Targeting SOX9 to Overcome Therapy Resistance in Cancer: Mechanisms, Strategies, and Clinical Outlook
The transcription factor SOX9 has emerged as a pivotal driver of therapy resistance across diverse cancer types, including gastric, ovarian, breast, and colorectal cancers.
Targeting SOX9 to Overcome Therapy Resistance in Cancer: Mechanisms, Strategies, and Clinical Outlook
Abstract
The transcription factor SOX9 has emerged as a pivotal driver of therapy resistance across diverse cancer types, including gastric, ovarian, breast, and colorectal cancers. This article synthesizes current research elucidating the molecular mechanisms by which SOX9 promotes chemoresistance, radioresistance, and resistance to targeted therapies like PARP inhibitors. It explores SOX9's role in maintaining cancer stemness, regulating DNA damage repair, and modulating the tumor immune microenvironment. For researchers and drug development professionals, the content provides a comprehensive overview of cutting-edge therapeutic strategies, from siRNA-loaded nanoparticles and small molecule inhibitors to biomarker development, offering a roadmap for designing clinical interventions to counteract SOX9-mediated treatment failure.
Unraveling SOX9: Its Central Role in Driving Cancer Therapy Resistance
SOX9 as a Master Regulator of Cancer Stemness and Chemoresistance
FAQs: Core Concepts and Mechanisms
What is the primary role of SOX9 in cancer development and therapy resistance? SOX9 is a transcription factor that acts as a master regulator of cancer stemness, directly driving chemotherapy resistance. It reprograms the transcriptional state of naive cancer cells into a stem-like state, enabling them to survive treatment. SOX9 is not merely a marker but is functionally sufficient to induce chemoresistance; its epigenetic upregulation alone can trigger significant resistance to platinum-based chemotherapy and induce the formation of a stem-like subpopulation in various cancers, including high-grade serous ovarian cancer (HGSOC) and gastric cancer [1] [2] [3].
In which cancer types has SOX9-mediated chemoresistance been most strongly documented? Evidence for SOX9-mediated chemoresistance spans multiple solid tumors. Key findings are summarized in the table below.
| Cancer Type | Key Findings on SOX9's Role in Chemoresistance |
|---|---|
| High-Grade Serous Ovarian Cancer (HGSOC) | SOX9 is epigenetically upregulated by platinum chemotherapy. It drives a stem-like transcriptional state, and its high expression correlates with shorter overall survival [1] [2]. |
| Gastric Cancer | SOX9 is part of the CDK1-SOX9-BCL-xL signaling axis. It transcriptionally upregulates the anti-apoptotic protein BCL-xL, enabling evasion of cisplatin-induced cell death [3]. |
| Osteosarcoma & Bone Tumors | SOX9 is overexpressed in high-grade, metastatic, recurrent tumors and those with poor response to therapy. Its expression is further elevated in patients receiving chemotherapy [4] [5]. |
| Lung Adenocarcinoma | SOX9 is upregulated in tumor tissues and promotes cell proliferation, migration, and invasion, which are key processes in cancer aggressiveness and treatment failure [6]. |
How does SOX9 contribute to the cancer stem cell (CSC) phenotype? SOX9 promotes the CSC phenotype through several interconnected mechanisms: it increases transcriptional divergence, a metric of cellular plasticity and stemness; it functions as a master regulator to maintain cells in an undifferentiated state, supporting self-renewal; and it regulates key signaling pathways like Wnt/β-catenin and ERBB, which are critical for CSC maintenance and tumorigenesis [1] [5] [7].
What is the relationship between SOX9 expression and patient prognosis? High SOX9 expression is consistently associated with poorer clinical outcomes. In HGSOC, patients in the top quartile of SOX9 expression have a significantly shorter overall survival probability. In osteosarcoma and other bone tumors, SOX9 overexpression is correlated with high tumor grade, metastasis, recurrence, and poor response to therapy [1] [5].
Troubleshooting Common Experimental Challenges
Challenge 1: How can I effectively modulate SOX9 expression in vitro? Effective modulation of SOX9 in cell line models requires specific tools and validation. Below is a table of common research reagents.
| Research Reagent / Tool | Function and Application in SOX9 Research |
|---|---|
| CRISPR/Cas9 with SOX9-targeting sgRNA | Used for stable gene knockout to study SOX9 loss-of-function and its impact on platinum sensitivity [1]. |
| Full-length human SOX9 plasmid (e.g., pCMV-Tag2V) | Used for ectopic overexpression to investigate SOX9's sufficiency in driving proliferation, migration, invasion, and chemoresistance [6] [3]. |
| SOX9-targeting siRNA/SHRNA pools | Used for transient gene knockdown to validate phenotypes observed in knockout models and to probe downstream mechanisms [6] [3]. |
| Anti-SOX9 antibody (for IHC/Western Blot) | Essential for validating SOX9 protein expression and localization in tissue samples (IHC) and cell lysates (Western Blot) [6]. |
| Pharmacological CDK1 inhibitor (e.g., Dinaciclib) | An indirect method to suppress SOX9 protein levels and transcriptional activity by disrupting the CDK1-SOX9 axis [3]. |
Experimental Protocol: Validating SOX9 Knockdown/Knockout Efficiency
- Transfection: Use an appropriate transfection reagent (e.g., Lipofectamine 2000 for plasmids, DharmaFECT1 for siRNA) according to the manufacturer's instructions [6] [3].
- Validation Timeline: Harvest cell lysates 48-72 hours post-transfection for protein and RNA analysis.
- qRT-PCR Analysis:
- Isolate total RNA using TRIzol reagent.
- Synthesize cDNA from 1 µg of total RNA.
- Perform qRT-PCR using SYBR Green and primers specific to SOX9.
- Calculate transcript levels using the 2-ΔΔCt method, normalizing to a housekeeping gene (e.g., HPRT or β-actin) [3].
- Western Blot Analysis:
Challenge 2: How do I functionally validate the role of SOX9 in chemoresistance? Experimental Protocol: Cisplatin Resensitization Assay
- Establish Resistant Models: Generate cisplatin-resistant cell lines by chronic, low-dose exposure to cisplatin. SOX9 upregulation is a hallmark of this process [3].
- Modulate SOX9: Knock down SOX9 in the resistant lines using siRNA or CRISPR/Cas9.
- Treat and Assess Viability: Treat parental and modified resistant cells with a range of cisplatin concentrations for 72 hours.
- Cell Viability Assay: Use the MTT assay:
- Seed cells in a 96-well plate.
- After cisplatin incubation, add 20 µl of MTT (5 mg/ml) to each well.
- Incubate for 4 hours at 37°C.
- Dissolve formazan crystals in DMSO and measure absorbance at 490-570 nm [6].
- Analysis: Calculate IC50 values. Successful SOX9 knockdown should significantly lower the IC50 in resistant cells, indicating resensitization.
Challenge 3: How can I investigate the SOX9-mediated in vivo chemoresistance? Experimental Protocol: Patient-Derived Xenograft (PDX) Model
- Implantation: Subcutaneously implant patient-derived gastric tumoroids or tumor fragments into immunodeficient mice (e.g., B6.Cg-Prkdcscid/SzJ) [3].
- Treatment Groups: Once tumors reach 100-150 mm³, randomize mice into groups:
- Vehicle control
- Cisplatin monotherapy (e.g., 1 mg/kg, i.p., weekly)
- CDK1 inhibitor (e.g., Dinaciclib, 20 mg/kg, i.p., 3 times/week) to target the SOX9 axis
- Combination therapy
- Monitoring: Measure tumor volume regularly. The combination therapy should synergistically reduce tumor volume compared to monotheracies [3].
- Endpoint Analysis: Harvest tumors for IHC or Western blot analysis to confirm downregulation of SOX9 and its target, BCL-xL, in the combination group.
Key Signaling Pathways and Mechanisms
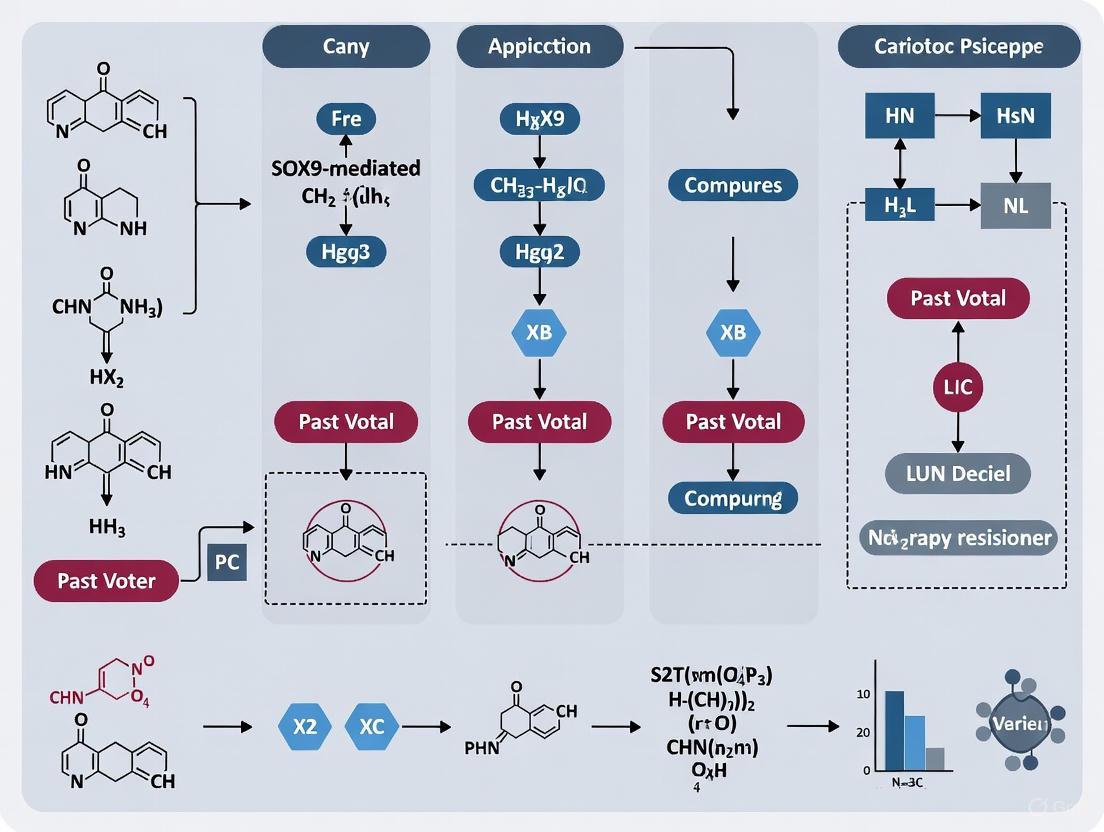
The CDK1-SOX9-BCL-xL axis is a critical pathway mediating chemoresistance in gastric cancer, and understanding its components is essential for troubleshooting. The following diagram illustrates this signaling cascade and the experimental strategies to target it.
This diagram shows how CDK1 stabilizes SOX9 via epigenetic silencing of miR-145, and how SOX9 then upregulates BCL-xL to promote chemoresistance. The dashed lines indicate points for experimental intervention.
Key Molecular Interactions:
- CDK1 Epigenetically Regulates SOX9: CDK1 phosphorylates and activates DNMT1, which drives methylation-dependent silencing of the microRNA miR-145. Since miR-145 normally represses SOX9, its silencing leads to SOX9 upregulation [3].
- SOX9 Transcriptionally Activates BCL-xL: SOX9 directly binds to the promoter of BCL-xL, an anti-apoptotic protein, increasing its expression and allowing cancer cells to evade cisplatin-induced apoptosis [3].
- SOX9 Drives Transcriptional Reprogramming: In ovarian cancer, SOX9 expression is sufficient to increase transcriptional divergence, reprogramming naive cells into a stem-like, drug-tolerant state [1].
The Scientist's Toolkit: Research Reagent Solutions
A curated list of essential materials for studying SOX9 is provided in the table below.
| Research Reagent / Tool | Function and Application in SOX9 Research |
|---|---|
| CRISPR/Cas9 with SOX9-targeting sgRNA | Used for stable gene knockout to study SOX9 loss-of-function and its impact on platinum sensitivity [1]. |
| Full-length human SOX9 plasmid (e.g., pCMV-Tag2V) | Used for ectopic overexpression to investigate SOX9's sufficiency in driving proliferation, migration, invasion, and chemoresistance [6] [3]. |
| SOX9-targeting siRNA/SHRNA pools | Used for transient gene knockdown to validate phenotypes observed in knockout models and to probe downstream mechanisms [6] [3]. |
| Anti-SOX9 antibody (for IHC/Western Blot) | Essential for validating SOX9 protein expression and localization in tissue samples (IHC) and cell lysates (Western Blot) [6]. |
| Pharmacological CDK1 inhibitor (e.g., Dinaciclib) | An indirect method to suppress SOX9 protein levels and transcriptional activity by disrupting the CDK1-SOX9 axis [3]. |
A critical signaling axis comprising CDK1, DNMT1, miR-145, and SOX9 has been identified as a key mediator of chemoresistance in gastric cancer (GC) [3]. This pathway represents an epigenetic control mechanism where the cell cycle regulator CDK1 stabilizes the transcription factor SOX9 through microRNA interference, enabling cancer cells to evade cisplatin-induced apoptosis [3] [8]. Within the broader context of overcoming SOX9-mediated therapy resistance, understanding and targeting this axis offers promising therapeutic strategies to re-sensitize resistant tumors to conventional chemotherapy [3].
Pathway Mechanism & Key Experimental Data
Core Pathway Mechanism
The CDK1-DNMT1-miR-145-SOX9 axis functions through a sequential epigenetic mechanism:
- CDK1 Activation: Cyclin-dependent kinase 1 (CDK1), typically overexpressed in gastric cancer, phosphorylates and activates DNA methyltransferase 1 (DNMT1) [3].
- Epigenetic Silencing: Activated DNMT1 drives methylation-dependent silencing of the miR-145 gene, a tumor suppressor microRNA [3] [8].
- SOX9 Derepression: Silencing of miR-145 relieves its post-transcriptional repression of SOX9 mRNA, leading to increased SOX9 protein levels [3].
- Anti-Apoptotic Activation: Elevated SOX9 transcriptionally upregulates the anti-apoptotic protein BCL-xL, directly mediating cisplatin resistance [3].
This pathway creates a coherent signaling cascade from cell cycle regulation to epigenetic modification and ultimately to transcriptional control of apoptosis effectors.
Key Experimental Findings
Table 1: Quantitative Experimental Findings from Key Studies
| Experimental Model | Key Finding | Quantitative Result | Significance/Outcome |
|---|---|---|---|
| Cisplatin-resistant GC cell lines [3] | Concurrent upregulation of CDK1 & SOX9 | Significant increase in protein levels | Establishes correlation in resistant phenotypes |
| CDK1 inhibition (Genetic & Pharmacological) [3] | Suppression of SOX9 levels & activity | Reduced SOX9 protein and transcriptional activity | Validates causal relationship |
| CDK1 inhibition with Dinaciclib in PDX models [3] | Tumor volume reduction & survival extension | Synergistic effect with cisplatin | Highlights therapeutic potential |
| miR-145 expression after 5-Aza treatment [8] | Upregulation of miR-145 | Increased expression | Confirms epigenetic silencing mechanism |
| SOX9 transcriptional target identification [3] | BCL-xL as direct SOX9 target | Increased BCL-xL expression | Links pathway to apoptosis evasion |
Essential Protocols for Pathway Investigation
Establishing Cisplatin-Resistant Cell Models
Purpose: Generate reliable in vitro models to study the CDK1-DNMT1-miR-145-SOX9 axis in chemoresistance [3].
Protocol:
- Cell Culture: Maintain gastric cancer cell lines (e.g., AGS, MKN28, MKN45) in appropriate media (F12 for AGS; RPMI 1640 for MKN28/45) supplemented with 10% FBS and 1% penicillin/streptomycin at 37°C with 5% CO₂ [3].
- Authentication: Authenticate cell lines using STR profiling and regularly test for mycoplasma contamination [3].
- Resistance Induction: Expose parental cells to progressively increasing concentrations of cisplatin over multiple passages.
- Validation: Confirm resistant phenotype through viability assays (e.g., MTT, CellTiter-Glo) comparing IC₅₀ values between parental and resistant lines. Validate upregulated CDK1 and SOX9 expression via western blotting [3].
Genetic Manipulation of Axis Components
Purpose: Functionally validate roles of individual axis components through targeted knockdown.
Knockdown Protocol (siRNA):
- Design: Use ON-TARGETplus human siRNA constructs for CDK1 (L-003224-00-0005) and SOX9 (L-021507-00-0005) with non-targeting siRNA (J-005834-05-0005) as control [3].
- Transfection: Utilize DharmaFECT1 transfection reagent following manufacturer's instructions [3].
- Timeline: Assay knockdown efficiency at 48-72 hours post-transfection via qPCR and western blot.
- Functional Assays: Subject knockdown cells to cisplatin treatment and assess viability, apoptosis (e.g., caspase activation, Annexin V staining), and colony formation.
Pharmacological Inhibition of CDK1
Purpose: Evaluate therapeutic potential of disrupting the axis using CDK1 inhibitors.
Protocol:
- Inhibitor Preparation: Reconstitute dinaciclib (Selleckchem, S2768) in DMSO per manufacturer's instructions [3].
- In Vitro Treatment: Treat cisplatin-resistant GC cells with dinaciclib (dose range: 10-100 nM) alone and in combination with cisplatin.
- In Vivo Administration: Utilize patient-derived xenograft (PDX) models. Administer dinaciclib (20 mg/kg) via intraperitoneal injection three times weekly for 4 weeks, combined with cisplatin (1 mg/kg) once weekly [3].
- Endpoint Analysis: Monitor tumor volume regularly and process tissues for IHC analysis of pathway components (CDK1, SOX9, BCL-xL).
Analyzing Epigenetic Regulation of miR-145
Purpose: Investigate DNMT1-mediated methylation silencing of miR-145.
DNA Methyltransferase Inhibition:
- Treatment: Expose resistant cells to DNA methyltransferase inhibitor 5-Aza-2'-deoxycytidine (5-Aza) [8].
- miRNA Quantification: Isolate total RNA using TRIzol reagent. Perform reverse transcription and qPCR using specific primers for mature miR-145. Normalize to appropriate small RNA controls (e.g., U6 snRNA) [3].
- Methylation Analysis: Perform bisulfite sequencing of the miR-145 promoter region to confirm methylation status changes following 5-Aza treatment or DNMT1 knockdown.
Troubleshooting Guides & FAQs
Frequently Asked Questions
Table 2: Key Research Reagent Solutions
| Reagent/Tool | Specific Example (Source) | Primary Function in Research |
|---|---|---|
| CDK1 Inhibitor | Dinaciclib (Selleckchem, S2768) [3] | Pharmacological inhibition of CDK1 kinase activity to disrupt the axis |
| siRNA for Knockdown | ON-TARGETplus siRNA pools (Horizon Discovery) [3] | Targeted genetic suppression of CDK1, SOX9, or DNMT1 |
| DNA Methyltransferase Inhibitor | 5-Aza-2'-deoxycytidine [8] | Demethylating agent to reverse miR-145 silencing |
| cisplatin-resistant cell lines | Derived from AGS, MKN28, MKN45 parents [3] | In vitro models for studying chemoresistance mechanisms |
| Patient-Derived Xenograft (PDX) Models | e.g., PDX539 [3] | In vivo models maintaining tumor heterogeneity for therapeutic testing |
| Anti-SOX9 Antibody | AB5535 (Sigma-Aldrich) [9] | Detection of SOX9 protein levels via western blot, IHC, or IF |
Q1: Our siRNA-mediated CDK1 knockdown shows insufficient protein reduction. What optimization steps are recommended?
A: Ensure transfection efficiency is optimized using a fluorescently-labeled control siRNA. Validate using multiple siRNA sequences targeting different CDK1 regions. Increase transfection reagent concentration or try alternative reagents. Extend knockdown time to 72-96 hours and confirm efficacy at both mRNA (qPCR) and protein (western blot) levels before functional assays.
Q2: When treating with dinaciclib, we observe high cytotoxicity in our resistant cell lines at low nanomolar doses. How should we adjust treatment?
A: Perform a detailed dose-response curve (e.g., 1-100 nM) to establish an IC₁₀-IC₃₀ range for combination studies. Cytotoxicity is expected with CDK1 inhibition; the key is using sublethal doses that sensitize to cisplatin. Consider pulse treatment (e.g., 6-24 hours) followed by recovery period before cisplatin exposure.
Q3: We cannot detect miR-145 upregulation following 5-Aza treatment in our resistant models. What could explain this?
A: Consider these possibilities: (1) The resistant model may utilize alternative resistance mechanisms not involving miR-145 silencing. (2) Optimize 5-Aza concentration (typical range 1-10 μM) and treatment duration (3-5 days with replenishment). (3) Confirm DNMT1 involvement by concomitant DNMT1 knockdown. (4) Verify miR-145 promoter methylation status via bisulfite sequencing.
Q4: In our PDX experiments, the combination of dinaciclib and cisplatin shows additive but not synergistic effects. What parameters should we revisit?
A: Re-evaluate: (1) Dosing schedule - staggered administration (e.g., dinaciclib before cisplatin) may improve synergy. (2) Tumor characterization - ensure PDX models express high baseline CDK1/SOX9. (3) Pathway analysis - verify target engagement by assessing SOX9 and BCL-xL reduction in treated tumors via IHC. (4) Consider testing additional CDK1 inhibitors to rule out off-target effects.
Pathway Visualization
Diagram 1: The CDK1-DNMT1-miR-145-SOX9 Axis in Gastric Cancer Chemoresistance. This pathway illustrates how CDK1 activation leads to epigenetic silencing of tumor suppressor miR-145 via DNMT1, resulting in SOX9 protein accumulation and subsequent transcriptional activation of the anti-apoptotic factor BCL-xL, ultimately conferring resistance to cisplatin-induced apoptosis [3] [8].
The transcription factor SOX9 has been identified as a critical driver of therapy resistance in high-grade serous ovarian cancer (HGSOC), the most common and lethal subtype of ovarian cancer [9] [1]. Chemotherapy resistance remains an urgent challenge in treating this disease, with nearly half of the more than 20,000 individuals diagnosed each year dying from the disease [10] [2]. Recent research has established that SOX9 is not only upregulated in chemoresistant ovarian cancer cells but also plays a functional role in mediating resistance to both conventional platinum-based chemotherapy and targeted PARP inhibitor (PARPi) therapies [9] [1] [2]. SOX9 expression is epigenetically upregulated in response to chemotherapy treatment in ovarian cancer cell lines and patient samples, positioning it as a key therapeutic target for overcoming treatment resistance [10] [2].
Molecular Mechanisms: How SOX9 Drives PARP Inhibitor Resistance
The USP28-SOX9 Regulatory Axis
Recent research has revealed a crucial molecular mechanism through which SOX9 promotes PARPi resistance in ovarian cancer. The deubiquitinating enzyme USP28 was identified as a novel interacting partner that stabilizes SOX9 protein levels [9] [11]. During olaparib treatment, the E3 ubiquitin ligase FBXW7 normally mediates SOX9 ubiquitination and subsequent degradation. However, USP28 inhibits this process, leading to SOX9 accumulation and enhanced DNA damage repair capability [9]. This stabilization of SOX9 by USP28 enables cancer cells to survive PARP inhibitor treatment through enhanced DNA repair mechanisms.
SOX9 as a Master Regulator of DNA Damage Repair Genes
Chromatin Immunoprecipitation Sequencing (ChIP-Seq) analysis has demonstrated that SOX9 directly binds to the promoters of key DNA damage repair (DDR) genes, including SMARCA4, UIMC1, and SLX4 [9]. By regulating these critical DDR components, SOX9 enhances the cancer cell's ability to repair DNA damage that would otherwise be lethal in the presence of PARP inhibition. This transcriptional regulation of DDR genes represents a fundamental mechanism by which SOX9-expressing cells bypass the synthetic lethality induced by PARP inhibitors in homologous recombination-deficient cells.
Figure 1: USP28-SOX9 Axis in PARPi Resistance. Under normal conditions, PARP inhibition causes DNA damage accumulation, triggering FBXW7-mediated SOX9 ubiquitination and degradation. In resistance, USP28 stabilizes SOX9, enabling transcription of DNA damage repair (DDR) genes and PARPi resistance. USP28 inhibitor AZ1 can block this stabilization.
SOX9-Mediated Cancer Stem Cell Reprogramming
Beyond its role in DNA damage repair, SOX9 drives chemoresistance by reprogramming ovarian cancer cells into stem-like cancer cells [10] [1]. Using CRISPR/Cas9 gene-editing to activate SOX9 expression, researchers found that increasing SOX9 expression reprogrammed ovarian cancer cells into tumor-initiating cells that continuously self-renew and proliferate, contributing significantly to chemotherapy resistance [10] [2]. Single-cell RNA sequencing of primary patient ovarian cancer tumors revealed a rare cluster of cells with high SOX9 expression and stem-like features, suggesting SOX9 serves as a master regulator of these treatment-resistant cells [10] [2].
Quantitative Data: SOX9 Expression and Therapeutic Response
Table 1: SOX9-Associated Clinical and Experimental Outcomes in Ovarian Cancer
| Metric | Experimental Finding | Clinical/Research Significance | Source |
|---|---|---|---|
| Patient Survival | Shorter overall survival in high SOX9 expressors (HR=1.33) | Patients in top SOX9 quartile had significantly worse survival | [1] |
| Chemotherapy Response | SOX9 upregulation within 72 hours post-carboplatin | Rapid response mechanism to platinum-based chemotherapy | [1] |
| PARPi Resistance | USP28 stabilization of SOX9 enhances olaparib resistance | Direct molecular mechanism of PARPi resistance identification | [9] |
| Stem Cell Population | Rare SOX9-high cluster in primary tumors | Enriched for cancer stem cells and chemoresistance modules | [1] |
Table 2: Key DNA Damage Repair Genes Regulated by SOX9 in Ovarian Cancer
| Gene | Function in DNA Damage Repair | SOX9 Binding Evidence | Therapeutic Implications |
|---|---|---|---|
| SMARCA4 | Chromatin remodeling, HR repair | ChIP-Seq confirmation | Potential biomarker for HR proficiency |
| UIMC1 | RAP80 complex, DNA damage signaling | ChIP-Seq confirmation | DSB repair regulation |
| SLX4 | DNA structure-specific endonuclease | ChIP-Seq confirmation | Resolution of DNA crosslinks |
Experimental Protocols: Key Methodologies for Studying SOX9 in PARPi Resistance
Protein-Protein Interaction Analysis (Co-Immunoprecipitation)
Purpose: To identify novel SOX9 interacting partners, particularly USP28 [9].
Detailed Protocol:
- Culture ovarian cancer cells (SKOV3, UWB1.289) in appropriate media [9].
- Wash cells twice with PBS and lyse using Western and IP Lysis Buffer with protease inhibitors [9].
- Centrifuge at 12,000 rpm for 5 minutes to collect cellular supernatants [9].
- Incubate 800 μg of cellular extract with 5 μL of primary antibodies (anti-SOX9, anti-USP28) or control IgG overnight at 4°C [9].
- Add protein A/G magnetic beads and incubate for 2 hours on a rotary shaker at 4°C [9].
- Wash beads three times with lysis buffer [9].
- Elute bound complexes by boiling in 2× SDS loading buffer for western blot analysis [9].
Troubleshooting Tips:
- Use HRP-conjugated secondary antibodies against rabbit IgG light chain to avoid interference from denatured IgG heavy chains [9].
- Include negative controls with normal rabbit/mouse IgG for each experiment [9].
- For flag-tagged proteins, use anti-Flag nanobody agarose beads for higher specificity [9].
Protein Stability and Ubiquitination Assays
Purpose: To assess SOX9 protein turnover and ubiquitination status in response to USP28 inhibition [9].
Detailed Protocol:
- Treat cells with cycloheximide (CHX, 100 μg/mL) to block new protein synthesis [9].
- Add USP28 inhibitor AZ1 (concentration range: 1-10 μM) or DMSO vehicle control [9].
- Harvest cells at time points (0, 1, 2, 4, 8 hours) post-treatment [9].
- Lyse cells in RIPA buffer with protease inhibitors [9].
- Perform western blotting with SOX9 antibody [9].
- For ubiquitination: Treat cells with MG132 (10 μM) for 4 hours before lysis to prevent proteasomal degradation [9].
- Perform co-IP with SOX9 antibody, followed by western blot with ubiquitin antibody [9].
Chromatin Immunoprecipitation Sequencing (ChIP-Seq)
Purpose: To identify genome-wide SOX9 binding sites and target DNA damage repair genes [9].
Detailed Protocol:
- Crosslink proteins to DNA with 1% formaldehyde for 10 minutes at room temperature.
- Quench crosslinking with 125 mM glycine for 5 minutes.
- Sonicate chromatin to 200-500 bp fragments.
- Immunoprecipitate with SOX9 antibody or control IgG overnight at 4°C.
- Collect immune complexes with protein A/G beads.
- Reverse crosslinks and purify DNA.
- Prepare sequencing libraries and perform high-throughput sequencing.
- Analyze sequencing data to identify SOX9 binding peaks, particularly in promoter regions of DDR genes.
Research Reagent Solutions: Essential Tools for SOX9-PARPi Research
Table 3: Key Reagents for Investigating SOX9-Mediated PARPi Resistance
| Reagent Category | Specific Examples | Application/Function | Experimental Notes |
|---|---|---|---|
| Cell Lines | SKOV3 (ovarian cancer), UWB1.289 (BRCA1-deficient), PARPi-resistant SKOV3 (SKOV3/Ola) | In vitro modeling of PARPi resistance | Generate resistant lines by incremental olaparib exposure [9] |
| Inhibitors | Olaparib (PARPi), AZ1 (USP28 inhibitor), THZ2 (CDK7/SE inhibitor) | Target validation and combination studies | AZ1 reduces SOX9 stability; THZ2 suppresses SE-driven SOX9 [9] [12] |
| Antibodies | SOX9 (AB5535), USP28 (17707-1-AP), FBXW7 (ab192328), γH2AX (ab81299) | Protein detection, Co-IP, immunofluorescence | γH2AX for DNA damage quantification [9] |
| Plasmids | pCMV-Flag-SOX9, pCMV-Flag-USP28, FBXW7 constructs | Overexpression and mechanistic studies | Flag-tag for purification and detection [9] |
The Scientist's Toolkit: Frequently Asked Questions
Q1: What is the most effective strategy to target SOX9 for overcoming PARPi resistance in ovarian cancer models?
A: Combined inhibition of USP28 and PARP has demonstrated significant efficacy. The USP28-specific inhibitor AZ1 reduces SOX9 protein stability and increases sensitivity to olaparib in ovarian cancer cells [9]. Additionally, super-enhancer inhibitors like THZ2 (targeting CDK7) and JQ1 (targeting BRD4) have shown promise in suppressing SOX9 expression and reversing chemoresistance in other cancer models, suggesting potential applicability in ovarian cancer [12].
Q2: How quickly does SOX9 expression change in response to chemotherapy, and what techniques can detect these changes?
A: SOX9 upregulation occurs rapidly after chemotherapy exposure. Studies show increased SOX9 at both RNA and protein levels within 72 hours of carboplatin treatment [1]. Detection methods include:
- Western blotting for protein level changes [9]
- qRT-PCR for mRNA expression [1]
- Single-cell RNA sequencing for population heterogeneity [1]
- Immunohistochemistry on patient samples pre- and post-chemotherapy [10]
Q3: What evidence supports SOX9's direct role in regulating DNA damage repair genes?
A: ChIP-Seq analysis provides direct evidence of SOX9 binding to promoter regions of key DDR genes including SMARCA4, UIMC1, and SLX4 [9]. Functional validation includes:
- Reduced expression of these DDR genes following SOX9 knockdown
- Increased DNA repair capacity in SOX9-overexpressing cells
- Enhanced sensitivity to PARPi when SOX9 is destabilized [9]
Q4: Are there reliable biomarkers to identify patients with SOX9-driven resistance?
A: Current evidence suggests:
- High SOX9 expression correlates with poorer overall survival [1]
- Post-treatment tumor samples show elevated SOX9 compared to pre-treatment [1]
- Single-cell analyses identify rare SOX9-high cell clusters with stem-like features [1]
- USP28 expression levels may predict SOX9 stabilization and PARPi resistance [9]
Q5: What are the major technical challenges in studying SOX9 protein stability, and how can they be addressed?
A: Common challenges and solutions:
- Rapid SOX9 turnover: Use proteasome inhibitors (MG132) to stabilize for detection [9]
- Complex regulation: Simultaneously monitor USP28 and FBXW7 activity [9]
- Context-dependent effects: Include multiple cell line models with different genetic backgrounds [9]
- Stem cell heterogeneity: Employ single-cell approaches to identify SOX9-high subpopulations [1]
The USP28-SOX9 axis represents a promising therapeutic target for overcoming PARP inhibitor resistance in ovarian cancer [9]. Combined inhibition of USP28 and PARP demonstrates the potential to disrupt SOX9-mediated DNA damage repair and resensitize resistant tumors [9]. Furthermore, the emerging role of SOX9 in promoting a stem-like, chemoresistant state underscores the importance of targeting this pathway to address tumor heterogeneity and plasticity [1]. Future research should focus on developing more specific SOX9 inhibitors, validating biomarkers for patient stratification, and exploring combination therapies that simultaneously target SOX9 stability and function. The mechanistic insights into SOX9's role in DNA damage repair and stem cell maintenance provide a strong foundation for developing next-generation therapeutic strategies to improve outcomes for ovarian cancer patients facing treatment resistance.
SOX9's Dual Role in the Tumor Microenvironment and Immune Evasion
FAQ: Troubleshooting SOX9-Mediated Therapy Resistance
Q1: My cancer cell lines are surviving platinum-based chemotherapy. Could SOX9 be involved, and how can I confirm this?
Yes, SOX9 is a key driver of chemoresistance. To confirm its role:
- Measure SOX9 Expression: Perform qPCR and Western Blot on treated vs. untreated cells. A significant upregulation of SOX9 at both RNA and protein levels post-treatment indicates involvement [1] [2].
- Functional Validation: Use CRISPR/Cas9 to knock out SOX9. Sensitization to carboplatin in knockout cells, evidenced by colony formation assays, confirms its functional role in resistance [1].
Q2: My in vivo model shows tumor relapse after therapy. How can I investigate if SOX9-expressing stem-like cells are responsible?
- Single-Cell RNA Sequencing: Analyze treatment-naive and post-treatment tumor cells. The presence and expansion of a rare cell cluster with high SOX9 expression and stemness gene signatures post-therapy indicates SOX9-driven plasticity [1].
- Immunohistochemistry: Stain patient-derived tumor microarrays for SOX9. Enrichment of SOX9+ cells in post-chemotherapy samples correlates with poor survival and resistance [1] [13].
Q3: The tumor immune microenvironment in my model is immunosuppressive. Is SOX9 contributing to this, and which immune cells should I focus on?
Absolutely. SOX9 recruits and activates immunosuppressive cells.
- Focus on Tregs and Macrophages: Utilize flow cytometry and immunofluorescence to quantify infiltrating regulatory T cells (Tregs) and M2-like tumor-associated macrophages (TAMs). SOX9 overexpression often correlates with increased levels of these cells [14] [15] [13].
- Check Immune Checkpoints: Analyze expression of PD-L1 on tumor cells. SOX9 can transactivate PD-L1, contributing to T-cell exhaustion [14] [15].
Q4: I am observing conflicting roles of SOX9—it seems to promote both tissue repair and tumor progression. Is this possible?
Yes. SOX9 is a "double-edged sword" with context-dependent functions [15].
- In Cancer: It promotes immune evasion, stemness, and chemoresistance.
- In Normal Physiology: It is essential for maintaining macrophage function, cartilage formation, and tissue regeneration [15]. Your experimental context (e.g., cancer vs. tissue injury model) determines its role.
Key Experimental Protocols for Investigating SOX9
Protocol 1: Establishing a SOX9-Driven Chemoresistance Model
Objective: To epigenetically induce SOX9 and confer a stem-like, chemoresistant state in ovarian cancer cells [1].
Methodology:
- Cell Line: Use high-grade serous ovarian cancer (HGSOC) lines (e.g., OVCAR4, Kuramochi).
- SOX9 Activation: Employ CRISPRa (activation) or treatment with epigenetic modulators (e.g., HDAC inhibitors) to upregulate endogenous SOX9 expression.
- Phenotypic Assays:
- Colony Formation Assay: Treat SOX9-activated and control cells with carboplatin. Count colonies after 1-2 weeks. SOX9-activated cells will show significant resistance and form more colonies [1].
- Stemness Evaluation: Analyze by flow cytometry for established cancer stem cell (CSC) markers (e.g., CD133, CD44). Perform spheroid formation assays in low-attachment plates.
- Transcriptomic Analysis: Perform bulk or single-cell RNA-Seq to confirm the induction of a stem-like transcriptional state and chemoresistance gene signatures [1].
Protocol 2: Assessing SOX9-Mediated Immune Evasion
Objective: To determine how SOX9 shapes an immunosuppressive tumor microenvironment (TME) [14] [15] [13].
Methodology:
- In Vitro Co-culture:
- Co-culture SOX9-overexpressing cancer cells with peripheral blood mononuclear cells (PBMCs) or purified T cells.
- Measure T-cell proliferation (e.g., CFSE dilution) and activation (e.g., CD69, IFN-γ production). SOX9 is expected to suppress T-cell function.
- In Vivo Validation:
- Mechanistic Insight:
- Use ChIP-qPCR to confirm SOX9 binding to the promoter regions of immune modulators like PD-L1 and CXCL12 [14].
The table below consolidates key quantitative findings on SOX9 from recent studies.
Table 1: Summary of Key SOX9-Related Data from Recent Research
| Cancer Type | SOX9's Role & Mechanism | Experimental Model | Key Quantitative Finding | Source |
|---|---|---|---|---|
| High-Grade Serous Ovarian Cancer (HGSOC) | Drives platinum resistance & stem-like state | HGSOC cell lines, patient scRNA-Seq | SOX9 expression significantly increased in post-chemotherapy patient cells (8 of 11 patients) [1]. | |
| Pan-Cancer (e.g., Liver Cancer) | Promotes immunosuppressive milieu | Bioinformatics analysis of TCGA data | SOX9 increases Treg infiltration and decreases CD8+ T-cell infiltration [14]. | |
| Glioblastoma (GBM) | Prognostic biomarker linked to immune infiltration | TCGA/GTEx database analysis | High SOX9 expression is an independent prognostic factor in IDH-mutant GBM and correlates with immune checkpoint expression [13]. | |
| Breast Cancer | Regulates tumor initiation and proliferation | BC cell lines (e.g., T47D, MCF-7) | SOX9 identified as a key driver in the progression of benign lesions to aggressive basal-like BC [7]. |
Signaling Pathways and Experimental Workflows
SOX9 in Immune Evasion and Chemoresistance
Experimental Workflow for SOX9 Functional Analysis
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for SOX9 Investigations
| Reagent / Tool | Function & Application | Key Considerations & Examples |
|---|---|---|
| CRISPR/Cas9 Systems | To knockout (KO) or activate (a) the endogenous SOX9 gene for functional validation. | Use SOX9-targeting sgRNAs. KO sensitizes to chemo; activation induces resistance [1] [2]. |
| SOX9 Antibodies | For detecting SOX9 protein levels via Western Blot, Immunohistochemistry (IHC), and Immunofluorescence (IF). | Validate antibodies for specific applications (IHC vs. WB). Critical for correlating SOX9 with patient prognosis [13]. |
| scRNA-Seq Platforms | To identify rare SOX9+ stem-like cell clusters and analyze tumor ecosystem heterogeneity. | Identify SOX9-expressing cells and their associated stemness/chemoresistance signatures in patient samples [1]. |
| Immune Cell Profiling Panels | Antibody panels for flow cytometry to quantify tumor-infiltrating immune cells (Tregs, CD8+ T cells, Macrophages). | Essential for demonstrating SOX9-mediated immunosuppression (e.g., increased Tregs, decreased CD8+ T cells) [14] [13]. |
| HDAC Inhibitors | Epigenetic modulators used to investigate and induce SOX9 upregulation. | Tool for mimicking the epigenetic changes that lead to SOX9-driven chemoresistance [1] [7]. |
Correlation of SOX9 Overexpression with Poor Prognosis Across Malignancies
The SRY-Box Transcription Factor 9 (SOX9) is a crucial transcription factor that controls growth, differentiation, and stemness of progenitor cells [16]. Originally recognized for its role in embryonic development, chondrogenesis, and sex determination, SOX9 is now established as a key driver in tumorigenesis [16] [17]. Research demonstrates that SOX9 protein regulates tumor initiation and progression by directly participating in tumor initiation, proliferation, migration, and chemotherapy resistance [16]. SOX9 overexpression is frequently observed across diverse malignancies and is increasingly associated with aggressive disease features and treatment failure [17]. Understanding SOX9-mediated mechanisms provides critical insights for developing novel therapeutic strategies to overcome treatment resistance in cancer.
Clinical Evidence: SOX9 Overexpression Correlates with Poor Prognosis
Quantitative Evidence from Meta-Analysis
A comprehensive meta-analysis of 17 studies involving 3,307 patients with solid tumors revealed that high SOX9 expression consistently correlates with poor clinical outcomes [17]. The pooled data demonstrate significant negative impacts on survival metrics across multiple cancer types.
Table 1: SOX9 Overexpression Impact on Survival Outcomes Based on Meta-Analysis
| Survival Metric | Hazard Ratio (HR) | 95% Confidence Interval | P-value | Statistical Model |
|---|---|---|---|---|
| Overall Survival (OS) | 1.66 | 1.36-2.02 | < 0.001 | Multivariate analysis |
| Disease-Free Survival (DFS) | 3.54 | 2.29-5.47 | 0.008 | Multivariate analysis |
Table 2: SOX9 Association with Clinicopathological Features
| Clinicopathological Feature | Association with SOX9 Overexpression | Statistical Measure |
|---|---|---|
| Tumor Size | Positive correlation | Pooled Odds Ratio (OR) |
| Lymph Node Metastasis | Positive correlation | Pooled Odds Ratio (OR) |
| Distant Metastasis | Positive correlation | Pooled Odds Ratio (OR) |
| Clinical Stage | Association with higher stage | Pooled Odds Ratio (OR) |
Prognostic Significance Across Specific Malignancies
The prognostic value of SOX9 extends across diverse tumor types, with studies confirming its negative impact in specific cancers:
- Breast Cancer: SOX9 overexpression drives basal-like breast cancer progression and is implicated in the transition from benign breast lesions to aggressive disease [16].
- Ovarian Cancer: High SOX9 expression indicates poor prognosis, lymph node metastasis, and chemotherapy resistance [9].
- Glioblastoma: SOX9 serves as a diagnostic and prognostic biomarker, with high expression particularly significant in IDH-mutant cases [18].
Mechanisms of SOX9-Mediated Therapy Resistance
SOX9 Drives Chemotherapy Resistance
Platinum Resistance in Ovarian Cancer
In high-grade serous ovarian cancer (HGSOC), SOX9 is epigenetically upregulated in response to chemotherapy treatment [19] [2]. This upregulation induces the formation of a stem-like subpopulation and significant chemoresistance in vivo [19]. Mechanistically, SOX9 increases transcriptional divergence, reprogramming the transcriptional state of naive cells into a stem-like state [19]. Single-cell analysis shows that chemotherapy treatment results in rapid population-level induction of SOX9 that enriches for this stem-like transcriptional state [19].
PARP Inhibitor Resistance in Ovarian Cancer
Recent research has identified a novel mechanism for SOX9-mediated PARP inhibitor (PARPi) resistance in ovarian cancer [9]. The deubiquitinating enzyme USP28 was identified as a novel interacting partner of SOX9 that inhibits ubiquitination and subsequent degradation of SOX9, which is normally mediated by the E3 ubiquitin ligase FBXW7 during olaparib treatment [9]. Chromatin immunoprecipitation sequencing (ChIP-Seq) analysis revealed that SOX9 binds to the promoters of key DNA damage repair (DDR) genes (SMARCA4, UIMC1, and SLX4), thereby regulating DDR processes in ovarian cancer [9].
Figure 1: USP28-SOX9 Axis Mediates PARPi Resistance. USP28 stabilizes SOX9 by counteracting FBXW7-mediated degradation. SOX9 then activates DNA damage repair genes, conferring resistance.
SOX9 as a Pioneer Factor in Transcriptional Reprogramming
SOX9 functions as a pioneer transcription factor capable of binding to cognate motifs in closed chromatin [20]. During cell fate reprogramming, SOX9 binds and opens key enhancers de novo while simultaneously recruiting co-factors away from original enhancers, which are subsequently silenced [20]. This reprogramming capacity enables SOX9 to drive transitions toward stem-like states associated with therapy resistance. When unhinged from normal regulation, sustained SOX9 expression activates oncogenic transcriptional regulators that chart the path to cancers typified by constitutive SOX9 expression [20].
SOX9 in Cancer Stem Cell Maintenance
SOX9 plays a crucial role in maintaining cancer stem-like cells (CSCs), a subpopulation responsible for treatment resistance and tumor recurrence [21]. In digestive system cancers, including pancreatic and hepatocellular carcinoma, SOX9 regulates self-renewal, tumorigenicity, and therapy resistance of CSCs [21]. In pancreatic cancer, nuclear factor-κB signaling epigenetically regulates SOX9 expression to promote CSC invasiveness [21]. Similarly, in hepatocellular carcinoma, SOX9 is necessary for tumor cell initiation, division, self-renewal, and tumorigenicity in CSCs [21].
The Scientist's Toolkit: Essential Research Reagents & Experimental Approaches
Table 3: Key Research Reagents for Investigating SOX9 in Cancer
| Reagent / Method | Specific Example / Product | Research Application | Key Findings Enabled |
|---|---|---|---|
| SOX9 Antibodies | Santa Cruz Biotechnology (sc-5535), Abcam (ab5535), Millipore | Immunohistochemistry, Western blot | Detection of SOX9 protein expression in tumor tissues |
| Cell Line Models | SKOV3/Ola (olaparib-resistant), T47D BC cell lines, MCF-7 | In vitro resistance studies | SOX9 role in G0/G1 cell cycle arrest; chemoresistance mechanisms |
| Gene Editing | CRISPR/Cas9 for SOX9 activation/knockout | Functional studies | Establishing causal role in stemness and chemoresistance |
| Animal Models | Krt14-rtTA;TRE-Sox9 mice, Xenograft models | In vivo tumorigenesis | SOX9-induced reprogramming and tumor initiation capacity |
| Small Molecule Inhibitors | AZ1 (USP28 inhibitor) | Therapeutic targeting | SOX9 destabilization and PARPi resensitization |
| Omics Approaches | CUT&RUN, ATAC-seq, scRNA-seq | Mechanistic studies | SOX9 binding sites, chromatin accessibility, cellular heterogeneity |
Frequently Asked Questions: Technical Troubleshooting Guide
SOX9 Detection & Expression Analysis
Q: What are the recommended methods for detecting SOX9 expression in patient tumor samples? A: Immunohistochemistry (IHC) is widely used with various SOX9 antibodies (Santa Cruz, Abcam, Millipore). Studies typically employ scoring systems like Percentage Score (PS > 2) or Immunoreactive Score (IRS > 5-6) [17]. For RNA detection, RNA sequencing from TCGA and GTEx databases provides reliable transcriptomic data [18]. Ensure proper controls as SOX9 expression can be heterogeneous within tumors.
Q: Why do I observe variable SOX9 expression in my cell culture models? A: SOX9 expression is highly context-dependent and influenced by multiple factors:
- Cell Density: Confluent cultures may show altered SOX9 expression
- Treatment Conditions: Chemotherapeutic agents can induce SOX9 upregulation [19] [2]
- Stemness State: Enrichment of cancer stem cells may increase SOX9 levels [21]
- Epigenetic Regulation: Histone modifications and chromatin accessibility affect SOX9 expression [20]
Functional Characterization of SOX9
Q: What is the most effective approach to establish SOX9's functional role in therapy resistance? A: Employ complementary gain-of-function and loss-of-function strategies:
- Gain-of-function: Inducible SOX9 expression systems to monitor temporal changes [20]
- Loss-of-function: CRISPR/Cas9 knockout or siRNA knockdown [19]
- Rescue experiments: Re-expression in knockout models Key readouts should include drug sensitivity assays, stem cell markers, and DNA damage repair capacity [9].
Q: How can I investigate SOX9's role as a pioneer transcription factor? A: Utilize these experimental approaches:
- CUT&RUN or ChIP-seq: Map SOX9 genomic binding sites [20]
- ATAC-seq: Assess chromatin accessibility changes [20]
- RNA-seq: Transcriptional profiling following SOX9 manipulation
- Co-immunoprecipitation: Identify SOX9 interaction partners [9]
Targeting SOX9 for Therapeutic Development
Q: What strategies show promise for targeting SOX9-mediated resistance? A: Several approaches are under investigation:
- USP28 Inhibition: AZ1 compound promotes SOX9 degradation and resensitizes to PARPi [9]
- Nanocarrier Delivery: SOX9 siRNA encapsulated in CSC-targeted nanocarriers [21]
- Epigenetic Modulators: Inhibitors of SOX9-upregulating pathways
- Combination Therapies: SOX9 targeting with conventional chemotherapy
Q: Are there concerns about toxicity when targeting SOX9? A: Yes, potential toxicity issues include:
- Gastrointestinal Toxicity: SOX9 inhibition may impair intestinal stem cell function and cause enteritis [21]
- Cartilage Defects: SOX9's role in chondrogenesis suggests possible joint toxicity Mitigation strategies include:
- Tissue-Specific Delivery: Targeted nanocarriers to minimize off-target effects [21]
- Intermittent Dosing: Transient versus continuous SOX9 inhibition
- SOX9 Inducers Post-Therapy: Local SOX9 delivery to protect normal tissues after radiation [21]
Key Experimental Protocols
Generating Chemoresistant Cells with Induced SOX9 Expression
Purpose: Establish cellular models of SOX9-mediated therapy resistance Procedure:
- Culture ovarian cancer cell lines (e.g., SKOV3, OVCAR8)
- Treat with sublethal concentrations of chemotherapeutic agent (e.g., cisplatin, olaparib)
- Confirm SOX9 upregulation via Western blot (validate with antibodies from Abcam or Santa Cruz)
- Use CRISPRa system for sustained SOX9 activation in naive cells [19]
- Validate stem-like properties through:
- Sphere formation assays
- Stem cell marker analysis (CD133, ALDH)
- Drug sensitivity profiling
Troubleshooting Tip: If SOX9 induction is insufficient, consider epigenetic priming with HDAC inhibitors to enhance chromatin accessibility [20].
Assessing SOX9-Protein Interactions via Co-Immunoprecipitation
Purpose: Identify novel SOX9 binding partners that regulate its stability Procedure:
- Transfect cells with Flag-tagged SOX9 construct
- Lyse cells in RIPA buffer with protease inhibitors
- Incubate lysates with anti-Flag magnetic beads overnight at 4°C
- Wash beads 3x with lysis buffer
- Elute bound complexes with 2× SDS loading buffer
- Analyze by Western blot for candidate interactors (e.g., USP28, FBXW7) [9]
Critical Controls: Include empty vector transfection and normal IgG controls to confirm specificity.
In Vivo Assessment of SOX9 Targeting in Combination Therapy
Purpose: Evaluate SOX9 inhibition for overcoming chemoresistance in preclinical models Procedure:
- Establish patient-derived xenografts or cell line-derived tumors
- Randomize mice into treatment groups:
- Vehicle control
- Standard chemotherapy alone
- SOX9 inhibitor (e.g., USP28 inhibitor AZ1) alone
- Combination therapy
- Administer treatments and monitor tumor volume
- Collect tumors for IHC analysis of SOX9, stem cell markers, and DNA damage (γH2AX)
- Assess metastasis and survival outcomes
Endpoint Analysis: Evaluate SOX9 protein stability, DNA repair capacity, and CSC population in residual tumors [9].
SOX9 overexpression represents a significant prognostic marker and therapeutic target across multiple malignancies. The transcription factor drives cancer progression through diverse mechanisms including stemness maintenance, transcriptional reprogramming, and therapy resistance. Targeting SOX9 through direct inhibition or modulation of its regulatory partners (e.g., USP28) offers promising avenues for overcoming resistance to conventional therapies. Future research should focus on developing clinically viable SOX9-targeting strategies with acceptable therapeutic windows, potentially through tissue-specific delivery approaches or rational combination therapies.
Therapeutic Arsenal: From SOX9 Inhibition to Combination Regimens
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents and their functions for developing SOX9 siRNA-loaded Lipid Nanoparticles (LNPs) based on the featured research.
| Research Reagent | Function/Explanation |
|---|---|
| DLin-MC3-DMA | An ionizable cationic lipid that encapsulates siRNA and facilitates endosomal escape [22]. |
| DSPC | A structural phospholipid that contributes to the stability and bilayer structure of the LNP [22]. |
| Cholesterol | Enhances nanoparticle stability and integrity by integrating into the lipid bilayer [22]. |
| DMG-PEG | A PEG-lipid that provides a hydrophilic layer to reduce nanoparticle aggregation and improve stability in biological fluids [22]. |
| DSPE-PEG-cRGDfK | A functionalized PEG-lipid used for active targeting; the cRGDfK peptide binds to integrins overexpressed on cancer cells, promoting tumor-specific uptake [22]. |
| siRNA against SOX9 (siSOX9) | The therapeutic agent responsible for degrading SOX9 mRNA, leading to the downregulation of the SOX9 oncoprotein [22]. |
| cRGDfK Peptide | A targeting ligand that binds specifically to αvβ3 integrins on colorectal cancer cells, enabling active targeting of LNPs to the tumor site [22]. |
Core Experimental Protocols
Protocol: Formulation and Preparation of Targeted siSOX9 LNPs
This protocol is adapted from methods used to create cRGDfK-modified LNPs (R-LNPs) for SOX9 siRNA delivery [22].
Step 1: Lipid Mixture Preparation
- Dissolve the lipid components in ethanol at a molar ratio of 50:38.5:10:1.5:0.5 (DLin-MC3-DMA: Cholesterol: DSPC: DMG-PEG: DSPE-PEG-cRGDfK). Ensure the total lipid concentration is 10 mM.
Step 2: Aqueous Phase Preparation
- Dilute the siSOX9 in a citrate buffer (pH 4.0) to a concentration of 0.2 mg/mL.
Step 3: Nanoparticle Formation
- Use a microfluidic device or a rapid mixing technique. Simultaneously pump the ethanolic lipid solution and the aqueous siRNA solution at a fixed flow rate (e.g., 1:3 volumetric ratio) into a mixing chamber to facilitate instantaneous LNP formation.
Step 4: Buffer Exchange and Purification
- Dialyze the freshly formed LNP suspension against a large volume of PBS (pH 7.4) for several hours at 4°C to remove ethanol and adjust the pH. Alternatively, use tangential flow filtration.
Step 5: Characterization
- Size and PDI: Use Dynamic Light Scattering (DLS). The optimized R-LNPs should have a uniform particle size of approximately 160 nm and a PDI below 0.21 [22].
- Zeta Potential: Measure using DLS. The zeta potential should be near-neutral (approx. +2.7 mV) [22].
- Encapsulation Efficiency: Use a Ribogreen assay. Quantify free siRNA before and after LNP disruption with a detergent. Aim for encapsulation efficiency >90% [22].
Protocol: In Vitro Functional Assessment of siSOX9 R-LNPs
This protocol outlines how to test the biological activity of the formulated LNPs in colorectal cancer cell lines.
Step 1: Cell Culture
- Maintain human colorectal cancer cell lines (e.g., HCT-116, Caco-2) in DMEM supplemented with 10% FBS and 1% penicillin-streptomycin at 37°C in a 5% CO2 atmosphere.
Step 2: Cellular Uptake and Internalization Pathway
- Seed cells in confocal dishes and treat with fluorescently labeled siSOX9 R-LNPs.
- To investigate the uptake mechanism, pre-treat cells for 1 hour with inhibitors for different pathways:
- Clathrin-mediated endocytosis: Chlorpromazine (10 µg/mL)
- Caveolae-mediated endocytosis: Filipin (5 µg/mL)
- Macropinocytosis: Amiloride (1 mM)
- Analyze intracellular fluorescence using confocal microscopy. Colocalization with lysosomal markers (e.g., LysoTracker) can be assessed to track LNP fate [22].
Step 3: Functional Assays
- Proliferation: Seed cells in 96-well plates. Treat with siSOX9 R-LNPs, non-targeted LNPs, and controls. After 72 hours, assess cell viability using a CCK-8 or MTT assay. Expect significant inhibition of proliferation in the siSOX9 R-LNP group [22].
- Migration & Invasion:
- Migration (Wound Healing): Create a scratch ("wound") in a confluent cell monolayer. Treat with LNPs and monitor wound closure over 24-48 hours. siSOX9 R-LNPs should significantly inhibit migration [22].
- Invasion (Transwell): Seed cells in Matrigel-coated transwell inserts. Treat with LNPs and allow cells to invade towards a serum gradient for 24-48 hours. Stain and count invaded cells. siSOX9 R-LNPs should reduce invasion [22].
Step 4: Molecular Efficacy Analysis (Western Blot)
- Lyse cells treated with siSOX9 R-LNPs and controls. Separate proteins by SDS-PAGE and transfer to a membrane.
- Probe the membrane with antibodies against:
- SOX9 (primary target)
- Downstream oncogenic mediators: β-catenin, Cyclin D1, c-Myc [22]
- Expected Outcome: Successful SOX9 knockdown should lead to reduced protein levels of SOX9, β-catenin, Cyclin D1, and c-Myc.
Data Presentation: Key Experimental Findings
Table 1: Physicochemical Characterization of Optimized siSOX9-LNPs
Summary of the key quality attributes for a successfully formulated batch of targeted LNPs [22].
| Parameter | Target Value / Result | Measurement Technique |
|---|---|---|
| Particle Size | 159.6 ± 0.93 nm | Dynamic Light Scattering (DLS) |
| Polydispersity Index (PDI) | 0.207 ± 0.016 | Dynamic Light Scattering (DLS) |
| Zeta Potential | 2.74 ± 0.35 mV | Dynamic Light Scattering (DLS) |
| siRNA Encapsulation Efficiency | 90.71 ± 1.63% | Ribogreen Assay |
Table 2: In Vitro and In Vivo Efficacy of siSOX9 R-LNPs
Summary of the functional outcomes observed in cellular and animal models of colorectal cancer [22].
| Experimental Model | Key Findings | Significance |
|---|---|---|
| In Vitro (HCT-116 & Caco-2 cells) | Significant inhibition of cell proliferation, migration, and invasion (P < 0.05 or 0.01). | Confirms anti-tumor effect of siSOX9 R-LNPs at the cellular level. |
| In Vivo (HCT-116 Xenograft Mice) | Significant inhibition of tumor growth and proliferation (P < 0.05 or 0.01). | Validates the therapeutic potential in a live animal model. |
| Molecular Analysis (In Vitro & In Vivo) | Downregulation of SOX9, β-catenin, Cyclin D1, and c-Myc protein levels. | Verifies on-target mechanism and disruption of key oncogenic pathways. |
Signaling Pathways and Experimental Workflow
Troubleshooting Guides and FAQs
Q1: Our siSOX9 LNPs show low encapsulation efficiency. What could be the cause and how can we improve it? A1: Low encapsulation efficiency is often related to suboptimal formulation conditions.
- Potential Cause 1: Incorrect lipid-to-siRNA ratio. The ratio of ionizable lipid to siRNA is critical for efficient complexation.
- Solution: Systemically vary the nitrogen (from lipid) to phosphate (from siRNA) ratio (N:P ratio) during formulation to find the optimum for your specific lipid mixture. A ratio between 3:1 and 6:1 is often a good starting point.
- Potential Cause 2: Inefficient mixing during LNP formation. Slow or inconsistent mixing leads to heterogeneous particles with poor encapsulation.
- Solution: Ensure rapid and turbulent mixing of the lipid and aqueous phases. Use a microfluidic device with controlled flow rates for reproducible results. Increasing the total flow rate while maintaining a fixed ratio can improve mixing efficiency.
Q2: Our targeted R-LNPs do not show superior cellular uptake or efficacy compared to non-targeted LNPs in vitro. What might be wrong? A2: This suggests the active targeting moiety is not functioning as intended.
- Potential Cause 1: The targeting ligand (cRGDfK) is not properly oriented or accessible on the LNP surface due to PEG density.
- Solution: Optimize the molar percentage of the DSPE-PEG-cRGDfK in the lipid formulation (e.g., test between 0.5-1.0%). A very high PEG density can create a steric barrier that shields the ligand.
- Potential Cause 2: The target receptor (e.g., αvβ3 integrin) is not sufficiently expressed in your chosen cell line.
- Solution: Validate the expression level of the target receptor in your cell line using flow cytometry or Western blot. Switch to a cell line with known high expression (e.g., HCT-116) for proof-of-concept studies.
Q3: The siSOX9 LNPs work well in vitro but show minimal therapeutic effect in our mouse xenograft model. What are the key factors to check? A3: The in vivo environment presents additional barriers.
- Potential Cause 1: The LNPs are unstable in the systemic circulation or are cleared too quickly by the mononuclear phagocyte system (MPS).
- Solution: Confirm the PEG-lipid (DMG-PEG) is included in the formulation at a sufficient concentration (e.g., 1.5-3%) to provide a stealth effect and prolong circulation time [22].
- Potential Cause 2: Inefficient extravasation and penetration into the tumor core.
- Solution: Use an orthotopic colorectal cancer model, which may better recapitulate the tumor microenvironment. Also, verify tumor-specific accumulation via in vivo imaging systems (IVIS) by using fluorescently labeled LNPs.
Q4: We observe significant cytotoxicity in our cell cultures after LNP treatment, even with control non-targeting LNPs. How can we address this? A4: General cytotoxicity often points to the formulation itself.
- Potential Cause: The composition or charge of the blank LNPs (without siRNA) is toxic, potentially due to the ionizable lipid or an overly positive surface charge.
- Solution:
- Test the cytotoxicity of blank LNPs (devoid of siRNA) to isolate the cause.
- Ensure the final LNP formulation has a near-neutral zeta potential, as highly positive charges can disrupt cell membranes [22].
- Consider testing alternative, more biodegradable ionizable lipids known for better safety profiles.
Q5: How does targeting SOX9 help overcome therapy resistance in colorectal cancer? A5: SOX9 is implicated in multiple resistance mechanisms. Targeting it disrupts these pro-survival pathways.
- Mechanism 1: DNA Damage Repair: SOX9 upregulates MMS22L, a key protein involved in DNA double-strand break repair. This pathway allows cancer cells to survive the DNA damage induced by chemotherapeutics like oxaliplatin. Silencing SOX9 impairs this repair mechanism, re-sensitizing cells to treatment [23].
- Mechanism 2: Cancer Stem Cell (CSC) Maintenance: SOX9 is a key regulator of cell plasticity and enriches for CSCs, which are often therapy-resistant. SOX9 promotes self-renewal, tumor initiation, and a mesenchymal phenotype, all associated with aggressive and resistant disease. Knocking down SOX9 reduces this stem-like population [24].
- Mechanism 3: Oncogenic Signaling: SOX9 interacts with and stabilizes β-catenin, and regulates downstream effectors like c-Myc and Cyclin D1. This reinforces the Wnt/β-catenin signaling axis, a key driver of CRC. siSOX9 disrupts this network, inhibiting tumor growth [22] [25].
This guide provides technical support for researchers employing the cyclin-dependent kinase (CDK) inhibitor dinaciclib in experimental models of cancer, with a specific focus on overcoming SOX9-mediated therapy resistance. Dinaciclib (SCH727965, MK-7965) is a potent, small-molecule, multi-CDK inhibitor that selectively targets CDK1, CDK2, CDK5, and CDK9 at nanomolar concentrations [26] [27] [28]. Its function in disrupting upstream regulators makes it a valuable tool for investigating mechanisms of chemoresistance driven by transcription factors like SOX9.
Recent findings establish that the transcription factor SOX9 is epigenetically upregulated in response to chemotherapy, promoting a stem-like, chemoresistant state in cancer cells such as high-grade serous ovarian cancer [2]. Furthermore, SOX9 contributes to PARP inhibitor resistance in ovarian cancer by enhancing DNA damage repair (DDR) [9]. Dinaciclib can indirectly target this resistance axis by inhibiting key CDKs upstream of SOX9-driven survival pathways. This resource offers detailed protocols and troubleshooting advice to support your experiments with dinaciclib.
Key Research Reagent Solutions
The table below lists essential reagents and their applications in dinaciclib-based experiments.
| Reagent / Material | Key Function / Application | Technical Notes |
|---|---|---|
| Dinaciclib (SCH727965) | A multi-CDK inhibitor targeting CDK1, CDK2, CDK5, and CDK9. Induces apoptosis and cell cycle arrest. | Typically used in vitro at low nanomolar concentrations (IC50 ~10-50 nM). Soluble in DMSO [26] [29]. |
| Lipofectamine 3000 | Transfection reagent for plasmid DNA and siRNA. | Used for CDK1 overexpression or knockdown studies to validate mechanism [26]. |
| pcDNA3.1-CDK1 Plasmid | Forced CDK1 expression to study resistance mechanisms. | Used in gain-of-function experiments [26]. |
| CDK1 siRNA | Knocks down CDK1 expression to confirm target specificity. | Restores dinaciclib sensitivity in resistant cell lines [26]. |
| Annexin V / PI Staining | Detection of apoptotic cells via Flow Cytometry. | Standard assay for quantifying dinaciclib-induced apoptosis [26] [29]. |
| TUNEL Assay Kit | Fluorescently labels DNA fragmentation in apoptotic cells. | Alternative method for apoptosis detection [26]. |
| Antibodies: p-Rb, Cyclin B1, c-MYC, Survivin, Cleaved PARP | Western Blot analysis of dinaciclib mechanism of action. | Dinaciclib treatment typically decreases levels of these proteins [26] [29]. |
| AZ1 (USP28 Inhibitor) | Induces degradation of SOX9 protein. | Potential combination agent with dinaciclib to overcome SOX9-mediated resistance [9]. |
Detailed Experimental Protocols
Core Protocol: Assessing Dinaciclib Efficacy and Apoptosis In Vitro
This is a foundational protocol for treating cancer cells with dinaciclib and measuring subsequent apoptosis, a key phenotypic readout.
Workflow:
Materials:
- Dinaciclib (reconstituted in DMSO to a stock concentration, e.g., 10 mM)
- Target cell lines (e.g., lymphoma Raji cells, triple-negative breast cancer PDX cells, ovarian cancer cells) [26] [29]
- Complete cell culture medium (e.g., RPMI-1640 or DMEM with 10% FBS)
- FITC Annexin V / Dead Cell Apoptosis Kit (or similar)
- Phosphate Buffered Saline (PBS)
- Flow cytometer
Step-by-Step Method:
- Cell Seeding: Prepare single-cell suspensions and seed cells into 6-well plates at a density of 1 × 10^6 cells per well in complete medium. Allow cells to adhere and grow for approximately 24 hours [26].
- Drug Treatment: Add dinaciclib to the treatment wells at the desired final concentration (e.g., 10-50 nM, based on your IC50 data). Include a negative control (DMSO vehicle at the same dilution as in drug-treated wells) [29].
- Incubation: Incubate the cells for 24 to 48 hours at 37°C in a 5% CO2 humidified incubator.
- Cell Harvesting: After incubation, collect both adherent and floating cells. Wash the cells once with cold PBS.
- Staining: Resuspend the cell pellet in 100 μL of 1X Annexin V Binding Buffer. Add 5 μL of FITC-Annexin V and 1 μL of a 100 μg/mL PI working solution (or as per kit instructions). Incubate the mixture for 15 minutes at room temperature in the dark [26].
- Analysis: Add 400 μL of Annexin V Binding Buffer to each tube and analyze the cells by flow cytometry within 1 hour. Use the following gating:
- Viable cells: Annexin V negative / PI negative.
- Early apoptotic cells: Annexin V positive / PI negative.
- Late apoptotic/necrotic cells: Annexin V positive / PI positive.
Advanced Protocol: Validating CDK1 Involvement in Dinaciclib Response
This protocol is critical for mechanistically confirming that observed phenotypes are due to CDK1 inhibition, especially in the context of overcoming resistance.
Workflow:
Materials:
- Dinaciclib-resistant cell line (generated by intermittent exposure to increasing dinaciclib concentrations from 4 μM to 20 μM) [26]
- CDK1 siRNA and non-targeting scramble siRNA [26]
- pcDNA3.1-CDK1 overexpression plasmid and empty vector control [26]
- Lipofectamine 3000 transfection reagent
- Opti-MEM serum-free medium
- Antibodies for CDK1, phospho-Rb, Cyclin B1, SOX9, and a loading control (e.g., β-actin)
Step-by-Step Method:
- Establishing Resistance: Generate a dinaciclib-resistant sublime by culturing parental cells with progressively increasing concentrations of dinaciclib (e.g., from 4 μM to 20 μM) over several months. Confirmed resistance should be validated via IC50 assays [26].
- Cell Transfection:
- Seed resistant cells at 60-70% confluency in 6-well plates 24 hours before transfection.
- For siRNA knockdown, complex 50 nM CDK1 siRNA or scramble siRNA with Lipofectamine 3000 in Opti-MEM as per manufacturer's instructions.
- For overexpression, complex 1 μg of pcDNA3.1-CDK1 or empty vector plasmid per 2 × 10^5 cells.
- Add complexes to cells and incubate for 48-72 hours [26].
- Validation and Treatment: Harvest a portion of the transfected cells to confirm CDK1 knockdown or overexpression by Western Blot. Treat the remaining transfected cells with dinaciclib for functional assays.
- Functional Assays:
- Colony Formation: Re-seed transfected and treated cells at low density (300 cells per well in a 6-well plate) in drug-free medium. Allow colonies to form for 1-2 weeks, then stain with 0.1% crystal violet and count. Knockdown of CDK1 should restore sensitivity, reducing colony formation [26].
- Cell Cycle Analysis: After dinaciclib treatment, fix cells in 70% ethanol overnight at 4°C. The next day, stain DNA with Propidium Iodide (PI/RNase solution) and analyze by flow cytometry. Dinaciclib typically induces G2/M phase arrest [26] [29].
- Western Blotting: Analyze key downstream targets. Dinaciclib should reduce phosphorylation of Rb and protein levels of Cyclin B1 and c-MYC. Correlate these changes with SOX9 expression levels if investigating its pathway [29] [9].
Troubleshooting Guides & FAQs
Common Experimental Challenges
| Problem | Potential Causes | Solutions & Verification Steps |
|---|---|---|
| Lack of Apoptosis | Incorrect dinaciclib concentration; Inherently resistant cell line. | - Perform a dose-response curve (1-100 nM) to determine IC50.- Use a positive control cell line known to be sensitive (e.g., some TNBC PDX models) [29].- Check for RB1 loss, which can confer resistance to CDK4/6 inhibitors but not necessarily to dinaciclib. |
| Insufficient Cell Cycle Arrest | Incomplete CDK inhibition; Cell line-specific variations. | - Verify drug activity by Western Blot for reduced Rb phosphorylation and Cyclin B1 levels [29].- Extend treatment time (e.g., to 24-48 hours).- Consider that some cell lines may show G0/G1 block instead of G2/M [27]. |
| High Background in Apoptosis Assay | Excessive cell handling; Necrosis due to drug toxicity. | - Handle cells gently to avoid mechanical damage.- Include a vehicle-only control to establish baseline death.- Use TUNEL staining as an alternative method to confirm apoptosis [26]. |
| Development of Resistance | Upregulation of compensatory pathways (e.g., CDK1, SOX9). | - In resistant sublines, check for CDK1 upregulation via Western Blot [26].- Knockdown CDK1 with siRNA to restore drug sensitivity [26].- Investigate SOX9 protein levels and test combination with a USP28 inhibitor (AZ1) to degrade SOX9 [9]. |
| Unclear Mechanism | Off-target effects of dinaciclib. | - Use targeted siRNA knockdown of individual CDKs (CDK1, CDK2, CDK9). Studies show CDK9 knockdown mimics dinaciclib's effect on reducing Cyclin B1 and c-MYC in TNBC [29]. |
Frequently Asked Questions (FAQs)
Q1: My cancer cell line is resistant to CDK4/6 inhibitors like palbociclib. Is dinaciclib still a viable option? A: Yes. Resistance to CDK4/6 inhibitors is common in cancers with RB1 loss or CCNE1 (Cyclin E) amplification. Dinaciclib targets different CDKs (1, 2, 5, 9) and has demonstrated efficacy in RB-deficient and CCNE1-amplified models where palbociclib failed, such as in cholangiocarcinoma and triple-negative breast cancer [27] [29].
Q2: How does dinaciclib connect to overcoming SOX9-mediated therapy resistance? A: While dinaciclib does not directly inhibit SOX9, it targets upstream and parallel pathways. SOX9 drives chemoresistance by promoting a stem-like state and enhancing DNA damage repair [2] [9]. Dinaciclib can counteract this by:
- Inhibiting CDK9, which is crucial for the transcription of key survival genes like MYC and CCNB1 (Cyclin B1) [29].
- Disrupting the Unfolded Protein Response (UPR) via CDK1/5 inhibition, a pathway that can be co-opted for cell survival under stress [28].
- Its effect can be enhanced by combining it with agents that target SOX9 stability, such as the USP28 inhibitor AZ1 [9].
Q3: What is a key molecular signature that confirms dinaciclib is working in my experiment? A: A successful cellular response to dinaciclib is characterized by a consistent set of molecular changes. You should observe a decrease in the protein levels of phospho-Rb, Cyclin B1, c-MYC, and survivin via Western Blot analysis [29]. This confirms effective inhibition of its CDK targets and engagement of the apoptotic machinery.
Q4: For in vivo studies, what is an effective dosing regimen for dinaciclib? A: In patient-derived xenograft (PDX) mouse models, dinaciclib is often administered intraperitoneally (IP) once a week. It has shown a favorable safety profile in preclinical models and can be effectively combined with standard chemotherapies like gemcitabine to produce robust and sustained tumor growth inhibition [27].
A compelling body of evidence has established the transcription factor SRY-box transcription factor 9 (SOX9) as a critical driver of therapy resistance in ovarian cancer. Recent studies have elucidated that SOX9 is not only highly expressed in ovarian cancer tissues, where its upregulation correlates with poor prognosis, lymph node metastasis, and chemotherapy resistance, but it is also epigenetically upregulated in response to chemotherapy treatment [1] [2]. This chemotherapy-induced SOX9 expression promotes a stem-like transcriptional state, reprogramming naive ovarian cancer cells into cancer stem cells (CSCs) that are inherently resistant to therapy [1] [2]. Furthermore, in the context of Poly (ADP-ribose) polymerase inhibitor (PARPi) resistance, elevated SOX9 expression contributes directly to olaparib resistance in ovarian cancer models, highlighting its role across multiple resistance modalities [9].
Mechanistic Insight: The USP28-SOX9 Axis in DNA Damage Repair and Resistance
Core Mechanism and Interaction
Recent research has uncovered a crucial molecular axis wherein the deubiquitinating enzyme USP28 stabilizes the SOX9 protein, thereby promoting resistance. The core mechanism can be summarized as follows:
- USP28 as a Novel Stabilizer: USP28 was identified as a novel interacting partner of SOX9. This interaction inhibits the ubiquitination and subsequent proteasomal degradation of SOX9 that is normally mediated by the E3 ubiquitin ligase FBXW7, particularly during olaparib treatment [9].
- Enhanced DNA Damage Repair: Stabilized SOX9 binds to the promoters of key DNA damage repair (DDR) genes, including SMARCA4, UIMC1, and SLX4. This binding regulates DDR processes, enhancing the cell's ability to repair DNA damage induced by PARP inhibition [9].
- Consequence on PARPi Sensitivity: By stabilizing SOX9, USP28 directly promotes olaparib resistance. Conversely, targeted inhibition of USP28 promotes the ubiquitination and degradation of SOX9, impairs DNA damage repair capabilities, and ultimately sensitizes ovarian cancer cells to PARPi [9].
The signaling pathway and protein interactions are illustrated in the diagram below.
Frequently Asked Questions (FAQs) for Researchers
Q1: What is the experimental evidence that USP28 directly regulates SOX9 protein stability?
A1: The interaction was confirmed through a series of key experiments:
- Co-immunoprecipitation (Co-IP): USP28 was physically identified as a novel binding partner of SOX9 in ovarian cancer cells [9].
- Ubiquitination Assays: In the presence of olaparib, the E3 ligase FBXW7 mediates SOX9 ubiquitination. Co-expression of USP28, but not a catalytically inactive mutant, significantly inhibited this ubiquitination [9].
- Cycloheximide (CHX) Chase Experiments: Treatment with the protein synthesis inhibitor cycloheximide showed that the half-life of SOX9 protein was significantly prolonged in cells overexpressing USP28. Conversely, inhibition of USP28 with the specific inhibitor AZ1 reduced SOX9 protein stability [9].
Q2: Beyond PARPi resistance, what other functional roles does SOX9 play in ovarian cancer?
A2: SOX9 is a multifunctional oncoprotein in ovarian cancer:
- Driver of Chemoresistance: SOX9 is sufficient to induce a stem-like transcriptional state and significant resistance to platinum-based chemotherapy [1].
- Promoter of Stemness: SOX9 expression reprogrammes the transcriptional state of naive cells into a stem-like state, enriching for tumor-initiating cells (TICs) that self-renew, proliferate, and contribute to therapy resistance [2] [10].
- Regulator of CSC-associated phenotypes: SOX9 is involved in cellular activities related to Cancer Stem Cells (CSCs), including anoikis-resistance, regulation of the CSC marker CD44, and spheroid formation [30].
Q3: How does targeting the USP28-SOX9 axis resensitize ovarian cancer cells to PARP inhibition?
A3: Resensitization occurs through a mechanistic cascade, as detailed below:
Experimental Workflow for USP28 Inhibition
The inhibition of USP28 by AZ1 initiates a cascade of molecular events culminating in PARPi resensitization. The key quantitative data supporting this conclusion is summarized in the table below.
Table 1: Key Experimental Findings Supporting USP28 Inhibition in Overcoming PARPi Resistance
| Experimental Model | Key Finding | Quantitative/Measured Outcome | Citation |
|---|---|---|---|
| Ovarian cancer cell lines (SKOV3, UWB1.289) | USP28 inhibition with AZ1 reduces SOX9 protein stability. | Decreased SOX9 protein half-life in cycloheximide chase assays. | [9] |
| PARPi-resistant ovarian cancer cells | USP28 inhibition increases sensitivity to olaparib. | Increased cytotoxicity and cell death in combination treatment (AZ1 + olaparib). | [9] |
| Xenograft models | Combined USP28 inhibitor and PARPi suppresses tumor growth. | Reduced tumor volume in olaparib-resistant xenografts compared to monotherapy. | [9] |
| Chromatin Immunoprecipitation Sequencing (ChIP-Seq) | SOX9 binds promoters of key DDR genes. | Identification of SOX9 binding peaks at promoters of SMARCA4, UIMC1, and SLX4. | [9] |
Q4: Are there other SOX family transcription factors implicated in PARPi resistance?
A4: Yes, the SOX family appears to play a broader role in therapy resistance. A separate recent study identified SOX5 as significantly upregulated in olaparib-resistant breast and ovarian cancer cells. Similar to SOX9, SOX5 contributes to PARPi resistance by upregulating DNA repair pathway genes, in this case by interacting with YAP1 and suppressing the Hippo pathway [31]. This suggests that targeting specific SOX family members or their common downstream effectors could be a viable strategy.
The Scientist's Toolkit: Essential Research Reagents and Protocols
To experimentally investigate the USP28-SOX9 axis, researchers require specific reagents and protocols. The following table compiles key tools used in the cited studies.
Table 2: Research Reagent Solutions for Studying the USP28-SOX9 Axis
| Reagent / Assay | Specific Example / Catalog Number | Function in Experimental Context | Citation |
|---|---|---|---|
| USP28 Inhibitor | AZ1 (S8904, Selleck Chemicals) | A specific small-molecule inhibitor used to block USP28 deubiquitinase activity, leading to SOX9 degradation. | [9] |
| PARP Inhibitor | Olaparib (AZD2281; Selleck Chemicals) | Used to induce DNA damage and select for/research PARPi resistance mechanisms. | [9] |
| SOX9 Antibody | AB5535 (Sigma-Aldrich/EMD Millipore) | For detection of SOX9 protein levels via Western Blot or Immunofluorescence. | [9] [30] |
| USP28 Antibody | 17707-1-AP (Proteintech) | For detection of USP28 protein levels via Western Blot or Co-Immunoprecipitation. | [9] |
| Co-IP Assay | Anti-Flag/HA Magnetic Beads (e.g., AlpaLifeBio) | To validate the physical interaction between USP28 and SOX9. | [9] |
| Cycloheximide (CHX) Chase Assay | CHX (S7418, Selleck Chemicals) | To measure the half-life and stability of the SOX9 protein upon USP28 inhibition. | [9] |
| Proteasome Inhibitor | MG132 (S2619, Selleck Chemicals) | Used to inhibit the proteasome, confirming ubiquitin-mediated degradation of SOX9. | [9] |
Detailed Experimental Protocol: Validating the USP28-SOX9 Interaction and Functional Consequences
This protocol outlines the key steps to confirm that USP28 regulates SOX9 stability and impacts PARPi sensitivity.
Objective: To demonstrate that pharmacological inhibition of USP28 reduces SOX9 protein levels and sensitizes ovarian cancer cells to olaparib.
Materials:
- Ovarian cancer cell lines (e.g., SKOV3, UWB1.289, or their PARPi-resistant derivatives).
- USP28 inhibitor: AZ1 (e.g., Selleck Chemicals, S8904).
- PARP inhibitor: Olaparib (e.g., Selleck Chemicals).
- Dimethyl sulfoxide (DMSO) as vehicle control.
- Cycloheximide (CHX).
- Western blot reagents and antibodies against SOX9, USP28, γH2AX (a DNA double-strand break marker), and a loading control (e.g., β-Actin).
- Cell viability assay kit (e.g., MTT or Cell Counting Kit-8).
Procedure:
- Cell Treatment:
- Seed cells in appropriate culture plates and allow to adhere overnight.
- Pre-treat cells with a determined concentration of AZ1 (e.g., 1-10 µM) or DMSO vehicle control for 4-6 hours.
- Subsequently, add olaparib at a relevant concentration (e.g., IC~50~ or higher) to the respective wells. Include controls with DMSO, AZ1 alone, and olaparib alone.
Protein Stability Assay (CHX Chase):
- After pre-treatment with AZ1 or DMSO, add cycloheximide (e.g., 50-100 µg/mL) to inhibit new protein synthesis.
- Harvest cell lysates at various time points (e.g., 0, 1, 2, 4, 6 hours) after CHX addition.
- Perform Western blot analysis to detect SOX9 protein levels. Quantify band intensity and plot SOX9 degradation over time to determine protein half-life.
Functional Output Analysis:
- DNA Damage Assessment: From the treated cells, harvest lysates and probe for γH2AX by Western blot. Higher γH2AX levels indicate increased DNA damage, suggesting impaired DDR due to SOX9 loss.
- Cell Viability/Proliferation: Seed cells in 96-well plates, treat with AZ1 and olaparib alone or in combination for 72-96 hours. Perform MTT or CCK-8 assay according to the manufacturer's instructions. Calculate the combination index (CI) to determine synergism (CI < 1) [9] [31].
Expected Results:
- AZ1 treatment should lead to a rapid decrease in SOX9 protein levels in the CHX chase assay.
- The combination of AZ1 and olaparib should result in higher γH2AX levels compared to either agent alone, indicating synergistic DNA damage.
- The combination treatment should show a significant reduction in cell viability compared to monotherapies, demonstrating synergistic killing.
Troubleshooting Guides
FAQ 1: Why is targeting SOX9 proposed to overcome therapy resistance?
Answer: SOX9 is a transcription factor that promotes resistance to chemotherapy and radiotherapy by enriching and protecting cancer stem cells (CSCs), a subpopulation of tumor cells with strong self-renewal capacity that are inherently resistant to therapy [4] [21]. SOX9 is overexpressed in various aggressive, metastatic, and recurrent tumors, where it drives key pro-tumorigenic processes [4] [7] [1].
- Key Evidence for Chemoresistance: In high-grade serous ovarian cancer (HGSOC), SOX9 expression is significantly induced following platinum-based chemotherapy. Patients with high SOX9 expression have a shorter overall survival, and experimentally, the ablation of SOX9 increases sensitivity to carboplatin [1]. Similarly, in ovarian cancer, SOX9 contributes to PARP inhibitor (PARPi) resistance by regulating key DNA damage repair (DDR) genes like
SMARCA4,UIMC1, andSLX4[9]. - Key Evidence for Radioresistance: Studies on gastrointestinal cancer indicate that the transcription factor SOX9 is a key mediator of radioresistance in reserve intestinal stem cells. SOX9 knockout intestinal crypts underwent apoptosis after radiotherapy, demonstrating its critical role in survival post-radiation [21].
FAQ 2: What are the primary molecular mechanisms by which SOX9 confers resistance?
Answer: SOX9 drives therapy resistance through multiple interconnected mechanisms, which can be targeted to re-sensitize tumors. The table below summarizes the key pathways and the cancer types in which they have been observed.
Table 1: Key Mechanisms of SOX9-Mediated Therapy Resistance
| Mechanism | Functional Role in Resistance | Relevant Cancer Types |
|---|---|---|
| Cancer Stem Cell (CSC) Enrichment | Promotes a stem-like, plastic transcriptional state; CSCs are inherently resistant to therapy and drive tumor recurrence [4] [1]. | Osteosarcoma, Ovarian cancer, Breast cancer [4] [7] [1] |
| DNA Damage Repair (DDR) Enhancement | Binds to promoters of DDR genes (SMARCA4, UIMC1, SLX4), enhancing the cell's ability to repair therapy-induced DNA damage [9]. |
Ovarian cancer [9] |
| Activation of Pro-Survival Pathways | Upregulates pathways like AKT and ERBB signaling, promoting cell survival and tumorigenesis despite therapeutic insult [21] [7]. | Pancreatic cancer, Hepatocellular carcinoma, Breast cancer [21] [7] |
| Immune Evasion | Helps latent cancer cells and CSCs avoid immune surveillance, allowing them to persist after treatment [7]. | Breast cancer [7] |
FAQ 3: Which specific SOX9 inhibition strategies show promise in combination with chemotherapy?
Answer: Several targeted strategies have shown efficacy in preclinical models for sensitizing cancer cells to chemotherapy.
Targeting SOX9 Stability via USP28 Inhibition:
- Mechanism: The deubiquitinating enzyme USP28 binds to SOX9 and inhibits its FBXW7-mediated ubiquitination and degradation. Inhibiting USP28 leads to increased degradation of SOX9 protein [9].
- Combination Protocol: The specific USP28 inhibitor AZ1 can be used to sensitize ovarian cancer cells to PARP inhibitors like olaparib.
- Experimental Workflow:
- Treat ovarian cancer cells (e.g., SKOV3, UWB1.289) with AZ1 (e.g., 1-10 µM) for 24 hours prior to and during olaparib treatment.
- Confirm SOX9 downregulation via Western Blot (antibodies: SOX9 AB5535).
- Assess efficacy using colony formation assays and monitor DNA damage via γH2AX immunofluorescence (antibody: ab81299) [9].
Direct SOX9 Gene Knockout:
- Mechanism: Using CRISPR/Cas9 to ablate the SOX9 gene directly removes the driver of resistance.
- Combination Protocol: SOX9-knockout HGSOC cell lines are treated with carboplatin.
- Experimental Workflow:
- Generate SOX9 knockout lines using CRISPR/Cas9 with SOX9-targeting sgRNA.
- Treat parental and KO cells with increasing doses of carboplatin.
- Measure sensitivity using a colony formation assay. SOX9 ablation significantly reduces colony formation post-carboplatin treatment [1].
Diagram: Strategies to inhibit SOX9 and overcome chemoresistance. Targeting SOX9 via genetic ablation or pharmacologically by inhibiting its stabilizer USP28 can restore sensitivity to chemotherapy.
FAQ 4: What considerations are needed for combining SOX9 inhibition with radiotherapy?
Answer: Combining SOX9 inhibition with radiotherapy requires a nuanced approach due to SOX9's dual role in promoting tumor radioresistance while also being crucial for the regeneration of some normal tissues.
- The Challenge: In gastrointestinal cancer, SOX9 is essential for the function of radioresistant reserve intestinal stem cells (rISCs), which are necessary for regenerating the intestinal epithelium after radiation-induced damage. Ablating SOX9 in these normal tissues leads to a lack of regeneration capacity and increased apoptosis after radiation [21].
- Proposed Solution:
- For Tumor Sensitization: Use targeted delivery systems for SOX9 inhibitors (e.g., siRNA, small molecule inhibitors) specifically to the tumor site to minimize systemic effects on normal radiosensitive tissues [21].
- For Normal Tissue Protection: Conversely, targeted delivery of SOX9 or its inducers (e.g., RelA, Fgf8) to normal intestinal tissue could upregulate rISC function to protect against high-dose radiation-induced enteritis and promote crypt repair [21].
Table 2: Experimental Reagents for Studying SOX9 in Radioresistance
| Research Reagent | Function/Application | Example Source/Catalog |
|---|---|---|
| AZ1 (USP28 Inhibitor) | Small molecule inhibitor that promotes SOX9 degradation; can be tested for radiosensitization. | Selleck Chemicals, S8904 [9] |
| SOX9 siRNA/sgRNA | For genetic knockdown/knockout of SOX9 to validate its role in radioresistance in vitro and in vivo. | Custom design or commercial libraries [1] |
| Anti-SOX9 Antibody | For detecting SOX9 protein levels by Western Blot or immunohistochemistry post-radiation. | Sigma-Aldrich, AB5535 [9] |
| Anti-γH2AX Antibody | Marker for DNA double-strand breaks; used to quantify radiation-induced DNA damage. | Abcam, ab81299 [9] |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating SOX9 Pathway Inhibition
| Category | Reagent | Brief Function/Explanation |
|---|---|---|
| Inhibition Tools | USP28 Inhibitor (AZ1) | Pharmacologically destabilizes SOX9 protein by blocking its deubiquitination [9]. |
| SOX9-targeting siRNA/sgRNA | Enables genetic knockdown or knockout of SOX9 to study its function and therapeutic necessity [1]. | |
| Detection & Validation | Anti-SOX9 Antibody | Essential for monitoring SOX9 expression and protein levels via Western Blot, IF, or IHC [9]. |
| Anti-γH2AX Antibody | Critical biomarker for quantifying DNA damage in response to combination therapy [9]. | |
| Cell Models | Patient-Derived Organoids | Physiologically relevant models for testing combination therapies in a context that preserves tumor microenvironment interactions [21]. |
| Therapy-Resistant Cell Lines | Isogenic cell lines with acquired resistance (e.g., SKOV3/Ola) are vital for studying resistance mechanisms [9]. |
Advanced Experimental Protocols
Protocol: Validating SOX9-Mediated Radiosensitization In Vitro
Aim: To determine if pharmacological inhibition of SOX9 enhances the cytotoxicity of radiotherapy in cancer cells.
Materials:
- Cancer cell line of interest (e.g., osteosarcoma, ovarian cancer)
- USP28 inhibitor (e.g., AZ1 from Selleckchem, #S8904)
- Radiation source (e.g., X-ray irradiator)
- Annexin V/PI apoptosis detection kit
- Anti-SOX9 and anti-γH2AX antibodies
Method:
- Cell Pretreatment: Seed cells and allow to adhere. Pre-treat cells with a determined IC₁₀-IC₂₀ concentration of AZ1 (e.g., 5 µM) or vehicle control (DMSO) for 24 hours.
- Radiation Treatment: Subject cells to a range of radiation doses (e.g., 2, 4, 6, 8 Gy).
- Post-Irradiation Incubation: Replace the medium (with or without AZ1) and incubate cells for 24-72 hours.
- Downstream Analysis:
- Clonogenic Survival Assay: Re-seed a known number of cells after irradiation and allow them to form colonies for 7-14 days. Fix, stain with crystal violet, and count colonies to assess long-term survival and reproductive death.
- Apoptosis Assay: Harvest cells 48 hours post-irradiation and analyze by flow cytometry using Annexin V/PI staining to quantify early and late apoptosis.
- DNA Damage Analysis: Perform immunofluorescence staining for γH2AX foci 2-4 hours post-irradiation to quantify persistent DNA double-strand breaks.
- SOX9 Level Confirmation: Harvest protein lysates post-treatment and confirm SOX9 downregulation by Western Blot.
Diagram: In vitro workflow for validating SOX9-mediated radiosensitization. Key steps include pretreatment with an inhibitor, irradiation, and multiple downstream readouts.
Frequently Asked Questions (FAQs) & Troubleshooting Guide
This section addresses common challenges researchers encounter when developing and validating SOX9 as a predictive biomarker for therapy resistance.
FAQ 1: What are the primary molecular mechanisms by which SOX9 confers therapy resistance?
- Answer: SOX9 drives treatment resistance through several established mechanisms. You should investigate these pathways in your model system:
- Stemness and Transcriptional Reprogramming: SOX9 reprograms the transcriptional state of cancer cells into a stem-like, drug-tolerant state. In high-grade serous ovarian cancer (HGSOC), SOX9 expression is sufficient to induce a stem-like population and significant platinum resistance [1].
- Enhanced DNA Damage Repair (DDR): SOX9 directly binds to the promoters of key DDR genes (e.g.,
SMARCA4,UIMC1,SLX4) to enhance repair capabilities. In ovarian cancer, the deubiquitinase USP28 stabilizes SOX9 protein, which in turn promotes resistance to PARP inhibitors by enhancing DDR [9]. - Activation of Pro-Survival Pathways: SOX9 can upregulate the ERBB signaling pathway and interact with pathways like TGF-β and Wnt/β-catenin to promote tumor cell survival and proliferation [16] [21].
- Immune Evasion: SOX9 helps latent cancer cells remain dormant in secondary sites and avoid immune surveillance under immunotolerant conditions [16].
FAQ 2: Our IHC results for SOX9 are inconsistent. What are the best practices for detecting SOX9 in formalin-fixed, paraffin-embedded (FFPE) tissue?
- Answer: Inconsistent immunohistochemistry (IHC) often stems from pre-analytical and analytical variables. Follow this protocol for reliable results:
- Antigen Retrieval: Use a citrate-based (pH 6.0) or EDTA-based (pH 9.0) retrieval buffer. The exact buffer and heating time (e.g., 20-30 minutes in a water bath or pressure cooker) should be optimized for your specific antibody and tissue type.
- Primary Antibody Incubation: Use a validated anti-SOX9 rabbit monoclonal antibody. Incubate at a recommended dilution (e.g., 1:200 to 1:500) overnight at 4°C. Always include both positive and negative control tissues on the same slide.
- Validation and Troubleshooting:
- Problem: High background. Solution: Titrate the primary antibody concentration and optimize the blocking step (e.g., use 5% normal goat serum for 1 hour).
- Problem: No signal. Solution: Confirm antigen retrieval efficacy and antibody activity. Validate your protocol in a cell line with known SOX9 expression (e.g., by Western blot).
- Problem: Nuclear and cytoplasmic staining. Solution: SOX9 is primarily a nuclear protein. Strong cytoplasmic staining may indicate non-specific binding; ensure antibody specificity using a knockout cell line or siRNA-mediated knockdown as a control.
FAQ 3: How can we functionally validate that SOX9 is directly responsible for resistance in our models?
- Answer: Beyond correlative expression studies, functional validation is crucial. Employ a combination of genetic and pharmacological approaches:
- Genetic Knockdown/Knockout: Use CRISPR/Cas9 or specific shRNAs to knockout/knockdown SOX9 in your resistant cell lines. A successful knockout should lead to increased sensitivity to the therapeutic agent, as demonstrated in HGSOC models where SOX9 ablation increased platinum sensitivity [1].
- Forced Overexpression: Overexpress SOX9 in a sensitive parent cell line. This should be sufficient to induce a resistant phenotype, confirming its functional role [1].
- Pharmacological Inhibition: If available, use inhibitors that target the SOX9 pathway. For instance, targeting its stabilizer (e.g., the USP28 inhibitor AZ1) can reduce SOX9 protein levels and re-sensitize cells to treatment [9].
- Rescue Experiments: Re-introduce SOX9 in knockout cells to confirm the reversal of the sensitive phenotype.
FAQ 4: What is the most reliable method to quantify SOX9 expression levels for prognostic stratification?
- Answer: The choice of method depends on your sample type and required precision.
- For Tissue Sections: Quantitative IHC (qIHC) using digital pathology platforms and image analysis software (e.g., QuPath, Halo) to calculate an H-score, which integrates the intensity and percentage of positive nuclei.
- For RNA Analysis: Droplet digital PCR (ddPCR) is highly recommended for absolute quantification of
SOX9mRNA from patient samples due to its superior sensitivity and precision compared to standard qRT-PCR, especially for detecting moderate expression changes [32]. - For High-Throughput Analysis: RNA-Sequencing (RNA-Seq) from bulk or single-cell preparations provides the most comprehensive data, allowing for correlation with genome-wide expression profiles [1].
Detailed Experimental Protocols
Protocol 1: Generating a SOX9 Knockout Model Using CRISPR/Cas9
This protocol details the creation of a SOX9 knockout cell line to study its role in therapy resistance [1].
Key Research Reagent Solutions:
| Reagent/Material | Function in the Protocol |
|---|---|
| SOX9-targeting sgRNA | Guides the Cas9 nuclease to the SOX9 genomic locus for a double-strand break. |
| Non-targeting control sgRNA | Control for non-specific effects of the CRISPR system. |
| Cas9 plasmid or ribonucleoprotein (RNP) complex | The nuclease enzyme that performs the DNA cleavage. |
| Lipofectamine CRISPRMAX | Transfection reagent for delivering ribonucleoprotein complexes into cells. |
| Puromycin | Antibiotic for selecting successfully transfected cells (if using a plasmid with a puromycin resistance gene). |
| T7 Endonuclease I or Surveyor Assay | Detects CRISPR-induced insertions/deletions (indels) at the target site. |
Methodology:
- sgRNA Design: Design and synthesize a sgRNA targeting an early exon of the human
SOX9gene. A non-targeting sgRNA should be used as a control. - Complex Formation: Complex the sgRNA with the Cas9 enzyme to form a ribonucleoprotein (RNP) complex according to the manufacturer's instructions.
- Cell Transfection: Transfect the RNP complex into your target cancer cell line (e.g., an ovarian or breast cancer line) using a transfection reagent like Lipofectamine CRISPRMAX.
- Selection and Cloning: 48 hours post-transfection, select cells with puromycin (if applicable) for 3-5 days. Then, single-cell clone the population by limiting dilution to isolate pure knockout clones.
- Validation:
- Genotypic: Extract genomic DNA from clones and amplify the targeted region by PCR. Analyze the PCR product using the T7 Endonuclease I assay or by Sanger sequencing to confirm indels.
- Phenotypic: Validate knockout at the protein level via Western blotting using an anti-SOX9 antibody. Functionally validate by treating the knockout and control cells with a chemotherapeutic agent (e.g., carboplatin) and performing a colony formation assay to confirm increased sensitivity [1].
Protocol 2: Assessing SOX9-Mediated Chemoresistance via Colony Formation Assay
This is a gold-standard functional assay to quantify the impact of SOX9 on cell survival post-treatment [1].
Methodology:
- Seed Cells: Seed SOX9 knockout and control cells in 6-well plates at a low density (e.g., 500-1000 cells/well, depending on the cell line's growth rate). Use triplicates for each condition.
- Treat with Chemotherapy: 24 hours after seeding, treat the cells with a range of concentrations of the chemotherapeutic drug (e.g., carboplatin, olaparib) or a vehicle control. The treatment duration should be 48-72 hours.
- Drug Removal and Recovery: After treatment, carefully remove the drug-containing medium, wash the cells with PBS, and add fresh culture medium.
- Incubate for Colony Formation: Allow the cells to grow for 1-3 weeks until visible colonies (typically >50 cells) form in the control wells. Do not disturb the plates during this period.
- Fix and Stain: Once colonies are formed, aspirate the medium, gently wash with PBS, and fix the colonies with 4% paraformaldehyde for 15-20 minutes. Then, stain with a 0.5% crystal violet solution for 30 minutes.
- Quantify: Rinse the plates with water, air-dry, and count the colonies manually or using automated colony-counting software. The results can be plotted as survival fractions to demonstrate that SOX9 knockout cells form significantly fewer colonies after treatment compared to controls [1].
Table 1: Association Between SOX9 Expression and Clinical Outcomes Across Cancers
This table synthesizes key clinical correlations of SOX9, informing its potential as a prognostic and predictive biomarker.
| Cancer Type | Association with SOX9 Expression | Clinical Outcome / Resistance Association | Citation |
|---|---|---|---|
| High-Grade Serous Ovarian Cancer (HGSOC) | Upregulated after platinum-based chemotherapy | Shorter overall survival; Drives platinum resistance | [1] |
| Breast Cancer | Frequently overexpressed | Associated with basal-like subtype, proliferation, metastasis, and endocrine therapy resistance | [16] [33] |
| Glioblastoma | Highly expressed | Prognostic value is context-dependent; may be associated with better prognosis in specific subgroups (e.g., lymphoid invasion) | [18] |
| Pancreatic Cancer | Upregulated | Promotes invasiveness of cancer stem cells (CSCs) and tumorigenesis | [21] [33] |
| Hepatocellular Carcinoma | Upregulated | Necessary for tumor initiation, self-renewal, and tumorigenicity in CSCs | [21] |
Table 2: Key Signaling Pathways and Effectors in SOX9-Mediated Resistance
This table summarizes the molecular players involved in SOX9-driven resistance, highlighting potential co-targets.
| Pathway / Mechanism | Key Effectors / Targets | Functional Outcome in Resistance | Citation |
|---|---|---|---|
| Stemness & Reprogramming | SOX9 (as a pioneer factor) | Induces a stem-like, drug-tolerant transcriptional state | [1] |
| DNA Damage Repair | SMARCA4, UIMC1, SLX4 | Enhances repair of therapy-induced DNA damage, leading to PARPi resistance | [9] |
| Protein Stabilization | USP28, FBXW7 | USP28 inhibits FBXW7-mediated degradation of SOX9, increasing its stability and pro-resistance activity | [9] |
| Kinase Signaling | AKT, SOX10 | SOX9 is an AKT substrate and regulates SOX10 to accelerate AKT-dependent tumor growth | [16] |
Pathway and Workflow Visualizations
SOX9 Drives Therapy Resistance
SOX9 Functional Validation Workflow
The Scientist's Toolkit: Essential Research Reagents
This table lists key reagents and their applications for studying SOX9 in the context of therapy resistance.
| Research Reagent | Specific Example / Catalog Number | Primary Function in SOX9 Research |
|---|---|---|
| Validated Antibodies | Anti-SOX9 (AB5535, Sigma) | Detection of SOX9 protein expression via IHC, Western Blot, and immunofluorescence. |
| CRISPR Reagents | SOX9-targeting sgRNA (e.g., Hs. SOX9 sgRNA) | Genetic knockout of SOX9 to establish causal roles in functional assays. |
| Expression Vectors | pCMV-Flag-SOX9 plasmid | Forced overexpression of SOX9 to validate its sufficiency in driving resistance. |
| Pharmacological Inhibitors | USP28 Inhibitor (AZ1) | Targets SOX9 stability; used to demonstrate that SOX9 degradation re-sensitizes cells to therapy [9]. |
| qPCR/ddPCR Assays | Hs_SOX9 ddPCR Probe Assay | Absolute quantification of SOX9 mRNA expression levels from patient samples or cell lines. |
Navigating Challenges in Targeting the SOX9 Pathway
Addressing Tumor Heterogeneity and Adaptive Resistance Mechanisms
Troubleshooting Guide: Overcoming SOX9-Mediated Therapy Resistance
This guide addresses common experimental challenges in cancer research related to the transcription factor SOX9, a key driver of therapy resistance across multiple cancer types.
FAQ 1: Why do our ovarian cancer cell models develop resistance to platinum-based chemotherapy, and what role does SOX9 play?
- Problem: Acquired chemoresistance in high-grade serous ovarian cancer (HGSOC) models following initial treatment response.
- Root Cause: The transcription factor SOX9 is epigenetically upregulated in response to chemotherapy. This reprogramming drives a stem-like transcriptional state, creating drug-tolerant persister cells [1] [2].
- Solution & Experimental Validation:
- Monitor SOX9 Dynamics: Use single-cell RNA sequencing (scRNA-seq) on patient samples pre- and post-neoadjuvant chemotherapy (NACT) to confirm SOX9 upregulation is a consistent early response. One study found SOX9 expression significantly increased in post-NACT tissues in 8 of 11 patients [1].
- Functional Validation: Perform CRISPR/Cas9-mediated knockout of SOX9. In HGSOC lines, this knockout significantly increases sensitivity to carboplatin, as measured by colony formation assays [1].
FAQ 2: How does SOX9 contribute to resistance beyond ovarian cancer, such as in PARP inhibitor resistance?
- Problem: Resistance to PARP inhibitors (PARPi) like olaparib in ovarian cancer.
- Root Cause: Elevated SOX9 expression contributes to olaparib resistance. The deubiquitinating enzyme USP28 stabilizes the SOX9 protein by inhibiting its FBXW7-mediated degradation. Stable SOX9 then binds to promoters of DNA damage repair (DDR) genes, enhancing DDR and fostering resistance [9].
- Solution & Experimental Protocol:
- Co-Immunoprecipitation (Co-IP): Confirm the USP28-SOX9 interaction. Lysate cells (e.g., SKOV3, UWB1.289) in RIPA buffer with protease inhibitors. Incubate 800 μg of cellular extract with SOX9 or control IgG antibodies overnight, followed by protein A/G magnetic beads. Analyze bound complexes by western blot [9].
- Target the Axis: Treat cells with the specific USP28 inhibitor AZ1. This promotes SOX9 ubiquitination and degradation, impairs DDR, and re-sensitizes cells to PARPi [9].
FAQ 3: Our bulk sequencing data is inconsistent. Could intratumoral heterogeneity and pre-existing SOX9+ subpopulations be the cause?
- Problem: Inconsistent molecular profiling results and variable initial treatment response.
- Root Cause: Intratumoral heterogeneity leads to pre-existing subclones with different genetic and phenotypic profiles. A rare cluster of SOX9-expressing cells with inherent stem-like and drug-tolerant properties can survive initial therapy and eventually dominate the resistant tumor [34] [1].
- Solution:
- Employ Single-Cell Technologies: Use scRNA-seq to identify and characterize rare SOX9+ subpopulations in treatment-naive tumors. These cells are highly enriched for cancer stem cell (CSC) markers and chemoresistance-associated gene modules [1].
- Measure Transcriptional Divergence: Use the P50/P50 metric (the sum of expression of the top 50% of genes divided by the bottom 50%) as a proxy for transcriptional plasticity and stemness, which is elevated in SOX9-high cells [1].
Table 1: Key Experimental Findings on SOX9-Mediated Resistance
| Finding | Experimental System | Quantitative Outcome | Significance |
|---|---|---|---|
| SOX9 KO increases platinum sensitivity [1] | HGSOC cell lines (OVCAR4, Kuramochi, COV362) with CRISPR/Cas9 KO | Significant increase in sensitivity to carboplatin (2-tailed Student's t-test, p = 0.0025) | Establishes causal role of SOX9 in chemoresistance. |
| SOX9 induction post-chemotherapy [1] | scRNA-seq of 11 HGSOC patient tumors (8,806 epithelial cells) | SOX9 significantly increased post-NACT (Wilcoxon's paired p = 0.032) | Confirms SOX9 upregulation is a clinically relevant response. |
| SOX9 as a prognostic marker [1] | Integrated microarray database (n=520 patients) | Shorter overall survival for top SOX9 quartile (HR = 1.33; log-rank p = 0.017) | Links high SOX9 expression to worse patient outcomes. |
| USP28 inhibition sensitizes to PARPi [9] | Ovarian cancer cell lines (SKOV3, UWB1.289) | AZ1 (USP28 inhibitor) reduces SOX9 stability and increases olaparib sensitivity. | Identifies a potential therapeutic strategy to overcome PARPi resistance. |
Essential Signaling Pathways and Workflows
SOX9 Stabilization and Resistance Mechanism
Experimental Workflow for SOX9 Functional Analysis
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Investigating SOX9-Mediated Resistance
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| CRISPR/Cas9 System | Genetic knockout or activation of SOX9. | Establishing causal relationship between SOX9 ablation and restored drug sensitivity [1]. |
| USP28 Inhibitor (AZ1) | Specific small molecule inhibitor of USP28. | Promoting SOX9 degradation to sensitize ovarian cancer cells to PARP inhibitors [9]. |
| SOX9 Antibodies | Detection of SOX9 protein levels via Western Blot, IF, IHC. | Quantifying SOX9 upregulation in response to chemotherapy in vitro and in patient samples [9] [1]. |
| PARP Inhibitor (Olaparib) | Inducer and tool for studying PARPi resistance. | Generating and studying resistant cell line models (e.g., SKOV3/Ola) [9]. |
| Co-IP Kits & Reagents | Protein-protein interaction studies. | Validating novel SOX9 interaction partners (e.g., USP28) [9]. |
| Single-Cell RNA-Seq Kits | Profiling transcriptional heterogeneity. | Identifying rare SOX9+ stem-like subpopulations in naive and treated tumors [1] [35]. |
Optimizing Delivery Systems for Nucleic Acid-Based SOX9 Therapies
Frequently Asked Questions (FAQs)
Q1: Why is SOX9 a significant target in cancer therapy? SOX9 is a transcription factor that is epigenetically upregulated in response to chemotherapy. It drives chemoresistance by reprogramming cancer cells into a stem-like, drug-tolerant state. Targeting SOX9 can potentially reverse this resistance and improve patient outcomes [1] [10].
Q2: What types of nucleic acid therapeutics can be used to target SOX9? The main classes are Antisense Oligonucleotides (ASOs) and small interfering RNAs (siRNAs). ASOs are single-stranded oligonucleotides that can inhibit SOX9 expression via RNase H1-dependent cleavage or steric hindrance. siRNAs are double-stranded RNAs that silence gene expression through the RNA interference (RNAi) pathway [36].
Q3: What is a major challenge in delivering SOX9-targeted nucleic acid therapies? A primary challenge is the efficient and safe delivery of these therapeutics to the target cells. Naked nucleic acids are unstable and susceptible to degradation by nucleases. Furthermore, they exhibit poor cellular uptake and require delivery systems to protect the payload and facilitate intracellular release [36].
Q4: What delivery systems are available for nucleic acid-based SOX9 therapies? Lipid Nanoparticles (LNPs) are a leading platform. They encapsulate nucleic acids, protect them from degradation, enhance cellular internalization, and promote endosomal escape for efficient cytoplasmic release [36] [37]. Other delivery platforms include viral vectors and ligand-conjugated approaches [36].
Q5: What are some key considerations when formulating Lipid Nanoparticles (LNPs)? Formulation is critical. The molar ratios of ionizable lipid, cholesterol, helper phospholipid, and PEG-lipid must be systematically optimized. This affects encapsulation efficiency, stability, and delivery efficacy. For instance, varying the ionizable lipid (e.g., SM-102) ratio from 40% to 60% can significantly impact performance [37].
Troubleshooting Guides
Issues with In Vitro Gene Silencing Efficiency
Problem: Low knockdown of SOX9 mRNA or protein in cell culture models.
| Possible Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Inefficient Transfection | Check nucleic acid encapsulation efficiency and particle size of LNP. | Optimize LNP formulation; use a validated positive control (e.g., siRNA against a housekeeping gene); increase transfection reagent concentration or use an alternative reagent [37]. |
| Poor Oligonucleotide Design | Use bioinformatics tools to check target accessibility and specificity. | Redesign ASO/siRNA sequence to target an accessible site on the SOX9 mRNA; include appropriate chemical modifications (e.g., 2'-O-methyl, phosphorothioate) to enhance stability and binding affinity [36]. |
| Insufficient Assay Sensitivity | Validate detection assay with a known control. | Use more sensitive detection methods like qRT-PCR with TaqMan probes or RNAscope for in situ hybridization to confirm SOX9 downregulation [38]. |
Issues with Lipid Nanoparticle (LNP) Formulation and Characterization
Problem: Low encapsulation efficiency, unstable particle size, or high polydispersity.
| Possible Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Suboptimal Lipid Ratios | Characterize LNP physicochemical properties (size, PDI, zeta potential). | Systematically screen lipid compositions. A representative optimized LNP for mRNA delivery contained SM-102 (ionizable lipid), cholesterol, DSPC, and DMG-PEG2000 in a 50:38.5:10:1.5 molar ratio [37]. |
| Impurities or Old Reagents | Check reagent expiration dates and storage conditions. | Use fresh, high-purity reagents; store ionizable lipids and PEG-lipids at -20°C protected from light and moisture [37]. |
| Inconsistent Mixing Process | Standardize the mixing speed, time, and buffer conditions. | Ensure rapid and reproducible mixing using microfluidics or T-tube apparatus; maintain a fixed total flow rate and aqueous-to-organic volume ratio [37]. |
Issues with In Vivo Efficacy and Toxicity
Problem: Lack of therapeutic effect or signs of toxicity in animal models.
| Possible Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Rapid Clearance & Off-Targeting | Track fluorescently labeled LNPs to analyze biodistribution. | Functionalize LNPs with targeting ligands (e.g., antibodies, peptides) specific to tumor-associated antigens; adjust PEG-lipid content to balance circulation time and cellular uptake [36]. |
| Immune Activation | Measure plasma cytokine levels (e.g., IFN-α, IL-6). | Use highly purified nucleic acids; incorporate modified nucleotides (e.g., pseudouridine) to reduce immunogenicity [36]. |
| Inefficient Tissue Penetration | Analyze LNP distribution in tumor sections. | Explore local delivery routes (e.g., intra-tumoral injection) if applicable; optimize particle size (typically 50-150 nm) for enhanced tumor penetration via the EPR effect [36]. |
Table 1: Key Physicochemical Properties of Optimized LNPs for Nucleic Acid Delivery
| Property | Target Value | Measurement Technique | Significance |
|---|---|---|---|
| Particle Size | 80 - 150 nm | Dynamic Light Scattering (DLS) | Influences biodistribution, tumor penetration, and cellular uptake [37]. |
| Polydispersity Index (PDI) | < 0.2 | Dynamic Light Scattering (DLS) | Indicates a homogeneous, monodisperse particle population for reproducible behavior [37]. |
| Zeta Potential | Near Neutral (Slightly Negative) | Laser Doppler Electrophoresis | Reduces non-specific interactions with serum proteins and cell membranes, improving circulation time [37]. |
| Encapsulation Efficiency | > 90% | Ribogreen Assay | Maximizes the amount of delivered therapeutic payload and minimizes waste/toxicity [37]. |
Table 2: Validated Oligonucleotide Sequences for SOX9 Targeting (Literature Examples)
| Therapeutic Type | Target Gene | Sequence / Identifier (if published) | Key Modifications | Reported Efficacy (In Vitro/In Vivo) |
|---|---|---|---|---|
| siRNA | SOX9 | Specific sequence not detailed in results | Not specified | Significant reduction in SOX9 protein; increased carboplatin sensitivity in HGSOC cell lines [1]. |
| ASO | SOX9 | Specific sequence not detailed in results | Not specified | Demonstrated efficient gene silencing; potential for "gapmer" design with phosphorothioate backbone and 2'-O-methyl RNA wings [36]. |
Experimental Protocols
Protocol: Formulating and Characterizing LNPs for siRNA/mRNA Delivery
This protocol is adapted from optimized methods for LNP preparation [37].
Materials:
- Ionizable lipid (e.g., SM-102)
- Cholesterol
- Helper phospholipid (e.g., DSPC)
- PEG-lipid (e.g., DMG-PEG2000)
- Nucleic acid (siRNA or mRNA) in sodium acetate buffer, pH 4.0
- Ethanol
- Microfluidic device or T-tube apparatus
- Dialysis cassettes (MWCO 10-20 kDa)
Method:
- Lipid Stock Solution Preparation: Dissolve the ionizable lipid, cholesterol, DSPC, and DMG-PEG2000 in ethanol at a molar ratio of 50:38.5:10:1.5.
- Aqueous Phase Preparation: Dilute the nucleic acid (siRNA or mRNA) in 25 mM sodium acetate buffer, pH 4.0.
- Nanoparticle Formation: Using a microfluidic device, rapidly mix the ethanolic lipid solution with the aqueous nucleic acid solution at a fixed flow rate (e.g., 1:3 volumetric ratio of lipid to aqueous phase) and a total flow rate of 12 mL/min.
- Dialyze: Immediately transfer the formed LNP suspension to a dialysis cassette and dialyze against a large volume of PBS (pH 7.4) for at least 4 hours at 4°C to remove ethanol and exchange the buffer.
- Sterile Filtration: Filter the final LNP formulation through a 0.22 µm sterile filter.
- Characterization: Measure particle size, PDI, and zeta potential using DLS. Determine encapsulation efficiency using a Ribogreen assay.
Protocol: Validating SOX9 Knockdown Using RNAscope In Situ Hybridization
This protocol follows the manufacturer's guidelines for sensitive RNA detection [38].
Materials:
- RNAscope Kit (e.g., 2.5 HD Reagent Kit)
- SOX9-specific target probes
- Positive control probe (e.g., PPIB)
- Negative control probe (e.g., dapB)
- Formalin-fixed, paraffin-embedded (FFPE) tissue sections
- HybEZ Hybridization System
Method:
- Sample Preparation: Bake FFPE tissue sections at 60°C for 1 hour. Deparaffinize and rehydrate through xylene and ethanol series.
- Pretreatment: Perform heat-induced epitope retrieval and protease treatment according to the kit's instructions to permeabilize the tissue.
- Hybridization: Apply the SOX9 target probes to the sample and incubate at 40°C for 2 hours in the HybEZ oven. Include positive and negative control probes on adjacent sections.
- Amplification and Detection: Perform the sequential amplifier and label probe incubations as per the kit's protocol to achieve signal amplification.
- Counterstaining and Mounting: Counterstain with Gill's Hematoxylin I (diluted 1:2) and mount with EcoMount or PERTEX mounting media.
- Imaging and Scoring: Image slides under a microscope. Score staining semi-quantitatively based on dots per cell:
- Score 0: <1 dot/10 cells
- Score 1: 1-3 dots/cell
- Score 2: 4-9 dots/cell
- Score 3: 10-15 dots/cell
- Score 4: >15 dots/cell with >10% dot clusters [38]
Signaling Pathway and Experimental Workflow
Research Reagent Solutions
Table 3: Essential Reagents for Nucleic Acid-Based SOX9 Therapy Development
| Reagent / Material | Function / Application | Example Product / Specification |
|---|---|---|
| Ionizable Cationic Lipid | Core component of LNPs; encapsulates nucleic acid and facilitates endosomal escape. | SM-102 [37] |
| PEG-Lipid | Stabilizes LNP formulation, reduces aggregation, and modulates pharmacokinetics. | DMG-PEG2000 [37] |
| SOX9-targeting Oligonucleotide | The active pharmaceutical ingredient that silences the SOX9 gene. | Custom-designed ASO or siRNA with chemical modifications (e.g., 2'-O-methyl, phosphorothioate) [36]. |
| RNAscope Assay Kit | Highly sensitive and specific in situ hybridization for visualizing SOX9 mRNA in tissue samples. | RNAscope 2.5 HD Reagent Kit; used with SOX9-specific target probes and control probes (PPIB, dapB) [38]. |
| Fluorometric Quantification Kit | Accurate and specific quantification of nucleic acid concentration, unaffected by contaminants. | Qubit RNA HS Assay Kit; essential for measuring RNA integrity and concentration during LNP formulation and quality control [39]. |
FAQs: SOX9 in Cancer and Tissue Homeostasis
What is the central "dual role" or "double-edged sword" nature of SOX9? SOX9 plays a complex and dual role in physiology and pathology. On one hand, it is crucial for normal tissue regeneration and repair, such as in cartilage formation and maintenance of stem cell populations. On the other hand, it is frequently overexpressed in various cancers, where it promotes tumor progression, stemness, and resistance to therapies, making it a potential therapeutic target [15] [33].
How does SOX9 contribute to therapy resistance in cancer? SOX9 drives resistance to multiple cancer treatments through several mechanisms. It can reprogram cancer cells into a stem-like, drug-tolerant state [1] [2]. It enhances DNA damage repair capabilities, contributing to resistance to PARP inhibitors and platinum-based chemotherapy [9]. It is also implicated in radioresistance in gastrointestinal cancers [21].
Why is targeting SOX9 for cancer therapy challenging? The primary challenge is balancing efficacy and toxicity. Inhibiting SOX9 to sensitize tumors to therapy may simultaneously impair its vital functions in normal tissue repair and stem cell maintenance. For example, SOX9 is essential for the regeneration of intestinal crypts after radiation injury; thus, its inhibition could exacerbate side effects like enteritis during radiotherapy [21].
What are the key regulatory mechanisms of SOX9 protein stability? The deubiquitinating enzyme USP28 is a key regulator that stabilizes the SOX9 protein by inhibiting its ubiquitination and subsequent degradation, which is mediated by the E3 ubiquitin ligase FBXW7. This stabilization promotes DNA damage repair and therapy resistance in ovarian cancer [9].
Does SOX9 interact with other major signaling pathways in cancer? Yes, SOX9 has extensive cross-regulation with major pathways. A well-documented interaction is with the canonical Wnt/β-catenin pathway. SOX9 can antagonize Wnt signaling by promoting the degradation of β-catenin and competing with TCF/LEF transcription factors. Conversely, Wnt signaling can also influence SOX9 expression, forming a subtle balance that controls cell fate [40].
Troubleshooting Guides
Problem: Inconsistent SOX9 Expression in Cell Models
Potential Cause 1: Epigenetic Plasticity SOX9 expression is subject to dynamic epigenetic regulation, including through super-enhancers, which can lead to heterogeneity in cell populations [1].
- Solution: Use single-cell RNA sequencing to characterize the presence of rare, high-SOX9 expressing subpopulations. Treat cells with epigenetic modulators to assess the stability of SOX9 expression.
Potential Cause 2: Post-translational Regulation SOX9 protein stability is regulated by ubiquitination. Inconsistent levels may be due to variable activity of stabilizing (e.g., USP28) or degrading (e.g., FBXW7) enzymes [9].
- Solution:
- Treat cells with a proteasome inhibitor (e.g., MG132). If SOX9 levels increase, protein turnover is a key factor.
- Modulate the USP28-FBXW7 axis. Use the USP28-specific inhibitor AZ1 to promote SOX9 degradation or overexpress FBXW7.
- Monitor protein half-life with cycloheximide chase assays.
Problem: Off-Target Toxicity in SOX9-Targeting Strategies
Potential Cause: Impairment of Physiological Repair Inhibiting SOX9 can disrupt its normal role in maintaining reserve stem cells and supporting tissue regeneration, such as in the intestine [21].
- Solution:
- Tissue-Specific Delivery: Develop nanocarrier systems conjugated with ligands that target cancer stem cells to deliver SOX9 inhibitors specifically to tumors.
- Temporal Control: For radiotherapy, consider administering SOX9 inducers to normal intestinal tissue after high-dose radiation is complete to promote crypt repair and regeneration, while using inhibitors concurrently with radiation to sensitize tumors [21].
- Inducible Systems: In regenerative medicine, use inducible gene expression systems (e.g., Tet-Off) to achieve transient, controlled SOX9 expression, mitigating long-term oncogenic risks [41].
Problem: Investigating SOX9-Mediated Chemoresistance
Potential Cause: SOX9-Driven Transcriptional Reprogramming Chemotherapy induces SOX9, which acts as a master regulator to drive a stem-like transcriptional state, leading to a drug-tolerant population [1] [2].
- Solution:
- Modeling: Generate chemoresistant cell lines by chronic, low-dose drug exposure and confirm SOX9 upregulation.
- Functional Validation: Use CRISPR/Cas9 to knockout SOX9 and perform colony formation assays to confirm increased drug sensitivity. Conversely, epigenetically upregulate SOX9 to demonstrate its sufficiency in inducing resistance.
- Mechanistic Studies: Employ ChIP-seq to identify SOX9 binding sites on promoters of DNA damage repair genes (e.g., SMARCA4, UIMC1, SLX4). Use RNA-seq to analyze the resulting transcriptional divergence and stemness signatures [1] [9].
Key Data Tables
Table 1: SOX9 in Therapy Resistance Across Cancers
| Cancer Type | Therapy | Mechanism of SOX9-Mediated Resistance | Key Experimental Evidence |
|---|---|---|---|
| High-Grade Serous Ovarian Cancer [1] [2] | Platinum-based Chemotherapy | Reprograms cancer cells into a stem-like, chemoresistant state; increases transcriptional divergence. | Bulk & single-cell RNA-seq; SOX9 KO increases sensitivity; SOX9 induction is sufficient for resistance. |
| Ovarian Cancer [9] | PARP Inhibitors (e.g., Olaparib) | Enhances DNA damage repair by binding promoters of DDR genes (SMARCA4, UIMC1, SLX4). | ChIP-seq; USP28 inhibition destabilizes SOX9 and re-sensitizes cells. |
| Gastrointestinal Cancer [21] | Radiotherapy | Maintains population of radioresistant reserve intestinal stem cells (rISCs). | SOX9 knockout crypts undergo apoptosis post-radiation; lack regeneration. |
| Various Cancers (e.g., Lung, Breast) [33] | Diverse Chemotherapies & Targeted Therapies | Regulation of drug efflux pumps (ABCB1, ABCG2), anti-apoptotic pathways, and ALDH1A3. | Correlation of high SOX9 with poor prognosis; in vitro models of resistance. |
Table 2: Research Reagent Solutions for SOX9 Studies
| Reagent / Tool | Function / Application | Key Consideration / Example |
|---|---|---|
| CRISPR/Cas9 KO/KI | Functional validation; generating stable engineered cell lines (e.g., SOX9 knockout, inducible expression). | AAVS1 "safe harbor" locus for knock-in to minimize off-target effects [41]. |
| USP28 Inhibitor (AZ1) | Promotes FBXW7-mediated ubiquitination and degradation of SOX9 protein. | Re-sensitizes ovarian cancer cells to PARP inhibitors [9]. |
| Tet-Off Inducible System | Allows precise, temporal control of SOX9 (and/or TGFβ1) transgene expression. | Mitigates risks of constitutive overexpression in regenerative applications [41]. |
| Co-Immunoprecipitation (Co-IP) | Identifies novel SOX9 protein interaction partners (e.g., USP28). | Use anti-Flag/HA nanobody magnetic beads to reduce IgG interference in WB [9]. |
| Single-cell RNA Sequencing (scRNA-seq) | Identifies rare, SOX9-high stem-like subpopulations in tumors pre/post-treatment. | Links SOX9 expression to chemoresistance gene modules in patient samples [1]. |
Experimental Protocols
Protocol 1: Assessing SOX9's Role in Chemoresistance Using CRISPR and Colony Formation
Background: This protocol is adapted from studies in ovarian cancer to establish a causal relationship between SOX9 expression and resistance to platinum-based drugs [1].
Methodology:
- Generate SOX9-Knockout Cells: Transduce HGSOC cell lines (e.g., OVCAR4, Kuramochi) with lentivirus expressing Cas9 and SOX9-targeting sgRNA. Use a non-targeting sgRNA as control.
- Verify Knockout: Confirm SOX9 ablation at the protein level via Western Blot using a validated SOX9 antibody.
- Treat with Chemotherapy: Treat parental and SOX9-KO cells with a range of carboplatin concentrations.
- Colony Formation Assay: After treatment, seed a fixed number of viable cells into new dishes and allow them to grow for 1-2 weeks without drug pressure.
- Fix and Stain: Fix cells with methanol or PFA and stain with crystal violet.
- Quantify: Count colonies (>50 cells). Plot survival curves and calculate IC50 values. A significant decrease in IC50 for SOX9-KO cells indicates SOX9-mediated resistance.
Protocol 2: Evaluating SOX9 Protein Stability and the Role of USP28
Background: This protocol is used to investigate post-translational regulation of SOX9, particularly its stabilization by USP28, which contributes to PARPi resistance [9].
Methodology:
- Inhibit Protein Synthesis: Treat ovarian cancer cells (e.g., SKOV3, UWB1.289) with cycloheximide (CHX, e.g., 100 µg/mL) to halt new protein synthesis.
- Apply Proteasome/USP28 Inhibitors: Co-treat cells with either:
- MG132 (proteasome inhibitor) to see if SOX9 is stabilized.
- AZ1 (USP28 inhibitor) to promote its degradation.
- Harvest Cells at Time Points: Collect cell lysates at 0, 1, 2, 4, and 8 hours post-treatment.
- Western Blot Analysis: Probe lysates for SOX9 and a loading control (e.g., β-actin).
- Quantify and Calculate Half-life: Measure band intensity. Plot SOX9 protein levels over time to calculate its half-life under different inhibitor conditions.
Signaling Pathway & Experimental Workflow Diagrams
SOX9 in Therapy Resistance and Repair
USP28-SOX9 Regulatory Axis
Overcoming Compensatory Pathways and Feedback Loops
Frequently Asked Questions (FAQs)
Q1: What are compensatory pathways and feedback loops in the context of SOX9-mediated therapy resistance? Compensatory pathways are alternative signaling routes that cancer cells activate when a primary therapeutic target is blocked. In SOX9-mediated resistance, negative feedback loops within key signaling pathways, when inhibited, can lead to the compensatory over-activation of upstream or parallel survival signals. For instance, suppression of the mTORC1/S6K axis can cause rebound activation of PI3K/Akt and ERK pathways, which can oppose the anti-tumor effects of therapy and promote a resistant state often characterized by SOX9 upregulation [42] [43]. SOX9 itself can be part of a positive feedback loop, such as the MALAT1-miR-101-SOX9 axis in lung cancer, where SOX9 activates the lncRNA MALAT1's transcription, which in turn sponges miR-101 to further elevate SOX9 expression, entrenching the chemoresistant phenotype [44].
Q2: How does SOX9 contribute to therapy resistance in cancer cells? SOX9 promotes therapy resistance through several interconnected mechanisms:
- Stemness and Self-Renewal: SOX9 reprograms cancer cells into stem-like, tumor-initiating cells (TICs) that are inherently more resistant to therapy [2] [45].
- Enhanced DNA Damage Repair: In ovarian cancer, SOX9 binds to the promoters of key DNA damage repair (DDR) genes like
SMARCA4,UIMC1, andSLX4, enhancing the cell's ability to repair therapy-induced DNA lesions and promoting resistance to PARP inhibitors [9]. - Drug Detoxification: SOX9 directly transactivates the gene for ALDH1A1, a key enzyme in the aldehyde dehydrogenase family. ALDH1A1 activity is a marker of cancer stem cells and contributes to chemoresistance by detoxifying chemotherapeutic agents like cisplatin [46].
- Metabolic Adaptation: In the tumor microenvironment, factors like hypoxia can promote chemoresistance by modifying SOX9 through lactylation, linking metabolic reprogramming to the stem-like, resistant state [47].
Q3: What techniques can I use to identify SOX9 upregulation in my resistant cell models? The following table summarizes key experimental approaches for detecting SOX9 upregulation.
| Method | What It Measures | Key Insight from Research |
|---|---|---|
| Western Blot / Immunofluorescence | SOX9 protein expression and cellular localization. | Elevated SOX9 protein is found in chemoresistant lung cancer cells and stem-like/progenitor cell populations [46] [45]. |
| RT-qPCR | SOX9 mRNA transcript levels. | SOX9 mRNA is significantly elevated in NSCLC cells after cisplatin exposure and in tumor samples versus normal tissue [46] [44]. |
| Chromatin Immunoprecipitation (ChIP) | Direct binding of SOX9 to specific DNA target regions. | ChIP-seq and ChIP-PCR validate SOX9 binding to promoters of target genes like ALDH1A1 and DDR genes [46] [9]. |
| Aldefluor Assay | ALDH enzymatic activity, a functional downstream output of SOX9. | SOX9 overexpression increases ALDH+ cell population, a hallmark of stem-like properties and chemoresistance [46] [45]. |
| Single-cell RNA Sequencing (scRNA-seq) | SOX9 expression heterogeneity within a tumor cell population. | Identifies rare clusters of cells with high SOX9 expression and stem-like features in primary patient tumors [2]. |
Q4: My ovarian cancer cell lines are developing resistance to PARP inhibitors. Could SOX9 be involved, and how can I test this? Yes, recent evidence directly implicates SOX9 in PARP inhibitor (PARPi) resistance. A 2025 study demonstrated that SOX9 is upregulated in olaparib-resistant ovarian cancer cells and promotes resistance by enhancing DNA damage repair [9].
- Diagnostic Experiments:
- Verify SOX9 Expression: Compare SOX9 protein and mRNA levels between your parental and PARPi-resistant lines via Western blot and RT-qPCR.
- Functional Genetic Screens: Use CRISPR/Cas9 to knockout (KO)
SOX9or siRNA to knock it down (KD) in your resistant line. A successful KO/KD should resensitize the cells to PARPi, demonstrated by viability assays (MTT) and clonogenic survival assays. - Assess DNA Repair Efficiency: In your SOX9 KO/KD model, monitor DNA damage repair efficiency. Perform immunofluorescence staining for key DNA damage markers like γH2AX. Softer SOX9 should result in persistent γH2AX foci after PARPi treatment, indicating impaired DDR [9].
Q5: What are the potential therapeutic strategies for overcoming SOX9-mediated resistance? Strategies are emerging that target SOX9 itself, its stability, or its downstream effectors.
- Target SOX9 Protein Stability: The deubiquitinating enzyme USP28 was identified as a key stabilizer of SOX9 protein. The USP28-specific inhibitor AZ1 promotes the degradation of SOX9 and has been shown to sensitize ovarian cancer cells to PARP inhibitors [9].
- Disrupt Transcriptional Networks: Target the positive feedback loops that maintain high SOX9. For example, disrupting the MALAT1-miR-101-SOX9 axis could theoretically break the cycle of SOX9 expression.
- Inhibit Downstream Effectors: Since SOX9 regulates ALDH1A1, targeting ALDH activity could circumvent one major resistance mechanism driven by SOX9 [46].
- Rational Combination Therapy: Given the role of compensatory pathways, combining a primary therapy (e.g., a PARPi or chemotherapy) with an inhibitor of a resistance pathway (e.g., a USP28 inhibitor) presents a promising clinical strategy [42] [9] [43].
Troubleshooting Guides
Problem: Unexpected Cell Survival After Chemotherapy or Targeted Therapy Treatment
Potential Cause: Upregulation of the transcription factor SOX9, leading to acquired therapy resistance through enhanced stemness, DNA repair, or drug detoxification.
Investigation and Solution Workflow: The following diagram outlines a systematic approach to diagnose and target SOX9-mediated resistance.
Step-by-Step Diagnostic Commands:
Confirm SOX9 Upregulation.
- Experiment: Compare SOX9 expression in resistant vs. parental isogenic cell lines.
- Protocol: Western Blot for SOX9.
- Reagents: RIPA Lysis Buffer, Protease Inhibitor Cocktail, BCA Protein Assay Kit, anti-SOX9 antibody (e.g., AB5535 from Sigma-Aldrich), HRP-conjugated secondary antibody.
- Procedure:
- Lyse ~1x10⁶ cells in RIPA buffer with inhibitors.
- Quantify protein concentration using BCA assay.
- Load 20-40 µg of protein per lane on an SDS-PAGE gel (8-15%).
- Transfer to PVDF membrane.
- Block with 5% non-fat milk for 1 hour.
- Incubate with primary anti-SOX9 antibody (dilution per datasheet) overnight at 4°C.
- Incubate with HRP-secondary antibody for 1 hour at room temperature.
- Visualize using ECL detection. Use β-actin as a loading control [46] [9].
Perform Functional Validation.
- Experiment: Knockdown or knockout SOX9 in resistant cells to test for resensitization.
- Protocol: CRISPR/Cas9 KO of SOX9.
- Reagents: SOX9-specific CRISPR guide RNA (gRNA), Cas9 expression plasmid, transfection reagent (e.g., Lipofectamine), puromycin for selection.
- Procedure:
- Design and clone gRNAs targeting critical exons of the
SOX9gene. - Co-transfect the gRNA and Cas9 plasmids into your resistant cell line.
- 48 hours post-transfection, select with puromycin for 1-2 weeks.
- Confirm KO efficiency via Western blot.
- Perform cell viability (MTT) and clonogenic survival assays with the therapeutic agent. Successful KO should show significantly reduced survival and colony formation [2].
- Design and clone gRNAs targeting critical exons of the
Investigate the Mechanism.
- Experiment: Aldefluor Assay to Measure Stem-like Properties.
- Reagents: Aldefluor Kit (contains BAAA substrate and DEA inhibitor).
- Procedure:
- Suspend 1x10⁶ cells in Aldefluor assay buffer.
- Divide the cell suspension into two tubes.
- Add the BAAA substrate to the test tube and an equal volume of the specific ALDH inhibitor (DEAB) to the control tube.
- Incubate at 37°C for 30-60 minutes.
- Analyze by flow cytometry. The ALDH+ population (DEAB-controlled) indicates stem-like cells, which should decrease upon SOX9 knockdown [46] [45].
- Experiment: Aldefluor Assay to Measure Stem-like Properties.
Problem: Inconsistent SOX9 Protein Detection or Rapid Degradation
Potential Cause: SOX9 is regulated by post-translational modifications, notably ubiquitination, which controls its stability.
Solution:
- Stabilize Protein for Detection: Treat cells with a proteasome inhibitor like MG132 (10-20 µM for 4-6 hours) prior to lysis. This prevents ubiquitin-mediated degradation and enhances SOX9 detection in Western blots [9].
- Investigate Regulators of Stability:
- Protocol: Co-Immunoprecipitation (Co-IP) for SOX9 Interactors.
- Reagents: Western and IP Lysis Buffer, anti-SOX9 antibody, protein A/G magnetic beads, control IgG.
- Procedure:
- Lyse cells and pre-clear the lysate.
- Incubate 500-800 µg of lysate with anti-SOX9 antibody or control IgG overnight at 4°C.
- Add protein A/G beads and incubate for 2 hours.
- Wash beads 3-4 times with lysis buffer.
- Elute bound proteins by boiling in SDS loading buffer and analyze by Western blot for potential binding partners like USP28 or FBXW7 [9].
- Protocol: Co-Immunoprecipitation (Co-IP) for SOX9 Interactors.
The Scientist's Toolkit: Research Reagent Solutions
The table below catalogs essential reagents for studying SOX9-mediated resistance, as cited in recent literature.
| Reagent / Tool | Function / Application | Example from Literature |
|---|---|---|
| AZ1 (USP28 Inhibitor) | Small molecule inhibitor that targets USP28, leading to decreased SOX9 protein stability. Used to sensitize cells to PARP inhibitors. [9] | Sensitized ovarian cancer cells to olaparib by promoting SOX9 degradation. [9] |
| Aldefluor Kit | Flow cytometry-based assay to identify and isolate cells with high ALDH activity, a marker for SOX9-driven stem-like properties. [46] [45] | Demonstrated that SOX9 overexpression increases the ALDH+ population in NSCLC and breast cells. [46] [45] |
| Anti-SOX9 Antibody | Detecting SOX9 protein expression via Western Blot, Immunofluorescence, and Immunoprecipitation. | Used to show SOX9 upregulation in cisplatin-resistant lung cancer and PARPi-resistant ovarian cancer. [46] [9] |
| CRISPR/Cas9 System | For generating stable SOX9 knockout cell lines to definitively establish its functional role in resistance. | SOX9 knockout reduced tumor growth and restored tamoxifen sensitivity in breast cancer models. [2] [45] |
| MG132 (Proteasome Inhibitor) | Inhibits the proteasome, stabilizing ubiquitinated proteins like SOX9. Useful for Co-IP experiments and studying protein turnover. [9] | Used to demonstrate that SOX9 degradation is mediated by the ubiquitin-proteasome system. [9] |
| siRNA/shRNA against SOX9 | For transient (siRNA) or stable (shRNA) knockdown of SOX9 expression to assess functional consequences on drug sensitivity. | SOX9 knockdown increased sensitivity to cisplatin, paclitaxel, and etoposide in NSCLC cells. [46] |
Key Signaling Pathways and Molecular Interactions
The diagram below synthesizes the core molecular mechanisms of SOX9-mediated therapy resistance as discussed in the FAQs and guides, highlighting potential therapeutic intervention points.
Strategies for Patient Stratification and Predicting Therapeutic Response
FAQs: Addressing Core Concepts in SOX9 Biology and Therapeutics
Q1: What is the primary clinical significance of SOX9 in cancer therapy? SOX9 is a transcription factor that drives chemotherapy resistance by reprogramming cancer cells into a drug-tolerant, stem-like state. Its upregulation is associated with significantly poorer overall survival in patients receiving platinum-based chemotherapy [1] [2].
Q2: How can researchers detect and quantify SOX9-mediated resistance in patient samples? Key methodologies include:
- Immunohistochemistry (IHC) on Tissue Microarrays (TMAs): Used to correlate SOX9 protein expression with treatment response outcomes, such as PSA progression-free survival in prostate cancer [48].
- Single-cell RNA Sequencing (scRNA-Seq): Identifies rare clusters of SOX9-expressing cells in tumors and tracks SOX9 induction after chemotherapy in longitudinal patient samples [1].
- Transcriptional Divergence Analysis: A metric (P50/P50) calculated from gene expression data that serves as an indicator of transcriptional plasticity and stemness, both hallmarks of SOX9 activity [1].
Q3: Does SOX9 have a role in sensitivity to any therapies? Yes, evidence suggests a context-dependent role. In Triple-Negative Breast Cancer (TNBC), elevated SOX9 expression is significantly associated with increased sensitivity to the CDK7 inhibitor THZ1, suggesting it may serve as a predictive biomarker for this specific therapeutic class [49].
Q4: What computational tools are available for predicting patient response beyond SOX9? The ENLIGHT platform is a transcriptomics-based pipeline that identifies clinically relevant genetic interactions to predict a patient's response to a wide variety of therapies across multiple cancer types, without requiring prior training on treatment response data [50].
Troubleshooting Guides: Experimental Pitfalls in SOX9 Research
Scenario 1: Inconsistent SOX9 Expression in Cell Line Models Post-Chemotherapy
Problem: Expected induction of SOX9 following platinum treatment is not observed or is highly variable across replicates. Solution:
- Verify Epigenetic Regulation: SOX9 upregulation is often epigenetically mediated. Confirm the integrity of your super-enhancer analysis (e.g., via H3K27ac ChIP-seq) in resistant versus naive cells [1].
- Check Treatment Timing and Dose: SOX9 induction can be acute. Perform a time-course experiment (e.g., 24, 48, 72 hours) and dose-response curve to establish optimal conditions for your specific cell line [1].
- Confirm Functional Knockout: When using CRISPR/Cas9 to ablate SOX9, use a colony formation assay to validate the resulting increase in platinum sensitivity, confirming a successful and functional knockout [1] [2].
Scenario 2: Difficulty in Linking SOX9 to a Stem-like Phenotype
Problem: Data linking SOX9 expression to cancer stem cell (CSC) properties like self-renewal are inconclusive. Solution:
- Utilize Single-cell Analysis: Apply scRNA-Seq to SOX9-high versus SOX9-low populations. Look for enrichment of established stemness gene modules and increased transcriptional divergence, a quantifiable measure of cellular plasticity [1].
- Functional Stemness Assays: Correlate SOX9 expression (via flow sorting or genetic reporters) with functional assays like tumorsphere formation in vitro and tumor initiation capacity in vivo [2] [7].
Scenario 3: Biomarker Validation Fails in Clinical Cohorts
Problem: SOX9 expression does not correlate with therapeutic response in a patient cohort. Solution:
- Consider Co-factors and Interactome: SOX9 can function in complexes with other factors like FOXC1 to regulate key pathways like MYC signaling. Analyze the expression of these partners, as the functional unit may be the relevant biomarker, not SOX9 alone [49].
- Refine Patient Stratification: Ensure the cohort is appropriately stratified. SOX9's role may be more pronounced in specific cancer subtypes, such as basal-like breast cancer or HGSOC, and its effect can be masked in heterogeneous patient groups [1] [7].
- Longitudinal Sampling: SOX9 is often induced by therapy. Analyze paired patient samples from pre- and post-treatment to capture therapy-induced SOX9 expression, which may be more informative than baseline levels alone [1].
Summarized Data Tables
Table 1: Clinical Correlations of SOX9 Across Cancer Types
| Cancer Type | Therapeutic Context | Correlation with SOX9 | Clinical Outcome Measure | Source |
|---|---|---|---|---|
| High-Grade Serous Ovarian Cancer (HGSOC) | Platinum Chemotherapy | Positive | Shorter Overall Survival | [1] |
| Metastatic Castration-Resistant Prostate Cancer (mCRPC) | Docetaxel Chemotherapy | Positive | Lower PSA Response Rate; Shorter PSA-PFS & OS | [48] |
| Triple-Negative Breast Cancer (TNBC) | CDK7 Inhibitor (THZ1) | Negative (Predictor of Sensitivity) | Lower IC₅₀ values (Increased Sensitivity) | [49] |
| Breast Cancer | General Prognosis | Positive | Poor Prognosis | [7] |
Table 2: Key Experimental Models for SOX9 Functional Studies
| Experimental Method | Key Function in SOX9 Research | Typical Readout |
|---|---|---|
| CRISPR/Cas9 Knockout | Validates necessity of SOX9 for chemoresistance | Increased platinum sensitivity in colony formation assays [1] |
| Endogenous Epigenetic Activation | Demonstrates sufficiency of SOX9 to drive resistance | Induction of stem-like transcriptional state and in vivo chemoresistance [1] |
| ChIP-sequencing | Identifies direct genomic targets and partners (e.g., FOXC1) | SOX9 binding sites at enhancers regulating MYC pathway [49] |
| scRNA-Seq on Patient Tumors | Identifies rare, native SOX9+ stem-like cells and therapy-induced shifts | Cluster of SOX9+ cells enriched for stemness and stress modules [1] |
Experimental Protocols
Protocol 1: Assessing SOX9-Mediated Chemoresistance In Vitro
Objective: To establish a causal link between SOX9 expression and platinum resistance in HGSOC cell lines. Materials: HGSOC cell line (e.g., OVCAR4, Kuramochi), carboplatin, CRISPR/Cas9 system for SOX9 knockout, CRISPR activation system for SOX9 induction, cultureware. Methodology:
- Genetic Manipulation:
- Generate SOX9-knockout cells using CRISPR/Cas9 with SOX9-targeting sgRNA.
- Generate SOX9-overexpressing cells using a CRISPR activation system to epigenetically upregulate the endogenous SOX9 locus.
- Treatment: Treat isogenic parental, KO, and OE cells with a range of carboplatin doses (e.g., 0-100 µM).
- Viability Assessment: Incubate for 10-14 days and perform a colony formation assay. Fix and stain colonies with crystal violet.
- Analysis: Count colonies and plot dose-response curves to calculate IC₅₀ values. Compare the sensitivity of KO and OE lines to parental controls. Statistical significance is typically determined by a two-tailed Student's t-test [1].
Protocol 2: Detecting SOX9 as a Biomarker via IHC
Objective: To correlate SOX9 protein levels with patient response to docetaxel in mCRPC. Materials: Formalin-fixed paraffin-embedded (FFPE) prostate biopsy samples, TMA constructor, anti-SOX9 antibody, IHC staining kit. Methodology:
- Cohort Selection: Identify a cohort of mCRPC patients with documented response to docetaxel and available pre-treatment biopsy tissue.
- TMA Construction: Core FFPE blocks from patient samples to construct a TMA.
- IHC Staining: Perform IHC staining on TMA sections using a validated anti-SOX9 antibody.
- Scoring: Score SOX9 expression by a pathologist (e.g., based on intensity and percentage of positive tumor cells). Dichotomize patients into SOX9-positive and SOX9-negative groups.
- Statistical Correlation: Correlate SOX9 status with clinical endpoints: PSA response rate (Chi-square test), PSA-PFS, and OS (Kaplan-Meier survival analysis with log-rank test) [48].
Signaling Pathways and Experimental Workflows
Diagram Title: SOX9 in Therapy Response and Resistance
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating SOX9 Function
| Reagent / Tool | Specific Example / Assay | Primary Function in Research |
|---|---|---|
| Validated SOX9 Antibodies | Immunohistochemistry (IHC) | Detecting SOX9 protein expression and localization in patient tissue samples [48]. |
| CRISPR/Cas9 Systems | KO (sgRNA) & Activation (dCas9-VPR) | Genetically validating the necessity and sufficiency of SOX9 in resistance phenotypes [1]. |
| scRNA-Seq Platforms | 10x Genomics | Profiling tumor heterogeneity, identifying rare SOX9+ stem-like cells, and analyzing transcriptional divergence [1]. |
| ChIP-seq Kits | H3K27ac, SOX9-specific | Mapping super-enhancer dynamics and direct genomic binding targets of SOX9 [1] [49]. |
| Transcriptomic Databases | TCGA, GEO | Correlating SOX9 expression with patient survival and treatment outcomes across cancers [1] [7]. |
Bench to Bedside: Validating SOX9-Targeted Strategies in Preclinical and Clinical Models
This technical support center provides essential guidance for researchers aiming to overcome SOX9-mediated therapy resistance in cancer. The transcription factor SOX9 (SRY-Box Transcription Factor 9) has been identified as a critical driver of chemoresistance in multiple cancers, including high-grade serous ovarian cancer and breast cancer [1] [7]. It promotes a stem-like transcriptional state, enabling cancer cells to survive chemotherapy and initiate new tumors [2]. This FAQ section addresses specific experimental challenges you might encounter when working with advanced in vivo models to study SOX9 mechanisms and develop therapeutic strategies.
Troubleshooting Guides & FAQs
Patient-Derived Xenograft (PDX) Models
Q1: Our PDX engraftment rates are consistently low. What are the key factors we should optimize?
Low engraftment success is a common challenge. The table below summarizes the primary factors to investigate and optimize.
Table: Troubleshooting Low PDX Engraftment Rates
| Factor | Problem | Solution |
|---|---|---|
| Mouse Strain | Using mice with insufficient immunodeficiency leads to immune rejection [51]. | Switch to more immunocompromised strains like NOD-SCID-IL2Rγnull (NSG) or BRG mice, which have higher success rates [51]. |
| Sample Quality & Processing | Sample viability is compromised during collection or processing; critical tumor microenvironment is lost [51]. | Implant fresh tumor fragments (2-3 mm³) instead of single-cell suspensions to better preserve stromal interactions and the tumor microenvironment [52] [51]. Use Matrigel to support engraftment. |
| Tumor Origin | Success rates vary naturally by cancer type and patient [51]. | Prioritize tumor samples from treatment-naive patients or from metastatic sites, which often have higher take rates. Manage expectations based on your specific cancer type. |
Q2: How do we ensure our PDX models faithfully represent the original patient tumor and its SOX9 expression?
Maintaining biological fidelity across passages is crucial for SOX9 research.
- Verification Workflow: Always authenticate your model after establishment (F0 to F2 generations) and before key experiments. This involves:
- Genomics: Perform short tandem repeat (STR) profiling to confirm human origin and match to the patient donor.
- Histology: Use immunohistochemistry (IHC) to compare the architecture and key biomarkers (e.g., SOX9, PAX8) between the patient tumor and the PDX model [52].
- Transcriptomics: Conduct RNA sequencing to verify that the SOX9-high and stem-like gene signature is conserved in the model [1] [2].
Conditional & Reversible Gene Knockout Models
Q3: We need to study essential genes where constitutive knockout is lethal. What is a modern, efficient method for generating conditional knockouts?
For diploid cells, CRISPR-FLIP is a highly efficient, one-step method to create bi-allelic conditional knockouts.
- Experimental Protocol:
- Design: Identify a target exon common to all transcripts in the first 50% of the SOX9 coding sequence. Ensure a compatible CRISPR gRNA site is nearby [53].
- Co-delivery: Co-transfect your cells (e.g., stem cells, organoids) with:
- A plasmid expressing Cas9 nuclease and the target-specific gRNA.
- A donor vector containing the FLIP cassette, flanked by homology arms for the target site. The cassette contains a puromycin resistance gene (
puroR) in its non-mutagenic orientation [53].
- Selection & Screening: Select transfected cells with puromycin. This enriches for cells where one allele has the FLIP cassette correctly integrated via HDR. Simultaneously, the CRISPR/Cas9 induces an NHEJ frameshift mutation in the second allele in a high percentage of clones [53].
- Induction: Transfer the FLIP cassette into its mutagenic orientation by delivering Cre recombinase, which inactivates the gene.
Diagram: Workflow for Conditional Knockout with CRISPR-FLIP
Q4: We want a reversible system to study SOX9 function dynamically. Is this possible?
Yes, the CRISPR-FLIP system can be modified to create reversible conditional alleles. The advanced FLIP-FlpE cassette includes FRT sites flanking the mutagenic components [53].
- Experimental Protocol:
- Targeting: Integrate the FLIP-FlpE cassette into your target gene (e.g., SOX9) using the standard CRISPR-FLIP protocol.
- Inactivation: Transfer the cassette to its mutagenic orientation with Cre recombinase to knockout the gene.
- Reversion: Express Flp recombinase to excise the entire mutagenic cassette, restoring normal gene function. This is invaluable for studying the reversibility of SOX9-driven phenotypes like chemoresistance [53].
Key Experimental Protocols & Methodologies
Protocol: Validating SOX9-Mediated Chemoresistance In Vivo
This protocol is adapted from studies establishing SOX9 as a key driver of platinum resistance in ovarian cancer [1] [2].
Model Generation:
- Use an established HGSOC cell line (e.g., OVCAR4, Kuramochi) or a PDX model.
- Experimental Group: Introduce a genetic construct to overexpress SOX9 in the cancer cells.
- Control Group: Use cells transduced with an empty vector control.
In Vivo Treatment:
- Implant cells orthotopically or subcutaneously into immunocompromised mice.
- Once tumors are palpable, randomize mice into two subgroups for each cell type:
- Treatment: Administer carboplatin (e.g., 50 mg/kg, i.p., weekly).
- Vehicle Control: Administer saline or the drug's solvent.
- Monitor tumor volume twice weekly.
Endpoint Analysis:
- Tumor Growth: Compare tumor growth curves and final weights between SOX9-overexpressing and control groups under chemotherapy.
- Ex Vivo Validation:
- Perform IHC on harvested tumors for SOX9 and stemness markers (e.g., ALDH1A1).
- Use qRT-PCR or RNA-Seq to analyze the expression of stemness and chemoresistance gene modules.
Protocol: Single-Cell RNA Sequencing to Identify SOX9-High Stem-like Cells
This protocol is critical for identifying the rare, therapy-resistant cell population driven by SOX9 [1].
Sample Preparation:
- Obtain single-cell suspensions from primary patient tumors or PDX models, both before and after chemotherapy.
- Crucial Step: Include a cell viability dye (e.g., Propidium Iodide) to ensure only live cells are sequenced.
Library Preparation & Sequencing:
- Use a platform like the 10x Genomics Chromium Controller to generate barcoded single-cell RNA-seq libraries.
- Sequence the libraries to a sufficient depth (e.g., 50,000 reads per cell).
Bioinformatic Analysis:
- Clustering: Use Seurat or Scanpy to perform dimensionality reduction (PCA, UMAP) and cluster cells based on gene expression patterns.
- SOX9 Population Identification: Identify clusters with high expression of SOX9 and a stem-like signature.
- Transcriptional Divergence: Calculate the P50/P50 transcriptional divergence score for each cell. This metric, defined as the sum of expression of the top 50% of genes divided by the sum of the bottom 50%, is amplified in stem-like cells and is a poor prognostic indicator [1].
Diagram: SOX9-Driven Pathway to Therapy Resistance
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Research Reagents for Investigating SOX9-Mediated Resistance
| Reagent / Tool | Function / Application | Key Considerations |
|---|---|---|
| NSG (NOD-SCID-IL2Rγnull) Mice | The preferred immunodeficient host for PDX engraftment due to the absence of T, B, and NK cell activity [52] [51]. | Higher cost; requires strict specific pathogen-free (SPF) housing conditions. |
| CRISPR-FLIP Donor Vector | A universal donor plasmid for one-step generation of conditional and reversible knockouts in diploid cells [53]. | Must be designed with homology arms specific to your target gene (e.g., SOX9). |
| Anti-SOX9 Antibody | Detection and visualization of SOX9 protein expression in tumor tissues via IHC and IF. | Validate for specificity in your model system; performance can vary between applications. |
| Cre-ER(T2) Inducible System | Enables tamoxifen-dependent, time-controlled Cre recombinase activity for inducing gene knockouts (e.g., in FLIP models) [53]. | Allows for temporal control of gene inactivation, crucial for studying adult-onset phenotypes. |
| Matrigel | Basement membrane extract used to support the engraftment of tumor fragments or cells in PDX modeling [51]. | Lot-to-lot variability exists; keep consistent for a given study. Requires cold handling. |
SOX9 is a transcription factor critical for embryonic development, stem cell maintenance, and cell fate determination [40]. In cancer research, SOX9 has emerged as a significant contributor to therapy resistance, tumor proliferation, and metastasis across various malignancies, including liver, lung, breast, and gastric cancers [15]. Its overexpression is associated with poor prognosis and enables cancer cells to evade multiple treatment modalities through complex molecular mechanisms [15] [54]. This technical support center provides a comparative analysis of three primary SOX9-targeting strategies—siRNA, small molecules, and epigenetic modulators—to assist researchers in overcoming SOX9-mediated therapy resistance.
SOX9 Molecular Mechanisms and Signaling Pathways
Key Structural and Functional Domains
The SOX9 protein contains several functionally critical domains that serve as potential targeting sites:
- High Mobility Group (HMG) Domain: Facilitates DNA binding and nuclear localization through embedded nuclear localization signals (NLS) [40] [15]
- Dimerization Domain (DIM): Enables homologous dimerization of SOX proteins [40]
- Transactivation Domains (TAM and TAC): Critical for interactions with coactivators and other transcription factors; TAC domain directly binds β-catenin ARM repeats, competing with TCF/LEF complexes [40] [15]
- PQA-rich Domain: Enhances transactivation potency [40]
SOX9 Signaling Cross-Talk in Cancer
SOX9 exhibits complex cross-regulation with key cancer signaling pathways, particularly the Wnt/β-catenin pathway, which represents a critical mechanism in SOX9-mediated therapy resistance [40]. The diagram below illustrates these core interactions.
SOX9-Wnt/β-catenin Cross-Regulation in Cancer: This diagram illustrates the complex cross-talk between SOX9 and the canonical Wnt signaling pathway, a key mechanism in SOX9-mediated therapy resistance. SOX9 antagonizes Wnt signaling by promoting β-catenin degradation through multiple mechanisms: (1) direct binding leading to ubiquitin/proteasome-dependent degradation; (2) induction of GSK3β nuclear translocalization; (3) transcriptional activation of MAML2, a β-catenin antagonist; and (4) competition with TCF/LEF for β-catenin binding [40]. In cancers, this regulatory balance is disrupted, contributing to proliferation and drug resistance.
Comparative Analysis of SOX9-Targeting Strategies
Quantitative Comparison of Targeting Modalities
Table 1: Comparative analysis of SOX9-targeting therapeutic modalities
| Parameter | siRNA/shRNA | Small Molecules | Epigenetic Modulators |
|---|---|---|---|
| Target Specificity | High (sequence-specific) | Moderate (protein domain-specific) | Low (genome-wide effects) |
| Development Timeline | 6-12 months for validation | 3-5 years for lead optimization | 2-4 years for approved drugs |
| Knockdown Efficiency | 50-95% mRNA reduction [55] [54] | Variable (dependent on binding affinity) | Indirect SOX9 modulation |
| Therapeutic Durability | Transient (siRNA) to stable (shRNA) [55] | Transient (requires continuous dosing) | Potentially long-lasting |
| Delivery Challenges | High (requires viral vectors/ nanoparticles) | Low to moderate (standard drug delivery) | Low (standard drug delivery) |
| Clinical Translation | Limited (mostly preclinical) | Advanced (multiple candidates) | Approved for other cancers (e.g., azacytidine, panobinostat) [56] |
| Key Limitations | Off-target effects, immune activation, delivery efficiency | Druggability, resistance mutations, toxicity | Non-specific effects, cellular toxicity |
| Best Applications | Target validation, functional studies, precision medicine | Chronic treatment, combination therapy | Overcoming epigenetic-driven resistance |
Technical Protocols and Methodologies
siRNA/shRNA-Mediated SOX9 Knockdown
Experimental Workflow for SOX9 Gene Silencing
SOX9 siRNA/shRNA Knockdown Workflow: This workflow outlines the key steps for effective SOX9 gene silencing, from careful target design to functional validation—particularly important given SOX9's role in Wnt/β-catenin signaling and therapy resistance [54].
Detailed Protocol: SOX9-Targeting siRNA Design and Delivery
Step 1: Target Sequence Selection
- Identify 21 nt sequences beginning with AA dinucleotide from the SOX9 mRNA sequence (NM_000346.3) [57]
- Select 2-4 target sequences with 30-50% GC content to maximize efficacy
- Avoid stretches of >4 T's or A's when using RNA pol III promoters
- Target different regions along the SOX9 coding sequence to overcome potential structural accessibility issues
Step 2: Specificity Validation
- Perform BLAST analysis against the appropriate genome database to ensure minimal off-target homology (<16-17 contiguous base pairs) [57]
- Design scrambled control siRNA with the same nucleotide composition but lacking sequence homology
Step 3: Hairpin Design for shRNA (for viral delivery)
- For lentiviral delivery systems, design DNA oligonucleotides encoding:
Step 4: Delivery and Transduction
- Package shRNA constructs into lentiviral particles for stable integration
- Transduce target cells using appropriate multiplicity of infection (MOI)
- Select stable knockdown cells using puromycin or other appropriate antibiotics
- For primary and non-dividing cells, lentiviral-based delivery remains the most viable technology [55]
Step 5: Validation of Knockdown Efficiency
- Assess SOX9 mRNA reduction using RT-qPCR 48-72 hours post-transfection
- Evaluate protein knockdown via Western blotting using SOX9-specific antibodies
- Confirm functional effects on Wnt/β-catenin signaling through β-catenin, cyclin D1, and c-Myc expression analysis [54]
Small Molecule Targeting of SOX9
Current Challenges and Approaches
- Direct Targeting Limitations: SOX9, like many transcription factors, presents significant druggability challenges due to its predominantly nuclear localization and protein-DNA/protein-protein interaction interfaces [58]
- Indirect Targeting Strategies: Focus on upstream regulators and modulators of SOX9 expression and activity, including:
- Kinase inhibitors affecting SOX9 phosphorylation
- Protein-protein interaction disruptors for SOX9-coactivator complexes
- Degradation inducers via proteasome pathway modulation
Experimental Validation Framework
- Establish high-throughput screening assays using SOX9-responsive reporter systems
- Validate hits in multiple cancer cell lines with endogenous SOX9 overexpression
- Assess effects on SOX9 transcriptional activity, protein stability, and nuclear localization
- Evaluate impact on downstream pathways, particularly Wnt/β-catenin signaling [40] [54]
Epigenetic Modulation of SOX9
Key Epigenetic Mechanisms Regulating SOX9
Table 2: Epigenetic regulators of SOX9 expression and activity
| Epigenetic Mechanism | Effect on SOX9 | Key Regulators | Experimental Assessment |
|---|---|---|---|
| Histone Acetylation | Transcriptional activation | p300, GCN5 [59] [60] | ChIP for H3K9ac, H3K27ac at enhancers |
| Histone Methylation | Context-dependent activation/repression | WDR5, Trithorax/COMPASS-like [59] | ChIP for H3K4me3 (active), H3K27me3 (repressive) |
| DNA Methylation | Promoter silencing | DNMTs [56] | Bisulfite sequencing of promoter CpG islands |
| Chromatin Remodeling | Accessibility modulation | SWI/SNF complexes | ATAC-seq, DNase-seq |
Protocol: Assessing Epigenetic Modifications at SOX9 Loci
Chromatin Immunoprecipitation (ChIP) for SOX9 Enhancer Regions
- Crosslink proteins to DNA in SOX9-expressing cancer cells using 1% formaldehyde
- Sonicate chromatin to 200-500 bp fragments
- Immunoprecipitate with antibodies against:
- H3K27ac (active enhancers) [59]
- H3K4me3 (active promoters)
- p300 (enhancer marking)
- Analyze enrichment at known SOX9 enhancers (eSR-A, e-ALDI) using qPCR [59]
- For genome-wide assessment, combine with ChIP-seq methodology
Troubleshooting Common Experimental Challenges
siRNA/shRNA-Specific Issues
Problem: Inefficient SOX9 Knockdown
- Potential Cause: Poor target site accessibility due to mRNA secondary structure or RNA-binding proteins
- Solution: Test multiple target sequences (minimum 2-4) spaced along the SOX9 coding region [57]
- Validation: Include positive control siRNA and monitor transfection efficiency with fluorescent dyes
Problem: Off-Target Effects
- Potential Cause: Sequence similarity to non-target genes
- Solution: Perform rigorous BLAST analysis during design phase; use two different siRNA sequences to confirm phenotype specificity [55]
- Validation: Transcriptome analysis (RNA-seq) to identify unintended gene expression changes
Problem: Poor Viral Transduction Efficiency
- Potential Cause: Suboptimal viral titer or target cell resistance to infection
- Solution: Concentrate lentiviral particles; use polybrene (4-8 μg/mL) to enhance infection; optimize multiplicity of infection (MOI) [55]
- Validation: Include fluorescent reporter (GFP/RFP) in viral construct to monitor transduction efficiency
Small Molecule Challenges
Problem: Lack of Direct SOX9 Inhibitors
- Current Limitation: Limited availability of specific, potent SOX9 small molecule inhibitors
- Alternative Approach: Focus on validated upstream regulators and critical co-factors identified through CRISPR or siRNA screens
- Experimental Strategy: Combination treatments targeting multiple nodes in SOX9-associated pathways
Epigenetic Modulator Issues
Problem: Non-Specific Effects of Epigenetic Drugs
- Potential Cause: Genome-wide activity of histone modifiers and DNA methyltransferases
- Solution: Use lowest effective concentrations; combine with genetic validation (siRNA) of target specificity
- Validation: Assess global epigenetic changes versus specific SOX9 locus effects
Research Reagent Solutions
Table 3: Essential reagents for SOX9-targeting experiments
| Reagent Category | Specific Examples | Application | Key Considerations |
|---|---|---|---|
| SOX9 Detection | Anti-SOX9 antibodies (Santa Cruz Biotechnology) [54] | Western blot, IHC, IF | Validate specificity in knockdown controls |
| siRNA/shRNA Vectors | Lentiviral FG12, pSilencer series [55] [57] | Stable knockdown | Include selection markers (puromycin) |
| Epigenetic Tools | p300 inhibitors (C646), HDAC inhibitors, DNMT inhibitors [59] [56] | Modulating SOX9 expression | Titrate for specific vs. global effects |
| Cell Line Models | PTC cell lines (TPC-1, BCPAP) [54], PDAC, glioma lines | Functional studies | Select lines with endogenous SOX9 overexpression |
| Pathway Reporters | Wnt/β-catenin (TOP/FOP flash), SOX9-responsive elements | Signaling activity | Normalize for transfection efficiency |
| Functional Assays | Transwell migration, Matrigel invasion, soft agar colony formation [54] | Phenotypic validation | Include appropriate controls for assay variability |
Frequently Asked Questions
Q: What is the most effective approach for achieving complete SOX9 ablation in vitro? A: For complete and sustained SOX9 knockdown, lentiviral-delivered shRNA provides the most robust solution, particularly for difficult-to-transfect cells and long-term studies [55]. However, always validate with multiple independent shRNA sequences to confirm phenotype specificity and rule off-target effects.
Q: How can I determine whether SOX9 is acting as an oncogene or tumor suppressor in my model system? A: SOX9 demonstrates context-dependent functions [15] [54]. Perform gain-of-function and loss-of-function experiments in your specific cellular context, and examine effects on Wnt/β-catenin signaling pathway components, as this represents a key SOX9 regulatory axis [40] [54].
Q: What are the best validation methods for confirming SOX9 targeting efficiency? A: Employ a multi-tiered validation approach:
- mRNA level: RT-qPCR with multiple reference genes
- Protein level: Western blotting and immunofluorescence
- Functional validation: Assessment of known SOX9 downstream targets (cyclin D1, c-Myc) and phenotypic assays (proliferation, invasion) [54]
- Pathway-specific validation: Wnt/β-catenin signaling activity through TOP/FOP flash reporter assays
Q: How can I overcome SOX9-mediated therapy resistance in cancer models? A: Consider combination approaches targeting both SOX9 and its associated resistance mechanisms:
- SOX9 knockdown with standard chemotherapeutics
- Epigenetic modulators to reverse SOX9 overexpression
- Wnt/β-catenin pathway inhibitors in SOX9-high contexts [40] [54]
- Focus on the SOX9-β-catenin cross-regulation as a key resistance node [40]
The comparative analysis of SOX9-targeting modalities reveals distinct advantages and limitations for each approach. siRNA/shRNA technologies offer high specificity and are ideal for target validation and functional studies, while small molecules and epigenetic modulators present more clinically translatable options despite current limitations in specificity. The complex cross-regulation between SOX9 and Wnt/β-catenin signaling represents a critical point of therapeutic intervention [40]. Future research should focus on developing more specific small molecule inhibitors, improving delivery systems for RNA-based therapies, and designing rational combination strategies that address SOX9-mediated resistance mechanisms across different cancer types.
SOX9 (SRY-Box Transcription Factor 9) is a transcription factor crucial for embryonic development and stem cell regulation. Recent research has established its significant role in cancer progression and therapy resistance. This guide provides technical support for validating SOX9 as a biomarker, focusing on methodologies to correlate its expression levels with patient treatment outcomes, a critical step in overcoming SOX9-mediated therapy resistance.
FAQs: SOX9 as a Biomarker and Therapy Resistance
1. What is the clinical significance of SOX9 expression in cancer? High SOX9 expression is frequently observed in various malignancies and is often correlated with aggressive disease features and poor prognosis. It drives cancer stemness, chemoresistance, and immune evasion. For instance, in high-grade serous ovarian cancer (HGSOC), patients in the top quartile of SOX9 expression had significantly shorter overall survival after platinum-based treatment [1]. Similarly, SOX9 upregulation is associated with resistance to PARP inhibitors in ovarian cancer and to platinum-based therapies across multiple cancer types [1] [61] [33].
2. How does SOX9 contribute to therapy resistance? SOX9 promotes resistance through several mechanisms:
- Stemness Reprogramming: It reprograms the transcriptional state of naive cancer cells into a stem-like, drug-tolerant state [1].
- Enhanced DNA Damage Repair: It binds to promoters of key DNA damage repair (DDR) genes like
SMARCA4,UIMC1, andSLX4, enhancing the cell's ability to survive chemotherapy-induced DNA damage [61]. - Protein Stability Regulation: The deubiquitinating enzyme USP28 stabilizes SOX9 protein by inhibiting its degradation, thereby promoting resistance [61].
- Immune Evasion: SOX9 helps latent cancer cells remain dormant in metastatic sites and avoid immune surveillance [7].
3. What are the key methodologies for quantifying SOX9 expression? Key techniques include:
- RNA Sequencing (RNA-seq): Used to analyze SOX9 expression and identify differentially expressed genes (DEGs) from databases like TCGA and GTEx [13] [18].
- Western Blotting: Validates SOX9 protein expression levels in tumor tissues versus normal tissues [13] [18].
- Immunohistochemistry (IHC): Allows for visualization and quantification of SOX9 protein in formalin-fixed, paraffin-embedded (FFPE) tumor samples [1].
- Single-cell RNA-Seq (scRNA-Seq): Reveals SOX9 expression heterogeneity and its upregulation in specific cell subpopulations following chemotherapy [1].
4. How is SOX9 expression correlated with clinical outcomes? Statistical analyses are employed to establish correlations:
- Kaplan-Meier (K-M) Analysis: Compares overall survival (OS) between patient groups with high versus low SOX9 expression [13] [18].
- Cox Regression Analysis: Identifies SOX9 as an independent prognostic factor, often in conjunction with other markers like IDH status in glioblastoma [13] [18].
- Nomogram Prognostic Models: Integrate SOX9 expression with other clinical variables (e.g., IDH status, other gene signatures) to individualize survival prediction [13].
Quantitative Correlations Between SOX9 and Treatment Outcomes Table 1: SOX9 as a Prognostic and Predictive Biomarker Across Cancers
| Cancer Type | Therapy Context | Correlation with High SOX9 | Proposed Mechanism | Statistical Evidence |
|---|---|---|---|---|
| High-Grade Serous Ovarian Cancer (HGSOC) [1] | Platinum-based Chemotherapy | Shorter Overall Survival | Induction of stem-like, drug-tolerant state | HR=1.33; log-rank P=0.017 |
| Glioblastoma (GBM) [13] [18] | Standard radio-chemotherapy | Better Prognosis in specific (IDH-mutant) subgroups | Association with immune infiltration | P < 0.05 |
| Ovarian Cancer [61] | PARP Inhibitors (Olaparib) | Resistance | Stabilization by USP28, enhanced DNA repair | N/A |
| Multiple Cancers (e.g., Lung, Liver, Breast) [33] | Various Chemotherapies & Targeted Therapies | Poor Prognosis & Resistance | Regulation of stemness, proliferation, and survival pathways | Correlation with tumor grade and survival |
Experimental Protocols
Protocol 1: Validating SOX9 Expression via RNA-seq and qRT-PCR
This protocol outlines the bioinformatic and experimental validation of SOX9 transcript levels.
Workflow Diagram: SOX9 mRNA Validation
Detailed Methodology:
- Data Acquisition: Obtain RNA-seq data (HTSeq-Count/FPKM) from public repositories like The Cancer Genome Atlas (TCGA) and Genotype-Tissue Expression (GTEx) database [13] [18].
- Bioinformatic Analysis:
- Experimental Validation (Wet-Lab):
- RNA Extraction: Extract total RNA from fresh-frozen or optimally preserved tissue samples using TRIzol reagent or commercial kits. Assess RNA integrity and purity.
- cDNA Synthesis: Synthesize cDNA using a reverse transcription kit with oligo(dT) and/or random primers.
- Quantitative RT-PCR (qRT-PCR): Perform qRT-PCR with SYBR Green or TaqMan assays. Use the following primers:
- SOX9 Forward: (Design sequence based on transcript variant, e.g., from NCBI Nucleotide)
- SOX9 Reverse: (Design sequence based on transcript variant)
- Reference Genes: GAPDH, ACTB, or HPRT1.
- Data Analysis: Calculate relative SOX9 expression using the 2^(-ΔΔCt) method.
Protocol 2: Assessing SOX9 Protein Function in Therapy Resistance
This protocol focuses on mechanistic studies linking SOX9 protein stability to drug resistance.
Workflow Diagram: SOX9 Protein Stability & Resistance
Detailed Methodology:
- Protein Interaction and Stabilization Assays:
- Co-Immunoprecipitation (Co-IP): Lyse cells in RIPA buffer with protease inhibitors. Incubate cell lysates with SOX9 antibody or control IgG overnight, followed by Protein A/G magnetic beads. Wash complexes and analyze by Western blot for SOX9 and its regulators (e.g., USP28, FBXW7) [61].
- Cycloheximide (CHX) Chase Assay: Treat cells (e.g., ovarian cancer SKOV3 lines) with CHX to inhibit new protein synthesis. Harvest cells at different time points (0, 1, 2, 4 hours) and perform Western blotting for SOX9. Compare protein half-life with and without inhibitor treatment (e.g., USP28 inhibitor AZ1) [61].
- Functional DNA Binding Assay (ChIP-Seq):
- Crosslinking and Sonication: Crosslink proteins to DNA in cells using formaldehyde. Lyse cells and sonicate to shear chromatin to 200-500 bp fragments.
- Immunoprecipitation: Incubate chromatin with SOX9-specific antibody. Use normal rabbit IgG as a control. Precipitate immune complexes.
- Library Prep and Sequencing: Reverse crosslinks, purify DNA, and prepare libraries for high-throughput sequencing.
- Bioinformatic Analysis: Map sequencing reads to the reference genome and call peaks to identify SOX9 binding sites, focusing on promoters of DDR genes [61].
- In Vitro Drug Sensitivity Assays:
- Treat SOX9-knockout or control cells with serial dilutions of therapeutical agents (e.g., Carboplatin, Olaparib) for 72 hours.
- Assess cell viability using assays like CCK-8 or colony formation. Calculate IC50 values. SOX9 knockout is expected to significantly increase sensitivity, reducing colony formation [1] [61].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for SOX9 Biomarker Research
| Reagent / Tool | Function / Application | Example Product / Assay |
|---|---|---|
| SOX9 Antibody | Detection and quantification of SOX9 protein via Western Blot, IHC, and Co-IP. | Anti-SOX9 (AB5535, Sigma-Aldrich) [61] |
| USP28 Inhibitor | Chemically inhibits USP28, leading to decreased SOX9 protein stability and increased degradation. | AZ1 (S8904, Selleck Chemicals) [61] |
| PARP Inhibitor | Induces synthetic lethality in HRD cells; used to study and overcome PARPi resistance. | Olaparib (AZD2281, Selleck Chemicals) [61] |
| CRISPR/Cas9 System | Genetic knockout of SOX9 to study its necessity in chemoresistance and tumorigenesis. | SOX9-targeting sgRNA and CRISPR/Cas9 [1] |
| Cell Lines | In vitro models for studying SOX9 function and therapy resistance mechanisms. | HGSOC lines (OVCAR4, Kuramochi); Ovarian cancer lines (SKOV3, UWB1.289) [1] [61] |
Troubleshooting Guides
Problem: Inconsistent SOX9 IHC Staining Across Tumor Sections
- Potential Cause: Heterogeneity of SOX9 expression within the tumor microenvironment [7].
- Solution: Score multiple representative regions of the tumor section. Use digital pathology platforms for quantitative, whole-slide analysis to account for heterogeneity.
Problem: Poor Correlation between SOX9 mRNA and Protein Levels
- Potential Cause: Post-translational regulation (e.g., ubiquitination) affecting SOX9 protein stability independent of transcription [61].
- Solution: Always complement RNA-based assays (qRT-PCR) with protein-level detection (Western Blot, IHC). Investigate protein stability using CHX chase assays and check the status of regulators like USP28.
Problem: High Background in Co-IP for SOX9 Interactors
- Potential Cause: Non-specific antibody binding or incomplete lysis.
- Solution: Optimize lysis buffer stringency and include stringent wash steps (e.g., high salt washes). Use HRP-conjugated secondary antibodies specific for the light chain to avoid interference from denatured IgG heavy chains in Western blot detection [61]. Validate interactions with complementary methods like mass spectrometry.
Profiling Resistance to SOX9-Targeted Therapies Across Cancer Types
The transcription factor SOX9 has emerged as a critical driver of therapy resistance across multiple cancer types. Initially recognized for its role in embryonic development and cell stemness, SOX9 is now established as a key regulator of cancer stem-like cells (CSCs) and a promoter of chemoresistance, radioresistance, and targeted therapy resistance. Understanding the molecular mechanisms underlying SOX9-mediated resistance is essential for developing effective strategies to overcome this significant clinical challenge. This technical support center provides comprehensive troubleshooting guides, experimental protocols, and analytical frameworks to help researchers profile and combat SOX9-driven resistance mechanisms in their cancer models.
SOX9 in Therapy Resistance: Key Mechanisms & Clinical Evidence
Quantitative Evidence of SOX9 in Cancer Resistance
Table 1: SOX9-Mediated Therapy Resistance Across Cancer Types
| Cancer Type | Therapy Resistance Mechanism | Key Findings | Clinical Impact |
|---|---|---|---|
| High-Grade Serous Ovarian Cancer | Platinum-based chemotherapy [2] [1] | SOX9 epigenetically upregulated after chemotherapy; induces stem-like transcriptional state | Shorter overall survival for patients with high SOX9 (HR=1.33) [1] |
| Ovarian Cancer | PARP inhibitor resistance [9] | USP28 stabilizes SOX9, enhancing DNA damage repair gene expression | Contributes to olaparib resistance; combination therapy potential |
| Gastrointestinal Cancer | Radiotherapy resistance [21] | SOX9 regulates radioresistant intestinal stem cells; crucial in CSCs | Potential for SOX9 inhibition to enhance radiotherapy efficacy |
| Breast Cancer | Chemotherapy and targeted therapy resistance [7] | Promotes cancer stem cell properties; regulates multiple resistance pathways | Associated with poor prognosis and treatment failure |
| Hepatocellular Carcinoma | Multiple therapy resistance [62] | Activates Wnt/β-catenin signaling; confers stemness features | Linked to poorer disease-free and overall survival |
| Glioblastoma | Prognostic biomarker [13] | High SOX9 expression correlates with IDH-mutant status | Diagnostic and prognostic biomarker potential |
Core Resistance Mechanisms
SOX9 drives therapy resistance through several interconnected molecular pathways:
- Cancer Stem Cell Reprogramming: SOX9 reprograms non-stem cancer cells into stem-like cells with inherent drug tolerance [2] [1]
- Enhanced DNA Damage Repair: SOX9 binds promoters of DNA repair genes (SMARCA4, UIMC1, SLX4), enhancing repair capability [9]
- Transcriptional Plasticity: SOX9 increases transcriptional divergence, enabling adaptive responses to therapy [1]
- Epigenetic Reprogramming: SOX9 is regulated by super-enhancers and epigenetic modifications in resistant cells [2] [1]
- Immune Evasion: SOX9 helps maintain dormant cancer cells that evade immune surveillance [7]
Troubleshooting SOX9 Research: Frequently Asked Questions
Q1: Our SOX9 knockout models show unexpected proliferation changes instead of the expected chemotherapy sensitization. What might be happening?
A: This reflects SOX9's context-dependent functions. In SOX9-depleted ovarian cancer cells, accelerated growth rates were observed without chemotherapy, while carboplatin sensitivity significantly increased [1]. This paradoxical effect underscores the importance of:
- Conducting baseline proliferation assays before resistance testing
- Using appropriate controls for context-specific SOX9 functions
- Implementing multiple SOX9 modulation approaches (CRISPR, siRNA, pharmacological) to confirm phenotype specificity
Q2: We're observing inconsistent SOX9 upregulation after platinum treatment in our ovarian cancer models. What factors affect this response?
A: SOX9 induction dynamics depend on several variables confirmed in primary patient samples [2] [1]:
- Temporal factors: Significant SOX9 upregulation occurs within 72 hours of carboplatin exposure
- Cell population heterogeneity: Single-cell analyses reveal rare SOX9-high populations even in treatment-naive tumors
- Epigenetic status: SOX9 is regulated by super-enhancers that vary between models
- Technical considerations: Ensure consistent timing post-treatment and use multiple detection methods (RNA, protein)
Q3: Our SOX9 inhibition strategy isn't reversing PARP inhibitor resistance. What alternative mechanisms should we investigate?
A: Consider the USP28-SOX9 stabilization axis identified in recent olaparib resistance mechanisms [9]:
- Check USP28 expression levels, as it stabilizes SOX9 against FBXW7-mediated degradation
- Test the USP28 inhibitor AZ1 in combination with SOX9 targeting
- Examine SOX9 ubiquitination status in your resistant models
- Analyze downstream DNA damage repair genes (SMARCA4, UIMC1, SLX4) for compensatory expression
Q4: We're struggling to identify reliable biomarkers for SOX9-mediated resistance. What approaches show clinical promise?
A: Multiple approaches have demonstrated utility:
- Single-cell RNA sequencing: Identifies rare SOX9-expressing stem-like clusters in primary tumors [1]
- Transcriptional divergence metrics: P50/P50 ratio quantifies SOX9-associated transcriptional plasticity [1]
- Immunohistochemical staining: SOX9 levels in patient samples pre- and post-chemotherapy correlate with resistance [2]
- Immune infiltration analysis: SOX9 correlates with specific immune cell populations in glioblastoma [13]
Essential Experimental Protocols
Protocol: Profiling SOX9-Mediated Chemoresistance in Ovarian Cancer Models
Background: This protocol establishes SOX9-driven chemoresistance in high-grade serous ovarian cancer (HGSOC) lines, based on methods that successfully modeled platinum resistance [2] [1].
Materials:
- HGSOC cell lines (OVCAR4, Kuramochi, COV362)
- Carboplatin or cisplatin
- SOX9 modulators: CRISPR/Cas9 system for knockout, expression vectors for overexpression
- Antibodies: SOX9 (AB5535, Sigma-Aldrich), β-actin loading control
- RNA sequencing capabilities for transcriptome analysis
Procedure:
- Establish baseline: Characterize endogenous SOX9 expression in your HGSOC lines via Western blot (20-40 μg protein lysate, 8-15% gel)
- Chemotherapy exposure: Treat cells with IC50 carboplatin for 72 hours; harvest samples at 24h, 48h, and 72h for SOX9 expression analysis
- SOX9 modulation:
- For knockout: Use CRISPR/Cas9 with SOX9-targeting sgRNA [1]
- For overexpression: Induce SOX9 expression via epigenetic modulators or expression vectors
- Functional resistance assays:
- Colony formation assays post-carboplatin treatment (2-tailed Student's t-test, expected p=0.0025) [1]
- Incucyte live-cell imaging for growth kinetics with/without chemotherapy
- Stemness characterization:
- Transcriptome analysis after SOX9 induction to identify stemness signatures
- Single-cell RNA sequencing to identify rare stem-like subpopulations
Troubleshooting:
- If SOX9 induction is inconsistent, verify epigenetic status and consider histone deacetylase inhibitors
- For poor colony formation, optimize seeding density and drug exposure duration
- Confirm SOX9 manipulation efficiency with parallel Western blot validation
Protocol: Assessing the USP28-SOX9 Axis in PARP Inhibitor Resistance
Background: This protocol evaluates the novel USP28-SOX9 stabilization mechanism in PARP inhibitor resistance, based on recent findings in ovarian cancer models [9].
Materials:
- Ovarian cancer cell lines (SKOV3, UWB1.289)
- PARP inhibitor (olaparib)
- USP28 inhibitor (AZ1)
- Proteasome inhibitor (MG132)
- Cycloheximide (CHX)
- Co-immunoprecipitation reagents
Procedure:
- Generate resistant models: Treat parental SKOV3 cells with increasing olaparib concentrations (0.1-10 μM) over 3-6 months
- Verify SOX9 involvement: Compare SOX9 protein levels in parental vs. resistant lines via Western blot
- Test USP28 dependence:
- Treat resistant cells with AZ1 (USP28 inhibitor) for 24h
- Measure SOX9 protein half-life using cycloheximide chase assay (100 μg/mL)
- Assess SOX9 ubiquitination with MG132 (10 μM, 6h) + immunoprecipitation
- Functional rescue experiments:
- Test olaparib sensitivity with/without AZ1 pretreatment
- Measure DNA damage repair capacity via γH2AX foci formation
- Assess colony formation under combination treatment
Validation:
- Confirm USP28-SOX9 interaction via co-immunoprecipitation
- Perform ChIP-seq for SOX9 binding to DNA repair gene promoters
- Evaluate downstream DNA repair genes (SMARCA4, UIMC1, SLX4) by qRT-PCR
Visualization: SOX9 Resistance Pathways
SOX9-Mediated Therapy Resistance Mechanism
Experimental Workflow for SOX9 Resistance Profiling
Research Reagent Solutions
Table 2: Essential Reagents for SOX9 Resistance Research
| Reagent/Category | Specific Examples | Application & Function | Validation Notes |
|---|---|---|---|
| SOX9 Antibodies | Anti-SOX9 (AB5535, Sigma-Aldrich) [9] | Western blot, IHC; detects SOX9 expression changes | Validate specificity with KO controls; works for protein-level analysis |
| SOX9 Modulators | CRISPR/Cas9 with SOX9 sgRNA [1] | Genetic knockout; establishes SOX9 necessity | Confirm efficiency via Western; off-target effects possible |
| SOX9 expression vectors [2] | SOX9 overexpression; tests sufficiency for resistance | Use inducible system for controlled expression | |
| Targeted Inhibitors | USP28 inhibitor (AZ1) [9] | Blocks SOX9 stabilization; reverses PARPi resistance | Use 1-10 μM range; monitor SOX9 degradation kinetics |
| Cell Line Models | HGSOC lines (OVCAR4, Kuramochi, COV362) [1] | Platinum resistance models; show SOX9 induction | Confirm SOX9 inducibility in your specific stock |
| PARPi-resistant derivatives (SKOV3/Ola) [9] | Models of acquired PARPi resistance | Maintain under selective pressure | |
| Functional Assays | Colony formation assay [1] | Quantifies long-term survival post-treatment | Standardize seeding density; multiple replicates essential |
| Single-cell RNA sequencing [1] | Identifies rare SOX9-high stem-like populations | Requires fresh viable cells; analyze transcriptional divergence |
Successfully profiling and targeting SOX9-mediated resistance requires a multi-faceted approach that addresses both the transcriptional and post-translational regulation of SOX9. Key strategic considerations include:
- Combination Therapies: Target SOX9 stabilization pathways (e.g., USP28 inhibitors with PARP inhibitors) rather than SOX9 itself [9]
- Timing Considerations: Intervene early in SOX9 induction before stable resistance establishment [2] [1]
- Heterogeneity Management: Address rare SOX9-high subpopulations through single-cell approaches [1]
- Biomarker Integration: Implement SOX9 expression and transcriptional divergence metrics for patient stratification [1] [13]
The experimental frameworks and troubleshooting guides provided here establish a foundation for developing comprehensive strategies to overcome SOX9-mediated therapy resistance across cancer types.
Clinical Trial Design Considerations for SOX9-Targeted Agents
FAQs on SOX9 Biology and Therapeutic Targeting
1. What is the clinical evidence that SOX9 is a relevant target in cancer therapy? SOX9 is a transcription factor frequently overexpressed in various solid malignancies, and its elevated expression is strongly correlated with poor patient prognosis and therapy resistance. In high-grade serous ovarian cancer (HGSOC), patients in the top quartile of SOX9 expression had significantly shorter overall survival compared to those in the bottom quartile. Research has demonstrated that SOX9 is not merely a biomarker but a functional driver of chemoresistance. Chemotherapy treatment robustly induces SOX9 upregulation within 72 hours in HGSOC cell lines, and this induction is recapitulated in patient tumors following platinum-based chemotherapy [1] [2]. Similar roles for SOX9 in driving resistance have been observed in other cancers, including PARP inhibitor resistance in ovarian cancer and immunotherapy resistance in lung cancer [9] [63].
2. What is the primary mechanistic role of SOX9 in promoting therapy resistance? SOX9 promotes therapy resistance through two key, interconnected mechanisms. First, it acts as a master regulator that reprograms the transcriptional state of naive cancer cells into a stem-like state. These cancer stem cells (CSCs) are inherently more drug-tolerant and possess self-renewal capabilities [1] [2]. Second, SOX9 enhances DNA damage repair (DDR) capabilities. In ovarian cancer, SOX9 binds to the promoters of key DDR genes (SMARCA4, UIMC1, and SLX4), enabling cells to more effectively repair chemotherapy-induced DNA damage [9]. This reprogramming into a stem-like state is associated with increased transcriptional divergence, a metric for transcriptional plasticity and a poor prognostic indicator [1].
3. What are the considerations for patient stratification in SOX9-targeted trials? Effective patient stratification should be based on biomarkers that indicate active SOX9-mediated resistance.
- SOX9 Expression Levels: Tumors with high SOX9 expression, especially those that show further induction post-chemotherapy, are prime candidates [1] [2].
- SOX9 Protein Stability Machinery: Tumors with high expression of deubiquitinating enzymes like USP28, which stabilizes the SOX9 protein, may be particularly sensitive to strategies that target SOX9 stability [9].
- Stemness and DDR Signatures: Patients whose tumors express gene signatures associated with a stem-like state or enhanced DNA damage repair could be prioritized for enrollment [1] [9].
- Immune Contexture: In cancers like lung cancer, high SOX9 expression creates an "immune cold" tumor microenvironment, which may predict poor response to immunotherapy alone and identify patients who could benefit from SOX9-targeted combinations [63].
Troubleshooting Guide: Overcoming SOX9-Mediated Resistance
Challenge 1: Targeting a Transcription Factor
Problem: SOX9 is a transcription factor, making it traditionally difficult to target with small-molecule inhibitors directly.
Solutions:
- Target Upstream Regulators: Focus on the pathways that control SOX9 expression and stability. For instance, the deubiquitinating enzyme USP28 stabilizes SOX9 by preventing its FBXW7-mediated degradation. The USP28-specific inhibitor AZ1 has been shown to reduce SOX9 protein levels and re-sensitize cancer cells to PARP inhibitors [9].
- Target Downstream Effectors: Identify and inhibit critical downstream genes in the SOX9 regulatory network. CDK7 inhibition has shown promise in SOX9-driven gallbladder cancer models by targeting super-enhancer-driven transcription dependencies [64].
- Epigenetic Modulation: Since SOX9 is regulated by super-enhancers, epigenetic drugs that disrupt super-enhancer function could indirectly dampen SOX9 expression and its oncogenic program [1] [64].
Challenge 2: Heterogeneity of SOX9-Positive Cells
Problem: SOX9-expressing cells can constitute a rare subpopulation within tumors, making it difficult to assess target engagement and therapeutic effect in bulk analyses.
Solutions:
- Leverage Single-Cell Technologies: Utilize single-cell RNA sequencing (scRNA-Seq) to identify and characterize the rare cluster of SOX9-high, stem-like cells in patient samples before and after treatment. This allows for precise monitoring of this subpopulation in response to therapy [1].
- Monitor Transcriptional Divergence: Use the transcriptional divergence metric (P50/P50) as a functional readout of SOX9 activity and stem-like plasticity at a single-cell level. A successful therapeutic intervention should reduce the overall transcriptional divergence in the tumor cell population [1].
Challenge 3: Rapid Development of Resistance to Single-Agent Therapies
Problem: As with most targeted therapies, monotherapies are likely to fail due to adaptive resistance and redundant pathways.
Solutions:
- Rational Combination Therapies: Design trials combining SOX9-targeting strategies with standard-of-care or other targeted agents.
- With Chemotherapy: A SOX9-targeting agent could be administered to prevent the emergence of a stem-like, chemoresistant subpopulation during platinum-based chemotherapy [1] [2].
- With PARP Inhibitors: In ovarian cancer, combining a USP28 inhibitor (to degrade SOX9) with a PARP inhibitor like olaparib has demonstrated efficacy in overcoming PARPi resistance [9].
- With Immunotherapy: In "immune cold" SOX9-high tumors (e.g., KRAS-mutant lung cancer), a SOX9-targeting agent could be used to remodel the tumor microenvironment and sensitize tumors to immune checkpoint inhibitors [63].
Experimental Protocols for Key Assessments
Protocol 1: Assessing SOX9-Mediated Transcriptional Reprogramming
Method: Single-Cell RNA Sequencing (scRNA-Seq) Analysis
- Sample Preparation: Generate single-cell suspensions from patient-derived xenografts (PDXs) or dissociated patient tumor samples, collected both pre- and post-treatment.
- Library Preparation & Sequencing: Use a standard scRNA-Seq platform (e.g., 10x Genomics) to prepare libraries and sequence according to manufacturer protocols.
- Bioinformatic Analysis:
- Clustering: Perform quality control, normalization, and clustering of cells using tools like Seurat or Scanpy.
- SOX9 Expression: Overlay SOX9 expression onto UMAP plots to identify SOX9-high clusters.
- Stemness Signature: Score cells for established stemness gene signatures.
- Transcriptional Divergence: Calculate the transcriptional divergence (P50/P50 ratio) for each cell as described [1]:
Sum of expression of top 50% expressed genes / Sum of expression of bottom 50% expressed genes.
- Interpretation: A successful SOX9-targeting agent will reduce the size of the SOX9-high cluster, decrease the average stemness score, and lower the transcriptional divergence of the tumor cell population [1].
Protocol 2: Validating SOX9 Protein Stability Mechanisms
Method: Co-immunoprecipitation (Co-IP) and Ubiquitination Assay
- Cell Lysis: Lyse ovarian cancer cells (e.g., SKOV3, UWB1.289) treated with a USP28 inhibitor (AZ1) or DMSO control in IP lysis buffer.
- Immunoprecipitation: Incubate cell lysates with an anti-SOX9 antibody or normal IgG (negative control) overnight at 4°C. Add protein A/G magnetic beads for 2 hours.
- Ubiquitination Detection: Wash beads, boil in SDS loading buffer, and analyze by Western blot.
- Probe the blot with an anti-Ubiquitin antibody to detect poly-ubiquitinated SOX9.
- Re-probe the blot with an anti-SOX9 antibody to confirm total immunoprecipitated SOX9.
- Interpretation: Inhibition of USP28 should result in increased poly-ubiquitination of SOX9, indicating that the pathway for its proteasomal degradation has been restored [9].
Key Signaling Pathways and Workflows
Diagram 1: SOX9-Driven Therapy Resistance Mechanism
Diagram 2: Strategy for Targeting SOX9 Stability
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents for investigating SOX9 biology and validating targeting strategies.
| Reagent / Tool | Function / Application | Example / Catalog Consideration |
|---|---|---|
| USP28 Inhibitor (AZ1) | A specific small-molecule inhibitor of USP28. Used to test the hypothesis that inhibiting USP28 will lead to SOX9 degradation and re-sensitization to therapy [9]. | Selleck Chemicals, S8904 |
| Anti-SOX9 Antibody | Essential for detecting SOX9 protein levels via Western Blot, Immunofluorescence, and Immunohistochemistry in cell lines and patient samples [9]. | Sigma-Aldrich, AB5535 |
| CRISPR/Cas9 SOX9 KO Kit | For generating SOX9 knockout cell lines to validate the necessity of SOX9 in therapy resistance and to study phenotypic consequences [1] [2]. | Multiple commercial vendors; use sgRNAs targeting SOX9. |
| FBXW7 Expression Plasmid | Used to overexpress the E3 ligase FBXW7, which promotes SOX9 ubiquitination and degradation. A tool for mechanistic studies [9]. | Addgene, various clones |
| PARP Inhibitor (Olaparib) | Standard-of-care PARP inhibitor for ovarian cancer. Used in combination studies with SOX9-targeting agents to overcome resistance [9]. | Selleck Chemicals, AZD2281 |
| CDK7 Inhibitor | Transcriptional inhibitor that targets super-enhancers. A potential strategy to disrupt the SOX9-driven oncogenic program in SOX9-high cancers [64]. | E.g., THZ1 |
Conclusion
SOX9 stands as a critical node in the complex network of cancer therapy resistance, orchestrating processes from stem cell maintenance and DNA repair to immune modulation. The collective evidence underscores the high translational potential of targeting SOX9, either directly or through its regulatory pathways, to re-sensitize tumors to standard treatments. Future research must focus on refining targeted delivery systems to improve therapeutic indices, validating robust SOX9-based biomarkers for patient selection, and designing innovative clinical trials that test SOX9 inhibition in rational combination regimens. Successfully overcoming SOX9-mediated resistance holds the promise of significantly improving survival outcomes for patients across multiple hard-to-treat cancers.
References
- 1. SOX9 drives a stem-like transcriptional state and platinum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483608/]
- 2. Transcription Factor Drives Chemotherapy Resistance in ... [https://news.feinberg.northwestern.edu/2025/10/30/transcription-factor-drives-chemotherapy-resistance-in-ovarian-cancer/]
- 3. CDK1 drives SOX9-mediated chemotherapeutic resistance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12506374/]
- 4. Sox9: A potential regulator of cancer stem cells in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11229887/]
- 5. The local and circulating SOX9 as a potential biomarker for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7292907/]
- 6. Upregulation of SOX9 promotes cell proliferation, migration ... [https://www.spandidos-publications.com/10.3892/ol.2015.3303]
- 7. SOX9: an important factor in regulating breast cancer [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-02730-0]
- 8. Focusing on a pivotal axis in chemoresistance [https://www.asbmb.org/asbmb-today/science/032424/focusing-on-a-pivotal-axis-in-chemoresistance]
- 9. USP28 promotes PARP inhibitor resistance by enhancing ... [https://www.nature.com/articles/s41419-025-07647-4]
- 10. Targeting SOX9 May Help Overcome Ovarian Cancer ... [https://breakthroughsforphysicians.nm.org/obgyn-research-article-transcription-factor-ovarian-cancer]
- 11. USP28 promotes PARP inhibitor resistance by enhancing ... [https://pubmed.ncbi.nlm.nih.gov/40240356/]
- 12. Super-enhancer inhibitors THZ2 and JQ1 reverse ... [https://www.oaepublish.com/articles/cdr.2025.105]
- 13. High expression of SOX9 is a diagnostic and prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277172/]
- 14. Role of the SOX family in cancer immune evasion [https://pmc.ncbi.nlm.nih.gov/articles/PMC11789896/]
- 15. SOX9: a novel janus-faced regulator in immunity and its ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1700812/full]
- 16. SOX9: an important factor in regulating breast cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360010/]
- 17. Upregulated SOX9 expression indicates worse prognosis in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5762580/]
- 18. High expression of SOX9 is a diagnostic and prognostic ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1531937/full]
- 19. SOX9 drives a stem-like transcriptional state and platinum ... [https://pubmed.ncbi.nlm.nih.gov/41031891/]
- 20. The pioneer factor SOX9 competes for epigenetic factors to ... [https://www.nature.com/articles/s41556-023-01184-y]
- 21. Inhibition of SOX9 may be an effective target for increasing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5451632/]
- 22. SOX9 siRNA Loaded Lipid Nanoparticles Actively Targeted [https://pubmed.ncbi.nlm.nih.gov/40717437/]
- 23. The SOX -MMS22L Axis Promotes Oxaliplatin 9 in... Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC8191464/]
- 24. SOX9-regulated cell plasticity in colorectal metastasis is ... [https://www.nature.com/articles/srep32350]
- 25. SOX9 is an atypical intestinal tumor suppressor controlling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5347687/]
- 26. Study of the mechanism by which dinaciclib induces apoptosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6675732/]
- 27. Dinaciclib, a cyclin-dependent kinase inhibitor, suppresses ... [https://www.nature.com/articles/s41598-020-75578-5]
- 28. Dinaciclib (SCH727965) inhibits the unfolded protein ... [https://pubmed.ncbi.nlm.nih.gov/24362465/]
- 29. Inhibition of cyclin dependent kinase 9 by dinaciclib ... [https://www.oncotarget.com/article/10870/text/]
- 30. LPA Regulates SOX9 in Ovarian Cancer Cells [https://www.gavinpublishers.com/article/view/lpa-regulates-sox9-in-ovarian-cancer-cells]
- 31. SOX5 inhibition overcomes PARP inhibitor resistance in ... [https://www.nature.com/articles/s41419-025-07660-7]
- 32. Current advances in prognostic and diagnostic biomarkers ... [https://www.sciencedirect.com/science/article/pii/S0753332221012749]
- 33. SOX9 as an emerging target for anticancer drugs and a ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644622002136]
- 34. Emerging insights of tumor heterogeneity and drug resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6902404/]
- 35. Single-cell transcriptomics reveals biomarker ... [https://www.nature.com/articles/s41523-025-00803-1]
- 36. Landscape of small nucleic acid therapeutics: moving from the bench to the clinic as next-generation medicines | Signal Transduction and Targeted Therapy [https://www.nature.com/articles/s41392-024-02112-8]
- 37. Optimized Lipid Nanoparticle-Mediated mRNA Co-Delivery of SOX5/SOX9 En | IJN [https://www.dovepress.com/optimized-lipid-nanoparticle-mediated-mrna-co-delivery-of-sox5sox9-ena-peer-reviewed-fulltext-article-IJN]
- 38. RNAscope Troubleshooting Guide and FAQ [https://acdbio.com/technical-support/solutions]
- 39. Nucleic Acid Quantification Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/nucleic-acid-purification-analysis-support-center/nucleic-acid-quantification-support/nucleic-acid-quantification-support-troubleshooting.html]
- 40. Cross-regulation between SOX9 and the canonical Wnt ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10469848/]
- 41. Enhanced disc regeneration through CRISPR/Cas9-mediated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465725/]
- 42. Suppression of feedback loops mediated by PI3K/mTOR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4222988/]
- 43. Signaling Pathways in Cancer: Therapeutic Targets ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8002322/]
- 44. MALAT1-miR-101-SOX9 feedback loop modulates the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5706876/]
- 45. A Sox2–Sox9 signalling axis maintains human breast ... [https://www.nature.com/articles/s41388-018-0656-7]
- 46. The SOX9-Aldehyde Dehydrogenase Axis Determines ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6944474/]
- 47. overcoming resistance in lung and colorectal cancer [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1554256/full]
- 48. Immunohistochemical staining of ERG and SOX as... | Oncotarget 9 [https://www.oncotarget.com/article/13407/text/]
- 49. interacts with FOXC1 to activate MYC and regulate... SOX 9 [https://pubmed.ncbi.nlm.nih.gov/32398735/]
- 50. Clinically oriented prediction of patient response to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10029756/]
- 51. Patient-derived xenograft models: Current status, challenges ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12179623/]
- 52. Patient-derived xenograft models in cancer therapy [https://www.nature.com/articles/s41392-023-01419-2]
- 53. One-step generation of conditional and reversible gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5777571/]
- 54. Knockdown of SOX9 Inhibits the Proliferation, Invasion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7840816/]
- 55. Short Hairpin RNA (shRNA): Design, Delivery, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3679364/]
- 56. Genetics, Epigenetic Mechanism - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK532999/]
- 57. siRNA Design Guidelines | Technical Bulletin #506 [https://www.thermofisher.com/us/en/home/references/ambion-tech-support/rnai-sirna/general-articles/-sirna-design-guidelines.html]
- 58. Discovery of small molecule cancer drugs [https://pmc.ncbi.nlm.nih.gov/articles/PMC3476506/]
- 59. Epigenetic control of SOX9 gene by the histone ... [https://www.sciencedirect.com/science/article/pii/S2405844024092041]
- 60. Histone acetylation influences the activity of Sox9-related ... [https://pubmed.ncbi.nlm.nih.gov/21173804/]
- 61. USP28 promotes PARP inhibitor resistance by enhancing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12003857/]
- 62. SOX9 Stem-Cell Factor: Clinical and Functional Relevance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6463569/]
- 63. Studying the Role of Sox9 in Lung Cancer [https://news.cuanschutz.edu/cancer-center/sox9-in-lung-cancer]
- 64. Super-Enhancer Reprograming Driven by SOX and... 9 [https://pubmed.ncbi.nlm.nih.gov/39492805/]