Targeting SOX9 with CRISPR-Cas9: A Guide for Immune Cell Engineering in Cancer and Disease
This article provides a comprehensive resource for researchers and drug development professionals on the application of CRISPR-Cas9 technology for modulating SOX9 in immune cell models.
Targeting SOX9 with CRISPR-Cas9: A Guide for Immune Cell Engineering in Cancer and Disease
Abstract
This article provides a comprehensive resource for researchers and drug development professionals on the application of CRISPR-Cas9 technology for modulating SOX9 in immune cell models. SOX9, a transcription factor with a dual 'Janus-faced' role in immunology, is a promising therapeutic target in cancer and inflammatory diseases. We explore the foundational biology of SOX9 in immune regulation, detail methodological strategies for its knockout or modulation in immune cells, address common troubleshooting and optimization challenges, and outline rigorous validation protocols. By integrating foundational knowledge with practical application and validation frameworks, this guide aims to accelerate the use of CRISPR-Cas9-engineered immune models in basic research and therapeutic development.
SOX9: The Janus-Faced Regulator of Immunity and a Prime Target for CRISPR Intervention
The Sex-determining Region Y-related High-Mobility Group Box 9 (SOX9) is a transcription factor with an evolutionarily conserved High Mobility Group (HMG) box DNA-binding domain that plays context-dependent roles in immunology [1]. This protein exhibits a remarkable dual nature: it can promote tumor immune escape by creating immunosuppressive environments, while in other settings, it drives tissue repair processes in conditions like osteoarthritis and liver fibrosis [1] [2]. This functional duality, akin to a "double-edged sword," positions SOX9 as a critical regulator at the intersection of immunity, cancer biology, and regenerative medicine [1]. With the advent of precise genetic tools like CRISPR-Cas9, researchers can now systematically dissect SOX9's complex functions in immune cell models, offering new avenues for therapeutic intervention in both cancer and inflammatory diseases.
Molecular Structure and Functional Domains of SOX9
The human SOX9 protein contains several functionally specialized domains that enable its diverse roles. These domains are organized from N- to C-terminus as follows [1]:
- Dimerization Domain (DIM): Facilitates protein-protein interactions
- HMG Box Domain: Binds DNA and contains nuclear localization/export signals
- Central Transcriptional Activation Domain (TAM)
- Proline/Glutamine/Alanine (PQA)-rich Domain: Essential for transcriptional activation
- C-terminal Transcriptional Activation Domain (TAC): Interacts with cofactors like Tip60
Table 1: Functional Domains of SOX9 Protein
| Domain | Position | Key Functions |
|---|---|---|
| Dimerization Domain (DIM) | N-terminal | Facilitates protein-protein interactions and complex formation |
| HMG Box Domain | Central | DNA binding, nuclear localization, DNA bending |
| Transcriptional Activation Domain (TAM) | Middle | Synergizes with TAC to enhance transcriptional potential |
| PQA-rich Domain | C-terminal | Necessary for transcriptional activation |
| Transcriptional Activation Domain (TAC) | C-terminal | Interacts with cofactors (e.g., Tip60), inhibits β-catenin |
The HMG domain enables SOX9 to recognize specific DNA sequences (CCTTGAG) and induce DNA bending, thereby altering chromatin architecture and facilitating the assembly of transcriptional complexes [1] [3]. The transcriptional activation domains (TAM and TAC) work synergistically to recruit additional co-factors that determine the specificity of SOX9's regulatory functions across different cellular contexts [1].
SOX9 in Tumor Immune Evasion: Mechanisms and Research Approaches
Key Mechanisms of Immune Evasion
In cancer biology, SOX9 frequently exhibits oncogenic properties through multiple mechanisms that enable tumors to evade immune surveillance [1] [4] [5]:
Modulation of Immune Cell Infiltration: SOX9 expression correlates with altered patterns of immune cell infiltration in the tumor microenvironment. In colorectal cancer, SOX9 negatively correlates with infiltration of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while positively correlating with neutrophils, macrophages, activated mast cells, and naive/activated T cells [1].
Impairment of Anti-Tumor Immunity: SOX9 overexpression negatively correlates with genes associated with the function of CD8+ T cells, NK cells, and M1 macrophages, effectively creating an "immune desert" microenvironment that promotes tumor immune escape [1].
Stemness and Dormancy Regulation: SOX9 helps maintain tumor cells in a stem-like, dormant state that evades immune detection, particularly in breast cancer models [5] [3]. This dormancy allows cancer cells to persist undetected for extended periods before potentially causing recurrence.
Immune Checkpoint Regulation: A SOX9-B7x (B7-H4) axis has been identified in breast cancer, where SOX9 upregulates this immune checkpoint molecule on dedifferentiated tumor cells, shielding them from T-cell-mediated killing [5].
Experimental Models and Data
Table 2: SOX9-Associated Immune Alterations in Cancer Microenvironments
| Cancer Type | Immune Parameter | Correlation with SOX9 | Functional Outcome |
|---|---|---|---|
| Colorectal Cancer | B cell infiltration | Negative | Reduced humoral anti-tumor immunity |
| Colorectal Cancer | CD8+ T cell function | Negative | Impaired cytotoxic T cell activity |
| Colorectal Cancer | Macrophage infiltration | Positive | Increased pro-tumor macrophage presence |
| Prostate Cancer | CD8+ CXCR6+ T cells | Decreased | Creation of "immune desert" microenvironment |
| Breast Cancer | B7x/B7-H4 expression | Positive | Protection from T cell-mediated killing |
| Multiple Cancers | Regulatory T cells | Positive | Enhanced immunosuppressive environment |
SOX9 in Tissue Repair and Regeneration: Protective Functions
Orchestrating Tissue Repair Mechanisms
In contrast to its pro-tumorigenic roles, SOX9 serves essential protective functions in tissue repair and regeneration across multiple organ systems:
Osteoarthritis and Cartilage Repair: SOX9 serves as the master transcription factor for chondrogenesis, directly regulating cartilage-specific matrix proteins including type II collagen and aggrecan [6]. In engineered mesenchymal stromal cells (MSCs), CRISPR-mediated SOX9 activation enhances chondrogenic potential and promotes cartilage integrity in osteoarthritic joints [6].
Liver Fibrosis and Granuloma Formation: During schistosomiasis infection, SOX9 is progressively upregulated in hepatic stellate cells (HSCs), cholangiocytes, and injured hepatocytes, where it orchestrates the formation of protective granulomas that contain parasitic egg toxins [2]. SOX9-deficient mice display disrupted granuloma architecture and more diffuse liver injury, highlighting its essential role in containing tissue damage [2].
Immune Modulation in Repair Contexts: In tissue repair scenarios, SOX9 helps maintain macrophage function and contributes to appropriate extracellular matrix deposition [1]. This stands in stark contrast to its tumor-promoting effects on macrophages, demonstrating how cellular context dictates functional outcomes.
Experimental Evidence for Protective Functions
Table 3: SOX9 in Tissue Repair and Regeneration Models
| Disease/Injury Model | SOX9 Function | Cell Types Involved | Experimental Outcome of SOX9 Manipulation |
|---|---|---|---|
| Osteoarthritis | Chondrogenesis master regulator | Chondrocytes, MSCs | CRISPRa-SOX9 enhances cartilage matrix production and integrity |
| Schistosomiasis liver infection | Granuloma formation and integrity | Hepatic stellate cells, hepatocytes | SOX9 deficiency causes disrupted granulomas and diffuse injury |
| Carbon tetrachloride liver fibrosis | Extracellular matrix production | Hepatic stellate cells | SOX9 loss alleviates fibrosis and improves liver function |
| General tissue repair | Macrophage function maintenance | Macrophages | SOX9 helps maintain reparative macrophage functions |
CRISPR-Cas9 Protocols for SOX9 Research in Immune Models
CRISPR-dCas9 System for SOX9 Activation and RelA Inhibition
The modular nature of CRISPR-dCas9 systems enables precise perturbation of SOX9 expression levels for functional studies in immune and stromal cell models [6]:
Experimental Workflow [6]:
Vector Construction:
- Clone lentiviral vectors expressing dSpCas9-VP64 (for activation) and dSaCas9-KRAB (for interference)
- Design and clone sgRNA expression vectors targeting SOX9 promoter regions and RelA transcription start sites
sgRNA Design and Screening:
- Design 5 sgRNAs for SOX9 targeting regions -74 to -276 bp upstream of transcription start site
- Design 5 sgRNAs for RelA targeting regions -41 to +155 bp relative to transcription start site
- Screen for optimal guide combinations using luciferase reporter assays and qPCR validation
Cell Engineering:
- Transduce bone marrow-derived mesenchymal stromal cells (BMSCs) with lentiviral vectors
- Select successfully transduced cells using antibiotic resistance (puromycin, blasticidin)
- Validate SOX9 upregulation and RelA knockdown via Western blot and qPCR
Functional Validation:
- Assess chondrogenic potential in pellet culture systems with TGF-β supplementation
- Evaluate immunomodulatory capacity through T cell suppression assays
- Test therapeutic efficacy in murine osteoarthritis models via intraarticular injection
Non-Viral RNP Delivery for SOX9 Knockout in Primary Cells
For primary human chondrocytes and immune cells, non-viral ribonucleoprotein (RNP) delivery offers high editing efficiency with minimal off-target effects [7]:
Step-by-Step Protocol [7]:
RNP Complex Assembly:
- Resuspend 60 pmol of purified Cas9 protein in 4.5 μL of electroporation buffer
- Combine with 5.2 μL (60 pmol) of synthetic sgRNA targeting SOX9 exon regions
- Incubate at room temperature for 10 minutes to form RNP complexes
Cell Preparation:
- Harvest primary human chondrocytes at 70-80% confluence (passage 2-4)
- Wash with PBS and resuspend at 1-2 × 10^6 cells per 100 μL of electroporation buffer
- Keep cells on ice until electroporation
Electroporation Parameters:
- Use Neon Transfection System (Thermo Fisher) with 10 μL tips
- Mix 100 μL cell suspension with pre-formed RNP complexes
- Electroporate using following parameters:
- Voltage: 1,400 mV
- Pulse Width: 10 ms
- Pulse Number: 3
- Immediately transfer cells to pre-warmed culture medium
Validation and Analysis:
- Assess editing efficiency 72 hours post-electroporation using T7E1 assay or next-generation sequencing
- Evaluate SOX9 knockout at protein level via Western blot (≥90% efficiency achievable)
- Analyze functional consequences in downstream assays (immune cell coculture, chondrogenesis, etc.)
Research Reagent Solutions for SOX9 Immunology Studies
Table 4: Essential Research Reagents for SOX9 Immune Function Studies
| Reagent Category | Specific Examples | Application/Function | Considerations for Immune Models |
|---|---|---|---|
| CRISPR Activation | dSpCas9-VP64, Sox9 sgRNAs | Precise SOX9 overexpression | Enables study of SOX9 gain-of-function in immune contexts |
| CRISPR Knockout | Cas9 RNP, SOX9-targeting sgRNAs | Complete SOX9 ablation | Ideal for primary immune cells with minimal off-target effects |
| Cell Models | BMSCs, primary chondrocytes, hepatocytes | Tissue repair studies | Primary cells best recapitulate native tissue properties |
| Animal Models | Surgical OA models, schistosomiasis infection | In vivo validation | Provides physiological context for immune interactions |
| Analysis Methods | scRNA-seq, CyTOF, multiplex IHC | Immune cell profiling | Enables comprehensive characterization of immune microenvironment changes |
| Immune Assays | T cell suppression, macrophage polarization | Functional immune analysis | Determines net effect of SOX9 on immune cell activity |
Therapeutic Implications and Future Directions
The dual nature of SOX9 in immunology presents both challenges and opportunities for therapeutic development. In oncology, SOX9 inhibition represents a promising strategy to counteract immune evasion and enhance response to checkpoint inhibitors [1] [5]. Conversely, in degenerative and inflammatory diseases such as osteoarthritis, targeted SOX9 activation could promote tissue regeneration while modulating destructive inflammation [6].
Future research directions should focus on:
Cell-Type Specific Targeting: Developing strategies to manipulate SOX9 in specific cell populations (e.g., cancer cells vs. reparative fibroblasts) to achieve desired therapeutic outcomes while minimizing side effects.
Context-Dependent Regulation: Understanding the signaling networks and epigenetic landscapes that determine whether SOX9 drives immune suppression versus tissue repair.
Advanced Delivery Systems: Optimizing viral and non-viral delivery methods for SOX9-targeting CRISPR systems to achieve spatial and temporal control of editing.
Combination Therapies: Exploring SOX9 modulation in combination with existing immunotherapies or regenerative medicine approaches.
The integration of precise genome engineering tools with sophisticated immune cell models will continue to elucidate the complex duality of SOX9 in immunological processes, ultimately enabling the development of targeted interventions for cancer, autoimmune diseases, and degenerative conditions.
The Sex-determining Region Y-related High-Mobility Group Box 9 (SOX9) protein is an evolutionarily conserved transcription factor that plays context-dependent, and often opposing, roles in cancer biology [1]. As a central regulator of embryonic development, chondrogenesis, and stem cell maintenance, SOX9 is frequently hijacked in malignancies, where its overexpression correlates strongly with tumor progression, therapeutic resistance, and poor patient prognosis [1] [8]. Beyond its established cell-autonomous functions in cancer cells, SOX9 is a pivotal orchestrator of the tumor microenvironment (TME), critically shaping immune cell infiltration and function. This application note details how SOX9 acts as a "double-edged sword," mediating both pro-tumorigenic immune evasion and, in specific contexts, tissue-reparative functions [1]. Framed within CRISPR-Cas9 research, we provide a detailed protocol for investigating SOX9 knockout in immune cell models to dissect its multifaceted role in cancer immunology.
SOX9 Structure and Functional Domains
The human SOX9 protein is a 509-amino acid polypeptide containing several key functional domains that govern its activity [1]:
- Dimerization Domain (DIM): Facilitates protein-protein interactions.
- HMG Box Domain: The defining DNA-binding motif that enables sequence-specific DNA binding and induces DNA bending.
- Transcriptional Activation Domains (TAM and TAC): Central and C-terminal domains that recruit co-activators to drive gene expression.
- P/Q/A-rich Domain: A proline/glutamine/alanine-rich region necessary for full transcriptional activation.
The embedded nuclear localization signal (NLS) within the HMG box ensures SOX9's nuclear translocation, which is essential for its function as a transcription factor [1].
Figure 1: Domain architecture of the human SOX9 protein, highlighting functional regions critical for its transcriptional activity.
SOX9-Mediated Remodeling of the Immune Microenvironment
SOX9 expression in tumors directly correlates with altered immune cell infiltration profiles, fostering an immunosuppressive TME. Bioinformatics analyses of human tumors reveal distinct patterns of immune cell association.
Table 1: Correlation between SOX9 Expression and Immune Cell Infiltration in Solid Tumors
| Immune Cell Type | Correlation with SOX9 | Reported Cancer Types | Functional Consequence |
|---|---|---|---|
| CD8+ T cells | Negative [1] | Colorectal Cancer [1] | Impaired cytotoxic T-cell function |
| Neutrophils | Positive [1] | Colorectal Cancer [1] | Increased immunosuppressive anergic neutrophils [1] |
| M2 Macrophages (TAMs) | Positive [1] [9] | Prostate Cancer, Glioblastoma [1] [9] | Promotion of an immunosuppressive milieu |
| Regulatory T cells (Tregs) | Positive [1] | Prostate Cancer [1] | Inhibition of effector T-cell activity |
| Naive/Activated T cells | Context-dependent [1] | Colorectal Cancer [1] | Altered T-cell activation dynamics |
| NK cells | Negative [1] | Pan-cancer analysis [1] | Reduced innate immune surveillance |
| M1 Macrophages | Negative [1] | Pan-cancer analysis [1] | Attenuation of anti-tumor immunity |
In glioblastoma (GBM), high SOX9 expression is closely linked to an immunosuppressive TME and shows promise as a diagnostic and prognostic biomarker, particularly in IDH-mutant cases [9]. Single-cell RNA sequencing of prostate cancer patients shows that SOX9-high tumor cells coexist with an "immune desert" TME, characterized by a loss of effector immune cells like CD8+CXCR6+ T cells and an enrichment of immunosuppressive Tregs and M2 macrophages [1].
Molecular Mechanisms of SOX9 in Immune Evasion and Stemness
SOX9 promotes tumor progression and therapy resistance through several key mechanisms:
Driving Chemoresistance and a Stem-like State
In high-grade serous ovarian cancer (HGSOC), SOX9 is epigenetically upregulated following platinum-based chemotherapy [8] [10]. This upregulation is sufficient to induce a stem-like transcriptional state and confer significant chemoresistance in vivo [8]. SOX9 expression is associated with increased transcriptional divergence, a metric for transcriptional plasticity and malleability that is amplified in cancer stem cells (CSCs) [8]. Analysis of patient samples pre- and post-neoadjuvant chemotherapy confirmed a significant population-level induction of SOX9, underscoring its role in adaptive chemoresistance [8].
Regulating Key Signaling Pathways
SOX9 interacts with multiple signaling pathways critical for cancer cell fate and immune interaction. It is a known repressor of the Wnt/β-catenin signaling pathway in certain contexts, such as bronchopulmonary dysplasia [11]. However, in cancers like ovarian cancer, its activity promotes pathways that maintain stemness. Furthermore, in vascular smooth muscle cells, SOX9 can be activated by the AMPK signaling pathway and subsequently bind to the STAT3 promoter to enhance phenotypic transformation [12], a pathway often co-opted in tumors.
Figure 2: Key molecular mechanisms of SOX9 in driving chemoresistance, phenotypic transformation, and immunosuppression.
Application Note: CRISPR-Cas9-Mediated SOX9 Knockout in an Immune Cell Co-Culture Model
Experimental Rationale
This protocol describes a methodology to investigate the cell-autonomous and non-cell-autonomous functions of SOX9 in cancer immunity. Using CRISPR-Cas9 to knockout SOX9 in cancer cells, followed by co-culture with immune cells, allows for the direct assessment of how SOX9 loss alters tumor-immune cell crosstalk, immune cell activation, and cytotoxic killing.
Detailed Protocol
Step 1: Design and Cloning of SOX9-Targeting sgRNAs
- Target Selection: Design 2-3 sgRNAs targeting early exons of the human SOX9 gene (e.g., within exon 1 or 2) to maximize frameshift potential. The HMG box domain (exons 2-3) is a critical target.
- sgRNA Sequences (Example):
- Cloning: Clone annealed sgRNA oligonucleotides into a lentiviral Cas9/sgRNA expression vector (e.g., lentiCRISPRv2). Include a non-targeting sgRNA as a negative control.
Step 2: Lentiviral Production and Cell Line Transduction
- Virus Production: Co-transfect HEK-293T cells with the lentiCRISPRv2-sgSOX9 plasmid and packaging plasmids (psPAX2, pMD2.G) using a standard transfection reagent.
- Virus Harvesting: Collect lentiviral supernatant at 48 and 72 hours post-transfection, concentrate via ultracentrifugation or PEG-it, and titrate.
- Target Cell Transduction: Transduce the target cancer cell line (e.g., OVCAR4 for ovarian cancer, a prostate cancer line, or a glioblastoma line) with the lentivirus in the presence of polybrene (8 µg/mL).
- Selection and Cloning: Select transduced cells with puromycin (1-2 µg/mL) for 5-7 days. Subsequently, single-cell clone the population by limiting dilution to isolate pure knockout clones.
Step 3: Validation of SOX9 Knockout
- Genomic DNA Analysis: Perform T7 Endonuclease I assay or Tracking of Indels by Decomposition (TIDE) analysis on PCR-amplified genomic target sites to confirm editing efficiency.
- Protein Analysis: Validate SOX9 knockout at the protein level by Western Blotting.
- Primary Antibody: Rabbit anti-SOX9 (1:1000 dilution)
- Lysis Buffer: RIPA buffer supplemented with protease and phosphatase inhibitors.
- Gel Electrophoresis: 4-12% Bis-Tris protein gel.
- Functional Validation: Confirm loss of function via qPCR for known SOX9 target genes (e.g., COL2A1 in chondrogenic models) or a significant reduction in colony formation in soft agar.
Step 4: Immune Cell Co-Culture and Functional Assays
- Immune Cell Isolation: Isve primary human CD8+ T cells or Natural Killer (NK) cells from healthy donor PBMCs using negative selection magnetic bead kits.
- Co-Culture Setup:
- Condition 1: SOX9-KO cancer cells + Immune cells
- Condition 2: Control (non-targeting sgRNA) cancer cells + Immune cells
- Use a 1:1 to 1:5 (cancer cell:immune cell) ratio in RPMI-1640 + 10% FBS. Include T-cell activation beads (e.g., CD3/CD28 Dynabeads) for T-cell co-cultures.
- Outcome Measures (48-72 hours post-co-culture):
- Flow Cytometry: Analyze immune cell activation markers (CD69, CD25 on T cells; CD107a degranulation on NK cells) and intracellular cytokines (IFN-γ, TNF-α).
- Cytotoxicity Assay: Use a real-time cell death assay (e.g., Incucyte Cytotoxicity Assay) or measure LDH release to quantify cancer cell killing.
- Cytokine Profiling: Use a multiplex ELISA (Luminex) to profile the culture supernatant for Th1/Th2 cytokines and chemokines.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for CRISPR-Cas9 SOX9 Knockout and Functional Validation
| Reagent / Tool | Function / Application | Example Product / Identifier |
|---|---|---|
| lentiCRISPRv2 vector | All-in-one lentiviral vector for Cas9 and sgRNA expression | Addgene #52961 |
| SOX9 Antibody (Rabbit mAb) | Validation of SOX9 knockout by Western Blot | Abcam ab185966, Cell Signaling #82630 |
| Puromycin | Selection of successfully transduced cells | Thermo Fisher, Cat# A1113803 |
| Lentiviral Packaging Mix | For production of lentiviral particles | psPAX2 & pMD2.G (Addgene) |
| Polybrene | Enhances lentiviral transduction efficiency | Sigma-Aldrich, H9268 |
| CD8+ T Cell Isolation Kit | Negative selection for primary human CD8+ T cells | Miltenyi Biotec, #130-096-495 |
| CD3/CD28 Activator | For T cell activation in co-culture assays | Gibco, #11131D |
| IFN-γ ELISA Kit | Quantification of T-cell effector cytokine | R&D Systems, #DY285B |
| Annexin V / Propidium Iodide | Flow cytometry-based apoptosis detection | BioLegend, #640914 / #421301 |
SOX9 is a master regulator of the tumor microenvironment, driving immune evasion by shaping a suppressive immune landscape and promoting a therapy-resistant, stem-like state in cancer cells. The application of CRISPR-Cas9 technology, as outlined in this note, provides a powerful and precise method to dissect the complex mechanisms by which SOX9 modulates tumor-immune interactions. The insights gained from such studies are vital for developing novel therapeutic strategies that target SOX9 or its downstream pathways to restore anti-tumor immunity and overcome chemoresistance.
The transcription factor SOX9 (SRY-related HMG-box 9) is a pivotal regulator of developmental processes, cell fate determination, and tissue homeostasis. As a key member of the SOX family of transcription factors, SOX9 contains a highly conserved high-mobility group (HMG) domain that enables specific DNA binding and modulation of transcriptional programs [13] [14]. Within the context of inflammatory diseases and cartilage homeostasis, SOX9 serves as a master regulator of chondrogenesis, directing the differentiation of mesenchymal progenitor cells into chondrocytes and maintaining the cartilage extracellular matrix (ECM) through transactivation of cartilage-specific genes including type II collagen (COL2A1) and aggrecan (ACAN) [13].
The critical role of SOX9 in skeletal development is evidenced by the fact that heterozygous mutations in and around the SOX9 gene cause Campomelic Dysplasia (CMPD), a severe skeletal malformation syndrome often associated with XY sex reversal [13]. Beyond development, SOX9 has emerged as a crucial factor in postnatal cartilage homeostasis and a promising therapeutic target for degenerative joint diseases like osteoarthritis (OA). OA is a prevalent joint disorder characterized by irreversible degradation of key ECM components, chondrocyte apoptosis, and inflammation, affecting over 500 million people worldwide and creating immense socioeconomic burden [6].
The integration of CRISPR-Cas9 technology into SOX9 research has revolutionized our ability to dissect its precise functions in immune cell models and cartilage biology, enabling the development of novel gene-editing approaches for therapeutic intervention. This Application Note delineates standardized protocols for investigating SOX9 in inflammatory contexts and for leveraging CRISPR-Cas9 to modulate SOX9 expression, providing researchers with robust methodologies to advance both basic science and translational applications.
SOX9 Biology and Mechanistic Insights
Molecular Structure and Functional Domains
The SOX9 protein contains several critical functional domains that determine its activity as a transcription factor:
- HMG Domain: A highly conserved ~79 amino acid DNA-binding domain that recognizes and binds to specific DNA sequences (A/TA/TCAAAG) in the minor groove, inducing DNA bending and facilitating the assembly of transcriptional complexes [13] [14].
- Dimerization Domain (DIM): Located upstream of the HMG domain, this domain enables DNA-dependent dimerization, with recent evidence suggesting it promotes homodimerization through DIM:HMG interactions rather than the previously hypothesized DIM:DIM interactions [13].
- Transactivation Domains: SOX9 contains two potent transactivation domains: TAM (Transactivation domain in the Middle) and TAC (Transactivation domain at the C-terminus). These domains synergize to activate chondrocyte-specific genes and interact with transcriptional co-activators including CBP, P300, and MED25 [13].
- PQA Domain: A unique vertebrate domain rich in prolines, glutamines, and alanines that helps stabilize SOX9 and facilitates transactivation without possessing intrinsic transactivation capability [13].
Table 1: SOX9 Protein Domains and Their Functions
| Domain | Location | Key Functions | Clinical Significance |
|---|---|---|---|
| HMG Domain | Central | DNA binding, DNA bending, nuclear import/export | All CMPD-causing missense mutations occur here |
| DIM Domain | Upstream of HMG | DNA-dependent dimerization | Mutations disrupt dimerization and cause CD |
| TAM | Middle region | Transcriptional activation, protein interactions | Essential for chondrogenic actions |
| TAC | C-terminus | Transcriptional activation, co-activator binding | Nonsense mutations cause CMPD |
| PQA | Variable | Protein stabilization, facilitates transactivation | Helps maintain SOX9 stability |
SOX9 as a Pioneer Transcription Factor
Emerging evidence positions SOX9 as a pioneer transcription factor capable of reprogramming cell fate by altering the chromatin landscape. In human umbilical vein endothelial cells (HUVECs), SOX9 expression alone is sufficient to activate mesenchymal genes and steer endothelial cells toward a mesenchymal fate through Endothelial-to-Mesenchymal Transition (EndMT) [14]. Genome-wide mapping of the chromatin landscape has revealed that SOX9 displays classic pioneer features, including opening of closed chromatin regions and leading to deposition of active histone modifications at previously silent regulatory elements. This reprogramming function is guided by the presence of SOX dimer motifs and enrichment of the histone variant H2A.Z [14].
Despite highly transient and dynamic SOX9 binding—possibly promoted through its eviction by histone phosphorylation—the changes SOX9 induces in the chromatin landscape and cell fate are persistent [14]. This pioneer capability enables SOX9 to initiate transcriptional programs that dictate cell identity and function, particularly in chondrogenesis and disease contexts.
SOX9 in Cartilage Homeostasis and Inflammation
In articular cartilage, SOX9 functions as a central regulator of ECM homeostasis by directly transactivating genes encoding critical cartilage matrix components, including collagen types II, IX, and XI, and aggrecan [13]. SOX9 operates in a complementary partnership with SOX5 and SOX6 (the SOX trio), which bind cooperatively with SOX9 on active enhancers and super-enhancers associated with hundreds of cartilage-specific genes, thereby potentiating SOX9's transactivation capacity [13].
Within the inflammatory context of osteoarthritis, pro-inflammatory cytokines such as interleukin-1β (IL-1β) and tumor necrosis factor-alpha (TNF-α) suppress SOX9 expression and activity, leading to decreased production of cartilage ECM components and increased expression of catabolic enzymes like matrix metalloproteinases (MMPs) and ADAMTS (a disintegrin and metalloproteinase with thrombospondin motifs) [15]. This imbalance accelerates cartilage degradation and disease progression. Notably, SOX9 overexpression can counteract these deleterious effects, restoring the anabolic-catabolic balance in chondrocytes even in the presence of inflammatory mediators [15].
Therapeutic Targeting of SOX9
Gene Therapy Approaches
Multiple gene therapy strategies have been developed to modulate SOX9 expression for therapeutic benefit:
Recombinant Adeno-Associated Virus (rAAV) Delivery: rAAV vectors enable long-term SOX9 expression in articular tissues. The therapeutic delivery of rAAV-SOX9 via polymeric micelles has been shown to counteract the effects of OA-associated inflammatory cytokines (IL-1β and TNF-α) in human articular chondrocytes, enhancing the deposition of ECM components and improving cell survival [15]. Polymeric micelles, particularly those based on polyethylene oxide (PEO) and polypropylene oxide (PPO), serve as effective carriers that prevent vector neutralization by antibodies present in patient joints.
Combination Therapies: Co-delivery of SOX9 with anti-inflammatory factors demonstrates enhanced therapeutic efficacy. For instance, simultaneous AAV-mediated delivery of SOX9 and IL-1Ra (interleukin-1 receptor antagonist) in surgically-induced OA animal models significantly improved abnormal gait, reduced subchondral bone lesions, decreased cartilage wear, and lowered pathological scores more effectively than either treatment alone [16]. This combination approach simultaneously addresses both the anabolic deficits (via SOX9) and inflammatory drivers (via IL-1Ra) of OA progression.
CRISPR-Based Modulation: The catalytically inactive dead Cas9 (dCas9) system enables precise transcriptional control of SOX9 without permanent genomic alterations. By fusing dCas9 to transcriptional activation domains (CRISPRa) or repression domains (CRISPRi), researchers can fine-tune SOX9 expression to therapeutic levels [6].
Table 2: Therapeutic Approaches for Modulating SOX9 Activity
| Therapeutic Approach | Mechanism | Key Findings | References |
|---|---|---|---|
| rAAV-SOX9 with polymeric micelles | Direct gene delivery to chondrocytes | Counters IL-1β and TNF-α effects; enhances ECM deposition | [15] |
| AAV co-delivery of SOX9 + IL-1Ra | Combined anabolic and anti-inflammatory strategy | Superior efficacy in reducing cartilage damage and pain | [16] |
| CRISPR-dCas9 SOX9 activation | Transcriptional upregulation without DNA cleavage | Enhances chondrogenic potential of MSCs; improves OA outcomes | [6] |
| Engineered MSC with SOX9/TGFβ1 | Cell therapy with enhanced chondrogenic capacity | Promotes disc regeneration; reduces inflammation | [17] |
CRISPR-Cas9 Applications in SOX9 Research
The versatility of CRISPR-Cas9 technology has enabled multiple innovative approaches for studying and manipulating SOX9:
Gene Editing and Reporter Systems: CRISPR-Cas9 has been utilized to introduce disease-relevant mutations into human induced pluripotent stem cells (iPSCs) for disease modeling. For instance, researchers have generated iPSC lines with heterozygous TRPV4 mutations (p.F273L and p.P799L) associated with chondrodysplasias in a SOX9-tdTomato reporter background, enabling real-time monitoring of cartilage differentiation through SOX9 expression [18].
Transcriptional Modulation: The dCas9 system allows precise control of SOX9 expression levels. In one application, researchers simultaneously activated SOX9 and inhibited RelA (a component of NF-κB signaling) in mesenchymal stromal cells (MSCs) using dSpCas9-VP64 and dSaCas9-KRAB, respectively [6]. This dual approach enhanced the chondrogenic potential of MSCs while dampening inflammatory responses, creating cells with improved therapeutic properties for OA treatment.
Multigene Engineering: CRISPR-Cas9 has enabled the integration of SOX9 along with other therapeutic factors into safe harbor loci. For example, tonsil-derived MSCs (ToMSCs) have been engineered with a tetracycline-off (Tet-off) regulatory system to co-express SOX9 and TGFβ1 following integration into the AAVS1 locus [17]. This approach enhances chondrogenic differentiation and ECM synthesis while minimizing oncogenic risks through controlled transgene expression.
Application Notes & Experimental Protocols
Protocol 1: CRISPR-Cas9-Mediated SOX9 Activation in Mesenchymal Stromal Cells
This protocol describes the simultaneous activation of SOX9 and inhibition of RelA in bone marrow-derived mesenchymal stromal cells (BMSCs) using CRISPR-dCas9 technology [6].
Materials
- Cell Line: Human bone marrow-derived mesenchymal stromal cells (BMSCs)
- CRISPR Plasmids:
- Lenti-dSpCas9-VP64 (for transcriptional activation)
- Lenti-dSaCas9-KRAB (for transcriptional repression)
- Lenti-EGFP-dual-gRNA (expressing two gRNA scaffolds for SpCas9 and SaCas9)
- Guide RNAs:
- SOX9-targeting: Sox9-2 (CGGGTTGGGTGACGAGACAGG) and Sox9-3 (ACTTACACACTCGGACGTCCC)
- RelA-targeting: RelA-1 (CCGAAATCCCCTAAAAACAGA) and RelA-3 (TGCTCCCGCGGAGGCCAGTGA)
- Culture Reagents: DMEM/F12 medium, fetal bovine serum (FBS), penicillin-streptomycin, polybrene
- Analysis Tools: qRT-PCR primers, Western blot antibodies for SOX9 and RelA
Procedure
Guide RNA Cloning:
- Design and synthesize oligonucleotides for SOX9 and RelA targeting guide RNAs (see sequences above).
- Clone gRNA sequences into the Lenti-EGFP-dual-gRNA vector using BsmBI restriction sites.
- Verify successful cloning by Sanger sequencing.
Lentiviral Production:
- Co-transfect HEK293T cells with the packaging plasmids (psPAX2 and pMD2.G) and the lentiviral vectors (Lenti-dSpCas9-VP64, Lenti-dSaCas9-KRAB, and Lenti-EGFP-dual-gRNA with SOX9 and RelA gRNAs) using polyethylenimine (PEI).
- Collect viral supernatants at 48 and 72 hours post-transfection.
- Concentrate lentiviral particles by ultracentrifugation at 70,000 × g for 2 hours.
- Resuspend viral pellets in PBS and aliquot for storage at -80°C.
Cell Transduction:
- Plate BMSCs at 50-60% confluence in 6-well plates.
- Transduce cells with a mixture of the three lentiviruses (dSpCas9-VP64, dSaCas9-KRAB, and EGFP-dual-gRNA) in the presence of 8 μg/mL polybrene.
- Centrifuge plates at 800 × g for 30 minutes (spinoculation) to enhance transduction efficiency.
- Replace virus-containing medium with fresh culture medium after 24 hours.
Selection and Validation:
- Sort successfully transduced cells by FACS based on EGFP expression 72 hours post-transduction.
- Validate SOX9 upregulation and RelA knockdown using qRT-PCR and Western blotting.
- Confirm functional effects through chondrogenic differentiation assays.
Figure 1: Workflow for CRISPR-mediated SOX9 activation in BMSCs
Expected Results
Successful implementation should yield:
- ≥3-fold increase in SOX9 mRNA expression compared to untransduced controls
- ≥60% reduction in RelA mRNA levels
- Enhanced chondrogenic differentiation capacity in pellet cultures
- Increased deposition of collagen type II and aggrecan in ECM
Protocol 2: Engineering SOX9/TGFβ1 Co-Expressing Tonsil-Derived MSCs
This protocol describes the generation of tonsil-derived mesenchymal stromal cells (ToMSCs) engineered to co-express SOX9 and TGFβ1 using CRISPR-Cas9-mediated integration into the AAVS1 safe harbor locus [17].
Materials
- Cell Source: Tonsil tissue from pediatric tonsillectomy (with appropriate ethical approval)
- CRISPR Components:
- pAAVS1-puro-Tetoff-SOX9-TGFβ1-CAG-tTA-Advanced plasmid
- pX458 plasmid expressing Cas9 and AAVS1-specific gRNA (5'-GGGGCCACTAGGGACAGGAT-3')
- Culture Reagents: DMEM/F12 medium, FBS, penicillin-streptomycin, puromycin, doxycycline
- Differentiation Media: StemPro Chondrogenesis, Osteogenesis, and Adipogenesis Differentiation Kits
Procedure
ToMSC Isolation and Culture:
- Obtain tonsil tissue from pediatric tonsillectomy with informed consent.
- Wash tissue twice with PBS and mince into small pieces (1-2 mm³).
- Digest tissue for 30 minutes at 37°C in RPMI 1640 medium containing 10 μg/mL DNase I and 210 U/mL collagenase type I.
- Filter digested tissue through a 100 μm cell strainer and wash with RPMI 1640 containing 20% FBS.
- Isolate mononuclear cells using Ficoll-Paque density gradient centrifugation.
- Seed cells at 1×10⁸ cells per T-125 flask in DMEM/F12 supplemented with 10% FBS, 100 μg/mL streptomycin, and 100 U/mL penicillin.
- Replace medium after 48 hours to remove non-adherent cells.
- Expand adherent cells and characterize by flow cytometry for MSC markers (CD44, CD73, CD90, CD105) and absence of hematopoietic markers (CD31, CD34, CD45).
CRISPR-Mediated Gene Integration:
- Co-transfect ToMSCs at passage 3-5 with pAAVS1-puro-Tetoff-SOX9-TGFβ1-CAG-tTA-Advanced and pX458-AAVS1 gRNA using Lipofectamine 3000.
- At 48 hours post-transfection, initiate selection with 1 μg/mL puromycin.
- Maintain selection for 7-10 days, replacing puromycin-containing medium every 3 days.
- Isolate single-cell clones by limiting dilution and expand for validation.
Validation of Engineered Cells:
- Confirm SOX9 and TGFβ1 transgene integration by genomic PCR across the 5' and 3' integration junctions.
- Verify doxycycline-regulated expression by treating cells with 1 μg/mL doxycycline for 72 hours and assessing SOX9 and TGFβ1 mRNA levels by qRT-PCR.
- Analyze protein expression by Western blot using anti-SOX9 and anti-TGFβ1 antibodies.
Functional Characterization:
- Assess chondrogenic differentiation capacity using pellet culture in chondrogenic differentiation medium for 21 days.
- Evaluate ECM production by Alcian blue staining for proteoglycans and immunohistochemistry for collagen type II.
- Compare chondrogenic potential with untransduced ToMSCs and single-factor expressing cells.
Figure 2: Workflow for engineering SOX9/TGFβ1-expressing ToMSCs
Expected Results
- Successful integration of SOX9 and TGFβ1 transgenes into the AAVS1 locus in >80% of puromycin-resistant clones
- Doxycycline-dependent transgene expression with >90% suppression in the presence of doxycycline
- Enhanced chondrogenic differentiation compared to control ToMSCs, evidenced by:
- 2-3 fold increase in collagen type II and aggrecan mRNA
- More intense Alcian blue staining indicating increased proteoglycan deposition
- Better organization of cartilage-like ECM in pellet cultures
Protocol 3: In Vivo Assessment of Engineered MSCs in Osteoarthritis Model
This protocol describes the evaluation of CRISPR-engineered SOX9-overexpressing MSCs in a surgical mouse model of osteoarthritis [6].
Materials
- Animals: 10-12 week old C57BL/6 mice (or appropriate strain for MSC compatibility)
- Surgical Materials: Microsurgical instruments, 30G needles, 5-0 vicryl suture
- Cells: CRISPR-engineered BMSCs with SOX9 activation and RelA inhibition
- Assessment Tools: von Frey filaments, MRI system, histological equipment
Procedure
Surgical Induction of Osteoarthritis:
- Anesthetize mice with ketamine/xylazine (100/10 mg/kg, i.p.) and confirm depth of anesthesia by absence of pedal reflex.
- Shave and disinfect the right knee joint area with alternating betadine and 70% ethanol.
- Make a medial parapatellar incision to expose the knee joint.
- Transect the anterior cruciate ligament (ACLT) and partially excise the medial meniscus (MMx) using microsurgical scissors.
- Irrigate the joint with sterile saline and close the incision in layers using 5-0 vicryl suture.
- Administer postoperative analgesia (buprenorphine, 0.1 mg/kg, s.c.) and monitor recovery.
Cell Administration:
- At 2 weeks post-surgery, randomize OA-induced mice into treatment groups:
- Group 1: CRISPR-engineered MSCs (SOX9 activation + RelA inhibition)
- Group 2: Unmodified MSCs
- Group 3: Cell culture medium (vehicle control)
- Prepare cells for injection by trypsinization, washing, and resuspension in sterile PBS at 1×10⁶ cells/10 μL.
- Anesthetize mice and inject 10 μL of cell suspension or vehicle into the joint space of the operated knee using a 30G needle.
- Repeat injection at 4 weeks post-surgery for sustained therapeutic effect.
- At 2 weeks post-surgery, randomize OA-induced mice into treatment groups:
Post-Treatment Assessment:
- Pain Monitoring: Assess mechanical allodynia using von Frey filaments weekly for 6 weeks following the first injection. Calculate 50% paw withdrawal threshold using the up-down method.
- Cartilage Integrity: At endpoint (8 weeks post-surgery), evaluate cartilage degradation using T2-weighted MRI. Score cartilage damage using the modified Kornaat grading system.
- Histological Analysis: Harvest knee joints, fix in 4% PFA, decalcify in EDTA, and embed in paraffin. Section at 5 μm thickness and stain with Safranin O/Fast Green and Hematoxylin & Eosin. Score histological changes using the OARSI grading system.
- Immunohistochemistry: Perform immunohistochemistry for collagen type II, aggrecan, and MMP-13 to evaluate anabolic and catabolic activity.
Expected Results
- CRISPR-engineered MSCs should demonstrate:
- Significant reduction in pain sensitivity compared to control groups (>50% improvement in mechanical allodynia thresholds)
- Improved cartilage integrity on MRI with lower degradation scores
- Enhanced proteoglycan retention on Safranin O staining
- Increased collagen type II and reduced MMP-13 expression on immunohistochemistry
- Better cell survival and integration into cartilaginous tissues
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for SOX9 and CRISPR-Cas9 Studies
| Reagent Category | Specific Examples | Application/Function | Source/Reference |
|---|---|---|---|
| CRISPR Plasmids | Lenti-dSpCas9-VP64, Lenti-dSaCas9-KRAB | Transcriptional activation/repression | [6] |
| Guide RNAs | Sox9-2: CGGGTTGGGTGACGAGACAGG, RelA-1: CCGAAATCCCCTAAAAACAGA | Target specific genomic loci | [6] |
| Cell Lines | Bone marrow MSCs, Tonsil-derived MSCs, Human OA chondrocytes | Model systems for chondrogenesis and inflammation | [6] [17] |
| Vector Systems | rAAV-SOX9, AAVS1-targeting plasmids | Gene delivery and safe harbor integration | [15] [17] |
| Cytokines & Inhibitors | IL-1β, TNF-α, IL-1Ra, doxycycline | Modeling inflammation and regulating transgene expression | [15] [16] |
| Analysis Tools | SOX9 antibodies (AF3045), COL2A1 antibodies, aggrecan antibodies | Protein detection and localization | [14] [17] |
Troubleshooting and Technical Considerations
Common Challenges in SOX9 Research
Variable Chondrogenic Differentiation Efficiency:
- Problem: Inconsistent results in chondrogenesis assays between MSC batches.
- Solution: Standardize MSC sources and passage numbers (use early passages P3-P6). Pre-screen MSC donors for chondrogenic capacity. Include positive controls in each experiment.
Inflammatory Cytokine Interference:
- Problem: Pro-inflammatory cytokines (IL-1β, TNF-α) inhibit SOX9 expression and activity.
- Solution: Include cytokine receptor antagonists (e.g., IL-1Ra) in culture media. Use lower cytokine concentrations that better mimic physiological levels in early OA.
CRISPR Off-Target Effects:
- Problem: Unintended genomic modifications with CRISPR-Cas9 systems.
- Solution: Use computational tools to design highly specific gRNAs. Employ high-fidelity Cas9 variants. Include multiple gRNA controls and validate findings with independent approaches.
Optimization Guidelines
- Cell Density: For chondrogenic differentiation, optimal cell density in pellet cultures is 2.5×10⁵ cells per pellet. Lower densities reduce ECM deposition, while higher densities limit nutrient diffusion.
- Viral Titration: For lentiviral transduction, perform preliminary titration experiments to determine the multiplicity of infection (MOI) that achieves >80% transduction efficiency without cytotoxicity.
- Timing Considerations: The therapeutic window for intervention in OA models is critical. Early intervention (2-4 weeks post-OA induction) typically yields better outcomes than late-stage treatment.
SOX9 represents a master regulatory transcription factor with profound importance in cartilage homeostasis, inflammatory joint diseases, and potential therapeutic applications. The integration of CRISPR-Cas9 technology has dramatically enhanced our ability to dissect SOX9 functions and develop novel gene- and cell-based therapies for conditions like osteoarthritis. The protocols detailed in this Application Note provide standardized methodologies for engineering SOX9-modified cells, assessing their therapeutic potential, and evaluating outcomes in relevant disease models.
Future directions in SOX9 research should focus on refining delivery systems for clinical translation, enhancing the specificity of CRISPR-based approaches, and developing more sophisticated disease models that better recapitulate the complex pathophysiology of human inflammatory joint diseases. As our understanding of SOX9 biology continues to evolve, so too will our ability to harness its therapeutic potential for the benefit of patients suffering from cartilage degradation and inflammatory joint conditions.
Rationale for SOX9 Knockout in Immune Cell Models for Basic and Translational Research
The transcription factor SOX9 is a pivotal regulator of development and tissue homeostasis, but its dysregulation is increasingly implicated in cancer progression and immune evasion. Utilizing CRISPR-Cas9 for SOX9 knockout (KO) in immune cell models provides a powerful approach to dissect its complex role at the nexus of tumor biology and immunology. SOX9 functions as a context-dependent "janus-faced" regulator in immunity, acting as a double-edged sword [1]. It is frequently overexpressed in solid malignancies, where its expression correlates with poor prognosis, while in certain contexts, it contributes to tissue repair and regeneration [19] [1]. A key rationale for targeting SOX9 is its established role in suppressing anti-tumor immunity. In KrasG12D-driven lung adenocarcinoma (LUAD) models, SOX9 expression functionally suppresses tumor-infiltrating CD8+ T cells, natural killer (NK) cells, and dendritic cells, thereby creating an immunosuppressive tumor microenvironment (TME) [19]. Furthermore, SOX9 drives tumor progression and immune escape by modulating the extracellular matrix, increasing collagen-related gene expression and tumor stiffness, which constitutes a physical barrier to immune cell infiltration [19]. In breast cancer, a SOX9-B7x axis has been identified that safeguards dedifferentiated tumor cells from immune surveillance [5]. Given its role as a pioneer factor that can bind closed chromatin and compete for epigenetic co-factors to switch cell fates, SOX9 is a master regulator of tumor cell identity and a compelling target for functional genomic interrogation [20]. Knocking out SOX9 in relevant immune and tumor models allows researchers to deconvolute these mechanisms and identify novel therapeutic vulnerabilities.
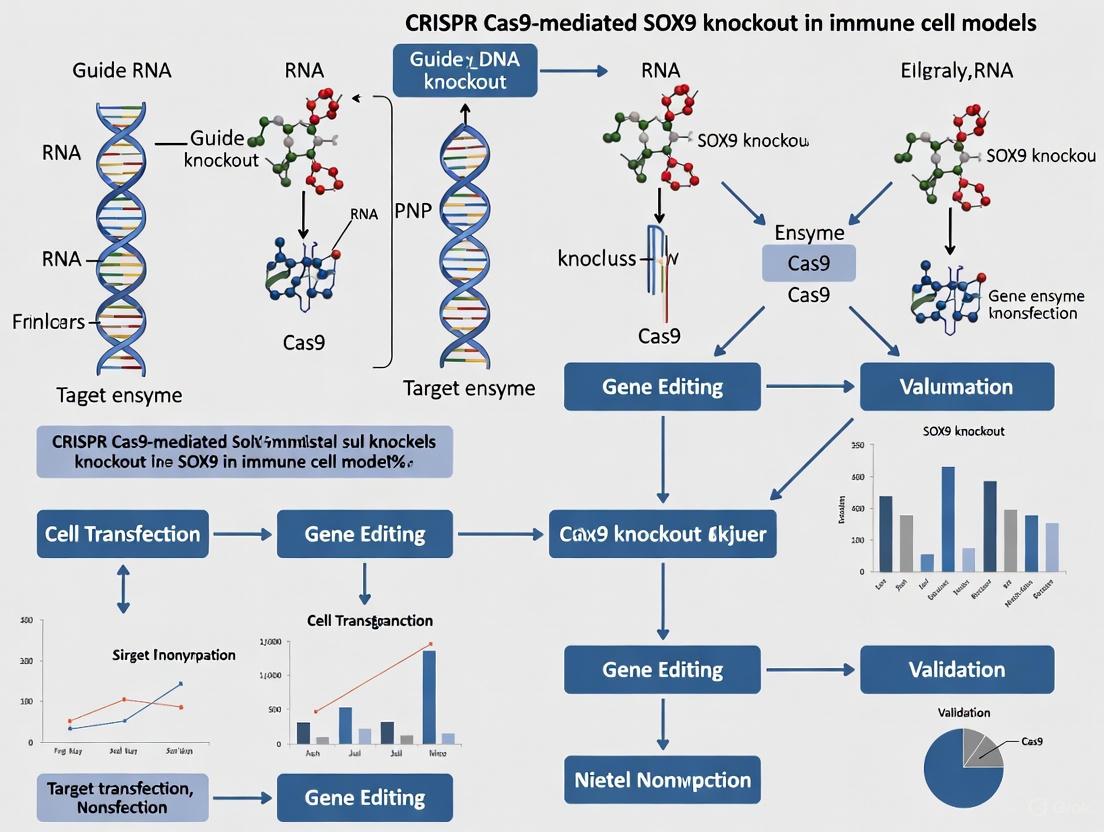
Experimental Design and Workflow
A typical workflow for investigating SOX9 through CRISPR-Cas9 knockout involves sequential stages from target design to functional validation, as outlined below.
Figure 1: Experimental workflow for SOX9 knockout studies, spanning from genetic targeting to functional analysis.
Detailed Protocol for CRISPR-Cas9-Mediated SOX9 Knockout
3.1 sgRNA Design and Vector Construction The initial step involves the design and cloning of single-guide RNAs (sgRNAs) against the SOX9 gene.
- sgRNA Design: Design 3-5 sgRNAs targeting early exons of the human or mouse SOX9 gene (Ensembl: ENSG00000125398 (human); ENSMUSG00000000567 (mouse)) to maximize frameshift probability. An example of a validated mouse sgRNA sequence is sgSox9.2: 5'-GACCGAGCTCAGCAAGATCG-3' [19].
- Controls: Include a non-targeting control sgRNA (e.g., targeting tdTomato).
- Cloning: Clone sgRNA sequences into an appropriate CRISPR plasmid, such as the lentiCRISPR v2 or a Cre-inducible pSECC system for in vivo models [19].
3.2 Delivery of CRISPR-Cas9 Components The choice of delivery system is critical for efficient gene editing.
- For Immune Cells or Cell Lines (In Vitro):
- Ribonucleoprotein (RNP) Transfection: Complex chemically modified sgRNA with recombinant Cas9 protein to form RNPs. Deliver using lipid-based transfection reagents or electroporation (e.g., Neon System). RNP delivery offers high efficiency with reduced off-target effects and rapid turnover [21].
- Lentiviral Transduction: For stable expression, package sgRNA and Cas9 into lentiviral particles. Transduce target cells and select with antibiotics (e.g., Puromycin) for 3-5 days.
- For In Vivo Models:
- Use recombinant Adeno-Associated Viruses (AAVs) or Lentiviruses for high transduction efficiency. For example, intratracheal delivery of lenti-Cre and lenti-sgRNA/SOX9 to induce lung-specific tumor models and SOX9 knockout simultaneously [19].
3.3 Generating and Validating KO Models
- Single-Cell Cloning: After delivery and selection, dilute cells to ~0.5 cells/well in a 96-well plate to isolate single-cell-derived clones.
- Genotypic Validation:
- PCR and Sequencing: Genomic DNA is extracted from clones. The targeted SOX9 locus is amplified by PCR and Sanger sequenced to confirm insertion/deletion (indel) mutations.
- Next-Generation Sequencing (NGS): For comprehensive off-target assessment, perform NGS on potential off-target sites predicted by in silico tools (e.g., Cas-OFFinder).
- Phenotypic Validation:
- Western Blotting: Confirm the absence of SOX9 protein. Use antibodies against SOX9 (e.g., AB5535, Millipore) and loading controls (e.g., β-Actin). A complete KO should show no band at ~61-64 kDa [22].
- Functional Assay: Validate loss of function via downstream targets. For instance, SOX9 KO in chondrosarcoma cells leads to an inability to activate MMP13 expression [22].
3.4 Key Phenotypic Assays for SOX9 KO Immune Models Post-validation, cells are subjected to functional assays.
- Proliferation and Clonogenicity:
- Immune Profiling via Co-culture and In Vivo Models:
- Co-culture SOX9 WT and KO tumor organoids with primed CD8+ T cells or NK cells. Measure immune-mediated killing by LDH release assay or flow cytometry for apoptosis (Annexin V/PI).
- Adoptive transfer of SOX9 KO cells into syngeneic immunocompetent mice. After 3-4 weeks, analyze tumors by flow cytometry for immune cell infiltration (CD45+, CD3+, CD8+, CD4+, NK1.1+, CD11c+ cells) [19].
- Therapeutic Sensitivity Screening:
- Treat SOX9 KO and control cells with a panel of therapeutics (e.g., chemotherapeutics, targeted therapies, oncolytic viruses). SOX9 KO in chondrosarcoma increased sensitivity to doxorubicin but reduced sensitivity to an oncolytic virus [22]. Assess viability after 72 hours.
Key Research Reagent Solutions
Table 1: Essential reagents and tools for SOX9 knockout studies.
| Reagent/Tool | Function/Application | Examples & Specifications |
|---|---|---|
| CRISPR Plasmids | Delivery of sgRNA and Cas9 nuclease. | lentiCRISPR v2, pSECC (combined Cre + CRISPR), pSpCas9(BB)-2A-Puro [19]. |
| Validated sgRNAs | Target-specific genomic cleavage. | Mouse: sgSox9.2 (5'-GACCGAGCTCAGCAAGATCG-3') [19]. Human: Design via online tools (e.g., Benchling). |
| Cas9 Protein | Formulation of RNP complexes for highly efficient editing. | Recombinant S. pyogenes Cas9 Nuclease, HPLC-purified. |
| Delivery Reagents | Introduction of CRISPR components into cells. | Lipofectamine CRISPRMAX, Neon Transfection System for electroporation [21]. |
| SOX9 Antibodies | Validation of knockout efficiency via Western Blot, IHC, and IF. | Rabbit anti-SOX9 (Millipore, AB5535); IHC/IF validated antibodies [19] [22]. |
| Cell Culture Models | In vitro platforms for functional studies. | HTB94 (human chondrosarcoma), mTC11/mTC14 (mouse KrasG12D lung tumor), primary immune cells [19] [22]. |
| In Vivo Models | Study SOX9 in tumor progression and immune evasion in a physiological context. | KrasLSL-G12D; Sox9flox/flox (KSf/f) mice; immunocompromised vs. syngeneic hosts [19]. |
Applications in Cancer Immunology and Data Interpretation
The application of SOX9 KO models has yielded critical insights into its role in cancer immunology, with quantitative findings summarized below.
Table 2: Key phenotypic outcomes of SOX9 knockout in cancer models.
| Model System | Phenotype of SOX9 Knockout | Quantitative & Functional Data | Source |
|---|---|---|---|
| KrasG12D LUAD (Mouse) | Reduced tumor development, burden, and progression; Enhanced survival. | - Tumor Burden: Significantly reduced.- Survival: KSf/f mice had significantly longer survival (p=0.0012).- Tumor Grade: Fewer high-grade (Grade 3) tumors.- Immunophenotype: Increased infiltration of CD8+ T, NK, and Dendritic cells. | [19] |
| Chondrosarcoma (HTB94 Cells) | Impaired proliferation, clonogenicity, and migration; Increased apoptosis and polyploidy. | - Doubling Time: Extended from 30h (control) to 42-49h (KO).- Clonogenicity: 50-75% reduction in soft agar colonies.- Therapeutic Response: Increased sensitivity to doxorubicin. | [22] |
| Breast Cancer Model | Immune evasion via the B7x immune checkpoint pathway. | - Mechanism: SOX9 transcriptionally activates B7x (B7-H4/VTCN1), an immune checkpoint molecule that inhibits T cell function. | [5] |
| Epidermal Stem Cells | Fate switching and tumorigenesis via pioneer factor activity. | - Mechanism: SOX9 binds closed chromatin, recruits co-factors to open new enhancers, and competitively depletes them from original fate enhancers, leading to silencing. | [20] |
The data generated from these protocols require careful interpretation. A successful SOX9 KO should be correlated with expected phenotypic changes, such as reduced proliferation and altered immune cell recruitment. It is crucial to confirm that observed effects are due to the loss of SOX9 and not off-target editing. This is achieved by using multiple sgRNAs and performing rescue experiments where SOX9 is re-expressed in the KO background. Furthermore, the cell-type and context-dependent nature of SOX9's function means that findings in one model system may not be universally applicable. For instance, while SOX9 is oncogenic in LUAD and chondrosarcoma, it can act as a tumor suppressor in other contexts like melanoma [19] [22] [1]. Therefore, conclusions should be drawn within the specific experimental framework of the immune cell model being studied.
A Practical Framework for CRISPR-Cas9-Mediated SOX9 Editing in Immune Cells
The selection of an appropriate CRISPR-based tool is a critical first step in designing functional genetic studies, particularly in complex systems like immune cells. For research focused on transcription factors such as SOX9 in immune cell models, the choice between traditional knockout (KO), CRISPR interference (CRISPRi), and CRISPR activation (CRISPRa) determines not only the experimental outcome but also the biological relevance of the findings. CRISPR-KO completely and permanently disrupts gene function, while CRISPRi and CRISPRa offer reversible, tunable control over gene expression without altering the underlying DNA sequence. This application note provides a structured framework for selecting and implementing these technologies, with specific consideration for manipulating SOX9—a transcription factor with complex, dual roles in immunobiology—in immune cell models.
Comparative Analysis of CRISPR Technologies
The table below summarizes the key operational and application characteristics of the three primary CRISPR tool types to guide your selection process.
Table 1: Comparison of Key CRISPR Tool Types
| Feature | CRISPR-Knockout (KO) | CRISPR Interference (CRISPRi) | CRISPR Activation (CRISPRa) |
|---|---|---|---|
| Molecular Mechanism | Nuclease-active Cas9 creates double-strand breaks, repaired by error-prone NHEJ. [23] | dCas9 fused to repressive domains (e.g., KRAB) blocks transcription or recruits chromatin condensers. [24] [25] | dCas9 fused to activator domains (e.g., VP64, p65, HSF1) recruits transcriptional machinery. [6] [26] |
| Effect on Gene | Permanent gene disruption via indels; complete loss of function. [23] | Reversible, tunable transcriptional repression; partial to strong knockdown. [24] [25] | Reversible, tunable transcriptional overexpression; can achieve supra-physiological levels. [6] |
| Best For | Studying essential gene functions, generating loss-of-function models, validating drug targets. | Studying essential genes, analyzing dose-dependent effects, functional screening. [24] | Studying gene overexpression, functional compensation, modeling gain-of-function diseases. [6] |
| Key Considerations | Potential for off-target mutations; not suitable for essential genes. | Repression can be incomplete (~70-95%); requires careful gRNA design to target promoter. [24] | Can exhibit cytotoxicity due to strong activator domains; activation levels can be highly variable. [26] |
Application Notes for SOX9 Research in Immune Cell Models
The SOX9 transcription factor exhibits a "double-edged sword" role in immunobiology, making the choice of CRISPR tool particularly consequential. [1]
- CRISPR-KO for SOX9: Ideal for investigating its fundamental, non-redundant functions in immune cell differentiation and function. Complete knockout can help map SOX9's role in transcriptional networks controlling processes like Tγδ17 cell commitment. [1]
- CRISPRi for SOX9: Recommended for modeling the partial or temporal downregulation of SOX9, which may occur in disease states or during fine-tuned immune responses. This approach is valuable for studying dose-dependent effects without the complete lethality that a full knockout might cause. [24]
- CRISPRa for SOX9: Highly suitable for modeling the pathologically elevated SOX9 levels observed in certain autoimmune contexts or solid tumors. [1] A 2024 study demonstrated that CRISPRa-mediated Sox9 activation in mesenchymal stromal cells enhanced their chondrogenic potential, showcasing its therapeutic potential. [6]
Detailed Experimental Protocols
Protocol 1: CRISPRi-Mediated Gene Silencing in Primary Human Immune Cells
This protocol is adapted from a 2025 study that successfully silenced pro-inflammatory genes (IL-6, CD40, IFN-γ) in primary human PBMCs and immune cell lines. [24] [25]
Workflow Overview:
Step-by-Step Procedure:
gRNA Design and Vector Construction:
- gRNA Design: Design 3-5 gRNAs targeting the promoter region of your target gene (e.g., SOX9), approximately -50 to -300 bp upstream of the transcription start site (TSS). [6]
- Vector Assembly: Clone the selected gRNA sequences into a lentiviral vector expressing a dCas9-KRAB fusion protein. A common system uses Staphylococcus aureus dCas9 (dSaCas9) for repression. [6]
Lentiviral Production:
- Co-transfect HEK-293T cells with the transfer plasmid (dCas9-KRAB + gRNA) and packaging plasmids (psPAX2, pMD2.G) using a standard transfection reagent.
- Collect the viral supernatant at 48 and 72 hours post-transfection. Concentrate the virus if necessary and titrate using a qRT-PCR-based method. [26]
Cell Transduction:
- For primary human CD4+ T cells or PBMCs: Activate cells with anti-CD3/CD28 beads for 48 hours. [27]
- Transduce activated cells with lentivirus at an MOI of 5-20 in the presence of polybrene (8 µg/mL). Centrifuge the culture plates at 800 × g for 30-60 minutes to enhance infection efficiency (spinoculation).
- Culture cells in RPMI-1640 medium supplemented with 10% FBS and 1% Penicillin-Streptomycin. [24]
Selection and Validation of Silencing:
Functional Validation:
- Perform downstream functional assays relevant to your research question. For immune cells, this may include:
- Flow Cytometry: Analyze surface activation markers (e.g., CD69, CD25) or intracellular cytokines. [24] [25]
- Cytokine Measurement: Use ELISA to quantify cytokine secretion in cell culture supernatants. [24]
- Proliferation Assays: Use dye dilution (e.g., CFSE) or metabolic activity assays to assess cell growth. [27]
- Perform downstream functional assays relevant to your research question. For immune cells, this may include:
Protocol 2: CRISPRa-Mediated SOX9 Activation
This protocol outlines the key steps for overexpressing SOX9, based on a system used to enhance the chondrogenic potential of mesenchymal stromal cells. [6]
Key Considerations:
- Cytotoxicity Warning: Vectors expressing strong transcriptional activators (e.g., p65-HSF1) can be cytotoxic. [26] Use inducible systems or closely monitor cell health and transgene expression levels.
- gRNA Design: For activation, gRNAs are typically designed to target regions slightly upstream of the TSS. [6]
Abbreviated Workflow:
- System Selection: Utilize a dual-vector system: one expressing dCas9-VP64 and a second expressing the gRNA along with helper activators (e.g., MS2-p65-HSF1). [6] [26]
- gRNA Design for SOX9: Design gRNAs targeting the Sox9 promoter. One study used guides at positions -74, -167, -276, and -198 bp relative to the TSS. [6]
- Delivery and Analysis: Follow steps 2-5 from the CRISPRi protocol above, transducing your target immune cells and validating activation via RT-qPCR and Western blot.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for CRISPR-Based Gene Regulation
| Reagent / Material | Function / Description | Example Use Case |
|---|---|---|
| dCas9-KRAB Fusion | The core effector for CRISPRi; KRAB domain recruits repressive complexes to silence gene expression. [24] | Constitutive or inducible repression of SOX9 in T cell lines. |
| dCas9-VP64 Fusion | A common base activator for CRISPRa; VP64 is a synthetic tetramer of the VP16 activation domain. [6] [26] | Foundational component for transcriptional activation of SOX9. |
| MS2-p65-HSF1 (MPH) | A recruited secondary activator that significantly enhances CRISPRa potency as part of the SAM system. [26] | Achieving strong, supra-physiological activation of SOX9 for functional studies. |
| Lentiviral Vectors | Efficient delivery system for stable integration of CRISPR components into hard-to-transfect cells like primary immune cells. [24] [27] | Transduction of primary human T cells or PBMCs. |
| Activation Beads | Anti-CD3/CD28 magnetic beads used to stimulate T cell proliferation and activation, which is required for lentiviral transduction. [27] | Preparing primary human T cells for transduction. |
Visualization of CRISPRi/a Mechanisms
The following diagram illustrates the core mechanisms of CRISPR interference and activation, showing how different dCas9 effector proteins regulate transcription at the target gene promoter.
The strategic selection of CRISPR tools—KO, i, or a—enables precise dissection of SOX9's Janus-faced roles in immunity. As the field advances, key developments are poised to enhance these applications. Artificial intelligence is now being used to design highly functional, novel CRISPR-Cas proteins with optimal properties, which could improve efficacy and specificity in immune cells. [28] Furthermore, the combination of CRISPR screening in primary human T cells with single-cell readouts is powerfully linking genetic variants to immune cell function and disease risk, opening new avenues for therapeutic discovery. [27] By carefully matching the scientific question to the appropriate CRISPR technology, researchers can continue to unravel the complex functions of SOX9 and other critical immune regulators, accelerating the path from basic science to clinical application.
Guide RNA (gRNA) Design and Delivery Strategies for Immune Cell Transfection
The application of CRISPR-Cas9 technology for genetic manipulation in immune cells represents a transformative approach in immunology research and therapeutic development. Efficient genome editing in these cells hinges on two critical components: the design of highly specific guide RNAs (gRNAs) and the selection of optimized delivery strategies that account for the unique challenges posed by immune cell biology. This application note provides detailed protocols and design considerations for CRISPR-Cas9-mediated gene knockout, with specific focus on SOX9 knockout in immune cell models. SOX9, a transcription factor with complex, dual roles in immune regulation, serves as an exemplary target due to its involvement in immune cell differentiation, function, and tumor immune evasion [1]. The guidance herein is structured to assist researchers in achieving efficient editing while maintaining high cell viability and function, which are paramount for successful experimental outcomes in immune cell research.
gRNA Design Principles for CRISPR-Cas9 Experiments
Fundamental Components of CRISPR gRNAs
The CRISPR guide RNA directs the Cas9 nuclease to a specific genomic locus. In its simplest form for experimental use, it exists as a single guide RNA (sgRNA), a single RNA molecule that incorporates two essential elements: the crRNA component, which contains a 17-20 nucleotide sequence complementary to the target DNA, and the tracrRNA scaffold, which facilitates binding to the Cas9 nuclease [29]. The target specificity of the entire complex is determined by the design of the crRNA spacer sequence.
Strategic Design for Gene Knockout
For a successful knockout strategy, aiming to disrupt the SOX9 gene function, gRNA design must prioritize locations that maximize the probability of a disruptive frameshift mutation following non-homologous end joining (NHEJ) repair.
- Target Site Selection: Target early exons encoding critical protein domains, such as the High Mobility Group (HMG) box DNA-binding domain of SOX9 [1]. Avoid regions too close to the N- or C-terminus to reduce the chance of truncated but partially functional proteins being expressed [30].
- PAM Sequence Requirement: The canonical SpCas9 nuclease requires a 5'-NGG-3' Protospacer Adjacent Motif (PAM) sequence immediately downstream of the target site on the non-target DNA strand. The target-specific 20-nucleotide gRNA sequence is selected directly 5' to this PAM [31] [32].
- Multi-gRNA Strategy: Using multiple gRNAs (e.g., 2-3) targeting the same gene can significantly increase editing efficiency and knockout confidence by generating multiple double-strand breaks [30].
Table 1: Key Considerations for gRNA Design for Gene Knockout
| Design Parameter | Recommendation | Rationale |
|---|---|---|
| Target Location | Early, functional exons | Maximizes likelihood of complete gene disruption |
| GC Content | 40-80% | Optimizes gRNA stability and binding efficiency [29] |
| Seed Sequence | No mismatches in 8-10 bases at 3' end | Critical for Cas9 cleavage activity [32] |
| Specificity | Unique in genome; minimal off-targets | Prevents unintended editing at homologous sites |
| PAM Site | NGG for SpCas9 | Essential for Cas9 recognition and cleavage |
In Silico Design and Validation
Computational tools are indispensable for designing high-quality gRNAs. These tools assess on-target efficiency and predict potential off-target sites across the genome.
- Synthego CRISPR Design Tool: Enables rapid design and validation of gRNAs with optimized on-target and reduced off-target activity scores for over 120,000 genomes [30].
- Benchling CRISPR Tool: Useful for integrated design of gRNAs and repair templates, leveraging up-to-date algorithms [30].
- CHOPCHOP & Cas-OFFinder: Popular tools for general gRNA design and specific off-target detection, respectively [29].
The workflow for designing a gRNA for SOX9 knockout can be summarized as follows:
Delivery Strategies for Immune Cells
The delivery of CRISPR components (Cas9 nuclease and gRNA) into immune cells is a major technical challenge due to their inherent resistance to foreign nucleic acid uptake. The choice of delivery method is critical for balancing high efficiency with maintained cell health and function.
Non-Viral Delivery: Electroporation
Electroporation uses electrical pulses to create transient pores in the cell membrane, allowing nucleic acids or ribonucleoproteins (RNPs) to enter the cell. It is highly effective for many immune cell types, especially T cells.
- RNP Complex Delivery: The gold standard for CRISPR in immune cells involves pre-complexing purified Cas9 protein with synthetic sgRNA to form an RNP complex, which is then delivered via electroporation. This method offers rapid activity, reduced off-target effects, and minimal cytotoxicity compared to plasmid DNA delivery [33].
- Optimized Parameters for Immune Cells: Different immune cell types require specific electroporation conditions. The Neon Transfection System, for example, provides pre-optimized protocols for high efficiency in primary T cells and various immune cell lines [33].
Table 2: Electroporation Parameters and Efficiency for Immune Cells (Adapted from Neon Transfection System Data) [33]
| Cell Type | Electroporation Parameters (10µL tips) | Transfection Efficiency (with DNA) | Transfection Efficiency (with mRNA) |
|---|---|---|---|
| Primary T Cells | 1600 V, 10 ms, 3 pulses | 84% | 96% |
| Jurkat (T-cell line) | 1700 V, 20 ms, 1 pulse | 86% | 95% |
| NK-92 (NK-cell line) | 1300 V, 10 ms, 3 pulses | 52% | 98% |
| THP-1 (Monocyte line) | 1600 V, 10 ms, 3 pulses | 42% | 88% |
Viral Vector Delivery
Viral transduction, particularly using lentiviral (LV) and gamma-retroviral (γRV) vectors, is a common method for stable gene expression in immune cells, including for delivering CRISPR components.
- Lentiviral Vectors: Capable of transducing both dividing and non-dividing cells. Modern self-inactivating (SIN) designs improve safety by reducing the risk of insertional mutagenesis [34]. VSV-G pseudotyping allows broad tropism across immune cell types.
- Gamma-Retroviral Vectors: Require target cell proliferation for integration, making them suitable for activated T cells. They generally show poor tropism for NK cells [34].
- Critical Quality Attributes (CQAs): Post-transduction, key metrics must be monitored: Transduction Efficiency (aim for 30-70% in clinical manufacturing), Cell Viability & Function (e.g., cytokine secretion, cytotoxicity), and Vector Copy Number (VCN) (typically kept below 5 copies/cell for safety) [34].
Application Note: SOX9 Knockout in Immune Cell Models
Background and Rationale
SOX9 is a transcription factor with a "double-edged sword" role in immunology. It can promote tumor immune escape by impairing immune cell function, making it a potential therapeutic target in cancer. Conversely, it helps maintain macrophage function and contributes to tissue repair [1]. Knocking out SOX9 in immune cell models (e.g., T cells, macrophages) is therefore a valuable strategy for investigating its specific immunomodulatory functions. Evidence shows that SOX9 ablation can increase sensitivity to chemotherapeutic agents like carboplatin in cancer models, highlighting its functional significance [8].
Detailed Protocol: RNP Electroporation of Primary Human T Cells
This protocol outlines a standardized method for knocking out SOX9 in primary human T cells using Cas9 RNP electroporation.
Workflow Overview:
Materials:
- Primary Human T Cells: Isolated from leukopak or PBMCs using Ficoll-Paque density gradient and negative selection kits [33].
- Culture Medium: Gibco OpTmizer CTS T-Cell Expansion SFM, supplemented with 2% human serum and a cytokine cocktail (e.g., IL-2) [33].
- Activation Reagents: Gibco Dynabeads Human T-Expander CD3/CD28.
- CRISPR Components: Recombinant SpCas9 protein and synthetic sgRNA targeting human SOX9.
- Electroporation System: Neon Transfection System with 10µL tips and Buffer R [33].
Step-by-Step Procedure:
T Cell Isolation and Activation:
- Isolate T cells from donor blood using a standardized Ficoll-Paque PLUS medium and an untouched human T cell isolation kit.
- Culture cells in pre-warmed OpTmizer medium with 2% human serum.
- Activate cells using CD3/CD28 Dynabeads at a bead-to-cell ratio of 1:1. Incubate for 3 days at 37°C, 5% CO2.
RNP Complex Assembly:
- Resuspend synthetic sgRNA (e.g., 10 µg) and Cas9 protein (e.g., 20 µg) in nuclease-free duplex buffer to a final volume of 10 µL. The molar ratio of Cas9:sgRNA is typically 1:2.
- Incubate the mixture at room temperature for 15-30 minutes to form the RNP complex.
Electroporation:
- Harvest 2 x 10^5 activated T cells per reaction. Centrifuge and resuspend the cell pellet in 10 µL of Buffer R.
- Mix the cell suspension with the pre-assembled RNP complex.
- Aspirate the cell-RNP mixture into a 10µL Neon Tip.
- Electroporate using the Neon Transfector with parameters optimized for primary T cells: 1600 V, 10 ms pulse width, 3 pulses [33].
- Immediately transfer the electroporated cells into pre-warmed 0.5 mL of complete medium in a 24-well plate.
Post-Transfection Culture:
- Culture the cells in complete medium supplemented with IL-2 (e.g., 100 U/mL) to support survival and expansion.
- Remove activation beads 3-5 days post-electroporation.
- Expand cells for 7-10 days, monitoring viability and density.
Validation and Functional Assessment
- Knockout Efficiency Validation: Assess editing efficiency 3-5 days post-electroporation.
- Tracking of Indels by Decomposition (TIDE): PCR-amplify the target region and sequence it to quantify the spectrum of indel mutations.
- Flow Cytometry: If available, use a SOX9-specific antibody to detect protein-level knockdown.
- Western Blot: Confirm the loss of SOX9 protein expression.
- Functional Assays:
- Proliferation Assay: Use live-cell imaging (e.g., Incucyte) to monitor potential growth changes in SOX9-knockout cells versus controls [8].
- Cytokine Secretion: Stimulate edited T cells and measure effector cytokines (e.g., IFN-γ) using ELISA or ELISpot.
- In Vitro Cytotoxicity: Co-culture edited T cells with target cells to assess any functional impact of SOX9 knockout on killing capacity.
Table 3: Key Research Reagent Solutions for Immune Cell CRISPR
| Reagent / Tool | Function / Application | Example Products / Providers |
|---|---|---|
| Synthetic sgRNA | High-purity, chemically modified gRNAs for improved stability and reduced immunogenicity in RNP delivery. | Synthego, Thermo Fisher Scientific [29] |
| Cas9 Nuclease | Wild-type and high-fidelity (HF) recombinant Cas9 protein for RNP formation. | IDT, Thermo Fisher Scientific, Sigma-Aldrich |
| Electroporation Systems | Instrumentation for high-efficiency nucleic acid and RNP delivery into hard-to-transfect immune cells. | Neon Transfection System (Thermo Fisher) [33] |
| T Cell Media & Supplements | Serum-free, optimized media and cytokine cocktails for the activation and expansion of primary T cells. | Gibco OpTmizer, IL-2, IL-7, IL-15 [33] [34] |
| gRNA Design Software | In silico tools for designing and scoring gRNAs for on-target efficiency and off-target effects. | Synthego Design Tool, Benchling, CHOPCHOP [29] [30] |
| Validation Assays | Kits and reagents for quantifying editing efficiency and functional outcomes. | TIDE/E, Flow Antibodies (SOX9), IFN-γ ELISpot kits |
Lung adenocarcinoma (LUAD) is the most common histological subtype of non-small cell lung cancer (NSCLC), with KRAS mutations occurring in approximately 30% of cases [35]. Among these, the KRASG12D mutation is particularly prevalent in never-smokers and presents significant therapeutic challenges [35] [36]. The SOX9 transcription factor has been identified as a key downstream effector of oncogenic KRAS signaling, contributing to tumor progression through mechanisms that remain incompletely understood [37] [19]. Recent evidence suggests that SOX9 plays a critical role in modulating the tumor immune microenvironment, making it an attractive target for immunotherapy combination strategies [37] [1]. This case study employs CRISPR/Cas9-mediated Sox9 knockout in a KrasG12D-driven murine LUAD model to investigate SOX9's specific contributions to tumor progression and anti-tumor immunity, providing a experimental framework for researchers exploring transcription factor targeting in immuno-oncology.
Background and Significance
The KRASG12D Mutation in Lung Adenocarcinoma
KRAS mutations are among the most common oncogenic drivers in LUAD, with the KRASG12D subtype representing 14-18% of all KRAS mutations [35]. Unlike the KRASG12C mutation which is more common in smokers, KRASG12D occurs most frequently in never-smokers (56%) and is associated with distinct clinical characteristics [36] [35]. From a therapeutic perspective, KRASG12D has proven more challenging to target directly than KRASG12C, though inhibitors such as MRTX1133 have entered clinical trials [36] [35]. KRASG12D mutations frequently co-occur with alterations in other genes including TP53 (33.6%), STK11 (15.9%), and KEAP1 (9.4%), which collectively shape tumor biology and therapeutic responses [35].
SOX9 as an Oncogenic Transcription Factor
SOX9 is a developmentally regulated transcription factor belonging to the SRY-related HMG-box family, crucial for proper tissue development and homeostasis [37] [1]. In cancer, SOX9 is frequently overexpressed across various solid malignancies and is associated with poor prognosis [37] [19]. In LUAD, SOX9 expression is significantly upregulated in KRAS-mutant tumors and drives multiple pro-tumorigenic processes including cell proliferation, inhibition of apoptosis, and promotion of stem cell features [19]. Structurally, SOX9 contains several functional domains: a dimerization domain (DIM), the HMG box DNA-binding domain, two transcriptional activation domains (TAM and TAC), and a proline/glutamine/alanine-rich domain [1]. The HMG domain facilitates nuclear localization and DNA binding, while the C-terminal TAC domain interacts with cofactors like Tip60 to enhance transcriptional activity [1].
SOX9 as a Regulator of Anti-Tumor Immunity
Emerging research has revealed that SOX9 plays a complex, "Janus-faced" role in immunoregulation [1]. In the tumor context, SOX9 functions predominantly as an immunosuppressive factor by remodeling the tumor microenvironment. Studies demonstrate that SOX9 expression negatively correlates with infiltration levels of cytotoxic CD8+ T cells, natural killer (NK) cells, and dendritic cells while promoting an immunosuppressive niche [37] [1]. Mechanistically, SOX9 significantly elevates collagen-related gene expression and increases collagen deposition, resulting in increased tumor stiffness that physically impedes immune cell infiltration [37] [19]. This multifaceted role in immune evasion positions SOX9 as a promising target for combination immunotherapy strategies.
Experimental Design and Model System
KrasG12D-Driven Murine Lung Adenocarcinoma Model
This study utilizes the KrasLSL-G12D genetically engineered mouse model (GEMM) which allows controlled expression of the KRASG12D oncogene specifically in lung epithelial cells upon Cre-mediated recombination [37] [19]. For more sophisticated temporal control, some experiments employed the Lung-iKRAS (L-iKRAS) model featuring doxycycline-inducible and reversible KRASG12D expression [36]. This inducible system enables researchers to activate KRASG12D expression during tumor initiation, then subsequently inactivate it to study effects on established tumors and the tumor microenvironment [36]. The experimental cohorts typically include:
- Control mice: KRAS wild-type or empty vector controls
- KrasG12D mice: Expressing oncogenic KRAS only
- KrasG12D;Sox9w/w (KSw/w): KRAS-driven tumors with wild-type SOX9
- KrasG12D;Sox9flox/flox (KSf/f): KRAS-driven tumors with conditional Sox9 knockout
Table 1: Key Genetically Engineered Mouse Models for SOX9 Studies in LUAD
| Model Name | Genetic Features | Induction Method | Key Applications |
|---|---|---|---|
| KrasLSL-G12D | Lox-Stop-Lox KRASG12D allele | Intratracheal lenti-Cre or ad-Cre | KRAS-driven tumor initiation and progression |
| L-iKRAS | TetO-KrasG12D; Ccsp-rtTA | Doxycycline in drinking water | Reversible KRAS expression for maintenance studies |
| KSw/w | KrasLSL-G12D; Sox9 wild-type | Cre recombination | Control for Sox9 knockout studies |
| KSf/f | KrasLSL-G12D; Sox9flox/flox | Cre recombination | Sox9 loss-of-function in established KRAS tumors |
Sox9 Knockout Strategies
CRISPR/Cas9-Mediated Sox9 Knockout
The pSECC CRISPR system was utilized to simultaneously deliver Cre recombinase for KRASG12D activation and Cas9 with guide RNAs for Sox9 knockout [37] [19]. This all-in-one system enables efficient tumor initiation and gene editing in vivo:
- Guide RNA Design: Three guide RNAs targeting murine Sox9 were designed and validated, with sgSox9.2 demonstrating highest efficiency for in vivo studies [19]
- Delivery Method: Intratracheal administration of lentiviral or adenoviral vectors containing pSECC-sgSox9.2-Cre to lung epithelial cells
- Controls: tdTomato guide RNA (sgTom) served as the control condition [19]
Cre-LoxP Mediated Conditional Knockout
For validation studies, a traditional Cre-LoxP approach was employed using KrasLSL-G12D mice crossed with Sox9flox/flox mice, allowing tissue-specific Sox9 deletion upon Cre administration [19]. This method provides more uniform Sox9 deletion across the lung epithelium and avoids potential heterogeneity associated with CRISPR delivery.
Key Experimental Findings
SOX9 Deletion Reduces Tumor Development and Progression
Sox9 knockout significantly impaired KRASG12D-driven tumorigenesis across multiple parameters and timepoints. Quantitative analyses revealed:
Table 2: Tumor Phenotypes in Sox9-Knockout Models
| Parameter | Control (sgTom) | Sox9 KO (sgSox9.2) | Statistical Significance | Time Point |
|---|---|---|---|---|
| Tumor Number | High (~15-20/lung) | Significantly reduced | p = 0.018 | 18-30 weeks |
| Tumor Burden | High (30-40% area) | Significantly reduced | p = 0.029 | 18-30 weeks |
| Grade 3 Tumors | 12 tumors | 1 tumor | p = 0.0008 | 24-30 weeks |
| Ki67+ Cells | 25-40% in SOX9+ tumors | <10% in SOX9- tumors | p = 0.00092 | Multiple timepoints |
| Overall Survival | Median 33 weeks (KRAS only) | Significantly extended | p = 0.0012 | Endpoint (380 days) |
Notably, tumor progression from low to high grade was markedly suppressed in Sox9-knockout models [19]. While control animals developed numerous Grade 3 tumors exhibiting dysplastic features (large nuclear-cytoplasmic ratio, pleomorphic nuclei, prominent nucleoli), Sox9-deficient lungs contained predominantly Grade 1-2 tumors with more benign histology [19]. The rare Grade 3 tumors that emerged in knockout models displayed only partial high-grade features and notably lacked the characteristic high nuclear-cytoplasmic ratio of fully progressed lesions [19].
SOX9 Remodels the Tumor Immune Microenvironment
Comprehensive immune profiling demonstrated that SOX9 fundamentally reshapes the tumor immune landscape toward an immunosuppressive state:
Table 3: Immune Cell Infiltration Changes with SOX9 Knockout
| Immune Cell Type | SOX9-High Tumors | SOX9-Knockout Tumors | Functional Consequence |
|---|---|---|---|
| CD8+ T Cells | Severely reduced | Significantly increased | Enhanced tumor cell killing |
| Natural Killer (NK) Cells | Suppressed | Increased infiltration and activity | Improved innate immune surveillance |
| Dendritic Cells | Limited tumor infiltration | Markedly increased | Enhanced antigen presentation |
| M2 Macrophages | Elevated | Reduced | Decreased immunosuppression |
| Tregs | Increased | Trend toward reduction | Reduced immune suppression |
Mechanistically, SOX9 was found to significantly elevate collagen-related gene expression and promote substantial collagen fiber deposition within tumors [37] [19]. This extracellular matrix remodeling increases tumor stiffness and creates a physical barrier to immune cell infiltration, particularly affecting dendritic cells whose migration capabilities are impaired in dense collagen matrices [37]. The consequent reduction in dendritic cell infiltration limits antigen presentation to T cells, resulting in diminished CD8+ T cell and NK cell recruitment and activation [37].
Immunocompetence is Required for Full SOX9 Phenotype
A critical finding emerged from tumor grafting experiments comparing growth in immunocompetent versus immunocompromised mice [19]. While SOX9 overexpression significantly enhanced tumor growth in syngeneic immunocompetent hosts, this growth advantage was substantially attenuated in immunodeficient mice [19]. This demonstrates that the pro-tumorigenic effects of SOX9 are partially dependent on its immunomodulatory functions rather than solely on cell-intrinsic growth advantages.
Detailed Methodologies
In Vivo Sox9 Knockout Using CRISPR/Cas9
pSECC Vector Preparation
The pSECC (lenti-sgRNA-PGK-Cre-EF1a-Cas9-2A-tdTomato) vector system was employed for concurrent CRISPR-mediated Sox9 knockout and Cre-dependent KRASG12D activation [19]:
- sgRNA Cloning: Sox9-targeting guide sequence (sgSox9.2: 5'-GACCCGAAGCGCAAGCTCGA-3') was cloned into the pSECC vector using BstXI/BlpI restriction sites [19]
- Control Vector: tdTomato-targeting sgRNA (sgTom) served as control
- Virus Production: Lentiviral particles were produced in HEK293T cells using standard packaging plasmids and concentrated by ultracentrifugation
- Titer Determination: Viral titers were determined by tdTomato+ cell quantification in infected HEK293T cells
Intratracheal Delivery and Tumor Induction
- Anesthesia: Mice were anesthetized with ketamine/xylazine mixture (100/10 mg/kg)
- Delivery: 50μL of lentiviral suspension (1×10^8 IU/mL) was administered intratracheally using a blunt-ended 22G catheter
- Monitoring: Tumor development was monitored weekly by micro-CT imaging starting at 8 weeks post-infection
- Endpoint Analysis: Animals were sacrificed at 18, 24, and 30 weeks for comprehensive tumor assessment
Tumor Organoid Culture and Allograft Experiments
3D Tumor Organoid Culture
- Cell Lines: Established KrasG12D mouse lung tumor cell lines (mTC11, mTC14) with low endogenous SOX9 were utilized [19]
- SOX9 Modulation: Lentiviral transduction for SOX9 overexpression (mSox9OE) or CRISPR knockout
- Organoid Culture: 5,000 cells/well were embedded in Growth Factor Reduced Matrigel and cultured in organoid media containing FGF10, EGF, Noggin, and R-spondin
- Quantification: Organoid size and number were quantified at days 7, 14, and 21 using brightfield microscopy and image analysis
Syngeneic Allograft Experiments
- Cell Preparation: 1×10^6 control or SOX9-overexpressing KrasG12D tumor cells in 100μL PBS
- Transplantation: Subcutaneous injection into flanks of syngeneic C57BL/6J mice (immunocompetent) or NSG mice (immunocompromised)
- Tumor Measurement: Tumor dimensions measured twice weekly with digital calipers
- Endpoint Analysis: Tumors harvested at 4 weeks for flow cytometry, IHC, and RNA analysis
Immune Profiling and Microenvironment Analysis
Flow Cytometry Immune Phenotyping
Single-cell suspensions from dissociated tumors were stained with the following antibody panels:
- T Cell Panel: CD45, CD3, CD4, CD8, FoxP3, PD-1, Tim-3, Lag-3
- Myeloid Panel: CD45, CD11b, Ly6G, Ly6C, F4/80, CD206, MHC-II, CD11c
- NK Cell Panel: CD45, NK1.1, CD49b, CD27, CD11b, CD107a, IFN-γ
- Analysis: Data acquired on 3-laser flow cytometer and analyzed using FlowJo software
Histological Analysis and Immunohistochemistry
- Tissue Processing: Lungs were inflation-fixed with 10% neutral buffered formalin, paraffin-embedded, and sectioned at 5μm
- H&E Staining: Standard hematoxylin and eosin staining for tumor grading and burden assessment
- IHC Staining: Automated IHC was performed for SOX9 (1:500, Millipore AB5535), Ki67 (1:1000, Abcam ab16667), Collagen I (1:500, Abcam ab34710), and CD8 (1:200, Cell Signaling 98941)
- Quantification: Five random fields per tumor were imaged and analyzed using ImageJ with cell counting and color deconvolution plugins
Gene Expression Analysis
- RNA Extraction: Total RNA from snap-frozen tissues using TRIzol reagent
- qRT-PCR: TaqMan assays for collagen genes (Col1a1, Col3a1, Col5a1), immune markers (Cd8a, Ncr1, Ccl5, Ifng), and SOX9 target genes
- Bulk RNA Sequencing: Library preparation with Illumina TruSeq and sequencing on NovaSeq 6000
- Single-Cell RNA Sequencing: 10X Genomics platform with cellranger pipeline for analysis
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for SOX9-KRAS Immunology Studies
| Reagent/Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| CRISPR/Cas9 System | pSECC vector (sgRNA+Cas9+Cre) | Simultaneous gene knockout and Cre recombination | All-in-one system simplifies in vivo editing [19] |
| Mouse Models | KrasLSL-G12D; Sox9flox/flox | Spontaneous LUAD with conditional Sox9 deletion | Ideal for studying tumor-immune interactions [37] [19] |
| Lentiviral Vectors | Lenti-Cre, lenti-sgSox9 | In vivo gene delivery to lung epithelium | Intratracheal delivery ensures lung-specific targeting [19] |
| Organoid Culture | Matrigel, FGF10, EGF, Noggin | 3D tumor growth mimicking in vivo architecture | Preserves tumor heterogeneity for drug testing [19] |
| Immune Profiling | Flow cytometry antibodies, MHC multimers | Comprehensive immune cell quantification | Panels should cover adaptive and innate immunity [37] |
| Extracellular Matrix | Collagen I antibodies, Masson's Trichrome | Visualization of stromal remodeling | Critical for assessing SOX9-mediated fibrosis [37] [19] |
Discussion and Future Perspectives
This case study establishes a robust experimental framework for investigating transcription factor function in cancer immunology using sophisticated GEMMs and genome editing tools. The findings demonstrate that SOX9 is a bona fide driver of KRAS-induced lung adenocarcinoma that promotes tumor progression through dual mechanisms: direct enhancement of tumor cell proliferation and remodeling of the tumor immune microenvironment toward an immunosuppressive state [37] [19].
The clinical implications of these findings are significant. SOX9 represents a promising therapeutic target, particularly in KRASG12D-driven LUAD where direct KRAS inhibition remains challenging [35]. Therapeutic strategies could include direct SOX9 inhibition, targeting downstream effectors of its immunosuppressive program, or combining SOX9-directed therapies with existing immunotherapies. The observed collagen deposition and increased tumor stiffness suggest that anti-fibrotic agents might reverse SOX9-mediated immune exclusion and improve response to checkpoint inhibitors [37].
For researchers building upon this work, several key directions emerge:
- Development of direct SOX9 inhibitors or degraders for therapeutic testing
- Investigation of SOX9's role in therapeutic resistance to KRAS inhibitors and immunotherapy
- Exploration of SOX9's immunomodulatory functions in other KRAS-mutant cancers
- Analysis of human LUAD samples to validate the SOX9-immune signature correlation
The integration of CRISPR/Cas9 technology with immuno-oncology models, as demonstrated here, provides a powerful approach to dissect complex tumor-immune interactions and identify novel therapeutic opportunities in KRAS-driven lung cancer.
Osteoarthritis (OA) is a painful and debilitating degenerative joint disease affecting over 500 million people worldwide, characterized by progressive cartilage destruction and synovial inflammation [6] [38]. Current treatments primarily focus on symptom management, with joint replacement representing the final surgical option [6]. Intra-articular injection of mesenchymal stromal cells (MSCs) has emerged as a promising therapeutic approach, offering both immunomodulatory properties and potential cartilage regeneration capabilities [6] [39]. However, the significant heterogeneity in MSC preparations has hampered treatment optimization and consistent clinical outcomes [6] [38].
This case study details an innovative strategy employing CRISPR-mediated gene regulation to enhance MSC therapy for OA. The approach simultaneously fine-tunes two key transcription factors: SOX9 activation via CRISPR activation (CRISPRa) and RelA inhibition via CRISPR interference (CRISPRi) [6]. SOX9 serves as the "master regulator" of chondrogenesis, directing chondrocyte differentiation and cartilage extracellular matrix production [6] [40]. Conversely, RelA (a major subunit of NF-κB) governs pro-inflammatory responses that drive OA pathogenesis [6]. This dual-target strategy represents a significant advancement beyond traditional gene knockout approaches, allowing for precise transcriptional fine-tuning to optimize MSC therapeutic potential while maintaining native regulatory dynamics.
Key Signaling Pathways in Osteoarthritis Pathogenesis
The therapeutic strategy targets two interconnected pathways critical to OA progression. The diagram below illustrates the core pathological and therapeutic mechanisms addressed in this case study.
SOX9 in Cartilage Homeostasis
SOX9 is a transcription factor essential for chondrocyte development and function, activating genes encoding critical cartilage extracellular matrix components including type II collagen (COL2A1) and aggrecan (ACAN) [6] [41]. In OA pathogenesis, SOX9 expression and protein stability are compromised through multiple mechanisms, including enhanced degradation mediated by altered lipid metabolism [41]. The diagram highlights how SOX9 degradation disrupts cartilage anabolism, creating an imbalance toward tissue destruction.
NF-κB/RelA in Inflammation
The NF-κB signaling pathway, particularly its RelA/p65 subunit, is activated by various OA stress factors including inflammatory cytokines (TNF-α, IL-1β), mechanical stress, and lipid mediators [6] [40]. RelA activation drives expression of catabolic enzymes such as matrix metalloproteinases (MMPs) and ADAMTS, which directly degrade cartilage matrix [6] [41]. Interestingly, NF-κB also directly regulates SOX9 expression, creating complex cross-talk between inflammatory and differentiation pathways [40].
Experimental Workflow and Protocol
The complete methodology from vector design to in vivo validation is outlined below, with the following diagram summarizing the key experimental stages.
CRISPR-dCas9 Vector Design and Construction
The protocol employs a dual-system approach for simultaneous transcriptional activation and repression [6]:
3.1.1. CRISPRa System for SOX9 Activation
- Activation construct: Lenti-dSpCas9-VP64 expressing a fusion of Streptococcus pyogenes dCas9 with transcriptional activation domain VP64
- SOX9-targeting gRNAs: Five gRNAs designed to target the SOX9 promoter region (positions -74 to -276 relative to TSS)
- Primary gRNA sequences:
- Sox9-2:
CGGGTTGGGTGACGAGACAGG(position -167) - Sox9-3:
ACTTACACACTCGGACGTCCC(position -276) - Sox9-4:
TGGACCGGATTTTGGAAGGG(position -124)
- Sox9-2:
3.1.2. CRISPRi System for RelA Inhibition
- Inhibition construct: Lenti-dSaCas9-KRAB expressing a fusion of Staphylococcus aureus dCas9 with transcriptional repression domain KRAB
- RelA-targeting gRNAs: Five gRNAs designed to target the RelA promoter region (positions -41 to -628)
- Primary gRNA sequences:
- RelA-1:
CCGAAATCCCCTAAAAACAGA(position -41) - RelA-2:
TGATGTGTTGCGTCCTCCGGC(position -628) - RelA-3:
TGCTCCCGCGGAGGCCAGTGA(position -189)
- RelA-1:
3.1.3. Dual gRNA Expression Vector
- Lenti-EGFP-dual-gRNA vector expressing two gRNA scaffolds for SpCas9 and SaCas9 respectively
- Enables simultaneous Sox9 activation and RelA repression when co-expressed with dSpCas9-VP64 and dSaCas9-KRAB
Lentiviral Production and MSC Transduction
3.2.1. Lentiviral Production
- Prepare lentiviral vectors using standard packaging systems (psPAX2, pMD2.G)
- Transfert HEK293T cells using polyethylenimine (PEI) or calcium phosphate methods
- Collect viral supernatants at 48h and 72h post-transfection, concentrate by ultracentrifugation
- Determine viral titer by transduction of HEK293T cells with serial dilutions
3.2.2. MSC Culture and Transduction
- Isplicate CD45-negative bone marrow-derived MSCs (BMSCs) from human donors or commercial sources
- Maintain in α-MEM supplemented with 10% FBS, 1% penicillin-streptomycin
- Transduce MSCs at passage 3-5 with lentiviral vectors at MOI of 10-20 in the presence of 8μg/mL polybrene
- Select successfully transduced cells using puromycin (1-2μg/mL) for 7 days
- Confirm transduction efficiency by EGFP fluorescence and quantitative PCR
In Vitro Validation assays
3.3.1. Chondrogenic Differentiation Potential
- Culture transduced MSCs in chondrogenic differentiation medium (TGF-β3, dexamethasone, ascorbate-2-phosphate, proline, ITS+ premix)
- Maintain pellet cultures for 21 days, changing medium every 2-3 days
- Assess chondrogenesis by:
- Histological analysis: Safranin O/Fast Green staining for proteoglycans
- Gene expression: qRT-PCR for SOX9, COL2A1, ACAN
- Immunohistochemistry: Type II collagen deposition
3.3.2. Immunomodulatory Potential
- Stimulate transduced MSCs with TNF-α (10ng/mL) and IL-1β (10ng/mL) for 24h
- Measure RelA/NF-κB activation by:
- Nuclear translocation: Immunofluorescence staining
- Target gene expression: qRT-PCR for NFKBIA and other NF-κB targets
- Co-culture with peripheral blood mononuclear cells (PBMCs) to assess T-cell suppression capacity
In Vivo OA Model Assessment
3.4.1. OA Model Establishment
- Use 10-12 week old C57BL/6J mice
- Induce OA by surgical destabilization of the medial meniscus (DMM model)
- Alternatively, use metabolic OA models through high-fat diet feeding
3.4.2. Cell Administration and Analysis
- Administer 10^5 CRISPR-enhanced MSCs in 10μL PBS via intra-articular injection 4 weeks post-OA induction
- Control groups: Inject with cell culture medium or unmodified MSCs
- Assess outcomes at 8-12 weeks post-injection:
- Pain behavior: Weight-bearing distribution and mechanical allodynia
- Cartilage integrity: OARSI scoring of Safranin O-stained sections
- Cell retention: Track EGFP-labeled cells in joint tissues
- Molecular analysis: Immunostaining for anabolic/catabolic factors
Key Experimental Results and Data
Quantitative Outcomes of CRISPR-Modified MSC Therapy
Table 1: Therapeutic Efficacy of CRISPR-Modified MSCs in Murine OA Model
| Parameter | Culture Medium Control | Unmodified MSCs | CRISPR-Modified MSCs | Assessment Method |
|---|---|---|---|---|
| Cartilage Degradation (OARSI Score) | 4.2 ± 0.3 | 3.1 ± 0.4 | 1.5 ± 0.2 | Histological scoring |
| Pain Reduction (%) | 0% | 28% ± 6% | 67% ± 8% | Weight-bearing asymmetry |
| SOX9 Expression (Fold Change) | 1.0 ± 0.1 | 1.8 ± 0.3 | 4.5 ± 0.6 | qRT-PCR |
| COL2A1 Expression (Fold Change) | 1.0 ± 0.2 | 2.1 ± 0.4 | 5.2 ± 0.7 | qRT-PCR |
| MMP13 Expression (% Reduction) | 0% | 22% ± 5% | 71% ± 6% | Immunohistochemistry |
| Cell Retention (Weeks) | N/A | 2-3 weeks | 6-8 weeks | EGFF fluorescence tracking |
| Synovial Inflammation (Score) | 3.8 ± 0.4 | 2.9 ± 0.3 | 1.4 ± 0.2 | Histological scoring |
Table 2: In Vitro Characterization of CRISPR-Modified MSCs
| Assessment | Unmodified MSCs | CRISPR-Modified MSCs | Experimental Conditions |
|---|---|---|---|
| Chondrogenic Differentiation | |||
| - Sulfated GAGs (μg/μg DNA) | 12.3 ± 1.5 | 28.7 ± 2.1 | Pellet culture, 21 days |
| - COL2A1 Protein | Moderate | Strong | IHC staining |
| - ACAN Expression (Fold) | 1.0 ± 0.2 | 3.8 ± 0.5 | qRT-PCR |
| Immunomodulatory Function | |||
| - NF-κB Activation (Fold) | 1.0 ± 0.1 | 0.3 ± 0.1 | TNF-α/IL-1β stimulation |
| - IL-6 Secretion (pg/mL) | 845 ± 75 | 290 ± 45 | TNF-α stimulation |
| - T-cell Suppression (%) | 42% ± 6% | 78% ± 7% | PBMC co-culture |
| Gene Expression Fine-Tuning | |||
| - SOX9 mRNA (Fold) | 1.0 ± 0.1 | 3.2 ± 0.4 | Basal conditions |
| - RelA mRNA (Fold) | 1.0 ± 0.1 | 0.4 ± 0.1 | Basal conditions |
Mechanistic Insights
The enhanced therapeutic efficacy of CRISPR-modified MSCs stems from multiple synergistic mechanisms:
4.2.1. Promoted Cartilage Integrity Modified MSCs significantly increased production of anabolic factors including type II collagen and aggrecan while enhancing SOX9-driven chondrogenic differentiation [6]. The fine-tuned SOX9 expression (approximately 3-4 fold increase) proved sufficient to drive robust chondrogenesis without causing hypertrophic differentiation.
4.2.2. Suppressed Catabolic Environment CRISPR-mediated RelA inhibition significantly reduced production of cartilage-degrading enzymes including MMP13 and ADAMTS, which are directly regulated by NF-κB signaling [6]. This created a more favorable microenvironment for cartilage preservation.
4.2.3. Enhanced Immunomodulation Modified MSCs demonstrated superior suppression of synovial inflammation and immune cell infiltration [6]. Single-cell RNA sequencing analysis of human OA synovium confirmed elevated NF-κB pathway activity in painful joints, validating RelA as a therapeutic target [6].
4.2.4. Improved Cell Retention A substantial number of modified MSCs survived in cartilaginous tissues including articular cartilage and meniscus for extended durations (6-8 weeks), suggesting enhanced engraftment potential compared to unmodified MSCs [6].
Research Reagent Solutions
Table 3: Essential Research Reagents for CRISPRa/i MSC Engineering
| Reagent/Category | Specific Examples | Function/Application | Notes |
|---|---|---|---|
| CRISPR System Components | dSpCas9-VP64, dSaCas9-KRAB | Transcriptional activation/repression | Use different Cas9 orthologs to avoid gRNA interference |
| gRNA Design | Sox9-2, Sox9-3, Sox9-4; RelA-1, RelA-2, RelA-3 | Target-specific gene regulation | Design multiple gRNAs per target; position near TSS |
| Delivery Vectors | Lenti-EGFP-dual-gRNA | Simultaneous gRNA expression | Include selection markers (puromycin) |
| Cell Culture Reagents | CD45- BMSCs, α-MEM, TGF-β3 | MSC isolation and chondrogenic differentiation | Use early passage cells (P3-P5) |
| Analytical Tools | Safranin O staining, OARSI scoring, qPCR assays | Outcome assessment | Validate with multiple methods |
| Animal Models | DMM surgical model, High-fat diet model | In vivo OA pathogenesis | Allow 4 weeks for OA development pre-treatment |
Technical Considerations and Troubleshooting
Optimization Parameters
gRNA Screening: The original study designed five gRNAs each for SOX9 and RelA, with varying efficiencies [6]. Comprehensive screening of multiple gRNAs is essential to identify the most effective sequences. Optimal gRNAs typically target regions -50 to -300 bp upstream of the transcription start site.
Expression Balancing: Simultaneous transcriptional activation and repression requires careful balancing of expression levels. Employ different antibiotic selection markers for individual constructs, and consider using bidirectional promoters for coordinated expression.
Delivery Optimization: Lentiviral transduction efficiency should be optimized for each MSC batch by testing various MOIs (typically 5-50) and polybrane concentrations (4-8μg/mL). Monitor transduction efficiency via EGFP fluorescence and confirm by quantitative PCR.
Common Challenges and Solutions
- Low Transduction Efficiency: Use early-passage MSCs, optimize viral concentration, include spinfection (centrifugation at 800-1000g for 30-60min)
- Insufficient Gene Regulation: Screen additional gRNAs, optimize dCas9-effector expression levels, consider synergistic gRNA combinations
- Reduced Chondrogenic Potential: Use fresh differentiation reagents, verify TGF-β3 activity, optimize cell density in pellet cultures
- Variable In Vivo Outcomes: Standardize OA induction, use consistent injection techniques, consider cell viability post-thaw
This case study demonstrates that CRISPR-dCas9-mediated fine-tuning of SOX9 and RelA represents a promising strategy for enhancing MSC-based osteoarthritis therapy. The simultaneous transcriptional activation of chondrogenic programs and repression of inflammatory signaling creates MSCs with superior cartilage-protective and immunomodulatory capacities [6].
The approach offers several advantages over conventional gene editing: it enables precise transcriptional control without permanent genomic alterations, maintains native feedback regulation, and allows dose-dependent effects more suitable for therapeutic applications [6]. The methodology can be adapted to target additional pathways involved in OA pathogenesis or extended to other cell-based therapies for degenerative joint diseases.
For researchers investigating SOX9 in immune cell models, this CRISPRa/i platform provides a valuable tool for probing gene function without complete knockout, enabling studies of graded gene expression effects on immune cell differentiation and function [1] [42]. The continued refinement of CRISPR-based transcriptional regulation will further enhance our ability to engineer therapeutic cells with optimized functional properties for musculoskeletal regeneration.
The Sex-determining Region Y-related High-Mobility Group Box 9 (SOX9) is a transcription factor with emerging roles in immune cell function and cancer biology, making it a compelling target for advanced cell therapies. While initially characterized for its crucial functions in chondrogenesis and organ development, recent research has illuminated SOX9's complex, context-dependent roles in immunomodulation. SOX9 exhibits dual functionality in immunology, acting as a "double-edged sword" by promoting immune escape in cancer on one hand, while contributing to tissue repair and macrophage function on the other [1]. This biological duality positions SOX9 as a strategic target for engineering more potent cellular immunotherapies.
In the tumor microenvironment, SOX9 expression drives immunosuppressive networks that protect malignant cells from immune surveillance. In lung adenocarcinoma (LUAD), SOX9 expression significantly elevates collagen-related gene expression and increases collagen fibers, creating a physical barrier that inhibits infiltration of cytotoxic immune cells [19]. SOX9-mediated suppression of tumor-infiltrating CD8+ T cells, natural killer (NK) cells, and dendritic cells establishes an "immune desert" microenvironment conducive to tumor progression [19]. This immunosuppressive function, coupled with SOX9's role in safeguarding dedifferentiated tumor cells from immune surveillance in breast cancer models [5], provides a compelling rationale for targeting SOX9 to enhance cancer immunotherapy.
The development of CRISPR-Cas9 technologies has enabled precise manipulation of SOX9 in therapeutic cell products. Both complete knockout using catalytically active Cas9 and sophisticated transcriptional modulation using nuclease-deficient dCas9 fused to effector domains have demonstrated significant potential for optimizing cell therapies [6]. This application note details current methodologies and experimental protocols for integrating SOX9 editing with CAR-T and other cell therapy platforms, providing researchers with practical frameworks for implementing these approaches.
Table 1: Functional Outcomes of SOX9 Manipulation in Preclinical Cancer Models
| Cancer Model | Intervention Type | Key Functional Outcomes | Impact on Tumor Growth | Immune Context |
|---|---|---|---|---|
| Lung adenocarcinoma (KrasG12D驱动) [19] | CRISPR-Cas9 knockout | Reduced tumor number and burden; suppressed progression to high-grade tumors | Significant reduction (p=0.018 tumor number; p=0.029 burden) | Decreased immune cell infiltration (CD8+ T, NK, dendritic cells) |
| Breast cancer [5] | Endogenous expression | Protection of dedifferentiated tumor cells from immune surveillance; B7x upregulation | Promoted tumor progression | Reduced tumor-infiltrating lymphocytes |
| Osteoarthritis [6] | CRISPR-dCas9 activation | Enhanced chondrogenic potential; downregulated inflammatory responses | Not applicable (therapeutic effect) | Suppressed immune cells in joints; immunomodulatory properties |
| Skin carcinogenesis [20] | Inducible overexpression | Fate switching from epidermal to hair follicle stem cells; BCC-like features | Tumor formation upon sustained expression | Microenvironment remodeling |
Table 2: SOX9 Editing Approaches and Technical Parameters
| Editing Approach | Delivery System | Efficiency Metrics | Cell Type | Functional Assessment |
|---|---|---|---|---|
| CRISPR-Cas9 knockout [19] | pSECC (CRISPR + Cre combined) | Significant reduction in SOX9+ tumors (0.52-19.05% vs 9.87-48.77% in controls) | Lung tumor cells | Tumor burden, grade distribution, Ki67+ proliferation |
| CRISPR-dCas9 activation [6] | Lentiviral dSpCas9-VP64 | Enhanced chondrogenic and immunomodulatory potentials | Mesenchymal stromal cells (MSCs) | Chondrogenesis assays, cytokine production, pain relief |
| CRISPR-dCas9 inhibition [6] | Lentiviral dSaCas9-KRAB | Downregulated inflammatory responses | Mesenchymal stromal cells (MSCs) | Inhibition of catabolic enzymes, inflammatory factor reduction |
| SOX9 reconstitution [20] | Tetracycline-inducible system | Nuclear SOX9 detection within 1 week; proliferation increase by week 2 | Epidermal stem cells | Lineage tracing, proliferation markers, tumor formation |
SOX9 Signaling Pathways in Immunity and Cancer
SOX9 Immunomodulatory Signaling Network: This diagram illustrates the multifaceted role of SOX9 in cancer immunity and the therapeutic rationale for its inhibition. SOX9 functions as a pioneer transcription factor that binds closed chromatin and initiates extensive reprogramming of the cellular state [20]. Through chromatin remodeling, SOX9 activates expression of immunosuppressive factors including B7x (B7-H4/VTCN1), which protects dedifferentiated tumor cells from immune surveillance in breast cancer models [5]. Simultaneously, SOX9 drives collagen production and extracellular matrix remodeling in lung adenocarcinoma, creating a fibrotic tumor microenvironment (TME) that physically impedes cytotoxic immune cell infiltration [19]. These coordinated mechanisms establish SOX9 as a central regulator of the immunosuppressive TME, highlighting the therapeutic potential of CRISPR-mediated SOX9 disruption for enhancing tumor immune recognition and elimination.
Experimental Workflow for SOX9 Editing in Cell Therapies
SOX9 Editing Workflow for Cell Therapy: Comprehensive pipeline for implementing SOX9 modifications in therapeutic cell products. The process begins with careful target identification within SOX9 regulatory regions or coding sequences, followed by design of multiple guide RNAs (gRNAs) to ensure efficient editing [6]. For transcriptional modulation, this involves designing gRNAs targeting promoter regions of SOX9 (for activation) or RelA (for inhibition), with optimal positioning relative to transcription start sites [6]. Delivery method selection is critical, with lentiviral vectors providing stable integration for dCas9 systems, while electroporation of ribonucleoprotein (RNP) complexes enables rapid, transient editing with reduced off-target risks [43]. Following delivery, comprehensive molecular validation confirms editing efficiency through Sanger sequencing, next-generation sequencing, or functional protein assays. Finally, edited cells undergo rigorous functional characterization including transcriptomic profiling, in vitro functional assays, and ultimately in vivo validation in immunocompetent animal models to assess therapeutic potential and safety profiles.
Detailed Experimental Protocols
Protocol 1: CRISPR-Cas9-Mediated SOX9 Knockout in Primary Human T Cells
Principle: This protocol utilizes CRISPR-Cas9 ribonucleoprotein (RNP) complexes for efficient, transient SOX9 gene disruption in primary human T cells, enhancing their cytotoxic potential without viral integration.
Materials:
- Primary human T cells from leukapheresis product
- CRISPR-Cas9 RNP complexes: Alt-R S.p. Cas9 nuclease and SOX9-specific sgRNA
- Electroporation system (e.g., Lonza 4D-Nucleofector)
- T cell expansion medium: X-VIVO 15 with 5% human AB serum and 300 IU/mL IL-2
- Activation beads: CD3/CD28 Dynabeads
- Flow cytometry antibodies: SOX9, CD3, CD8, CD4, CD62L, CD45RO
- Genomic DNA extraction kit
- T7 Endonuclease I mutation detection assay
Procedure:
- T Cell Activation: Isolate PBMCs via density gradient centrifugation. Activate T cells using CD3/CD28 beads at 3:1 bead:cell ratio in expansion medium for 24 hours.
- RNP Complex Formation: Combine 60 pmol of Alt-R S.p. Cas9 nuclease with 120 pmol of SOX9 sgRNA in duplex buffer. Incubate 10-20 minutes at room temperature to form RNP complexes.
- Electroporation: Harvest 1×10^6 activated T cells, resuspend in 20 μL P3 Primary Cell solution. Add RNP complexes and electroporate using CM-137 program on 4D-Nucleofector. Immediately transfer to pre-warmed expansion medium.
- Post-Electroporation Culture: Maintain cells at 0.5-1×10^6 cells/mL in expansion medium with IL-2. Remove activation beads after 72 hours.
- Editing Efficiency Validation:
- Day 3: Extract genomic DNA. Amplify SOX9 target region by PCR. Perform T7E1 assay per manufacturer's instructions.
- Day 5: Analyze SOX9 protein expression by intracellular flow cytometry.
- Functional Assays: Evaluate cytokine production (IFN-γ, IL-2) by ELISA upon stimulation. Assess cytotoxic activity against tumor cells in real-time cytotoxicity assays.
Technical Notes: For optimal results, include a non-targeting sgRNA control. Test multiple sgRNAs targeting different SOX9 exons. Determine editing efficiency across multiple donors to account for variability.
Protocol 2: CRISPR-dCas9-Mediated SOX9/RelA Dual Modulation in MSCs
Principle: This protocol employs catalytically dead Cas9 (dCas9) fused to transcriptional activation (VP64) and repression (KRAB) domains for simultaneous SOX9 activation and RelA inhibition in mesenchymal stromal cells (MSCs), enhancing their chondrogenic and immunomodulatory potential.
Materials:
- Human bone marrow-derived MSCs (passage 3-5)
- Lentiviral vectors: Lenti-dSpCas9-VP64, Lenti-dSaCas9-KRAB, Lenti-EGFP-dual-gRNA
- Polybrene (8 μg/mL)
- MSC growth medium: α-MEM with 10% FBS, 1% GlutaMAX
- Chondrogenic differentiation medium: STEMPRO Chondrogenesis Differentiation Kit
- Antibodies: Anti-SOX9, anti-RelA, anti-aggrecan, anti-collagen type II
- qPCR primers: SOX9, RELA, ACAN, COL2A1, NFKBIA
Procedure:
- Guide RNA Design: Design and clone SOX9-activating gRNAs (e.g., Sox9-2: CGGGTTGGGTGACGAGACAGG) and RelA-repressing gRNAs (e.g., RelA-1: CCGAAATCCCCTAAAAACAGA) into Lenti-EGFP-dual-gRNA vector [6].
- Lentiviral Production: Generate lentivirus in HEK293T cells using standard packaging plasmids. Concentrate virus by ultracentrifugation.
- MSC Transduction: Plate MSCs at 1×10^4 cells/cm². Transduce with lentiviral vectors in presence of 8 μg/mL polybrene. Centrifuge at 800×g for 30 minutes (spinoculation). Replace medium after 8 hours.
- Selection and Expansion: After 72 hours, sort EGFP+ cells by FACS. Expand positively transduced cells for subsequent experiments.
- Molecular Validation:
- qPCR Analysis: Extract total RNA, synthesize cDNA, and perform qPCR for SOX9, RelA, and chondrogenic markers.
- Western Blotting: Confirm SOX9 upregulation and RelA downregulation at protein level.
- Functional Characterization:
- Chondrogenesis Assay: Pellet 2.5×10^5 cells by centrifugation. Culture in chondrogenic medium for 21 days. Analyze sulfated glycosaminoglycan content by Alcian blue staining.
- Immunomodulatory Assay: Co-culture engineered MSCs with peripheral blood mononuclear cells stimulated with anti-CD3/CD28. Measure IFN-γ production by ELISA.
Technical Notes: Use different Cas9 orthologs (SpCas9 and SaCas9) to prevent gRNA crosstalk. Include multiple gRNAs per target for enhanced efficacy. Monitor cell morphology and proliferation rates post-transduction.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents for SOX9 Editing Applications
| Reagent Category | Specific Product Examples | Research Application | Technical Considerations |
|---|---|---|---|
| CRISPR Nucleases | Alt-R S.p. Cas9 Nuclease V3, HiFi Cas9 | SOX9 knockout in immune cells | HiFi Cas9 reduces off-target effects in primary cells |
| CRISPR Activation | dSpCas9-VP64, dSaCas9-VP64 | SOX9 transcriptional activation | Multiple gRNAs enhance activation efficacy |
| CRISPR Inhibition | dSpCas9-KRAB, dSaCas9-KRAB | RelA/NF-κB pathway repression | KRAB domain provides strong repression |
| Delivery Systems | Lentiviral packaging systems, Alt-R CRISPR Electroporation Enhancer | RNP delivery to primary T cells | Enhancer improves editing efficiency in hard-to-transfect cells |
| Validation Tools | SOX9 monoclonal antibodies (RYM1C11), T7 Endonuclease I, Flow cytometry panels | Editing efficiency and functional validation | Multiplex validation approaches recommended |
| Cell Culture | CTS Immune Cell Serum-Free Medium, STEMPRO Chondrogenesis Differentiation Kit | Specialized maintenance of therapeutic cells | Xeno-free media preferred for clinical translation |
| gRNA Design | Alt-R CRISPR-Cas9 sgRNA, Custom sgRNA synthesis | Target-specific guide RNA | Design 3-5 gRNAs per target for screening |
Concluding Remarks and Future Perspectives
The integration of SOX9 editing with cell therapy platforms represents a promising frontier in immunotherapy optimization. Current evidence suggests that context-dependent modulation of SOX9—whether through complete knockout in effector immune cells or precise transcriptional regulation in stromal cells—can significantly enhance therapeutic efficacy by countering immunosuppressive mechanisms in the tumor microenvironment. The dual role of SOX9 in both immune regulation and tissue development necessitates careful consideration of the specific therapeutic context and potential on-target, off-tissue effects.
Future directions in this field will likely focus on multiplexed editing approaches that simultaneously target SOX9 alongside other immunomodulatory genes such as PD-1, TGFβR2, or FAS [44] [43]. The emergence of more precise editing technologies including base editing and prime editing offers opportunities for nuanced SOX9 modulation without double-strand breaks. Additionally, the development of inducible systems for temporal control of SOX9 editing may provide enhanced safety profiles for clinical translation. As synthetic biology continues to advance, engineered SOX9-responsive gene circuits may enable smart cell therapies that dynamically adapt to the therapeutic environment, further expanding the potential of SOX9-edited cellular therapeutics for cancer and inflammatory diseases.
Overcoming Technical Hurdles in CRISPR-Cas9 SOX9 Knockout Experiments
The development of advanced cell-based therapies, particularly those involving CRISPR-Cas9 genome editing, has emerged as a promising treatment modality for a wide range of diseases, including cancers, autoimmune disorders, and degenerative conditions [45]. Immune cells such as T cells, natural killer (NK) cells, and macrophages are being engineered to enhance their therapeutic efficacy and safety profiles. However, a significant technical challenge persists: the efficient delivery of biomolecules and genome-editing tools into these difficult-to-transfect cells [45] [46].
The fundamental cause of low transfection efficiency in immune cells lies in their inherent biological characteristics. Primary immune cells, directly isolated from living tissue, have limited proliferative capacity in vitro and are highly sensitive to culture conditions, with physical or chemical stimuli during transfection often triggering stress responses or apoptosis [47]. Their membrane structures are often denser and more stable, with charge characteristics unfavorable for the attachment and internalization of transfection complexes [47]. Furthermore, immune cells possess potent innate immune mechanisms that can recognize and degrade exogenous nucleic acids, creating additional barriers to successful transfection [46].
In the specific context of CRISPR-Cas9 SOX9 knockout research, efficient delivery of editing components is crucial for studying chondrogenesis and immune cell development. SOX9 serves as a master transcriptional regulator in chondrocyte differentiation, and its manipulation in immune models could provide valuable insights into joint diseases and immune-mediated cartilage destruction [6]. This application note provides a systematic framework for optimizing transfection protocols to achieve high-efficiency gene editing in challenging immune cell populations.
Understanding the Biological Barriers
Innate Immune Recognition of Foreign Nucleic Acids
The innate immune response to cytosolic DNA represents a significant barrier to successful transfection in immune cells. This protective mechanism, intended to protect the host from viral infections, can inhibit the delivery and expression of therapeutic transgenes in gene and cell therapies [46]. Transcriptomic analyses have revealed that key proteins involved in the innate immune response to cytosolic DNA are highly upregulated after transfection or constitutively expressed in difficult-to-transfect cells.
When immune cells detect transfected DNA through cytosolic or nuclear DNA sensors, they initiate a signaling cascade that culminates in the activation of cytokines and the expression of cytokine-stimulated genes (CSGs) that can directly inhibit transgene expression [46]. For example, the DNA sensor IFI16 has been shown to decrease plasmid-driven transgene expression by directly binding and blocking viral promoters [46]. Research demonstrates that overexpression of IFI16 significantly decreases transfection efficiency, highlighting the critical role of this pathway in limiting gene delivery [46].
Cell Type-Specific Challenges
Different immune cell types present unique challenges for transfection, as summarized in the table below.
Table 1: Transfection Challenges in Different Immune Cell Types
| Cell Type | Key Challenges | Notable Characteristics |
|---|---|---|
| T Cells | Relatively easier to transfect when activated, but sensitive to cytotoxicity | High proliferative capacity upon CD3/CD28 activation; upregulated receptor expression enhances viral susceptibility [34] |
| NK Cells | Low baseline transduction efficiency; strong antiviral defenses | Innate immune properties and restriction factors limit gene delivery; often require higher viral titers or tropism-engineered vectors [34] |
| Macrophages | Low proliferative capacity; specialized functions limit transfection | Receptor expression profiles dictate transduction efficiency; polarization state affects transfection outcomes [45] [34] |
| Dendritic Cells | Difficult to transfect; lower proliferative capacity | Receptor-mediated entry depends on specific surface markers; non-integrating vectors often preferred [34] |
Optimization Strategies for Improved Transfection
Physical Transfection Methods: Electroporation
Electroporation has proven to be one of the most effective methods for transfecting difficult-to-transfect immune cells. This technique uses an electrical field to create temporary pores in the cell membrane, allowing for the introduction of genetic material such as CRISPR-Cas9 components [48]. Optimization of electroporation parameters is crucial for balancing high transfection efficiency with maintained cell viability.
Recent advances in electroporation technology have demonstrated remarkable success in immune cell engineering. The MaxCyte ExPERT platform has achieved transfection efficiencies of nearly 80% in T cells, NK cells, and macrophages within one day of electroporation, with no significant impact on cell viability [45]. Importantly, these systems enable seamless scaling – for NK cells, optimized conditions were successfully scaled from 1.3 million cells to 2.5 billion cells with no drop in efficiency or viability [45]. Similarly, for T cells, conditions optimized at 120 million cells were used to engineer 3.9 billion cells without re-optimization [45].
For CRISPR-SOX9 knockout experiments, ribonucleoprotein (RNP) electroporation offers significant advantages. The RNP complex is cleared from cells rapidly, reducing off-target effects and immune responses [7]. A recent study demonstrated that electroporation significantly enhanced transfection and editing efficiency in primary human cells while preserving high cell viability, achieving knockout efficiencies of approximately 90% [7].
Viral Transduction Optimization
Viral transduction remains a highly efficient method for gene delivery in immune cells, with each viral platform offering distinct advantages and limitations.
Table 2: Viral Vector Systems for Immune Cell Transduction
| Vector System | Transgene Expression | Payload Capacity | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Lentivirus (LV) | Stable, integrating | ~8 kb | Transduces dividing & non-dividing cells; broad tropism with VSV-G pseudotyping [34] [48] | Insertional mutagenesis risk (reduced with SIN designs) [34] |
| Gamma-retrovirus (γRV) | Stable, integrating | ~8 kb | Robust integration in proliferating cells [34] | Only transduces dividing cells; poor NK cell tropism; innate immune recognition [34] |
| Adenovirus (AV) | Transient, non-integrating | ~8 kb | High efficiency across immune cells; rapid production [34] [48] | Pronounced immunogenicity; limited payload capacity [34] |
| Adeno-associated virus (AAV) | Transient, non-integrating | ~4.7 kb | Favorable safety profile; low immunogenicity [34] [48] | Small payload capacity; requires capsid engineering for immune cell targeting [34] |
To optimize viral transduction for CRISPR-SOX9 editing, several strategies have proven effective:
- Cell pre-activation: Enhancing viral receptor expression through CD3/CD28 stimulation for T cells or cytokine priming for NK cells [34]
- Vector engineering: Utilizing pseudotyped vectors with enhanced tropism for specific immune cell types [34]
- Process enhancements: Implementing spinoculation to enhance cell-vector contact and careful titration of multiplicity of infection (MOI) [34]
- Transduction enhancers: Incorporating additives such as poloxamers or protamine sulfate to improve transduction efficiency [34]
Chemical and Non-Viral Methods
While viral methods generally offer higher efficiency, non-viral approaches provide advantages in safety, cost, and simplicity. Chemical transfection methods utilize cationic lipids, polymers, or lipid/polymer hybrids to form complexes with nucleic acids that facilitate cellular uptake through endocytosis [46] [48].
Key optimization parameters for chemical transfection include:
- Serum-compatible formulations: Selecting transfection reagents that maintain stability and efficiency in serum-containing media to reduce cellular stress [47]
- Lipid:RNA/DNA ratio optimization: Determining the optimal mass ratio or charge ratio (N/P ratio) to generate nanoparticles with uniform size and appropriate surface charge [47]
- Exposure time reduction: Limiting transfection complex exposure to 1-4 hours to mitigate cytotoxicity while maintaining sufficient nucleic acid uptake [47]
- Endosomal escape enhancers: Incorporating compounds such as chloroquine or novel ionizable lipids that disrupt endosomal membranes and promote nucleic acid release into the cytoplasm [47]
For CRISPR-Cas9 editing, lipid nanoparticles (LNPs) have shown promise for RNP delivery, though electroporation generally achieves higher efficiency in primary immune cells [7].
CRISPR-Cas9 SOX9 Knockout Workflow
The following diagram illustrates the optimized workflow for CRISPR-Cas9 mediated SOX9 knockout in difficult-to-transfect immune cells:
gRNA Design and Validation
Efficient gRNA design is critical for successful SOX9 knockout. Multiple computational tools are available to predict gRNA on-target efficiency and minimize off-target effects:
Table 3: gRNA Design Tools and Their Key Features
| Tool Name | On-Target Scoring Method | Off-Target Scoring Method | Key Features |
|---|---|---|---|
| CRISPick | Rule Set 3 [49] | Cutting Frequency Determination (CFD) [49] | User-friendly interface; developed by Broad Institute [49] |
| CHOPCHOP | Rule Set 1, CRISPRscan [49] | Homology analysis [49] | Supports various CRISPR-Cas systems; visual off-target representations [49] |
| CRISPOR | Rule Set 2, CRISPRscan [49] | MIT specificity score, CFD [49] | Detailed off-target analysis; position-specific mismatch scoring [49] |
| GenScript Tool | Rule Set 3 [49] | CFD [49] | Integrated ordering capability; supports SpCas9 and AsCas12a [49] |
Key parameters for efficient gRNA design include:
- On-target efficiency: Predicted editing efficiency at the intended target site, influenced by factors such as nucleotide composition (preference for A in middle positions, avoidance of GGG motifs) and position-specific nucleotides (G in position 20 is favorable) [50]
- Off-target risk minimization: Comprehensive genome-wide analysis of potential off-target sites with significant homology to the target sequence [49] [50]
- GC content: Optimal range of 40-60%, with extremes (>80% or <20%) associated with reduced efficiency [50]
For SOX9 targeting, multiple gRNAs should be designed and empirically validated using a positive control gene such as RELA, which has well-characterized editing efficiency across immune cell types [51].
CRISPR Component Delivery
For SOX9 knockout in immune cells, the ribonucleoprotein (RNP) delivery method is preferred over plasmid DNA due to reduced immune recognition and faster kinetics. The optimized protocol involves:
RNP Complex Assembly:
- Combine 10 µg of high-purity Cas9 protein with 5 µg of synthetic sgRNA (molar ratio 1:2.5)
- Incubate at room temperature for 15-20 minutes to form RNP complexes
- Use modified sgRNAs with 2'-O-methyl-3'-phosphonoacetate to enhance stability and reduce immune stimulation [7]
Electroporation Parameters:
- Use specialized buffers such as P3 or P5 primary cell solutions
- Optimize cell density to 1-2×10^7 cells/mL in electroporation cuvettes
- Apply cell type-specific electrical parameters (typically 1500-1700V for T cells, 1400-1600V for NK cells)
- Immediately transfer electroporated cells to pre-warmed complete medium with cytokines (IL-2 for T cells, IL-15 for NK cells) [45] [7]
Critical Controls for CRISPR Experiments
Appropriate controls are essential for validating SOX9 knockout experiments and interpreting results accurately:
- Transfection controls: Fluorescent reporters (e.g., GFP mRNA) to assess delivery efficiency [51]
- Positive editing controls: Validated gRNAs targeting genes with known high editing efficiency (e.g., RELA, TRAC) [51]
- Negative editing controls: Scrambled gRNA with no genomic target, gRNA-only, or Cas9-only conditions [51]
- Mock controls: Cells subjected to transfection conditions without nucleic acids to account for stress responses [51]
Troubleshooting and Quality Assessment
Assessing Transfection and Editing Efficiency
Comprehensive quality control is essential for successful CRISPR-SOX9 knockout experiments. The following parameters should be monitored:
- Transfection efficiency: Quantified using fluorescent reporters or immunofluorescence staining, typically 24 hours post-transfection [34]
- Cell viability: Assessed via trypan blue exclusion or Annexin V/7-AAD staining, with targets >70% for electroporation and >85% for viral transduction [34]
- Editing efficiency: Measured using T7E1 assay, TIDE analysis, or next-generation sequencing 72-96 hours post-transfection [7] [51]
- Phenotypic validation: Western blot for SOX9 protein expression loss and functional assays for downstream effects [7]
Troubleshooting Common Issues
Table 4: Troubleshooting Guide for Common Transfection Problems
| Problem | Potential Causes | Solutions |
|---|---|---|
| Low Transfection Efficiency | Suboptimal delivery parameters; innate immune activation; insufficient cell activation [46] [47] | Optimize voltage/waveform (electroporation); increase MOI (viral); use serum-compatible reagents; enhance cell activation [47] [34] |
| Poor Cell Viability | Excessive electrical pulses; cytotoxic transfection reagents; high viral load [47] [34] | Reduce pulse duration/voltage; shorten reagent exposure time; decrease MOI; add cytokine support (IL-2, IL-7, IL-15) [47] [34] |
| High Off-Target Effects | Low-specificity gRNA; excessive RNP concentration; prolonged expression from plasmids [49] [50] | Redesign gRNA with improved specificity scores; use RNP instead of plasmid; titrate RNP to lowest effective concentration [49] [7] |
| Inconsistent Editing Between Cell Donors | Donor variability in DNA repair efficiency; differences in cell state and activation [34] [7] | Standardize cell activation protocol; pre-screen donors for transfection competence; use pooled donors for allogene approaches [34] |
Table 5: Key Research Reagent Solutions for Immune Cell Transfection
| Reagent/Category | Specific Examples | Function & Application |
|---|---|---|
| Electroporation Systems | MaxCyte ExPERT platform; Lonza 4D-Nucleofector [45] [7] | Physical delivery of CRISPR components via electrical pulses; scalable from research to clinical manufacturing [45] |
| Viral Vector Systems | Lentivirus (VSV-G pseudotyped); Gamma-retrovirus [34] | Stable integration of large genetic payloads; suitable for long-term transgene expression in proliferating immune cells [34] |
| Chemical Transfection Reagents | Lipofectamine CRISPRMAX; BioRender TransIT-X2 [47] | Lipid-based nanoparticles for RNP or nucleic acid delivery; optimized for difficult-to-transfect cells [47] |
| gRNA Design Tools | CRISPick; CHOPCHOP; CRISPOR [49] | Computational prediction of gRNA efficiency and specificity; reduces experimental optimization time [49] |
| Cell Activation Reagents | CD3/CD28 antibodies; IL-2, IL-7, IL-15 cytokines [34] | Enhances cell susceptibility to transduction/transfection; improves viability and expansion post-editing [34] |
| Editing Validation Tools | T7E1 assay; ICE Analysis; NGS platforms [7] [51] | Quantification of indel formation and editing efficiency; essential for protocol optimization and QC [51] |
Optimizing transfection efficiency in difficult immune cell lines requires a systematic approach that addresses both biological barriers and technical parameters. Through the implementation of optimized electroporation protocols, careful gRNA design, and rigorous quality control measures, researchers can achieve efficient CRISPR-Cas9 mediated SOX9 knockout in even the most challenging immune cell models. The strategies outlined in this application note provide a roadmap for developing robust, reproducible genome editing workflows that will advance both basic research and therapeutic applications in immune cell engineering.
As the field continues to evolve, emerging technologies such as novel electroporation platforms, advanced vector engineering, and improved bioinformatic tools will further enhance our ability to manipulate immune cells for research and therapeutic purposes. By adhering to the principles of careful optimization, appropriate controls, and comprehensive validation, researchers can overcome the challenges of low efficiency transfection and unlock the full potential of CRISPR-based genome editing in immune cell models.
The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR)-Cas9 system has revolutionized genome editing by enabling precise modification of target genes or transcripts, with significant applications in functional genomics and therapeutic development [52] [53]. However, a substantial challenge impeding its clinical translation is CRISPR off-target editing—the non-specific activity of the Cas nuclease at sites other than the intended target, causing undesirable or unexpected effects on the genome [54]. This genotoxicity concern is particularly critical in therapeutic contexts where off-target edits in oncogenes or tumor suppressor genes could have life-threatening consequences [54]. The wild-type Cas9 from Streptococcus pyogenes (SpCas9) can tolerate between three and five base pair mismatches between the guide RNA (gRNA) and target DNA, meaning it can potentially create double-stranded breaks at multiple genomic sites bearing similarity to the intended target [54]. Within the specific context of SOX9 knockout research in immune cell models, precise editing is paramount, as off-target effects could confound the interpretation of SOX9's complex, dual role in immunobiology [1]. This Application Note provides a detailed framework of strategies and protocols to mitigate off-target risks through optimized gRNA design and the use of high-fidelity Cas9 variants.
gRNA Design Strategies for Minimizing Off-Target Effects
The initial and most crucial step in minimizing off-target effects is the careful design and selection of gRNAs. Optimal gRNA design focuses on maximizing on-target efficiency while minimizing potential off-target activity through computational prediction and specific sequence characteristics.
Computational Design and Selection
Begin gRNA design by using specialized software to rank all possible gRNAs for your target site based on their predicted on-target to off-target activity ratio [54]. Tools such as CRISPOR employ algorithms that evaluate multiple factors and provide a score or ranking; high-ranking gRNAs will have high predicted on-target activity and a lower risk of off-target editing [54]. It is considered best practice to select several of the top-ranking gRNAs for empirical testing, as the top-ranked guide in silico may not yield the best results in a biological model [54].
Table 1: Key Considerations for Optimal gRNA Design
| Design Factor | Optimal Characteristic | Rationale | Tool/Tool Function |
|---|---|---|---|
| Specificity | High on-target/off-target activity ratio | Minimizes binding at similar, non-target sites | CRISPOR ranking algorithms |
| GC Content | ~40-60% | Stabilizes DNA:RNA duplex; increases on-target efficiency [54] | Sequence composition analysis |
| gRNA Length | 20 nucleotides or less | Reduces risk of off-target activity [54] | Customizable design parameters |
| Chemical Modifications | 2'-O-methyl analogs (2'-O-Me), 3' phosphorothioate bonds (PS) | Reduces off-target edits, increases on-target efficiency [54] | Specified during synthetic gRNA order |
gRNA Sequence and Modification
Beyond computational selection, the physical and chemical properties of the gRNA itself are critical. Guides with higher GC content in their targeting sequence stabilize the DNA:RNA duplex when the guide binds to the target, which increases on-target editing efficiency and reduces off-target binding [54]. Furthermore, shorter gRNAs of 20 nucleotides or less have been demonstrated to lower the risk of off-target activity [54]. For the highest level of specificity, particularly in clinically-oriented research, employing gRNAs with chemical modifications is a powerful strategy. The addition of 2'-O-methyl analogs (2'-O-Me) and 3' phosphorothioate bonds (PS) to synthetic gRNAs can significantly reduce off-target edits while simultaneously improving efficiency at the target site [54].
High-Fidelity Cas9 Variants and Engineered Nucleases
Beyond gRNA optimization, the choice of the nuclease itself is a primary determinant of editing fidelity. While wild-type SpCas9 has a reasonable risk of off-target editing, numerous engineered variants and alternative nucleases have been developed to address this limitation.
High-Fidelity Cas9 Variants
High-fidelity Cas9 variants represent a significant advancement for applications requiring minimal off-target effects. These engineered proteins, such as HF1 (High-Fidelity 1), incorporate a series of rationally designed mutations that reduce non-specific DNA binding, significantly improving the safety profile of the editor [55] [54]. It is crucial to note, however, that this improvement often comes at the cost of reduced on-target editing efficiency, which can limit the broader application of some high-fidelity editors in therapeutic contexts [55]. This efficacy-safety trade-off remains a critical barrier for safe and effective in vivo genome editing. High-fidelity nucleases are specifically designed to have reduced off-target cleavage, but this does not always equate to reduced off-target DNA binding. For instance, if using a high-fidelity catalytically dead Cas9 (dCas9) for transcriptional regulation (CRISPRi) or epigenetic editing, the likelihood of off-target binding and subsequent effects may not be reduced [54].
Alternative Nucleases and Editing Systems
A wide array of alternative Cas nucleases is now available, including Cas12 and Cas13, which have different off-target profiles compared to SpCas9 [54]. Furthermore, CRISPR-derived technologies that do not create double-strand breaks (DSBs) can inherently reduce the likelihood of off-target mutations. Base editing and prime editing can utilize catalytically dead Cas9 (dCas9) to bind DNA without cutting it, or a Cas9 nickase (nCas9) to create single-stranded breaks, thereby minimizing undesired indels [54] [56]. A nickase-based system can employ a dual-guide approach to produce a similar effect to a DSB while substantially reducing the chance of off-target editing [54].
Table 2: Comparison of CRISPR Systems for Mitigating Off-Target Effects
| CRISPR System | Mechanism | Key Advantage for Off-Target Reduction | Consideration for SOX9 Knockout |
|---|---|---|---|
| Wild-type SpCas9 | Creates DSBs | Benchmark for efficiency | High off-target risk confounds immune phenotype analysis [54] |
| High-Fidelity Cas9 (e.g., HF1) | Engineered mutations reduce non-specific DNA binding | Significantly lower off-target cleavage [55] [54] | Potential trade-off with on-target efficiency [55] |
| Cas9 Nickase (nCas9) | Creates single-strand breaks; requires paired gRNAs | Dramatically reduced off-target indels [54] | Requires two target sites; higher design complexity |
| dead Cas9 (dCas9) - CRISPRi | Binds DNA without cutting; represses transcription | No DSBs = fewer genotoxic off-targets [6] [56] | Enables reversible SOX9 knockdown rather than knockout |
| Base Editor (e.g., ABE, CBE) | nCas9 fused to deaminase; direct base conversion | DSB-independent; lower indel rates [55] | Requires suitable PAM and target base for SOX9 disruption |
| AI-Guided Cas9 (e.g., AncBE4max-AI-8.3) | AI-predicted mutations enhance Cas9 performance | 2-3-fold increase in average editing efficiency [55] | Represents next-generation variant with high fidelity & efficiency |
Recent innovations leverage artificial intelligence to engineer superior Cas9 variants. For instance, the AI-designed variant AncBE4max-AI-8.3, which incorporates eight point mutations, achieves a 2-3-fold increase in average editing efficiency compared to its parent construct [55]. This demonstrates the potential of AI-guided protein engineering to develop "one-size-fits-all" solutions that enhance the performance of diverse gene-editing tools without compromising specificity [55].
Experimental Protocol for SOX9 Knockout with Off-Target Mitigation
This protocol outlines the steps for targeting SOX9 in immune cell models, incorporating the strategies detailed above to minimize off-target effects.
gRNA Design and Preparation (Weeks 1-2)
- Target Identification: Identify the specific exon or regulatory region of the SOX9 gene to target. Consider the functional domains of SOX9, such as the HMG box or transcriptional activation domains (TAM, TAC), to maximize knockout impact [1].
- In Silico gRNA Design:
- Use a design tool like CRISPOR to generate a list of potential gRNAs targeting the selected SOX9 sequence.
- Input the genomic sequence around the target site. The tool will output a list of gRNAs with their predicted efficiency and off-target scores.
- Selection Criteria: Prioritize gRNAs with a high specificity score (indicating a low number of predicted off-target sites) and a GC content between 40% and 60%.
- gRNA Procurement: Select the top 3-5 ranked gRNAs for empirical testing. For enhanced performance, procure synthetic gRNAs with chemical modifications (e.g., 2'-O-Me and PS bonds) [54].
CRISPR Delivery and Cell Selection (Weeks 3-5)
- Nuclease Selection: Based on the requirement for fidelity versus efficiency, choose an appropriate nuclease. For a standard knockout with high fidelity, a high-fidelity Cas9 variant like HF1 is recommended. For the highest specificity with minimal DSBs, a base editor system is preferable.
- Delivery into Immune Cells: Deliver the CRISPR components (selected nuclease and gRNA) into your target immune cells (e.g., primary T cells, macrophage cell lines) using an appropriate method (electroporation for primary cells, lentiviral transduction for hard-to-transfect lines).
- Control: Include a non-targeting gRNA control to account for background effects.
- Cell Culture and Expansion: Culture the transfected cells for at least 72-96 hours to allow for gene editing and degradation of the edited protein.
Analysis and Validation of Editing (Weeks 5-6)
- Genomic DNA Extraction: Harvest cells and extract genomic DNA using a standard kit.
- On-Target Efficiency Analysis:
- Design PCR primers flanking the SOX9 target site and perform PCR amplification.
- Sanger sequence the PCR product and analyze the traces using the Inference of CRISPR Edits (ICE) tool [57] [54].
- ICE will calculate the overall editing efficiency (% indels) and the knockout score (percentage of sequences predicted to cause a frameshift) [57].
- Off-Target Analysis:
- From the initial CRISPOR output, compile a list of the top ~10-20 predicted off-target sites for the gRNA used.
- Design PCR primers for these candidate sites and perform targeted amplicon sequencing via next-generation sequencing (NGS) to quantify indel frequencies at these loci [54]. Sites with indel frequencies significantly above background (non-targeting control) indicate true off-target activity.
- Functional Validation:
- Confirm SOX9 knockout at the protein level via western blotting or flow cytometry.
- Perform functional assays relevant to the immune cell model. Given SOX9's role in immunobiology, this may include assays for cytokine production, cell differentiation, or chemotaxis to contextualize the knockout phenotype [1].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Tools for CRISPR-Cas9 SOX9 Knockout
| Reagent/Tool | Function/Purpose | Example/Format |
|---|---|---|
| gRNA Design Tool | Predicts on-target efficiency and potential off-target sites to guide gRNA selection. | CRISPOR [54] |
| High-Fidelity Cas9 Nuclease | Engineered Cas9 protein with reduced off-target cleavage activity for more specific editing. | HF1 Cas9 [55] [54] |
| Chemically Modified Synthetic gRNA | Enhanced gRNA stability and specificity; reduces off-target edits. | 2'-O-Me/PS modified sgRNA [54] |
| Analysis Software (ICE) | Analyzes Sanger sequencing data from edited pools to determine editing efficiency and knockout score. | EditCo's ICE Tool [57] |
| Off-Target Prediction & Detection Assay | Identifies and quantifies potential off-target editing sites. | GUIDE-seq, CIRCLE-seq [54] [58] |
| AI-Guided Cas9 Variant | High-performance Cas9 with mutations predicted by AI to boost editing efficiency. | AncBE4max-AI-8.3 [55] |
| Transfer Learning Framework | A computational method to improve off-target prediction accuracy, especially with limited data. | Similarity-based pre-evaluation & model fine-tuning [58] |
The successful application of CRISPR-Cas9 for SOX9 knockout in immune cell models hinges on a multi-faceted strategy that prioritizes specificity from experimental conception through validation. By integrating computational gRNA design, the selection of high-fidelity or novel AI-engineered nucleases, rigorous analytical methods like ICE, and comprehensive off-target profiling, researchers can significantly mitigate the risks associated with off-target editing. This approach ensures that observed phenotypic changes in immune function can be confidently attributed to the targeted perturbation of SOX9, a transcription factor with a critical and complex role in immunity [1]. As the field progresses, the adoption of these combined strategies will be essential for generating robust, reproducible, and clinically relevant data in CRISPR-based immunological research.
In the field of genetic engineering, particularly for CRISPR-Cas9-mediated gene knockout studies targeting key developmental regulators like SOX9, ensuring clonal purity is not merely a technical step but a fundamental requirement for data integrity. The generation of immune cell models with defined genetic backgrounds necessitates the derivation of populations from a single progenitor cell, guaranteeing that the resulting population is genetically uniform and that observed phenotypes can be confidently attributed to the intended modification [21]. The process of single-cell isolation and expansion, however, presents significant challenges, including cellular stress during isolation, low viability post-isolation, and the phenotypic drift that can occur during the lengthy expansion phase [7] [59]. This application note provides detailed, actionable protocols for achieving high clonal purity, framed within the context of CRISPR-Cas9 SOX9 knockout research in immune cell models, to support researchers and drug development professionals in their functional genomics and therapeutic development work.
Single-Cell Isolation Methodologies
Selecting the appropriate isolation technique is critical and depends on factors such as cell type sensitivity, available equipment, and required throughput. The following section compares the most common methods and provides a detailed protocol for each.
Table 1: Comparison of Single-Cell Isolation Methods
| Method | Principle | Throughput | Cell Viability & Stress | Sample Input | Equipment Needs | Best Suited For |
|---|---|---|---|---|---|---|
| Fluorescence-Activated Cell Sorting (FACS) | Electric charge and fluorescence-based sorting [59]. | High (thousands of cells/sec) [59]. | High stress; can reduce viability of sensitive cells [59]. | Requires large sample input [59]. | Expensive, specialized flow cytometer [59]. | High-throughput sorting based on complex surface markers. |
| Limiting Dilution Cloning (LDC) | Serial dilution for random single-cell distribution in wells [60] [59]. | Low, slow process [59]. | Low stress but highly inefficient [60] [59]. | Minimal input, but low efficiency [59]. | Basic tissue culture equipment [59]. | Labs without access to specialized sorting equipment. |
| Microfluidic Platforms (e.g., CellGem) | Gravity-based microwell capture for single-cell isolation [59]. | High, processes many cells efficiently [59]. | Gentle process, preserves viability of sensitive cells [59]. | Works with small, rare samples [59]. | Simple, user-friendly device [59]. | Sensitive primary cells (e.g., immune cells, chondrocytes) and precious samples. |
Protocol 1: Limiting Dilution Cloning (LDC)
This protocol is adapted from established guidelines for isolating single-cell clones after CRISPR-Cas9 editing [60].
Experimental Workflow:
Calculate Cell Dilution:
- Based on the editing efficiency and estimated cell viability, calculate the number of single clones needed to obtain a desired knockout clonal cell line [60]. For example, for a homozygous KO with 50% cleavage efficiency, the probability of both alleles being knocked out in any cell is 25%. Factoring in the probability of a frameshift-inducing indel (~2/3), the chance of a homozygous KO per cell is approximately 11% [60].
- To plate at a density of 0.8 cells per well, resuspend the transfected or transduced cells at a density of 8 cells/mL in complete growth medium [60].
Plate Cells:
Expand Clones:
- Incubate the plates in a 37°C, 5% CO2 incubator.
- Visually scan the plates for single-cell colonies as soon as small aggregates are visible under a 4X microscope (typically after the first week, depending on the cell line). Continue incubation for an additional 2–3 weeks to expand the clonal populations [60].
Protocol 2: Single-Cell Isolation by FACS
This protocol provides a standard procedure for sorting single cells using a flow cytometer [60].
Experimental Workflow:
Prepare Single-Cell Suspension:
- Wash the CRISPR-edited cell population with PBS.
- Add an appropriate volume of trypsin or TrypLE cell dissociation reagent and incubate at 37°C for 2–5 minutes.
- Neutralize the dissociation reagent with complete growth medium. Pipette the cells up and down several times to ensure a single-cell suspension with no clumps [60].
- Centrifuge the cells at 300 × g for 5 minutes to pellet, then aspirate the supernatant.
Stain and Filter Cells:
- Resuspend 1 × 10^6 cells in 1 mL of ice-cold FACS buffer (e.g., PBS with 1-2% FBS).
- Add a viability dye, such as propidium iodide (PI), to a final concentration of 1 µg/mL.
- Filter the cell suspension through a suitable cell strainer (e.g., 35-70 µm) to remove any remaining aggregates before sorting [60].
Sort Single Cells:
- Using a flow cytometer with single-cell sorting capability, sort the PI-negative (viable), single cells based on desired light-scattering properties or fluorescence markers.
- Sort one cell per well into a 96-well plate containing 100 µL of pre-warmed complete growth medium, which may include 1X antibiotics [60].
Expand Clones:
- Incubate the plates in a 37°C, 5% CO2 incubator.
- Scan the plates for single-cell colonies after 7-14 days using a microscope. Perform image analysis to confirm that colonies are derived from single cells.
- Continue incubation for an additional 2–3 weeks to expand clonal populations for characterization [60].
Protocol 3: Microfluidic Isolation (CellGem System)
This protocol outlines the use of the CellGem platform, a gentle microfluidic alternative for sensitive cells like primary immune cells [59].
Experimental Workflow:
Prepare Cell Suspension:
- Use cells in the logarithmic (log) phase of growth for high viability.
- Prepare a single-cell suspension at a concentration of approximately 1 x 10^6 cells/mL. Filter the suspension with a cell strainer to remove clumps and ensure a monodisperse population [59].
Load CellGem Chip:
- Load the prepared cell suspension into the CellGem device.
- Allow the cells to settle by gravity for at least 3 minutes into the capture wells. Rushing this step reduces capture efficiency.
- Select a capture well size appropriate for the diameter of your target immune cells [59].
Transfer and Culture:
- After cell capture, flip the device to transfer the isolated cells from the capture wells into adjacent culture wells, again using gravity.
- Once in the culture wells, each cell can grow and divide to form a single-cell-derived colony.
- These colonies can later be transferred to larger culture vessels for further expansion [59].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Clonal Isolation and Validation
| Item | Function/Application | Example Specifications/Notes |
|---|---|---|
| CRISPR-Cas9 RNP Complex | The gene editing machinery. Complexing Cas9 protein with sgRNA as a Ribonucleoprotein (RNP) increases editing efficiency and reduces off-target effects [7]. | Ideal for primary cells; cleared rapidly from cells post-editing [7]. |
| Cell Dissociation Reagent | Generating a high-viability single-cell suspension for sorting or dilution. | TrypLE or similar enzymes are gentle alternatives to trypsin [60]. |
| FACS Buffer | Maintaining cell viability and preventing clumping during fluorescence-activated cell sorting. | PBS supplemented with 1-2% Fetal Bovine Serum (FBS) or BSA. Keep ice-cold [60]. |
| Viability Stain | Distinguishing live from dead cells during FACS to ensure only viable clones are isolated. | Propidium Iodide (PI) at 1 µg/mL final concentration [60]. |
| 96-well Tissue Culture Plates | The vessel for single-cell expansion and clonal outgrowth. | Tissue culture-treated, sterile plates. |
| Growth Medium with Supplements | Supporting the survival and proliferation of single cells, which is more demanding than bulk culture. | Often requires additional supplements like FGF2 for primary cells [7]. |
Validation of Clonal Purity and SOX9 Knockout
Following isolation and expansion, rigorous validation is required to confirm both clonal origin and successful genetic modification.
Experimental Protocol for Genotypic Validation:
Genomic DNA Extraction and PCR:
- Extract genomic DNA from a portion of the expanded clonal cells using a commercial kit.
- Design PCR primers flanking the CRISPR-Cas9 target site within the SOX9 gene. Perform PCR amplification using this genomic DNA as a template.
Sequence Analysis:
- Purify the PCR products and submit them for Sanger sequencing.
- Analyze the sequencing chromatograms for the presence of indels (insertions or deletions) at the target site. Tools like TIDE (Tracking of Indels by Decomposition) or ICE (Inference of CRISPR Edits) can be used to quantify editing efficiency in a mixed population, but a pure clonal sequence should show a clean, unambiguous sequence trace indicative of a bi-allelic edit or a double peak for a heterozygous edit [60].
Phenotypic Validation:
- Western Blotting: Confirm the absence of SOX9 protein in the knockout clones. Prepare protein lysates from wild-type and knockout clones and perform Western blotting using a validated anti-SOX9 antibody [7].
- Functional Assays: For immune cell models, downstream functional assays (e.g., differentiation capacity, cytokine secretion profiles, or migration assays) should be performed to characterize the phenotypic consequences of the SOX9 knockout.
Troubleshooting and Concluding Remarks
Achieving clonal purity is a meticulous process. Common challenges and their solutions are summarized below.
Table 3: Troubleshooting Guide for Single-Cell Isolation and Expansion
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| Low Clonal Survival | Cellular stress during isolation; inadequate culture conditions for single cells. | Optimize dissociation protocol; use conditioned medium or ROCK inhibitor to improve single-cell viability [59]. |
| No Clonal Growth | Over-dilution in LDC; excessive pressure during FACS. | Confirm cell viability and counting accuracy; use gentler sorting methods like microfluidics for sensitive cells [59]. |
| Mixed Genotypes in a "Clone" | Wells started with more than one cell; cell splitting or aggregation during culture. | Use microscopic verification post-isolation (e.g., with CellGem); ensure a true single-cell suspension before sorting [59]. |
| Low Editing Efficiency in Clones | Inefficient CRISPR delivery or cutting in the parent pool. | Prior to isolation, optimize RNP delivery (e.g., via electroporation) and confirm high editing efficiency in the pooled population [7]. |
In conclusion, the successful generation of a clonally pure SOX9 knockout immune cell model hinges on a well-optimized workflow from CRISPR delivery to single-cell isolation and rigorous validation. The choice of isolation method should be tailored to the specific cell model and available resources. By adhering to these detailed protocols and validation strategies, researchers can ensure the genetic fidelity of their models, thereby producing reliable and interpretable data for both basic research and therapeutic development.
The precision of CRISPR-Cas9 genome editing has revolutionized genetic research, yet significant challenges persist when targeting genes within complex genomic landscapes. The presence of multi-copy genes and highly homologous pseudogenes can confound even the most carefully designed editing strategies, leading to unintended off-target effects and compromised experimental integrity. This challenge is particularly acute in immune cell research, where accurate genetic models are essential for elucidating gene function and developing therapeutic interventions.
Within the context of SOX9 knockout studies in immune cell models, navigating this complexity becomes paramount. SOX9, a transcription factor with critical roles in immunity, tumor progression, and differentiation, presents unique challenges due to its regulatory complexity and potential genomic parallels [1]. This application note provides detailed methodologies and strategic frameworks for addressing multi-copy genes and pseudogenes, enabling more reliable CRISPR-Cas9 outcomes in immunology research.
Understanding the Challenge: Pseudogenes and Multi-Copy Genes
Pseudogene-Mediated Gene Conversion in CRISPR Editing
Pseudogenes, while historically considered genomic fossils, present active obstacles to precise genome editing through their sequence homology with functional genes. A documented case of pseudogene-directed homology repair demonstrates the tangible risk these sequences pose. When researchers attempted CRISPR-Cas9-mediated excision of exon 2 in the CD33 gene in a human monocyte cell line, they isolated unexpected clones that retained the exon but had lost antibody binding affinity [61].
Subsequent sequencing revealed these cells had undergone gene conversion from the nearby SIGLEC22P pseudogene, located 13.5 kb away from CD33. Despite sharing only approximately 87% sequence identity over 1,800 bp, the pseudogene served as an endogenous homology-directed repair (HDR) template during DNA repair, introducing three missense mutations (p.N20K, p.F21I, and p.W22R) that altered the resulting protein [61]. This case underscores that pseudogenes with even modest homology can participate in repair processes, yielding unanticipated editing outcomes.
SOX9 Genomic Context and Immunological Relevance
In immune cell research, SOX9 presents particular challenges and opportunities. As a master transcriptional regulator, SOX9 participates in diverse immune processes, including T cell development and macrophage function [1]. It exhibits context-dependent dual functions—acting as both an activator and repressor across diverse immune cell types [1]. Successful editing of SOX9 in immune models requires careful consideration of its genomic environment, including potential homologous sequences that might confound targeting strategies.
The therapeutic targeting of SOX9 is complicated by its "double-edged sword" nature in immunology. It can promote immune escape in tumors yet also contributes to tissue regeneration and repair [1]. This functional complexity necessitates precise editing approaches that can isolate specific functions without collateral genomic disruption.
Detection and Analysis Methods
Advanced Off-Target Detection Strategies
Comprehensive identification of potential off-target sites is a critical first step in navigating genomic complexity. The table below summarizes key methodologies for detecting off-target editing events, ranging from biased prediction-based approaches to unbiased genome-wide screening:
Table 1: Methods for Detecting CRISPR-Cas9 Off-Target Activity
| Method | Principle | Advantages | Limitations |
|---|---|---|---|
| GUIDE-seq [62] | Captures double-strand breaks with double-stranded oligonucleotides followed by sequencing | Genome-wide, unbiased identification; straightforward wet-lab protocol | Requires efficient dsODN delivery; potential toxicity in some cell types |
| BLESS [62] | Direct in situ breaks labeling, enrichment on streptavidin, and NGS | No exogenous bait introduced; applicable to tissue samples | Sensitive to fixation timing; requires large cell numbers |
| Digenome-seq [62] | In vitro nuclease-digested whole genome sequencing | Sensitive, genome-wide profiling; cell-free system | Does not account for cellular context or chromatin environment |
| Targeted Deep Sequencing [62] | Amplification and sequencing of computationally predicted off-target sites | Quantitative and sensitive for known sites | Biased toward predicted sites; may miss unexpected off-target events |
Quantitative Analysis of Editing Efficiency
Rigorous quantification of editing outcomes is essential for evaluating strategy success. The following table outlines key quantitative metrics and methods for assessing CRISPR editing efficiency and specificity in complex genomic regions:
Table 2: Quantitative Assessment Methods for CRISPR Editing
| Parameter | Measurement Approach | Acceptance Criteria |
|---|---|---|
| On-target efficiency | Amplicon sequencing with indel quantification | Typically >70% indel rate for knockout studies |
| Off-target editing | GUIDE-seq or targeted sequencing of predicted sites | No significant editing at top predicted off-target sites |
| Pseudogene conversion events | Allele-specific PCR and Sanger sequencing | No detectable transfer from homologous sequences |
| Karyotypic integrity | Karyotyping or CNV analysis | Normal ploidy without chromosomal abnormalities |
For SOX9 editing validation, additional functional assays should be employed, including qPCR for SOX9 target genes, flow cytometry for immune cell markers, and in vitro differentiation assays to confirm functional knockout without compensatory effects from homologous genes [1] [6].
Experimental Protocols
Comprehensive gRNA Design and Validation Workflow
The following diagram illustrates the recommended workflow for designing and validating gRNAs targeting genomically complex regions like SOX9:
Protocol: gRNA Design for Genomically Complex Regions
Materials:
- Genomic databases: ENSEMBL, UCSC Genome Browser
- gRNA design tools: CHOPCHOP, CRISPRscan, CRISPick
- Homology search tools: BLAST, UCSC In-Silico PCR
- Cell line: Appropriate immune cell model (e.g., THP-1, U937, or primary cells)
Procedure:
- Target Identification: Identify SOX9 exonic regions critical for function, avoiding areas with high homology to other sequences.
- In Silico Design:
- Input SOX9 target sequences into multiple gRNA design tools
- Apply stringent specificity filters (minimize off-target predictions)
- Cross-reference with pseudogene databases (e.g., GENCODE pseudogene annotations)
- Homology Assessment:
- Perform BLAST analysis of candidate gRNAs against the reference genome
- Flag gRNAs with significant homology (≥12bp contiguous identity) to non-target loci
- Check for homology with SOX family genes (SOX8, SOX10) which share conserved HMG-box domains [1]
- Specificity Scoring:
- Rank gRNAs by specificity scores from multiple algorithms
- Prioritize gRNAs with minimal predicted off-target sites
- Select 3-5 candidate gRNAs for experimental validation
- Experimental Validation:
- Clone gRNAs into appropriate CRISPR vector
- Transfect immune cells and culture for 72 hours
- Extract genomic DNA and assess editing efficiency via T7E1 assay or sequencing
- Quantify indel percentages for each gRNA
Strategy for Avoiding Pseudogene Interference
The following protocol outlines specific steps to minimize pseudogene-mediated editing artifacts, based on the documented case of SIGLEC22P interference with CD33 editing [61]:
Protocol: Preventing Pseudogene Interference
Materials:
- CRISPR reagents: High-fidelity Cas9 (eSpCas9(1.1) or SpCas9-HF1) [62]
- Sequencing primers: Flanking target site and potential pseudogene regions
- Control templates: Wild-type and pseudogene sequence plasmids
Procedure:
- Pseudogene Identification:
- Annotate all pseudogenes with homology to SOX9 using pseudogene databases
- Calculate percentage identity and length of homologous regions
- Note genomic locations and relative orientation to SOX9
gRNA Exclusion Zone Definition:
- Exclude gRNAs targeting regions with >80% homology to pseudogenes
- Avoid gRNAs with 12+ bp contiguous perfect matches to pseudogenes
- Design gRNAs that span non-homologous regions or incorporate mismatches to pseudogenes
Experimental Controls:
- Include positive control for pseudogene amplification in PCR assays
- Design allele-specific PCR primers to distinguish between target and pseudogene
- Sequence both target and pseudogene loci in edited clones
Analysis for Gene Conversion:
- Screen edited clones for unexpected sequence patterns
- Compare edited sequence with both target and pseudogene references
- Test for loss of specific epitopes (as in CD33/P67.6 example) [61]
CRISPR Workflow for SOX9 Editing in Immune Cells
The diagram below outlines the complete experimental workflow for SOX9 knockout in immune cell models, incorporating specificity enhancements:
Protocol: SOX9 Knockout in Immune Cell Models
Materials:
- Immune cells: U937 (human monocyte), THP-1 (monocytic), or primary human T-cells
- CRISPR components: High-fidelity Cas9, validated SOX9 gRNAs, delivery system
- Culture reagents: Appropriate media, cytokines, differentiation agents
- Analysis tools: Flow cytometry antibodies, qPCR primers, functional assay reagents
Procedure:
- gRNA Preparation:
- Use gRNAs validated through Protocol 4.1
- Clone into appropriate high-fidelity Cas9 expression vector
- Prepare lentiviral particles or ribonucleoprotein complexes for delivery
Cell Transduction:
- For suspension immune cells, use electroporation for RNP delivery
- For difficult-to-transfect cells, use lentiviral transduction with appropriate biosafety
- Include control cells receiving Cas9 only or non-targeting gRNA
Selection and Cloning:
- Apply appropriate selection (antibiotics, FACS sorting) if using vector-based system
- Isolate single cells by limiting dilution or FACS into 96-well plates
- Expand clones for 3-4 weeks with appropriate conditioning
Genotypic Validation:
- Screen clones for SOX9 editing by PCR of target region
- Sequence top candidates to characterize specific indel patterns
- Identify clones with biallelic frameshift mutations
Off-Target Assessment:
- Perform GUIDE-seq or targeted sequencing of predicted off-target sites
- Confirm absence of editing at pseudogene loci
- Validate karyotypic integrity
Phenotypic Characterization:
- Assess SOX9 protein loss by Western blot or flow cytometry
- Evaluate downstream effects on SOX9 target genes
- Perform immune functional assays relevant to research questions
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Complex CRISPR Editing
| Reagent Category | Specific Examples | Function & Application |
|---|---|---|
| High-Fidelity Cas9 Variants | eSpCas9(1.1), SpCas9-HF1, HypaCas9 [62] | Reduce off-target editing while maintaining on-target efficiency |
| Computational Design Tools | CHOPCHOP, CRISPick, CRISPRscan | Identify specific gRNAs with minimal off-target potential |
| Off-Target Detection Kits | GUIDE-seq, BLESS, Digenome-seq kits [62] | Genome-wide identification of off-target editing events |
| Immune Cell Delivery Systems | Neon Transfection System, Lonza Nucleofector | Efficient RNP delivery to difficult-to-transfect immune cells |
| Specificity-Enhanced gRNA Scaffolds | Modified sgRNAs with truncated spacers [62] | Improved specificity through reduced non-specific interactions |
| Pseudogene-Specific PCR Primers | Custom-designed allele-discriminating primers | Distinguish between target gene and pseudogene sequences |
| Immune Cell Characterization Panels | Flow cytometry antibodies for T-cell, macrophage markers | Validate immune phenotype after SOX9 editing |
The growing sophistication of CRISPR-based research demands parallel advances in managing genomic complexity. The strategies outlined here provide a framework for addressing the specific challenges posed by multi-copy genes and pseudogenes, with particular application to SOX9 research in immune models. The documented case of pseudogene-mediated gene conversion in CD33 editing serves as a cautionary example of the unexpected pathways through which homology can compromise editing precision [61].
For SOX9 research specifically, the dual roles of this transcription factor in immunity underscore the importance of precise editing. SOX9's involvement in both T cell development and macrophage function means that incomplete or inaccurate editing could lead to misinterpretation of immune phenotypes [1]. The protocols described here emphasize rigorous validation to ensure that observed effects truly stem from SOX9 manipulation rather than confounding genomic artifacts.
As CRISPR technology continues to evolve, emerging approaches like base editing and prime editing may offer additional pathways for navigating genomic complexity, potentially providing alternative strategies for discriminating between highly homologous sequences. Similarly, advances in bioinformatic prediction of problematic genomic regions will further enhance our ability to design optimal editing strategies from the outset.
The integration of careful gRNA design, appropriate Cas9 variants, and comprehensive validation represents the current gold standard for managing multi-copy genes and pseudogenes in CRISPR research. By adopting these practices, researchers can significantly enhance the reliability of their findings in SOX9 immune biology and other genetically complex systems.
Rigorous Validation of SOX9 Knockout: From DNA to Phenotype
Within the framework of CRISPR-Cas9 SOX9 knockout studies in immune cell models, confirming the presence and spectrum of induced insertions and deletions (indels) is a critical step in validating experimental outcomes. The selection of an appropriate sequencing method directly influences the accuracy, depth, and scalability of this genomic validation. Sanger sequencing, coupled with computational decomposition algorithms, offers a cost-effective and rapid approach for initial efficiency estimates, while Next-Generation Sequencing (NGS) provides a comprehensive, high-resolution view of the entire editing landscape [63] [64]. This application note details protocols and comparative metrics for both methods, contextualized for researchers engineering immune cell models via SOX9 knockout.
The following workflow diagram outlines the core decision-making process for selecting and implementing these validation strategies.
Comparative Analysis of Sanger Sequencing and NGS
The choice between Sanger sequencing and NGS depends on the required resolution, throughput, and project resources. Sanger sequencing, analyzed with tools like ICE or TIDE, is sufficient for rapid assessment of editing efficiency in bulk cell populations. In contrast, NGS is indispensable for detecting complex heterogeneous edits, precise sequence reconstruction, and identifying rare editing events in a mixed cell population, which is crucial for characterizing polyclonal immune cell lines [63] [65].
Table 1: Method Selection Guide for Indel Confirmation
| Parameter | Sanger Sequencing + Decomposition Analysis | Next-Generation Sequencing (NGS) |
|---|---|---|
| Best Use Case | Rapid initial screening and bulk efficiency estimation [66] | Deep characterization of complex indel spectra and rare variants [63] [65] |
| Typical Workflow Cost | Low (~100-fold reduction vs. NGS) [66] | High |
| Handling of Complex Indels | Variable accuracy; performance decreases with complexity [63] | High accuracy and resolution [63] |
| Throughput | Low to medium | High to very high |
| Key Metric | Indel Percentage / Knockout Score (from ICE, TIDE) [66] | Variant Allele Frequency (VAF) & precise sequence data [65] |
| Quantitative Nature | Semi-quantitative (inference-based) | Fully quantitative (direct counting) |
| Limitations | Limited detection of rare (<5%) or highly complex indels [63] | Higher cost, longer turnaround, complex data analysis [65] |
Table 2: Performance Profile of Sanger Sequence Deconvolution Tools
| Tool | Reported Key Feature | Indel Frequency Accuracy | Performance Notes |
|---|---|---|---|
| DECODR | Deconvolution of Complex DNA Repair [63] | High (most accurate for majority of samples) [63] | Most useful for identifying specific indel sequences [63] |
| ICE (Inference of CRISPR Edits) | User-friendly, batch analysis of hundreds of samples [66] | Reasonable accuracy for simple indels [63] | Provides a Knockout Score (proportion of frameshift indels) [66] |
| TIDE (Tracking of Indels by Decomposition) | Rapid analysis of editing efficiency and indel distribution [63] [67] | Reasonable accuracy for simple indels [63] | Values become more variable with complex indels [63] |
| SeqScreener | Online tool from Thermo Fisher Scientific [63] | Reasonable accuracy for simple indels [63] | Performance similar to TIDE and ICE for simple edits [63] |
Sanger Sequencing Protocol for Initial Efficiency Assessment
This protocol is designed for the rapid validation of CRISPR-Cas9 editing following SOX9 targeting in immune cells.
Genomic DNA (gDNA) Extraction and Target Amplification
- Extract gDNA: Harvest edited immune cells and extract high-quality genomic DNA using a standard silica-column or magnetic-bead based kit. Ensure DNA integrity by spectrophotometry (A260/280 ratio ~1.8) and quantify using a fluorometric method.
- Design PCR Primers: Design primers to amplify a 300-500 bp region flanking the SOX9 gRNA target site. The amplicon should be centered on the expected cut site, typically 3 bases upstream of the Protospacer Adjacent Motif (PAM) sequence.
- Amplify Target Locus: Perform PCR amplification of the target locus from the bulk edited cell population using a high-fidelity DNA polymerase. Include a negative control (wild-type, unedited cells) and a positive control if available.
- Typical Reaction Setup:
- gDNA: 50-100 ng
- High-fidelity PCR Master Mix: 1X
- Forward Primer (10 µM): 0.5 µL
- Reverse Primer (10 µM): 0.5 µL
- Nuclease-free water to 50 µL
- Thermocycling Conditions:
- Initial Denaturation: 98°C for 30 s
- 30-35 cycles of: 98°C for 10 s, 60°C for 30 s, 72°C for 30 s
- Final Extension: 72°C for 2 min
- Typical Reaction Setup:
- Purify PCR Products: Clean the amplified PCR products using a PCR purification kit to remove primers, enzymes, and salts. Validate amplification and purity by agarose gel electrophoresis.
Sanger Sequencing and Computational Analysis
- Sanger Sequencing: Submit the purified PCR amplicons for Sanger sequencing using one of the PCR primers. It is critical to also sequence the amplicon from the wild-type control sample.
- Analyze with ICE (Recommended Workflow):
- Access the ICE webtool (Synthego).
- Upload the Sanger sequencing chromatogram file (
.ab1) from the edited sample as the "Experimental Sample." - Upload the chromatogram from the wild-type control as the "Control Sample."
- Input the 20-nucleotide gRNA target sequence (excluding the PAM sequence) used for the SOX9 knockout.
- Select the appropriate nuclease (e.g., SpCas9) from the dropdown menu.
- Run the analysis. The tool will decompose the mixed sequencing trace and compare it to the wild-type reference [66].
- Interpret Results:
- Indel Percentage: The primary metric for editing efficiency, representing the percentage of sequences with non-wild-type indels.
- Knockout (KO) Score: The proportion of cells with a frameshift or a large (21+ bp) indel, which is a strong predictor of functional gene knockout [66].
- R² Value: The goodness-of-fit for the decomposition model. A value above 0.9 indicates high confidence in the result, while values below 0.8 suggest the data may be unreliable [66].
- Indel Spectrum: A list of the specific insertions and deletions identified, along with their relative abundances.
NGS Protocol for High-Resolution Indel Characterization
For a complete picture of editing outcomes in a polyclonal SOX9 knockout immune cell population, NGS is the gold standard.
Library Preparation and Sequencing
- Amplify Target Locus: Using the same purified gDNA and PCR primers as in Section 3.1, amplify the target locus. However, the primers must be tagged with Illumina-style adapter overhangs.
- Forward Primer Overhang:
5´-TCGTCGGCAGCGTCAGATGTGTATAAGAGACAG-[Locus-Specific Forward Sequence]-3´ - Reverse Primer Overhang:
5´-GTCTCGTGGGCTCGGAGATGTGTATAAGAGACAG-[Locus-Specific Reverse Sequence]-3´
- Forward Primer Overhang:
- Clean Amplified Products: Purify the PCR products as before.
- Attach Dual Indices and Sequencing Adaptors: In a limited-cycle PCR, attach unique dual indices (barcodes) and full sequencing adapters to each sample using a kit such as the Illumina Nextera XT Index Kit. This allows for multiplexing—pooling multiple samples in a single sequencing run.
- Clean and Pool Libraries: Purify the final indexed libraries and quantify them using a fluorometric method. Combine equimolar amounts of each library into a single pool.
- Sequence: Denature and dilute the pooled library according to the sequencer's specifications and load onto an Illumina sequencer (e.g., MiSeq) for paired-end sequencing (2x150 bp or 2x250 bp is typical). Aim for a minimum of 50,000-100,000 reads per sample to confidently detect low-frequency indels.
Bioinformatic Analysis
- Demultiplexing: The sequencer's software will generate FASTQ files by assigning reads to each sample based on their unique barcodes.
- Quality Control and Trimming: Use tools like FastQC to assess read quality. Trim low-quality bases and adapter sequences with tools like Trimmomatic or Cutadapt.
- Alignment: Map the quality-filtered reads to the reference genome (e.g., GRCh38) or a custom reference sequence containing the wild-type SOX9 target locus using a splice-aware aligner like BWA-MEM or STAR.
- Variant Calling: Identify insertions and deletions around the target site using specialized CRISPR variant callers such as CRISPResso2, amplicon indel analyzer (AIA), or other NGS analysis pipelines [65]. These tools are designed to handle the high indel density typical of CRISPR editing sites.
- Interpret Results:
- Variant Allele Frequency (VAF): For each unique indel, the VAF is calculated as (Number of reads supporting the variant / Total reads at that position) * 100. This provides a direct, quantitative measure of each edit's abundance.
- Indel Spectrum: A comprehensive list of all detected insertion and deletion sequences and their frequencies, allowing for the reconstruction of the precise editing landscape.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Tools for CRISPR Validation
| Item | Function/Application | Example Product/Note |
|---|---|---|
| High-Fidelity DNA Polymerase | Accurate amplification of the target locus from gDNA for both Sanger and NGS. | KOD One PCR Master Mix [63], Q5 Hot Start High-Fidelity Master Mix [67] |
| gRNA & Control Kits | Pre-designed, validated gRNAs for positive control loci to benchmark editing efficiency. | TrueGuide Synthetic gRNA Controls (e.g., human HPRT) [64] |
| Genomic Cleavage Detection (GCD) Kit | Rapid, gel-based method for preliminary estimation of indel formation. | GeneArt Genomic Cleavage Detection Kit [64] |
| Sanger Deconvolution Software | Web-based tools to calculate indel percentages from Sanger traces of bulk PCR products. | ICE (Synthego) [66], TIDE [63] [67], DECODR [63] |
| NGS Amplicon Library Prep Kit | Streamlined workflow for preparing barcoded sequencing libraries from PCR amplicons. | Illumina Nextera XT DNA Library Preparation Kit |
| NGS CRISPR Analysis Software | Bioinformatics tools for precise quantification and characterization of indels from NGS data. | CRISPResso2, Sophia DDM [65] |
A tiered approach to genomic validation is most effective for CRISPR-Cas9 SOX9 knockout projects in immune cells. Initial screening and efficiency calculations with Sanger sequencing and ICE/TIDE analysis provide a fast and cost-effective entry point. For publications or when a deep understanding of the editing profile is required, NGS delivers the necessary resolution and quantitative power to fully characterize the knockout model. The protocols and comparative data outlined herein provide a clear roadmap for researchers to confidently verify their gene editing outcomes.
In the context of CRISPR-Cas9-mediated SOX9 knockout research in immune cell models, transcriptomic validation serves as a critical quality control step that extends far beyond simple DNA sequencing. While CRISPR-Cas9 technology has revolutionized genetic engineering, emerging evidence indicates that conventional validation methods focusing solely on target site DNA sequencing are insufficient for characterizing the full spectrum of transcriptional consequences. Approximately 50% of CRISPR-edited cell lines exhibit unexpected mRNA misregulation or novel protein products despite successful frameshift induction [68]. This application note details comprehensive RNA-sequencing (RNA-seq) protocols specifically designed to validate SOX9 knockout efficiency while simultaneously detecting unintended splicing events and transcriptomic alterations that may confound experimental results in immune cell research.
The SOX9 transcription factor presents particular challenges for CRISPR validation due to its complex regulatory roles in both transcription and alternative splicing processes [69]. Proper validation requires specialized approaches that can distinguish between complete knockout, partial knockdown, and aberrant transcript production that may retain functionality. The protocols outlined herein provide a standardized framework for researchers to authenticate their SOX9 knockout models while identifying potential confounding factors that could impact downstream phenotypic analyses in immunology studies.
The Critical Need for RNA-seq in CRISPR Validation
Limitations of DNA-Centric Validation Approaches
Traditional CRISPR validation methods primarily rely on PCR amplification of the target genomic region followed by Sanger sequencing or next-generation sequencing. While these approaches effectively detect indels at the DNA level, they fail to capture the full transcriptional consequences of CRISPR editing. DNA-based methods cannot identify:
- Unintended splicing alterations caused by disruption of exonic splicing enhancers (ESEs) or silencers [68]
- Alternative translation initiation events that bypass premature termination codons [68]
- Complex rearrangement events such as inter-chromosomal fusions or large deletions [70]
- Nonsense-mediated decay (NMD) escape through transcript variants or inefficient decay mechanisms [68]
These limitations are particularly relevant for SOX9 research, as the gene's complex regulation and essential functions demand rigorous validation approaches.
Prevalence of Unintended Transcriptional Consequences
Multiple studies have demonstrated that unanticipated transcriptional outcomes are common in CRISPR-edited cell lines:
Table 1: Frequency of Unintended Transcriptional Events in CRISPR-Edited Cell Lines
| Event Type | Frequency | Detection Method | Functional Impact |
|---|---|---|---|
| Aberrant protein products | ~30% of cell lines [68] | Western blot with multiple antibodies | Potential neomorphic functions |
| mRNA misregulation | ~50% of cell lines [68] | RT-PCR, RNA-seq | Compromised knockout validity |
| Exon skipping | Case studies [68] | Transcript-specific analysis | Altered protein domains |
| Alternative translation initiation | Case studies [68] | Protein sequencing, mass spec | Truncated protein products |
These findings underscore the necessity of incorporating transcriptomic validation into standard CRISPR workflow, particularly for critical regulators like SOX9 where partial functionality could significantly impact research outcomes in immune cell models.
Experimental Design and Workflow
Comprehensive RNA-seq Validation Strategy
A robust transcriptomic validation protocol for SOX9 knockout in immune cells incorporates both short-read and long-read sequencing technologies to capture the full spectrum of potential transcriptional alterations:
Figure 1: Comprehensive workflow for transcriptomic validation of SOX9 knockout in immune cell models, integrating both short-read and long-read RNA-seq approaches.
Table 2: Key Research Reagent Solutions for RNA-seq Validation of CRISPR Knockouts
| Category | Specific Product/Technology | Function in Validation Pipeline |
|---|---|---|
| RNA Extraction | AllPrep DNA/RNA Mini Kit (Qiagen) [71] | Simultaneous DNA/RNA extraction for integrated analysis |
| RNA Quality Control | TapeStation 4200 (Agilent) [71] | RNA integrity number (RIN) assessment |
| Library Preparation | TruSeq stranded mRNA kit (Illumina) [71] | Short-read RNA-seq library construction |
| Long-Read Sequencing | Oxford Nanopore Technologies [72] | Full-length transcript identification |
| Computational Tools | Trinity [70] | De novo transcript assembly |
| Computational Tools | SUPPA2, DEXseq [72] | Differential transcript usage analysis |
| Validation Reagents | Custom antibodies targeting different SOX9 epitopes [68] | Protein-level confirmation of knockout |
Wet-Lab Protocols
RNA Extraction and Quality Control from Immune Cells
Protocol: High-Quality RNA Isolation for Transcriptomic Validation
Cell Lysis and Homogenization
- Harvest 1-5 × 10^6 SOX9-targeted immune cells by centrifugation
- Use AllPrep DNA/RNA Mini Kit (Qiagen) for simultaneous DNA/RNA extraction [71]
- Process cells through QIAshredder columns to ensure complete homogenization
RNA Purification
- Bind RNA to silica membrane columns
- Perform on-column DNase digestion using RNase-Free DNase Set
- Elute in 30-50 μL RNase-free water
- Determine concentration using Qubit 2.0 RNA HS Assay
Quality Assessment
- Analyze RNA integrity using TapeStation 4200 with High Sensitivity RNA ScreenTape [71]
- Accept samples with RIN ≥ 8.5 for sequencing
- Verify absence of genomic DNA contamination via no-RT control PCR
Troubleshooting Note: Immune cells, particularly activated subsets, may present challenges for RNA integrity due to high RNase content. Immediate processing or preservation in RNA stabilization reagents is critical.
Library Preparation and Sequencing
Protocol: Stranded RNA-seq Library Construction
RNA Selection and Fragmentation
- Use 100-1000 ng total RNA as input
- Perform poly-A selection using magnetic oligo(dT) beads
- Fragment RNA to 200-300 bp fragments using divalent cations at 94°C
cDNA Synthesis and Library Construction
- Synthesize first-strand cDNA using reverse transcriptase with actinomycin D
- Perform second-strand synthesis with dUTP incorporation for strand specificity
- Use TruSeq stranded mRNA kit (Illumina) following manufacturer's protocol [71]
Library Quality Control and Sequencing
- Assess library quality using TapeStation 4200 [71]
- Quantify using Qubit dsDNA HS Assay
- Sequence on NovaSeq 6000 with 150 bp paired-end reads, targeting 40-60 million reads per sample
Alternative Protocol: Long-Read RNA-seq for Isoform Detection
Library Preparation for Nanopore Sequencing
- Use 500 ng total RNA with poly-A selection
- Prepare libraries using Ligation Sequencing Kit (SQK-LSK110)
- Load on R9.4.1 flow cells
Sequencing Parameters
- Run for 72 hours or until sufficient coverage achieved
- Target 5-10 million reads per sample
- Use direct RNA sequencing for modified base detection if needed
Bioinformatics Analysis Pipeline
Core Computational Workflow
The bioinformatics pipeline for CRISPR validation requires specialized approaches to detect both intended knockout effects and unintended transcriptional consequences:
Figure 2: Bioinformatics pipeline for comprehensive detection of intended knockout effects and unintended transcriptional events in SOX9-edited immune cells.
Key Analysis Modules
Module 1: SOX9 Knockout Confirmation
- Align reads to reference genome (hg38) using STAR aligner [71]
- Quantify SOX9 expression levels using Kallisto [71] or similar tools
- Confirm significant reduction in SOX9 expression (≥90% decrease expected)
- Verify absence of SOX9 protein-coding transcripts via Trinity assembly [70]
Module 2: Unintended Splicing Event Detection
- Identify alternative splicing events using SUPPA2 or DEXseq [72]
- Detect exon skipping, intron retention, and alternative splice site usage
- Focus on SOX9-targeted exon and flanking regions
- Compare splicing patterns to wild-type controls
Module 3: Fusion Transcript and Rearrangement Detection
- Use de novo transcript assembly with Trinity to identify novel transcripts [70]
- Screen for inter-chromosomal and intra-chromosomal fusion events
- Detect large deletions affecting multiple exons
- Validate findings through PCR and Sanger sequencing
Module 4: Off-target Transcriptional Effects
- Perform differential expression analysis on entire transcriptome
- Identify genes co-regulated with SOX9 or affected by knockout
- Pathway enrichment analysis to detect functional consequences
Quantitative Metrics for Knockout Validation
Table 3: Key Quantitative Metrics for SOX9 Knockout Validation
| Validation Metric | Target Value | Calculation Method | Interpretation |
|---|---|---|---|
| SOX9 Expression Reduction | ≥90% decrease | TPM or FPKM compared to control | Confirms knockout efficacy |
| Fusion Transcript Detection | 0 in validated clones | De novo assembly with Trinity [70] | Absence of major rearrangements |
| Exon Skipping Frequency | <5% of transcripts | Percent Spliced In (PSI) metrics | Minimal splicing disruption |
| NMD Efficiency | ≥95% reduction mutant transcripts | Ratio of mutant to wild-type alleles | Effective transcript elimination |
| Off-target Differential Expression | <100 genes altered | DESeq2 or edgeR analysis | Minimal transcriptome-wide effects |
Validation and Orthogonal Confirmation
Protein-Level Validation
While RNA-seq provides comprehensive transcriptional assessment, protein-level validation remains essential for confirming functional knockout:
Western Blot Protocol:
- Use multiple antibodies targeting different SOX9 epitopes (N-terminal, C-terminal, internal) [68]
- Include positive and negative controls
- Quantify band intensity using densitometry
- Confirm ≥95% reduction in SOX9 protein levels
Alternative Protein Detection Methods:
- Immunofluorescence microscopy for subcellular localization
- Mass spectrometry for absolute quantification
- Flow cytometry for immune cell population analysis
Functional Validation in Immune Cell Models
Given the context of immune cell research, functional validation assays should include:
- Cytokine profiling to detect alterations in immune signaling
- Proliferation assays to assess functional consequences of SOX9 loss
- Differentiation capacity in relevant immune cell subsets
- Transcriptional profiling of known SOX9 target genes
Case Studies and Troubleshooting
Common Challenges and Solutions
Table 4: Troubleshooting Guide for SOX9 Knockout Validation
| Challenge | Potential Causes | Solution Approaches |
|---|---|---|
| Persistent SOX9 Expression | Incomplete editing, alternative isoforms | Single-cell cloning, isoform-specific assays |
| Unexpected Protein Products | Alternative translation initiation [68] | Western blot with multiple antibodies, mass spectrometry |
| Splicing Alterations | Disrupted exonic splicing enhancers [68] | RT-PCR with exon-specific primers, minigene assays |
| Fusion Transcripts | Chromosomal rearrangements [70] | Long-read sequencing, genomic PCR validation |
| Variable Knockout Efficiency | Immune cell heterogeneity | Single-cell RNA-seq, flow sorting before analysis |
Interpretation Guidelines
When analyzing RNA-seq data from SOX9 knockout immune cells:
- Confirm knockout efficacy through significant reduction in SOX9 transcripts
- Document unintended events but distinguish between technical artifacts and biological relevance
- Prioritize validation of events that could potentially confound experimental results
- Consider biological context - some alternative transcripts may be cell-type specific
Comprehensive transcriptomic validation using RNA-seq represents an essential component of rigorous CRISPR-Cas9 experimentation, particularly for critical regulators like SOX9 in immune cell models. The integrated approach outlined in this application note—combining short-read and long-read sequencing with specialized bioinformatic analyses—enables researchers to confidently confirm successful knockout while identifying potential confounding factors that might otherwise compromise experimental outcomes. As CRISPR technologies continue to evolve, standardized validation protocols will be increasingly important for ensuring the reliability and reproducibility of genetic research in immunology and beyond.
The generation of a complete SOX9 knockout in immune cell models using CRISPR-Cas9 technology requires rigorous confirmation at the protein level to ensure the success of functional genomic studies. Proteomic validation is essential, as transcript levels may not accurately reflect functional protein ablation due to post-transcriptional compensation mechanisms. This application note details a standardized framework for confirming SOX9 knockout using orthogonal validation methodologies combining Western blot and mass spectrometry, specifically tailored for hard-to-transfect immune cells like THP-1 monocytes. The dual-verification approach controls for methodological limitations inherent in any single technique, providing researchers with a validated path to reliable protein ablation data critical for downstream immunological assays.
The transcription factor SOX9 plays a context-dependent role in immune regulation, functioning as a "double-edged sword" by promoting immune escape in cancers while contributing to tissue maintenance and repair in inflammatory conditions like osteoarthritis [1]. In immune cells, SOX9 influences T-cell lineage commitment and is overexpressed in certain B-cell lymphomas, making precise genetic manipulation crucial for disentangling its complex functions [1]. This protocol establishes a robust workflow for SOX9 protein validation, enabling researchers to confidently proceed with investigations into SOX9's role in immune cell differentiation, function, and therapeutic targeting.
Experimental Design and Workflow
The following workflow integrates CRISPR-Cas9 gene editing with orthogonal protein validation methods to ensure comprehensive confirmation of SOX9 ablation in immune cell models.
Figure 1: Orthogonal validation workflow for SOX9 protein ablation confirmation. The integrated approach combines antibody-based (Western blot) and antibody-independent (LC-MS/MS) methods to ensure reliable verification of CRISPR-Cas9-mediated knockout.
Key Advantages of Orthogonal Validation
- Methodological Independence: Western blot provides semi-quantitative size-based separation, while LC-MS/MS offers absolute quantification based on mass-to-charge ratios, controlling for technique-specific artifacts [73].
- Comprehensive Coverage: Western blot confirms absence of full-length SOX9 protein, while mass spectrometry detects potential truncated variants that might retain functionality.
- Quality Control: Cross-verification between methods reduces false positives/negatives and controls for antibody specificity issues or mass spectrometry interference [73] [74].
Materials and Reagents
Research Reagent Solutions
Table 1: Essential research reagents for SOX9 knockout validation
| Reagent/Category | Specific Examples & Specifications | Function/Application |
|---|---|---|
| Cell Line Model | THP-1 human monocytes [75] | Hard-to-transfect immune cell model for CRISPR-Cas9 studies |
| CRISPR Delivery | Lentiviral vectors with sgRNA expression cassettes [75] | Enables stable gene delivery with high efficiency in suspension immune cells |
| Selection Antibiotic | Puromycin (concentration optimization required) [75] | Selection of successfully transduced cells |
| SOX9 Antibodies | Validated anti-SOX9 antibodies for Western blot [73] | Detection of SOX9 protein ablation; requires application-specific validation |
| Mass Spec Standards | Stable Isotope Labeled (SIL) peptides for SOX9 [76] | Internal standards for absolute quantification via LC-MS/MS |
| Protein Standards | Purified RBP4/TTR for method validation [76] | Quantitation standards for mass spectrometry calibration |
| Lysis Buffers | RIPA buffer with protease/phosphatase inhibitors | Protein extraction while maintaining integrity |
| Digestion Enzymes | Trypsin Platinum (Promega) [76] | Protein digestion for mass spectrometry analysis |
Protocol for SOX9 Knockout in Immune Cells
CRISPR-Cas9-Mediated Gene Editing in THP-1 Cells
This protocol adapts established methods for hard-to-transfect immune cell lines [75], specifically optimized for SOX9 ablation.
- sgRNA Design and Cloning: Design sgRNAs targeting exons encoding critical SOX9 functional domains (HMG box or transcriptional activation domains) [1]. Clone validated sgRNA sequences into a lentiviral CRISPR vector (e.g., lentiCRISPRv2) using BsmBI restriction sites. Verify constructs by Sanger sequencing.
- Lentiviral Production and Transduction: Package lentiviral particles in HEK293T cells using psPAX2 and pMD2.G packaging plasmids. Concentrate virus via ultracentrifugation. Transduce THP-1 cells at MOI 5-10 in the presence of 8 μg/mL polybrene. Centrifuge at 800 × g for 30-60 minutes (spinoculation) to enhance infection efficiency.
- Selection and Clonal Isolation: Begin puromycin selection (0.5-2 μg/mL, concentration requires optimization) 48 hours post-transduction. Maintain selection for 7-10 days until control cells (non-transduced) are completely dead. For clonal isolation, perform limiting dilution in 96-well plates or use single-cell sorting via FACS.
Sample Preparation for Proteomic Analysis
- Protein Extraction: Harvest 1-2 × 10^7 cells by centrifugation. Wash twice with ice-cold PBS. Lyse cells in RIPA buffer (150 mM NaCl, 1% NP-40, 0.5% sodium deoxycholate, 0.1% SDS, 50 mM Tris pH 8.0) supplemented with protease and phosphatase inhibitors. Incubate on ice for 30 minutes with occasional vortexing. Clarify by centrifugation at 14,000 × g for 15 minutes at 4°C. Quantify protein concentration using BCA assay.
- Sample Allocation: Divide each protein sample into two aliquots: one for Western blot analysis (directly adding Laemmli buffer) and one for mass spectrometry analysis (stored at -80°C in RIPA buffer).
Western Blot Validation Protocol
Electrophoresis and Immunoblotting
- Gel Electrophoresis: Load 20-30 μg of protein per lane on 4-12% Bis-Tris polyacrylamide gels. Include positive control (wild-type cell lysate) and negative control (knockout candidate) in adjacent lanes. Run electrophoresis at 120-150V for 60-90 minutes using MOPS or MES running buffer.
- Protein Transfer: Transfer to PVDF membrane using wet or semi-dry transfer systems. For SOX9 (∼61 kDa), use 100V for 60 minutes (wet transfer) or 25V for 30 minutes (semi-dry) in transfer buffer containing 20% methanol.
- Immunodetection: Block membrane with 5% non-fat milk in TBST for 1 hour. Incubate with validated anti-SOX9 primary antibody (dilution per manufacturer's recommendation) overnight at 4°C. Wash 3× with TBST, then incubate with HRP-conjugated secondary antibody for 1 hour at room temperature. Detect using enhanced chemiluminescence substrate and image with digital imaging system.
Controls and Quantification
- Essential Controls: Include wild-type cells (positive control), knockout candidates (experimental), and no primary antibody (background control). For loading control, probe for housekeeping proteins (β-actin, GAPDH, or tubulin) on the same membrane after stripping or on parallel gels.
- Densitometric Analysis: Quantify band intensities using ImageJ or similar software. Calculate SOX9 expression normalized to loading control. Successful knockout should show >95% reduction compared to wild-type control.
Mass Spectrometry Validation Protocol
Sample Preparation and Digestion
- Protein Digestion: Denature 50 μg of protein in 2 M urea, 50 mM ammonium bicarbonate (pH 7.8). Reduce with 5 mM dithiothreitol (DTT) at 37°C for 30 minutes. Alkylate with 15 mM iodoacetamide at room temperature for 30 minutes in the dark. Dilute urea concentration to <1 M with 50 mM ammonium bicarbonate. Digest with trypsin (1:20-1:50 enzyme-to-protein ratio) at 37°C for 12-16 hours. Stop reaction with 0.5% trifluoroacetic acid (TFA).
- Peptide Cleanup: Desalt peptides using C18 solid-phase extraction tips or columns. Elute with 50-80% acetonitrile/0.1% TFA. Dry peptides in a vacuum concentrator and reconstitute in 0.1% formic acid for LC-MS/MS analysis.
LC-MS/MS Analysis and Quantification
- Liquid Chromatography: Use a nanoflow UHPLC system with C18 column (75 μm × 25 cm, 1.6 μm particles). Inject 1-2 μg of peptides. Separate with a 60-120 minute gradient from 2% to 30% acetonitrile in 0.1% formic acid at 300 nL/min.
- Mass Spectrometry: Operate instrument in data-dependent acquisition mode. Use full MS scans (m/z 350-1500) at resolution 120,000, followed by MS/MS of the most intense ions at resolution 15,000. Use higher-energy collisional dissociation (HCD) with normalized collision energy 28-32.
- SOX9-Specific Monitoring: Include targeted inclusion of SOX9-specific peptides based on in silico digestion. For absolute quantification, spike in stable isotope-labeled (SIL) synthetic peptides as internal standards [76].
Data Analysis and Interpretation
Quantitative Metrics for Validation
Table 2: Validation metrics and acceptance criteria for SOX9 ablation confirmation
| Validation Parameter | Western Blot | LC-MS/MS | Acceptance Criteria |
|---|---|---|---|
| SOX9 Detection | Band intensity at ∼61 kDa | Peptide spectrum matches | >95% reduction in knockout vs. control |
| Specificity Control | Size correspondence with standard | Retention time alignment | Exact mass (±10 ppm) and correct RT |
| Quantitation Range | Semi-quantitative (linear dynamic range ∼10²) | Absolute quantitation (linear range: 0.5-6 μM for proteins) [76] | Calibration curve R² > 0.99 |
| Precision | Inter-gel CV < 15% | Inter-day CV < 12% [76] | Within stated variability limits |
| Sensitivity | Low ng range | Low fmol range | Detect < 10% of wild-type expression |
| Orthogonal Correlation | Band intensity vs. peptide abundance | Peptide abundance vs. band intensity | Pearson r > 0.9 between methods |
Data Interpretation Guidelines
- Confirmation of Successful Knockout: SOX9 should be undetectable or show >95% reduction in both Western blot (no visible band at ∼61 kDa) and mass spectrometry (no SOX9-specific peptides above limit of detection) compared to wild-type controls.
- Identification of Partial Knockout: If Western blot shows reduced but detectable signal, and mass spectrometry confirms presence of SOX9 peptides, this may indicate incomplete editing or mixed population. Subcloning may be required.
- Detection of Truncated Variants: If Western blot shows smaller bands but mass spectrometry detects SOX9 peptides, this may indicate in-frame mutations producing truncated proteins. Further characterization needed.
Troubleshooting Common Issues
Method-Specific Challenges
- Western Blot Specificity: If non-specific bands appear, optimize antibody dilution, include additional negative controls, or try different antibody clones. Orthogonal validation using knockout cells is essential [73].
- Mass Spectrometry Sensitivity: If SOX9 peptides are not detected in controls, optimize digestion efficiency, check instrument calibration, or include peptide enrichment strategies. Use internal standards to account for recovery variations [76].
- Inconsistent Results Between Methods: If Western blot shows ablation but mass spectrometry detects SOX9 peptides (or vice versa), investigate potential methodological artifacts. For Western blot, epitope masking or transfer efficiency issues may occur. For mass spectrometry, peptide interference or ionization efficiency variations may be responsible.
The orthogonal validation approach combining Western blot and mass spectrometry provides a robust framework for confirming SOX9 protein ablation in CRISPR-Cas9-edited immune cell models. This dual-method strategy controls for the limitations inherent in either technique alone, ensuring reliable knockout validation before proceeding to functional studies. The protocols outlined here for THP-1 cells can be adapted to other immune cell models with appropriate optimization of transduction conditions and validation parameters. Through rigorous proteomic confirmation of SOX9 ablation, researchers can confidently investigate the multifaceted roles of this transcription factor in immune regulation, cancer immunology, and inflammatory disease mechanisms.
Figure 2: Downstream applications of validated SOX9 knockout immune cell models. Confirmed protein ablation enables investigation of SOX9 functions in immune regulation, with implications for cancer immunotherapy, autoimmune diseases, and inflammatory disorders.
The transcription factor SOX9 plays a complex, janus-faced role in immunology, acting as a critical regulator in tumor immune escape, inflammatory diseases, and tissue repair [1]. Within the tumor microenvironment, SOX9 overexpression is associated with impaired immune cell function, contributing to immunosuppression [1] [19]. Functional validation of CRISPR-Cas9-mediated SOX9 knockout in immune cell models requires a multifaceted approach assessing immune cell function, cytokine secretion, and performance in co-culture systems that recapitulate cell-cell interactions. This application note provides detailed protocols for comprehensively evaluating the functional consequences of SOX9 manipulation in immunobiological contexts.
SOX9 in Immune Regulation: Rationale for Functional Validation
SOX9 significantly influences immune cell differentiation and function. It participates in γδ T-cell lineage commitment by activating Rorc and key Tγδ17 effector genes (Il17a, Blk) [1]. In cancer contexts, SOX9 expression negatively correlates with genes associated with CD8+ T-cell, NK cell, and M1 macrophage function, while showing positive correlation with immunosuppressive memory CD4+ T cells [1]. Research in lung adenocarcinoma demonstrates that SOX9 suppresses immune cell infiltration and functionally impairs tumor-associated CD8+ T cells, natural killer cells, and dendritic cells [19]. These findings establish SOX9 as a significant immunomodulator requiring thorough functional assessment following genetic perturbation.
Essential Research Reagent Solutions
The table below summarizes key reagents essential for executing SOX9 functional validation assays:
Table 1: Essential Research Reagents for SOX9 Immune Functional Validation
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| CRISPR Components | dSpCas9-VP64 (for activation), dSaCas9-KRAB (for inhibition), sgRNA expression vectors [6] | CRISPRa/i-mediated SOX9 perturbation; precise transcriptional control without DNA cleavage. |
| Cell Culture Models | Primary T-cells, macrophage cell lines, melanoma cell lines (MALME-3M, SK-MEL-5), 2D3 Jurkat-derived T-cell reporter line [77] | Provide physiologically relevant systems for immune function assays and co-culture studies. |
| Co-culture Reporter System | 2D3 cell line (TCR-negative, CD8+, PD-1+, NFAT-responsive eGFP reporter) [77] | Quantifies T-cell activation via NFAT pathway signaling in immune evasion studies. |
| Analytical Tools | Flow cytometry antibodies (CD8, CD4, NK cell markers), cytokine ELISA/LEGENDplex kits, H3K27ac HiChIP reagents [78] [19] | Immune phenotyping, cytokine secretion profiling, enhancer-promoter interaction mapping. |
Methodological Workflow for Comprehensive Validation
The following diagram illustrates the integrated experimental workflow for validating SOX9 knockout in immune cell models:
Detailed Experimental Protocols
Protocol 1: Cytokine Secretion Profiling in SOX9-Modified T-Cell Subsets
Purpose: To quantitatively assess the impact of SOX9 knockout on cytokine production patterns across differentiated T-helper cell subsets.
Materials:
- SOX9-knockout and control T-cells
- T-cell activation/expansion kit (anti-CD3/CD28 beads)
- Th1 polarization: IL-12 (20 ng/mL), anti-IL-4 (10 µg/mL)
- Th2 polarization: IL-4 (20 ng/mL), anti-IFN-γ (10 µg/mL)
- Th17 polarization: TGF-β (2 ng/mL), IL-6 (30 ng/mL), IL-1β (10 ng/mL), anti-IFN-γ (10 µg/mL), anti-IL-4 (10 µg/mL)
- Treg polarization: TGF-β (5 ng/mL), IL-2 (100 U/mL)
- Cytokine detection: LEGENDplex multi-analyte flow assay or ELISA kits
Procedure:
- T-Cell Differentiation: Isolate naïve CD4+ T-cells from SOX9-KO and control models using magnetic bead separation. Activate cells with plate-bound anti-CD3 (5 µg/mL) and soluble anti-CD28 (2 µg/mL) under respective polarization conditions for 5-7 days.
- Restimulation: Harvest polarized T-cells, wash, and restimulate with PMA (50 ng/mL) and ionomycin (1 µg/mL) in the presence of protein transport inhibitor for 5 hours.
- Cytokine Measurement:
- Intracellular staining: Fix and permeabilize cells using cytofix/cytoperm kit, then stain with fluorochrome-conjugated antibodies against subset-specific cytokines (IFN-γ for Th1, IL-4/IL-5/IL-13 for Th2, IL-17A for Th17).
- Secreted cytokine quantification: Collect culture supernatants after 24-48 hours of restimulation. Analyze using LEGENDplex bead-based immunoassay according to manufacturer's instructions.
Data Analysis: Compare cytokine profiles between SOX9-KO and control cells across subsets. Normalize data to cell counts and report as mean fluorescence intensity (intracellular) or concentration (secreted).
Protocol 2: Co-culture Assessment of T-Cell Activation Using NFAT Reporter System
Purpose: To evaluate the functional consequence of SOX9 manipulation in cancer cells on T-cell activation using a standardized reporter system.
Materials:
- 2D3 T-cell reporter line (Jurkat-derived, TCR-negative, CD8+, PD-1+, NFAT-responsive eGFP) [77]
- SOX9-knockout and control cancer cell lines (e.g., melanoma lines MALME-3M, SK-MEL-5)
- Antigen-presenting cells (T2 or U266B1 lines)
- Flow cytometry with GFP detection capability
- CRISPRi machinery (dCas9-KRAB) for SOX9 knockdown if knockout not available
Procedure:
- CRISPR-Mediated SOX9 Perturbation: If not already established, perform SOX9 knockdown in cancer cells using lentiviral delivery of dCas9-KRAB and SOX9-targeting sgRNAs. Include non-targeting sgRNA control.
- Co-culture Setup: Seed cancer cells (SOX9-KD and control) in 96-well plates at 1×10^4 cells/well. After 24 hours, add 2D3 T-cells at 2:1 effector:target ratio. Include controls for baseline GFP expression.
- Activation Measurement: After 24 hours of co-culture, harvest cells and analyze by flow cytometry for GFP fluorescence intensity as measure of NFAT activation. Gate on live 2D3 cells (typically based on size and lack of adherent markers).
- Validation: Confirm SOX9 modulation by parallel Western blot or RT-qPCR analysis of cancer cells.
Data Analysis: Calculate fold-change in GFP+ 2D3 cells and mean fluorescence intensity (MFI) in SOX9-KD versus control co-cultures. Statistical analysis via Student's t-test (for two groups) or ANOVA (multiple comparisons).
Protocol 3: High-Throughput CRISPRi Screening in Co-culture Models
Purpose: To identify SOX9-regulated immune modulators using arrayed CRISPR interference screening in co-culture systems.
Materials:
- pSLQ1371 sgRNA expression plasmid or similar [77]
- BstX1 and BlpI restriction enzymes for plasmid digestion
- dCas9-KRAB-expressing cancer cell lines
- 2D3 T-cell reporter line
- Lentiviral packaging plasmids (pCMV-dR8.91, pMD2.G)
- High-throughput flow cytometry or automated imaging system
Procedure:
- sgRNA Library Preparation: Digest pSLQ1371 plasmid with BstX1 (37°C, 3 hours), purify, then digest with BlpI (37°C, 3 hours) with phosphatase treatment to prevent re-ligation [77].
- Lentiviral Production: Transfert HEK293T/17 cells with sgRNA plasmids and packaging vectors using transfection reagent. Harvest virus-containing supernatant at 48 and 72 hours post-transfection.
- Cell Transduction: Transduce dCas9-KRAB-expressing cancer cells with sgRNA library at MOI<1 to ensure single integration. Include non-targeting sgRNA controls.
- Co-culture Screening: Co-culture transduced cancer cells with 2D3 reporter T-cells as in Protocol 2. After 24-48 hours, analyze T-cell activation via GFP expression.
- Hit Identification: Sort GFP-low and GFP-high populations. Isolve genomic DNA and amplify integrated sgRNA sequences for NGS to identify enriched/depleted sgRNAs.
Data Analysis: Normalize sgRNA counts, calculate fold-changes between populations, and use MAGeCK or similar algorithms to identify significantly enriched genes.
Expected Results and Data Interpretation
Quantitative Profiles of SOX9-Mediated Immune Modulation
Table 2: Expected Cytokine Secretion Profiles in SOX9-Knockout T-Cell Subsets
| T-Cell Subset | Key Cytokines | Expected Change with SOX9 KO | Potential Research Significance |
|---|---|---|---|
| Th1 Cells | IFN-γ, TNF-α | ↑ Secretion (1.5-2.5 fold) [79] | Enhanced anti-tumor cellular immunity; potential autoimmunity risk |
| Th2 Cells | IL-4, IL-5, IL-13 | ↓ Secretion (0.4-0.7 fold) [79] | Reduced allergic/asthma responses; impaired parasite immunity |
| Th17 Cells | IL-17A, IL-17F | ↓ Secretion (0.3-0.6 fold) [1] | Reduced autoimmunity; potential compromise to mucosal immunity |
| Treg Cells | IL-10, TGF-β | Context-dependent alteration [79] | Modulated immunosuppression in tumor microenvironment |
SOX9-Knockout Effects on Co-culture T-Cell Activation
Table 3: Anticipated Co-culture Phenotypes in SOX9-Modified Systems
| Experimental Model | Readout | Expected SOX9-KO Effect | Biological Interpretation |
|---|---|---|---|
| Cancer Cell:T-Cell Co-culture | NFAT-GFP+ T-cells [77] | ↑ 30-60% GFP+ cells | Reduced tumor immune evasion mechanisms |
| SOX9-KO Cancer Cells | T-cell Cytotoxicity | ↑ Target cell killing (20-40%) | Enhanced anti-tumor immune response |
| SOX9-KO T-cells | Exhaustion Markers (PD-1, TIM-3) | ↓ Surface expression (0.5-0.8 fold) | Improved T-cell persistence in tumor microenvironment |
| Macrophage Co-culture | M1/M2 Polarization Ratio | Shift toward M1 phenotype [1] | Promoted pro-inflammatory, anti-tumor state |
Troubleshooting and Technical Considerations
- Low KO Efficiency: Optimize RNP delivery by testing electroporation parameters or lipid nanoparticle formulations specific to primary immune cells [7].
- Variable Polarization: Validate T-cell subset differentiation using intracellular cytokine staining and key transcription factors (T-bet for Th1, GATA-3 for Th2, RORγt for Th17, FoxP3 for Treg).
- High Background in Co-culture: Include proper controls: T-cells alone, cancer cells alone, and non-relevant antigen presentations to establish baseline activation.
- CRISPRi Efficiency: Validate SOX9 knockdown at protein level before functional assays; test multiple sgRNAs for consistent phenotypes.
Comprehensive functional validation of CRISPR-Cas9-mediated SOX9 knockout requires integrated assessment across immune phenotyping, cytokine profiling, and co-culture models. The protocols detailed herein enable researchers to systematically decipher SOX9's multifaceted roles in immune regulation, particularly its context-dependent functions in tumor immunity and inflammation. These approaches provide a framework for evaluating SOX9-targeting strategies in both basic immunology research and therapeutic development for cancer and immune-related diseases.
Within functional genomics research, particularly in the study of transcription factors like SOX9 in immune cell models, selecting the appropriate perturbation strategy is crucial for generating biologically relevant data. CRISPR-Cas9 knockout (CRISPRko) permanently disrupts gene function by creating double-strand breaks, while CRISPR interference (CRISPRi) and CRISPR activation (CRISPRa) provide reversible, titratable control over gene expression without altering the DNA sequence itself [80] [81]. This Application Note details the comparative outcomes of these approaches, providing structured protocols and resources for researchers investigating SOX9 and similar targets in immunology and drug development.
The core technological difference lies in the Cas9 protein employed. CRISPRko uses nuclease-active Cas9, whereas CRISPRi/a uses a catalytically dead Cas9 (dCas9) that retains DNA-binding ability but lacks cutting activity [82] [81]. When dCas9 is fused to repressor domains like KRAB, it blocks transcription (CRISPRi); when fused to activator complexes like VPR or SAM, it enhances transcription (CRISPRa) [80] [83].
Comparative Outcomes in Functional Genomics
Key Characteristics and Applications
The choice between these modalities significantly influences experimental outcomes and biological interpretations, especially when studying pleiotropic factors like SOX9.
Table 1: Comparative Analysis of CRISPRko, CRISPRi, and CRISPRa Outcomes
| Parameter | CRISPRko (Knockout) | CRISPRi (Interference) | CRISPRa (Activation) |
|---|---|---|---|
| Molecular Outcome | Permanent DNA disruption; indels cause frameshifts [81] | Reversible transcript knockdown; no DNA alteration [82] | Transcriptional upregulation; no DNA alteration [81] |
| Cas9 Form | Nuclease-active Cas9 | dCas9-KRAB repressor fusion [82] | dCas9-activator fusion (e.g., VPR, SAM) [80] |
| Effect on Expression | Complete loss of function | Tunable repression (typically 60-99%) [81] | Tunable activation (up to 1,000-fold) [80] |
| gRNA Target Site | Early exons to disrupt coding sequence [82] | -50 to +300 bp from TSS (optimal: +100 bp downstream) [82] | -400 to -50 bp from TSS [82] |
| Reversibility | Irreversible | Reversible and titratable [81] | Reversible and titratable [81] |
| Cytotoxicity & Genotoxicity | High (DSB-induced; p53 response; genomic instability) [82] | Minimal (no DNA cleavage) [82] [84] | Minimal (no DNA cleavage) [84] |
| Study of Essential Genes | Lethal; precludes study of fitness effects [82] [81] | Enables study via partial knockdown [82] [81] | Enables study of overexpression phenotypes [80] |
| Ideal for Non-Coding RNAs | Challenging (requires large deletions) [82] | Excellent for lncRNAs, promoters [82] [81] | Excellent for lncRNAs, enhancers [80] [81] |
| Phenotype Mimicry | Resembles null mutations | Mimics partial inhibition (e.g., drug action) [81] | Mimics oncogene/tumor suppressor overexpression [80] |
Contextualizing SOX9 Research in Immune Models
In immune cell models, the choice of CRISPR modality can reveal different facets of SOX9 biology. SOX9 plays a complex, "double-edged sword" role in immunology, acting as both an oncogene and a regulator of tissue repair [1].
CRISPRko (Complete Loss-of-Function): Successfully used to demonstrate that SOX9 ablation sensitizes high-grade serous ovarian cancer cells to platinum-based chemotherapy [8]. However, this complete knockout would be unsuitable for studying SOX9's essential roles in cell survival or for mimicking partial therapeutic inhibition.
CRISPRi (Tunable Knockdown): Ideal for modeling dose-dependent effects of SOX9 suppression, which is relevant for understanding its roles in tumor immune escape. SOX9 expression negatively correlates with CD8+ T cell and NK cell function, and its repression could potentially enhance anti-tumor immunity [1]. CRISPRi allows researchers to titrate repression to avoid lethal phenotypes while studying these immunomodulatory effects.
CRISPRa (Controlled Overexpression): Enables study of SOX9 upregulation, which is sufficient to induce a stem-like transcriptional state and significant chemoresistance [8]. CRISPRa can also be used therapeutically; for example, engineered SOX9 overexpression in mesenchymal stromal cells enhances extracellular matrix restoration and reduces inflammation in disc regeneration studies [17].
Experimental Protocols
Protocol 1: CRISPRko for SOX9 Knockout in Immune Cell Lines
Objective: To generate permanent SOX9 knockout cells to study the effects of complete gene loss on immune function and chemosensitivity.
Materials:
- Plasmid: lentiCRISPRv2 (Addgene #52961) or similar CRISPRko vector
- Cell Line: Relevant immune/model cell line (e.g., THP-1, K562, Jurkat)
- SOX9-targeting gRNA: Designed to target early exons (see Table 2 for sequences)
- Controls: Non-targeting gRNA control
Workflow:
Detailed Steps:
gRNA Design and Cloning:
- Design gRNAs targeting early exons of SOX9 to maximize frameshift probability. The gRNA sequence
GACGAAGCGCTGCAAAAtargets exon 2 and has been successfully used for SOX9 knockout [8]. - Clone annealed oligonucleotides into BsmBI-digested lentiCRISPRv2 vector.
- Verify sequence via Sanger sequencing.
- Design gRNAs targeting early exons of SOX9 to maximize frameshift probability. The gRNA sequence
Lentiviral Production:
- Co-transfect HEK293T cells with the lentiCRISPRv2-gRNA plasmid and packaging plasmids (psPAX2, pMD2.G) using PEI transfection reagent.
- Collect viral supernatant at 48 and 72 hours post-transfection.
- Concentrate virus using Lenti-X Concentrator if needed.
Cell Transduction:
- Plate target cells at 50% confluency in 6-well plates.
- Add viral supernatant with 8 μg/mL polybrene.
- Centrifuge at 800 × g for 30-60 minutes (spinoculation) to enhance infection efficiency.
Selection and Clonal Isolation:
- Begin puromycin selection (concentration determined by kill curve) 48 hours post-transduction.
- Maintain selection for 5-7 days until control cells are dead.
- For clonal isolation, dilute cells to 0.5 cells/well in 96-well plates or use FACS sorting.
Validation of Knockout:
- Genomic DNA: Extract genomic DNA and amplify the target region. Use T7 Endonuclease I assay or Sanger sequencing to detect indels.
- Protein: Confirm SOX9 loss via Western blotting using anti-SOX9 antibody (MilliporeSigma, AB5535).
Phenotypic Assessment:
Protocol 2: CRISPRi/a for Tunable SOX9 Modulation in Primary Immune Cells
Objective: To achieve reversible, titratable control of SOX9 expression in primary human T cells or HSPCs to study dose-dependent effects on differentiation and function.
Materials:
- CRISPRi: dCas9-KRAB mRNA [83]
- CRISPRa: dCas9-VPR mRNA [83]
- Chemically Modified sgRNAs: Targeting SOX9 promoter (see Table 2)
- Primary Cells: Human CD34+ HSPCs or CD3+ T cells
- Delivery System: Neon Transfection System (Thermo Fisher)
Workflow:
Detailed Steps:
gRNA Design and Synthesis:
- For CRISPRi: Design sgRNAs targeting from -50 to +300 bp relative to the SOX9 TSS, with optimal efficacy in the first 100 bp downstream [82].
- For CRISPRa: Design sgRNAs targeting from -400 to -50 bp upstream of the SOX9 TSS [82].
- Use chemically modified sgRNAs (e.g., 2'-O-methyl 3' phosphorothioate) to enhance stability [83].
Ribonucleoprotein (RNP) Complex Formation:
- For CRISPRi: Combine 10 μg of dCas9-KRAB mRNA with 5 μg of SOX9-targeting sgRNA in sterile tubes.
- For CRISPRa: Combine 10 μg of dCas9-VPR mRNA with 5 μg of SOX9-targeting sgRNA.
- Incubate at room temperature for 10 minutes to allow complex formation.
Electroporation of Primary Cells:
- Isolate primary CD34+ HSPCs or CD3+ T cells from healthy donor samples.
- Use Neon Transfection System with the following optimized conditions for T cells [83]:
- Voltage: 1,350 V
- Width: 10 ms
- Pulses: 3
- Resuspend 1 × 10^6 cells in 100 μL Buffer R with the RNP complex and electroporate.
Validation of Modulation:
- Time Course: Assess SOX9 expression at 24, 48, 72, and 96 hours post-electroporation.
- mRNA Level: Use RT-qPCR with SOX9-specific primers.
- Protein Level: Use intracellular flow cytometry or Western blotting.
Functional Assays:
- For HSPCs: Investigate SOX9's role in differentiation trajectories using colony-forming unit assays [83].
- For T cells: Assess the effect of SOX9 modulation on activation markers (CD25, CD69) and cytokine production.
Kinetics and Reversibility:
- Monitor SOX9 expression daily for 5-6 days to confirm the transient nature of modulation, with effects typically returning to baseline within this timeframe [83].
Research Reagent Solutions
Table 2: Essential Research Reagents for CRISPRko, CRISPRi, and CRISPRa Studies
| Reagent Category | Specific Product/System | Function & Application Notes |
|---|---|---|
| CRISPRko Plasmids | lentiCRISPRv2 (Addgene #52961) | All-in-one vector expressing Cas9 and gRNA; for stable knockout generation [8] |
| CRISPRi/a dCas9 Effectors | dCas9-KRAB (CRISPRi); dCas9-VPR (CRISPRa) | Nuclease-dead Cas9 fused to transcriptional modulators; available as mRNA for transient delivery [83] |
| SOX9-Targeting gRNAs | CRISPRko: GACGAAGCGCTGCAAAA [8] |
Validated sequence for efficient SOX9 exon targeting |
| Delivery Systems | Lentivirus (stable expression); Electroporation (mRNA/RNP) | Lentivirus for cell lines; electroporation for primary cells (lower toxicity) [83] |
| Validation Antibodies | Anti-SOX9 (MilliporeSigma AB5535) | Validated for Western blot to confirm SOX9 protein loss (KO) or modulation (i/a) |
| Primary Cell Culture | Human CD34+ HSPCs; CD3+ T cells | Primary immune cells for physiologically relevant models [83] |
| Selection Agents | Puromycin (for lentiviral selection) | Selects for successfully transduced cells; concentration requires kill curve determination |
| sgRNA Design Tools | CRISPick, CHOPCHOP | Algorithms incorporating optimal positioning for CRISPRi/a (TSS-proximal) [82] |
The choice between CRISPRko and CRISPRi/a represents a fundamental strategic decision in functional genomics, particularly for multifaceted transcription factors like SOX9 in immune models. CRISPRko provides definitive, permanent loss-of-function data, making it ideal for validating essential roles and modeling complete genetic deficiency. In contrast, CRISPRi and CRISPRa offer reversible, tunable control that better mimics therapeutic interventions and allows study of essential genes and non-coding regions. For comprehensive SOX9 studies, a combined approach—using CRISPRko to establish null phenotypes and CRISPRi/a to model nuanced expression modulation—will yield the most physiologically and therapeutically relevant insights for drug development targeting immune pathways.
Conclusion
The strategic knockout of SOX9 using CRISPR-Cas9 in immune cell models presents a powerful approach to dissect its complex immunological functions and unlock new therapeutic avenues. This synthesis underscores that successful experimentation hinges on a seamless integration of foundational knowledge, robust methodological execution, proactive troubleshooting, and multi-layered validation. The future of this field lies in leveraging these refined models to decipher detailed mechanisms of SOX9 in immune evasion and tissue homeostasis, ultimately informing the development of next-generation, SOX9-targeted immunotherapies for cancer and autoimmune disorders. As delivery systems improve and CRISPR tools become even more precise, the clinical translation of engineered immune cells with modulated SOX9 activity moves from a compelling possibility to an imminent reality.
References
- 1. SOX9: a novel janus-faced regulator in immunity and its ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1700812/full]
- 2. SOX9 plays an essential role in myofibroblast driven hepatic ... [https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1012928]
- 3. SOX9: an important factor in regulating breast cancer [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-02730-0]
- 4. Role of the SOX family in cancer immune evasion [https://pmc.ncbi.nlm.nih.gov/articles/PMC11789896/]
- 5. A SOX9-B7x axis safeguards dedifferentiated tumor cells ... [https://www.sciencedirect.com/science/article/pii/S1534580723005518]
- 6. CRISPR-mediated Sox9 activation and RelA inhibition ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11405173/]
- 7. Streamlined, single-step non-viral CRISPR-Cas9 knockout ... [https://arthritis-research.biomedcentral.com/articles/10.1186/s13075-024-03294-w]
- 8. SOX9 drives a stem-like transcriptional state and platinum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483608/]
- 9. High expression of SOX9 is a diagnostic and prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277172/]
- 10. SOX9 drives a stem-like transcriptional state and platinum ... [https://www.jci.org/articles/view/186467]
- 11. Role of Sox9 in BPD and its effects on the Wnt/β-catenin ... [https://www.nature.com/articles/s41420-023-01795-2]
- 12. SOX9 mediates the phenotypic transformation of vascular ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1592594/full]
- 13. SOX9 in cartilage development and disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6956855/]
- 14. SOX9 reprograms endothelial cells by altering the chromatin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9410909/]
- 15. Therapeutic Delivery of rAAV sox9 via Polymeric Micelles Counteracts the Effects of Osteoarthritis-Associated Inflammatory Cytokines in Human Articular Chondrocytes - PubMed [https://pubmed.ncbi.nlm.nih.gov/32630578/]
- 16. Co-delivery of IL-1Ra and SOX9 via AAV inhibits inflammation and promotes cartilage repair in surgically induced osteoarthritis animal models | Gene Therapy [https://www.nature.com/articles/s41434-025-00515-y]
- 17. Enhanced disc regeneration through CRISPR/Cas9-mediated ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04600-2]
- 18. CRISPR/Cas9 gene editing of a SOX9 reporter human ... [https://www.sciencedirect.com/science/article/pii/S1873506120302439]
- 19. SOX9 drives KRAS-induced lung adenocarcinoma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11809655/]
- 20. The pioneer factor SOX9 competes for epigenetic factors to ... [https://www.nature.com/articles/s41556-023-01184-y]
- 21. Editing SOX Genes by CRISPR-Cas - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC8583549/]
- 22. SOX9 Knockout Induces Polyploidy and Changes Sensitivity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7589851/]
- 23. CRISPR Gene Editing Workflow: A Step-by-Step Guide [https://www.cd-genomics.com/blog/crispr-gene-editing-workflow-a-step-by-step-guide/]
- 24. CRISPR interference-mediated silencing of pro ... [https://www.sciencedirect.com/science/article/abs/pii/S1567576925012470]
- 25. CRISPR interference-mediated silencing of pro ... [https://pubmed.ncbi.nlm.nih.gov/40680607/]
- 26. Cytotoxicity of activator expression in CRISPR-based ... [https://www.nature.com/articles/s41467-025-63570-4]
- 27. Genetic and epigenetic screens in primary human T cells ... [https://www.nature.com/articles/s41588-025-02301-3]
- 28. Design of highly functional genome editors by modelling ... [https://www.nature.com/articles/s41586-025-09298-z]
- 29. The Complete Guide to Understanding CRISPR sgRNA [https://www.synthego.com/guide/how-to-use-crispr/sgrna/]
- 30. How To Design Guide RNA for CRISPR [https://www.synthego.com/guide/how-to-use-crispr/design-grna-crispr/]
- 31. CRISPR: Guide to gRNA design [https://www.snapgene.com/guides/design-grna-for-crispr]
- 32. CRISPR Guide [https://www.addgene.org/guides/crispr/]
- 33. Delivery Solutions For Immune Cells [https://www.thermofisher.com/us/en/home/life-science/cell-culture/cell-culture-learning-center/cell-culture-resource-library/cell-culture-transfection-application-notes/delivery-solutions-immune-cells.html]
- 34. Optimizing viral transduction in immune cell therapy ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06524-0]
- 35. Targeting KRASG12D mutation in non-small cell lung cancer [https://www.nature.com/articles/s41417-024-00778-4]
- 36. KRASG12D drives immunosuppression in lung ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11721295/]
- 37. SOX9 drives KRAS-induced lung adenocarcinoma ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/37258742/]
- 38. CRISPR-mediated Sox9 activation and RelA inhibition ... [https://pubmed.ncbi.nlm.nih.gov/38879753]
- 39. CRISPR-Modified Mesenchymal Stromal Cells Show ... [https://crisprmedicinenews.com/news/crispr-modified-mesenchymal-stromal-cells-show-therapeutic-potential-in-osteoarthritis/]
- 40. The role of NF-κB-SOX9 signalling pathway in osteoarthritis [https://www.sciencedirect.com/science/article/pii/S2405844024132227]
- 41. Chondrocyte fatty acid oxidation drives osteoarthritis via ... [https://www.nature.com/articles/s41467-025-60037-4]
- 42. Editing SOX Genes by CRISPR-Cas: Current Insights and ... [https://www.mdpi.com/1422-0067/22/21/11321]
- 43. CRISPR in Cancer Therapeutics: CAR T, NK, TCR and ... [https://www.synthego.com/blog/crispr-cancer-therapy/]
- 44. CMN Weekly (26 September 2025) [https://crisprmedicinenews.com/news/cmn-weekly-26-september-2025-your-weekly-crispr-medicine-news/]
- 45. MaxCyte Helps Engineer Difficult-to-Transfect Immune Cells [https://maxcyte.com/webinar/icle-engineering-difficult-to-transfect-immune-cells-using-electroporation/]
- 46. Transcriptomic analysis of the innate immune response to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9800263/]
- 47. Improve Transfection in Difficult Cell Lines [https://www.bocsci.com/resources/proven-strategies-to-improve-transfection-efficiency-in-difficult-cell-lines.html?srsltid=AfmBOoqBe3SAwfrPPG5HcTowCkRZeRRWN3avDliVnNdX-fOM-JV-030e]
- 48. Cell transfection: Methods, emerging applications, and ... [https://www.abcam.com/en-us/knowledge-center/cell-biology/cell-transfection]
- 49. A Guide to Efficient CRISPR gRNA Design: Principles and ... [https://www.genscript.com/a-guide-to-efficient-crispr-grna-design-principles-and-design-tools.html]
- 50. CRISPR–Cas9 gRNA efficiency prediction: an overview of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9023298/]
- 51. Ensure Proper Controls in Your CRISPR Experiments [https://www.synthego.com/blog/controls-crispr-experiments/]
- 52. Off-target effects in CRISPR-Cas genome editing for ... [https://www.sciencedirect.com/science/article/pii/S2162253125001908]
- 53. Off-target effects in CRISPR-Cas genome editing for ... [https://pubmed.ncbi.nlm.nih.gov/40777742/]
- 54. CRISPR Off-Target Editing: Prediction, Analysis, and More [https://www.synthego.com/blog/crispr-off-target-editing/]
- 55. AI-guided Cas9 engineering provides an effective strategy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12583830/]
- 56. CRISPR innovations in tissue engineering and gene editing [https://www.sciencedirect.com/science/article/pii/S0024320524007100]
- 57. Step-by-Step Guide for Analyzing CRISPR Editing Results ... [https://www.editco.bio/step-by-step-ice-guide]
- 58. Similarity-based transfer learning with deep ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12571277/]
- 59. Make Your Single Cell Isolation Protocol Easy with CellGem [https://www.atlantisbioscience.com/blog/make-your-single-cell-isolation-protocol-easy-with-cellgem/?srsltid=AfmBOoobdG-immj4pd_644MWpyQl3kzqYqWTtcPuLNns2Wtx4XdIIxQj]
- 60. Guidelines For Clone Isolation and Validation [https://www.thermofisher.com/us/en/home/life-science/genome-editing/genome-editing-learning-center/genome-editing-resource-library/crispr-validated-protocols/guidelines-clone-isolation-validation.html]
- 61. Pseudogene-Mediated Gene Conversion After CRISPR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8575057/]
- 62. Methods for Optimizing CRISPR-Cas9 Genome Editing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4976696/]
- 63. Systematic Comparison of Computational Tools for Sanger ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10854981/]
- 64. Verification of CRISPR Gene Editing Efficiency [https://www.thermofisher.com/us/en/home/life-science/genome-editing/genome-editing-learning-center/genome-editing-resource-library/crispr-validated-protocols/verification-crispr-gene-editing-efficiency.html]
- 65. A targeted next-generation sequencing panel for ... [https://www.nature.com/articles/s41598-025-08039-6]
- 66. How To Use ICE: A Detailed Guide for Analyzing CRISPR ... [https://www.synthego.com/guide/how-to-use-crispr/ice-analysis-guide/]
- 67. Comparative Analysis of Methods for Assessing On-Target ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11932317/]
- 68. CRISPR-Cas9-based mutagenesis frequently provokes on- ... [https://www.nature.com/articles/s41467-019-12028-5]
- 69. SOX9 has distinct regulatory roles in alternative splicing ... [https://www.genscript.com/reference_peer-reviewed_literature_34347.html]
- 70. Techniques for Validating CRISPR Changes Using RNA- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12027141/]
- 71. Clinical and analytical validation of a combined RNA ... [https://www.nature.com/articles/s43856-025-00934-3]
- 72. Long-read RNA-sequencing reveals transcript-specific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12308531/]
- 73. Antibody Validation Essentials: Orthogonal Strategy - CST Blog [https://blog.cellsignal.com/hallmarks-of-validation-orthogonal-strategy]
- 74. Regulatory Consequences: New Protein-Impurity Guidelines [https://www.bioprocessintl.com/sponsored-content/regulatory-consequences-of-new-protein-impurity-guidelines]
- 75. Protocol for Generation of Single-Gene Knockout in Hard- ... [https://pubmed.ncbi.nlm.nih.gov/40655415/]
- 76. Development and Validation of a Novel LC-MS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11908197/]
- 77. A co-culture model to study modulators of tumor immune ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1444886/full]
- 78. Systematic decoding of functional enhancer connectomes ... [https://www.nature.com/articles/s41556-025-01737-3]
- 79. CRISPR–Cas9 applications in T cells and adoptive T cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11010303/]
- 80. CRISPRi and CRISPRa screens in mammalian cells for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5886776/]
- 81. CRISPRa and CRISPRi [https://www.synthego.com/guide/crispr-methods/crispri-crispra/]
- 82. CRISPRa and CRISPRi: Why You Need These Powerful ... [https://bitesizebio.com/47575/crispra-and-crispri/]
- 83. Targeted regulation of transcription in primary cells using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8559706/]
- 84. The Potential and Pitfalls of CRISPRa [https://frontlinegenomics.com/crispra-therapeutic-applications/]