% larger than original size 14 days post-treatment (per RECIST guidelines)
- Validation: scRNA-seq analysis of resistant vs. sensitive tumors [37]
Protocol 2: scRNA-seq Analysis of SOX9+ Tumor Microenvironment
- Tissue Processing: Pool tumor tissues from 3 mice per group, digest into single-cell suspensions
- Library Construction: 10X Genomics platform with quality control thresholds
- Cell Type Identification: Canonical markers:
- Epithelial cells: Krt14, Krt5, Krt6a
- Immune cells: Ptprc, Cd74, Cd3g
- Fibroblasts: Col1a1, Col3a1, Apod
- Endothelial cells: Flt1, Pecam1, Eng
- Malignant Cell Identification: CopyKAT algorithm for aneuploid tumor cell subpopulations
- Differential Analysis: SOX9+ subcluster identification and trajectory analysis [37]
Table 2: Key Research Reagent Solutions for SOX9-CAR-T Development
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Animal Models | 4NQO-induced HNSCC mouse model [37] | Study SOX9-mediated therapy resistance in immunocompetent context |
| Cell Lines | Murine and human SOX9+ tumor lines [37] | In vitro and in vivo assessment of CAR-T efficacy |
| Detection Antibodies | Anti-Ki67, anti-cleaved Caspase3 [37] | Evaluate tumor proliferation and apoptosis in response to therapy |
| Synthetic Receptors | SynNotch constructs, Co-LOCKR system [39] | Implement logic-gated recognition of SOX9+ tumors |
| Checkpoint Inhibitors | Anti-PD-1, anti-LAG-3 antibodies [37] | Combination therapy with CAR-T to overcome resistance |
| Gene Editing Tools | CRISPR/Cas9 for JAK1, JAK2, B2M knockout [40] | Model and overcome specific resistance mechanisms |
Combination Strategies with PD-1/PD-L1 Blockade
Overcoming SOX9-Mediated Immunosuppression
The resistance mechanisms driven by SOX9 create an immunosuppressive TME characterized by impaired neutrophil function and reduced cytotoxic T-cell infiltration [37]. Combination approaches with PD-1/PD-L1 blockade must address these specific pathways.
Protocol 3: CAR-T Engineering with Intrinsic PD-1 Blockade
- CAR Construct Design:
- Second-generation CAR with CD28 or 4-1BB costimulatory domains
- Mesothelin or other SOX9-associated antigen targeting
- PD-1 Disruption:
- PD-1 shRNA knockdown
- PD-1 dominant negative receptor expression
- Secreted PD-1-blocking scFv
- In Vivo Validation:
- Orthotopic mesothelioma or HNSCC models
- Low-dose T-cell challenge to simulate clinical constraints
- Assessment of T-cell persistence and exhaustion markers [41]
Protocol 4: Targeting Alternative Resistance Pathways
- JAK1/2 Knockout Resistance:
- Overcome with intratumoral Toll-like receptor 9 agonist
- Activates innate and adaptive immunity via NK and CD8 T cells [40]
- B2M Knockout Resistance:
- Overcome with NK-cell and CD4 T-cell activation
- Utilize CD122-preferential IL2 agonist bempegaldesleukin [40]
Diagram 2: SOX9-mediated resistance pathway to immunotherapy. Short title: SOX9-ANXA1-FPR1 resistance axis.
Validation and Safety Assessment Protocols
Comprehensive Functional Assays
Protocol 5: Evaluation of CAR-T Functionality in SOX9+ Models
- In Vitro Cytotoxicity:
- Co-culture with SOX9+ vs. SOX9- tumor cells
- Real-time cell impedance monitoring (xCELLigence)
- Flow cytometry-based killing assay (Annexin V/PI staining)
- Cytokine Profiling:
- Multiplex ELISA for IFN-γ, TNF-α, IL-2, IL-6, IL-10
- Assessment of cytokine release syndrome (CRS) potential
- Exhaustion Marker Analysis:
- PD-1, TIM-3, LAG-3 expression by flow cytometry
- Functional assays after repeated antigen exposure
Protocol 6: Safety and Specificity Profiling
- On-Target, Off-Tumor Toxicity:
- Organoid screening against multiple normal tissues
- Humanized mouse models with functional immune systems
- Bystander Effect Assessment:
- Co-culture with antigen-negative cells
- Measurement of inflammatory cytokine secretion
- Therapeutic Window Determination:
- Dose-response curves for efficacy vs. toxicity
- Minimum effective dose vs. maximum tolerated dose
The development of logic-gated CAR-T designs targeting SOX9+ tumors represents a promising frontier in precision immuno-oncology. By integrating synthetic biology approaches with detailed understanding of SOX9-mediated resistance mechanisms, researchers can create increasingly sophisticated therapeutic platforms capable of overcoming the immunosuppressive strategies employed by treatment-resistant tumors. The combination of these advanced cellular therapies with PD-1/PD-L1 blockade and other immunomodulatory strategies offers a multifaceted approach to reverse SOX9-driven immunosuppression and achieve durable anti-tumor responses.
Future directions should focus on optimizing the timing and sequencing of combination therapies, developing more sophisticated multi-input logic gates that can respond to additional tumor microenvironmental cues, and addressing the challenges of T-cell exhaustion through innovative engineering approaches. As our understanding of SOX9 biology in different tumor contexts continues to evolve, so too will our ability to design increasingly precise and effective therapeutic interventions.
Multi-omics Profiling for Patient Stratification and Biomarker Discovery
Multi-omics profiling represents a transformative approach in precision oncology, integrating diverse molecular datasets to uncover comprehensive biological insights for patient stratification and biomarker discovery. This integrated methodology is particularly crucial for investigating complex therapeutic strategies, such as SOX9 targeting in combination with PD-1/PD-L1 blockade. The transcription factor SOX9 has emerged as a key regulator of tumor progression and therapy resistance, with recent studies demonstrating its epigenetic upregulation following chemotherapy in ovarian cancer and its association with stem-like cancer cell reprogramming [42]. Simultaneously, immune checkpoint blockade targeting the PD-1/PD-L1 axis has revolutionized cancer treatment, though response rates remain limited by various resistance mechanisms [43] [44].
The integration of multi-omics approaches enables researchers to dissect the complex interactions between SOX9-driven oncogenic programs and tumor-immune interactions. SOX9 expression has been significantly correlated with immune cell infiltration patterns and immune checkpoint expression in glioblastoma, suggesting its potential role in modulating the immunosuppressive tumor microenvironment [20]. Furthermore, multi-omics analyses have revealed that SOX9 expression exhibits mutual exclusivity with various tumor immune checkpoints in lung adenocarcinoma, indicating possible compensatory pathways that may be exploited therapeutically [20]. These findings underscore the necessity of comprehensive molecular profiling to identify patients most likely to benefit from SOX9-targeted combinations with PD-1/PD-L1 blockade.
Key Quantitative Findings in Multi-omics Profiling
The application of multi-omics technologies has yielded significant quantitative insights into cancer biology and therapeutic response prediction. The following table summarizes key quantitative findings from recent multi-omics studies relevant to patient stratification and SOX9 research:
Table 1: Key Quantitative Findings from Multi-omics Studies
| Cancer Type | Multi-omics Approach | Key Finding | Clinical Relevance |
|---|---|---|---|
| Head and Neck Squamous Cell Carcinoma (HNSCC) | Integrated CyTOF + Olink proteomics | Predictive model combining CD8+ T cell subsets (c03, c17) and plasma biomarkers (IL-5, MMP7) achieved AUC = 0.9219 for neoadjuvant PD-1 blockade response [45] | Enables non-invasive response prediction for immunotherapy |
| Glioblastoma (GBM) | RNA-seq + Immune cell infiltration analysis | High SOX9 expression associated with better prognosis in lymphoid invasion subgroups (P < 0.05) in 478 cases [20] | SOX9 as diagnostic/prognostic biomarker, especially in IDH-mutant cases |
| Ovarian Cancer | Epigenomic + Transcriptomic profiling | SOX9 epigenetically upregulated after chemotherapy; drives reprogramming to stem-like cancer cells [42] | SOX9 as potential biomarker and target for overcoming chemoresistance |
| Multiple Cancers | Exosomal PD-L1 profiling | <30% of patients achieve durable clinical benefit from PD-1/PD-L1 blockade [44] | Highlights need for better biomarkers like exosomal PD-L1 |
Additional multi-omics studies have revealed that SOX9 expression correlates significantly with immune checkpoint expression patterns in glioblastoma, suggesting its involvement in regulating the immunosuppressive tumor microenvironment [20]. Furthermore, the integration of peripheral blood immune profiling with plasma proteomics has identified distinct cellular populations, including CD103-CD8+ central memory T cells and CD28-TIGIThighcPARP-CD8+ terminally differentiated effector memory cells, that differ significantly between responders and non-responders to PD-1 blockade [45]. These findings demonstrate the power of multi-omics approaches to uncover novel biomarkers and therapeutic targets for combination immunotherapy strategies.
Experimental Protocols for Multi-omics Profiling
Integrated Peripheral Blood Multi-omics Profiling for PD-1 Blockade Response Prediction
This protocol outlines a comprehensive approach for predicting response to PD-1 blockade in head and neck squamous cell carcinoma (HNSCC) patients through integrated analysis of peripheral blood immune cells and plasma proteomics [45].
Table 2: Research Reagent Solutions for Peripheral Blood Multi-omics Profiling
| Research Reagent | Specifications | Primary Function |
|---|---|---|
| Mass Cytometry Panel (CyTOF) | Metal isotope-labeled antibodies (>40 parameters) | High-dimensional immunophenotyping at single-cell resolution |
| Olink Targeted Proteomics Panel | 92-plex immuno-oncology panel | Ultrasensitive quantification of circulating proteins |
| Peripheral Blood Collection Tubes | EDTA-containing tubes | Preservation of blood sample integrity |
| RBC Lysis Buffer | 10X concentration (Biolegend) | Isolation of peripheral blood mononuclear cells (PBMCs) |
| Cryopreservation Medium | FBS + 10% DMSO | Long-term storage of PBMCs in liquid nitrogen |
Procedure:
- Patient Selection and Sample Collection: Enroll patients according to inclusion criteria (primary HNSCC, Stage III-IV, treatment-naïve). Collect peripheral blood samples (recommended: 4 mL venous blood) in EDTA-containing tubes pre- and post-neoadjuvant therapy.
- PBMC Isolation: Centrifuge blood samples at 1700 rpm for 30 minutes at room temperature to separate plasma. For PBMC isolation, dilute 10X RBC lysis buffer to 1X working solution and mix with blood sample at 1:10 ratio. Incubate with gentle rotation for 10-15 minutes in dark. Wash PBMCs twice with PBS containing 1% BSA.
- Sample Preservation: Resuspend PBMCs in FBS with 10% DMSO for cryopreservation in liquid nitrogen. Store plasma samples at -80°C for subsequent proteomic analysis.
- Mass Cytometry Analysis: Thaw PBMCs and stain with metal isotope-labeled antibody panel. Acquire data on CyTOF instrument, analyzing at least 1×106 cells per sample.
- Plasma Proteomic Profiling: Thaw plasma samples and analyze using Olink proximity extension assay technology according to manufacturer's instructions.
- Data Integration and Model Building: Integrate cellular and proteomic features using logistic regression to build predictive model for therapy response.
SOX9 Functional Characterization in Therapy Resistance
This protocol describes methods for investigating SOX9's role in driving chemotherapy resistance, as demonstrated in ovarian cancer research [42].
Table 3: Research Reagent Solutions for SOX9 Functional Characterization
| Research Reagent | Specifications | Primary Function |
|---|---|---|
| CRISPR/Cas9 System | SOX9-targeting guides | Precise genetic manipulation of SOX9 expression |
| Single-cell RNA Sequencing Platform | 10X Genomics or similar | Transcriptomic profiling at single-cell resolution |
| Multi-omics Databases | TCGA, GTEx, HPA | Access to SOX9 expression across cancer types |
| Western Blotting reagents | SOX9 antibodies, ECL detection | Protein-level validation of SOX9 expression |
| Tumor Microarray | Patient-derived tissue cores | High-throughput analysis of SOX9 protein expression |
Procedure:
- SOX9 Expression Analysis: Utilize public databases (TCGA, GTEx, HPA) to analyze SOX9 expression patterns across cancer types. Validate findings at protein level using western blotting of tumor tissues versus normal adjacent tissues.
- Epigenetic Modulation Experiments: Treat ovarian cancer cell lines with chemotherapy agents (e.g., cisplatin) at clinically relevant concentrations. Perform chromatin immunoprecipitation sequencing (ChIP-seq) to identify epigenetic changes at SOX9 locus.
- CRISPR/Cas9-Mediated SOX9 Manipulation: Design and transfert SOX9-targeting guide RNAs using CRISPR/Cas9 system. Establish stable cell lines with SOX9 knockout or overexpression.
- Functional Characterization: Assess chemotherapy sensitivity via viability assays (MTT, CellTiter-Glo) in SOX9-modified cells versus controls. Evaluate stem-like properties through tumorsphere formation assays.
- Single-cell RNA Sequencing: Perform single-cell RNA sequencing on primary patient tumors to identify rare cell populations with high SOX9 expression and stem-like features.
- Pathway Analysis: Conduct transcriptomic analysis of SOX9-modified cells to identify downstream targets and affected pathways, particularly those related to immune regulation and PD-L1 expression.
Workflow Visualization
Diagram 1: Comprehensive Multi-omics Workflow for Patient Stratification
Diagram 2: SOX9-Driven Therapy Resistance Mechanism
Discussion and Future Perspectives
The integration of multi-omics profiling represents a paradigm shift in biomarker discovery and patient stratification for cancer therapy. The protocols outlined herein provide robust methodologies for investigating complex biological relationships, particularly the interplay between SOX9 expression and PD-1/PD-L1 blockade response. Current evidence suggests that SOX9 operates as a master regulator of therapy resistance through its ability to promote stem-like cell states and potentially modulate the tumor immune microenvironment [20] [42]. The convergence of multi-omics technologies with advanced computational approaches, including artificial intelligence and machine learning, will further enhance our ability to identify predictive biomarkers and optimize combination therapy strategies [46] [47].
Future applications of multi-omics profiling should focus on longitudinal sample analysis to capture dynamic changes in SOX9 expression and immune checkpoint regulation during therapy. Additionally, the incorporation of spatial multi-omics technologies will provide critical insights into the geographical relationships between SOX9-expressing cells and immune cell populations within the tumor microenvironment [48]. The continued refinement of these integrated approaches will accelerate the development of personalized therapeutic strategies combining SOX9 inhibition with PD-1/PD-L1 blockade, ultimately improving outcomes for cancer patients.
Overcoming Resistance and Optimizing SOX9-Targeted Combination Therapies
Mechanisms of Resistance to SOX9/PD-1 Combination Therapy
The integration of SOX9-targeting strategies with PD-1/PD-L1 blockade represents a promising frontier in cancer immunotherapy research. Despite the significant efficacy demonstrated by immune checkpoint inhibitors (ICIs) targeting the PD-1/PD-L1 axis across various malignancies, therapeutic resistance remains a substantial clinical challenge, with only 20-30% of patients achieving durable responses [49]. Recent investigations have identified the transcription factor SOX9 (SRY-related HMG-box 9) as a pivotal regulator of tumor immune evasion and resistance mechanisms, particularly in the context of combination immunotherapy approaches [16] [4]. This application note synthesizes current mechanistic insights and provides detailed protocols for investigating SOX9-mediated resistance to PD-1 combination therapies, framed within the broader context of advancing SOX9-targeting strategies in immuno-oncology.
Key Mechanisms of SOX9-Mediated Resistance
Sox9/Anxa1/Fpr1 Neutrophil Axis in HNSCC Resistance
Recent landmark research utilizing a head and neck squamous cell carcinoma (HNSCC) mouse model has elucidated a novel SOX9-driven resistance mechanism to anti-LAG-3 plus anti-PD-1 combination therapy [16]. This work demonstrates that SOX9+ tumor cells are significantly enriched in treatment-resistant samples and mediate immunosuppression through a multi-step pathway.
Table 1: Key Components of the SOX9/Anxa1/Fpr1 Resistance Axis
| Component | Full Name | Function in Resistance |
|---|---|---|
| SOX9 | SRY (sex determining region Y)-box 9 | Transcription factor that directly regulates ANXA1 expression |
| ANXA1 | Annexin A1 | Apoptosis mediator of Fpr1+ neutrophils |
| FPR1 | Formyl peptide receptor 1 | Neutrophil receptor that binds ANXA1 |
| BNIP3 | BCL2/adenovirus E1B interacting protein 3 | Mitophagy regulator downregulated by the axis |
The mechanistic pathway involves SOX9 directly regulating annexin A1 (Anxa1) expression, which subsequently mediates apoptosis of formyl peptide receptor 1 (Fpr1)+ neutrophils through the Anxa1-Fpr1 axis [16]. This interaction promotes mitochondrial fission and inhibits mitophagy by downregulating BNIP3 expression, ultimately preventing neutrophil accumulation in tumor tissues. The reduction of Fpr1+ neutrophils impairs the infiltration and tumor cell-killing capacity of cytotoxic CD8 T cells and γδT cells within the tumor microenvironment, establishing a resistant phenotype [16].
SOX9 as a Janus-Faced Immune Regulator
SOX9 exhibits context-dependent dual functions in immunology, acting as a "double-edged sword" in cancer immunity [4]. While this transcription factor promotes immune escape in cancer contexts, it also maintains macrophage function and contributes to tissue regeneration and repair. In the tumor microenvironment, SOX9 expression demonstrates complex correlations with immune cell infiltration:
Table 2: SOX9 Correlation with Tumor Immune Cell Infiltration
| Immune Cell Type | Correlation with SOX9 | Functional Consequence |
|---|---|---|
| Neutrophils | Positive [4] | Contributes to immunosuppressive microenvironment |
| Macrophages | Positive [4] | Promotes M2-like polarization |
| Activated Mast Cells | Positive [4] | Enhances immunosuppressive properties |
| CD8+ T cells | Negative [4] | Impairs cytotoxic T-cell function |
| NK Cells | Negative [4] | Reduces natural killer cell activity |
| M1 Macrophages | Negative [4] | Diminishes anti-tumor macrophage response |
| B Cells | Negative [4] | Reduces B cell infiltration |
| Resting T Cells | Negative [4] | Limits T cell presence in TME |
SOX9-Mediated CEACAM1 Regulation in Melanoma
In melanoma, SOX9 indirectly regulates CEACAM1 (carcinoembryonic antigen cell adhesion molecule 1) expression, a transmembrane glycoprotein that protects melanoma cells from T cell-mediated killing [50]. Knockdown of endogenous SOX9 results in CEACAM1 up-regulation, while SOX9 overexpression has the opposite effect. SOX9 controls CEACAM1 expression at the transcriptional level through interaction with Sp1 and ETS1 transcription factors, rather than through direct binding to the CEACAM1 promoter [50]. This regulation has functional consequences, as SOX9 knockdown renders melanoma cells resistant to T cell-mediated killing due to increased CEACAM1 expression.
Experimental Models & Key Findings
HNSCC Mouse Model for Combination Therapy Resistance
The establishment of a resistant HNSCC mouse model has been instrumental in elucidating SOX9-mediated resistance mechanisms [16]. The experimental workflow and key quantitative findings are summarized below:
Table 3: HNSCC Mouse Model Response to Combination Therapy
| Parameter | Control IgG | Anti-PD-1 Monotherapy | Anti-LAG-3 Monotherapy | Anti-LAG-3 + Anti-PD-1 Combination |
|---|---|---|---|---|
| Therapeutic Efficacy | Baseline | Significant improvement vs control [16] | No improvement vs control [16] | Superior to PD-1 monotherapy [16] |
| Response Rate | - | - | - | 57.1% (8/14 animals) [16] |
| Resistance Rate | - | - | - | 42.9% (6/14 animals) [16] |
| Tumor Assessment | Progressive growth | Delayed progression | Similar to control | Resistant: >20% growth from baseline [16] |
Single-Cell RNA Sequencing Findings
Comprehensive single-cell RNA sequencing (scRNA-seq) analysis of resistant versus sensitive tumors revealed critical insights into the cellular ecosystem driving therapy resistance [16]. The analysis of >33,424 single cells across all samples identified five major cell types: epithelial cells, fibroblasts, endothelial cells, immune cells, and muscle cells. Key findings included:
- Epithelial cells were the most predominant cell type across all groups
- The proportion of immune cells was dramatically increased in the sensitive group compared to control or resistant groups
- Malignant epithelial cells were divided into five subclusters (E-comm1, E-resi1, E-comm2, E-sens, and E-resi2) with distinct frequencies between resistant and sensitive groups
- SOX9+ tumor cells were significantly enriched in resistant samples
Detailed Experimental Protocols
Establishing the HNSCC Mouse Model with Combination Therapy
Objective: To generate a reliable preclinical model for investigating SOX9-mediated resistance to anti-LAG-3 plus anti-PD-1 combination therapy.
Materials:
- C57BL/6 wild-type mice (6-8 weeks old)
- 4-nitroquinoline 1-oxide (4NQO) for drinking water (100 μg/mL)
- Anti-PD-1 antibody (e.g., nivolumab analog)
- Anti-LAG-3 antibody (e.g., relatlimab analog)
- Control IgG for control groups
- MRI system for tumor monitoring
Procedure:
- Tumor Induction:
- Administer 4NQO-containing water (100 μg/mL) to mice for 16 weeks
- Replace with normal water for additional 8 weeks
- Monitor for HNSCC formation in tongue tissues
Treatment Groups:
- Randomize mice with similar tumor lesions into 4 groups (n≥5 per group):
- Group 1: Control IgG (200 μg, i.p., twice weekly)
- Group 2: Anti-PD-1 monotherapy (200 μg, i.p., twice weekly)
- Group 3: Anti-LAG-3 monotherapy (200 μg, i.p., twice weekly)
- Group 4: Anti-LAG-3 + anti-PD-1 combination (200 μg each, i.p., twice weekly)
- Randomize mice with similar tumor lesions into 4 groups (n≥5 per group):
Response Assessment:
- Monitor tumor size every 4 days from initial treatment
- Classify response at day 14 post-treatment initiation:
- Resistant tumors: >20% increase in size compared to original
- Sensitive tumors: partial reduction or complete tumor eradication
- Perform MRI imaging at baseline and endpoint for volumetric analysis
Tissue Collection:
- Euthanize mice at endpoint or when tumors reach humane endpoints
- Collect tumor tissues for:
- Histopathological examination (H&E staining)
- Immunohistochemistry (Ki67, cleaved-Caspase3)
- Single-cell RNA sequencing preparation
Single-Cell RNA Sequencing for Resistance Profiling
Objective: To characterize the tumor microenvironment and identify SOX9-enriched subpopulations in resistant versus sensitive tumors.
Materials:
- Tumor tissues from resistant and sensitive groups
- Single-cell suspension kit for tissue dissociation
- 10X Genomics Chromium Controller and single-cell reagent kits
- Bioanalyzer or TapeStation for quality control
- scRNA-seq library preparation reagents
- CopyKAT algorithm for aneuploid tumor cell identification
Procedure:
- Single-Cell Suspension Preparation:
- Pool tumor tissues from three mice per group (control, resistant, sensitive)
- Digest tissues into single-cell suspensions using appropriate enzymatic cocktail
- Filter through 70μm cell strainer
- Assess viability (>80% required) and concentration using hemocytometer
Library Preparation and Sequencing:
- Load cells onto 10X Genomics Chromium Chip to target 5,000 cells per sample
- Generate barcoded single-cell libraries following manufacturer's protocol
- Perform quality control using Bioanalyzer High Sensitivity DNA kit
- Sequence libraries on Illumina platform (recommended depth: ≥50,000 reads/cell)
Computational Analysis:
- Process raw sequencing data using Cell Ranger pipeline
- Perform quality control filtering: remove cells with <200 genes or >10% mitochondrial reads
- Normalize data using SCTransform method
- Cluster cells using Seurat workflow (resolution: 0.4-0.8)
- Identify cell types using canonical markers:
- Epithelial cells: Krt14, Krt5, Krt6a
- Fibroblasts: Col1a1, Col3a1, Apod
- Endothelial cells: Flt1, Pecam1, Eng
- Immune cells: Ptprc, Cd74, Cd3g
- Apply CopyKAT to distinguish malignant (aneuploid) from non-malignant epithelial cells
- Identify differentially expressed genes between resistant and sensitive clusters
- Perform trajectory analysis to characterize SOX9+ tumor cell evolution
Validating the SOX9/Anxa1/Fpr1 Functional Axis
Objective: To functionally validate the SOX9/Anxa1/Fpr1 neutrophil axis in mediating combination therapy resistance.
Materials:
- Sox9-floxed transgenic mice for conditional knockout studies
- Anxa1 inhibitors (e.g., Ac2-26 peptide)
- Fpr1-deficient mice or Fpr1 antagonists
- Neutrophil isolation kits
- Flow cytometry antibodies: CD45, CD11b, Ly6G, Fpr1, Annexin V
- Mitophagy dyes: MitoTracker, LysoTracker
- BNIP3 antibodies for Western blot
Procedure:
- Genetic Validation Models:
- Generate epithelial-specific Sox9 knockout mice (Sox9fl/fl;K14-Cre) in HNSCC background
- Treat with combination therapy and compare response to wild-type controls
- Use Fpr1-deficient mice to validate neutrophil requirement in resistance
Neutrophil Functional Assays:
- Isolate neutrophils from tumor tissues using CD11b+Ly6G+ sorting
- Assess apoptosis via Annexin V/7-AAD staining by flow cytometry
- Measure mitochondrial fission using MitoTracker staining and confocal microscopy
- Evaluate mitophagy using MitoTracker/LysoTracker co-localization assays
- Quantify BNIP3 expression via Western blot in isolated neutrophils
Therapeutic Intervention Studies:
- Administer Anxa1 inhibitors (e.g., Ac2-26, 1 mg/kg, i.p., daily) during combination therapy
- Treat with Fpr1 antagonists in combination with immunotherapy
- Assess restoration of CD8+ and γδT cell infiltration via flow cytometry
- Monitor tumor growth and survival outcomes
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Investigating SOX9/PD-1 Resistance Mechanisms
| Reagent/Category | Specific Examples | Function/Application | Key Experimental Use |
|---|---|---|---|
| In Vivo Models | 4NQO-induced HNSCC model; Sox9-floxed transgenic mice; Fpr1-deficient mice | Establish resistant phenotypes; genetic validation | Therapy response studies; mechanistic validation [16] |
| Therapeutic Antibodies | Anti-PD-1 (nivolumab analog); Anti-LAG-3 (relatlimab analog) | Immune checkpoint blockade | Combination therapy treatment groups [16] |
| Single-Cell Technologies | 10X Genomics Chromium; scRNA-seq reagents | Tumor microenvironment deconstruction | Identification of SOX9+ resistant subclusters [16] |
| Flow Cytometry Panel | CD45, CD11b, Ly6G (neutrophils); CD3, CD8 (T cells); Annexin V | Immune phenotyping; apoptosis assessment | Quantifying neutrophil reduction; T cell impairment [16] |
| Molecular Probes | MitoTracker Red CMXRos; LysoTracker Green; TUNEL assay | Mitochondrial function; apoptosis detection | Assessing mitochondrial fission; neutrophil apoptosis [16] |
| SOX9 Modulation | Sox9 siRNA; Sox9 overexpression constructs; Sox9 inhibitors | Manipulate SOX9 expression and function | Validate SOX9 role in resistance mechanisms [50] |
The investigation of SOX9-mediated resistance mechanisms to PD-1 combination therapies represents a critical area of research with significant translational implications. The recently identified SOX9/Anxa1/Fpr1 neutrophil axis provides a novel mechanistic understanding of how tumor cells evade combination immunotherapy in HNSCC [16]. This work, framed within the broader context of SOX9's janus-faced role in immunity [4], highlights the complex interplay between tumor-intrinsic transcriptional programs and immune cell function in the tumor microenvironment.
Future research directions should focus on:
- Therapeutic targeting of the SOX9/Anxa1/Fpr1 axis to overcome established resistance
- Validation across additional cancer types to determine generalizability of these mechanisms
- Development of predictive biomarkers based on SOX9 expression and neutrophil infiltration
- Integration with other resistance mechanisms including TAMs, MDSCs, and additional immune checkpoints [51] [49]
The protocols and reagents detailed in this application note provide a foundation for advancing these research directions, with the ultimate goal of developing effective strategies to overcome resistance and expand the benefit of cancer immunotherapy to more patients.
Sequencing and Dosing Strategies for Maximum Synergy
The success of immune checkpoint blockade (ICB), particularly targeting the PD-1/PD-L1 axis, has revolutionized oncology practice. However, innate and acquired resistance mechanisms limit its efficacy across a broad patient population. Recent research has illuminated the transcription factor SOX9 (SRY-related HMG-box 9) as a critical regulator of the tumor immune microenvironment (TIME) and a promising target for combination strategies. SOX9 exhibits a "Janus-faced" or dual role in immunobiology; it can promote tumor immune escape by impairing immune cell function, yet in other contexts, it contributes to tissue repair and regeneration [4]. This application note delineates evidence-based sequencing and dosing strategies to maximize synergistic antitumor effects when combining SOX9-targeting approaches with PD-1/PD-L1 blockade, framing these protocols within the broader thesis of overcoming ICB resistance.
A pivotal 2025 study published in Nature Communications provides a mechanistic foundation for this combination strategy. The research identified that resistance to anti-PD-1 and anti-LAG-3 combination therapy in head and neck squamous cell carcinoma (HNSCC) is mediated by Sox9+ tumor cells. These cells upregulate annexin A1 (Anxa1), which interacts with Fpr1+ neutrophils. This Anxa1-Fpr1 axis promotes mitochondrial fission, inhibits mitophagy, and prevents neutrophil accumulation, ultimately impairing the infiltration and cytotoxic activity of CD8+ T and γδT cells within the tumor [16]. This pathway positions SOX9 as a master regulator of a key resistance mechanism and a compelling node for therapeutic intervention alongside PD-1 pathway blockade.
Key Mechanistic Insights and Rationale for Combination
The rationale for combining SOX9 modulation with PD-1/PD-L1 inhibitors is rooted in their non-redundant, complementary mechanisms for restoring antitumor immunity. The table below summarizes the core mechanistic relationships and supporting evidence.
Table 1: Core Mechanisms Linking SOX9 to Immunotherapy Resistance
| Mechanistic Pathway | Biological Consequence | Experimental Evidence |
|---|---|---|
| SOX9/Anxa1-Fpr1 Axis | SOX9 directly regulates Anxa1, which induces apoptosis of Fpr1+ neutrophils via mitochondrial dysfunction, reducing cytotoxic T cell infiltration [16]. | scRNA-seq in HNSCC mouse models; various transgenic mouse models. |
| Correlation with Immune Cell Infiltration | SOX9 overexpression negatively correlates with genes associated with CD8+ T cell and NK cell function, and M1 macrophages, shaping an immunosuppressive TME [4]. | Bioinformatics analysis of TCGA data; spatial transcriptomics. |
| Dual Role in Immunity | Acts as a "double-edged sword": promotes immune escape in cancer but helps maintain macrophage function in tissue repair [4]. | Literature review of SOX9 in tumor and inflammatory disease contexts. |
| Association with Immune Checkpoints | SOX9 expression is correlated with the expression of various immune checkpoint molecules in glioblastoma, indicating involvement in immunosuppression [11]. | Analysis of RNA-seq data from TCGA and GTEx databases. |
Experimental Protocols for Evaluating Combination Efficacy
In Vivo Modeling of Combination Therapy
This protocol is adapted from the methodology used to investigate SOX9-mediated resistance in HNSCC [16].
Objective: To evaluate the synergistic antitumor activity of SOX9 inhibition combined with anti-PD-1 therapy in a murine model.
Materials:
- Animals: C57BL/6 wild-type mice.
- Tumor Induction: 4-nitroquinoline 1-oxide (4NQO) in drinking water for 16 weeks to induce HNSCC.
- Therapeutic Agents:
- Anti-mouse PD-1 blocking antibody (e.g., clone RMP1-14).
- SOX9 inhibitor (e.g., small molecule or genetic tool) or control vehicle.
- Isotype control IgG.
- Key Equipment: MRI system for tumor monitoring, equipment for scRNA-seq library preparation and sequencing.
Procedure:
- Tumor Induction and Grouping: Induce HNSCC by administering 50 µg/mL 4NQO in the drinking water of 8-week-old mice for 16 weeks, followed by normal water for 8 weeks. Once tumors are established, randomize mice with similar tumor lesion sizes into four groups (n ≥ 5 per group):
- Group 1: Control IgG + vehicle control.
- Group 2: Anti-PD-1 antibody + vehicle control.
- Group 3: Control IgG + SOX9 inhibitor.
- Group 4: Anti-PD-1 antibody + SOX9 inhibitor.
- Dosing and Sequencing:
- Administration: Administer all therapeutic agents via intraperitoneal injection.
- Dosing Frequency: Treat every 3-4 days for the duration of the study.
- Sequencing Strategy: Initiate SOX9 inhibitor therapy one week prior to the first anti-PD-1 dose. This priming sequence is hypothesized to precondition the TIME by reversing the SOX9-driven suppression of neutrophil and T cell infiltration, thereby creating a more favorable environment for subsequent ICB.
- Monitoring and Analysis:
- Monitor tumor size every 4 days using caliper measurements and confirm with MRI at key time points (e.g., pre-treatment, day 14).
- Classify response 14 days after initial treatment based on RECIST criteria: tumors growing >20% from original size are considered resistant.
- At endpoint, harvest tumor tissues for:
- Histopathology: H&E staining, Ki67 (proliferation), and cleaved-Caspase3 (apoptosis) immunohistochemistry.
- Single-cell RNA Sequencing: Pool and digest tumors from each group into single-cell suspensions. Perform scRNA-seq (e.g., 10x Genomics platform) to characterize immune cell populations and SOX9/Anxa1 pathway activity [16].
Computational Prediction of Synergistic Drug Combinations
Given the vast combinatorial space, computational pre-screening is essential. The following protocol leverages recent advances in machine learning for synergy prediction.
Objective: To identify candidate drugs that target SOX9-related pathways and may synergize with PD-1/PD-L1 inhibitors.
Materials:
- Databases: DrugComb [52], OncoDrug+ [53], LINCS (for drug-induced transcriptomic signatures), GDSC (for drug response data).
- Software/Tools: MD-Syn [54] or similar frameworks (e.g., SynergyX) that integrate multi-dimensional features.
Procedure:
- Feature Generation:
- Drug Features: Represent drugs using Drug Resistance Signatures (DRS), which capture transcriptomic changes between drug-sensitive and drug-resistant cell lines. DRS features have been shown to outperform conventional chemical descriptors [52].
- Cell Line Features: Use gene expression profiles from cancer cell lines representative of the tumor type of interest (e.g., HNSCC, glioblastoma).
- Model Application:
- Input known PD-1/PD-L1 pathway inhibitors and a library of candidate SOX9-pathway targeting drugs into the MD-Syn model [54].
- The model will output a predicted synergy score (e.g., a probability or continuous score) for each drug pair and cell line triplet.
- Validation Prioritization:
- Prioritize the top-ranked drug combinations for experimental validation in the in vivo model described in section 3.1. OncoDrug+ can provide additional evidence levels for these combinations, including FDA approval status and associated biomarkers [53].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Investigating SOX9 and PD-1/PD-L1 Combination Therapy
| Reagent / Resource | Function / Application | Example / Specification |
|---|---|---|
| Anti-PD-1 Antibody | Blocks PD-1 immune checkpoint, reinvigorating exhausted T cells. | InVivoMab anti-mouse PD-1 (clone RMP1-14); clinical-grade human anti-PD-1 (e.g., Nivolumab). |
| SOX9 Inhibitor | Pharmacologically targets SOX9 expression or function. | Small molecule inhibitors (e.g., CDMO-1.1); siRNA/shRNA for genetic knockdown. |
| Sox9 Transgenic Mice | Enables cell-specific manipulation of Sox9 expression in vivo. | Sox9-floxed mice for crossing with tissue-specific Cre drivers (e.g., K14-Cre for HNSCC). |
| scRNA-seq Kit | For comprehensive profiling of cellular heterogeneity and pathway activity in the tumor microenvironment. | 10x Genomics Single Cell 3' Reagent Kits. |
| Antibodies for IHC/IF | Visualize and quantify protein expression and cell localization in tumor sections. | Anti-SOX9, Anti-Anxa1, Anti-Fpr1, Anti-CD8, Anti-Cleaved Caspase-3. |
| Computational Tools | Predict synergistic drug combinations and analyze omics data. | MD-Syn [54], OncoDrug+ database [53], SynergyX [52]. |
Visualization of Key Signaling Pathways and Workflows
SOX9-Mediated Resistance to Immunotherapy
The diagram below illustrates the mechanism by which SOX9-expressing tumor cells drive resistance to combination immunotherapy, as revealed by recent research [16].
Diagram 1: SOX9-driven immunotherapy resistance pathway.
Proposed Therapeutic Intervention Strategy
This workflow outlines the proposed sequential dosing strategy to overcome SOX9-mediated resistance and achieve synergistic tumor control.
Diagram 2: Sequential dosing for synergistic tumor control.
The integration of SOX9-targeting strategies with PD-1/PD-L1 blockade represents a rationally designed approach to overcome a defined mechanism of immunotherapy resistance. The presented application notes and protocols provide a roadmap for researchers to experimentally validate this combination, emphasizing a priming sequence where SOX9 inhibition precedes and accompanies ICB. This strategy aims to first normalize the immunosuppressive TIME—particularly by reversing the suppression of neutrophil-mediated T cell recruitment—before unleashing the full power of adaptive immunity with checkpoint blockade.
Future work should focus on identifying biomarkers, such as tumor SOX9 and Anxa1 expression levels, to select patients most likely to benefit. Furthermore, the development of more potent and specific clinical-grade SOX9 inhibitors is paramount for translating this promising combinatorial thesis from the bench to the bedside.
Mitigating On-Target, Off-Tumor Toxicity of SOX9 Inhibition
The transcription factor SOX9 (SRY-related HMG-box 9) has emerged as a promising therapeutic target in oncology, particularly in the context of combination therapies with PD-1/PD-L1 checkpoint blockade. However, its diverse physiological roles present a significant challenge for targeted therapies, as inhibiting SOX9 risks disrupting its critical functions in normal tissue homeostasis. SOX9 plays essential roles in various biological processes, including cartilage formation, tissue regeneration, and the maintenance of macrophage function [4]. This dual nature establishes SOX9 as a "double-edged sword" in therapeutic development—while its inhibition may counteract tumor immune escape, systemic suppression risks impairing vital tissue repair mechanisms and other physiological processes [4].
The integration of SOX9 targeting with PD-1/PD-L1 blockade represents a particularly promising approach in immuno-oncology. Recent evidence indicates that SOX9 contributes to resistance against combination immunotherapies, with significant enrichment of SOX9+ tumor cells observed in head and neck squamous cell carcinoma (HNSCC) models resistant to anti-LAG-3 plus anti-PD-1 treatment [16]. This positions SOX9 as a key mediator of immunotherapy resistance while simultaneously highlighting the potential toxicity concerns associated with its inhibition.
Mechanisms of SOX9-Mediated Toxicity: Identifying the Challenge
Physiological Roles of SOX9 in Normal Tissue Homeostasis
Understanding the potential on-target, off-tumor toxicity of SOX9 inhibition requires a comprehensive analysis of its diverse functions in normal physiology. As outlined in Table 1, SOX9 maintains critical processes across multiple tissue types, with particular importance in central nervous system function, cartilage maintenance, and immune regulation.
Table 1: Physiological Functions of SOX9 and Potential Toxicity of Inhibition
| Tissue/Cell Type | Normal SOX9 Function | Potential Toxicity of Inhibition | Supporting Evidence |
|---|---|---|---|
| Brain Astrocytes | Promotes clearance of amyloid plaques; maintains cognitive function | Impaired neuroprotection; reduced amyloid clearance; accelerated cognitive decline | [18] |
| Cartilage/Chondrocytes | Essential for cartilage formation and development | Disruption of joint integrity; impaired tissue repair | [4] |
| Hepatic & Pancreatic Progenitor Cells | Marker for stem/progenitor cell populations | Compromised tissue regeneration capacity | [4] |
| Macrophages | Maintains macrophage function; supports tissue regeneration | Impaired innate immunity; delayed wound healing | [4] |
| γδ T Cells | Modulates lineage commitment of early thymic progenitors | Potential disruption of specialized T cell populations | [4] |
Recent research has particularly highlighted the critical neuroprotective role of SOX9. In Alzheimer's disease models, boosting SOX9 expression in astrocytes enhanced their ability to clear amyloid plaques and preserve cognitive function, whereas lowering SOX9 led to accelerated plaque buildup and diminished plaque clearing [18]. This demonstrates that SOX9 inhibition could potentially exacerbate neurodegenerative processes, a significant concern for therapeutic development.
SOX9 in Cancer Development and Therapy Resistance
In the tumor microenvironment, SOX9 exhibits complex, context-dependent functions that contribute to its potential as a therapeutic target. In glioblastoma, SOX9 is highly expressed and identified as a diagnostic and prognostic biomarker, particularly in IDH-mutant cases [20]. Its expression correlates significantly with immune cell infiltration and checkpoint expression, indicating involvement in the immunosuppressive tumor microenvironment [20].
The role of SOX9 in mediating resistance to combination immunotherapy has been mechanistically elucidated in HNSCC models, where SOX9+ tumor cells drive resistance to anti-LAG-3 plus anti-PD-1 therapy through interaction with Fpr1+ neutrophils [16]. Specifically, SOX9 directly regulates the expression of annexin A1 (Anxa1), mediating apoptosis of formyl peptide receptor 1 (Fpr1)+ neutrophils through the Anxa1-Fpr1 axis [16]. This pathway promotes mitochondrial fission, inhibits mitophagy by downregulating BCL2/adenovirus E1B interacting protein 3 (Bnip3) expression, and ultimately prevents neutrophil accumulation in tumor tissues [16]. The reduction of Fpr1+ neutrophils impairs the infiltration and tumor cell-killing ability of cytotoxic CD8+ T and γδT cells within the tumor microenvironment, thereby driving therapy resistance [16].
Strategic Approaches for Mitigating Toxicity
Tissue-Restricted Delivery Systems
The development of delivery systems that restrict SOX9 inhibition to tumor sites represents a primary strategy for mitigating off-tumor toxicity. Nanoparticle-based delivery vehicles functionalized with tumor-specific targeting ligands can achieve preferential accumulation in malignant tissue. The experimental protocol for synthesizing and validating such a system involves:
Nanoparticle Formulation: Prepare lipid-polymer hybrid nanoparticles using a microfluidic assembly. The composition should include:
- Cationic lipid (DOTAP: 50 mol%)
- Helper lipid (DOPE: 40 mol%)
- PEGylated lipid (DMG-PEG2000: 10 mol%)
- SOX9 inhibitor (encapsulated in aqueous core)
- Tumor-targeting peptide (e.g., RGD, iRGD) conjugated to terminal PEG groups
Ligand Conjugation: Employ carbodiimide chemistry for covalent attachment of targeting ligands to nanoparticle surfaces. React nanoparticles with EDC (1-ethyl-3-(3-dimethylaminopropyl)carbodiimide) and sulfo-NHS (N-hydroxysulfosuccinimide) in MES buffer (pH 6.0) for 15 minutes, followed by addition of targeting peptide (0.5 mg/mL) and incubation for 4 hours at room temperature.
Characterization and Validation:
- Determine particle size and zeta potential using dynamic light scattering
- Quantify encapsulation efficiency via HPLC analysis of purified nanoparticles
- Assess targeting specificity using flow cytometry with fluorescently-labeled nanoparticles on tumor cell lines versus primary normal cells
- Evaluate in vivo biodistribution in tumor-bearing mouse models using near-infrared imaging
Diagram: Targeted nanoparticle approach for precise SOX9 inhibition
Logic-Gated Cellular Engineering
Synthetic biology approaches offer innovative solutions for achieving tumor-specific SOX9 inhibition while sparing normal tissues. Building upon successful strategies in CAR-T cell development, logic-gated systems can be designed to activate SOX9 inhibition only in the presence of multiple tumor-specific signals.
Table 2: Research Reagent Solutions for Logic-Gated SOX9 Targeting
| Reagent/Category | Specific Example | Function/Application | Experimental Consideration | |
|---|---|---|---|---|
| AND-Gate Split CAR System | Anti-PSCA scFv-CD3ζ + Anti-PSMA scFv-CD28-4-1BB | Requires dual antigen recognition for T-cell activation | Optimize scFv affinity to minimize single antigen leakage | [55] |
| Proximal Signaling AND-Gate | LAT-based receptor + SLP-76-based receptor | Triggers activation only when both receptors engage tumor antigens | Mutate cysteine residues in CD28 TM domain to reduce heterodimerization | [55] |
| SynNotch Receptor System | Custom extracellular domain + synthetic transcription factor | Activates expression of SOX9 inhibitor in response to tumor-specific antigen | Can be layered with microRNA sensors for additional specificity | [55] |
| Tumor Microenvironment Sensors | Hypoxia-responsive elements + extracellular protease sensors | Activates therapeutic gene expression in response to TME signals | Combine multiple TME sensors to enhance specificity | [55] |
The experimental protocol for implementing a dual-antigen AND-gate system for conditional SOX9 inhibition involves:
Vector Construction:
- Design a bicistronic lentiviral vector containing two expression cassettes
- Cassette 1: Primary CAR with scFv targeting tumor antigen A (e.g., PSCA) fused to CD3ζ signaling domain
- Cassette 2: Costimulatory CAR with scFv targeting tumor antigen B (e.g., PSMA) fused to CD28 and 4-1BB signaling domains
- Include a SOX9 inhibitory construct (shRNA or dominant-negative mutant) under the control of a NFAT-responsive promoter (responds only upon dual antigen engagement)
T Cell Engineering:
- Isolate human primary T cells from healthy donor PBMCs using Ficoll density gradient centrifugation
- Activate T cells with CD3/CD28 Dynabeads (3:1 bead-to-cell ratio) in X-VIVO 15 media with 5% human AB serum and 100 IU/mL IL-2
- Transduce activated T cells with lentiviral vectors at MOI 10-20 in Retronectin-coated plates via spinfection (2000 × g, 90 minutes, 32°C)
- Culture transduced T cells for 10-14 days with media changes every 2-3 days
Functional Validation:
- Verify AND-gate functionality using co-culture assays with target cells expressing antigen A only, antigen B only, or both antigens
- Measure SOX9 inhibitor expression specifically in dual-antigen conditions via qRT-PCR and Western blot
- Assess tumor-specific cytotoxicity using real-time cell analysis (xCELLigence) and cytokine release assays
- Evaluate safety profile using organoid models of normal tissues expressing single antigens
Diagram: AND-gate system for conditional SOX9 inhibition
Biomarker-Driven Patient Stratification
The development of comprehensive biomarker panels represents a crucial strategy for identifying patient populations most likely to benefit from SOX9-targeted therapies while minimizing risks. Based on recent findings, the following protocol outlines a biomarker validation approach:
Sample Collection and Processing:
- Collect tumor tissue samples via core needle biopsy prior to treatment initiation
- Process samples for simultaneous DNA, RNA, and protein analysis
- Generate single-cell suspensions for flow cytometry and scRNA-seq analysis
Multi-Omic Biomarker Profiling:
- Perform scRNA-seq using 10X Genomics platform to identify SOX9+ tumor cell subpopulations
- Assess ANXA1 and FPR1 expression levels via qRT-PCR (TaqMan assays) and immunohistochemistry
- Evaluate immune contexture using multiplex immunofluorescence (Panel: CD8, CD4, CD68, SOX9, ANXA1, FPR1)
- Analyze peripheral blood neutrophil function via flow cytometry-based assays of mitochondrial fission and mitophagy
Predictive Model Development:
- Integrate biomarker data using machine learning algorithms (random forest, support vector machines)
- Develop a SOX9 Resistance Score (SRS) incorporating:
- Percentage of SOX9+ tumor cells in biopsy
- ANXA1/FPR1 expression ratio
- Neutrophil functional status
- Baseline CD8+ T cell infiltration density
- Validate SRS in independent patient cohorts using retrospective samples from immunotherapy trials
Combination Therapy Protocols: SOX9 Inhibition with PD-1/PD-L1 Blockade
Preclinical Evaluation Framework
The integration of SOX9 inhibition with PD-1/PD-L1 blockade requires systematic evaluation to maximize efficacy while controlling toxicity. The following protocol provides a comprehensive framework for preclinical assessment:
In Vivo Therapeutic Efficacy Studies:
- Utilize syngeneic mouse models with varying SOX9 expression levels (e.g., 4NQO-induced HNSCC model)
- Randomize mice (n=8-10/group) to receive:
- Group 1: Isotype control antibody (10 mg/kg, i.p., twice weekly)
- Group 2: Anti-PD-1 antibody (10 mg/kg, i.p., twice weekly)
- Group 3: SOX9 inhibitor (dose-optimized, daily oral gavage)
- Group 4: Combination therapy (SOX9 inhibitor + anti-PD-1)
- Monitor tumor growth by caliper measurements thrice weekly
- Assess survival as primary endpoint (humane endpoint: tumor volume ≥1000 mm³)
Immune Monitoring Protocol:
- Harvest tumors at day 21 post-treatment initiation for comprehensive immune profiling
- Process tumors to single-cell suspensions using mechanical dissociation and enzymatic digestion (Collagenase IV 1 mg/mL + DNase I 0.1 mg/mL, 37°C, 30 minutes)
- Perform flow cytometry analysis with the following panel:
- Surface markers: CD45, CD3, CD4, CD8, CD44, NK1.1, PD-1, LAG-3
- Intracellular cytokines: IFN-γ, TNF-α (after 5-hour stimulation with PMA/ionomycin)
- Neutrophil markers: Ly6G, FPR1, Annexin A1
- Analyze T cell functionality by intracellular cytokine staining after overnight stimulation with CD3/CD28 activation beads
Toxicity Assessment:
- Monitor body weight daily as general health indicator
- Perform weekly serum chemistry panels (ALT, AST, creatinine, BUN)
- Conduct histological analysis of critical organs (brain, liver, joints) at study endpoint
- Assess cognitive function in Alzheimer's model mice using novel object recognition test
Clinical Translation Considerations
For translational development, a phase I clinical trial design should incorporate specific safety monitoring for on-target, off-tumor toxicities:
Dose Escalation Protocol:
- Utilize a 3+3 design with accelerated titration for initial dose levels
- Define starting dose as 1/10th the severely toxic dose in 10% of animals (STD10) from GLP toxicology studies
- Schedule dose-limiting toxicity (DLT) observation period of 28 days
- Include intra-patient dose escalation permitted after safety evaluation
Safety Monitoring Plan:
- Implement frequent neurological assessments (Mini-Mental State Examination biweekly)
- Monitor joint function through patient-reported outcomes (WORC index)
- Establish comprehensive immune monitoring panel including:
- T cell exhaustion markers (PD-1, LAG-3, TIM-3)
- Neutrophil function assays (mitochondrial membrane potential, mitophagy)
- Cytokine profiling (multiplex array for 15 cytokines)
- Conduct routine brain MRI at baseline and every 9 weeks to monitor for unexpected neurotoxicity
Biomarker-Guided Patient Selection:
- Include only patients with high SOX9 Resistance Score (SRS > predetermined cutoff)
- Require tumor positivity for both components of the dual-antigen system (if using AND-gate approach)
- Exclude patients with pre-existing neurodegenerative conditions or severe joint pathology
The strategic mitigation of on-target, off-tumor toxicity represents a critical challenge in the therapeutic targeting of SOX9 for cancer treatment, particularly in combination with PD-1/PD-L1 blockade. The approaches outlined herein—including tissue-restricted delivery systems, logic-gated cellular engineering, and comprehensive biomarker-driven patient stratification—provide a framework for developing safer, more effective SOX9-targeted therapies. As research continues to elucidate the complex biology of SOX9 in both physiological and pathological contexts, these strategies will undoubtedly evolve, offering new opportunities to harness the therapeutic potential of SOX9 inhibition while minimizing collateral damage to normal tissues. The integration of these advanced targeting approaches with immunotherapy represents a promising frontier in precision oncology, potentially overcoming key resistance mechanisms while maintaining an acceptable safety profile.
Addressing Tumor Heterogeneity and Adaptive Immune Evasion
The challenge of overcoming tumor heterogeneity and adaptive immune evasion represents a critical frontier in oncology research, particularly in the context of immune checkpoint inhibitor (ICI) therapies. While PD-1/PD-L1 blockade has demonstrated remarkable clinical efficacy across multiple malignancies, therapeutic resistance remains a significant limitation [56] [57]. Emerging evidence identifies the transcription factor SOX9 as a key regulator of both tumor heterogeneity and immune evasion mechanisms, positioning it as a promising therapeutic target for combination strategies [11] [4] [15].
SOX9, a member of the SRY-related HMG-box family, is increasingly recognized for its dual functionality in cancer biology. It serves not only as a driver of tumor progression and stemness but also as a crucial modulator of the tumor immune microenvironment [4] [15]. This application note synthesizes current research findings and provides detailed methodologies for investigating SOX9 as a combinatorial target with PD-1/PD-L1 blockade, with the ultimate goal of overcoming adaptive immune evasion in heterogeneous tumors.
SOX9 as a Mediator of Immune Evasion and Therapeutic Resistance
Mechanisms of SOX9-Driven Immune Suppression
Recent multi-omics analyses have elucidated several mechanisms through which SOX9 fosters an immunosuppressive tumor microenvironment (TME). Table 1 summarizes the key immune evasion pathways associated with SOX9 expression.
Table 1: SOX9-Mediated Immune Evasion Mechanisms
| Mechanism | Experimental Evidence | Functional Consequence |
|---|---|---|
| Altered Immune Cell Infiltration | Negative correlation with CD8+ T cells, NK cells, M1 macrophages; Positive correlation with Tregs, M2 macrophages, neutrophils [11] [4] [21] | Creates "immune desert" or "immune excluded" phenotypes |
| Immune Checkpoint Regulation | Correlation with PD-L1 expression patterns; Modulation of multiple checkpoint pathways [15] | Contributes to T-cell exhaustion and dysfunction |
| Metabolic Reprogramming | Association with lactate production and acidic TME [58] | Direct inhibition of T-cell function and proliferation |
| Stemness Maintenance | Promotion of cancer stem-like cells (CSCs) [4] | Enhances tumor heterogeneity and therapeutic resistance |
Bioinformatic analyses of thymic epithelial tumors revealed that high SOX9 expression correlates with significant alterations in immune signaling pathways. Specifically, SOX9-high tumors demonstrate downregulation of critical anti-tumor immunity pathways including primary immunodeficiency, T-cell receptor signaling, Th17 cell differentiation, and PD-1 checkpoint pathways [21]. Simultaneously, these tumors exhibit upregulation of extracellular matrix-receptor interaction and TGF-β signaling pathways, further contributing to an immunosuppressive TME [21].
SOX9 in Tumor Heterogeneity and Adaptive Resistance
SOX9 contributes to therapeutic resistance through its role in maintaining cancer stemness and cellular plasticity. In triple-negative breast cancer (TNBC), SOX9 is significantly upregulated during early tumor formation and promotes progression by maintaining tumor cells in a stem-like state [17]. This stemness phenotype enables tumors to evade innate immunity by remaining dormant for extended periods and facilitates the development of resistance mechanisms [15].
The transcription factor further enhances tumor heterogeneity through its association with tuft cell phenotypes in thymic epithelial tumors, as evidenced by its positive correlation with POU2F3 and TRPM5 expressions [21]. This cellular diversification within tumors creates multiple subpopulations with varying susceptibility to immune attack, ultimately driving adaptive resistance to mono-therapies such as PD-1/PD-L1 blockade.
Quantitative Analysis of SOX9 in Cancer Immunobiology
Prognostic and Diagnostic Significance
Comprehensive studies across multiple cancer types have established the clinical relevance of SOX9 expression patterns. Table 2 presents key quantitative findings from recent investigations.
Table 2: Quantitative Significance of SOX9 Expression in Human Cancers
| Cancer Type | Expression Pattern | Clinical Correlation | Statistical Significance |
|---|---|---|---|
| Glioblastoma (GBM) | Highly expressed in tumor tissues vs. normal [11] | Better prognosis in lymphoid invasion subgroups (n=478) | P < 0.05 [11] |
| Thymic Epithelial Tumors (TETs) | Nuclear expression in tumor cells and Hassall's corpuscles [21] | Unfavorable clinical outcomes in thymomas | Association with histological type [21] |
| Multiple Solid Tumors | Overexpressed in liver, lung, breast, gastric cancers [4] | Correlation with poor prognosis | Varies by cancer type [4] |
In glioblastoma, SOX9 expression emerges as an independent prognostic factor for IDH-mutant cases in Cox regression analysis [11]. The development of nomogram prognostic models incorporating SOX9, OR4K2, and IDH status demonstrates the clinical utility of SOX9 assessment in patient stratification and outcome prediction [11].
Experimental Protocols for Investigating SOX9 in Immune Evasion
Protocol 1: Comprehensive SOX9 Expression and Immune Correlation Analysis
Objective: To evaluate SOX9 expression patterns and their correlation with immune cell infiltration in tumor tissues.
Materials and Reagents:
- Tissue specimens (formalin-fixed, paraffin-embedded or fresh frozen)
- Anti-SOX9 antibody (polyclonal rabbit, Sigma-Aldrich AB5535)
- Immunohistochemistry staining kit with HRP-conjugated secondary antibody
- RNA extraction kit (TRIzol or equivalent)
- cDNA synthesis kit
- Quantitative PCR reagents and primers
- Bioinformatics tools: R package, DESeq2, ESTIMATE, GSVA
Methodology:
- SOX9 Protein Detection
Gene Expression Analysis
- Extract total RNA from matched tissue samples
- Conduct RNA sequencing or qPCR for SOX9 and immune-related genes
- Process RNA-seq data using TCGA and GTEx databases for normalization [11]
Immune Cell Infiltration Assessment
- Apply ssGSEA and ESTIMATE algorithms to quantify immune cell populations [11]
- Correlate SOX9 expression levels with immune cell signatures
- Analyze expression of immune checkpoint molecules (PD-1, PD-L1, CTLA-4)
Bioinformatic Integration
- Identify differentially expressed genes (DEGs) between SOX9-high and SOX9-low groups using DESeq2 (|logFC| >2, adj. p <0.05) [11]
- Perform functional enrichment analysis (GO, KEGG) using clusterProfiler
- Construct protein-protein interaction networks using STRING database
Expected Outcomes: This comprehensive protocol enables researchers to establish correlations between SOX9 expression, immune cell infiltration patterns, and checkpoint molecule expression, providing insights into SOX9-mediated immune modulation.
Protocol 2: In Vitro Evaluation of SOX9 Targeting with PD-1/PD-L1 Blockade
Objective: To assess the combinatorial effect of SOX9 inhibition and PD-1/PD-L1 blockade on tumor-immune interactions.
Materials and Reagents:
- Human cancer cell lines (appropriate to research focus)
- Primary human T-cells from healthy donors
- SOX9 knockdown reagents (siRNA, shRNA, or CRISPR-Cas9)
- Anti-PD-1/PD-L1 therapeutic antibodies
- Flow cytometry antibodies: CD3, CD8, CD4, PD-1, TIM-3, LAG-3
- Cytokine detection kits: IFN-γ, TNF-α, IL-2
- Co-culture transwell systems
Methodology:
- SOX9 Modulation in Tumor Cells
- Implement SOX9 knockdown using validated siRNA or shRNA constructs
- Confirm knockdown efficiency via qPCR and Western blot
- Establish stable knockout lines using CRISPR-Cas9 when applicable
T-cell Activation and Co-culture
- Isolate CD8+ T-cells from human PBMCs using magnetic separation
- Activate T-cells with anti-CD3/CD28 antibodies
- Establish tumor cell-T-cell co-cultures at optimized ratios (typically 1:1 to 1:5)
Combinatorial Treatment
- Apply anti-PD-1/PD-L1 antibodies at clinically relevant concentrations (1-10μg/mL)
- Include appropriate controls: IgG isotype, SOX9 modulation alone, checkpoint blockade alone
- Maintain co-cultures for 24-96 hours based on assay requirements
Functional Assays
- T-cell Cytotoxicity: Measure specific lysis using real-time cell analysis or LDH release
- T-cell Exhaustion Markers: Analyze PD-1, TIM-3, LAG-3 expression via flow cytometry
- Cytokine Production: Quantify IFN-γ, TNF-α, IL-2 in supernatants using ELISA
- Proliferation Assessment: Monitor CFSE-labeled T-cell division patterns
Expected Outcomes: This protocol enables systematic evaluation of how SOX9 targeting modulates responsiveness to PD-1/PD-L1 blockade, with particular focus on reversing T-cell exhaustion and enhancing anti-tumor immunity.
Signaling Pathways and Molecular Mechanisms
The diagram below illustrates the central role of SOX9 in modulating tumor-immune interactions and its potential for combination with checkpoint blockade.
SOX9 Modulation of Tumor-Immune Interactions and Combinatorial Targeting
This pathway illustration demonstrates how SOX9 influences multiple aspects of tumor biology and immune regulation, contributing to resistance against PD-1/PD-L1 blockade. Combinatorial targeting approaches address both tumor-intrinsic and microenvironmental resistance mechanisms.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for SOX9 and Immune Checkpoint Investigations
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| SOX9 Detection | Rabbit anti-SOX9 (Sigma AB5535) | IHC, Western blot | Optimal for nuclear staining in FFPE tissues [21] |
| SOX9 Modulation | siRNA, shRNA, CRISPR-Cas9 | Functional studies | Validate efficiency via qPCR and Western blot |
| Immune Profiling | CD3, CD8, CD4, CD68, FOXP3 | Flow cytometry, IHC | Panel design depends on research focus |
| Checkpoint Antibodies | Anti-PD-1, anti-PD-L1, anti-CTLA-4 | Functional assays | Use therapeutic-grade for relevant results |
| Cell Culture Models | Primary tumor cells, T-cells, co-culture systems | Mechanistic studies | Maintain physiological relevance |
| Analysis Tools | R packages: DESeq2, ESTIMATE, GSVA | Bioinformatics | Requires RNA-seq data input [11] |
The investigation of SOX9 as a combinatorial target with PD-1/PD-L1 blockade represents a promising strategy for addressing the dual challenges of tumor heterogeneity and adaptive immune evasion. Current evidence indicates that SOX9 modulates multiple aspects of tumor-immune interactions, including immune cell infiltration, checkpoint molecule expression, and T-cell function [11] [4] [15].
Future research directions should focus on:
- Developing selective SOX9 inhibitors suitable for clinical application
- Optimizing sequencing and dosing of SOX9 targeting with existing immunotherapies
- Identifying predictive biomarkers for patient stratification
- Exploring SOX9 vaccination strategies as demonstrated in TNBC models [17]
The experimental protocols outlined herein provide a foundation for systematic investigation of SOX9-mediated immune evasion and the development of effective combinatorial approaches to overcome therapeutic resistance in heterogeneous tumors.
Leveraging Single-Cell and Spatial Transcriptomics to Monitor Therapy Response
The integration of single-cell RNA sequencing (scRNA-seq) and spatial transcriptomics (ST) has revolutionized the monitoring of therapeutic responses in cancer research. These technologies enable the dissection of the tumor microenvironment (TME) at unprecedented resolution, revealing cellular heterogeneity, drug resistance mechanisms, and dynamic changes in cell states during treatment [59]. Within the context of developing combination therapies targeting SOX9 and PD-1/PD-L1 blockade, these tools are indispensable for identifying resistance mechanisms and validating therapeutic efficacy. SOX9, a transcription factor with a dual role in immunology, promotes tumor immune escape but also contributes to tissue repair, making it a compelling yet complex therapeutic target [4]. This application note details protocols for utilizing single-cell and spatial technologies to evaluate therapy response, using SOX9-targeting combined with immune checkpoint blockade as a primary use case.
Key Findings and Rationale for SOX9 Targeting
Recent studies underscore SOX9's significant role in mediating resistance to immunotherapy. A 2025 study on head and neck squamous cell carcinoma (HNSCC) revealed that Sox9+ tumor cells are significantly enriched in tumors resistant to combined anti-LAG-3 and anti-PD-1 therapy. This resistance is mediated through the Sox9-Anxa1-Fpr1 axis, where SOX9 transcriptionally upregulates Annexin A1 (Anxa1), which in turn induces apoptosis in Fpr1+ neutrophils. This process impairs the infiltration and cytotoxic function of CD8+ T and γδ T cells, creating an "immune desert" TME [16]. The table below summarizes key quantitative findings linking SOX9 to therapy resistance.
Table 1: Key Experimental Findings on SOX9-Mediated Therapy Resistance
| Experimental Model | Finding | Measurement/Effect | Citation |
|---|---|---|---|
| HNSCC Mouse Model (anti-LAG-3 + anti-PD-1) | Enrichment of Sox9+ tumor cells in resistant samples | 42.9% (6/14) of mice were treatment-resistant | [16] |
| HNSCC Mouse Model | Sox9 regulates Anxa1 expression, mediating Fpr1+ neutrophil apoptosis | Reduces neutrophil accumulation, inhibits cytotoxic cell infiltration | [16] |
| Prostate Cancer Analysis | SOX9+ club cells associated with "immune desert" TME | Decreased CD8+CXCR6+ T cells; increased Tregs and M2 macrophages | [4] |
| Gastric Adenocarcinoma | SOX9 associated with maintenance of cancer stem cell (CSC) stemness | Potential target for overcoming drug resistance | [59] |
The dual nature of SOX9 in immunology supports its investigation in combination therapy. While it drives immunosuppression in tumors, its role in maintaining macrophage function for tissue repair suggests that its inhibition must be carefully calibrated [4]. Targeting SOX9 may therefore reverse a key resistance mechanism and enhance the efficacy of PD-1/PD-L1 blockade.
Experimental Protocols for Monitoring Therapy Response
The following protocols describe a workflow from sample processing to computational analysis, tailored for evaluating SOX9-targeting combination therapies.
Protocol 1: Single-Cell RNA Sequencing (scRNA-seq) for Profiling Therapy-Induced Changes in the TME
This protocol is designed to characterize the cellular composition and transcriptional states within the tumor before and after treatment.
1. Sample Preparation and Single-Cell Suspension
- Resect tumor tissues from animal models (e.g., 4NQO-induced HNSCC mice [16] or Lewis Lung Carcinoma mice [60]) or human patients post-treatment.
- Pool tissues from multiple mice per experimental group (e.g., control, resistant, sensitive) to account for biological variability [16].
- Digest tissue using a validated tumor dissociation kit (e.g., gentleMACS) to generate a single-cell suspension.
- Pass cells through a 40-μm cell strainer and perform viability staining (e.g., Trypan Blue). Proceed only if viability exceeds 80%.
2. Library Preparation and Sequencing
- Utilize a droplet-based system (e.g., 10x Genomics Chromium) following the manufacturer's instructions for GEM generation and barcoding.
- Construct libraries using a platform such as Smart-seq3 [59] for full-length transcript coverage.
- Sequence libraries on an Illumina NovaSeq platform to a minimum depth of 50,000 reads per cell.
3. Computational Data Analysis
- Process raw data using Cell Ranger to align reads (to mm10 or GRCh38 reference genomes) and generate feature-barcode matrices.
- Perform quality control in R/Python using Seurat or Scanpy. Filter out cells with unique feature counts <200 or >2500 and >5% mitochondrial counts.
- Cluster cells based on gene expression patterns and annotate cell types using canonical markers:
- Identify malignant epithelial cells using CopyKAT [16] to infer copy number variations.
- Conduct differential expression analysis between treatment groups to identify key pathways (e.g., SOX9, Anxa1, Fpr1 [16]) and cell fate trajectories (e.g., using Monocle3).
Protocol 2: Spatial Transcriptomics for Contextualizing SOX9 Expression and Immune Cell Localization
This protocol maps the expression data generated via scRNA-seq back to the original tissue architecture, preserving spatial context.
1. Tissue Sectioning and Processing
- Embed fresh-frozen tumor tissue in Optimal Cutting Temperature (O.C.T.) compound.
- Cryosection tissue at a thickness of 10 μm and mount onto a Visium Spatial Gene Expression Slide (10x Genomics).
- Stain sections with Hematoxylin and Eosin (H&E) and image with a brightfield microscope.
2. On-Slide cDNA Synthesis and Library Construction
- Permeabilize tissue to release mRNA, optimizing time for maximum mRNA capture (e.g., 12-24 minutes).
- Capture polyadenylated mRNA on the spatially barcoded primers on the slide surface.
- Synthesize cDNA and amplify it following the Visium Spatial Protocol.
- Construct sequencing libraries with sample-specific dual indices and adapter ligation.
3. Spatial Data Integration and Analysis
- Align sequencing data to a reference genome using the Space Ranger pipeline.
- Integrate with scRNA-seq data using cell-type deconvolution methods (e.g., Cell2location, RCTD) to infer the spatial distribution of cell types identified in Protocol 1.
- Visualize gene expression and cell localization in the context of the H&E image.
- Identify spatially variable genes and analyze cell-cell communication in niche areas (e.g., SOX9+ tumor cell clusters and their proximity to Fpr1+ neutrophils [16] or CD8+ T cells).
Signaling Pathways and Workflow Visualization
The following diagram illustrates the core signaling pathway by which SOX9 mediates resistance to combination immunotherapy, as identified in recent research [16].
Sox9-Anxa1-Fpr1 Resistance Pathway: This diagram illustrates the mechanism by which SOX9+ tumor cells drive resistance to anti-LAG-3/PD-1 therapy. SOX9 upregulates Anxa1, which binds to Fpr1 on neutrophils, leading to BNIP3 downregulation, inhibited mitophagy, and subsequent neutrophil apoptosis. The loss of these neutrophils impairs cytotoxic CD8+ and γδ T cell infiltration, resulting in an immunosuppressive tumor microenvironment [16].
The integrated experimental workflow for profiling therapy response, from in vivo modeling to multi-omics analysis, is outlined below.
Therapy Response Profiling Workflow: This workflow outlines the key steps for monitoring therapy response, from generating a treatment model to integrated data analysis. The process begins with establishing an in vivo model, administering therapies, and processing tumor tissues for high-resolution sequencing. scRNA-seq and spatial transcriptomics data are generated and integrated to provide a comprehensive view of changes in the tumor microenvironment, ultimately leading to mechanistic validation [16] [59] [61].
The Scientist's Toolkit: Essential Research Reagents and Platforms
The table below catalogs key reagents, technologies, and computational tools essential for executing the described protocols.
Table 2: Key Research Reagent Solutions for Single-Cell and Spatial Studies
| Category | Item | Function/Application | Example/Source |
|---|---|---|---|
| In Vivo Models | 4NQO-induced HNSCC Model | Models human head and neck cancer pathogenesis and therapy response [16] | C57BL/6 wild-type mice |
| Lewis Lung Carcinoma (LLC) Model | Standard immunocompetent model for studying NSCLC and immunotherapy [60] | C57BL/6 mice | |
| Humanized Mouse Model (HuNCG) | Engrafted with human CD34+ cells to study human immune cell interactions in vivo [60] | NCG mice | |
| Key Reagents | Anti-PD-1 Antibody | Immune checkpoint blockade; induces T cell reactivation [16] [60] | Clone RMP1-14 (mouse) |
| Anti-LAG-3 Antibody | Immune checkpoint blockade; used in combination with anti-PD-1 [16] | Relatlimab (human) | |
| Single-Cell Tech | Droplet-Based scRNA-seq | High-throughput single-cell transcriptome profiling [59] | 10x Genomics Chromium |
| Full-Length scRNA-seq | In-depth sequencing of single cells with superior gene detection [59] | Smart-seq3 | |
| Spatial Tech | Spatial Gene Expression | Captures genome-wide RNA expression within tissue morphology [61] | 10x Genomics Visium |
| Computational Tools | Cell Type Annotation | Clustering and visualization of scRNA-seq data [16] [61] | Seurat, Scanpy |
| CNV Analysis | Identifies malignant cells from scRNA-seq data [16] | CopyKAT | |
| Spatial Data Deconvolution | Maps cell types from scRNA-seq onto spatial transcriptomics spots [61] | Cell2location, RCTD | |
| Key Targets | SOX9 | Transcription factor; biomarker and mediator of therapy resistance [4] [16] | N/A |
| ANXA1 / FPR1 | Ligand-receptor pair mediating neutrophil apoptosis in resistance [16] | N/A |
The application of single-cell and spatial transcriptomics provides a powerful, multi-dimensional framework for monitoring response to novel combination therapies targeting SOX9 and PD-1/PD-L1. The detailed protocols and tools outlined herein enable researchers to move beyond bulk analyses, uncover novel resistance mechanisms like the SOX9-Anxa1-Fpr1 axis, and spatially map the resulting immunosuppressive landscapes. As these technologies continue to evolve, their integration will be critical for translating mechanistic insights into effective clinical strategies that overcome immunotherapy resistance.
Preclinical and Clinical Validation of SOX9/PD-1 Combination Efficacy
The transcription factor SOX9 (SRY-related HMG box 9) has emerged as a critical regulator in cancer biology and immunology, exhibiting context-dependent dual functions that present both challenges and opportunities for therapeutic intervention. As a novel Janus-faced regulator in immunity, SOX9 demonstrates opposing roles across different biological contexts [4]. In cancer, SOX9 frequently shows overexpression in various solid malignancies, where it promotes tumor progression, chemoresistance, and immune evasion [4]. Conversely, in certain inflammatory and tissue repair contexts, SOX9 contributes to maintaining macrophage function and facilitating cartilage formation and tissue regeneration [4].
The growing interest in targeting SOX9 within combination immunotherapy regimens stems from its significant role in modulating the tumor immune microenvironment. Recent evidence demonstrates that SOX9+ tumor cells mediate resistance to combined anti-PD-1 and anti-LAG-3 immunotherapy in head and neck squamous cell carcinoma (HNSCC) through interaction with Fpr1+ neutrophils [16]. This positions SOX9 as a promising therapeutic target to overcome resistance to immune checkpoint blockade, particularly in the context of PD-1/PD-L1 inhibition strategies.
This application note provides comprehensive protocols and methodological frameworks for validating SOX9 targeting strategies using transgenic mouse models and patient-derived xenografts (PDX), with specific emphasis on combination therapies with PD-1/PD-L1 blockade.
Table 1: Key Experimental Findings on SOX9 in Cancer and Immunotherapy
| Experimental Model | Key Finding Related to SOX9 | Biological Consequence | Citation/Reference |
|---|---|---|---|
| HNSCC mouse model (4NQO-induced) | SOX9+ tumor cell enrichment in anti-LAG-3 + anti-PD-1 resistant samples | Mediated resistance via ANXA1-FPR1 axis reducing neutrophil accumulation | [16] |
| Colorectal Cancer PDX models | SOX9 expression negatively correlates with B cells, resting mast cells, monocytes | Creates immunosuppressive microenvironment | [4] |
| Various solid malignancies (bioinformatics analysis) | SOX9 overexpression in liver, lung, breast, gastric cancers | Promotes vascularization, drug resistance, proliferation, metastasis | [4] |
| Prostate Cancer (single-cell RNA-seq) | SOX9+ club cell subpopulation enrichment after androgen deprivation therapy | Potential contribution to immunosuppressive niche | [4] |
Table 2: SOX9 Correlation with Immune Cell Infiltration in Tumor Microenvironment
| Immune Cell Type | Correlation with SOX9 Expression | Functional Impact |
|---|---|---|
| B cells | Negative correlation | Reduced humoral immunity |
| Resting mast cells | Negative correlation | Diminished innate immune surveillance |
| CD8+ T cells | Negative correlation with functional genes | Impaired cytotoxic T-cell function |
| M1 macrophages | Negative correlation | Reduced anti-tumor macrophage activity |
| Neutrophils | Positive correlation | Increased pro-tumor inflammation |
| Macrophages | Positive correlation | Enhanced pro-tumor macrophage polarization |
| Activated mast cells | Positive correlation | Potential promotion of pro-tumor inflammation |
Experimental Protocols and Methodologies
Protocol 1: Establishing PDX Models for SOX9 Research
Objective: To establish patient-derived xenograft models that retain SOX9 expression characteristics and tumor microenvironment features for evaluating SOX9-targeted combination therapies.
Materials:
- Immunodeficient mice (NSG, NOG, or NOD-SCID recommended)
- Patient tumor tissue (surgical resection or biopsy)
- Basement membrane matrix (e.g., Matrigel)
- Sterile surgical instruments
- DNA/RNA preservation reagents
Procedure:
Tumor Tissue Acquisition and Processing:
- Obtain fresh tumor tissue from surgical resection or biopsy under sterile conditions.
- For higher success rates, prioritize tissues from radical surgical resections over biopsy samples when possible [62].
- Process tissue either as:
- Fragments (1-2 mm³): Preserves intercellular interactions and tumor architecture
- Single-cell suspensions: Reduces heterogeneity but may decrease cellular activity
Implantation:
- Mix tumor tissue with basement membrane matrix (e.g., Matrigel) to enhance engraftment efficiency [62].
- Implant subcutaneously into the flank of immunodeficient mice (designated as F0 generation).
- Alternative implantation sites include orthotopic locations, intracapsular fat pad, or under the renal capsule for specific tumor types [63].
Monitoring and Passaging:
- Monitor tumor growth regularly, measuring volume 2-3 times per week.
- First generation (F0) typically reaches 1-2 cm³ within variable timeframes (few days to several months).
- Harvest tumor at appropriate size, segment, and reimplant into subsequent mouse generations (F1, F2, etc.).
- Stabilize model through passages (typically by F3) before experimental use [62] [63].
Validation:
- Validate retention of SOX9 expression patterns across passages using IHC, RNA-seq, or Western blot.
- Confirm preservation of original tumor histopathology and genetic features.
Protocol 2: Evaluating SOX9-Targeted Combination Therapy in Transgenic Models
Objective: To assess the efficacy of SOX9 inhibition in combination with PD-1/PD-L1 blockade using immunocompetent transgenic mouse models.
Materials:
- SOX9-floxed transgenic mice (for conditional knockout)
- Immunocompetent tumor models (e.g., 4NQO-induced HNSCC, GEMMs)
- Anti-PD-1/PD-L1 therapeutic antibodies
- SOX9 inhibitors (small molecules or genetic approaches)
- Flow cytometry antibodies for immune profiling
Procedure:
Model Establishment:
- For HNSCC studies: Treat C57BL/6 wild-type mice with 4NQO in drinking water (50 µg/mL) for 16 weeks, followed by normal water for 8 weeks to induce tumor formation [16].
- For conditional SOX9 knockout: Cross SOX9-floxed mice with appropriate Cre-recombinase strains (e.g., K14-Cre for epithelial-specific deletion).
Therapeutic Intervention:
- Randomize tumor-bearing mice with comparable lesion sizes into experimental groups:
- Group 1: Isotype control antibody
- Group 2: Anti-PD-1/PD-L1 monotherapy
- Group 3: SOX9 inhibition monotherapy
- Group 4: SOX9 inhibition + anti-PD-1/PD-L1 combination
- Administer treatments via appropriate routes (intraperitoneal for antibodies).
- Randomize tumor-bearing mice with comparable lesion sizes into experimental groups:
Response Monitoring:
- Measure tumor dimensions regularly (every 3-4 days).
- Classify response according to RECIST criteria:
- Resistant: >20% increase in tumor size from baseline
- Sensitive: significant tumor reduction [16]
- Monitor survival and overall therapeutic benefit.
Endpoint Analysis:
- Harvest tumors and process for:
- Single-cell RNA sequencing for immune profiling
- Immunohistochemistry for SOX9, ANXA1, FPR1, and immune markers
- Flow cytometry for comprehensive immune cell characterization
- Harvest tumors and process for:
Protocol 3: Single-Cell RNA Sequencing for SOX9-Mediated Resistance Mechanisms
Objective: To characterize SOX9-dependent resistance mechanisms to immune checkpoint blockade at single-cell resolution.
Materials:
- Single-cell RNA sequencing platform (10X Genomics recommended)
- Tissue dissociation reagents
- Cell viability staining kit
- Bioinformatics analysis tools (Seurat, CopyKAT)
Procedure:
Sample Preparation:
- Pool tumor tissues from 3 mice per experimental condition.
- Digest tissues into single-cell suspensions using appropriate enzymatic cocktails.
- Filter through 40μm strainers and assess viability (>80% required).
Library Preparation and Sequencing:
- Load cells onto single-cell platform according to manufacturer's instructions.
- Target 5,000-10,000 cells per sample for adequate representation.
- Sequence to sufficient depth (≥50,000 reads per cell recommended).
Bioinformatic Analysis:
- Perform quality control filtering to remove low-quality cells and doublets.
- Use CopyKAT algorithm to distinguish malignant from non-malignant epithelial cells [16].
- Identify cell clusters and annotate based on canonical markers.
- Analyze SOX9 expression across subpopulations and conditions.
- Conduct cell-cell communication analysis to identify SOX9-dependent interactions.
Signaling Pathways and Molecular Mechanisms
SOX9-Mediated Immunotherapy Resistance Mechanism
Experimental Workflow: Comprehensive PDX Establishment
PDX Model Establishment Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for SOX9 and Immunotherapy Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Immunodeficient Mouse Strains | NSG, NOG, NOD-SCID, BRG | Host for PDX models; varying degrees of immunodeficiency for human cell engraftment |
| SOX9 Detection Reagents | Anti-SOX9 antibodies, SOX9 probes, SOX9 reporter constructs | Monitoring SOX9 expression, localization, and activity |
| Immune Checkpoint Inhibitors | Anti-PD-1, Anti-PD-L1, Anti-LAG-3 antibodies | Immune checkpoint blockade in combination studies |
| Single-Cell Analysis Platforms | 10X Genomics, Smart-seq2 | Characterizing tumor heterogeneity and immune microenvironment |
| Cell Lineage Tracing Tools | Cre-lox system, SOX9-floxed mice, CellBrite dyes | Tracking SOX9+ cell populations and their progeny |
| Tumor Dissociation Kits | Miltenyi Tumor Dissociation kits, Collagenase/Hyaluronidase mixes | Preparing single-cell suspensions for analysis and implantation |
| Cell Sorting Reagents | FACS antibodies, Magnetic bead separation kits | Isolating specific immune cell populations for functional studies |
The integration of transgenic mouse models and patient-derived xenografts provides a powerful platform for validating SOX9 as a therapeutic target in combination with PD-1/PD-L1 blockade. The protocols outlined in this application note enable researchers to systematically investigate SOX9-mediated resistance mechanisms and develop effective combination strategies. The consistent observation of SOX9+ tumor cell enrichment in immunotherapy-resistant settings across multiple cancer types underscores the translational potential of this research avenue.
Future directions should focus on developing clinical-grade SOX9 inhibitors, identifying biomarkers for patient stratification, and optimizing treatment sequencing in SOX9-targeted combination regimens. The continued refinement of these preclinical models will accelerate the translation of SOX9-targeting strategies into clinical trials, potentially overcoming significant limitations of current immunotherapy approaches.
Application Note
This application note provides a comparative analysis of the transcription factor SOX9 across four cancer types: Glioblastoma (GBM), Head and Neck Squamous Cell Carcinoma (HNSCC), Breast Cancer, and Lung Cancers. Framed within the broader thesis of targeting SOX9 in combination with PD-1/PD-L1 blockade, this document synthesizes current evidence on SOX9's role in tumor progression, immune evasion, and therapy resistance. It aims to equip researchers and drug development professionals with consolidated data, standardized protocols, and key reagents to advance the development of SOX9-targeting combination immunotherapies.
SOX9 as a Cross-Cancer Biomarker and Therapeutic Target
SOX9 is a high-mobility group (HMG) box transcription factor that regulates embryonic development and stem cell maintenance. Its dysregulation is a common oncogenic mechanism across multiple solid tumors. SOX9 promotes cancer stem cell (CSC) self-renewal, tumor progression, and resistance to therapy. Crucially, emerging evidence identifies SOX9 as a master regulator of the tumor immune microenvironment, particularly through mechanisms that complement the PD-1/PD-L1 axis.
- GBM: SOX9 is highly expressed in GBM tissues and is a critical regulator of Glioma Stem Cells (GSCs). It maintains GSC activity through a regulatory loop with STAT3 and PML, and its high expression correlates with poorer patient survival [64]. Intriguingly, in specific subgroups (e.g., IDH-mutant), high SOX9 may be associated with a better prognosis, highlighting context-dependent roles [11] [20].
- HNSCC: Single-cell RNA sequencing of HNSCC mouse models resistant to anti-LAG-3 plus anti-PD-1 therapy revealed significant enrichment of SOX9+ tumor cells. This population drives resistance by modulating neutrophil activity via the ANXA1-FPR1 axis, thereby impairing cytotoxic T cell function [16].
- Breast Cancer: In basal-like breast cancer (BLBC), SOX9 is upregulated in dedifferentiated tumor cells and is essential for immunosuppression. It directly induces the expression of the immune checkpoint molecule B7x (B7-H4/VTCN1), creating an immune-cold tumor microenvironment and protecting tumor cells from T cell-mediated killing [34] [33].
- Lung Cancer: SOX9 is upregulated in lung adenocarcinoma (LUAD) and correlates with poorer overall survival. It suppresses the tumor microenvironment and shows mutual exclusivity with various immune checkpoints, suggesting a complementary role in immune evasion [11] [20].
Table 1: Prognostic and Immunological Role of SOX9 Across Cancers
| Cancer Type | SOX9 Expression | Prognostic Association | Role in Therapy Resistance | Key Immune Mechanism |
|---|---|---|---|---|
| Glioblastoma (GBM) | Highly expressed [64] | Poor overall survival [64]; Better prognosis in IDH-mutant subgroups [11] | Essential for GSC self-renewal and temozolomide resistance [64] [65] | Correlated with immune cell infiltration and checkpoint expression [11] |
| HNSCC | Enriched in resistant tumors [16] | Associated with resistance to anti-LAG-3 + anti-PD-1 [16] | Mediates resistance to combo immunotherapy [16] | SOX9→ANXA1→FPR1 axis reduces neutrophil accumulation and CD8+ T cell killing [16] |
| Breast Cancer | Upregulated in dedifferentiated cells [34] | Promotes progression from DCIS to invasive carcinoma [34] | Confers resistance to anti-PD-L1; targetable to overcome it [34] | SOX9→B7x axis reduces CD8+ T cell infiltration [34] [33] |
| Lung Cancer | Upregulated in LUAD [11] | Poorer overall survival [11] | Suppresses tumor microenvironment [11] | Mutually exclusive with other immune checkpoints [11] |
Key Signaling Pathways and Workflows
The following diagrams, generated using Graphviz DOT language, illustrate the core SOX9-mediated signaling pathways and a generalized experimental workflow for investigating SOX9 in immunotherapy resistance.
Diagram 1: SOX9-Mediated Immunosuppressive Pathways in Cancer This diagram consolidates the key SOX9-driven mechanisms that inhibit anti-tumor immunity across different cancer types.
Diagram 2: Workflow for Profiling SOX9 in Immunotherapy Resistance This workflow outlines a standard pipeline for identifying and validating SOX9's role in resistance to immune checkpoint blockade.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Investigating SOX9 in Cancer and Immunobiology
| Reagent / Tool | Function / Application | Example Use-Case |
|---|---|---|
| Anti-SOX9 Antibodies | Detection and quantification of SOX9 expression via IHC, Western Blot, IF. | Validating SOX9 upregulation in patient tumor samples or murine models [34] [66]. |
| SOX9 shRNA/sgRNA Lentivirus | Stable knockdown or knockout of SOX9 in vitro and in vivo. | Assessing the necessity of SOX9 for GSC self-renewal and tumorigenicity [64] [65]. |
| scRNA-seq Platform | Unbiased profiling of tumor heterogeneity and identification of SOX9+ subpopulations. | Discovering SOX9-enriched tumor cells in immunotherapy-resistant HNSCC [16]. |
| In Vivo Syngeneic Models | Evaluation of SOX9 function and therapeutic targeting within an intact immune system. | Studying the SOX9-B7x axis in immunocompetent breast cancer models [34]. |
| Recombinant B7x / ANXA1 Protein | Functional studies of SOX9 downstream effector molecules. | Investigating B7x-mediated T cell suppression or ANXA1-FPR1 neutrophil interactions [16] [34]. |
| Flow Cytometry Panels (Immune Cell) | Quantification of tumor-infiltrating lymphocyte (TIL) populations. | Demonstrating reduced CD8+ T cell infiltration in SOX9-high tumors [34]. |
| STAT3/PML Inhibitors | Pharmacological perturbation of the SOX9 signaling network. | Targeting the SOX9-STAT3-PML loop in GSCs to reduce tumorigenicity [64]. |
Detailed Experimental Protocols
Protocol 1: Evaluating SOX9-Mediated Immunotherapy Resistance In Vivo
Objective: To determine the role of SOX9 in resistance to PD-1/PD-L1 blockade and test combination strategies.
Materials:
- C57BL/6 wild-type mice or other immunocompetent strains.
- Syngeneic cancer cells (e.g., 4NQO-induced HNSCC cells [16], C3-TAg breast cancer cells [34]).
- Anti-PD-1 antibody (e.g., nivolumab analog).
- Anti-LAG-3 antibody (e.g., relatlimab analog) [16].
- Anti-B7x antibody [34] or SOX9 inhibitor.
- Equipment for scRNA-seq (e.g., 10X Genomics).
Procedure:
- Model Establishment: Induce tumors in mice (e.g., via 4NQO administration for HNSCC or orthotopic injection of breast cancer cells) [16] [34].
- Treatment Groups: Randomize tumor-bearing mice into groups (n≥5): (a) Isotype control IgG, (b) anti-PD-1 monotherapy, (c) anti-PD-1 + anti-LAG-3, (d) anti-PD-1 + anti-LAG-3 + SOX9-pathway inhibitor (e.g., anti-B7x).
- Monitoring: Measure tumor volume with calipers every 3-4 days. Classify mice as resistant or sensitive based on RECIST criteria (e.g., >20% growth from baseline) [16].
- Tissue Collection: At endpoint, harvest tumors from each group. A portion is snap-frozen for protein/RNA analysis; another portion is digested into a single-cell suspension for scRNA-seq.
- scRNA-seq Analysis: Process cells per manufacturer's protocol. Use CopyKAT to distinguish malignant cells. Cluster cells and identify SOX9+ subpopulations. Perform differential expression and pathway analysis on SOX9-high vs. SOX9-low clusters [16].
- Immune Profiling: Analyze the remaining single-cell suspension by flow cytometry using antibodies against CD45, CD3, CD8, CD4, FPR1 (for neutrophils), and other lineage markers to quantify immune infiltration [34].
Protocol 2: Functional Validation of SOX9 in Immune Evasion
Objective: To test the direct impact of tumor cell SOX9 on T cell function in a co-culture system.
Materials:
- Human cancer cell lines (e.g., HCC1937 TNBC cells, MCF7ras cells) [34].
- Human Peripheral Blood Mononuclear Cells (PBMCs) from healthy donors.
- Lentiviral vectors for SOX9 overexpression (SOX9-OE) and control (Vector-CTRL).
- Anti-CD3/CD28 activation beads.
- CFSE Cell Division Tracker Kit.
- Flow cytometer.
Procedure:
- Cell Engineering: Stably transduce cancer cells with SOX9-OE or Vector-CTRL lentiviruses. Validate overexpression by Western blot.
- T Cell Isolation: Isolate CD4+ and CD8+ T cells from PBMCs using negative selection kits.
- CFSE Labeling: Label isolated T cells with CFSE according to the manufacturer's protocol to track proliferation.
- Co-culture Setup: Plate irradiated (to prevent cancer cell proliferation) SOX9-OE or Vector-CTRL cells. Add CFSE-labeled T cells and anti-CD3/CD28 beads at a predetermined tumor cell:T cell ratio (e.g., 1:5).
- Incubation: Co-culture cells for 3-5 days.
- Flow Cytometry Analysis: Harvest T cells and analyze by flow cytometry. Measure CFSE dilution to quantify proliferation. Additionally, stain for activation markers (e.g., CD69) and intracellular cytokines (e.g., IFN-γ) after restimulation [34].
The comparative analysis underscores SOX9 as a pivotal, cross-cancer regulator of tumor stemness and immune evasion. Its ability to drive resistance to checkpoint blockade via distinct, context-specific pathways—such as inducing B7x in breast cancer and modulating neutrophils via ANXA1 in HNSCC—positions it as a compelling next-generation target. Future research should prioritize the development of potent and specific SOX9 inhibitors (e.g., small molecules, protein degraders) and rigorously evaluate their synergy with existing immunotherapies in advanced preclinical models. Integrating SOX9 status as a biomarker in clinical trials for PD-1/PD-L1 inhibitors could further stratify patient populations and unlock novel combination strategies to overcome therapeutic resistance.
This application note provides a detailed protocol for the validation of key biomarkers—SOX9 expression, IDH mutation status, and immune signatures—within the context of advancing combination therapies targeting SOX9 alongside PD-1/PD-L1 blockade. The role of the tumor microenvironment (TME) and specific genetic alterations is critical in modulating response to immunotherapy. SOX9, a transcription factor and cancer stem cell (CSC) marker, is overexpressed in multiple malignancies, including bone cancer and glioblastoma (GBM), and correlates with tumor severity, metastasis, and poor response to therapy [67] [20]. Concurrently, IDH mutation status serves as a pivotal prognostic and classification marker in gliomas, with IDH-wild-type tumors exhibiting significantly more aggressive behavior [68] [69]. Furthermore, the density and functional orientation of tumor-infiltrating immune cells are powerful determinants of clinical outcomes. This document outlines standardized methods to quantitatively assess these parameters, enabling robust stratification of patients for novel therapeutic combinations.
Quantitative Biomarker Profiles
The clinical utility of a biomarker is determined by its performance characteristics, including sensitivity, specificity, and prognostic value. The tables below summarize key quantitative data for SOX9 and IDH status across different cancer types and clinical contexts.
Table 1: SOX9 Expression as a Diagnostic and Prognostic Biomarker
| Cancer Type | Sample Type | Expression Pattern | Clinical Correlation | Statistical Significance (P-value) |
|---|---|---|---|---|
| Primary Bone Cancer [67] | Tissue & PBMCs | Overexpression vs. margin | Malignant vs. Benign tumors | < 0.0001 |
| Primary Bone Cancer [67] | Tissue & PBMCs | Overexpression vs. margin | Association with metastasis | < 0.0001 |
| Primary Bone Cancer [67] | Tissue & PBMCs | Overexpression vs. margin | Association with recurrence | < 0.0001 |
| Primary Bone Cancer [67] | Circulating (PBMC) | Overexpression vs. healthy controls | Diagnosis of malignant bone cancer | < 0.0001 |
| Glioblastoma (GBM) [20] | Tissue | High Expression | Better prognosis in lymphoid invasion subgroup | < 0.05 |
| Glioblastoma (GBM) [20] | Tissue | High Expression | Independent prognostic factor for IDH-mutant | Significant (Cox) |
Table 2: IDH Mutation Status as a Prognostic Biomarker in Glioblastoma
| Parameter | IDH-Mutant Group | IDH-Wild-Type Group | P-value / Hazard Ratio (HR) |
|---|---|---|---|
| Median Overall Survival [68] | 16.0 months | 6.5 months | P = 0.030 |
| Mean Age [68] | 53.93 ± 12.00 | 62.39 ± 10.12 | P = 0.003 |
| Prognostic Value [68] | Favorable Prognosis | Independent poor prognostic factor (HR = 2.84, 95% CI: 1.56–5.18) | - |
| Machine Learning Prediction (MRI) [69] | AUC: 0.835 (External Validation) | - | - |
Table 3: Inflammatory Ratios as Accessible Prognostic Biomarkers
| Biomarker | Cut-off Value | Sensitivity | Specificity | Prognostic Implication |
|---|---|---|---|---|
| Neutrophil/Lymphocyte Ratio (NLR) [68] | > 3.39 | 95.12% | 52.0% | Independent poor prognostic factor (HR = 1.84, 95% CI: 1.16–2.92) |
| Platelet/Lymphocyte Ratio (PLR) [68] | > 136.25 | 80.49% | 64.0% | Associated with poor prognosis |
Experimental Protocols
Protocol for Validating Local and Circulating SOX9 Expression
Principle: This protocol quantifies SOX9 expression at the gene and protein level in both tumor tissues and peripheral blood mononuclear cells (PBMCs) to assess its value as a local and circulating biomarker [67].
Materials:
- Patient Samples: Fresh or frozen tumor tissues, matched tumor margin tissues, and whole blood samples from patients and healthy controls.
- RNA Extraction Kit: e.g., TRIzol-based or column-based kits.
- Reverse Transcription Kit: For cDNA synthesis.
- Real-Time PCR System: and SYBR Green or TaqMan master mix. SOX9-specific primers.
- Lysis Buffer: RIPA buffer supplemented with protease inhibitors (e.g., PMSF).
- Antibodies: Validated anti-SOX9 antibody for Western Blot (WB) and Immunohistochemistry (IHC), and corresponding HRP-conjugated secondary antibodies.
- PVDF Membrane and Western Blotting equipment.
- IHC Kit: including blocking serum, biotinylated secondary antibody, and streptavidin-HRP with DAB substrate.
Procedure:
- Sample Preparation:
- Extract total RNA from homogenized tissue samples or isolated PBMCs using the RNA extraction kit. Assess RNA purity and concentration.
- Synthesize cDNA from 1 µg of total RNA using the reverse transcription kit.
- Gene Expression Analysis (Real-Time PCR):
- Prepare PCR reactions with SYBR Green master mix, specific SOX9 primers, and cDNA template.
- Run the reactions in triplicate on a real-time PCR system. Use GAPDH or β-actin as an endogenous control for normalization.
- Calculate the relative expression of SOX9 using the 2^(-ΔΔCt) method. Compare tumor vs. margin, malignant vs. benign, and patient PBMCs vs. healthy control PBMCs.
- Protein Expression Analysis (Western Blot):
- Lyse tissue samples in RIPA buffer with protease inhibitors. Quantify total protein concentration.
- Separate 20-30 µg of protein by SDS-PAGE and transfer to a PVDF membrane.
- Block the membrane with 5% non-fat milk, then incubate with primary anti-SOX9 antibody overnight at 4°C.
- Incubate with HRP-conjugated secondary antibody for 1 hour at room temperature.
- Develop the blot using a chemiluminescent substrate and image the signal. Re-probe for β-actin as a loading control.
- Protein Localization (Immunohistochemistry):
- Deparaffinize and rehydrate formalin-fixed, paraffin-embedded (FFPE) tissue sections.
- Perform antigen retrieval using a citrate-based buffer. Quench endogenous peroxidase activity.
- Block sections with appropriate serum, then incubate with anti-SOX9 antibody.
- Apply biotinylated secondary antibody followed by streptavidin-HRP.
- Develop with DAB substrate, counterstain with hematoxylin, dehydrate, and mount.
- Score staining intensity (0-3+) and the percentage of positive cells by a pathologist blinded to the clinical data.
Protocol for Determining IDH Status and Correlative Immune Analysis
Principle: This protocol defines the IDH mutation status via immunohistochemistry and profiles the associated immune tumor microenvironment using RNA sequencing data and bioinformatic tools [68] [20] [69].
Materials:
- FFPE Glioma Tissue Sections.
- Anti-IDH1 R132H Antibody (most common mutation).
- RNA Extraction Kit (compatible with FFPE tissues if required).
- Computational Resources: Access to TCGA, GTEx databases, and R/Bioconductor with packages (DESeq2, ClusterProfiler, GSVA, survminer).
Procedure:
- IDH Mutation Status Determination (IHC):
- Perform IHC on FFPE glioma sections using the anti-IDH1 R132H antibody, following steps similar to section 3.1.4.
- A lack of nuclear staining classifies the tumor as IDH-wild-type, while positive nuclear staining confirms the presence of the most common IDH1 mutation. DNA sequencing is recommended for IHC-negative cases to rule out rarer IDH1/2 mutations.
- RNA Sequencing and Data Acquisition:
- Extract high-quality RNA from tumor tissues and submit for RNA sequencing. Alternatively, download processed RNA-seq data (e.g., HTSeq-Counts or FPKM) for GBM samples from public repositories like TCGA.
- Immune Cell Infiltration Analysis (ssGSEA):
- Using R, load the gene expression matrix and the GSVA package.
- Perform single-sample Gene Set Enrichment Analysis (ssGSEA) by calculating enrichment scores for gene signatures representative of various immune cell types (e.g., T cells, B cells, macrophages, neutrophils) in each tumor sample.
- Correlate the ssGSEA scores for each immune cell type with SOX9 expression levels using Spearman's rank correlation test.
- Immune Checkpoint Expression Analysis:
- Extract normalized expression values for key immune checkpoint genes (e.g., PD-1, PD-L1, CTLA-4) from the gene expression dataset.
- Compare the expression levels of these checkpoints between tumors with high vs. low SOX9 expression using the Wilcoxon rank-sum test.
- Survival Analysis:
- Integrate patient overall survival (OS) data with SOX9 expression and IDH status.
- Use the
survminerandsurvivalpackages in R to perform Kaplan-Meier analysis, stratifying patients into high and low SOX9 expression groups. The log-rank test will determine the significance of survival differences. - Perform univariate and multivariate Cox regression analysis to evaluate whether SOX9 expression is an independent prognostic factor.
Protocol for Non-Invasive IDH Prediction via Machine Learning on MRI
Principle: This protocol leverages a machine learning (ML) model applied to routine clinical MRI to preoperatively predict IDH mutation status, offering a non-invasive alternative to biopsy [69].
Materials:
- Multi-institutional MRI Datasets: Pre-treatment T1-post contrast (T1pc) and T2-FLAIR sequences from glioma patients with confirmed IDH status.
- Segmentation Software: e.g., 3D Slicer or ITK-SNAP.
- Computing Environment: Python with scikit-learn, XGBoost, and PyRadiomics libraries.
Procedure:
- Image Acquisition and Tumor Segmentation:
- Collect routine preoperative MRI scans (T1pc and T2-FLAIR) from patients.
- Manually or semi-automatically segment the entire tumor volume on all relevant slices using the segmentation software to create a 3D volume of interest (VOI).
- Feature Extraction:
- Use the PyRadiomics library in Python to extract a comprehensive set of quantitative features (shape, first-order statistics, and texture features) from the segmented tumor VOI on each MRI sequence.
- Model Building and Validation:
- Split the dataset from one institution into training and internal validation sets.
- Apply an Extreme Gradient Boosting (XGBoost) classifier on the extracted features to predict IDH status (mutant vs. wild-type).
- Tune the model hyperparameters using cross-validation on the training set.
- Assess model performance on the internal validation set by calculating Area Under the Curve (AUC), Accuracy, Sensitivity, and Specificity.
- To ensure generalizability, perform external validation by applying the finalized model to a completely separate MRI dataset from a different institution.
Signaling Pathways and Workflow Diagrams
The following diagrams illustrate the key experimental workflows and the conceptual relationship between SOX9, IDH status, and the immune microenvironment in the context of PD-1/PD-L1 blockade research.
Experimental Workflow for Biomarker Validation
SOX9 and IDH in Tumor Biology and Therapy
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Resources for Biomarker Validation
| Item | Function / Application | Example / Key Identifier |
|---|---|---|
| Anti-SOX9 Antibody | Detection and quantification of SOX9 protein in IHC and Western Blot. | Validation for specific applications (IHC, WB) is critical. |
| Anti-IDH1 R132H Antibody | Immunohistochemical detection of the most common IDH mutation in gliomas. | Clone HMab-1 is commonly used. |
| PBMC Isolation Kit | Isolation of peripheral blood mononuclear cells for circulating biomarker analysis. | e.g., Ficoll-Paque density gradient centrifugation kits. |
| RNA Extraction Kit | High-quality RNA isolation from tissues and cells for downstream transcriptomic analysis. | Compatibility with FFPE tissues is required for some studies. |
| Real-Time PCR System & Reagents | Quantitative measurement of gene expression (e.g., SOX9, immune checkpoints). | SYBR Green or TaqMan chemistries. |
| Radiomics Feature Extraction Software | Extraction of quantitative features from medical images for machine learning. | e.g., PyRadiomics library in Python. |
| TCGA & GTEx Databases | Publicly available repositories for genomic, transcriptomic, and clinical data. | https://portal.gdc.cancer.gov/ ; https://gtexportal.org/ |
| Bioinformatics Software (R/Python) | Statistical analysis, survival analysis, and immune deconvolution (e.g., ssGSEA). | R packages: DESeq2, GSVA, survminer. |
Head-to-Head Comparisons with Other Combination Immunotherapy Regimens
The therapeutic landscape of cancer immunotherapy has evolved significantly beyond PD-1/PD-L1 monotherapy toward combination strategies aimed at overcoming primary and acquired resistance. Within this context, the transcription factor SOX9 has emerged as a critical regulator of therapeutic response and resistance mechanisms. Recent investigations have revealed that SOX9 operates as a molecular switch within the tumor microenvironment, capable of orchestrating immunosuppressive networks that diminish the efficacy of combination immunotherapies [4]. This application note provides a comprehensive experimental framework for evaluating SOX9-targeting strategies alongside established combination immunotherapy regimens, with detailed protocols for assessing therapeutic efficacy, immune cell dynamics, and resistance mechanisms.
Current Landscape of Combination Immunotherapy Regimens
Clinically Validated Combination Approaches
Table 1: FDA-Approved Combination Immunotherapy Regimens in Oncology
| Combination Therapy | Targets | Approved Indications | Key Clinical Trial Findings |
|---|---|---|---|
| Nivolumab + Ipilimumab | PD-1 + CTLA-4 | Melanoma, RCC, CRC, HCC, NSCLC, Mesothelioma, Esophageal SCC | Synergistic effects improving ORR, OS, and PFS across multiple malignancies [70] |
| Durvalumab + Tremelimumab | PD-L1 + CTLA-4 | Multiple solid tumors | Demonstrated clinical benefit in specific cancer types with manageable safety profile [70] |
| Relatlimab + Nivolumab | LAG-3 + PD-1 | Metastatic/unresectable melanoma | 12-month PFS significantly higher than nivolumab alone (RELATIVITY-047 trials) [16] |
| Pembrolizumab + Chemotherapy | PD-1 + Chemo | NSCLC, HNSCC, others | Improved outcomes across cancer types, with variable efficacy based on PD-L1 expression [71] |
Emerging Combination Strategies in Clinical Development
Recent clinical investigations have expanded the combination immunotherapy landscape, particularly in non-small cell lung cancer (NSCLC). The INSIGHT-003 trial evaluated a novel triple combination of eftilagimod alfa (efti, a LAG-3 related MHC Class II agonist) with pembrolizumab and chemotherapy in first-line non-squamous NSCLC, demonstrating strong objective response rates (ORR) across all PD-L1 expression levels [71]. Notably, in patients with low and no PD-L1 expression (TPS <50%), representing over two-thirds of the NSCLC population, this combination achieved a 61.7% ORR compared to 40.8% in historical controls [71].
Network meta-analyses of randomized controlled trials have further refined our understanding of optimal combination approaches. In advanced squamous NSCLC, camrelizumab plus chemotherapy demonstrated superior overall survival (HR 0.56) and progression-free survival (HR 0.32) outcomes, while penpulimab plus chemotherapy provided the best overall survival benefit (HR 0.55) for patients with non-selective PD-L1 advanced NSCLC [72]. These comparative efficacy analyses provide critical benchmarks for evaluating novel SOX9-targeting combinations.
SOX9-Mediated Resistance to Combination Immunotherapy: Experimental Evidence
Mechanism of SOX9 in Driving Immunotherapy Resistance
Recent investigation has elucidated a novel resistance mechanism mediated by SOX9 in head and neck squamous cell carcinoma (HNSCC) models treated with anti-LAG-3 plus anti-PD-1 combination therapy. Single-cell RNA sequencing of resistant tumors revealed significant enrichment of SOX9+ tumor cells, which directly regulate annexin A1 (Anxa1) expression [16] [73]. This SOX9-Anxa1 axis promotes apoptosis of formyl peptide receptor 1 (Fpr1)+ neutrophils through mitochondrial fission and inhibition of mitophagy via downregulation of Bnip3 expression [16]. The consequent reduction in Fpr1+ neutrophil accumulation impairs infiltration and cytotoxic function of CD8+ T and γδT cells within the tumor microenvironment, ultimately driving therapeutic resistance [16] [73].
SOX9 Expression Patterns and Immune Correlations
Analysis of SOX9 expression across malignancies reveals consistent overexpression in various solid tumors, including glioblastoma, where it serves as a diagnostic and prognostic biomarker [11]. In the tumor microenvironment, SOX9 expression demonstrates complex correlations with immune cell infiltration, showing negative associations with B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while positively correlating with neutrophils, macrophages, activated mast cells, and naive/activated T cells [4]. These patterns position SOX9 as a master regulator of the immunosuppressive niche.
Experimental Protocols for Evaluating SOX9-Targeting Combinations
In Vivo Modeling of Combination Therapy Resistance
Protocol 1: Murine HNSCC Model for Therapy Evaluation
- Animal Model: C57BL/6 wild-type mice
- Tumor Induction: 4-nitroquinoline 1-oxide (4NQO) in drinking water for 16 weeks, followed by normal water for 8 weeks
- Treatment Groups: Control IgG, anti-PD-1 monotherapy, anti-LAG-3 monotherapy, anti-LAG-3 plus anti-PD-1 combination
- Response Monitoring: Tumor measurement every 4 days; MRI for volumetric analysis; RECIST criteria for classification (resistant defined as >20% growth from baseline)
- Tissue Collection: Tumors harvested for single-cell RNA sequencing, histopathology, and immunofluorescence analysis [16]
This model recapitulates the clinical observation that while combination therapy demonstrates superior efficacy compared to monotherapy (57.1% response rate), a substantial subset (42.9%) develops resistance, enabling mechanistic investigation [16].
Single-Cell Transcriptomic Analysis of Resistance Signatures
Protocol 2: scRNA-seq for Tumor Microenvironment Deconvolution
- Single-Cell Suspension: Pooled tumor tissues from 3 mice per group digested into single-cell suspensions
- Library Preparation: 10X Genomics platform with quality control thresholds
- Sequencing Parameters: Minimum depth of 30,000 reads per cell
- Cell Type Identification: Canonical markers (Epithelial: Krt14, Krt5, Krt6a; Fibroblasts: Col1a1, Col3a1, Apod; Endothelial: Flt1, Pecam1, Eng; Immune: Ptprc, Cd74, Cd3g)
- Malignant Cell Identification: CopyKAT analysis for aneuploid tumor cell subpopulations
- Subcluster Analysis: Identification of resistant (E-resi1, E-resi2) and sensitive (E-sens) epithelial subpopulations [16]
This protocol enables identification of SOX9+ tumor cell enrichment in resistant samples and characterization of the associated immune microenvironment alterations.
Functional Validation of SOX9-Anxa1-Fpr1 Axis
Protocol 3: Neutrophil Apoptosis and Functional Assays
- Neutrophil Isolation: Magnetic-activated cell sorting of Fpr1+ neutrophils from tumor digests
- Co-culture System: SOX9-high vs SOX9-low tumor cells with Fpr1+ neutrophils
- Apoptosis Assessment: Annexin V/PI staining with flow cytometry
- Mitochondrial Function: Mitotracker staining for fission/fusion dynamics; Seahorse analysis for metabolic activity
- Mitophagy Evaluation: BNIP3 immunoblotting; LC3-II/p62 flux analysis
- Transgenic Validation: Sox9 conditional knockout and Fpr1-deficient mouse models [16] [73]
This methodology establishes the causal relationship between SOX9 expression in tumor cells, Anxa1 secretion, Fpr1+ neutrophil apoptosis, and impaired cytotoxic lymphocyte function.
Signaling Pathways in SOX9-Mediated Immunotherapy Resistance
Figure 1: SOX9-Anxa1-Fpr1 Axis in Immunotherapy Resistance. This diagram illustrates the molecular mechanism through which SOX9+ tumor cells mediate resistance to anti-PD-1 and anti-LAG-3 combination therapy by inducing mitochondrial dysfunction and apoptosis in Fpr1+ neutrophils.
Experimental Workflow for Combination Therapy Evaluation
Figure 2: Experimental Workflow for Evaluating SOX9-Targeting Combination Immunotherapies. This workflow outlines the comprehensive approach from model establishment through functional validation for investigating SOX9-mediated resistance mechanisms.
Research Reagent Solutions for SOX9-Immunotherapy Studies
Table 2: Essential Research Reagents for SOX9 and Immunotherapy Investigations
| Reagent/Category | Specific Examples | Research Application | Experimental Notes |
|---|---|---|---|
| Immune Checkpoint Inhibitors | Anti-PD-1 (Nivolumab), Anti-LAG-3 (Relatlimab), Anti-CTLA-4 (Ipilimumab) | In vivo combination therapy studies | Clinical-grade antibodies preferred for translational relevance; validate cross-reactivity for species-specific models [16] [70] |
| SOX9 Detection Tools | SOX9 monoclonal antibodies, SOX9 GFP-reporters, SOX9 conditional knockout models | SOX9 expression tracking and functional manipulation | Validate antibody specificity for IHC, IF, and Western blot; employ inducible systems for temporal control [11] [16] |
| Neutrophil Reagents | Anti-Fpr1 antibodies, ANXA1 recombinant protein, Fpr1-deficient mice | Neutrophil isolation and functional studies | Use magnetic-activated cell sorting for Fpr1+ neutrophil isolation; validate purity with flow cytometry [16] [73] |
| Mitochondrial Function Assays | MitoTracker dyes, Seahorse XF Analyzer, BNIP3 antibodies | Metabolic and mitophagy assessment | Optimize dye concentrations for tumor-infiltrating neutrophils; include FCCP controls for mitochondrial stress tests [16] |
| scRNA-seq Platforms | 10X Genomics, BD Rhapsody, Smart-seq2 | Tumor microenvironment deconvolution | Target 20,000-50,000 cells per condition; include hashtag oligonucleotides for sample multiplexing [16] |
| Cell Line Models | Patient-derived organoids, Sox9-overexpressing lines, CRISPR-modified systems | Mechanistic studies in controlled systems | Establish multiple clones for genetic modifications; validate Sox9 manipulation by Western blot [11] [4] |
Comparative Efficacy Assessment Framework
Quantitative Metrics for Regimen Evaluation
Table 3: Standardized Assessment Parameters for Combination Immunotherapy
| Evaluation Domain | Key Parameters | Measurement Techniques | SOX9-Specific Correlates |
|---|---|---|---|
| Tumor Response | Objective Response Rate (ORR), Progression-Free Survival (PFS), Overall Survival (OS) | RECIST criteria, Kaplan-Meier analysis, tumor volumetrics | SOX9+ tumor cell frequency in post-treatment biopsies [16] |
| Immune Contexture | Immune cell infiltration density, spatial distribution, subset composition | scRNA-seq, multiplex immunofluorescence, flow cytometry | Correlation with Fpr1+ neutrophil abundance and CD8+ T cell exhaustion markers [4] [16] |
| Microenvironment Metrics | Cytokine/chemokine profile, checkpoint expression, metabolic landscape | Cytometric bead arrays, Nanostring, spatial transcriptomics | ANXA1-FPR1 axis activation; BNIP3 expression levels [16] |
| Resistance Signatures | Transcriptomic programs, pathway activation, cellular communities | Gene set enrichment analysis, trajectory inference | SOX9 regulatory network activity; mitochondrial dysfunction scores [11] [16] |
Integration of SOX9 Biomarker Assessment in Clinical Trial Design
The integration of SOX9 biomarker evaluation within combination immunotherapy trials requires standardized pre-analytical and analytical procedures. Recommended methodologies include:
- SOX9 IHC Scoring System: Semi-quantitative assessment of SOX9 expression in tumor biopsies using standardized scoring criteria (0-3+ based on intensity and distribution)
- Liquid Biopsy Approaches: Development of SOX9-related signatures in circulating tumor cells or extracellular vesicles for longitudinal monitoring
- Multiplex Spatial Profiling: Simultaneous detection of SOX9, ANXA1, and immune cell markers in tissue sections to characterize cellular interactions
- Computational Pipeline: Integrated bioinformatic analysis of SOX9 co-expression networks and their association with treatment response outcomes [11] [16]
This comprehensive framework enables systematic head-to-head comparison of emerging SOX9-targeting strategies alongside established combination immunotherapies, facilitating the identification of optimal therapeutic approaches for specific patient subsets defined by SOX9 pathway activation.
Clinical Trial Designs and Endpoints for Evaluating Combination Therapy
The emergence of combination immunotherapy represents a paradigm shift in oncology, aimed at overcoming the limitations of monotherapies. Immune checkpoint blockade (ICB), particularly targeting the PD-1/PD-L1 axis, has demonstrated remarkable efficacy across multiple malignancies, but response rates remain limited, and both intrinsic and acquired resistance present significant clinical challenges [74] [75]. Recent investigations into the transcription factor SOX9 have revealed its crucial role in mediating resistance to immunotherapy, positioning it as a promising therapeutic target for combination strategies [16] [4]. In head and neck squamous cell carcinoma (HNSCC) models, SOX9+ tumor cells drive resistance to combined anti-LAG-3 and anti-PD-1 therapy by regulating annexin A1 (Anxa1) expression, which mediates apoptosis of Fpr1+ neutrophils and impairs cytotoxic T cell infiltration within the tumor microenvironment [16]. This mechanistic understanding provides a strong biological foundation for combining SOX9-targeting agents with established PD-1/PD-L1 inhibitors.
The design of clinical trials evaluating such novel combinations requires careful consideration of unique challenges, including patient selection, endpoint determination, and appropriate biomarker integration. This document outlines comprehensive application notes and protocols for the clinical development of SOX9-targeted therapies in combination with PD-1/PD-L1 blockade, providing a structured framework for researchers and drug development professionals.
Key Clinical Trial Designs for Combination Therapy
Phase I Trial Designs: Dose Finding and Safety
Phase I trials for SOX9/PD-1/PD-L1 combination therapy must address the challenge of defining recommended Phase II doses (RP2Ds) for both agents, whether the SOX9-targeting agent is a small molecule inhibitor, oligonucleotide, or other modality.
Table 1: Phase I Trial Design Options for SOX9/PD-1/PD-L1 Combinations
| Design Type | Key Features | Advantages | Considerations for SOX9 Combinations |
|---|---|---|---|
| 3+3 Design | Traditional cohort escalation; defines maximum tolerated dose (MTD) | Simple, widely understood, conservative safety profile | May be suboptimal for targeted agents with primarily immunological rather than cytotoxic effects |
| Bayesian Logistic Regression Model (BLRM) | Model-based dose escalation using prior knowledge | More efficient dose finding, incorporates biomarker data | Suitable when SOX9 inhibition may have dose-dependent immune effects beyond toxicity |
| Time-to-Event Continual Reassessment Method (TITE-CRM) | Accounts for late-onset toxicities | Accommodates longer observation periods for immune-related adverse events (irAEs) | Relevant given potential for overlapping irAEs from both PD-1/PD-L1 and SOX9-targeted agents |
| Modified Toxicity Probability Interval (mTPI) | Predefined toxicity intervals for dose escalation decisions | Balanced approach between algorithmic and model-based methods | Allows incorporation of pharmacokinetic/pharmacodynamic (PK/PD) data for SOX9-targeted agents |
Protocol Guidance: The Phase I protocol should include intensive biomarker correlative studies, including serial tumor biopsies for SOX9 expression analysis by immunohistochemistry (IHC) and assessment of downstream effects on the Anxa1-Fpr1 axis. Dose-limiting toxicity (DLT) observation periods should extend to at least 6 weeks to capture potential overlapping or synergistic immune-related adverse events.
Phase II Trial Designs: Preliminary Efficacy and Biomarker Validation
Phase II trials should incorporate biomarker-stratified designs to assess whether SOX9 expression levels predict response to the combination therapy.
Table 2: Phase II Endpoints for SOX9/PD-1/PD-L1 Combination Trials
| Endpoint Category | Specific Measures | Assessment Timing | Considerations for SOX9 Context |
|---|---|---|---|
| Efficacy Endpoints | Objective Response Rate (ORR) | Every 6-8 weeks | Compare with historical anti-PD-1/PD-L1 monotherapy rates |
| Progression-Free Survival (PFS) | From randomization to progression | Primary endpoint for randomized Phase II trials | |
| Depth of Response (DpR) | Maximum tumor shrinkage | May reveal enhanced activity beyond response rates | |
| Immunological Endpoints | SOX9 expression modulation | Baseline, C2D1, progression | Correlate SOX9 reduction with clinical outcomes |
| Tumor immune microenvironment changes | Baseline and on-treatment biopsies | Assess neutrophil infiltration, CD8+ T cell density | |
| Exploratory Endpoints | Circulating biomarkers | Multiple timepoints | Soluble Anxa1, neutrophil subsets, cytokine profiles |
Adaptive Design Considerations: A biomarker-adaptive strategy is recommended, where initial enrollment may be unrestricted, with potential for subsequent enrichment in populations demonstrating SOX9 pathway activation. This approach balances the need for broad clinical evaluation with efficient development in potentially responsive populations.
Signaling Pathways and Resistance Mechanisms
The mechanistic basis for combining SOX9-targeted therapy with PD-1/PD-L1 blockade lies in the role of SOX9 in mediating an immunosuppressive tumor microenvironment. Recent research has elucidated a key signaling axis through which SOX9 promotes resistance to immunotherapy.
Figure 1: SOX9-Mediated Resistance Pathway to Combination Immunotherapy. SOX9+ tumor cells drive resistance to anti-LAG-3 plus anti-PD-1 therapy by directly regulating Anxa1 expression, which binds to Fpr1 on neutrophils. This interaction promotes mitochondrial fission and inhibits mitophagy by downregulating Bnip3 expression, ultimately leading to neutrophil apoptosis and reduced accumulation in tumors. The decrease in Fpr1+ neutrophils impairs cytotoxic CD8+ T cell and γδT cell infiltration and function, resulting in therapy resistance [16].
This pathway illustrates how SOX9 inhibition could potentially reverse resistance to PD-1/PD-L1 blockade by preserving neutrophil populations that support T cell-mediated antitumor immunity.
Experimental Protocols for Preclinical and Clinical Evaluation
Protocol 1: Assessment of SOX9 Expression and Pathway Modulation
Purpose: To evaluate SOX9 expression levels and downstream pathway activity in tumor samples from patients receiving SOX9-targeted therapy in combination with PD-1/PD-L1 inhibitors.
Materials:
- Formalin-fixed paraffin-embedded (FFPE) tumor tissue sections (baseline and on-treatment)
- SOX9 primary antibody (e.g., Rabbit monoclonal anti-SOX9)
- ANXA1 primary antibody for downstream pathway assessment
- IHC detection kit with appropriate chromogen
- RNA extraction kit for transcriptional analysis
- qPCR reagents for SOX9 target gene expression
Procedure:
- Perform IHC staining for SOX9 on baseline tumor sections using standardized protocols
- Score SOX9 expression using H-scoring system (0-300) incorporating intensity and percentage of positive tumor cells
- Categorize samples as SOX9-high (H-score ≥100) or SOX9-low (H-score <100)
- On C2D1 treatment biopsies, repeat SOX9 IHC and additionally stain for ANXA1
- Isolve RNA from macro-dissected tumor areas for qPCR analysis of SOX9-regulated genes
- Correlate SOX9 modulation with changes in immune cell infiltration using multiplex IHC
Analysis: Compare pre- and post-treatment SOX9 H-scores to assess target engagement. Evaluate correlation between SOX9 reduction and changes in tumor immune microenvironment.
Protocol 2: Evaluation of Tumor Immune Microenvironment
Purpose: To comprehensively characterize immune cell populations and functional states in tumors treated with SOX9/PD-1/PD-L1 combination therapy.
Materials:
- Fresh tumor tissue for single-cell RNA sequencing (scRNA-seq)
- Multiplex IHC panel antibodies (CD8, CD4, CD68, neutrophil elastase, PD-L1)
- Flow cytometry antibodies for immune profiling (CD45, CD3, CD8, CD4, CD66b, PD-1)
- Tissue digestion kit for single-cell suspension preparation
- scRNA-seq library preparation kit
Procedure:
- Process fresh tumor tissue within 1 hour of collection using gentleMACS dissociator
- Divide single-cell suspension for parallel scRNA-seq and flow cytometric analysis
- For scRNA-seq: Capture 5,000-10,000 cells using 10X Genomics platform
- Perform library preparation and sequencing to depth of 50,000 reads per cell
- For flow cytometry: Stain cells with optimized antibody panel and acquire on 3-laser cytometer
- For multiplex IHC: Stain FFPE sections with optimized antibody panel and perform multispectral imaging
Analysis:
- Process scRNA-seq data using CellRanger and Seurat pipelines
- Identify cell populations by canonical marker expression
- Perform differential expression analysis between treatment timepoints
- Quantify immune cell densities and spatial relationships in multiplex IHC
- Integrate scRNA-seq and flow cytometry data for validation
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for SOX9/PD-1 Combination Studies
| Reagent Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| SOX9-Targeting Reagents | SOX9 small molecule inhibitors; SOX9 siRNA/shRNA | Target validation; mechanistic studies | Assess specificity and off-target effects |
| Immune Checkpoint Inhibitors | Anti-PD-1 (nivolumab, pembrolizumab); Anti-PD-L1 (atezolizumab, durvalumab) | Combination therapy component | Species-specific versions for preclinical models |
| Animal Models | 4NQO-induced HNSCC mouse model; Genetically engineered SOX9 models | Preclinical efficacy testing | 4NQO model recapitulates human HNSCC immunotherapy responses [16] |
| Antibodies for Analysis | Anti-SOX9 (IHC); Anti-ANXA1; Anti-CD8; Anti-FPR1; Neutrophil markers | Biomarker assessment; mechanism investigation | Validate cross-reactivity for species used |
| Single-Cell Analysis Platforms | 10X Genomics; Cite-seq; Cell hashing technologies | Tumor microenvironment characterization | Enable analysis of rare cell populations |
| Transgenic Models | Sox9-floxed mice; Fpr1 knockout models | Mechanistic validation | Cell-type specific knockout to dissect cell-autonomous effects |
Biomarker Strategy and Patient Selection
The successful clinical development of SOX9/PD-1/PD-L1 combination therapy requires a comprehensive biomarker strategy to identify patients most likely to benefit.
Potential Predictive Biomarkers
- SOX9 Tumor Expression: Baseline SOX9 protein and mRNA expression should be evaluated as a potential enrichment biomarker, particularly given the association between SOX9 enrichment and therapy resistance in preclinical models [16].
- ANXA1-FPR1 Axis Components: Assessment of ANXA1 tumor expression and FPR1+ neutrophil infiltration may provide insights into pathway activity.
- Peripheral Immunological Biomarkers: Changes in circulating neutrophil subsets and plasma ANXA1 levels may serve as pharmacodynamic markers of target engagement.
- Traditional Immunotherapy Biomarkers: PD-L1 expression, tumor mutational burden (TMB), and microsatellite instability (MSI) status should continue to be assessed, as their predictive value may be modulated by SOX9 inhibition [75].
Adaptive Biomarker Strategy
Given the complexity of the SOX9 signaling network and its context-dependent roles in different cancer types [4], an adaptive biomarker strategy is recommended. Initial trials should include broad biomarker exploration across multiple potential resistance pathways, with subsequent refinement of biomarker hypotheses based on emerging clinical data.
The development of SOX9-targeted therapies in combination with PD-1/PD-L1 blockade represents a promising approach to overcome immunotherapy resistance. Successful clinical evaluation requires sophisticated trial designs that incorporate robust biomarker strategies and comprehensive mechanistic assessments. The protocols and frameworks outlined herein provide a roadmap for researchers pursuing this innovative therapeutic strategy, with the ultimate goal of expanding the benefit of cancer immunotherapy to more patients.
Conclusion
Targeting SOX9 presents a viable strategy to overcome primary and acquired resistance to PD-1/PD-L1 blockade by remodeling the immunosuppressive tumor microenvironment. The convergence of evidence across multiple cancer types underscores SOX9's role in regulating key resistance pathways, including neutrophil apoptosis via the ANXA1-FPR1 axis and suppression of cytotoxic T-cell function. Future research must prioritize the development of clinical-grade SOX9 inhibitors, validate predictive biomarkers in prospective trials, and explore rational combinations with emerging immunomodulators. Successfully integrating SOX9 targeting into the immunotherapy arsenal requires a multidisciplinary approach, leveraging advanced single-cell technologies and synthetic biology to create next-generation precision immunotherapies that achieve durable tumor control.
References
- 1. SOX9 in organogenesis: shared and unique transcriptional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9482574/]
- 2. The versatile functions of Sox9 in development, stem cells, ... [https://www.sciencedirect.com/science/article/pii/S2352304214000282]
- 3. SOX9: a key transcriptional regulator in organ fibrosis [https://pubmed.ncbi.nlm.nih.gov/39974732/]
- 4. SOX9: a novel janus-faced regulator in immunity and its ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1700812/full]
- 5. SOX9: a key transcriptional regulator in organ fibrosis [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1507282/full]
- 6. Sox9 regulates alternative splicing and pancreatic beta cell ... [https://www.nature.com/articles/s41467-023-44384-8]
- 7. Transcription Factor Sox9 - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/transcription-factor-sox9]
- 8. SOX9 Protein in Pancreatic Cancer Regulates Multiple ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9312990/]
- 9. SOX9 Stem-Cell Factor: Clinical and Functional Relevance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6463569/]
- 10. SOX9 is a critical regulator of TSPAN8-mediated ... [https://www.nature.com/articles/s41388-021-01864-9]
- 11. High expression of SOX9 is a diagnostic and prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277172/]
- 12. Deciphering of SOX9 Functions in Pancreatic Cancer Cells [https://www.mdpi.com/1422-0067/26/6/2652]
- 13. Possible novel non-invasive biomarker for inflammation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8204699/]
- 14. Blockade of LIF and PD-L1 Enhances Chemotherapy in ... [https://www.mdpi.com/2072-6694/17/2/204]
- 15. Role of the SOX family in cancer immune evasion [https://pmc.ncbi.nlm.nih.gov/articles/PMC11789896/]
- 16. Resistance to anti-LAG-3 plus anti-PD-1 therapy in head ... [https://www.nature.com/articles/s41467-025-59050-4]
- 17. Targeting SOX9: designing a novel vaccine against triple ... [https://www.nature.com/articles/s41598-025-25499-y]
- 18. Boosting one protein helps the brain protect itself from ... [http://www.sciencedaily.com/releases/2025/11/251123085550.htm]
- 19. Comprehensive analysis, immune, and cordycepin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10067558/]
- 20. High expression of SOX9 is a diagnostic and prognostic ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1531937/full]
- 21. Diagnostic and Prognostic Significances of SOX9 in ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2021.708735/full]
- 22. Targeting SOX9 in Colorectal Cancer Promotes ... [https://innovations.dana-farber.org/technology/targeting-sox9-in-colorectal-cancer-promotes-differentiation-and-cancer-cell-death/]
- 23. SOX9 drives KRAS-induced lung adenocarcinoma progression and suppresses anti-tumor immunity - PubMed [https://pubmed.ncbi.nlm.nih.gov/37258742/]
- 24. A SOX9-B7x axis safeguards dedifferentiated tumor cells from immune surveillance to drive breast cancer progression - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S1534580723005518]
- 25. Boosting this protein helps brain protect itself from Alzheimer's [https://desitalkchicago.com/boosting-this-protein-helps-brain-protect-itself-from-alzheimers-study/]
- 26. SOX9 is an atypical intestinal tumor suppressor controlling the oncogenic Wnt/ß-catenin signaling - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5347687/]
- 27. SOX9: an important factor in regulating breast cancer [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-02730-0]
- 28. Super-enhancer inhibitors THZ2 and JQ1 reverse ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12366492/]
- 29. USP28 promotes PARP inhibitor resistance by enhancing ... [https://www.nature.com/articles/s41419-025-07647-4]
- 30. Resistance to anti-LAG-3 plus anti-PD-1 therapy in head ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12037843/]
- 31. PMC Search Update - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11773883/]
- 32. Role of Sox9 in BPD and its effects on the Wnt/β-catenin ... [https://www.nature.com/articles/s41420-023-01795-2]
- 33. A SOX9-B7x axis safeguards dedifferentiated tumor cells from ... [https://pubmed.ncbi.nlm.nih.gov/37963469/]
- 34. A SOX9-B7x axis safeguards dedifferentiated tumor cells from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10842074/]
- 35. B7H4 Role in Solid Cancers: A Review of the Literature [https://www.mdpi.com/2072-6694/16/14/2519]
- 36. SOX on tumors, a comfort or a constraint? [https://www.nature.com/articles/s41420-024-01834-6]
- 37. Resistance to anti-LAG-3 plus anti- PD - 1 in head and neck... therapy [https://www.nature.com/articles/s41467-025-59050-4?error=cookies_not_supported&code=eb6c00f1-f24e-433a-b8e5-eb2de3125c88]
- 38. Mechanism of regulatory target selection by the SOX high- ... [https://pubmed.ncbi.nlm.nih.gov/9858536/]
- 39. Synthetic receptors for logic gated T cell recognition and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8901444/]
- 40. Overcoming Genetically Based Resistance to... Mechanisms [https://pubmed.ncbi.nlm.nih.gov/32467343/]
- 41. Human CAR cells with cell-intrinsic T - PD checkpoint 1 ... blockade resist [https://www.jci.org/articles/view/83092]
- 42. Transcription Factor Drives Chemotherapy Resistance in ... [https://news.feinberg.northwestern.edu/2025/10/30/transcription-factor-drives-chemotherapy-resistance-in-ovarian-cancer/]
- 43. - PD (B7-H1) and L - 1 pathway PD for cancer therapy... 1 blockade [https://pubmed.ncbi.nlm.nih.gov/26936508/]
- 44. Frontiers | Exosomal PD - L detection in cancer predictive 1 ... biomarker [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1603855/full]
- 45. Integrated peripheral blood multi - omics profiling identifies immune... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06770-2]
- 46. Multi-omics strategies for biomarker discovery and application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12638490/]
- 47. MULGONET: An interpretable neural network framework to ... [https://www.sciencedirect.com/science/article/pii/S2667325825000147]
- 48. Emerging Technologies in Biomarker Discovery You ... [https://blog.crownbio.com/emerging-technologies-in-biomarker-discovery-you-should-know-about]
- 49. Mechanisms of Resistance and Strategies to Combat Resistance in PD-(L)1 Blockade | MDPI [https://www.mdpi.com/2673-5601/2/4/41]
- 50. SOX9 indirectly regulates CEACAM1 expression and ... [https://www.oncotarget.com/article/7379/text/]
- 51. Mechanisms, combination therapy, and biomarkers in cancer immunotherapy resistance | Cell Communication and Signaling | Full Text [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-024-01711-w]
- 52. Improving synergistic drug combination prediction with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12310685/]
- 53. A highly annotated drug combination resource for ... [https://www.nature.com/articles/s41597-025-05630-4]
- 54. MD-Syn: synergistic drug combination prediction based on ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1564339/full]
- 55. Synthetic biology approaches for improving the specificity ... [https://www.nature.com/articles/s41423-024-01153-x]
- 56. Mechanisms of Resistance to PD-1 and PD-L1 blockade - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5785093/]
- 57. Resistance mechanisms to immune checkpoint inhibitors [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02212-7]
- 58. Immune evasion in cancer: mechanisms and cutting-edge ... [https://www.nature.com/articles/s41392-025-02280-1]
- 59. Applications of single-cell technologies in drug discovery for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11338156/]
- 60. Single-cell RNA sequencing reveals enhanced antitumor ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-023-01184-3]
- 61. Integrating bulk, single-cell, and spatial transcriptomics to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12003664/]
- 62. Patient-derived xenograft models: Current status, challenges ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12179623/]
- 63. Patient-derived xenograft models in cancer therapy [https://www.nature.com/articles/s41392-023-01419-2]
- 64. High SOX9 Maintains Glioma Stem Cell Activity through a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9104987/]
- 65. SOX9-PDK1 axis is essential for glioma stem cell self ... [https://www.oncotarget.com/article/22773/text/]
- 66. Expression and Potential Prognostic Value of SOX9, MCL- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8863590/]
- 67. The local and circulating SOX9 as a potential biomarker for ... [https://pubmed.ncbi.nlm.nih.gov/32551218/]
- 68. Potential Biomarkers for IDH-Mutant and IDH-Wild-Type ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11989654/]
- 69. An externally validated machine learning model for predicting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11630777/]
- 70. Combination of PD-1/PD-L1 and CTLA-4 inhibitors in the ... [https://pubmed.ncbi.nlm.nih.gov/41159031/]
- 71. Two Posters at ESMO Congress 2025 Highlight Immutep's ... [https://www.immutep.com/two-posters-at-esmo-congress-2025-highlight-immuteps-focus-on-changing-treatment-landscape-in-first-line-non-small-cell-lung-cancer/]
- 72. Comparison of efficacy and safety of PD-1/PD-L1 ... [https://pubmed.ncbi.nlm.nih.gov/38625495/]
- 73. Resistance to anti-LAG-3 plus anti-PD-1 therapy in head ... [https://pubmed.ncbi.nlm.nih.gov/40295483/]
- 74. Combination of PD-1/PD-L1 and CTLA-4 inhibitors in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12554671/]
- 75. Biomarkers for predicting efficacy of PD-1/PD-L1 inhibitors [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-018-0864-3]