The Double-Edged Sword: Balancing SOX9 Inhibition in Cancer with Tissue Repair Side Effects
SOX9 inhibition presents a promising therapeutic strategy for overcoming radioresistance and eradicating cancer stem cells in malignancies like gastrointestinal cancer.
The Double-Edged Sword: Balancing SOX9 Inhibition in Cancer with Tissue Repair Side Effects
Abstract
SOX9 inhibition presents a promising therapeutic strategy for overcoming radioresistance and eradicating cancer stem cells in malignancies like gastrointestinal cancer. However, this approach carries significant risks of impairing critical tissue repair mechanisms. This article synthesizes current evidence demonstrating that SOX9 suppression compromises stem cell functionality in skin wound healing, intestinal epithelium regeneration, cartilage maintenance, and vascular integrity. We explore methodological approaches for targeted inhibition, strategies to mitigate adverse effects, and comparative analyses across tissue types. For researchers and drug development professionals, this comprehensive review highlights the crucial balance between therapeutic efficacy and tissue toxicity, providing a framework for developing safer, more precise SOX9-targeted therapies.
SOX9's Essential Roles in Tissue Homeostasis and Regeneration
Molecular Characteristics of SOX9
What are the key structural features that enable SOX9's function as a transcription factor?
SOX9 is a 509-amino acid protein containing several functionally critical domains that facilitate its role as a transcription factor. The High Mobility Group (HMG) box domain is the defining feature that enables sequence-specific DNA binding to the consensus motif (A/T)(A/T)CAA(A/T)G, bending DNA into an L-shaped complex and altering target gene expression. Other essential domains include: the dimerization domain (DIM) located upstream of the HMG domain that facilitates formation of homo- and heterodimers with other SOXE proteins; two transcriptional activation domains (TAM in the middle and TAC at the C-terminus) that interact with cofactors to enhance transcriptional activity; and a proline/glutamine/alanine (PQA)-rich domain that stabilizes the protein and enhances transactivation capabilities [1] [2] [3].
How is SOX9 activity regulated at the molecular level?
SOX9 undergoes extensive post-translational modifications that regulate its stability, intracellular localization, and transcriptional activity. Key regulatory mechanisms include phosphorylation by protein kinase A (PKA) at serine residues S64 and S181, which enhances DNA-binding affinity and promotes nuclear translocation. SUMOylation can either enhance or repress SOX9 transcriptional activity depending on cellular context. Additionally, the ubiquitin-proteasome pathway degrades SOX9 in specific cell types like hypertrophic chondrocytes, and microRNAs post-transcriptionally inhibit SOX9 expression during lung development, chondrogenesis, and neurogenesis [2]. SOX9 typically functions by forming complexes with partner transcription factors, and its transcriptional output depends on both the specific binding sites and cofactors recruited in different cellular contexts [2].
SOX9 in Development and Stem Cell Biology
How does SOX9 function as a pioneer factor in cell fate determination?
Recent research has established SOX9 as a bona fide pioneer factor capable of binding to cognate motifs in closed chromatin and initiating cell fate switching. In skin reprogramming models, SOX9 binds to closed chromatin at hair follicle stem cell enhancers within one week of induction, before nucleosome displacement and chromatin opening occur. This pioneering activity enables SOX9 to divert embryonic epidermal stem cells into becoming hair follicle stem cells by simultaneously activating new enhancers while indirectly silencing previous epidermal enhancers through competition for limited epigenetic co-factors [4]. This fate-switching capability demonstrates SOX9's powerful role in developmental reprogramming.
What is SOX9's role in intestinal stem cell maintenance?
In the intestinal epithelium, SOX9 functions as a downstream target of Wnt signaling and helps maintain Wnt-dependent intestinal progenitors. SOX9 expression follows a gradient increasing from duodenum to distal colon and is restricted to the proliferative crypt zone in adults. It acts to repress differentiation genes including Cdx2 and Muc2, thereby maintaining progenitor cells in an undifferentiated state. Conditional inactivation studies demonstrate that SOX9 loss increases crypt cell proliferation and elevates expression of Wnt target genes cMYC and Cyclin D1, confirming its importance in intestinal stem cell regulation [5].
SOX9 in Tissue Repair and Regeneration
How does SOX9 contribute to regeneration after tissue injury?
SOX9-expressing cells demonstrate significant regenerative capacity across multiple tissue types. In radiation-induced lung injury models, SOX9-expressing cells promote regeneration of lung tissues, and their ablation leads to severe phenotypes after radiation damage. Lineage tracing in Sox9CreER; RosatdTomato mice revealed that SOX9+ cells are indispensable for repair and reconstruction following injury, with the PI3K/AKT pathway identified as a key mechanism mediating this regenerative effect [6]. Similarly, in cartilage and inflamed tissues, SOX9 helps maintain macrophage function and contributes to cartilage formation and tissue repair [1].
What role does SOX9 play in the balance between regeneration and fibrosis?
SOX9 appears to function as a "double-edged sword" in tissue repair, playing roles in both regenerative processes and pathological fibrosis. While SOX9 promotes regeneration in various contexts, its persistent activation can drive fibrotic processes in multiple organs including cardiac, liver, kidney, and pulmonary fibrosis [3]. In tracheal fibrosis models, SOX9 knockdown alleviates fibrosis by inhibiting granulation tissue proliferation, reducing inflammation and ECM deposition, and promoting apoptosis of granulation tissue. This fibrotic activity operates through the Wnt/β-catenin-SOX9 axis, with inhibition of SOX9 significantly reducing tracheal fibrosis after injury [7].
Experimental Protocols for SOX9 Research
Genetic Lineage Tracing of SOX9-Expressing Cells
Purpose: To track the fate and contribution of SOX9-expressing cells in development, homeostasis, and regeneration.
Detailed Methodology:
- Utilize Sox9CreER transgenic mice (available from Jackson Laboratory) crossed with appropriate reporter lines (e.g., RosatdTomato or RosaEYFP)
- Administer tamoxifen (Sigma, T5648-1G) via intraperitoneal injection at 0.08 mg/g body weight daily for three consecutive days to activate Cre recombinase
- Allow appropriate chase periods depending on research question (days to weeks)
- Induce tissue injury if studying regeneration (e.g., radiation injury using 16 Gy targeted thoracic radiation for lung injury models)
- Collect tissues at predetermined endpoints (e.g., 3, 7, 14, and 30 days post-injury)
- Process tissues for histological analysis, immunofluorescence, or flow cytometry to quantify SOX9-lineage cell contributions to regeneration [6]
SOX9 Knockdown in Fibrosis Models
Purpose: To investigate SOX9 function in fibrotic processes and evaluate its therapeutic potential.
Detailed Methodology:
- Establish tracheal fibrosis model in rats using tracheal brushing injury
- Implement SOX9 knockdown using siRNA or shRNA approaches
- Monitor fibrotic progression through histological analysis (H&E, Masson's trichrome staining)
- Assess expression of mesenchymal and ECM markers (collagen, α-SMA) via immunohistochemistry or Western blot
- Evaluate Wnt/β-catenin pathway activity by measuring β-catenin and p-GSK3β levels
- Quantify functional outcomes including granulation tissue area, epithelial regeneration, and apoptosis rates (TUNEL assay) [7]
Table 1: SOX9 Expression Across Biological Contexts
| Biological Context | SOX9 Expression Level | Functional Outcome | Key Regulatory Pathways |
|---|---|---|---|
| Intestinal Adenomas | Significantly upregulated | Impaired differentiation, cancer initiation | WNT/β-catenin [8] |
| Ovarian Cancer (Post-Chemo) | Consistently increased | Chemoresistance, stem-like state | Super-enhancer mediated epigenetic regulation [9] |
| Radiation-Induced Lung Injury | Elevated during repair | Tissue regeneration, stem cell activation | PI3K/AKT [6] |
| Tracheal Fibrosis | Markedly upregulated | ECM deposition, fibrosis progression | Wnt/β-catenin-SOX9 axis [7] |
| Normal Adult Lung | Sparse in bronchi, minimal in alveoli | Tissue homeostasis | Baseline maintenance [6] |
Troubleshooting Common SOX9 Research Challenges
Why might SOX9 inhibition produce conflicting results in different tissue repair models?
The conflicting effects of SOX9 inhibition stem from its context-dependent dual functions. In regenerative contexts like radiation-induced lung injury, SOX9 inhibition compromises repair, while in fibrotic diseases, it alleviates pathology. This dichotomy arises because SOX9 regulates both positive regenerative processes and pathological extracellular matrix deposition. Researchers should carefully consider the specific biological context, timing of intervention, and SOX9's differential interaction with signaling pathways (e.g., PI3K/AKT in regeneration vs. Wnt/β-catenin in fibrosis) when interpreting inhibition experiments [1] [6] [7].
How can researchers account for SOX9's complex regulation in experimental design?
SOX9 is regulated at multiple levels including transcriptionally, post-transcriptionally via miRNAs, and through extensive post-translational modifications. To comprehensively assess SOX9 activity, researchers should:
- Monitor both mRNA and protein levels, as discrepancies can indicate post-transcriptional regulation
- Analyze phosphorylation status (particularly S64 and S181) when investigating PKA-mediated regulation
- Consider using multiple detection methods (IHC, IF, Western) due to potential epitope masking from modifications
- Include controls for SOX9 dimerization state and partner transcription factors that significantly influence its activity [2]
What technical considerations are crucial for accurate SOX9 detection and quantification?
SOX9's nuclear localization and modification status present specific technical challenges. For immunohistochemistry, heat-induced epitope retrieval is essential, and antibody validation using SOX9-deficient controls is critical. For flow cytometry, nuclear extraction protocols may improve detection. When quantifying SOX9 in fibrosis models, IHC scoring should account for both intensity (0-3+) and percentage of positive cells, with the final score calculated as the product of these values [6]. Researchers should also be aware that SOX9 expression patterns can be highly compartmentalized, as seen in the intestinal crypt and tracheal epithelium.
Research Reagent Solutions
Table 2: Essential Research Reagents for SOX9 Studies
| Reagent/Catalog Number | Application | Key Features | Experimental Considerations |
|---|---|---|---|
| Sox9CreER mice (JAX Stock) | Lineage tracing | Inducible Cre expression from Sox9 locus | Tamoxifen dose and timing critical for specific labeling [6] |
| Anti-SOX9 (Millipore AB5535) | IHC/IF | Well-validated for paraffin sections | Optimal at 1:200 dilution; requires antigen retrieval [6] |
| siRNA/SOX9 pools | Knockdown studies | Efficient SOX9 suppression | Validate efficiency and monitor off-target effects [7] |
| Perifosine (Beyotime SC0227) | Pathway inhibition | AKT inhibitor for PI3K/AKT studies | Use 250 mg/kg/week in mouse models [6] |
| SC79 (Beyotime SF2730) | Pathway activation | AKT pathway agonist | Use 5 mg/kg/week in mouse models [6] |
Signaling Pathway Diagrams
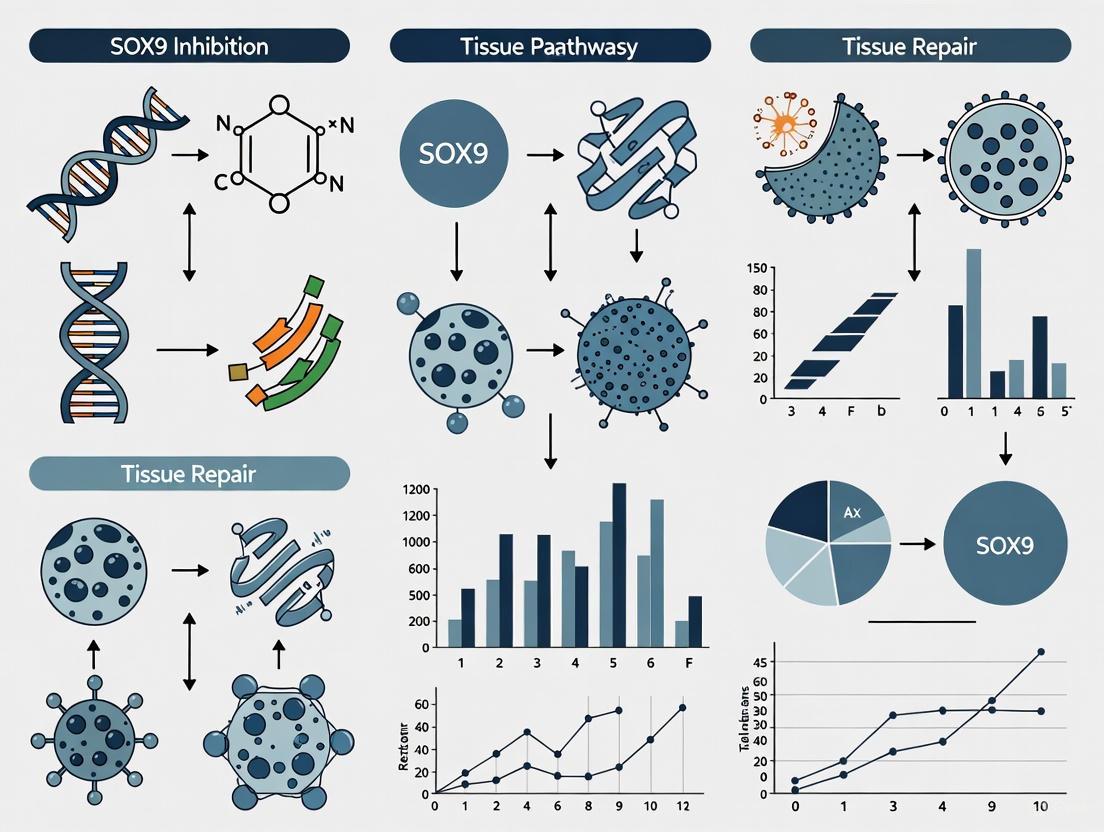
Figure 1: SOX9 in Wnt/β-catenin Signaling Pathway. This diagram illustrates the positive feedback loop between SOX9 and Wnt signaling, showing how SOX9 both responds to and enhances pathway activity through GSK3β phosphorylation and β-catenin stabilization, ultimately driving proliferation and ECM gene expression in fibrosis and cancer contexts [8] [7].
Figure 2: SOX9 in PI3K/AKT-Mediated Regeneration. This diagram shows how SOX9-expressing cells activate the PI3K/AKT pathway to promote both proliferation and proper differentiation, ultimately driving tissue regeneration following injury as demonstrated in radiation-induced lung injury models [6].
Molecular Anatomy of the SOX9 Protein
SOX9 is a transcription factor characterized by several key functional domains that enable its diverse roles in cellular regulation. The protein structure includes a high-mobility group (HMG) box domain responsible for sequence-specific DNA binding, a dimerization domain (DIM), two transcriptional activation domains (TAM and TAC), and a proline/glutamine/alanine (PQA)-rich domain [1] [10]. The HMG domain facilitates DNA binding and induces significant bending by forming an L-shaped complex in the minor groove of DNA, while the transactivation domains interact with transcriptional co-activators to regulate gene expression [2] [10].
Regulatory Mechanisms: SOX9 undergoes extensive post-transcriptional modifications that influence its stability, localization, and activity. These include phosphorylation by protein kinase A (PKA) which enhances DNA-binding affinity and promotes nuclear translocation, and SUMOylation which context-dependently either enhances or represses SOX9-dependent transcription [2]. The ubiquitin-proteasome pathway also regulates SOX9 by degrading it in specific cellular contexts, while various microRNAs target SOX9 transcripts to control its expression [2].
Key Signaling Pathways Regulated by SOX9
SOX9 interacts with multiple critical signaling pathways to control cellular processes, with its functional outcomes depending on cellular context and binding partners.
Pathway-Specific Mechanisms: In the Wnt/β-catenin pathway, SOX9 directly interacts with β-catenin to inhibit its transcriptional activity during chondrocyte differentiation [2]. SOX9 also serves as a significant genetic target downstream of AKT signaling, where it promotes AKT-dependent tumor growth in triple-negative breast cancer by regulating SOX10 expression [11]. Through these interactions, SOX9 occupies a central position in coordinating multiple signaling outputs that determine cellular fate.
SOX9 in Cellular Proliferation and Cell Cycle Control
SOX9 exerts significant control over cellular proliferation through direct regulation of cell cycle progression and apoptotic pathways. In triple-negative breast cancer (TNBC) cells, SOX9 knockdown resulted in suppressed cell proliferation and colony formation, with apoptosis increased and the cell cycle arrested at the G0/G1 phase [12]. This demonstrates SOX9's critical role in maintaining continuous cell cycle progression.
Quantitative Effects of SOX9 Manipulation on Proliferation:
Table 1: SOX9 Knockdown Effects on Cancer Cell Proliferation
| Cell Type | Intervention | Proliferation Outcome | Cell Cycle Effects | Apoptosis Changes | Citation |
|---|---|---|---|---|---|
| TNBC (MDA-MB-231) | SOX9 inhibition | Suppressed | G0/G1 phase arrest | Increased | [12] |
| TNBC (MDA-MB-436) | SOX9 inhibition | Suppressed | G0/G1 phase arrest | Increased | [12] |
| HGSOC | SOX9 knockout | Increased platinum sensitivity | Accelerated growth rate without chemotherapy | Not specified | [9] |
| Breast cancer (T47D) | SOX9 involvement | Antiproliferative | G0/G1 blockage | Not specified | [11] |
Molecular Mechanisms: SOX9 promotes proliferation through multiple mechanisms, including direct interaction with and activation of the polycomb group protein Bmi1 promoter, which suppresses the activity of the tumor suppressor InK4a/Arf sites [11]. SOX9 also collaborates with Slug (SNAI2) to encourage breast cancer cell proliferation and metastasis, and serves as a target for miR-215-5p, where SOX9 overexpression can reverse the miR's inhibitory effects on BC cell growth [11].
SOX9-Mediated Regulation of Migration and Invasion
SOX9 significantly enhances cellular migration and invasion capabilities across multiple cancer types. In TNBC models, Transwell and wound-healing assays demonstrated that SOX9 inhibition markedly decreased the migration and invasion of MDA-MB-231 and MDA-MB-436 cells [12]. This establishes SOX9 as a potent driver of metastatic behavior in aggressive cancers.
Migration and Invasion Mechanisms: SOX9 regulates the expression of motility-related genes and facilitates epithelial-to-mesenchymal transition. In colorectal cancer, the lncRNA MALAT1/miR-145/SOX9 axis plays a critical role in regulating cancer cell invasion and migration, with SOX9 upregulation promoting these aggressive behaviors [13]. SOX9 also interacts with various components of the tumor microenvironment, including cancer-associated fibroblasts and tumor-associated macrophages, to create conditions favorable for invasion and metastasis [11].
SOX9 in Cell Survival and Death Decisions
SOX9 plays a complex role in determining cell fate, influencing decisions between survival, apoptosis, and chemoresistance. In TNBC models, SOX9-knockdown cells showed increased apoptosis, indicating that SOX9 normally functions to promote survival pathways [12]. Additionally, SOX9 expression induces significant resistance to platinum-based chemotherapy in high-grade serous ovarian cancer (HGSOC) [9].
Chemoresistance Mechanisms: SOX9 drives chemoresistance through multiple pathways. It increases transcriptional divergence, reprogramming the transcriptional state of naive cells into a stem-like state that is more resistant to chemotherapy [9]. SOX9 expression is epigenetically upregulated following chemotherapy treatment, and this upregulation induces the formation of a stem-like subpopulation with significant chemoresistance capabilities in vivo [9]. In ovarian cancer, single-cell analysis revealed that chemotherapy treatment results in rapid population-level induction of SOX9 that enriches for this stem-like transcriptional state [9].
Table 2: SOX9 in Cancer Survival and Chemoresistance
| Cancer Type | Survival Function | Chemoresistance Role | Mechanism | Clinical Correlation | Citation |
|---|---|---|---|---|---|
| HGSOC | Promotes cell survival | Drives platinum resistance | Transcriptional reprogramming to stem-like state | High SOX9 = shorter survival | [9] |
| Breast Cancer | Prevents apoptosis | Not specified | Regulation of apoptotic pathways | Not specified | [12] [11] |
| Multiple Cancers | Maintains stem cell populations | Confers multidrug resistance | Immune evasion, stress response | Poor prognosis | [1] [11] |
Experimental Protocols for SOX9 Research
SOX9 Knockdown Using Lentiviral Vectors
Protocol Objective: To achieve stable knockdown of SOX9 in cancer cell lines to study its functional roles.
Materials:
- Lentivirus vector pGCSIL-GFP (or similar)
- shRNA sequences targeting SOX9
- 293T cells for virus packaging
- Lipofectamine 2000 transfection reagent
- Target cells (e.g., MDA-MB-231, MDA-MB-436)
Methodology:
- Design and clone SOX9-targeting shRNA sequences into lentivirus vector
- Example sequences: shSOX9-1: 5′-GCATCCTTCAATTTCTGTATA-3′; shSOX9-2: 5′-GCGGAGGAAGTCGGTGAAGAA-3′ [12]
- Co-transfect expression plasmid with helper plasmids into 293T cells using Lipofectamine 2000
- Harvest lentiviruses at 48 and 72 hours post-transfection
- Infect target cells using multiplicity of infection (MOI) of 20
- Assess knockdown efficiency after 72 hours via RT-qPCR or Western blot
Validation Assays:
- Cell Counting Kit-8 (CCK-8) assay for proliferation
- Colony formation assay (14-day culture)
- Flow cytometry for cell cycle and apoptosis analysis
- Transwell and wound-healing assays for migration/invasion [12]
CRISPR-dCas9 System for SOX9 Activation
Protocol Objective: To precisely activate SOX9 expression without permanent genomic changes.
Materials:
- Lenti-dSpCas9-VP64 vector for CRISPR activation
- Lenti-EGFP-dual-gRNA vector for guide RNA expression
- SOX9-targeting sgRNAs
- Bone marrow stromal cells (BMSCs) or other target cells
Methodology:
- Design sgRNAs targeting SOX9 promoter region
- Example: Sox9-1: GAGCTAGCCGTGATTGGCCCG; Sox9-2: CGGGTTGGGTGACGAGACAGG [14]
- Co-express dSpCas9-VP64 and sgRNAs in target cells
- Validate SOX9 upregulation via RT-qPCR and Western blot
- Assess functional outcomes: chondrogenic potential, gene expression changes
Applications: This system enables fine-tuning of SOX9 expression to desired levels, useful for studying its role in differentiation and disease models [14].
Essential Research Reagents and Tools
Table 3: Key Research Reagents for SOX9 Studies
| Reagent/Tool | Specific Example | Function/Application | Experimental Use |
|---|---|---|---|
| SOX9 shRNAs | shSOX9-1, shSOX9-2, shSOX9-3 | Gene knockdown | Lentiviral-mediated SOX9 silencing [12] |
| CRISPR-dCas9 System | dSpCas9-VP64, SOX9 sgRNAs | Gene activation | Precise SOX9 upregulation [14] |
| Cell Viability Assay | Cell Counting Kit-8 (CCK-8) | Proliferation measurement | Quantifying cell growth after SOX9 manipulation [12] |
| Migration Assay | Transwell chambers | Migration/invasion assessment | Studying metastatic potential [12] |
| Colony Formation Assay | Giemsa staining | Clonogenic potential | Measuring long-term proliferation capacity [12] |
| Apoptosis Assay | Flow cytometry with Annexin V | Cell death quantification | Determining survival effects of SOX9 [12] |
Frequently Asked Questions (FAQs)
Q1: Why does SOX9 appear to have contradictory roles in different cancer types?
A1: SOX9 exhibits context-dependent functions based on cell type, signaling environment, and interacting partners. While typically oncogenic, it can display tumor-suppressive activity in specific contexts. This functional duality arises from SOX9's ability to interact with different partner transcription factors and recruit either co-activators or repressors depending on the cellular context [1] [2].
Q2: What are the most reliable methods for detecting SOX9 functional activity in cells?
A2: Combine multiple approaches: (1) Quantitative PCR and Western blot for expression levels; (2) Functional assays (CCK-8, colony formation) for proliferation; (3) Transwell and wound-healing for migration/invasion; (4) Flow cytometry for cell cycle and apoptosis analysis. Validation should include both gain-of-function and loss-of-function approaches [12] [9].
Q3: How does SOX9 contribute to chemoresistance, and can this be targeted therapeutically?
A3: SOX9 drives chemoresistance through multiple mechanisms: (1) Promoting a stem-like transcriptional state; (2) Increasing transcriptional plasticity; (3) Enhancing DNA damage repair pathways; (4) Activating survival signaling networks. Targeting SOX9 directly remains challenging, but upstream regulators (e.g., miRNAs) or downstream effectors may provide alternative therapeutic avenues [9] [11].
Q4: What considerations are important when studying SOX9 in tissue repair versus cancer contexts?
A4: Key considerations include: (1) SOX9 expression duration (transient in repair vs. sustained in cancer); (2) Cellular context (stem/progenitor cells in repair vs. transformed cells in cancer); (3) Microenvironment interactions; (4) Dose-dependent effects. In tissue repair, SOX9 promotes beneficial outcomes like cartilage maintenance, while in cancer these same proliferative and survival functions drive pathology [15] [14].
Technical Troubleshooting Guide
Problem: Inconsistent SOX9 knockdown results across experiments.
- Potential Cause: shRNA off-target effects or inefficient viral transduction
- Solution: Use multiple distinct shRNAs to confirm phenotype specificity; optimize viral titer and transduction conditions; include rescue experiments with SOX9 cDNA resistant to shRNA targeting
Problem: Poor cell viability following SOX9 manipulation.
- Potential Cause: Excessive SOX9 suppression affecting essential cellular functions
- Solution: Titrate knockdown/knockout conditions; use inducible systems for temporal control; consider cell-type specific SOX9 dependencies
Problem: Discrepancy between SOX9 mRNA and protein expression measurements.
- Potential Cause: Post-transcriptional regulation or protein stability issues
- Solution: Implement protein degradation inhibitors if necessary; check for miRNA regulation; ensure antibody specificity in Western blots
Problem: Variable migration/invasion assay results with SOX9 modulation.
- Potential Cause: Microenvironmental factors or assay condition inconsistencies
- Solution: Standardize matrix composition in invasion assays; control for serum concentration in chemotaxis; use multiple complementary migration assays
FAQs: SOX9 in Intestinal Biology and Radiotherapy
Q1: What is the functional difference between SOX9-high and LGR5-high intestinal stem cells? SOX9-high cells represent a quiescent, radioresistant reserve intestinal stem cell (rISC) population, while LGR5-high cells represent active, proliferating intestinal stem cells (aISCs). Under homeostatic conditions, SOX9-high cells are slow-cycling and function as a reserve pool. Following injury, such as high-dose irradiation, these rISCs can convert into aISCs to drive epithelial regeneration. The loss of SOX9 function leads to the depletion of these label-retaining cells and dramatically increases intestinal sensitivity to radiation damage [16] [17].
Q2: Our research indicates that SOX9 inhibition could be a promising radiosensitization strategy for cancer. What is a critical consideration for this therapeutic approach? A critical consideration is the dual role of SOX9. While inhibiting SOX9 may sensitize tumor cells to radiation, it can simultaneously impair the regenerative capacity of healthy tissues. SOX9 is essential for maintaining reserve stem cells and promoting tissue repair in the intestinal epithelium. Therefore, a key research challenge is developing targeted inhibition strategies that affect cancerous tissue without compromising the intrinsic radioresistance and repair mechanisms of normal tissues, such as those in the intestine [16] [1] [17].
Q3: What are the primary molecular mechanisms by which SOX9 confers radioresistance? Evidence suggests that SOX9-dependent radioresistance is not primarily attributed to enhanced DNA repair or cell cycle arrest. Instead, research in mouse models indicates that SOX9 limits proliferation in reserve stem cells, maintaining them in a quiescent or slow-cycling state that is inherently more resistant to radiation-induced damage. The exact downstream pathways are under investigation, but this control of proliferative status is a key mechanism [16] [17].
Experimental Protocols: Key Methods for Investigating SOX9 Function
Protocol 1: Isolating and Characterizing Reserve Intestinal Stem Cells
This protocol is adapted from methodologies used to demonstrate that SOX9-high cells are label-retaining, radioresistant rISCs [16] [17].
Label-Retention Assay (LRC Identification):
- Administration: Utilize transgenic mice (e.g., histone 2B-YFP) or implant subcutaneous osmotic minipumps to deliver nucleotide analogs like EdU (5-ethynyl-2’-deoxyuridine) or BrdU over a sustained period (e.g., 7-14 days).
- Washout: Remove the pump or stop administration and allow a chase period of 8-12 days for the label to be diluted from rapidly dividing cells.
- Identification: Quiescent or slow-cycling rISCs will retain the label and can be identified as Label-Retaining Cells (LRCs) via immunohistochemistry or flow cytometry.
Cell Sorting and Single-Cell Analysis:
- Mouse Models: Use reporter mice such as
Lgr5-EGFPandSox9-EGFP. - Tissue Processing: Dissociate jejunal crypts into single-cell suspensions.
- Fluorescence-Activated Cell Sorting (FACS): Isulate distinct populations:
Lgr5(high)(aISCs) andSox9(high)(rISCs). - Single-Cell Gene Expression: Use an integrated microfluidics platform (e.g., Fluidigm C1 system) to perform quantitative PCR on single cells for a panel of genes, including aISC markers (
Lgr5,Ascl2), rISC markers (Bmi1,Hopx,Lrig1), and lineage differentiation markers.
- Mouse Models: Use reporter mice such as
Protocol 2: Lineage Tracing and Functional Regeneration Assay
This protocol tests the stem cell capacity and radioresistance of SOX9-expressing cells in vivo [16] [17].
Genetic Lineage Tracing:
- Mouse Model: Use
Sox9-CreERT2mice crossed with a reporter line (e.g.,ROSA26-loxP-STOP-loxP-tdTomato). - Induction: Administer tamoxifen (e.g., 2 mg intraperitoneally) to activate Cre recombinase and indelibly label SOX9-expressing cells and their progeny with tdTomato.
- Analysis: Track the lineage over time to assess multipotency and contribution to epithelial regeneration.
- Mouse Model: Use
Radiation Injury Model:
- Treatment: Expose
SOX9knockout mice and control littermates to a high dose of irradiation (e.g., 12-14 Gy). - Assessment:
- Crypt Survival: Quantify the number of regenerating crypts per intestinal circumference 3-5 days post-irradiation.
- Cell Death: Analyze apoptosis levels (e.g., by TUNEL staining) shortly after irradiation.
- Proliferation: Assess cell cycle re-entry and proliferation during the regenerative phase (e.g., by EdU pulse or Ki-67 staining).
- Treatment: Expose
Table 1: Key Findings from SOX9 Knockout Studies in Mouse Intestine
| Experimental Readout | Observation in SOX9-KO vs. Control | Experimental Model |
|---|---|---|
| Label-Retaining Cells (LRCs) | Significantly lost or reduced [16] [17] | Inducible SOX9 knockout mice |
| Crypt Regeneration Post-Irradiation | Severely impaired [16] [17] | Conditional SOX9 knockout mice after high-dose irradiation |
| Radiation Sensitivity | Markedly increased [16] [17] | Crypt survival assay in SOX9 knockout mice |
| Proliferation in LRCs | Dysregulated / Increased [16] | EdU/Ki-67 staining in label-retaining, SOX9-high cells |
| Single-Cell Marker Co-expression | A subset of crypt-based Sox9(high) cells co-express Lgr5, Bmi1, Lrig1, and Hopx [16] |
FACS-isolated Sox9(high) cells from reporter mice |
Table 2: Essential Research Reagents for SOX9 Functional Studies
| Reagent / Tool | Function and Application | Example Use Case |
|---|---|---|
Sox9-EGFP Reporter Mouse |
Enables identification and fluorescence-activated cell sorting of SOX9-expressing cells [16] | Isolating pure populations of Sox9(high) and Sox9(low) intestinal epithelial cells for transcriptomic analysis. |
Sox9-CreERT2 Mouse Line |
Allows for inducible, lineage-specific genetic manipulation or lineage tracing of SOX9-expressing cells [16] [17] | Tracing the fate of SOX9+ cells during homeostasis or after injury via tamoxifen-induced activation. |
Conditional Sox9 Allele (Sox9fl/fl) |
Enables tissue-specific or inducible knockout of SOX9 when crossed with appropriate Cre drivers [16] [18] | Generating intestinal-epithelial specific SOX9 knockout mice (Sox9fl/fl;VillinCre or VillinCreERT2) to study gene function. |
Lgr5-EGFP Reporter Mouse |
Serves as a benchmark for identifying active intestinal stem cells (aISCs) for comparative studies [16] | Directly comparing gene expression profiles and functional properties of Sox9(high) rISCs versus Lgr5(high) aISCs. |
Signaling Pathways and Experimental Workflows
Figure 1: SOX9 Regulation and Function in Reserve Intestinal Stem Cells. SOX9 expression is activated by the Wnt/β-catenin/TCF4 pathway. It maintains a quiescent, slow-cycling state in reserve ISCs, limiting proliferation and conferring radioresistance. Upon radiation injury, these SOX9-high rISCs can convert to an active state to drive epithelial regeneration [16] [19] [17].
Figure 2: Experimental Workflow for Characterizing SOX9 Function. A typical integrated approach to study SOX9, combining cell sorting and omics analysis with in vivo lineage tracing and functional knockout models to define its role in stem cell biology and radioresistance [16] [17].
Technical Troubleshooting Guides
SOX9 Knockdown Efficiency Issues
Problem: Inconsistent SOX9 knockdown in human umbilical cord mesenchymal stem cells (HUC-MSCs) using lentiviral vectors.
Solution:
- Verify Viral Titer: Confirm lentivirus concentration exceeds 1x10^8 TU/mL before transduction.
- Optimize MOI: Perform multiplicity of infection (MOI) gradient test (e.g., MOI 10-50) using scramble shRNA control.
- Selection Pressure: Apply 1 μg/mL puromycin selection for 15 days with doxycycline induction (80 μg/mL) for shRNA expression [20].
- Validation: Always confirm knockdown via qRT-PCR and Western blot before functional assays.
Prevention: Use fresh viral aliquots; maintain consistent cell passage numbers (P3-P4); include positive and negative controls in all experiments.
Poor HUC-MSC Migration in Transwell Assays
Problem: Reduced migratory capacity of SOX9-deficient HUC-MSCs in Transwell migration assays.
Solution:
- Cell Preparation: Use low-glucose DMEM with 10% FBS; ensure cell viability >95% before assay.
- Proper Seeding: Seed 1×10^5 cells/well in top chamber with 8-μm pores; serum-starve for 4-6 hours prior to assay.
- Fixation & Staining: Fix migrated cells with 4% paraformaldehyde for 15 minutes; stain with 0.1% crystal violet for 20 minutes [20].
- Quantification: Count cells in six random visual fields under 100x magnification.
Troubleshooting: Check FBS concentration in lower chamber as chemoattractant (5-10%); verify pore size not clogged; ensure consistent incubation time (typically 6-24 hours).
Inconsistent In Vivo Burn Healing Results
Problem: Variable repair outcomes in rat burn models with SOX9-modified HUC-MSCs.
Solution:
- Standardize Burn Model: Use consistent deep second-degree burn creation method; control for burn depth histologically.
- Cell Delivery: Apply 1-2x10^6 HUC-MSCs per burn site in PBS buffer; use consistent delivery method (topical vs. injection).
- Timing: Begin treatment within 2 hours post-burn for optimal effect [20].
- Control Groups: Include shSOX9-transfected HUC-MSCs, sh-control transfected HUC-MSCs, and PBS-only groups.
Monitoring: Assess healing daily; measure wound contraction; collect tissue samples at multiple time points for histological analysis of Ki67, CK14, and CK18 expression [20].
Frequently Asked Questions (FAQs)
Q1: What is the molecular rationale for targeting SOX9 in burn wound healing?
A1: SOX9 serves as a master regulator of mesenchymal stem cell function. Knockdown studies demonstrate that SOX9 depletion inhibits HUC-MSC proliferation and migration, reduces expression of critical cytokines (IL-6, IL-8), growth factors (GM-CSF, VEGF), and stemness-related genes (OCT4, SALL4). This directly impairs burn repair capacity and accessory structure regeneration (hair follicles, glands) [20].
Q2: How does SOX9 influence cutaneous regeneration versus fibrosis?
A2: SOX9 exhibits dual functionality. In physiological regeneration, SOX9 promotes proper tissue patterning and accessory structure formation. However, in pathological contexts, SOX9 drives endothelial-to-mesenchymal transition (EndMT), contributing to excessive fibrosis and scarring. Conditional knockout of Sox9 in murine endothelium significantly reduces pathological EndMT and scar area [21].
Q3: What are the key downstream effectors of SOX9 in wound healing?
A3: Key downstream mediators include:
- Cytokines/Growth Factors: IL-6, IL-8, GM-CSF, VEGF
- Stemness Markers: OCT4, SALL4
- Proliferation Markers: Ki67
- Differentiation Markers: CK14, CK18 for epithelial lineages [20]
Q4: Which signaling pathways interact with SOX9 during tissue repair?
A4: SOX9 interacts with multiple pathways:
- Wnt/β-catenin: HUC-MSC exosomes activate β-catenin signaling via Wnt4 [20]
- Notch Pathway: Antagonistic relationship with Rbpj; Rbpj deletion enhances Sox9 and EndMT [21]
- Hedgehog Signaling: Upregulates Sox9 expression in pathological EndMT [21]
- NF-κB Pathway: Positively regulates SOX9 expression in chondrogenesis [22]
Q5: What experimental models are best for studying SOX9 in burn repair?
A5: Optimal models include:
- In Vitro: HUC-MSCs with lentiviral SOX9 knockdown for migration/proliferation studies [20]
- In Vivo: Rat deep second-degree burn models with HUC-MSC transplantation [20]
- Genetic Models: Endothelial-specific Sox9 knockout mice (Sox9fl/fl/Cdh5-CreER) for fibrosis analysis [21]
- Therapeutic Testing: Topical siRNA against Sox9 in murine wound models [21]
Table 1: Functional Consequences of SOX9 Knockdown in HUC-MSCs
| Parameter | Effect of SOX9 KD | Experimental Method | Magnitude of Change |
|---|---|---|---|
| Proliferation | Decreased | CCK-8 assay & cell counting | Significant reduction at 24-48h [20] |
| Migration | Impaired | Transwell assay | ~60% reduction vs. control [20] |
| IL-6/IL-8 | Reduced expression | qRT-PCR | Significant downregulation [20] |
| GM-CSF/VEGF | Reduced expression | qRT-PCR | Significant downregulation [20] |
| OCT4/SALL4 | Reduced expression | qRT-PCR | Significant downregulation [20] |
| In Vivo Repair | Impaired | Rat burn model | Poor accessory structure regeneration [20] |
Table 2: SOX9 in Different Experimental Models of Tissue Repair
| Model System | SOX9 Role | Key Findings | Reference |
|---|---|---|---|
| HUC-MSCs + Burn | Pro-repair | Enhances proliferation, migration, cytokine secretion | [20] |
| Endothelial Sox9 KO | Anti-fibrotic | Reduces EndMT and scar area | [21] |
| BMSCs + Nicotine | Chondrogenic | Histone hypo-acetylation suppresses SOX9-mediated repair | [23] |
| Topical Sox9 siRNA | Anti-fibrotic | Blocks pathological EndMT, reduces scarring | [21] |
Signaling Pathway Diagrams
Research Reagent Solutions
Table 3: Essential Research Reagents for SOX9 Studies
| Reagent/Category | Specific Product/Example | Function/Application | Key Details |
|---|---|---|---|
| Cell Source | HUC-MSCs | Primary cell model for repair studies | Isolate from umbilical cord; use P3-P4; culture in low-glucose DMEM + 10% FBS [20] |
| Knockdown System | Lentiviral shSOX9 | SOX9 inhibition | pGPH1/Neo vector; puromycin selection (1 μg/mL, 15 days); doxycycline induction (80 μg/mL) [20] |
| In Vivo Model | Rat burn model | Therapeutic testing | Deep second-degree burns; monitor accessory structure regeneration [20] |
| Detection Antibodies | Anti-Ki67, Anti-CK14, Anti-CK18 | Histological assessment | Evaluate proliferation and differentiation in regenerated tissue [20] |
| SOX9 Inhibitor | Sox9 siRNA | Therapeutic intervention | Topical application reduces scar area by blocking EndMT [21] |
| Analysis Method | qRT-PCR primers for SOX9 targets | Molecular profiling | IL-6, IL-8, GM-CSF, VEGF, OCT4, SALL4 [20] |
Core Concepts: SOX9 in Tissue Homeostasis and Disease
What is the primary function of SOX9 in cartilage, and why is it a target for therapeutic inhibition? SOX9 (SRY-related high-mobility group box gene 9) is a pivotal transcription factor for chondrocyte function. It acts as a master regulator of chondrogenesis by transactivating essential cartilage-specific genes, such as those for type II collagen, and is mandatory for proper cartilage development and repair [24]. In the context of therapeutic inhibition, SOX9 is often targeted in oncology because it is frequently overexpressed in various solid cancers, where it promotes tumor proliferation, metastasis, chemoresistance, and the maintenance of cancer stem-like cells (CSCs). Inhibiting SOX9 is seen as a strategy to eradicate CSCs and sensitize tumors to treatments like radiotherapy [25] [1].
What role does SOX9 play in the vasculature, particularly in smooth muscle and endothelial cells? SOX9 plays a complex and context-dependent role in the vasculature. In Vascular Smooth Muscle Cells (VSMCs), SOX9 drives a phenotypic transformation from a contractile to a synthetic, proliferative state. This transition is a key event in pathologies like in-stent restenosis and vascular aging, where SOX9 promotes neointimal hyperplasia and extracellular matrix (ECM) remodeling [26] [27]. In Endothelial Cells, SOX9 has been identified as an early transcriptional driver of Endothelial-to-Mesenchymal Transition (EndMT). In conditions like atherosclerosis, exposure to oxidized low-density lipoprotein (oxLDL) upregulates SOX9, leading to a loss of endothelial identity and a gain of mesenchymal characteristics in endothelial progenitor cells [28].
What is the central thesis regarding the side effects of SOX9 inhibition on tissue repair? The central thesis is that while SOX9 inhibition holds therapeutic promise, particularly in oncology, it poses a significant risk of impairing vital tissue repair mechanisms. This is because SOX9 is a critical promoter of chondrogenesis for cartilage repair and a regulator of stem/progenitor cell function. Therefore, systemic inhibition of SOX9 may lead to unintended consequences, such as weak cartilage regeneration and impaired healing of endothelial and other tissues, by disrupting these essential physiological processes [23] [25] [28].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 1: Essential Reagents for Investigating SOX9 Biology and Inhibition
| Reagent / Tool | Primary Function / Application | Example from Literature |
|---|---|---|
| siRNA/shSOX9 | Knockdown of SOX9 expression to study loss-of-function phenotypes. | Silencing SOX9 reversed oxLDL-induced EndMT in ECFCs and attenuated neointimal hyperplasia in a rat carotid injury model [28] [27]. |
| Sox9fl-fl / Cdh5CreERt2 Mice | Endothelial-specific, inducible knockout of Sox9 for in vivo lineage tracing and functional studies. | Used to demonstrate that endothelial-specific Sox9 knockout abrogates EndMT in a high-fat diet murine model [28]. |
| α7-nAChR Inhibitor (MLA) | Pharmacological inhibitor used to dissect specific signaling pathways upstream of SOX9. | Methyllycaconitine (MLA) was used to verify that nicotine suppresses SOX9 and chondrogenesis via the α7-nicotinic acetylcholine receptor [23]. |
| Oxidized LDL (oxLDL) | Inducer of EndMT and SOX9 expression in endothelial cell models. | Treatment of ECFCs with oxLDL (12.5-50 µg/mL) induced SOX9 expression and triggered EndMT [28]. |
| Platelet-Derived Growth Factor-BB (PDGF-BB) | Inducer of VSMC phenotypic transformation and proliferation. | Used in vitro to stimulate SOX9 expression and nuclear translocation in primary VSMCs, driving their proliferation and migration [27]. |
| Dual-Luciferase Reporter Assay | Used to validate direct transcriptional regulation by SOX9 on target gene promoters. | Identified that SOX9 directly binds to the STAT3 promoter to enhance its activity in VSMCs [27]. |
Troubleshooting Guide: SOX9 Inhibition in Tissue Repair Research
FAQ 1: We are investigating SOX9 inhibition to sensitize gastrointestinal cancers to radiotherapy, but observe severe toxicity in intestinal models. What could be the mechanism? This is a predicted, on-target side effect. SOX9 is crucial for the function of reserve intestinal stem cells (rISCs), which are responsible for epithelial regeneration and are relatively radioresistant. When SOX9 is inhibited, these rISCs lose their regenerative capacity and undergo apoptosis following radiation exposure, leading to the observed enteritis [25]. Troubleshooting Protocol:
- Confirm On-Target Effect: Use a SOX9 reporter cell line or qPCR to verify that your inhibitor effectively reduces SOX9 transcriptional activity in your intestinal organoid model.
- Assess Functional Regeneration: Perform a crypt regeneration assay ex vivo. Compare the formation of new organoids from single intestinal crypts treated with your SOX9 inhibitor versus control after a sub-lethal dose of radiation (e.g., 8-10 Gy).
- Mitigation Strategy: Consider a localized or targeted delivery system for the SOX9 inhibitor (e.g., nanoparticle-conjugated inhibitors) to minimize exposure to healthy intestinal tissue. Alternatively, explore the temporal administration of SOX9 inducers post-radiation to boost crypt repair [25].
FAQ 2: Our in vivo cartilage repair study shows that a potential therapeutic agent worsens healing. We suspect it inadvertently suppresses SOX9. How can we confirm this and identify the upstream pathway? This mirrors findings where nicotine was shown to weaken cartilage repair by suppressing SOX9. Your investigation should focus on the SOX9 promoter's epigenetic status and its key upstream regulators [23]. Troubleshooting Protocol:
- In Vivo Confirmation: Re-generate your cartilage defect model (e.g., in rat) and administer the therapeutic agent. Perform immunohistochemistry on the regenerated tissue for SOX9 protein levels and key chondrogenic markers (e.g., type II collagen). A concomitant decrease would support your hypothesis.
- In Vitro Mechanism Analysis:
- Model: Use Bone Marrow-derived Mesenchymal Stem Cells (BMSCs) induced to chondrogenically differentiate.
- Treatment: Apply your therapeutic agent at relevant concentrations.
- Upstream Analysis: Measure intracellular Ca2+ levels (e.g., with Fluo-4 AM dye) and calcineurin (CaN) activity using a commercial assay kit. The nicotine study found this pathway activates NFATc2, which suppresses SOX9 [23].
- Epigenetic Analysis: Perform Chromatin Immunoprecipitation (ChIP) with antibodies against NFATc2 and acetylated histones (H3K9ac, H3K14ac) on the SOX9 promoter. A successful pathway inhibition would show increased NFATc2 binding and decreased histone acetylation at the SOX9 promoter.
- Rescue Experiment: Co-treat cells with your agent and a selective inhibitor of the identified upstream pathway (e.g., a calcineurin inhibitor like Cyclosporine A) to see if chondrogenic differentiation can be restored.
FAQ 3: In our model of atherosclerosis, SOX9 inhibition successfully blocks EndMT but also unexpectedly impairs endothelial progenitor self-renewal. Why does this happen? This occurs because SOX9 has distinct, separable functions in the same cell type. In endothelial colony-forming cells (ECFCs), SOX9 activation drives the transcriptional reprogramming of EndMT. However, its basal expression is also involved in regulating the self-renewal capacity of these vessel-resident progenitors. Ablating SOX9 therefore disrupts both pathological transition and essential progenitor maintenance [28]. Troubleshooting Protocol:
- Phenotypic Separation: Use RNA-sequencing and ATAC-sequencing on your SOX9-knockdown ECFCs. Analyze the data to identify gene clusters and chromatin regions specifically associated with the EndMT program (e.g., loss of CD31, gain of α-SMA) versus those governing self-renewal (e.g., cell cycle regulators).
- Functional Assays: Conduct a single-cell colony formation (self-renewal) assay. Compare the ability of control, SOX9-knockdown, and SOX9-overexpressing ECFCs to form high-proliferative potential colonies. This will quantitatively confirm the self-renewal defect.
- Alternative Strategy: Instead of global SOX9 knockout, aim to therapeutically target the specific co-factors or downstream genes that SOX9 recruits to drive EndMT, while sparing its other regulatory functions. The data from Step 1 will be critical for identifying these specific targets.
Experimental Protocols for Key Findings
Protocol 1: Evaluating the Impact of a Compound on SOX9-Mediated Cartilage Repair
This protocol is based on the methodology used to investigate nicotine's effect on SOX9 in cartilage repair [23].
Workflow:
Detailed Steps:
- In Vivo Cartilage Repair Model:
- Create full-thickness cartilage defects in the femoral condyles of rats.
- Transplant BMSCs into the defect site.
- Administer your test compound systemically (e.g., via osmotic minipump) at a clinically relevant dose for a duration sufficient for repair (e.g., 12 weeks). Include vehicle control and untreated groups.
- Analysis: Harvest the repaired tissue. Perform histological scoring (e.g., ICRS score) and immunohistochemistry (IHC) for SOX9 and type II collagen to quantitatively assess repair quality and SOX9 expression.
- In Vitro Chondrogenic Differentiation:
- Isolate and culture BMSCs.
- Induce chondrogenic differentiation in pellet or micromass culture.
- Treat with a dose range of your compound (e.g., 0.1 to 100 µM). Include a positive control for SOX9 suppression (e.g., 10 µM nicotine) and a negative control (vehicle).
- Rescue Experiments: Co-treat with pathway-specific inhibitors, such as Methyllycaconitine (MLA, 10 µM) for α7-nAChR or siRNA against NFATc2.
- Outcome Measures:
- Chondrogenesis: Alcian blue or Safranin O staining for proteoglycans; qPCR for SOX9, COL2A1, ACAN.
- Upstream Signaling: Measure intracellular Ca2+ with fluorescent dyes (e.g., Fluo-4 AM) and calcineurin activity with a colorimetric assay kit.
- Epigenetics: Perform ChIP-qPCR on the SOX9 promoter region using antibodies against acetylated H3K9 and H3K14.
Protocol 2: Dissecting SOX9's Role in Endothelial-Mesenchymal Transition (EndMT)
This protocol is adapted from studies on oxLDL-induced EndMT in endothelial colony-forming cells (ECFCs) [28] [29].
Workflow:
Detailed Steps:
- Cell Culture and Treatment:
- Isolate and culture human ECFCs from cord blood or placenta on collagen-coated flasks in EGM-2 medium.
- Induce EndMT by treating ECFCs with oxLDL (25-50 µg/mL) for 5 days, refreshing media every 2-3 days.
- Genetic Manipulation:
- Transduce ECFCs with lentivirus carrying either shRNA targeting SOX9 (shSOX9) or a SOX9 overexpression (SOX9 OE) construct. Include scrambled shRNA (shSCR) and empty vector controls.
- Select stable pools with puromycin (1 µg/mL for 5 days).
- Phenotypic Characterization:
- Flow Cytometry: Analyze the expression of endothelial (CD31, CD34) and mesenchymal (CD90, α-SMA) surface markers.
- Functional Assays:
- Capillary Formation: Seed cells on Matrigel and quantify tube network formation after 48 hours.
- Migration: Perform a scratch/wound healing assay and measure closure percentage over 24-48 hours.
- Contractility: Use a collagen contraction assay and measure gel area reduction over 72 hours.
- Self-Renewal Assay: This is critical for detecting side effects. FACS-sort single ECFCs into collagen-coated wells. Culture for 14 days, then count and classify colonies based on size: High Proliferative Potential (>500 cells), Low Proliferative Potential (>250 cells), and endothelial clusters (>50 cells).
- Molecular Analysis:
- RNA-seq/ATAC-seq: Perform these assays on control and SOX9-manipulated ECFCs to identify global transcriptional and chromatin accessibility changes driven by SOX9 during EndMT.
Supporting Data & Pathway Diagrams
Table 2: Quantitative Effects of SOX9 Manipulation in Different Tissue Contexts
| Tissue/Cell Type | Intervention | Key Quantitative Outcome | Biological Implication |
|---|---|---|---|
| Cartilage (in vivo rat model) [23] | Nicotine (2 mg/kg/d) | Suppressed SOX9 expression; impaired cartilage repair score. | Nicotine exposure compromises cartilage regeneration via SOX9 downregulation. |
| ECFCs (Endothelial Progenitors) [28] | oxLDL (50 µg/mL) | 3.2-fold reduction in CD34+ cells; 2.2% of cells gained CD90 expression. | oxLDL induces a full EndMT phenotype in progenitor cells. |
| ECFCs (Endothelial Progenitors) [28] | shSOX9 + oxLDL | Reversal of oxLDL-induced EndMT marker shift and morphology. | SOX9 is necessary for executing the oxLDL-induced EndMT program. |
| VSMCs (in vitro) [27] | PDGF-BB + shSOX9 | Suppressed VSMC proliferation and migration. | SOX9 is a critical mediator of VSMC phenotypic transformation. |
| Intestinal Stem Cells [25] | SOX9 knockout + Radiation | Loss of crypt regeneration; increased apoptosis. | SOX9 is essential for the radioresistance and regenerative capacity of reserve intestinal stem cells. |
Integrated Pathway Diagram: SOX9 in Tissue Integrity and Disease This diagram synthesizes the key signaling pathways involving SOX9 in cartilage, vasculature, and stem cells, illustrating both its physiological roles and the potential side effects of its inhibition.
FAQs: Navigating the SOX9 Dual-Role Dilemma in Research
FAQ 1: How can the same transcription factor, SOX9, drive both tissue repair and cancer progression?
SOX9's functional paradox is rooted in context-dependent regulation. Its activity is determined by the cellular niche, its binding partners, and post-translational modifications [30] [2]. In healthy tissue, SOX9 activation is a transient, tightly regulated process essential for regeneration. However, in cancer, this regulation is lost, leading to sustained, constitutive SOX9 expression that drives tumorigenesis and stemness [4]. A key study in kidney injury showed that the fate of a tissue microenvironment—towards scarless repair (SOX9on-off) or fibrosis (SOX9on-on)—depends on the precise dynamics of SOX9 activity [31].
FAQ 2: What are the primary risks of systemic SOX9 inhibition for cancer therapy?
The main risk is the impairment of normal tissue regeneration and repair, particularly in tissues reliant on SOX9-positive stem and progenitor cells. For instance, SOX9 is crucial for the function of reserve intestinal stem cells (rISCs), which are essential for epithelial regeneration following injury, such as radiation exposure [25]. Inhibiting SOX9 could ablate this radioresistant cell population, leading to severe complications like enteritis. Similarly, in osteoarthritis, SOX9 is vital for chondrogenic differentiation and cartilage maintenance [14] [22].
FAQ 3: Which signaling pathways upstream of SOX9 should we monitor in our models?
Your experimental models should closely monitor the key signaling pathways that regulate SOX9 expression and activity. The following table summarizes the major regulators.
| Signaling Pathway | Effect on SOX9 | Relevant Biological Context |
|---|---|---|
| Wnt/β-catenin | Upregulation & Interaction [30] [32] [2] | Hepatocellular Carcinoma, Intestinal Stem Cells |
| NF-κB | Direct transcriptional upregulation [22] [25] | Inflammation, Chondrogenesis, Pancreatic Cancer |
| TGFβ/Smad | Activation [32] | Hepatocellular Carcinoma |
| Hedgehog (Hh) | Upregulation [30] [2] | Chondrogenesis, Liver Fibrosis |
FAQ 4: What are the best practices for detecting meaningful changes in SOX9 activity in vivo?
Beyond measuring mRNA and total protein levels, employ these functional and spatial assessments:
- Assess Functional Output: Monitor well-established downstream targets, such as Osteopontin (OPN) in HCC [32] or Collagen type II (Col2a1) in chondrogenesis [2].
- Perform Temporal Analysis: SOX9's role is defined by its kinetics. Use time-course experiments to distinguish between transient (regenerative) and sustained (oncogenic) expression [31] [4].
- Implement Spatial Context: Use techniques like immunofluorescence or in situ hybridization to determine if SOX9 is expressed in the correct stem/progenitor cell niche and not in aberrant locations [4].
Troubleshooting Guides
Problem 1: Differentiating SOX9's Pro-Regenerative vs. Pro-Oncogenic Functions
Challenge: In an in vivo model, it is difficult to determine whether SOX9 expression is contributing to wound healing or promoting pre-malignant changes.
Solution: Implement a multi-parameter assessment strategy to classify the SOX9-positive cell population.
Solution A: Molecular Phenotyping
- Action: Co-stain for SOX9 with markers of cell fate and proliferation.
- Rationale: Regenerative SOX9 is often associated with differentiation markers (e.g., Col2a1 in cartilage), while oncogenic SOX9 is linked to sustained proliferation markers (e.g., Ki-67) and stemness genes (e.g., Nanog) [32] [4].
Solution B: Temporal Tracking
- Action: Measure SOX9 levels at multiple time points after injury (e.g., days 1, 3, 7, 14).
- Rationale: A peak and subsequent decline in SOX9 suggest a regenerative response. Persistent elevation beyond the normal healing window suggests a potential pathological switch towards a pro-oncogenic state [31] [4].
Problem 2: Overcoming SOX9-Mediated Therapy Resistance
Challenge: Cancer stem cells (CSCs) with high SOX9 expression demonstrate resistance to chemotherapy and radiation [30] [32] [33].
Solution: Target the mechanisms that stabilize SOX9 protein or its downstream effectors.
Solution A: Disrupt SOX9 Protein Stability
- Action: Investigate the inhibition of deubiquitinating enzymes like USP28, which stabilizes SOX9 by preventing its FBXW7-mediated degradation [33].
- Protocol Note: The USP28-specific inhibitor AZ1 has been shown to promote SOX9 degradation and sensitize ovarian cancer cells to PARP inhibitors [33]. Consider co-treatment strategies.
Solution B: Modulate Downstream Pathways
- Action: In SOX9-high cancers, target downstream effector pathways like Wnt/β-catenin [32].
- Rationale: SOX9 regulates key resistance pathways; simultaneous inhibition may overcome inherent treatment resistance.
Key Experimental Data and Protocols
Quantitative Evidence of SOX9's Dual Role
Table 1: SOX9 in Human Cancers - Correlation with Poor Prognosis [30]
| Cancer Type | SOX9 Status | Clinical Correlation |
|---|---|---|
| Hepatocellular Carcinoma | Overexpression | Poor overall survival, Poor disease-free survival |
| Breast Cancer | Overexpression | Promotes metastasis, Poor overall survival |
| Prostate Cancer | Overexpression | High clinical stage, Poor relapse-free survival |
| Colorectal Cancer | Overexpression | Promotes cell proliferation, senescence inhibition, chemoresistance |
Table 2: SOX9 in Regeneration & Tissue Repair
| Experimental Context | SOX9 Function | Key Experimental Finding |
|---|---|---|
| Kidney Injury [31] | Fate Switch | SOX9on-on state linked to fibrosis; SOX9on-off state linked to scarless repair. |
| Intestinal Regeneration [25] | Stem Cell Maintenance | SOX9 knockout reserve intestinal stem cells impaired regeneration after radiation. |
| Osteoarthritis Therapy [14] | Chondrogenesis | CRISPRa-mediated Sox9 activation in MSCs enhanced cartilage repair in a mouse model. |
Detailed Protocol: CRISPR-dCas9 for Modulating SOX9 and NF-κB in MSC Therapy
This protocol is adapted from a study enhancing mesenchymal stromal cell (MSC) therapy for osteoarthritis [14].
1. Objective: To simultaneously activate SOX9 and inhibit RelA (a key NF-κB subunit) in human MSCs to enhance chondrogenic potential and immunomodulatory properties.
2. Materials:
- Lentiviral Vectors:
- Lenti-dSpCas9-VP64 (for transcriptional activation, CRISPRa)
- Lenti-dSaCas9-KRAB (for transcriptional repression, CRISPRi)
- Lenti-EGFP-dual-gRNA vector (to express two guide RNAs)
- Validated sgRNA Sequences [14]:
- For Sox9 activation: Sox9-2:
CGGGTTGGGTGACGAGACAGG; Sox9-3:ACTTACACACTCGGACGTCCC - For RelA inhibition: RelA-1:
CCGAAATCCCCTAAAAACAGA; RelA-3:TGCTCCCGCGGAGGCCAGTGA
- For Sox9 activation: Sox9-2:
- Cell Culture Media: Standard MSC growth medium and chondrogenic differentiation medium.
3. Workflow:
- Cell Preparation: Culture primary human bone marrow-derived MSCs (CD45⁻ population) in standard growth medium.
- Virus Production & Transduction: Package the lentiviral constructs in HEK293T cells. Co-transduce MSCs with the three vectors (dSpCas9-VP64, dSaCas9-KRAB, and the dual-gRNA vector).
- Cell Selection: Use fluorescence-activated cell sorting (FACS) to isolate EGFP-positive cells successfully transduced with the gRNA vector.
- Validation:
- qRT-PCR & Western Blot: Confirm SOX9 upregulation and RelA downregulation.
- In Vitro Chondrogenesis: Pellet transduced MSCs in chondrogenic differentiation medium for 21 days. Analyze via safranin O staining (proteoglycans) and immunostaining for collagen type II.
- In Vivo Application: In a surgical mouse model of OA, administer intra-articular injections of the modified MSCs and monitor cartilage degradation and pain relief compared to control groups.
Research Reagent Solutions
Table 3: Essential Reagents for SOX9 Functional Studies
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| CRISPR-dCas9 Systems (VP64/KRAB) | Precise transcriptional activation (CRISPRa) or interference (CRISPRi) of SOX9. | Enhancing chondrogenic potential of MSCs by fine-tuning SOX9 levels [14]. |
| SOX9 Reporter Vector (e.g., SOX9-EGFP) | FACS-based isolation of SOX9-positive and negative cell populations. | Isolating SOX9+ cancer stem cells from hepatocellular carcinoma cell lines for functional assays [32]. |
| USP28 Inhibitor (e.g., AZ1) | Promotes ubiquitin-mediated degradation of SOX9 protein. | Re-sensitizing ovarian cancer cells to PARP inhibitors by reducing SOX9 stability [33]. |
| OPN (Osteopontin) Measurement | Acts as a surrogate, serum-based marker for SOX9+ CSCs. | Correlating SOX9 activity in HCC tumors with a measurable biomarker in patient blood [32]. |
Signaling Pathway and Experimental Workflow Diagrams
Approaches to SOX9 Inhibition and Assessment of Repair Impairment
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary considerations when choosing between shRNA knockdown and CRISPR-i for inhibiting SOX9 in tissue repair models? The choice depends on the required duration of suppression, the need for reversibility, and potential off-target effects. shRNA knocks down gene expression at the mRNA level, leading to a transient, reversible suppression that is suitable for studying acute effects or essential genes where a complete knockout would be lethal [34]. CRISPR-i, which inhibits transcription at the DNA level, can offer higher specificity and fewer off-targets, but its effect can be more persistent [34]. For SOX9, which has a dual role in promoting cancer stemness but also in tissue regeneration, a reversible system like shRNA might be preferable for initial functional studies to avoid irreversible damage to repair mechanisms [25] [1].
FAQ 2: We are observing inconsistent SOX9 knockdown efficiency with our shRNA constructs. What could be the cause? Inconsistent shRNA efficiency can stem from several factors:
- Off-target effects: shRNA is notorious for sequence-dependent off-target effects. Re-design the shRNA sequence using updated algorithms and validate with multiple constructs targeting different regions of the SOX9 transcript [34].
- Delivery and expression: Ensure your viral delivery system (lentivirus/retrovirus) has high titer and transduction efficiency. Check the promoter in your shRNA vector (e.g., U6 or H1) for proper activity in your specific cell type.
- SOX9 protein stability: The SOX9 protein may have a long half-life. Even with successful mRNA knockdown, protein levels may persist. Allow sufficient time (e.g., 72-96 hours) post-transduction before assessing knockdown and monitor both mRNA (by qRT-PCR) and protein (by immunoblotting) levels.
FAQ 3: Could the inhibition of SOX9 during our in vivo experiments inadvertently worsen tissue damage? Yes, this is a critical risk. SOX9 is essential for the function of reserve intestinal stem cells (rISCs) and their capacity for epithelial regeneration following injury, such as from radiation [25]. In cartilage and other tissues, SOX9 helps maintain macrophage function and contributes to tissue repair [1]. Therefore, inhibiting SOX9, while potentially therapeutic for cancer, may impair tissue repair mechanisms. It is crucial to include detailed histological analysis and functional regeneration assays in your animal models to monitor these potential side effects.
FAQ 4: What is a key advantage of using small-molecule inhibitors for SOX9 in a drug discovery context? A significant advantage is the ability to achieve temporal and dose-dependent control. Unlike genetic tools that permanently or semi-permanently alter gene expression, small-molecule inhibitors can be administered at specific times and in titratable concentrations. This allows researchers to precisely interrogate the effects of acute versus chronic SOX9 inhibition and to potentially dissect its different roles in various biological processes [25].
FAQ 5: How can we improve the therapeutic window when targeting SOX9 for cancer treatment to spare healthy tissue? Emerging strategies focus on targeted delivery. For example, using nanocarriers conjugated with ligands that specifically target cancer stem cells (CSCs) can help deliver SOX9 inhibitors or siRNA directly to tumor cells, thereby reducing exposure to healthy tissues like the intestinal epithelium that rely on SOX9 for repair [25]. Another proposed strategy is to use SOX9 inducers in normal intestinal tissue specifically after high-dose radiotherapy to promote crypt repair and regeneration, while simultaneously inhibiting SOX9 in the tumor [25].
Troubleshooting Guides
Problem: Low Efficiency in CRISPR-i Mediated SOX9 Repression
| Observed Issue | Potential Causes | Recommended Solutions |
|---|---|---|
| Poor repression of SOX9 | Inefficient guide RNA (gRNA) design [34]. | Redesign gRNAs targeting the SOX9 promoter or enhancer regions. Use validated design tools and select multiple gRNAs for testing. |
| Low efficiency of RNP delivery [34]. | Switch to a ribonucleoprotein (RNP) delivery format, which often yields higher editing efficiencies and more reproducible results than plasmid-based delivery. | |
| Insufficient dCas9 expression. | Use a high-titer viral vector (e.g., lentivirus) for dCas9 delivery and confirm expression via immunoblotting. Ensure the KRAB or other repressor domain is functional. |
Problem: High Off-Target Effects in shRNA Experiments
| Observed Issue | Potential Causes | Recommended Solutions |
|---|---|---|
| Unanticipated phenotypic effects | Sequence-dependent off-target silencing [34]. | Use a pool of multiple distinct shRNAs to ensure the phenotype is consistent. Employ bioinformatics tools to predict and minimize off-target binding. |
| Activation of immune responses | Sequence-independent interferon response [34]. | Use validated shRNA constructs with modified nucleotides to reduce immune activation. Use appropriate controls (e.g., scrambled shRNA) to account for non-specific effects. |
Problem: Cytotoxicity from Small-Molecule SOX9 Inhibitors
| Observed Issue | Potential Causes | Recommended Solutions |
|---|---|---|
| Death in non-target cells | Lack of specificity of the inhibitor. | Source inhibitors from different vendors or with distinct chemical scaffolds to confirm the on-target effect. Perform a counter-screen against related transcription factors. |
| Impaired tissue regeneration in in vivo models | On-target inhibition of SOX9 in healthy stem cells [25] [1]. | Titrate the inhibitor to the lowest effective dose. Implement intermittent dosing schedules to allow for recovery of repair mechanisms. Monitor tissue health with histology. |
Experimental Protocols
Detailed Protocol 1: Lentiviral shRNA-Mediated Knockdown of SOX9
Objective: To achieve transient knockdown of SOX9 in mammalian cells for functional studies.
Reagents:
- SOX9-targeting shRNA plasmids (e.g., from MISSION shRNA library)
- Non-targeting scrambled shRNA control plasmid
- HEK-293T cells for virus production
- Target cells (e.g., cancer cell line)
- Packaging plasmids (psPAX2, pMD2.G)
- Polybrene
- Puromycin
Methodology:
- Virus Production:
- Co-transfect HEK-293T cells with the shRNA plasmid and packaging plasmids (psPAX2, pMD2.G) using a standard transfection reagent.
- Replace media after 6-8 hours. Collect viral supernatant at 48 and 72 hours post-transfection.
- Concentrate the virus by ultracentrifugation if necessary.
Target Cell Transduction:
- Plate target cells and transduce with viral supernatant in the presence of 8 µg/mL Polybrene.
- Spinfect by centrifuging plates at 800-1000 x g for 30-60 minutes at 32°C to enhance efficiency.
Selection and Validation:
- 24 hours post-transduction, begin selection with puromycin (dose determined by kill curve) for at least 48 hours.
- Maintain cells for 72-96 hours post-transduction before analysis.
- Validate knockdown efficiency via:
- qRT-PCR: Measure SOX9 mRNA levels relative to a housekeeping gene (e.g., GAPDH).
- Western Blot: Probe for SOX9 protein (≈64 kDa) using a specific antibody.
Detailed Protocol 2: CRISPR Interference (CRISPR-i) for SOX9 Repression
Objective: To achieve specific and reversible transcriptional repression of the SOX9 gene.
Reagents:
- Plasmid expressing dCas9-KRAB (e.g., pLV hU6-sgRNA hUbC-dCas9-KRAB-T2a-Puro)
- gRNA expression plasmid or synthetic gRNA targeting the SOX9 promoter
- Lipofectamine 3000 or similar transfection reagent for plasmids; or, for RNP delivery, synthetic gRNA and purified dCas9-KRAB protein.
Methodology:
- gRNA Design and Preparation:
- Design 3-5 gRNAs targeting the region from -50 to -500 bp upstream of the SOX9 transcription start site (TSS).
- Cloning: If using plasmids, clone annealed oligos into the BsmBI site of the gRNA expression vector.
- RNP Complexing: If using RNP, complex purified dCas9-KRAB protein with synthetic gRNA at a molar ratio of 1:2.5 and incubate at room temperature for 10 minutes before delivery.
Cell Transfection/Nucleofection:
- For plasmids: Co-transfect the dCas9-KRAB and gRNA plasmids into your target cells using a standard method.
- For RNP: Deliver the pre-complexed RNP into cells via nucleofection for highest efficiency, especially in hard-to-transfect cells.
Analysis:
- Allow 72-96 hours for repression to establish.
- Assess repression efficiency by qRT-PCR and Western Blot, as described in Protocol 1.
- Confirm specificity by checking the expression of unrelated genes and potential off-target genes.
Data Presentation
Table 1: Comparison of shRNA, CRISPR-i, and Small-Molecule Inhibitors for SOX9 Inhibition
| Feature | shRNA Knockdown | CRISPR-i | Small Molecule Inhibitors |
|---|---|---|---|
| Molecular Target | mRNA [34] | DNA (Promoter/Enhancer) [34] | SOX9 protein or its co-factors |
| Level of Intervention | Post-transcriptional [34] | Transcriptional [34] | Post-translational |
| Reversibility | Reversible [34] | Reversible [34] | Reversible (dose-dependent) |
| Typical Efficiency | Moderate to High (≥70% knockdown) | High (≥80% repression) | Varies by compound |
| Key Advantage | Studied in essential genes [34] | High specificity, fewer off-targets [34] | Temporal and dose control [25] |
| Key Limitation | High off-target effects [34] | Persistent effects, delivery complexity [34] | Potential lack of specificity |
| Key Application | Initial functional screens, acute inhibition | Long-term, specific repression studies | Drug development, in vivo studies |
Table 2: Quantitative Data on Gene Silencing Technologies
| Parameter | RNAi (shRNA) | CRISPR (CRISPR-i/Knockout) |
|---|---|---|
| Time to Assess Effect | 3-5 days (knockdown) | 3-7 days (knockout/repression) |
| Editing/Silencing Efficiency | Varies; 50-90% (knockdown) | Often >90% (knockout) [34] |
| Phenotype | Knockdown (mRNA reduced) | Knockout (gene disrupted) or Repression (transcription blocked) |
| Primary Repair Mechanism | N/A (acts via RISC) | Non-Homologous End Joining (NHEJ) for knockout; no cleavage for CRISPR-i [34] |
Pathway Diagrams and Visualizations
Experimental Workflow for shRNA & CRISPR-i
SOX9's Dual Role in Cancer and Tissue Repair
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for SOX9 Inhibition Studies
| Reagent / Tool | Function / Description | Example Use Case |
|---|---|---|
| SOX9 shRNA Plasmids | DNA vectors encoding short hairpin RNAs for RNAi-mediated knockdown of SOX9 mRNA. | Creating stable cell lines with reduced SOX9 expression for proliferation and stemness assays. |
| dCas9-KRAB & SOX9 sgRNAs | A nuclease-deficient Cas9 fused to a KRAB repressor domain and guide RNAs targeting the SOX9 promoter. | Achieving reversible, transcriptional repression of SOX9 without altering the DNA sequence. |
| SOX9 Small-Molecule Inhibitors | Chemical compounds that directly or indirectly disrupt SOX9 protein function or stability. | In vivo studies for cancer therapy or acute in vitro inhibition to study downstream signaling. |
| Anti-SOX9 Antibody | Validated primary antibody for detecting SOX9 protein levels via Western Blot or Immunofluorescence. | Essential validation tool to confirm knockdown/repression efficiency at the protein level. |
| Lentiviral Packaging System | Plasmids (psPAX2, pMD2.G) for producing lentiviral particles to deliver genetic tools into target cells. | Enables efficient transduction of shRNA or CRISPR-i components into a wide range of cell types. |
| Puromycin | A selection antibiotic that kills non-transduced cells, allowing for the enrichment of successfully transduced cells. | Selection of cell populations stably expressing shRNA or dCas9-KRAB after viral transduction. |
Troubleshooting Guide: Common Experimental Challenges
Table 1: Troubleshooting Nanocarrier Delivery in SOX9 Research
| Problem Symptom | Potential Cause | Solution | Relevant to SOX9 Studies |
|---|---|---|---|
| Low Transfection Efficiency | Nanocarrier instability; incorrect N:P ratio; insufficient endosomal escape. | Optimize lipid/polymer to mRNA ratio (N:P ratio); include endosomolytic agents (e.g., chloroquine). | Critical for SOX9 mRNA delivery to chondrocytes [35]. |
| High Cytotoxicity | Cationic nanocarrier surface charge; cytotoxic components; impurities from synthesis. | Use biodegradable lipids (e.g., SM-102); incorporate PEGylated lipids (e.g., DMG-PEG2000) to reduce charge. | Prevents damage to healthy cartilage cells during SOX9 therapy [36] [35]. |
| Rapid Clearance from Blood | Opsonization and uptake by the Mononuclear Phagocyte System (MPS). | Functionalize surface with polyethylene glycol (PEG) to create "stealth" nanoparticles. | Extends circulation time for systemic SOX9-targeted delivery [37] [36]. |
| Poor Target Tissue Accumulation | Non-specific distribution; biological barriers (e.g., dense cartilage, tumor microenvironment). | Utilize active targeting with ligands (e.g., peptides, antibodies); leverage tissue-specific characteristics (e.g., pH, enzymes). | Essential for reaching SOX9-positive cells in specific tissues [37] [38]. |
| Inconsistent Batch Quality | Non-standardized synthesis methods; variable component purity. | Adopt reproducible microfluidic mixing techniques; implement rigorous physicochemical characterization (size, PDI, zeta potential). | Ensures reproducible SOX9 gene expression and therapeutic outcomes [35]. |
Frequently Asked Questions (FAQs)
Q1: What are the primary types of nanocarriers used for targeted delivery, and which are most suitable for transcription factor delivery like SOX9?
The primary nanocarriers include lipid-based nanoparticles (LNPs), polymeric nanoparticles, and liposomes. For delivering large biomolecules like SOX9 mRNA or plasmids, LNPs are often the most suitable. They are highly efficient in encapsulating nucleic acids, protecting them from degradation, and facilitating cellular uptake and endosomal escape. Recent studies have successfully used optimized LNPs for the co-delivery of SOX5 and SOX9 mRNA into chondrocytes for osteoarthritis treatment, demonstrating high efficacy and reduced inflammation [35].
Q2: How can I assess the potential cytotoxic effects of my nanocarrier formulation on healthy cells?
A combination of in vitro assays is recommended to comprehensively evaluate cytotoxicity, which is crucial when researching SOX9's role in tissue repair. Key methods include:
- Cell Viability/Cytotoxicity Assays: Use kits like Cell Counting Kit-8 (CCK-8) or Calcein/PI staining to quantify live and dead cells [35].
- Cell Morphology Observation: Monitor changes in cell shape and adhesion using microscopy.
- Mechanistic Studies: Investigate the generation of Reactive Oxygen Species (ROS) and mitochondrial membrane potential using assays like JC-1 [36] [35]. These are vital as SOX9 is involved in maintaining cellular function.
Q3: What strategies can I use to improve the nuclear delivery of therapeutics targeting transcription factors like SOX9?
Achieving efficient nuclear delivery is a key challenge. Two main strategies are:
- Passive Nuclear Targeting: Designing nanocarriers small enough (typically <40 nm) to pass through the nuclear pore complex. This can be achieved by modulating the nanocarrier's size, morphology, and surface charge [37].
- Active Nuclear Targeting: Incorporating Nuclear Localization Signals (NLS) into your nanocarrier system. NLS are short peptide sequences that are recognized by importin proteins, which actively transport cargo into the nucleus [37]. This is particularly relevant for strategies aiming to modulate SOX9 gene expression directly.
Q4: My nanocarriers are accumulating in the liver and spleen instead of the target tissue. How can I reduce this off-target accumulation?
This is a common issue due to the body's natural filtration and immune systems. To reduce off-target accumulation:
- PEGylation: Coat the surface of nanocarriers with polyethylene glycol (PEG) to create a "stealth" effect, reducing opsonization and recognition by immune cells in the liver and spleen [37] [36].
- Ligand-Based Active Targeting: Functionalize the nanocarrier surface with targeting moieties (e.g., antibodies, peptides, folates) that bind specifically to receptors overexpressed on your target cells. This enhances retention and uptake in the desired tissue [39] [38].
Q5: In the context of SOX9 research, what are the key in vivo considerations for testing nanocarrier systems aimed at tissue repair?
When moving to in vivo models, focus on:
- Biodistribution and Pharmacokinetics: Track where the nanocarriers go in the body (biodistribution) and how long they circulate (pharmacokinetics). This helps confirm target tissue delivery and assess off-target exposure [36].
- Therapeutic Efficacy in Disease Models: Use established animal models (e.g., ACLT-induced osteoarthritis in rats [35]) to test if the SOX9-modulating therapy effectively promotes tissue repair, reduces degeneration, and restores function.
- Comprehensive Safety Profile: Evaluate not just efficacy but also signs of toxicity in major organs (e.g., liver, kidney) and monitor for immune reactions [36] [38].
Experimental Protocols for Key Applications
Protocol 1: Formulating and Characterizing mRNA-Loaded Lipid Nanoparticles (LNPs) for SOX9 Delivery
This protocol is adapted from methods used for successful SOX5/SOX9 co-delivery [35].
Materials:
- Ionizable Lipid: e.g., SM-102
- Helper Lipid: e.g., 1,2-Distearoyl-sn-glycero-3-phosphocholine (DSPC)
- Cholesterol
- PEGylated Lipid: e.g., DMG-PEG2000
- mRNA payload: e.g., SOX9 mRNA
- Ethanol (absolute)
- Citrate Buffer (e.g., 10 mM, pH 4.0)
- Microfluidic device (e.g., NanoAssemblr, Ignite)
- Dialysis membranes (MWCO 10-20 kDa)
Method:
- Lipid Stock Preparation: Dissolve the ionizable lipid, DSPC, cholesterol, and DMG-PEG2000 in ethanol at a specific molar ratio. A representative ratio is 50:38.5:10:1.5 (SM-102:Cholesterol:DSPC:DMG-PEG2000) [35].
- Aqueous Phase Preparation: Dilute the SOX9 mRNA in citrate buffer (pH 4.0).
- Nanoparticle Formation: Use a microfluidic device to mix the ethanolic lipid solution and the aqueous mRNA solution at a controlled flow rate ratio (typically 1:3 to 1:5, aqueous-to-ethanol). The rapid mixing facilitates spontaneous LNP formation.
- Dialyze and Filter: Dialyze the formed LNPs against a large volume of PBS (pH 7.4) for several hours to remove ethanol and exchange the buffer. Sterile-filter the final formulation through a 0.22 µm membrane.
- Characterization:
- Size and PDI: Measure by Dynamic Light Scattering (DLS).
- Zeta Potential: Measure using a Zetasizer.
- Encapsulation Efficiency: Quantify using a RiboGreen assay.
- Morphology: Visualize using Transmission Electron Microscopy (TEM).
Protocol 2: Evaluating Chondrocyte Transfection and SOX9 Expression In Vitro
Materials:
- Primary chondrocytes or chondrocyte cell line
- SOX9-LNPs (from Protocol 1)
- Chondrogenic differentiation medium
- Anti-SOX9 antibody [35]
- Anti-Collagen II antibody [35]
- DAPI staining solution
- Cell culture plates
Method:
- Cell Seeding: Plate chondrocytes in appropriate culture vessels and allow them to adhere overnight.
- Transfection: Treat cells with the SOX9-LNP formulation. Include controls (e.g., untreated cells, empty LNPs).
- Immunofluorescence Staining:
- After 24-48 hours, fix cells with 4% paraformaldehyde.
- Permeabilize with 0.1% Triton X-100.
- Block with a suitable blocking serum.
- Incubate with primary antibody against SOX9 and a cartilage matrix marker like Collagen II.
- Incubate with fluorescently-labeled secondary antibodies (e.g., CoraLite488, CoraLite594).
- Counterstain nuclei with DAPI.
- Image using a fluorescence microscope.
- Functional Analysis: Assess downstream therapeutic effects by measuring the expression of key extracellular matrix components (e.g., Aggrecan, Collagen II) via Western Blot or ELISA.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Nanocarrier-based SOX9 Delivery
| Item | Function/Application in Research | Example from Literature |
|---|---|---|
| SM-102 (Ionizable Lipid) | Core component of LNPs; encapsulates and protects mRNA; enables endosomal escape. | Used in LNP formulations for SOX5/SOX9 mRNA co-delivery to chondrocytes [35]. |
| DMG-PEG2000 (PEGylated Lipid) | Provides a hydrophilic surface coating; enhances nanoparticle stability and circulation time; reduces non-specific uptake. | A standard component in LNP recipes to prevent rapid clearance [35]. |
| dCas9-VP64 / dCas9-KRAB | CRISPR activation/interference systems for precise upregulation (SOX9) or knockdown (e.g., RelA) without altering DNA sequence. | Used to engineer MSCs with enhanced chondrogenic potential via SOX9 activation [14]. |
| Anti-SOX9 Antibody | Detects and validates SOX9 protein expression levels in transfected cells or tissue sections via Western Blot, IF, or IHC. | Used to confirm SOX9 upregulation in chondrocytes and engineered MSCs [35] [14]. |
| Cell Viability/Cytotoxicity Kits (e.g., CCK-8, Calcein/PI) | Assess the biosafety and potential toxic side effects of nanocarrier formulations on healthy, non-target cells. | Critical for evaluating the biocompatibility of novel LNP systems [36] [35]. |
Experimental Workflows and Signaling Pathways
LNP Workflow
SOX9 Pathway
Nanocarrier Targeting
Frequently Asked Questions (FAQs)
Q1: What is the central role of SOX9 in stem cell biology, and why is it a target for inhibition studies? SOX9 is a transcription factor crucial for cell fate determination during embryonic development and for the maintenance and specification of adult stem cell pools [2]. It is expressed in stem cell niches and acts as a key regulator of self-renewal and differentiation in tissues derived from all three germ layers [2]. In the context of research, SOX9 inhibition is studied because its dysregulation is implicated in various diseases. In cancer, SOX9 is often overexpressed and promotes tumor growth, metastasis, and therapy resistance [25] [1]. Conversely, its precise regulation is also essential for normal tissue repair, with a recent study highlighting that the persistence of SOX9 activity after injury can switch the outcome from scarless regeneration to fibrosis [31].
Q2: After suppressing SOX9 in our intestinal organoid model, we observed a stark contradiction: some organoids died, while others showed hyperproliferation. Why would this happen? This apparent contradiction reflects the complex, context-dependent role of SOX9 and is a key finding in the field. Your observations are consistent with published data:
- Loss of Regenerative Capacity: SOX9 is required for the function of reserve intestinal stem cells (rISCs). Studies show that SOX9 knockout intestinal epithelium lacks regeneration capacity after injury, such as radiotherapy, and undergoes apoptosis [25]. This explains the cell death you observe.
- Paradoxical Hyperproliferation and Tumor Suppression: On the other hand, conditional knock-out of Sox9 targeted in the intestinal epithelium in vivo has been shown to lead to hyperplasia and dysplasia [40]. This suggests that SOX9 can also act as a tumor suppressor in the intestine, and its loss can remove a brake on proliferation. The eventual outcome in your model likely depends on factors like the specific cell type affected, the completeness of SOX9 suppression, and the presence of other genetic or signaling alterations.
Q3: Our team is investigating liver fibrosis. A recent publication suggested SOX9 has a "switch" function. What does this mean for our in vitro disease modeling? A 2024 research highlight confirmed that within the same injured kidney microenvironment, the differential between scarless repair and fibrosis depends on SOX9 activity [31]. Cells that successfully regenerated switched off SOX9 (SOX9on-off), while cells in areas that became fibrotic maintained SOX9 in a sustained "on" state (SOX9on-on) [31]. For your in vitro modeling of liver fibrosis, this implies that merely detecting SOX9 is not sufficient; you must design experiments that can track the dynamics of SOX9 expression over time. The therapeutic goal may not be to inhibit SOX9 entirely, but to find ways to manipulate this "switch" off after its initial pro-regenerative phase to prevent fibrosis.
Q4: We are using a tamoxifen-inducible Cre system for conditional SOX9 knockout, but our results are highly variable and mosaic. How can we improve consistency? Mosaicism is a recognized challenge with inducible Cre systems [41]. One group investigating SOX9 in the adult eye reported "substantial variability in both the extent and distribution of Sox9 inactivation" using the CAG-CreERTM system, which they identified as a "significant limitation" for consistent mechanistic studies [41]. To mitigate this:
- Optimize Tamoxifen Administration: Systematically titrate the concentration and timing of tamoxifen treatment to find the optimal window for your specific model.
- Implement Rigorous Inclusion Criteria: Use a validated secondary marker (e.g., a co-expressed fluorescent reporter) to identify and selectively analyze only the cells that have undergone efficient recombination.
- Acknowledge the Limitation: In your methodology, explicitly state the mosaic nature of the model and report the efficiency of recombination, as this transparency is critical for interpreting results [41].
Q5: What are the primary mechanisms by which SOX9 inhibitors work? SOX9 inhibitors function through several distinct mechanisms to disrupt SOX9 activity [42]:
- Small Molecules: These can bind to the SOX9 protein, preventing it from binding to its target DNA sequences.
- RNA Interference (RNAi): Using small interfering RNAs (siRNAs) or short hairpin RNAs (shRNAs) to specifically target and degrade SOX9 messenger RNA (mRNA), thereby reducing protein production.
- Gene Editing: Employing technologies like CRISPR/Cas9 to knock out or edit the SOX9 gene for a permanent loss of function.
Troubleshooting Common Experimental Issues
Problem: Inconsistent Cell Growth or Viability Post-SOX9 Suppression
| Potential Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Off-target effects of siRNA/shRNA | - Perform RT-qPCR and western blot to confirm SOX9 knockdown specificity.- Use multiple distinct siRNA sequences targeting SOX9. | - Include a scrambled siRNA control.- Validate key findings with a second, independent knockdown method (e.g., CRISPRi or pharmacological inhibitor if available). |
| Critical level of SOX9 required | - Titrate the concentration of siRNA/inhibitor to establish a dose-response curve.- Use a time-course experiment to monitor effects. | - Avoid complete ablation; aim for a partial knockdown that mimics pathological conditions. Research indicates there is a critical level of endogenous active SOX9 needed to maintain cell growth [40]. |
| Variable transfection efficiency | - Use a fluorescently-labeled negative control siRNA to estimate efficiency under your microscope.- Analyze transfection efficiency via flow cytometry. | - Optimize transfection reagent and protocol for your specific cell type.- Consider using viral vectors (lentivirus, retrovirus) for more stable and uniform gene delivery. |
| Microbial contamination | - Regularly test cultures for mycoplasma using PCR-based detection kits. | - Adhere to strict aseptic techniques.- Use antibiotics and antimycotics in culture media as a preventative measure [43]. |
Problem: Discrepant Phenotypes Across Different Cell Culture Models (2D vs. 3D)
| Observation | Underlying Principle | Resolution Strategy |
|---|---|---|
| Greater resistance to SOX9 inhibition in 3D spheroids/organoids | Cells in 3D cultures exhibit differential nutrient/oxygen gradients, altered cell-cell contacts, and changed gene expression profiles, which can influence cell survival and signaling pathway activity [44]. | - Do not expect identical IC50 values between 2D and 3D systems.- Characterize the baseline SOX9 expression and activity in your 3D model before perturbation. |
| Difficulties in achieving uniform SOX9 suppression in 3D models | Physical barriers in 3D structures can prevent uniform delivery of viral vectors, transfection reagents, or small molecule inhibitors [44]. | - Optimize the method of delivery (e.g., electroporation for organoids).- Extend the duration of treatment and confirm penetration via immunohistochemistry on sectioned samples. |
Key Signaling Pathways and Workflows
SOX9 in Stem Cell Regulation and Disease
Experimental Workflow for SOX9 Suppression Studies
Research Reagent Solutions
The following table details essential materials and reagents for studying SOX9 in stem cell models.
| Reagent Category | Specific Examples / Assays | Function in Experiment |
|---|---|---|
| SOX9 Suppression Tools | siRNA, shRNA (lentiviral), CRISPR/Cas9 (knockout), Small Molecule Inhibitors | To specifically reduce or ablate SOX9 expression or function for loss-of-function studies [25] [42]. |
| Detection & Validation | Anti-SOX9 Antibodies (for Western Blot, IHC/IF), SOX9 qPCR Assays, SOX9 Luciferase Reporter | To confirm the efficiency of SOX9 suppression and measure baseline expression levels [40]. |
| Cell Phenotyping Assays | Cell Titer-Glo (Viability), Caspase-Glo (Apoptosis), CFSE/EdU (Proliferation), Colony Formation Assay | To quantify the functional consequences of SOX9 suppression on cell growth, death, and clonogenic potential [25] [40]. |
| Stem Cell & Differentiation Markers | Antibodies for CDH6, LGR5, Keratins (cornea), Photoreceptor Markers (retina), GFAP (gliosis) | To assess stem cell identity and differentiation status following SOX9 manipulation in tissue-specific contexts [31] [41]. |
| Pathway Analysis Tools | TOPFlash/FOPFlash Reporter (Wnt/β-catenin), Phospho-Specific Antibodies, scRNA-seq Kits | To investigate the molecular mechanisms downstream of SOX9, such as its interaction with the Wnt/β-catenin pathway [2] [40]. |
The effects of SOX9 suppression are highly tissue and context-dependent. The table below summarizes key phenotypic outcomes.
| Tissue / System | Observed Phenotype After SOX9 Suppression | Key References |
|---|---|---|
| Intestinal Epithelium | - Ablation of regenerative capacity after injury (e.g., radiotherapy).- Increased apoptosis in crypts.- Can lead to hyperplasia/dysplasia (context-dependent). | [25] [40] |
| Corneal Limbus | - Loss of clonogenic capacity in limbal stem cells.- Impaired differentiation of corneal cells. | [41] |
| Retina | - Severe retinal degeneration.- Loss of Müller glial cells and photoreceptors via apoptosis.- Reactive gliosis. | [41] |
| Kidney Repair | - Promotion of scarless regeneration (when SOX9 is switched off).- Persistence of SOX9 leads to fibrosis and failed repair. | [31] |
| Various Cancers | - Suppression of tumor growth, metastasis, and cancer stem cell (CSC) self-renewal.- Increased sensitivity to radiotherapy and chemotherapy. | [25] [42] [1] |
Troubleshooting Guides and FAQs
This technical support center provides solutions for common challenges in establishing and validating in vivo models for tissue repair research, with a specific focus on investigating the side effects of SOX9 inhibition.
Wound Healing Models
Q: My animal model shows high variability in wound closure rates. What are the key factors to control?
A: High variability often stems from inconsistent wound creation or animal behavior. Key troubleshooting steps include:
- Standardized Wound Creation: Use an approved, disposable skin biopsy punch for precise and uniform wound size.
- Post-Procedural Housing: House animals individually post-operation to prevent cage-mates from interfering with the wound site, which can skew healing rates.
- Optimal Dosing Verification: Ensure test compounds are effective. For example, a 10% ointment of Annona reticulata leaf extract showed an epithelialization period of 13 ± 0.32 days, which was superior to the standard medication silver sulfadiazine at 14.20 ± 0.38 days [45].
Intestinal Damage Models
Q: How can I reliably induce and quantify intestinal epithelial damage in a zebrafish model?
A: Utilize a transgenic zebrafish model with nitroreductase/metronidazole-mediated ablation of intestinal epithelial cells (IECs). This offers a controlled, inducible system [46].
- Model Validation: Confirm damage induction by monitoring for the overexpression of
igfbp1a(insulin-like growth factor binding protein 1a), a key marker upregulated during intestinal damage in this model [46]. - Functional Assessment: Use morpholino-mediated knockdown of
igfbp1a. An effective model will show exacerbated intestinal damage and impaired regeneration uponigfbp1aknockdown, validating the system's sensitivity [46].
Q: The "leaky gut" phenotype in my murine model is inconsistent. How can I improve the reliability?
A: Focus on robustly inducing gut microbiota (GMB) dysbiosis and accurately measuring downstream effects.
- Induction Protocol: Administer colistin (an antibiotic) in drinking water (150 mg/L) and/or intragastric doses of E. coli (1x10^9 CFU/100 µL) every 7 days over a 3-week period to disrupt the gut microbiome [47].
- Quantification of Permeability: Assess gut barrier integrity by measuring the downregulation of intestinal tight junction proteins ZO-1 and Occludin via RT-PCR and immunofluorescence. Subsequently, confirm systemic translocation by measuring elevated serum levels of lipopolysaccharide (LPS) [47].
Osteoarthritis (OA) Models
Q: When modeling the gut-joint axis in osteoarthritis, how do I confirm that gut dysbiosis is driving joint pathology?
A: A successful "double-hit" model requires correlating specific gut changes with joint inflammation and damage.
- Characterize Dysbiosis: Confirm a successful first "hit" via 16S rRNA sequencing. Look for a marked increase in Firmicutes and a reduction in Bacteroidota, leading to a decreased Bacteroidota/Firmicutes (B/F) ratio [47].
- Link to Joint Health: Correlate these gut changes with OA severity. Bacteroidota and a higher B/F ratio are positively associated with intestinal barrier integrity and negatively correlated with OA progression. Conversely, Firmicutes abundance shows a positive correlation with inflammation and OA deterioration [47].
- Assess Joint Inflammation: In the synovium, demonstrate an upregulation of inflammation-related genes and a shift in macrophage polarization towards the M1 (pro-inflammatory) phenotype, shown by increased expression of CD86 and an elevated CD86/CD206 ratio [47].
Summarized Quantitative Data from Key Studies
Table 1: Analgesic and Anti-inflammatory Efficacy of Annona reticulata Leaf Extract (In Vivo)
| Test Model | Dose | Key Result | Significance/Outcome |
|---|---|---|---|
| Acetic acid-induced writhing | 400 mg/kg | 75% inhibition of pain | Significant peripheral analgesic effect [45] |
| Hot plate test | 400 mg/kg | 80% analgesic efficacy (at 90 min) | Significant central analgesic effect [45] |
| Formalin-induced paw licking | 400 mg/kg | Inhibition of 32.31% (acute phase) and 66.61% (chronic phase) | Effect on both immediate and inflammatory pain [45] |
| Xylene-induced ear edema | 200 & 400 mg/kg | Reduced ear edema (p < 0.001) | Significant anti-inflammatory activity [45] |
| Cotton pellet-induced granuloma | 200 & 400 mg/kg | Reduced granuloma formation (p < 0.001) | Significant anti-inflammatory activity [45] |
Table 2: Key Parameters in a Murine "Double-Hit" Osteoarthritis Model [47]
| Parameter | Control Group | Gut Dysbiosis Groups (Colistin / E. coli) |
|---|---|---|
| Gut Microbiota | Normal B/F ratio | Marked increase in Firmicutes; decrease in Bacteroidota & B/F ratio |
| Intestinal Barrier | Normal ZO-1, Occludin | Downregulation of ZO-1 and Occludin |
| Systemic Inflammation | Normal serum LPS | Elevated serum LPS |
| Macrophage Polarization | Normal CD86/CD206 | Increased CD86, leading to a higher CD86/CD206 ratio (M1 shift) |
| OA Severity (OARSI score) | Baseline | Significantly higher than control |
Experimental Protocols
- Animal Allocation: Divide mice into groups (e.g., Control, Standard Drug, Test Extract at two doses).
- Burn Wound Creation: Anesthetize mice and create a standardized, full-thickness burn wound on the dorsum.
- Treatment Administration: Apply the test formulation (e.g., 10% w/w ointment of aqueous plant extract) and the standard drug (e.g., silver sulfadiazine) topically to the wound area daily.
- Monitoring and Endpoint: Monitor wounds daily. The primary endpoint is the epithelialization period, defined as the number of days until the wound surface is completely covered by new epithelial tissue with no raw wound bed remaining.
- Induce Gut Dysbiosis (First Hit):
- Colistin Group: Administer colistin-supplemented drinking water (150 mg/L) for the study duration.
- E. coli Group: Administer a suspension of E. coli (1x10^9 CFU/100 µL) intragastrically every 7 days over a 3-week period.
- Surgical OA Induction (Second Hit):
- Anesthetize mice and perform a medial parapatellar ligament incision.
- Bluntly dissect the infrapatellar fat pad and transect the tibial collateral ligament to destabilize the medial meniscus (DMM).
- For sham controls, open and close the joint cavity without ligament transection.
- Post-Op Management: Allow mice to run in an exercise wheel for 1.5 hours daily to promote joint movement and pathology.
- Terminal Analysis: Euthanize animals 4 weeks post-surgery. Collect joint tissue for histological scoring (OARSI system) and synovium for gene expression analysis. Collect blood and intestinal tissue for LPS and tight junction protein analysis, respectively.
Signaling Pathways and Experimental Workflows
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Featured In Vivo Models
| Reagent / Model | Function / Purpose | Key Consideration |
|---|---|---|
| Colistin [47] | Antibiotic used to induce specific Gram-negative gut microbiota dysbiosis. | Prepare as a 150 mg/L solution in sterile drinking water for oral administration. |
| Escherichia coli (ATCC 25922) [47] | Non-pathogenic strain used to directly alter gut microbiota composition. | Resuspend in PBS to a final concentration of 1x10^9 CFU/mL for intragastric gavage. |
| Nitroreductase/Metronidazole System [46] | Enables controlled, inducible ablation of intestinal epithelial cells in transgenic zebrafish. | Ideal for high-throughput screening of modulators of mucosal healing. |
| Anti-ZO-1 & Anti-Occludin Antibodies [47] | Used in immunofluorescence and RT-PCR to assess gut barrier integrity ("leaky gut"). | Downregulation indicates increased intestinal permeability. |
| Aqueous Leaf Extract of Annona reticulata [45] | Test intervention with documented analgesic, anti-inflammatory, and wound healing properties. | For topical wound healing, formulate as a 10% (w/w) ointment. |
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: My SOX9 inhibition experiment shows a reduction in cell proliferation, but the Ki67 drop is less than expected. What could be the cause? A suboptimal reduction in Ki67 can often be traced to two main issues:
- Incomplete SOX9 Knockdown: Always confirm the efficiency of your SOX9 inhibition at both the mRNA and protein levels. Use quantitative PCR (qPCR) for transcriptional validation and Western blot for protein-level confirmation. Inadequate knockdown will result in a muted phenotypic response.
- Wrong Assay Timing: Ki67 is a marker for all active phases of the cell cycle (G1, S, G2, and M), but not quiescent cells (G0). Analyzing cells too soon after inhibition may not capture the full effect, as cells need time to arrest. Ensure you have conducted a time-course experiment to identify the peak effect, typically 48-96 hours post-transfection.
Q2: After SOX9 knockdown, how do I distinguish between a general cytotoxic effect and a specific impairment of stemness properties? This is a critical control. Follow this logical workflow:
- Step 1 - Assess General Cell Health: Perform a basic viability assay (e.g., CCK-8, Trypan Blue exclusion) on the bulk cell population. A small reduction in viability is expected, but massive cell death indicates potential off-target toxicity.
- Step 2 - Quantify Proliferation: Use an EdU (5-ethynyl-2'-deoxyuridine) assay to specifically label newly synthesized DNA in S-phase cells, providing a more precise proliferation metric than viability assays [16].
- Step 3 - Evaluate Stemness-Specific Functions: Conduct a functional assay like a tumorsphere formation assay under low-attachment conditions. A significant reduction in sphere number and size, disproportionate to the effect on bulk viability, strongly indicates a specific impairment of self-renewal capacity [48].
- Step 4 - Measure Stemness Markers: Confirm the molecular phenotype by quantifying protein levels of key stemness markers like SOX2, NANOG, and OCT4 via Western blot [48] [20].
Q3: In a wound healing model, SOX9 knockdown impairs regeneration. What biomarkers can I use to confirm the mechanism involves reduced keratinocyte migration and proliferation? You can create a multi-faceted biomarker profile to pinpoint the mechanism:
- Proliferation: Immunostaining for Ki67 and EdU incorporation in the wound margin will show reduced proliferating keratinocytes.
- Migration & Cytokeratin Expression: Immunohistochemistry (IHC) for Cytokeratin 14 (CK14), a marker for proliferative basal keratinocytes, and Cytokeratin 18 (CK18) will likely show decreased expression, confirming impaired keratinocyte function [20] [49].
- Stemness & Paracrine Signaling: Isolate and analyze cells from the wound bed for stemness markers (OCT4, SALL4). Furthermore, since SOX9 knockdown in mesenchymal stem cells reduces secretion of pro-healing factors like VEGF, IL-6, and IL-8, profiling this secretome via ELISA can provide a powerful functional correlate [20].
The following tables summarize key quantitative findings from published research on the consequences of SOX9 inhibition across different biological contexts.
Table 1: Impact of SOX9 Inhibition on Cellular Markers and Functional Outcomes
| Cell / Tissue Type | SOX9 Inhibition Method | Key Biomarker Reductions | Functional Outcomes | Citation |
|---|---|---|---|---|
| Human Umbilical Cord MSCs (HUC-MSCs) | Lentiviral shRNA Knockdown | - Ki67, CK14, CK18 (IHC)- Cytokines (IL-6, IL-8)- Growth Factors (VEGF, GM-CSF)- Stemness genes (OCT4, SALL4) | - Inhibited proliferation & migration- Impaired cutaneous wound healing in rats- Reduced hair follicle/ gland regeneration | [20] [49] |
| Glioblastoma Stem Cells (GSCs) | Lentiviral shRNA Knockdown | - Stemness biomarkers (CD133, Nestin, SOX2, NANOG) (Western Blot) | - Decreased tumorsphere formation- Reduced stemness frequency (limiting dilution assay)- Inhibited malignant phenotypes | [48] |
| Bone Tumors (Human) | Analysis of patient samples | - SOX9 overexpression correlated with high grade, metastasis, and recurrence | - Poor response to therapy | [50] |
| Intestinal Stem Cells (Mouse) | Conditional Knockout | - Loss of Label-Retaining Cells (LRCs) | - Increased radiation sensitivity- Impaired epithelial regeneration | [16] |
Table 2: Biomarker Correlation with Clinical and Pathological Features in Bone Cancer
| Clinical Feature | Local SOX9 in Tumor Tissue | Circulating SOX9 in PBMCs | Citation |
|---|---|---|---|
| Tumor Type | Malignant > Benign | Malignant > Benign | [50] |
| Tumor Grade | High > Low | High > Low | [50] |
| Metastasis | Present > Absent | Present > Absent | [50] |
| Therapy Response | Poor > Good | Poor > Good | [50] |
| Chemotherapy | Treated > Untreated | Treated > Untreated | [50] |
Detailed Experimental Protocols
Protocol 1: Validating SOX9 Knockdown and Its Effects on Stemness in Cell Lines
This protocol is adapted from methodologies used in glioblastoma and MSC studies [48] [20].
SOX9 Knockdown:
- Tool: Use lentiviral particles encoding short hairpin RNA (shRNA) targeting SOX9. A non-targeting scramble shRNA must be used as a negative control (shNC).
- Transduction: Transduce target cells (e.g., U87, LN229 glioma cells, or HUC-MSCs) using an appropriate transfection reagent like Lipofectamine 2000.
- Selection: Establish stable cell lines by selecting with 1 μg/ml puromycin for 10-15 days.
Validation of Knockdown:
- qPCR: Isolate total RNA and synthesize cDNA. Perform real-time qPCR using TaqMan or SYBR Green probes with SOX9-specific primers. Normalize to a housekeeping gene (e.g., β-actin).
- Western Blot: Lyse cells and quantify protein. Separate proteins by SDS-PAGE, transfer to a PVDF membrane, and probe with anti-SOX9 antibody. Use an anti-β-actin antibody as a loading control.
Assessing Stemness Phenotype:
- Tumorsphere Formation Assay: Seed single cells (1,000-10,000 cells/well) in low-attachment plates with serum-free medium supplemented with B27, EGF, and bFGF. Incubate for 7-14 days. Count the number and measure the diameter of formed spheres.
- Western Blot for Stemness Markers: Analyze protein lysates from knockdown and control cells for levels of CD133, Nestin, SOX2, and NANOG.
- In Vitro Limiting Dilution Assay: Seed cells in a serial dilution (e.g., from 1000 to 1 cell/well) in 96-well low-attachment plates. After 1-2 weeks, score wells for sphere formation. Use extreme limiting analysis software to calculate stem cell frequency.
Protocol 2: Quantifying Proliferation and Cytokeratin Changes in Vitro
Cell Proliferation Assays:
- Cell Counting Kit-8 (CCK-8): Seed cells in a 96-well plate. At 12, 24, 36, and 48 hours, add CCK-8 solution and incubate for 2 hours. Measure the absorbance at 450 nm.
- EdU Incorporation Assay: Use a commercial EdU kit (e.g., Click-iT). Incubate cells with EdU for 2 hours, then fix, permeabilize, and perform the "click" reaction to label incorporated EdU with a fluorescent dye. Analyze by flow cytometry or fluorescence microscopy to determine the percentage of S-phase cells [16].
Analysis of Cytokeratin Expression:
- Immunofluorescence/Immunohistochemistry: Culture cells on chamber slides or collect tissue samples. Fix with 4% paraformaldehyde, permeabilize with Triton X-100, and block. Incubate with primary antibodies against CK14 and CK18 overnight, followed by incubation with fluorescently-labeled or enzyme-conjugated (for DAB development) secondary antibodies. Counterstain with DAPI (for IF) or hematoxylin (for IHC) and image.
- Quantification: Use image analysis software (e.g., ImageJ) to quantify the fluorescence intensity or the percentage of positively stained cells across multiple fields of view.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for SOX9 and Biomarker Impairment Research
| Reagent | Function / Target | Example Application |
|---|---|---|
| SOX9 shRNA Lentiviral Particles | Specific knockdown of SOX9 gene expression | Generating stable SOX9-knockdown cell lines to study loss-of-function effects [48] [20]. |
| Anti-SOX9 Antibody | Detection and quantification of SOX9 protein | Western Blot, Immunohistochemistry (IHC), Immunofluorescence (IF) for validation [48] [50]. |
| Anti-Ki67 Antibody | Marker for proliferating cells (all active cell cycle phases) | IHC/IF to quantify changes in proliferation rates in tissue or cells after intervention [20] [49]. |
| Anti-Cytokeratin 14/18 Antibodies | Markers for specific epithelial cell types (e.g., basal keratinocytes) | IHC/IF to assess tissue integrity and differentiation status in wound healing or regeneration models [20] [49]. |
| Anti-Stemness Marker Antibodies (SOX2, NANOG, OCT4, CD133) | Detection of core stemness transcription factors and surface markers | Western Blot or Flow Cytometry to evaluate the potency and self-renewal capacity of stem cell populations [48] [20]. |
| Click-iT EdU Assay Kit | Specific labeling of S-phase DNA for proliferation quantification | More precise and safer alternative to traditional ^3H-thymidine incorporation for measuring cell proliferation [16]. |
Signaling Pathways and Experimental Workflows
Diagram Title: SOX9 Inhibition Cascade from Molecular to Functional Effects
Diagram Title: Experimental Workflow for SOX9 Impairment Studies
FAQs and Troubleshooting Guides
Q1: After SOX9 knockdown in our cellular model, we are not observing the expected inhibition of cell migration. What could be the cause?
- A1: Several factors could explain this discrepancy. First, confirm the efficiency of your SOX9 knockdown using western blot or RT-qPCR. Incomplete suppression may not produce a phenotypic effect [51] [12]. Second, consider the cell type and context. SOX9 can have opposing roles; it promotes migration in papillary thyroid cancer and triple-negative breast cancer cells but acts as a tumor suppressor in colorectal cancer [51] [52] [12]. Ensure your model's biological context aligns with your expected outcome. Third, review your Transwell or wound-healing assay protocol. For invasion assays, ensure Matrigel is properly applied and that the chemoattractant (e.g., 10% FBS) is fresh and present only in the lower chamber to create a valid gradient [51] [12].
Q2: When performing a colony formation assay following SOX9 inhibition, the results are inconsistent between technical replicates. How can we improve reproducibility?
- A2: Inconsistency often stems from cell seeding density and handling. Key steps include:
- Accurate Single-Cell Suspension: Ensure cells are properly dissociated and pipetted into a single-cell suspension before seeding to prevent clumping.
- Low-Density Seeding: Seed cells at a low and consistent density (e.g., 50–1,000 cells per well of a 6-well plate, determined by a pilot experiment) to allow isolated colony growth without confluence [12].
- Minimal Disturbance: Avoid moving the plates for at least the first 5-7 days to prevent disrupting early colony formation.
- Standardized Staining: Fix colonies with 4% paraformaldehyde and stain with Giemsa or crystal violet only after visible colonies have formed (typically after 10-14 days) [12]. A colony is typically defined as a cluster of >50 cells.
Q3: We suspect SOX9 inhibition is affecting cytokine secretion and the inflammatory microenvironment in our tendon repair model. Which signaling pathways and secreted factors should we prioritize investigating?
- A3: In the context of tissue repair, SOX9 is linked to key inflammatory and matrix-remodeling pathways. Your investigation should focus on:
- The cGAS-STING Pathway: Cytosolic mitochondrial DNA (mtDNA) leakage, which can occur with cellular stress, activates the cGAS-STING pathway, driving a potent inflammatory response. SOX9 may be involved in maintaining mitochondrial integrity [53].
- Key Cytokines and Markers: In a tendon injury model, SOX9 expression coincides with the restoration of tendon function. Monitor the expression of
α-SMA(a marker for myofibroblasts),Postn(periostin, involved in ECM maintenance), andCol I(collagen type I) via RT-PCR and immunohistochemistry [54]. The upregulation ofα-SMAandPostnis particularly pronounced at the injury site during the repair process [54]. - Extracellular DNA (exDNA): Senescent or damaged cells release exDNA, which can activate Toll-like receptors (TLRs) on immune cells like macrophages, amplifying inflammation. This is a relevant pathway in intervertebral disc degeneration and may be applicable to tendon research [53].
Summarized Quantitative Data from Key Studies
Table 1: Functional Endpoints Following SOX9 Knockdown or Inhibition
| Cell/Tissue Type | Experimental Manipulation | Effect on Migration/Invasion | Effect on Colony Formation | Key Molecular Changes | Citation |
|---|---|---|---|---|---|
| Papillary Thyroid Cancer (TPC-1, BCPAP cells) | SOX9 knockdown via siRNA | Significant inhibition of migration and invasion in Transwell assays. | Significant inhibition of proliferation and colony formation. | Downregulation of β-catenin, cyclin D1, c-Myc; Suppression of EMT. | [51] |
| Triple-Negative Breast Cancer (MDA-MB-231, MDA-MB-436 cells) | SOX9 knockdown via shRNA-lentivirus | Decreased migration and invasion in Transwell and wound-healing assays. | Suppressed cell proliferation and colony formation. | Cell cycle arrest at G0/G1; Increased apoptosis. | [12] |
| Mouse Achilles Tendon Injury Model | Chronological evaluation post-injury | N/A | N/A | Upregulation of Sox9, α-SMA, Postn, and Col I mRNA at injury site during repair. | [54] |
| Vascular Smooth Muscle Cells (VSMCs) | SOX9 knockdown in vitro | Suppressed PDGF-BB-induced migration. | Suppressed PDGF-BB-induced proliferation. | Inhibition of phenotypic transformation; Downstream of AMPK signaling. | [27] |
Table 2: Key Research Reagent Solutions for SOX9 Functional Studies
| Reagent / Material | Function / Application | Example from Literature | Citation |
|---|---|---|---|
| siRNA / shRNA (lentivirus) | Knockdown of SOX9 gene expression to study loss-of-function. | Sequences used: 5′-GCAGCGACGUCAUCUCCAAdTdT-3′ (siRNA); 5′-GCATCCTTCAATTTCTGTATA-3′ (shRNA). |
[51] [12] |
| Transwell Chamber (with/without Matrigel) | In vitro assessment of cell migration (no coating) and invasion (Matrigel coating). | Used to quantify the number of migratory/invasive cells after SOX9 knockdown. | [51] [12] |
| CCK-8 / MTT Assay Kits | Colorimetric measurement of cell proliferation and viability. | Used to track proliferation rates over 24-72 hours in SOX9-knockdown cells. | [51] [12] |
| Antibodies: α-SMA, Postn, SOX9 | Immunohistochemistry (IHC) / Western Blot to localize and quantify protein expression. | IHC used to show SOX9, α-SMA, and Postn localization at tendon injury sites. | [54] [27] |
| Tankyrase Inhibitors (XAV939, IWR-1) | Small molecule inhibitors that stabilize SOX9 protein by blocking its PARylation-dependent degradation. | Used in chondrocytes to promote SOX9 activity and cartilage matrix anabolism. | [55] |
Detailed Experimental Protocols
Protocol 1: Transwell Migration and Invasion Assay
This protocol is adapted from methodologies used to study SOX9 in cancer cell migration [51] [12].
- Cell Preparation: 24-48 hours post-transfection with SOX9-targeting siRNA/shRNA, trypsinize the cells (e.g., TPC-1, BCPAP, or MDA-MB-231). Wash and resuspend in serum-free medium.
- Chamber Setup:
- For Invasion: Thaw Matrigel on ice. Coat the upper surface of a Transwell chamber (8.0-µm pore size) with a thin layer of diluted Matrigel (e.g., 1:8 in serum-free medium) and incubate at 37°C for 30 min to gel.
- For Migration: Use an uncoated Transwell chamber.
- Seeding: Add 1x10^4 to 5x10^4 cells in 100-200 µL of serum-free medium to the upper chamber.
- Chemoattraction: Add 500 µL of medium containing 10% FBS to the lower chamber as a chemoattractant. Ensure no bubbles block the membrane pores.
- Incubation: Incubate the plates for 24-48 hours at 37°C in a 5% CO2 incubator.
- Fixation and Staining: Carefully remove cells from the upper surface of the membrane with a cotton swab. Fix cells that have migrated to the lower surface with 4% paraformaldehyde for 20 minutes, then stain with 0.1% crystal violet for 30 minutes.
- Quantification: Wash, air dry, and capture images of the membrane under a light microscope (e.g., 100x magnification). Count the number of cells in multiple random fields to calculate the average number of migrated/invaded cells per field.
Protocol 2: Colony Formation Assay
This protocol is based on experiments performed in breast cancer cells after SOX9 knockdown [12].
- Cell Seeding: After establishing stable SOX9-knockdown cells, trypsinize and count them. Seed cells into 6-well plates at very low densities (e.g., 50, 100, 250, and 500 cells per well) in complete medium. Include sufficient replicates.
- Incubation: Culture the cells for 10-14 days, replacing the medium with fresh complete medium every 3-4 days. Do not disturb the plates during the initial growth phase.
- Colony Staining: Once macroscopic colonies are visible, terminate the assay. Aspirate the medium, wash with PBS, and fix the colonies with 4% paraformaldehyde for 20 minutes at room temperature. Remove the fixative and stain with Giemsa stain for 20 minutes.
- Quantification: Gently rinse the plate with water and air dry. Count the number of colonies, where a colony is defined as a cluster of >50 cells. Calculate the colony formation efficiency: (Number of colonies / Number of cells seeded) × 100%.
Signaling Pathway and Experimental Workflow Diagrams
Mitigating Tissue Repair Deficits During SOX9-Targeted Therapy
FAQs: Balancing SOX9 Inhibition with Tissue Repair
Q1: Why is SOX9 considered a "double-edged sword" in therapeutic targeting? SOX9 plays a complex and dual role in physiology. On one hand, it acts as an oncogene in many solid cancers, promoting tumor immune escape, proliferation, and chemoresistance, making it a valuable therapeutic target. On the other hand, it is essential for maintaining macrophage function, contributing to cartilage formation, tissue regeneration, and repair in various organs. Inhibiting it systemically or at the wrong time can thus impair vital regenerative processes [1].
Q2: What are the key regenerative processes that SOX9 inhibition might disrupt? Evidence from multiple studies shows SOX9 is critical for:
- Cartilage repair and osteoarthritis (OA) treatment: SOX9 is a master regulator of chondrogenesis. Its activation in mesenchymal stromal cells (MSCs) enhances their chondrogenic potential for treating OA [56].
- Tendon regeneration: SOX9 is significantly upregulated during the early and middle stages of tendon healing (peaking at 1-2 weeks post-injury) and is concurrently expressed with the formation of the epitenon's pre-structure, which is essential for functional restoration [54].
- Lung injury repair: SOX9-expressing cells are crucial for regeneration after radiation-induced lung injury (RILI) and in chemically-induced acute lung injury (CALI), where they promote epithelial repair through proliferation and regulation of inflammatory responses [6] [57].
- General tissue repair: SOX9 helps maintain macrophage function and is a key transcriptional regulator in the repair of inflamed tissues [1].
Q3: What temporal expression patterns of SOX9 should inform dosing schedules? The timing of SOX9 expression varies by tissue and injury type. The table below summarizes key temporal patterns from experimental models.
Table 1: Temporal Expression of SOX9 in Tissue Repair Models
| Tissue/Injury Model | Key Time Points of SOX9 Involvement | Functional Role | Citation |
|---|---|---|---|
| Achilles Tendon Injury (Mouse) | - 1-2 weeks post-op: Significant upregulation.- 4 weeks post-op: Expression decreases as function restores. | Critical for early-to-middle stage restoration; linked to pre-structure of epitenon formation. | [54] |
| Radiation-Induced Lung Injury (Mouse) | Increased number of Sox9-expressing cells observed after damage; essential for repair and reconstruction. | Promotes regeneration of lung tissue; ablation of these cells leads to severe post-radiation damage. | [6] |
| Chemical-Induced Acute Lung Injury (Mouse) | Sox9+ alveolar type 2 cells proliferate predominantly in the damaged alveolar region during injury. | Promotes epithelial regeneration through orderly differentiation and regulation of inflammation. | [57] |
| Skin & Hair Follicle Reprogramming | Nuclear SOX9 detected within 1 week of induction in epidermal stem cells; a rise in proliferation follows by week 2. | Acts as a pioneer factor to switch stem cell fates from epidermal to hair follicle stem cells. | [4] |
Q4: What are the critical signaling pathways involved in SOX9-mediated regeneration? Key pathways include:
- PI3K/AKT Pathway: Enriched in Sox9-expressing cells during lung epithelium regeneration. Inhibition of this pathway suppresses the regenerative effects of these cells [6].
- Wnt/β-catenin Signaling: SOX9 employs two distinct mechanisms to inhibit this pathway, which is crucial for its role in chondrogenesis and fate determination [58].
Troubleshooting Guides
Problem: Impaired Tissue Regeneration Following SOX9 Inhibitor Treatment
- Potential Cause: The inhibition window overlaps with the critical early phase of the repair process, where SOX9 is highly expressed and functional.
- Solutions:
- Characterize the Expression Timeline: Before administering inhibitors, establish a detailed timeline of SOX9 expression in your specific injury model. Refer to Table 1 for guidance.
- Implement a Pulses Dosing Strategy: Design a dosing schedule that avoids the peak regenerative phase (e.g., the first 1-2 weeks in a tendon injury model [54]). Administer the inhibitor either before the injury occurs or after the initial regenerative peak has passed.
- Utilize a Conditional Knockout Model: If possible, use an inducible knockout system (e.g., Sox9flox/flox;SftpcCre−ERT2 mice [57]) to ablate SOX9 after the primary repair phase is complete, allowing you to study the effects of late-stage inhibition.
Problem: Variable Therapeutic Outcomes in Cancer Models Targeting SOX9
- Potential Cause: The dual role of SOX9 is creating conflicting effects. While it may be driving tumor progression, it might also be involved in the health of surrounding non-malignant tissue or in the function of certain immune cells.
- Solutions:
- Analyze the Immune Microenvironment: Use bioinformatics and immunohistochemistry to analyze the correlation between SOX9 expression and tumor immune cell infiltration. SOX9 can negatively correlate with anti-tumor immune cells like CD8+ T cells and NK cells [1].
- Employ Localized Delivery: Explore localized drug delivery systems (e.g., hydrogels [59]) to maximize inhibitor concentration at the tumor site while minimizing systemic exposure and off-target effects on regenerating tissues elsewhere.
- Combine with Immunomodulators: Consider combining SOX9 inhibition with immunotherapy agents to counteract its role in creating an "immune desert" microenvironment [1].
Experimental Protocols
Protocol 1: Evaluating SOX9 Expression in a Tendon Injury Model
This protocol is adapted from a study investigating SOX9 localization during tendon healing [54].
- Animal Model: Perform a partial excision (e.g., 0.3 mm wide) of the Achilles tendon in mice.
- Tissue Collection: Collect tendon samples at critical time points post-operation (e.g., 1 week, 2 weeks, 4 weeks) and from sham-operated controls.
- Functional Analysis: Conduct a physiological torque test to quantitatively assess functional restoration over time.
- mRNA Analysis: Perform RT-PCR on tendon tissue to measure Sox9 mRNA levels. Compare expression levels across time points.
- Protein Localization: Perform immunohistochemical (IHC) staining on tissue sections using a validated anti-SOX9 antibody to identify the specific cells expressing SOX9 protein during repair.
- Morphological Analysis: Conduct H&E and Azan staining to correlate SOX9 expression with histological changes, collagen fiber appearance, and tissue architecture.
Protocol 2: Assessing the Role of SOX9 in Lung Regeneration
This protocol is based on studies using lineage tracing to define the role of SOX9-expressing cells in lung repair [6] [57].
- Animal Model:
- Obtain Sox9-CreERT2; Ai9 tdTomato reporter mice.
- Induce SOX9 lineage tracing by intraperitoneally injecting tamoxifen (e.g., 0.08 mg/g body weight for 3 consecutive days) to permanently label SOX9-expressing cells and their progeny.
- Induce Injury:
- For Radiation-Induced Lung Injury (RILI): Subject anesthetized mice to whole-thorax radiation (e.g., a single 16 Gy dose), lead-shielding the rest of the body [6].
- For Chemical-Induced Lung Injury (CALI): Expose mice to a controlled concentration of a chemical agent (e.g., 8.33 mg/L phosgene for 5 minutes) [57].
- Tissue Analysis:
- Collect lung tissues at various time points post-injury.
- Use fluorescence microscopy to track the location, proliferation, and differentiation of the tdTomato-labeled SOX9-lineage cells.
- Perform co-immunofluorescence staining with cell-type-specific markers (e.g., Pro-SPC for AEC2 cells) to identify the fate of the labeled cells.
- Functional Blocking: To confirm the necessity of SOX9+ cells, use a different mouse model (e.g., Sox9flox/flox; RosaDTA) to ablate these cells upon tamoxifen administration and compare injury outcomes to controls.
Signaling Pathways and Logical Workflows
Diagram 1: The Dual Outcome of SOX9 Inhibition Based on Timing. This workflow illustrates how the timing of SOX9 inhibition relative to the injury event is critical. Correct timing spares the essential regenerative phase, while incorrect timing disrupts key cellular processes, leading to impaired healing.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for SOX9 and Regeneration Studies
| Reagent / Model | Specific Example | Function / Application | Key Consideration |
|---|---|---|---|
| Conditional KO Mice | Sox9flox/flox mice [57] | Allows tissue-specific or timed deletion of Sox9 gene to study loss-of-function. | Cross with cell-type-specific Cre drivers (e.g., SftpcCre−ERT2 for lung). |
| Lineage Tracing Mice | Sox9-CreERT2; Ai9 tdTomato [6] [57] | Permanently labels SOX9+ cells and all their progeny after tamoxifen induction for fate mapping. | Critical for tracking the contribution of SOX9+ cells to regeneration. |
| SOX9 Antibodies | Anti-SOX9 (e.g., H-90, AB5535) [1] [6] | Detects SOX9 protein in tissues (IHC, IF) or lysates (Western Blot). | Validate for specific applications (IHC vs. WB). |
| CRISPR/dCas9 System | dCas9-SOX9 activator [56] | Enables targeted gene activation of SOX9 for gain-of-function studies. | Used to enhance chondrogenic potential in MSCs. |
| Injury Models | Achilles tendon partial excision [54], Whole-thorax radiation [6], Phosgene inhalation [57] | Provide controlled, reproducible contexts to study SOX9 in tissue repair. | Choose a model relevant to your research focus and ensure ethical approval. |
| Pathway Agonists/Inhibitors | AKT agonist (SC79); AKT inhibitor (Perifosine) [6] | Tools to manipulate the PI3K/AKT pathway, which is downstream of SOX9 in regeneration. | Confirm efficacy and specificity in your model system. |
A central challenge in modern oncology is the development of therapies that can selectively eliminate cancer stem cells (CSCs) while preserving normal stem cell function, particularly their crucial role in tissue repair and homeostasis. This paradox arises because CSCs and normal stem cells share many surface markers and signaling pathways. The transcription factor SOX9 exemplifies this dilemma, as it plays critical roles in both cancer progression and normal tissue regeneration. This technical support guide addresses specific experimental issues researchers encounter when designing tissue-specific delivery systems that target CSC markers while protecting normal stem cell function, with particular attention to mitigating SOX9 inhibition side effects on tissue repair mechanisms.
Frequently Asked Questions (FAQs) and Troubleshooting Guides
FAQ 1: How can I target cancer stem cell markers without damaging normal stem cells involved in tissue repair?
The Challenge: Most CSC surface markers (approximately 73%) are derived from markers present on human embryonic or adult stem cells, creating significant risk of off-target effects on normal tissue maintenance and repair [60] [61].
Troubleshooting Guide:
| Issue | Possible Cause | Solution |
|---|---|---|
| Damage to intestinal crypt cells during GI cancer therapy | SOX9 inhibition affecting reserve intestinal stem cells (rISCs) | Implement spatial control of SOX9 inhibitors using nanocarriers targeted to CSC-specific glycans; consider SOX9 inducer administration post-radiotherapy to protect normal tissue [25] |
| Poor cartilage repair in osteoarthritis models | Off-target effects on chondrogenic differentiation | Utilize CRISPR-dCas9 systems for fine-tuned SOX9 activation (not overexpression) in mesenchymal stromal cells to enhance chondrogenesis while avoiding oncogenic transformation [14] |
| Therapeutic resistance and tumor recurrence | CSC plasticity and heterogeneity | Combine SOX9-targeting approaches with conventional therapies and microenvironment modulators to address multiple CSC subpopulations [62] |
Experimental Protocol Validation: When testing SOX9 inhibition strategies, always include parallel assessments of tissue repair capacity in relevant normal stem cell populations:
- Establish baseline SOX9 expression in both CSCs and corresponding normal stem cells
- Monitor expression of differentiation markers (Collagen II, Aggrecan for chondrocytes; villin for intestinal epithelium) during inhibition experiments
- Implement functional repair assays (cartilage defect models, intestinal crypt regeneration) to quantify tissue repair compromise
FAQ 2: What experimental models best recapitulate the SOX9 duality in cancer versus tissue repair?
The Challenge: SOX9 demonstrates context-dependent functions, acting as an oncogene in many cancers while remaining essential for cartilage maintenance and intestinal crypt regeneration [1] [25].
Troubleshooting Guide:
| Model System | Advantages | Limitations | Best Applications |
|---|---|---|---|
| CRISPR-engineered MSCs with tunable SOX9 [14] | Precise control over expression levels; mimics potential therapeutic approach | May not fully capture tumor microenvironment | Testing tissue-specific delivery systems for osteoarthritis |
| Intestinal organoids with SOX9 knockout [25] | Direct assessment of crypt regeneration capacity | Does not incorporate immune components | Evaluating GI toxicity of SOX9-targeting therapies |
| Xenograft models with CSC markers [60] | Evaluates tumor initiation and propagation | Limited human microenvironment components | Validating CSC-specific targeting approaches |
| Rat tail needle puncture IVD model [63] | Assesses SOX9 role in disc regeneration | Species-specific differences in healing | Testing regenerative therapies involving SOX9 activation |
Key Technical Consideration: When using the tetracycline-off (Tet-off) regulatory system for SOX9 expression control [63], ensure thorough validation of off-target effects by:
- Performing RNA-seq analysis after induction
- Verifying specificity with multiple gRNA designs
- Testing minimal effective induction levels to reduce non-specific effects
FAQ 3: How can I design drug delivery systems that distinguish between CSCs and normal stem cells?
The Challenge: The similarity between CSC surface markers and normal stem cell markers creates significant hurdles for targeted delivery systems [60] [61].
Quantitative Data on Shared Markers:
Table: CSC Markers Shared with Normal Stem Cells and Their Expression Patterns
| Marker | Expression in hESCs | Expression in Adult Stem Cells | Expression in Normal Tissues | Associated Cancers |
|---|---|---|---|---|
| CD133 | Yes [60] | Hematopoietic, Neural, Prostate [60] | Rare (proliferative cells) [60] | Breast, prostate, colon, glioma, liver, lung, ovary [60] |
| CD90 (Thy-1) | Yes [60] | Mesenchymal, Cardiac [60] | Rare (T-cells, neurons) [60] | Brain, liver [60] |
| SSEA-4 | Yes [61] | Mesenchymal, Cardiac [61] | Rare [61] | Teratocarcinoma, breast [61] |
| EpCAM (CD326) | Yes [60] | No [60] | Rare (epithelial cells) [60] | Colon, pancreas, liver [60] |
Experimental Workflow for Targeted Delivery System Development:
The Scientist's Toolkit: Research Reagent Solutions
Key Reagents for SOX9-Related Research
Table: Essential Research Reagents for CSC Targeting and Tissue Repair Studies
| Reagent | Function/Application | Example Use | Considerations |
|---|---|---|---|
| CRISPR-dCas9-VP64 system [14] | Transcriptional activation of SOX9 | Enhancing chondrogenic potential of MSCs for cartilage repair | Enables fine-tuning of expression levels without permanent genetic changes |
| CRISPR-dSaCas9-KRAB system [14] | Transcriptional repression of RelA/NF-κB | Reducing inflammatory responses in engineered MSCs | Can be used simultaneously with activation systems for multi-gene regulation |
| Tet-off inducible system [63] | Controlled transgene expression | Regulating SOX9 and TGFβ1 co-expression in MSCs | Allows temporal control to minimize continuous overexpression risks |
| AAVS1 safe harbor targeting [63] | Precise transgene integration | Reducing oncogenic risks of SOX9/TGFβ1 overexpression | Provides more predictable expression patterns |
| α7-nAChR inhibitors (e.g., MLA) [64] | Blocking nicotine-induced SOX9 suppression | Studying molecular mechanisms of SOX9 regulation in chondrogenesis | Important for elucidating environmental impacts on tissue repair |
| NFATc2 siRNA [64] | Investigating SOX9 epigenetic regulation | Determining histone acetylation mechanisms in SOX9 expression | Useful for studying transcriptional control in both CSCs and normal stem cells |
Signaling Pathway Mapping: SOX9 in Cancer vs. Tissue Repair
Advanced Technical Considerations
Quantitative Assessment of SOX9 Inhibition Side Effects
Table: Documented Side Effects of SOX9 Perturbation in Different Tissues
| Tissue Type | SOX9 Inhibition Consequences | SOX9 Activation Consequences | Experimental Evidence |
|---|---|---|---|
| Intestinal epithelium | Compromised crypt regeneration after radiation; increased apoptosis [25] | Enhanced reserve intestinal stem cell function and radioresistance [25] | SOX9 knockout models show lack of regeneration capacity after radiotherapy [25] |
| Articular cartilage | Suppressed chondrogenic differentiation of BMSCs; weak cartilage repair [64] | Enhanced chondrogenesis and cartilage matrix production; improved OA outcomes [14] | Nicotine-induced SOX9 suppression mediates poor cartilage repair in defect models [64] |
| Pancreatic cancer | Reduced CSC invasiveness and tumorigenicity [25] | Promoted EMT, invasion, and chemoresistance [1] | NF-κB mediated SOX9 regulation enhances CSC properties [25] |
| Intervertebral disc | Impaired disc hydration and ECM synthesis [63] | Enhanced aggrecan and type II collagen production; reduced inflammation [63] | SOX9 and TGFβ1 co-expression in ToMSCs promotes disc regeneration [63] |
Strategies to Minimize Tissue Repair Side Effects
Spatial Control Mechanisms:
- Implement nanocarriers conjugated with ligands targeting CSC-specific glycans [25]
- Utilize differential endocytosis rates between CSCs and normal stem cells
- Develop activation systems responsive to tumor microenvironment cues (hypoxia, pH)
Temporal Control Approaches:
- Employ Tet-off systems for inducible SOX9 modulation [63]
- Schedule inhibitor administration to avoid conflict with normal tissue repair phases
- Implement pulsatile delivery systems that align with CSC cell cycle patterns
Combinatorial Strategies:
- Pair SOX9 inhibitors with tissue-specific protectors for normal stem cells
- Utilize lower-dose multi-target approaches rather than single-agent high-dose inhibition
- Develop feedback-controlled systems that adjust dosing based on biomarker detection
By addressing these specific technical challenges and implementing the recommended troubleshooting approaches, researchers can advance toward more selective targeting strategies that effectively eliminate CSCs while preserving the critical tissue repair functions of normal stem cells.
Frequently Asked Questions (FAQs)
FAQ 1: Why is a combination approach (SOX9 inhibition followed by induction) necessary? SOX9 has a context-dependent, "double-edged sword" role in biology. In cancers, it is often overexpressed and drives tumor progression, immune escape, and chemoresistance, making it a valuable therapeutic target. However, in many healthy tissues, SOX9 is essential for the function of stem and progenitor cells that mediate tissue regeneration and repair. A combination approach aims to leverage this duality: inhibiting SOX9 to treat the primary disease, followed by carefully controlled induction to restore the regenerative capacity of non-targeted healthy tissues that may be adversely affected [1] [25] [65].
FAQ 2: In which tissue repair contexts is SOX9 known to be critical? Research has identified SOX9 as a key player in the regeneration of multiple tissues, which are potential candidates for post-therapeutic SOX9 induction.
- Lung Repair: Sox9-positive alveolar type 2 epithelial cells are crucial for promoting epithelial regeneration after chemically-induced acute lung injury and radiation-induced lung injury (RILI) [66] [6].
- Intestinal Repair: SOX9 is required for the maintenance and function of reserve intestinal stem cells (rISCs), which are critical for epithelial regeneration after insults like radiation [25].
- Skeletal Regeneration: A Sox9-expressing subpopulation in the periosteum acts as "messenger cells" that are indispensable for orchestrating large-scale bone regeneration, such as in rib repair [67].
- Liver Homeostasis: SOX9 is involved in liver regeneration and is a marker for hepatic progenitor cells [1] [65].
FAQ 3: What are the primary challenges in implementing this combination strategy? The most significant challenge is achieving tissue-specific targeting. Inducing SOX9 systemically after its inhibition could potentially reactivate dormant cancer stem cells or promote minimal residual disease. Furthermore, the timing and dosage of SOX9 induction require precise calibration to achieve optimal regeneration without triggering fibrosis or other pathologies [25] [68].
FAQ 4: Which signaling pathways are involved in SOX9-mediated regeneration? SOX9-mediated repair processes engage several key signaling pathways, which can be potential targets for pharmacological intervention.
- PI3K/AKT Pathway: This pathway is enriched in Sox9-expressing cells during lung epithelium regeneration and is critical for their proliferative and regenerative effects [6].
- Hedgehog (Hh) Signaling: In skeletal regeneration, Sox9+ periosteal cells require Hh signaling to non-autonomously orchestrate the differentiation of neighboring callus cells. The role of Hh in this repair context is distinct from its role in development [67].
Troubleshooting Guides
Problem 1: Failure to Observe Functional Tissue Regeneration After SOX9 Induction
- Potential Cause: Inefficient or off-target delivery of the SOX9 inducer.
- Solution: Validate the delivery system using a reporter construct. For localized injuries (e.g., skeletal, articular), consider intra-tissue or intra-articular injection of inducer-loaded biomaterials or engineered cells. For systemic delivery, develop lipid nanoparticles (LNPs) or viral vectors decorated with tissue-specific targeting ligands [25] [56].
- Potential Cause: The tissue microenvironment is inhibitory due to chronic inflammation or fibrosis.
- Solution: Pre-condition the target tissue by co-administering anti-inflammatory agents (e.g., corticosteroids) or anti-fibrotics alongside SOX9 inducers. Analysis of the epigenetic landscape via ATAC-seq or CUT&RUN may reveal if chromatin at key regenerative enhancers remains inaccessible [4] [69].
Problem 2: Unintended Activation of Oncogenic or Pro-Fibrotic Programs
- Potential Cause: Sustained, high-level expression of SOX9.
- Solution: Utilize a drug-inducible gene expression system (e.g., tetracycline/doxycycline-controlled, tamoxifen-controlled CreER[T]) to allow for precise temporal control. Fine-tune the dose and duration of the inducing agent to achieve therapeutic levels of SOX9 without triggering malignancy. In models, sustained SOX9 expression in epidermal stem cells leads to features of basal cell carcinoma [4].
- Potential Cause: SOX9 is a known promoter of fibrosis in multiple organs.
- Solution: Meticulously monitor established fibrotic markers (e.g., α-SMA, collagen deposition) in the target tissue post-induction. Implement an induction regimen that uses pulsed, rather than continuous, SOX9 activation to mitigate fibrotic risk [68].
The following table summarizes quantitative findings from key studies on SOX9's role in regeneration and therapy response.
Table 1: Key Quantitative Data on SOX9 in Regeneration and Therapy
| Observation / Finding | Experimental System | Quantitative Outcome | Significance / Implication |
|---|---|---|---|
| SOX9 & Chemoresistance | iCCA patients receiving chemotherapy [65] | Median survival: 62 mo (Low SOX9) vs. 22 mo (High SOX9) | High SOX9 confers resistance; post-chemo induction may be risky. |
| SOX9 in Lung Regeneration | Mouse model of radiation-induced lung injury (RILI) [6] | Ablation of Sox9+ cells led to severe phenotypes; PI3K/AKT pathway enriched. | Sox9+ cells are essential; PI3K/AKT is a key regenerative pathway. |
| SOX9 in Intestinal Radioresistance | SOX9 knockout mouse intestinal epithelium after RT [25] | KO crypts lacked regeneration capacity and underwent apoptosis. | SOX9 is required for radioresistance and regeneration of rISCs. |
| Sox9+ Cells in Bone Repair | Mouse rib bone resection model [67] | ~6% of periosteal cells are Sox9+ "messenger" cells. | A small, specific progenitor population orchestrates large-scale repair. |
Detailed Experimental Protocols
Protocol 1: Evaluating SOX9-Induced Regeneration in a Murine Model of Radiation-Induced Enteritis This protocol models a common side effect of abdominal radiotherapy and tests the efficacy of post-therapeutic SOX9 induction.
- Step 1: Induction of Injury. Subject adult mice (e.g., C57BL/6) to abdominal irradiation (e.g., 12-16 Gy) using a small animal irradiator with appropriate lead shielding to focus the beam.
- Step 2: Post-Therapeutic SOX9 Induction.
- Step 3: Tissue Collection and Analysis. Sacrifice mice at defined timepoints (e.g., 3, 7, 14 days post-injury).
- Histology: H&E staining to assess crypt architecture and villus blunting. Alcian Blue staining for goblet cells.
- Proliferation: Immunofluorescence (IF) for Ki67 or EdU labeling to quantify regenerating crypts.
- Lineage Tracing: In genetic models, use
Sox9-CreER; Rosa26-lsl-tdTomatomice. Administer tamoxifen to label Sox9+ cells and track their contribution to regenerated epithelium [6]. - Functional SOX9 Readout: Immunohistochemistry (IHC) for SOX9 protein and qPCR for known target genes (e.g.,
Col2a1).
Protocol 2: CRISPR-dCas9 Mediated Fine-Tuning of SOX9 in Cell Therapy This protocol uses advanced gene editing to enhance the therapeutic potential of MSCs for conditions like osteoarthritis, a model for controlled SOX9 delivery.
- Step 1: Vector Design and Transduction.
- Design lentiviral vectors encoding:
- dCas9-SOX9: A catalytically dead Cas9 (dCas9) fused to a transcriptional activator (e.g., VP64) and targeted to the endogenous SOX9 promoter.
- dCas9-RelA: A dCas9 fused to a transcriptional repressor (e.g., KRAB) and targeted to the RelA (p65) promoter to concurrently dampen inflammation [56].
- Transduce human bone marrow-derived MSCs with these vectors.
- Design lentiviral vectors encoding:
- Step 2: In Vitro Validation.
- Chondrogenesis: Culture transduced MSCs in chondrogenic induction medium (TGF-β3). Analyze via:
- qPCR: for chondrogenic markers (COL2A1, ACAN, SOX9).
- Histology: Alcian Blue and Safranin O staining for proteoglycan deposition.
- Immunofluorescence: for Collagen Type II.
- Immunomodulation: Treat cells with TNF-α and measure secretion of anti-inflammatory factors (e.g., IL-10, TGF-β) via ELISA.
- Chondrogenesis: Culture transduced MSCs in chondrogenic induction medium (TGF-β3). Analyze via:
- Step 3: In Vivo Testing.
- Inject the engineered MSCs intra-articularly into a murine model of osteoarthritis (e.g., surgically-induced).
- Assess outcomes via pain behavior tests, histopathological scoring (OARSI system) of cartilage degradation, and IHC for cartilage matrix components and inflammatory markers [56].
Signaling Pathway and Strategy Diagrams
Diagram Title: SOX9 Inhibition-Induction Combination Strategy
Diagram Title: SOX9-Driven Regenerative Signaling Network
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for SOX9 Combination Therapy Research
| Reagent / Tool | Function & Application | Key Considerations |
|---|---|---|
Inducible Transgenic Mice (e.g., Krt14-rtTA;TRE-Sox9, Sox9-CreER) [4] [6] |
Enables temporal and/or tissue-specific control of SOX9 expression in vivo for regeneration studies. | Choose a promoter (Krt14, Villin, Sftpc) relevant to your target tissue. Tamoxifen vs. Doxycycline inducibility offers different temporal control. |
Lineage Tracing Reporter Mice (e.g., Rosa26-lsl-tdTomato) [66] [6] |
Fates and quantifies the contribution of SOX9-expressing cells and their progeny to regenerated tissues. | Critical for validating the cellular mechanism of repair. |
| CRISPR-dCas9 Systems (VP64 activators, KRAB repressors) [56] | Allows for precise fine-tuning of endogenous SOX9 (and other genes like RelA) levels in cell therapies. |
Superior to cDNA overexpression as it modulates the native gene locus. Requires efficient delivery (lentivirus, AAV). |
| Small Molecule Pathway Agonists/Inhibitors (e.g., SC79 [AKT agonist], Perifosine [AKT inhibitor]) [6] | Used to manipulate signaling pathways (PI3K/AKT) downstream of SOX9 to validate their role in regeneration. | Essential for mechanistic studies. Confirm specificity and optimize dose to avoid off-target effects. |
| Specific Anti-SOX9 Antibodies (for IHC, IF, WB) [65] [6] | Validates SOX9 protein localization and expression levels in tissue sections and cell lysates. | Confirm antibody specificity for IHC (nuclear staining). Use alongside mRNA analysis (qPCR, RNA-ISH) for comprehensive data [67]. |
This guide addresses a critical challenge in therapeutic SOX9 inhibition: the unintended disruption of essential tissue repair and homeostasis mechanisms. SOX9 is a master regulator in numerous biological processes, and its systemic inhibition can lead to significant side effects, particularly affecting cartilage, pancreatic function, and immune regulation. The following FAQs, troubleshooting guides, and experimental protocols are designed to help researchers identify, understand, and overcome these obstacles by focusing on strategies that modulate specific downstream effectors, thereby bypassing the need for broad SOX9 suppression.
Key Consequences of SOX9 Inhibition
| Affected System | Documented Consequence of SOX9 Loss | Proposed Compensatory Mechanism |
|---|---|---|
| Pancreatic Beta Cells | Disrupted alternative splicing; impaired insulin secretion; glucose intolerance [70] | Targeted activation of SRSF5 functional splice variants [70] |
| Cartilage & Bone | Impaired chondrogenesis; exacerbated osteoarthritis [14] | CRISPR-dCas9-mediated fine-tuning of SOX9 and RelA in MSC therapies [14] |
| Immune Regulation | Disrupted balance in pro/anti-inflammatory responses; potential impact on tissue repair [1] | Modulation of macrophage polarization and T-cell function downstream of SOX9 [1] |
| Organ Fibrosis | Altered fibrotic progression in heart, liver, kidney, and lung [68] | Targeting specific SOX9-mediated fibrotic signaling pathways (e.g., TGF-β) [68] |
Frequently Asked Questions (FAQs)
1. What are the most sensitive tissue repair systems to SOX9 inhibition, and what are the first signs of dysfunction? The most sensitive systems are pancreatic beta cells and chondrogenic (cartilage) tissues. The first signs include:
- Metabolic Dysfunction: In beta cells, the earliest sign is a stunted first-phase insulin secretion in response to a glucose challenge, progressing to glucose intolerance. This occurs due to defective alternative splicing of genes critical for beta cell function, even before a significant reduction in total insulin content [70].
- Cartilage Degradation: In models of osteoarthritis (OA), SOX9 depletion is linked to failed cartilage repair, increased pain, and elevated expression of inflammatory markers like NFKBIA and RELA within the joint [14].
2. Which specific downstream effectors of SOX9 can be targeted to rescue cartilage repair without directly reactivating SOX9? The goal is to promote chondrogenesis and counteract inflammation through SOX9-independent pathways.
- Pro-Chondrogenic Factors: Focus on delivering or upregulating key secreted factors that are normally produced by SOX9-replete cells. Engineered mesenchymal stromal cells (MSCs) can be used to express factors beneficial to cartilage integrity, even in a SOX9-low environment [14].
- Inflammatory Pathway Inhibition: Simultaneously target the transcription factor RelA (a subunit of NF-κB). Inhibiting RelA suppresses the production of catabolic enzymes and inflammatory cytokines in osteoarthritic joints, creating a more permissive environment for repair [14].
3. Our in vivo model shows compensatory fibrosis following SOX9 inhibition. What alternative pathways are driving this? SOX9 is a known regulator of organ fibrosis, and its inhibition can disrupt normal repair, leading to pathological scarring. Key drivers to investigate include:
- TGF-β Signaling: This is a primary pathway interacting with SOX9 in fibrotic processes across the heart, liver, kidney, and lung [68].
- Extracellular Matrix (ECM) Components: Monitor the accumulation of collagen and fibronectin. The dynamic nature of fibrosis means that SOX9 inhibition may alter the normal balance of ECM synthesis and degradation [68].
- Epigenetic Regulators: Assess the methylation status of the SOX9 promoter and enhancer regions, as this can be a compensatory mechanism that further dysregulates its expression and contributes to disease progression [68].
4. What is a reliable in vitro protocol to screen for compounds that mimic the pro-repair functions of SOX9? A robust screening system utilizes human mesenchymal stromal cells (MSCs) directed toward chondrogenesis.
- Cell Model: Primary human bone marrow stromal cells (BMSCs) [14].
- Key Assays:
- Chondrogenic Differentiation: Culture cells in chondrogenic differentiation medium and quantify sulfated glycosaminoglycan (sGAG) deposition (e.g., with Alcian Blue or DMMB assay) as a primary readout for cartilage matrix production [14].
- Gene Expression Analysis: Use qPCR to monitor the expression of key chondrogenic markers such as COL2A1 and ACAN [14].
- Inflammatory Challenge: Treat cells with IL-1β or TNF-α to model an inflammatory environment and measure the suppression of NF-κB-driven reporters (e.g., NFKBIA expression) to identify compounds with dual chondrogenic and anti-inflammatory activity [14].
Troubleshooting Guides
Problem 1: Impaired Insulin Secretion in Beta Cell Models Post-SOX9 Knockdown
Potential Cause: Disruption of alternative splicing networks, particularly the loss of functional protein-coding splice variants of the serine-rich splicing factor SRSF5, a key downstream effector of SOX9 [70].
Solution:
- Step 1: Confirm the Splicing Defect. Perform RNA-Seq or RT-PCR analysis on known SRSF5 targets in your beta cell model to identify a shift toward non-functional isoforms [70].
- Step 2: Bypass the Defect. Transfert cells with a plasmid expressing the functional, protein-coding SRSF5 splice variant. The goal is to restore the splicing landscape downstream of SOX9.
- Step 3: Functional Rescue. Measure glucose-stimulated insulin secretion (GSIS) after SRSF5 rescue. A successful intervention should restore the first-phase insulin secretion peak.
Experimental Workflow for Problem 1:
Problem 2: Failure of Cartilage Repair in Preclinical OA Models with SOX9-Targeting Therapy
Potential Cause: Broad SOX9 inhibition prevents necessary chondrogenesis and fails to control the inflammatory joint environment [14].
Solution: Implement a Combination Cell Therapy.
- Step 1: Engineer "Enhanced" MSCs. Use CRISPR-dCas9 technology to simultaneously fine-tune the expression of key transcription factors in MSCs. Specifically, use CRISPRa to activate Sox9 and CRISPRi to repress RelA [14]. This creates a cell product with high chondrogenic and immunomodulatory potential.
- Step 2: Intra-articular Delivery. Administer these modified MSCs via intra-articular injection into the osteoarthritic joint.
- Step 3: Monitor Outcomes. Assess therapy success through:
- Histology: Significant attenuation of cartilage degradation (e.g., OARSI scoring).
- Behavioral Tests: Palliation of OA pain (e.g., weight-bearing asymmetry).
- Molecular Analysis: Promoted expression of cartilage-integrity factors and inhibited catabolic enzymes.
Experimental Workflow for Problem 2:
The Scientist's Toolkit: Research Reagent Solutions
Key Materials and Reagents for Featured Experiments
| Reagent / Tool | Function / Application | Key Consideration for Bypass Strategies |
|---|---|---|
| CRISPR-dCas9 System (VP64/KRAB) [14] | Fine-tuned transcriptional activation (CRISPRa) of Sox9 and inhibition (CRISPRi) of RelA. | Enables precise modulation of gene expression to desired levels without radical knockout, optimizing MSC therapy. |
| Chondrogenic Differentiation Medium [14] | Directing BMSCs toward chondrocyte differentiation in vitro. | Essential for validating the pro-chondrogenic capacity of engineered MSCs or candidate compounds pre-injection. |
| SRSF5 Expression Plasmid [70] | Rescue of defective insulin secretion in SOX9-depleted beta cells. | Must contain the protein-coding, functional splice variant to bypass the SOX9-mediated splicing defect. |
| Factor H & Ba Plasma Assays [71] | Biomarkers for monitoring alternative complement pathway activation. | Critical for diagnosing immune-related side effects if SOX9 inhibition inadvertently affects innate immunity. |
Detailed Experimental Protocol: CRISPR-Enhanced MSC Therapy for OA
This protocol is adapted from published work demonstrating efficacy in attenuating OA progression in a surgical mouse model [14].
Objective: To generate and validate mesenchymal stromal cells (MSCs) with enhanced chondrogenic and immunomodulatory potential for rescuing cartilage repair in the context of SOX9 inhibition.
Part 1: Lentiviral Vector Construction
- Construct Lenti-dSpCas9-VP64: This vector expresses a fusion protein for CRISPRa, based on Streptococcus pyogenes Cas9 and the transcriptional activation domain VP64 [14].
- Construct Lenti-dSaCas9-KRAB: This vector is for CRISPRi, based on Staphylococcus aureus Cas9 and the transcriptional repression domain KRAB [14].
- Construct Lenti-EGFP-dual-gRNA: Design and clone guide RNA (gRNA) sequences into this vector. Effective sequences for targeting include:
Part 2: Cell Culture and Viral Transduction
- Isolate and culture CD45-negative bone marrow stromal cells (BMSCs) from mouse or human sources.
- Co-transduce BMSCs with the three lentiviral constructs (Lenti-dSpCas9-VP64, Lenti-dSaCas9-KRAB, and Lenti-EGFP-dual-gRNA) to generate the modified "enhanced" MSC population.
- Use fluorescence-activated cell sorting (FACS) to isolate EGFP-positive cells, indicating successful transduction.
Part 3: In Vitro Validation
- Chondrogenic Potential: Culture transduced and control MSCs in chondrocyte differentiation medium. Assess chondrogenesis by:
- qPCR: Measure the upregulation of Sox9 and chondrogenic markers (Col2a1, Acan).
- Histology: Analyze pellet cultures for proteoglycan deposition using Alcian Blue staining.
- Immunomodulatory Potential: Challenge cells with TNF-α and/or IL-1β.
- qPCR/ELISA: Measure the reduced expression and secretion of inflammatory mediators (e.g., IL-6) and the NF-κB target Nfkbia.
Part 4: In Vivo Efficacy Testing
- OA Model Induction: Use a surgical model (e.g., destabilization of the medial meniscus) to induce OA in mice.
- Therapy Administration: At defined post-surgery, perform intra-articular injections of either:
- Group 1: Enhanced MSCs (experimental)
- Group 2: Unmodified MSCs (control)
- Group 3: Cell culture medium (vehicle control)
- Outcome Assessment:
- Pain Behavior: Monitor weight-bearing asymmetry over time.
- Histopathology: At endpoint, score cartilage degradation, osteophyte size, and synovitis using standardized systems (e.g., OARSI score).
- Molecular Analysis: Immunostaining for SOX9, matrix components (e.g., COL2), and catabolic enzymes (e.g., MMP13) in joint sections.
The transcription factor SOX9 is a critical regulator of cell fate, differentiation, and tissue homeostasis in multiple organ systems. In the context of therapeutic research, particularly in oncology, SOX9 inhibition has emerged as a strategy to target cancer stem-like cells (CSCs) and overcome therapy resistance [25] [1] [33]. However, this approach is complicated by SOX9's vital protective roles in healthy tissues. This technical support guide outlines the specific adverse effects—enteritis, impaired wound closure, and cartilage degradation—that researchers may encounter during experiments involving SOX9 inhibition. It provides troubleshooting methodologies to monitor, validate, and manage these effects within a preclinical research setting, ensuring the accurate interpretation of experimental outcomes.
Troubleshooting Guide: SOX9 Inhibition Side Effects
Enteritis and Impaired Intestinal Regeneration
Problem Statement: Researchers observe significant weight loss, diarrhea, and histological evidence of intestinal damage (shortened villi, loss of crypt architecture) in animal models following the administration of a SOX9 inhibitor, especially when combined with radiotherapy or other cytotoxic agents.
Background & Mechanism: The intestinal epithelium relies on stem cells for constant regeneration. SOX9 is highly expressed in reserve intestinal stem cells (rISCs), a quiescent cell population essential for epithelial repair following injury. SOX9 knockout studies demonstrate that the absence of SOX9 leads to a catastrophic failure of intestinal regeneration after insults like radiation, resulting in severe enteritis [25]. The mechanism involves the loss of a crucial radioresistant and regenerative cell population.
Troubleshooting Questions and Solutions:
Q1: How can I confirm that the observed enteritis is specifically linked to SOX9 inhibition in intestinal stem cells?
- Solution: Implement lineage tracing and immunohistochemical validation.
- Experimental Protocol: Utilize a transgenic mouse model (e.g.,
SOX9-CreER;R26-tdTomato). Administer tamoxifen to label SOX9-expressing cells and their progeny, then administer your SOX9 inhibitor. Post-treatment, analyze intestinal sections via fluorescence microscopy and co-stain for stem cell markers (e.g.,Lgr5for active ISCs). A specific decrease in theSOX9+rISC population and its derived lineages, coupled with increased tissue damage, confirms the on-target effect of your inhibitor [25]. - Key Reagents:
SOX9-CreERmouse line,R26-tdTomatoreporter line, Tamoxifen, Anti-Lgr5 antibody for IHC.
- Experimental Protocol: Utilize a transgenic mouse model (e.g.,
- Solution: Implement lineage tracing and immunohistochemical validation.
Q2: My therapeutic intervention requires SOX9 inhibition but causes debilitating enteritis. How can I mitigate this side effect?
- Solution: Consider a targeted delivery system or a rescue strategy for normal tissue.
- Experimental Protocol: Develop a nanoparticle-based delivery system conjugated with ligands that specifically target your cancer cells (e.g., using CSC-specific surface glycans). This approach aims to concentrate the SOX9 inhibitor within the tumor, sparing the intestinal crypts [25]. Alternatively, in a separate control group, you can attempt to protect the intestines by locally delivering a SOX9 inducer (e.g., via targeted expression of
Fgf8orRelA) to bolster the function of rISCs during and after the completion of the cytotoxic therapy [25].
- Experimental Protocol: Develop a nanoparticle-based delivery system conjugated with ligands that specifically target your cancer cells (e.g., using CSC-specific surface glycans). This approach aims to concentrate the SOX9 inhibitor within the tumor, sparing the intestinal crypts [25]. Alternatively, in a separate control group, you can attempt to protect the intestines by locally delivering a SOX9 inducer (e.g., via targeted expression of
- Solution: Consider a targeted delivery system or a rescue strategy for normal tissue.
Table 1: Monitoring and Validation Parameters for SOX9 Inhibition-Associated Enteritis
| Parameter | Method/Assay | Expected Outcome with SOX9 Inhibition |
|---|---|---|
| Clinical Observation | Daily body weight measurement | >10% weight loss |
| Histopathology | H&E staining of jejunum/ileum | Shortened villi, crypt loss, inflammatory infiltrate |
| Cell Proliferation | EdU or BrdU incorporation assay | Reduced proliferation in crypts |
| Stem Cell Fate | IHC for OLFM4 (aISC marker) |
Relative preservation of OLFM4+ cells |
| Stem Cell Fate | IHC for SOX9 (rISC marker) |
Significant depletion of SOX9+ rISC population |
| Functional Regeneration | γ-Irradiation (8-12 Gy) challenge | Failure to regenerate crypts, high mortality |
Cartilage Degradation and Osteoarthritis
Problem Statement: In animal studies, systemic or intra-articular SOX9 inhibition leads to loss of cartilage matrix proteoglycans, erosion of articular cartilage, and accelerated development of osteoarthritis (OA), confounding the interpretation of drug efficacy and toxicity.
Background & Mechanism: SOX9 is a master transcription factor for chondrogenesis, directly transactivating essential cartilage extracellular matrix (ECM) genes like COL2A1 (type II collagen) and ACAN (aggrecan) [72] [24] [73]. It safeguards the chondrocyte lineage by preventing dedifferentiation and conversion to osteoblasts. SOX9 deficiency in chondrocytes prompts a rapid loss of the cartilage phenotype, characterized by proteoglycan loss, and in growth plates, swift closure via chondrocyte dedifferentiation and osteoblastogenesis [72]. Furthermore, in obesity-related OA, elevated fatty acid oxidation in chondrocytes can lead to SOX9 degradation, driving disease progression [74].
Troubleshooting Questions and Solutions:
Q1: How do I quantitatively assess cartilage degradation in my model following SOX9 inhibition?
- Solution: Use the standardized OARSI (Osteoarthritis Research Society International) scoring system for robust, semi-quantitative histopathological evaluation.
- Experimental Protocol: After sacrifice, isolate knee or hip joints. Fix, decalcify, paraffin-embed, and section. Perform Safranin O/Fast Green staining to visualize proteoglycans (red) and collagen (green). Score each joint blindly using the OARSI system (e.g., 0-6 for mice), which grades the severity and extent of cartilage erosion. SOX9 inhibition is expected to significantly increase the OARSI score [72] [74].
- Solution: Use the standardized OARSI (Osteoarthritis Research Society International) scoring system for robust, semi-quantitative histopathological evaluation.
Q2: The observed cartilage damage is significant. How can I determine if it's due to direct ECM loss or chondrocyte fate change?
- Solution: Perform lineage tracing and molecular analysis of chondrocyte-specific markers.
- Experimental Protocol: Use a chondrocyte-specific inducible Cre mouse model (e.g.,
AcanCreERT2) crossed with a reporter (e.g.,R26-tdTomato) and administer your SOX9 inhibitor. Analyze joint sections for:- Dedifferentiation: Co-stain for the chondrocyte reporter (
tdTomato) and progenitor/osteogenic markers (Nt5e,Runx2,Sp7). The appearance oftdTomato+cells expressing these non-chondrocytic markers indicates lineage fate change [72]. - Matrix Gene Expression: Perform RNA in situ hybridization or qRT-PCR on articular cartilage extracts for key anabolic genes (
Col2a1,Acan). SOX9 inhibition should lead to a marked downregulation of these transcripts [72] [74].
- Dedifferentiation: Co-stain for the chondrocyte reporter (
- Experimental Protocol: Use a chondrocyte-specific inducible Cre mouse model (e.g.,
- Solution: Perform lineage tracing and molecular analysis of chondrocyte-specific markers.
Table 2: Key Analyses for SOX9 Inhibition-Associated Cartilage Defects
| Analysis Type | Target | Technique | Interpretation of Positive Result |
|---|---|---|---|
| Histology | Proteoglycan content | Safranin O Staining | Loss of red stain indicates proteoglycan depletion |
| Histology | Cartilage structure | H&E / Toluidine Blue | Surface fibrillation, chondrocyte cluster formation |
| Lineage Tracing | Chondrocyte fate | AcanCreERT2;R26-tdTomato + IHC |
tdTomato+ cells express Runx2 or Sp7 (osteoblast markers) |
| Gene Expression | Anabolic markers | qRT-PCR / RNAscope | Downregulation of SOX9, COL2A1, ACAN |
| Gene Expression | Catabolic markers | qRT-PCR / RNAscope | Upregulation of MMP13, ADAMTS5 |
| Protein Level | SOX9 protein stability | Western Blot / IHC | Decreased SOX9 protein, increased ubiquitination |
The following diagram illustrates the core molecular mechanisms by which SOX9 inhibition in chondrocytes leads to cartilage degradation, integrating direct transcriptional effects with metabolic dysregulation.
Mechanisms of Cartilage Degradation by SOX9 Inhibition
Impaired Wound Closure
Problem Statement: Wound healing assays, either in vivo or in vitro using keratinocytes or fibroblasts, show significantly delayed closure rates following SOX9 modulation.
Background & Mechanism: While the search results do not provide a direct molecular link between SOX9 and wound closure in skin, SOX9 is a well-established pioneer factor that dictates cell fate decisions in epidermal stem cells [4]. It is plausible that its inhibition could disrupt the intricate balance of proliferation and differentiation required for re-epithelialization during wound healing. SOX9's role in other cell types involved in repair, such as its function in regulating macrophage activity and overall tissue regeneration, further supports its potential impact on wound closure [1].
Troubleshooting Questions and Solutions:
Q1: How can I pinpoint which phase of wound healing (proliferation, migration, differentiation) is impaired by SOX9 inhibition?
- Solution: Conduct a detailed time-course analysis of the wound healing process.
- Experimental Protocol:
- In Vivo: Create standardized full-thickness skin wounds on a rodent model. Administer the SOX9 inhibitor systemically or topically. Monitor wound area daily for closure rate. Harvest wound tissue at specific time points (e.g., days 3, 7, 14) for histology.
- Proliferation: IHC for
Ki-67in the wound margin epidermis. - Re-epithelialization: H&E staining to measure the length of the migrating epithelial tongue.
- Differentiation: IHC for differentiation markers (
KRT10,LOR) in neo-epidermis.
- Proliferation: IHC for
- In Vitro: Perform a scratch assay on a monolayer of keratinocytes treated with a SOX9 inhibitor. Use live-cell imaging to track the collective and individual cell migration dynamics into the scratch zone. Subsequently, fix cells and stain for actin (
Phalloidin) and nuclei (DAPI) to analyze cytoskeletal remodeling at the wound edge.
- In Vivo: Create standardized full-thickness skin wounds on a rodent model. Administer the SOX9 inhibitor systemically or topically. Monitor wound area daily for closure rate. Harvest wound tissue at specific time points (e.g., days 3, 7, 14) for histology.
- Experimental Protocol:
- Solution: Conduct a detailed time-course analysis of the wound healing process.
Q2: Could the impaired wound closure be related to changes in stem cell behavior?
- Solution: Analyze the fate and proliferation of epidermal stem cells (EpdSCs) in the wound.
- Experimental Protocol: Use a lineage tracing model (
Krt14-CreER;R26-tdTomato) to label EpdSCs. Induce labeling, create wounds, and administer the SOX9 inhibitor. Analyze wound tissue to determine ifSOX9-inhibited EpdSCsfail to proliferate, migrate, or appropriately differentiate into the new epithelium, potentially due to a failure in executing a wound-induced gene program [4].
- Experimental Protocol: Use a lineage tracing model (
- Solution: Analyze the fate and proliferation of epidermal stem cells (EpdSCs) in the wound.
The Scientist's Toolkit: Essential Research Reagents
This table lists key reagents, as identified in the search results, that are essential for studying the biology of SOX9 and the adverse effects of its inhibition.
Table 3: Key Research Reagents for SOX9 and Tissue Repair Studies
| Reagent / Tool | Type | Primary Function in Research | Example Application |
|---|---|---|---|
AcanCreERT2 Mouse |
Genetic Model | Enables tamoxifen-inducible, chondrocyte-specific gene knockout or lineage tracing. | Studying cell-autonomous effects of SOX9 deletion in cartilage [72]. |
Krt14-rtTA; TRE-Sox9 Mouse |
Genetic Model | Allows doxycycline-inducible, epidermal stem cell-specific SOX9 overexpression. | Studying SOX9's pioneer role in cell fate switching and cancer [4]. |
| CRISPR-dCas9 System | Molecular Tool | Enables targeted gene activation (e.g., SOX9) or inhibition (e.g., RelA). |
Engineering MSCs with enhanced chondrogenic potential for OA therapy [56]. |
| OARSI Scoring System | Histological Protocol | Standardized semi-quantitative scoring of OA severity in joint sections. | Validating and quantifying cartilage degradation in models [72] [74]. |
| AZ1 (USP28 Inhibitor) | Small Molecule | Promotes ubiquitination and degradation of SOX9 protein. | Testing SOX9 stabilization's role in therapy resistance (e.g., in ovarian cancer) [33]. |
| Trimetazidine | Small Molecule | Inhibits fatty acid oxidation (FAO); activates AMPK. | Rescuing SOX9 degradation in metabolic OA models [74]. |
FAQs on SOX9 Inhibition in Research
Q1: Is the cartilage degradation caused by SOX9 inhibition reversible? A: The reversibility likely depends on the duration and extent of inhibition. Short-term, partial inhibition may allow for recovery upon drug withdrawal, especially if the chondrocyte progenitor population remains intact. However, prolonged and complete SOX9 deficiency leads to irreversible changes like chondrocyte dedifferentiation and osteoblastogenesis, resulting in permanent growth plate closure and cartilage damage [72]. Recovery experiments, where the inhibitor is withdrawn and tissue is monitored over time, are crucial to determine this in your specific model.
Q2: Can I use a systemic SOX9 inhibitor without observing these adverse effects? A: It is highly challenging. Given SOX9's critical functions in intestines, cartilage, and other tissues, systemic inhibition will likely produce on-target side effects. The key is to develop targeted delivery strategies. The literature suggests using nanocarriers conjugated with ligands specific to your target cells (e.g., CSCs) to minimize exposure to healthy tissues [25]. Alternatively, local administration (e.g., intra-articular for joint disease) can circumvent systemic toxicity.
Q3: Are there any biomarkers to monitor these adverse effects in vivo? A: Yes, both serum and tissue biomarkers can be employed.
- For Cartilage Degradation: Monitor serum or synovial fluid levels of collagen cleavage products (e.g., C2C, CTX-II) and proteoglycan fragments. These are released during ECM breakdown and correlate with OA severity. A rise in these biomarkers following SOX9 inhibition would indicate active cartilage catabolism [74].
- For Intestinal Damage: Serum citrulline, a product of intestinal epithelial cells, is a reliable marker of functional enterocyte mass and can indicate the severity of intestinal injury [25].
Q4: My data shows SOX9 inhibition is effective against my tumor model, but animals succumb to enteritis. What are my options? A: This is a common translational hurdle. Consider these strategies:
- Dose Scheduling: Implement intermittent dosing schedules (e.g., "drug holidays") to allow for intestinal crypt recovery between cycles of therapy.
- Protective Co-Treatment: As mentioned in the troubleshooting guide, investigate the co-administration of a SOX9 inducer (e.g., FGF8, RelA activators) specifically targeted to the intestines to protect the rISC compartment during systemic SOX9 inhibitor therapy [25].
- Combination Therapy: Lower the dose of your SOX9 inhibitor and combine it with a standard chemotherapeutic agent. This may achieve synergistic anti-tumor effects while reducing the single-agent toxicity to a manageable level.
Frequently Asked Questions (FAQs) and Troubleshooting Guides
FAQ 1: What are the primary mechanisms by which SOX9 inhibition might cause tissue-specific toxicity, particularly in organ systems like the kidney and intestine?
Answer: SOX9 inhibition can lead to tissue-specific toxicity through two primary mechanisms: impairing cellular repair and promoting programmed cell death. Research has shown that SOX9 is a crucial pro-survival factor in renal tubular epithelial cells (RTECs). A kinome-wide screen identified a CDKL5-SOX9 regulatory axis, where stress-activated CDKL5 kinase suppresses SOX9, leading to increased cell death in kidney injury models [75]. In the intestines, SOX9 is essential for the maintenance and radioresistance of reserve intestinal stem cells (rISCs). Inhibition of SOX9 compromises the epithelium's regenerative capacity, making it susceptible to damage from insults like radiation therapy [25].
Troubleshooting Guide: Mitigating Renal Toxicity in SOX9-Targeted Experiments
- Problem: Unanticipated renal tubular damage or elevated kidney injury markers (e.g., Kim-1, Ngal) in preclinical models following SOX9 inhibition.
- Potential Cause: The therapeutic inhibition of SOX9 is inadvertently mimicking the pathogenic CDKL5-SOX9 axis, disrupting the pro-survival signal in RTECs [75].
- Solutions:
- Monitor CDKL5 Activity: Implement assays to measure CDKL5 kinase activity and phosphorylation status in renal tissue. Elevated levels may indicate a high risk of SOX9 suppression-related toxicity [75].
- Biomarker Panel: Beyond standard serum creatinine and BUN, include specific biomarkers like Kim-1 and Ngal in your toxicology studies for early detection of RTEC injury [75].
- Dose Optimization: Carefully titrate the inhibitor dosage and schedule to achieve the desired therapeutic effect in the target tissue while minimizing on-target toxicity in the kidneys.
FAQ 2: How can we leverage computational models to predict tissue-specific toxicity for novel SOX9 inhibitors early in the drug development pipeline?
Answer: Quantitative Structure-Activity Relationship (QSAR) models and other machine learning frameworks are valuable tools for early toxicity prediction. A systematic review of tissue-specific QSAR models highlights their use in predicting heart, lung, liver, CNS, and kidney toxicity [76]. More advanced models now incorporate Genotype-Phenotype Differences (GPD) between preclinical models and humans. These GPD-based models assess differences in gene essentiality, tissue expression, and network connectivity of the drug target (e.g., SOX9) to better predict human-specific toxic outcomes, such as neurotoxicity and cardiotoxicity, which are major causes of clinical failure [77].
Troubleshooting Guide: Addressing Gaps in QSAR Model Predictions
- Problem: A novel SOX9 inhibitor is predicted to have low toxicity by standard QSAR models, but you suspect risks due to the complex biology of SOX9.
- Potential Cause: Traditional chemical property-based models may overlook the biological context of SOX9's dual roles in different tissues [77].
- Solutions:
- Utilize GPD-Enhanced Models: Employ machine learning frameworks that integrate GPD features. This provides a more biologically grounded prediction by accounting for human-specific responses [77].
- Define the Applicability Domain (AD): Ensure the chemical space of your novel inhibitor falls within the AD of the QSAR model. Predictions for chemicals outside the model's training set are unreliable [76].
- Tissue-Specific Model Selection: Prioritize models specifically developed and validated for the tissues of highest concern for SOX9 biology, such as kidney, liver, and cartilage/ bone [76].
FAQ 3: Our in vitro models show efficacy for a SOX9-targeting therapy, but in vivo models reveal significant toxicity. How can we bridge this translational gap?
Answer: This is a common challenge, often stemming from the failure of in vitro systems to recapitulate the complex tissue microenvironment and systemic homeostasis of a whole organism. The "double-edged sword" nature of SOX9—where it promotes repair in some tissues (e.g., cartilage, intestine) but drives pathology in others (e.g., certain cancers)—further complicates translation [25] [1]. A critical factor is the difference in genotype-phenotype relationships (GPD) between cell lines/animal models and humans [77].
Troubleshooting Guide: Improving Translational Predictivity
- Problem: Promising in vitro results for a SOX9 inhibitor fail to translate to in vivo models due to off-target or on-target toxicity in unexpected tissues.
- Potential Cause: The in vitro system lacks the complexity of tissue-specific stem cell niches, immune interactions, and organ crosstalk where SOX9 operates [25] [75].
- Solutions:
- Incorporate Advanced Models: Use more complex in vitro systems, such 3D organoids or co-cultures with immune cells, to better model the tissue microenvironment where SOX9 functions [1].
- Conduct Tiered In Vivo Dosing: Begin with a thorough toxicokinetic (TK) analysis in vivo to understand the drug's exposure in different tissues. This helps determine if toxicity is due to higher than expected drug accumulation in sensitive organs [78].
- Profile Tissue-Specific Responses: Design in vivo studies to include detailed histological and molecular analyses of tissues where SOX9 is known to be critical, such as the kidneys, intestines, and cartilage [25] [75].
Data Presentation Tables
Table 1: Key Tissue-Specific Toxicities and Biomarkers Associated with SOX9 Pathway Perturbation
| Tissue/Organ | Potential Toxicity | Associated Biomarkers / Key Findings | Relevant Context |
|---|---|---|---|
| Kidney | Acute Kidney Injury (AKI), RTEC death | ↑ Kim-1, ↑ Ngal, ↑ BUN, ↑ Creatinine; Mediated via CDKL5-SOX9 axis [75]. | On-target toxicity from SOX9 inhibition disrupting pro-survival signals. |
| Intestine | Mucositis, Impaired regeneration post-injury | Loss of radioresistance in reserve intestinal stem cells (rISCs) [25]. | On-target effect; critical for patients receiving abdominal radiotherapy. |
| Cartilage | Impaired repair, Exacerbated OA | Reduced chondrogenic potential; Downregulation of cartilage integrity factors [14]. | On-target effect conflicting with therapeutic use in osteoarthritis. |
| Liver / Pancreas | Variable (context-dependent) | SOX9 is a marker for hepatic/pancreatic progenitor cells; role in Cancer Stem Cells (CSCs) [79] [1]. | Toxicity risk depends on whether SOX9 inhibition affects normal stem cell pools or only CSCs. |
Table 2: Evaluation of Predictive Model Types for Tissue-Specific Toxicity Assessment
| Model Type | Key Principles | Advantages | Limitations for SOX9-Targeted Therapies |
|---|---|---|---|
| QSAR Models [76] | Predicts toxicity from chemical structure. | High efficiency, rapid results, leverages public databases. | Often trained on small datasets; may miss SOX9's complex biological context [76]. |
| GPD-Based ML Models [77] | Incorporates differences in gene essentiality and tissue expression between models and humans. | Biologically grounded; better predicts human-specific neuro/cardio toxicity [77]. | Requires extensive genetic and phenotypic data; model accessibility can be poor [76] [77]. |
| In Vivo Preclinical Toxicology [78] | Direct assessment of toxicity in rodent and non-rodent models. | Provides integrated systemic and tissue-level data; regulatory requirement. | Poor translatability to humans due to inter-species biological differences [77]. |
Experimental Protocols
Detailed Methodology: Assessing SOX9 Inhibition-Related Renal Toxicity In Vivo
This protocol is adapted from studies investigating the CDKL5-SOX9 axis in Acute Kidney Injury (AKI) [75].
1. Objective: To evaluate the potential nephrotoxic effect of a novel SOX9 inhibitor using a mouse model of cisplatin-induced AKI.
2. Materials:
- Mice (e.g., C57BL/6)
- SOX9 inhibitor (formulated for injection)
- Cisplatin (for AKI model induction)
- Equipment for blood and tissue collection
- ELISA kits for BUN, Creatinine, Kim-1, Ngal
- Antibodies for Western Blot (anti-SOX9, anti-phospho-CDLK5, anti-Kim-1)
3. Procedure:
- Step 1: Group Allocation. Randomize mice into four groups (n=8-10):
- Group 1 (Vehicle Control): Receive vehicle only.
- Group 2 (SOX9 Inhibitor Control): Receive SOX9 inhibitor at the proposed therapeutic dose.
- Group 3 (Disease Control): Receive cisplatin (e.g., 20 mg/kg, single i.p. injection) + vehicle.
- Group 4 (Treatment Group): Receive cisplatin + SOX9 inhibitor.
- Step 2: Dosing and Monitoring. Administer treatments as per group designation. Monitor mice daily for weight loss and signs of distress.
- Step 3: Sample Collection. 72 hours post-cisplatin injection, collect blood via cardiac puncture under anesthesia. Collect both kidneys: one snap-frozen in liquid N2 for protein analysis, one fixed in formalin for histology.
- Step 4: Functional and Biomarker Analysis.
- Measure BUN and serum creatinine levels from blood samples.
- Homogenize frozen kidney tissue and perform Western Blot analysis for SOX9, phospho-CDLK5, and Kim-1 protein levels.
- Perform ELISA on tissue homogenates or serum to quantify Ngal.
- Step 5: Histological Assessment. Process fixed kidney tissue, section, and stain with Hematoxylin and Eosin (H&E). Score tubular damage (e.g., necrosis, cast formation) in a blinded manner.
4. Data Interpretation: A significant exacerbation of renal injury in Group 4 compared to Group 3 (e.g., higher BUN/creatinine, elevated Kim-1/Ngal, worse tubular damage score) indicates that SOX9 inhibition sensitizes the kidney to insult. Concurrent reduction in renal SOX9 protein and increase in phospho-CDLK5 would validate the on-target mechanism [75].
Signaling Pathways and Experimental Workflows
Diagram 1: SOX9's Dual Role in Tissue Repair and Toxicity
Diagram 2: Workflow for Integrated Preclinical Safety Profiling
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating SOX9 Inhibition and Toxicity
| Research Reagent | Function / Application | Example Use in SOX9 Studies |
|---|---|---|
| siRNA/shRNA targeting SOX9 [42] | RNA interference to knock down SOX9 mRNA and protein levels. | Validating on-target effects and probing SOX9 function in in vitro toxicity assays [75]. |
| CDKL5 Kinase Inhibitors [75] | Small molecule inhibitors to block CDKL5 kinase activity. | Mechanistic studies to confirm if toxicity is mediated via the CDKL5-SOX9 axis in renal models [75]. |
| Anti-Kim-1 / Anti-Ngal Antibodies [75] | Detection of kidney injury biomarkers via ELISA, Western Blot, or IHC. | Sensitive detection of renal tubular injury in preclinical models treated with SOX9 inhibitors [75]. |
| CRISPR/dCas9 Systems (for CRISPRa/i) [14] | Precise activation (CRISPRa) or interference (CRISPRi) of endogenous SOX9 or RelA. | Fine-tuning SOX9 expression to study threshold effects or to engineer cells with enhanced therapeutic profiles [14]. |
| Chondrogenesis Differentiation Kits | In vitro induction of chondrocyte differentiation from mesenchymal stromal cells (MSCs). | Assessing the impact of SOX9 inhibition on cartilage formation and repair mechanisms [14]. |
Comparative Tissue Vulnerability and Therapeutic Window Assessment
This guide explores the heightened sensitivity of the intestinal and skin epithelia to perturbations, with a specific focus on the consequences of inhibiting the transcription factor SOX9. These tissues share a fundamental characteristic: they are rapidly self-renewing, a process critically dependent on adult stem cell populations. SOX9 has been identified as a key regulator in both intestinal stem cells (ISCs) and epidermal stem cells, governing essential functions like proliferation, differentiation, and cell survival [80] [81]. Therefore, therapeutic strategies aimed at SOX9 inhibition, while potentially beneficial in contexts like cancer, carry a significant risk of disrupting the delicate balance of tissue maintenance and repair in the intestine and skin [82] [83]. This analysis provides a framework for researchers to understand, anticipate, and troubleshoot related challenges in their experimental and drug development workflows.
Vulnerability Profiles of Intestine and Skin
Quantitative Comparison of Tissue Vulnerabilities
Table 1: Comparative Vulnerability Profile of Intestine and Skin
| Feature | Intestinal Epithelium | Epidermal (Skin) Epithelium |
|---|---|---|
| Self-Renewal Rate | Entire epithelium renewed every 1-6 days in mammals [80] | Constant renewal; process culminates in terminally differentiated cells on the surface [81] |
| Stem Cell Niche | Crypts [80] | Basal layer of the interfollicular epidermis and hair follicle bulge [81] |
| Key SOX9 Function | Maintains reserve intestinal stem cells (rISCs); critical for radioresistance and regeneration post-injury [83] | Promotes keratinocyte proliferation; inhibits differentiation; protects from UVB-induced apoptosis [81] |
| Consequence of SOX9 Loss/Inhibition | Depletion of rISCs; impaired crypt regeneration and failure to recover from damage like radiation [83] | Disrupted epidermal barrier; impaired healing; potentially increased susceptibility to apoptosis [81] |
| Associated Pathologies from Dysfunction | Radiation enteritis; impaired healing [83] | Psoriasis; Basal Cell Carcinoma; impaired wound closure [81] |
Key Signaling Pathways and Molecular Mechanisms
Table 2: Key Molecular Regulators of Vulnerability in Intestine and Skin
| Molecular Regulator | Tissue | Function and Mechanism |
|---|---|---|
| Lgr5 | Intestine | Marker for actively proliferating stem cells; expressed in T3-induced proliferating cell clusters during development/remodeling [80]. |
| p21 | Skin & Intestine | Cell cycle inhibitor. SOX9 overexpression in skin keratinocytes downregulates p21, enhancing proliferation [81]. In melanoma, SOX9 induces cell cycle arrest by upregulating p21 [82]. |
| β-catenin | Skin | SOX9's C-terminal transcriptional activation domain (TAC) can inhibit β-catenin activity during chondrocyte differentiation, indicating a potential interplay in fate decisions [1]. |
| PRAME | Skin (Melanoma) | A melanoma antigen that acts as a dominant repressor of the retinoic acid (RA) receptor. SOX9 downregulates PRAME, restoring RA sensitivity in melanoma cells [82]. |
Figure 1: SOX9 Inhibition Side Effects on Tissue Repair. This diagram illustrates the distinct yet parallel pathways through which SOX9 inhibition disrupts critical repair mechanisms in the intestine and skin, leading to clinical manifestations.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating SOX9 Biology
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| CRISPR-dCas9 Systems (CRISPRa/i) | Precise transcriptional activation (CRISPRa) or interference (CRISPRi) of SOX9 or its targets without altering DNA sequence [14]. | Engineered MSCs with enhanced chondrogenic potential (Sox9 activation) and downregulated inflammation (RelA inhibition) for OA therapy [14]. |
| Inducible Transgenic Mouse Models (e.g., Krt14-rtTA; TRE-Sox9) | Spatially and temporally controlled gene expression in specific cell types (e.g., epidermal stem cells) in vivo [4]. | To study the real-time reprogramming of adult epidermal stem cells upon SOX9 re-activation and model BCC development [4]. |
| Recombinant Adenovirus (Sox9 or miR-Sox9) | Efficient overexpression or knockdown of SOX9 in vitro and in vivo via direct injection or transduction [81]. | Intradermal injection in rat skin to study SOX9's role in epidermal thickening and differentiation; or in cultured keratinocytes to assess UVB-induced apoptosis [81]. |
| Organoid Culture Systems | 3D ex vivo models that recapitulate the structure and function of native tissue, derived from adult stem cells [80]. | Modeling intestinal development, stem cell function, and response to toxins or therapeutic agents in a controlled environment. |
| ChIP-seq / CUT&RUN | Mapping the genome-wide binding sites of SOX9 and its associated epigenetic marks on chromatin [4]. | Identifying direct transcriptional targets of SOX9 and understanding its role as a pioneer factor in fate switching. |
Troubleshooting Guides & FAQs
Frequently Asked Questions (FAQs)
Q1: We are developing a SOX9 inhibitor for gastrointestinal cancer. What is the primary tissue repair-related toxicity we should monitor in our pre-clinical models? A1: The primary toxicity is radiation enteritis-like pathology and impaired intestinal regeneration. SOX9 is essential for the function and maintenance of reserve intestinal stem cells (rISCs), which are crucial for crypt regeneration after injury [83]. Inhibiting SOX9 will deplete these cells, rendering the intestine unable to repair itself following cytotoxic insults like radiotherapy or the inherent turnover of the epithelium.
Q2: In our in vitro skin model, SOX9 knockdown leads to unexpected cell death even without added stress. What is a potential mechanism? A2: SOX9 has pro-survival functions in epidermal keratinocytes. It protects cells from UVB-induced apoptosis by reducing PARP cleavage [81]. Its knockdown likely makes keratinocytes more vulnerable to baseline apoptotic signals. Investigate markers of apoptosis (e.g., cleaved caspase-3) and consider using lower-confluence cultures or supplementing with survival factors to mitigate this effect during experiments.
Q3: Why would a SOX9-targeted therapy designed for one tissue (e.g., cartilage in osteoarthritis) potentially cause side effects in a completely different tissue like the intestine or skin? A3: SOX9 is a master regulator with context-dependent functions across multiple tissues. While its activation in mesenchymal stromal cells (MSCs) can promote cartilage repair [14], it is equally critical for the stem cells maintaining the intestine and skin [83] [81]. A systemic therapeutic would not be tissue-specific, thereby disrupting SOX9's vital homeostatic roles in these other self-renewing organs, leading to side effects like impaired wound healing or gut damage.
Q4: Our data shows that SOX9 overexpression in melanoma cells inhibits proliferation, but literature suggests it promotes proliferation in normal keratinocytes. Is this a contradiction? A4: No, this highlights the context-dependent, "double-edged sword" nature of SOX9 [1]. In normal keratinocytes, SOX9 promotes proliferation and inhibits differentiation [81]. However, in certain cancers like melanoma, it can act as a tumor suppressor by inducing cell cycle arrest through upregulation of p21 [82]. The cellular outcome of SOX9 manipulation depends heavily on the cell type, its inherent molecular landscape, and disease state.
Troubleshooting Common Experimental Challenges
Challenge 1: Inconsistent Phenotype in SOX9 Knockdown Animal Models
- Potential Cause: The inherent redundancy and compensatory mechanisms within biological systems. Other SOX family members or related pathways may compensate for the loss of SOX9.
- Solution:
- Confirm Knockdown Efficiency: Use multiple methods (qPCR, Western blot, IHC) to verify SOX9 is reduced at both RNA and protein levels in the target tissue.
- Analyze Multiple Time Points: The phenotype may be time-sensitive. Analyze animals at different timepoints post-knockdown to capture transient or evolving effects.
- Inducible Knockdown Models: Use inducible Cre-lox or similar systems to achieve acute, rather than chronic, SOX9 deletion. This can help bypass developmental compensation and reveal the direct function of SOX9 in adult tissue maintenance [4].
Challenge 2: Differentiating Between Direct and Indirect Effects of SOX9 Inhibition
- Potential Cause: SOX9 is a transcription factor that regulates a vast network of downstream genes. Observed effects could be several steps removed from its direct action.
- Solution:
- Chromatin Immunoprecipitation (ChIP): Perform ChIP-seq or CUT&RUN to identify direct genomic binding targets of SOX9 in your cell or tissue of interest [4]. This distinguishes direct targets from genes affected by secondary cascades.
- Time-Course Experiments: Combine ChIP with RNA-seq over a time course after SOX9 inhibition. Direct targets will show rapid changes in expression following SOX9 dissociation from chromatin.
- Mechanistic Reconstitution: If SOX9 inhibits differentiation by repressing a specific gene, test whether restoring that gene's expression is sufficient to rescue the differentiation block even in the presence of SOX9.
Detailed Experimental Protocols
Protocol: Assessing Intestinal Regeneration After SOX9 Perturbation
Objective: To evaluate the functional impact of SOX9 inhibition on the regenerative capacity of the intestinal epithelium following a targeted injury.
Materials:
- SOX9 inhibitor or corresponding vehicle control.
- Laboratory mice (e.g., inducible SOX9 knockout or wild-type).
- Irradiation source (e.g., γ-irradiator) for controlled injury induction.
- Tissue fixation buffer (e.g., 10% Neutral Buffered Formalin).
- Antibodies for immunohistochemistry: Anti-SOX9, Anti-Olfm4, Anti-Ki67.
- Key Control: Include a group where a SOX9 inducer (e.g., via targeted nanocarrier) is administered post-injury to test if it can rescue regeneration, as hypothesized in [83].
Method:
- Pre-treatment: Administer SOX9 inhibitor or vehicle control to mice for a predetermined period (e.g., 3-5 days) to achieve target engagement before injury.
- Induce Injury: Subject mice to a sublethal dose of whole-body irradiation (e.g., 8-12 Gy) to deplete the sensitive actively proliferating stem cells and challenge the reserve ISC compartment [83].
- Monitor Recovery: Continue inhibitor/vehicle treatment and monitor mice daily. Sacrifice cohorts at critical timepoints (e.g., 24, 72, and 96 hours post-irradiation).
- Tissue Collection and Analysis:
- Collect the small intestine, Swiss-roll it, and fix for histology.
- Perform H&E staining to assess general crypt morphology and villus structure.
- Conduct immunohistochemistry for SOX9, the stem cell marker Olfm4, and the proliferation marker Ki67.
- Quantitative Analysis: Count the number of regenerating crypts (defined as crypts containing ≥10 Ki67+ cells) per intestinal circumference. Measure the percentage of crypts that are SOX9-positive.
Troubleshooting Note: If no regenerative defect is observed, consider titrating the radiation dose or the concentration of the SOX9 inhibitor. The rISC population is notably radioresistant, so a sufficient challenge and potent inhibition are required to unmask the phenotype [83].
Protocol: Evaluating SOX9's Role in Keratinocyte Function In Vitro
Objective: To determine the effect of SOX9 modulation on human epidermal keratinocyte proliferation, differentiation, and apoptosis.
Materials:
- Primary Human Epidermal Keratinocytes (HEKa).
- Keratinocyte-SFM medium with growth supplements.
- Recombinant adenovirus: Ad-GFP (control), Ad-GFP-SOX9 (for overexpression), Ad-miR-SOX9 (for knockdown) [81].
- Calcium chloride (for inducing differentiation).
- UVB light source.
- Western blot reagents: Antibodies against SOX9, Involucrin, Loricrin, cleaved PARP, p21.
- Cell proliferation assay kit (e.g., MTT or BrdU).
Method:
- Cell Culture and Transduction: Culture HEKa in growth medium. At 50-60% confluence, transduce with Ad-GFP, Ad-GFP-SOX9, or Ad-miR-SOX9 at a predetermined MOI.
- Proliferation Assay: 24h post-transduction, seed cells for proliferation assay. Measure cell viability/proliferation daily for 3-4 days using the chosen assay kit.
- Differentiation Assay: 24h post-transduction, switch cells to high-calcium medium (e.g., 1.2 mM CaCl₂) to induce differentiation. Maintain some cells in low-calcium medium as an undifferentiated control. Harvest cells 48-72h later for Western blot analysis of differentiation markers (Involucrin, Loricrin) and p21.
- Apoptosis Assay: 48h post-transduction, expose cells to a calibrated dose of UVB irradiation (e.g., 20-50 mJ/cm²). Harvest cells 24h post-UVB and analyze lysates by Western blot for cleaved PARP as a marker of apoptosis.
Expected Outcomes: As demonstrated in [81], SOX9 overexpression should enhance proliferation, suppress differentiation marker expression, and protect against UVB-induced apoptosis. SOX9 knockdown should have the opposite effects.
Troubleshooting Guide: SOX9 Inhibition in Tissue Repair Models
This guide addresses common experimental challenges when investigating SOX9 inhibition and its dose-response effects on tissue repair mechanisms.
FAQ 1: In our lung organoid model, SOX9 inactivation produces conflicting branching phenotypes compared to literature. What could explain this?
- Issue: Discrepancies in branching morphogenesis outcomes after SOX9 inhibition.
- Solution:
- Check Model System Differences: Studies show significant differences between murine and human lung development. SOX9 inactivation in human embryonic stem cell (hESC)-derived lung organoids reduces proliferative capacity and promotes apoptosis but does not completely block lung epithelium differentiation, unlike some mouse models where it causes lethal branching defects [84].
- Verify Knockout Efficiency: Use genotyping to confirm complete indel formation in both SOX9 alleles. In human models, the transactivation domain is often targeted [84].
- Assess Timing of Inhibition: The stage of development (e.g., pseudoglandular vs. canalicular) is critical. Use precise, stage-specific promoters or inducible systems (e.g., Tet-off) for inactivation [84] [63].
- Preventative Best Practice: Always use matched control cell lines (e.g., wild-type H9 hESCs) and confirm SOX9 protein depletion via Western blot alongside genomic confirmation [84].
FAQ 2: We observe unexpected hepatotoxicity in our in vivo SOX9 inhibition study. Is this a known off-target effect?
- Issue: Liver toxicity during systemic SOX9 inhibition experiments.
- Solution:
- Review SOX9 Expression Baselines: SOX9 is expressed in embryonic liver progenitor cells. Assess baseline SOX9 in adult liver in your specific model, as it can reactivate during regeneration [1].
- Optimize Delivery and Dosing: Consider tissue-specific, targeted delivery systems (e.g., hydrogel-based local delivery) to minimize systemic exposure and reduce liver load [59].
- Evaluate Alternative Mechanisms: Conduct RNA-Seq to determine if toxicity stems from off-target CRISPR/Cas9 activity or disruption of related SOX family genes. Use gRNAs with validated specificity and include multiple control groups [14] [63].
- Preventative Best Practice: Perform a thorough pilot dose-escalation study, monitoring standard liver enzymes (ALT, AST) and histology to establish a therapeutic window before main experiments.
FAQ 3: Our chondrogenesis assay shows high variability in ECM output after titrating a SOX9 inhibitor. How can we improve reproducibility?
- Issue: Inconsistent production of aggrecan and type II collagen in mesenchymal stromal cell (MSC) chondrogenesis assays.
- Solution:
- Standardize Differentiation Protocols: Use precisely defined chondrogenic differentiation media containing dexamethasone, cAMP, and IBMX. Replace media every 3-4 days consistently [84] [63].
- Co-activate Compensatory Pathways: SOX9 inhibition can be partially rescued by activating parallel pathways. Consider testing the co-expression of TGFβ1, which synergistically enhances SOX9-driven extracellular matrix (ECM) synthesis [63].
- Quantify ECM Robustly: Use quantitative methods like qRT-PCR for ACAN and COL2A1, supplemented by Alcian blue staining and spectrophotometric quantification, rather than qualitative scoring alone [63].
- Preventative Best Practice: Use low-passage cells, aliquot all induction factors to minimize freeze-thaw variability, and include a internal positive control (e.g., a well-defined SOX9 activator sample) in every assay plate.
FAQ 4: Dose-dependent SOX9 inhibition unexpectedly promotes a pro-inflammatory response in our joint injury model. How should we investigate this?
- Issue: Increased inflammation or expression of catabolic enzymes at certain inhibitor concentrations.
- Solution:
- Investigate Cross-Talk with NF-κB Pathway: SOX9 and the NF-κB pathway (via transcription factor RelA) can exhibit mutual antagonism. Inhibiting SOX9 may disinhibit RelA, increasing MMP13 and IL6 expression. Validate by measuring phospho-RelA and NF-κB target genes (e.g., NFKBIA) [14].
- Profile Immune Cell Infiltration: Use flow cytometry to characterize changes in macrophage polarization (M1 vs. M2) and T-cell populations in the synovium or regenerating tissue [1] [14].
- Titrate for Biphasic Effects: The role of SOX9 in immunity is "Janus-faced." Re-test a wider range of doses; very low doses of inhibitor might paradoxically stimulate a pro-repair response, while high doses drive inflammation [1].
- Preventative Best Practice: When setting up a new injury model, include a comprehensive dose-range finder experiment that measures not only structural repair markers but also a panel of key inflammatory cytokines.
Table 1: SOX9 Manipulation Outcomes in Regenerative Tissue Models
| Tissue / Disease Model | Intervention Type | Key Outcome Measures | Observed Threshold / Effective Dose | Reference |
|---|---|---|---|---|
| Osteoarthritis (OA) | CRISPR/dCas9-SOX9 activation in BMSCs | Cartilage degradation attenuation, pain relief | Significant palliation of OA pain vs. unmodified cells [14] | [14] |
| Intervertebral Disc (IVD) Degeneration | ToMSCs with SOX9 & TGFβ1 co-expression | Disc hydration (MRI), Aggrecan & COL2A1 synthesis, inflammation reduction | Superior ECM synthesis & reduced mechanical allodynia vs. single-factor [63] | [63] |
| Human Lung Organoids | SOX9 gene knockout in hESCs | Proliferative capacity, Apoptosis, Epithelial differentiation | Reduced proliferation, promoted apoptosis, no block in differentiation [84] | [84] |
| Bronchopulmonary Dysplasia (BPD) | Exogenous SOX9 plasmid | Radial alveolar count (RAC), AEC-II to AEC-I differentiation | Improved alveolarization, increased RAC value [85] | [85] |
Detailed Experimental Protocols
Protocol 1: Generating SOX9-Modified Human Lung Organoids
This protocol outlines the creation of SOX9-null lung organoids from human embryonic stem cells (hESCs) to study the role of SOX9 in lung development and repair [84].
SOX9 Knockout in hESCs:
- Design: Use two gRNAs (e.g., 5′-GGGCTGTAGGCGATCTGTTGGGG-3′ and 5′-TCCTACTACAGCCACGCGGCAGG-3′) targeting exon 3 of the SOX9 gene, cloned into a CRISPR/Cas9 plasmid with a puromycin resistance gene.
- Transfection & Selection: Transfect H9 hESCs with gRNAs and Cas9 plasmid. Apply puromycin selection post-transfection. Seed cells at limiting dilution for subcloning.
- Genotyping: Isolate genomic DNA from individual colonies. Screen for SOX9 deletion by PCR amplification and sequencing of the fragment spanning the two gRNA sites.
Stepwise Differentiation to Lung Organoids:
- Definitive Endoderm (Days 1-3): Culture hESCs at ~90% confluence for 3 days in RPMI1640 medium with 100 ng/mL activin A and 2 μM CHIR99021.
- Anterior Foregut Endoderm (Days 4-7): Switch to Advanced DMEM/F12 supplemented with 200 ng/mL Noggin, 500 ng/mL FGF4, 2 μM CHIR99021, and 10 μM SB431542.
- "Ventralized" AFE (Days 8-14): Embed cells in Matrigel for 3D culture. Culture in DMEM/F12 with 20 ng/mL BMP4, 0.5 μM all-trans retinoic acid, 3.5 μM CHIR99021, 1% Glutamax, and 2% B27 supplement.
- Lung Progenitor Induction (Days 15-21): Culture VAFE-enriched cells in DMEM/F12 with 3 μM CHIR99021, 10 ng/mL FGF10, 10 ng/mL KGF, and 20 μM DAPT.
- Airway Organoid Maturation (Day 21+): Culture in Ham’s F12 medium with 50 nM dexamethasone, 100 nM 8-Br-cAMP, 100 nM IBMX, 10 ng/mL KGF, 1% B-27, 0.25% BSA, 15 mM HEPES, 0.8 mM CaCl2, and 0.1% ITS premix.
Protocol 2: Engineering SOX9 & TGFβ1 Co-Expressing MSCs for Disc Regeneration
This protocol details the use of CRISPR/Cas9 to genetically engineer tonsil-derived MSCs (ToMSCs) for enhanced intervertebral disc regeneration [63].
Isolation and Culture of ToMSCs:
- Obtain human tonsil tissue fragments from consented patients.
- Wash with PBS, mince, and digest for 30 min at 37°C in RPMI 1640 with 10 μg/mL DNase I and 210 U/mL collagenase type I.
- Filter digested tissue, wash, and isolate mononuclear cells using Ficoll-Paque density gradient centrifugation.
- Seed cells in Dulbecco’s modified Eagle’s medium F12 supplemented with 10% FBS, 100 μg/mL streptomycin, and 100 U/mL penicillin.
Genetic Engineering with CRISPR/Cas9:
- Vector Construction: Clone a single cistronic gene cassette containing SOX9 and TGFβ1 (separated by P2A sequences) into the AAVS1 "safe harbor" locus of a plasmid under a Tet-off inducible promoter. Include a C-terminal 6His tag on TGFβ1 for detection.
- Transfection: Transfect ToMSCs with the constructed plasmid (e.g., pAAVS1-puro-Tetoff-SOX9-TGFβ1-CAG-tTA-Advanced) and CRISPR/Cas9 components.
- Validation: Confirm successful integration and protein expression via Western blot and qRT-PCR. Test inducibility by withdrawing doxycycline from the culture medium.
In Vivo Assessment in Rat Model:
- IVD Degeneration Model: Induce degeneration in rat tail discs via needle puncture.
- Cell Administration: Inject engineered ToMSCs into the injured disc space.
- Outcome Monitoring:
- Functional Pain: Assess mechanical allodynia weekly for 6 weeks using the von Frey test.
- Structural Repair: Evaluate disc hydration via T2-weighted MRI and perform histological analysis for aggrecan and type II collagen.
Signaling Pathways and Experimental Workflows
SOX9 in Chondroprotection & Inflammation
MSC Engineering for Disc Regeneration
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for SOX9 and Tissue Regeneration Research
| Reagent / Material | Function / Application | Example & Notes |
|---|---|---|
| CRISPR/dCas9 Systems | For precise gene activation (CRISPRa) or inhibition (CRISPRi) of SOX9. | dSpCas9-VP64 (activation), dSaCas9-KRAB (inhibition); allows fine-tuning without permanent knockout [14]. |
| Tet-Off Inducible System | Controls the timing of transgene (e.g., SOX9, TGFβ1) expression. | Enables temporal control; expression is active in the absence of doxycycline, mitigating risks of continuous overexpression [63]. |
| AAVS1 Safe Harbor Targeting Plasmid | Ensures stable, predictable transgene integration without disrupting endogenous genes. | pAAVS1-puro-Tetoff-SOX9-TGFβ1-CAG-tTA-Advanced plasmid for safe genetic engineering of MSCs [63]. |
| Chondrogenic Differentiation Media | Induces chondrocyte differentiation from MSC sources. | Contains dexamethasone, 8-Br-cAMP, IBMX, ITS, and KGF. Essential for in vitro cartilage formation assays [84] [63]. |
| Tonsil-derived MSCs (ToMSCs) | A potent MSC source for cartilage and disc regeneration studies. | High proliferation rates, lower immunogenicity. Isolated from pediatric tonsillectomy tissue [63]. |
| Lung Organoid Culture Media | For stepwise differentiation of hPSCs into 3D lung organoids. | Sequential media containing Activin A, CHIR99021, Noggin, FGF4, BMP4, and retinoic acid [84]. |
The transcription factor SOX9 (SRY-related HMG-box gene 9) represents a critical regulatory node governing fundamental cellular processes across diverse tissue types. As a transcription factor containing a highly conserved high mobility group (HMG) box DNA-binding domain, SOX9 regulates gene expression programs essential for development, stem cell maintenance, and tissue repair [2] [42]. Recent research has illuminated its complex, context-dependent functionalities, wherein SOX9 can act as both a promotor of regenerative repair and a driver of pathological fibrosis and cancer progression [31] [1]. This technical support document addresses the practical experimental challenges inherent to investigating SOX9-dependent pathways, with particular emphasis on the implications of SOX9 inhibition for tissue repair mechanisms. The dual nature of SOX9—demonstrated by its capacity to facilitate scarless regeneration when appropriately regulated yet promote fibrotic outcomes when persistently activated—necessitates precise methodological approaches for researchers and drug development professionals [31] [86]. This guide provides standardized protocols, troubleshooting resources, and analytical frameworks to support rigorous investigation of SOX9 biology across different tissue contexts and experimental models.
Key Molecular Signatures of SOX9 Activity
SOX9 activation triggers distinct transcriptional programs and cellular behaviors that vary significantly by tissue type and physiological context. The table below summarizes the principal SOX9-dependent molecular signatures observed across different tissue environments.
Table 1: Comparative SOX9-Dependent Molecular Signatures Across Tissues
| Tissue/Cell Type | SOX9-Associated Molecular Signature | Functional Outcome | Experimental Model |
|---|---|---|---|
| Kidney Tubular Cells | SOX9on → CDH6+ (Cadherin-6); SOX9off → CDH6- [31] | Regeneration vs. Fibrosis Switch: SOX9 persistence → fibrosis; SOX9 shutdown → scarless repair [31] | Mouse kidney injury model [31] |
| Intestinal Stem Cells | SOX9 maintains reserve stem cell population; regulates proliferation via cell cycle arrest/DNA repair genes [25] | Radioresistance: Promotes regeneration after radiation-induced injury [25] | SOX9 knockout intestinal epithelium [25] |
| Hepatocellular Carcinoma | SOX9 promotes self-renewal, tumorigenicity, symmetrical cell division in Cancer Stem Cells (CSCs) [25] | Tumor Propagation: Essential for cancer stem cell maintenance [25] | Xenograft mouse models [25] |
| Type 2 Alveolar Cells (Lung) | SOX9 inversely correlates with β-catenin; promotes AEC-II → AEC-I differentiation [85] | Alveolar Differentiation: Alleviates bronchopulmonary dysplasia (BPD) pathology [85] | Hyperoxia-induced BPD rat model [85] |
| Colorectal Cancer | SOX9 loss → EMT, SOX2 stem cell factor upregulation, increased invasion [52] | Tumor Suppression: SOX9 inactivation promotes progression and metastasis [52] | Apc/Sox9 double mutant mouse model [52] |
| Chondrocytes & Cartilage | Activates Col2a1, Col9a1, Col11a2, Acan; represses Col10a1 [2] | Chondrogenesis: ECM production and inhibition of hypertrophy [2] | Campomelic dysplasia models [2] |
Essential Research Reagent Solutions
The investigation of SOX9-dependent pathways requires a specialized toolkit of research reagents designed to modulate and measure SOX9 activity in various experimental systems.
Table 2: Essential Research Reagents for SOX9 Investigation
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| SOX9 Inhibitors | Small molecule inhibitors (targeting SOX9-DNA binding), SOX9-siRNA, SOX9-shRNA [42] | Cancer research (CSC targeting), modulation of stem cell differentiation [25] [42] | Potential enteritis side effect from reduced intestinal regeneration; consider tissue-specific delivery systems [25] |
| SOX9 Activators/Inducers | Fgf8, RelA (NF-κB pathway) [25] | Enhancing radioresistance in normal intestinal tissue, promoting crypt repair [25] | Timing critical—post-injury application may support regeneration [25] |
| Genetic Models | CDX2P-CreERT2; Apcfl/fl; Sox9fl/fl mice [52] | Studying SOX9 in intestinal tumorigenesis, regeneration, and tissue-specific knockout [52] | Tamoxifen-inducible system allows temporal control; Apc/Sox9 double mutants show enhanced invasion [52] |
| Detection Antibodies | Anti-SOX9 (nuclear localization), Anti-β-catenin (nuclear/cytoplasmic vs. membrane), Anti-SPC (AEC-II), Anti-AQP5 (AEC-I) [85] [52] | Lineage tracing, protein localization assessment, differentiation status [85] [52] | Subcellular localization critical for interpretation (nuclear SOX9 = active) [85] |
| Nanocarrier Systems | Ligand-targeted nanocarriers conjugated with SOX9 inhibitors/siRNA [25] | Tissue-specific delivery to minimize side effects, CSC-targeting [25] | Glycan-based ligands show promise for CSC-specific targeting [25] |
Signaling Pathway Visualizations
SOX9 in Renal Repair and Fibrosis Switch
Figure 1: SOX9 Switch in Renal Repair vs. Fibrosis. SOX9 activation after injury can lead to either regeneration or fibrosis depending on its persistence, with CDH6 as a key marker of the fibrotic pathway [31].
SOX9-Wnt/β-catenin Regulatory Circuit
Figure 2: SOX9-Wnt/β-catenin Regulatory Circuit. This mutual antagonism regulates differentiation in lung development and maintains tissue homeostasis in colorectal epithelium [85] [52].
Experimental Protocols & Methodologies
Protocol: Assessing SOX9-Dependent Renal Repair and Fibrosis
Background: This protocol outlines the methodology for evaluating the dual role of SOX9 in renal regeneration versus fibrosis, based on the SOX9 switch mechanism identified by Aggarwal et al. [31].
Materials:
- CDX2P-CreERT2 transgenic mice (or other tissue-specific inducible Cre models)
- Tamoxifen for Cre induction
- Antibodies: anti-SOX9, anti-CDH6, anti-β-catenin
- Single-cell RNA sequencing platform
- Histopathology reagents (H&E staining, Masson's Trichrome for fibrosis)
Procedure:
- Animal Model Establishment:
- Induce kidney injury in mouse model (e.g., ischemia-reperfusion, toxin-mediated)
- Administer tamoxifen to activate Cre recombinase in inducible systems
Temporal Sampling:
- Collect tissue samples at multiple timepoints: 24h, 72h, 7d, 14d, 28d post-injury
- Process samples for (a) histology, (b) protein analysis, (c) single-cell RNA sequencing
Single-Cell RNA Sequencing:
- Prepare single-cell suspensions from kidney tissue
- Perform scRNA-seq using standard platforms (10X Genomics, etc.)
- Analyze data for SOX9 expression trajectories and co-expression with CDH6
Lineage Tracing:
- Utilize Sox9-CreERT2;Rosa26-tdTomato mice for lineage tracing
- Track descendant cells at different timepoints post-injury
Functional Assessment:
- Evaluate renal function (serum creatinine, BUN)
- Quantify fibrotic area (Masson's Trichrome)
- Assess tubular injury score (histopathology)
Troubleshooting:
- Issue: Inconsistent SOX9 activation after injury Solution: Optimize injury model severity; verify Cre recombinase activity with reporter mice
- Issue: Poor single-cell viability for sequencing Solution: Optimize digestion protocol; use viability enrichment methods
Protocol: Evaluating SOX9 Inhibition in Cancer Stem Cell Models
Background: This protocol describes methods for investigating SOX9 inhibition in cancer stem cells (CSCs), particularly relevant for gastrointestinal cancers and therapeutic development [25].
Materials:
- SOX9 inhibitors (small molecules) or SOX9-siRNA/shRNA
- Nanocarrier systems (for targeted delivery)
- Cancer stem cell lines (pancreatic, hepatocellular, colorectal)
- Radiation source (for radioresistance studies)
- Sphere formation assay reagents
Procedure:
- SOX9 Inhibition:
- Treat CSCs with SOX9 inhibitors or transfected with SOX9-targeting siRNA
- Include appropriate controls (vehicle, scrambled siRNA)
- Use nanocarrier-conjugated inhibitors for targeted approaches
Radioresistance Assay:
- Irradiate cells at varying doses (2-8 Gy)
- Assess cell survival (clonogenic assay)
- Measure apoptosis (Annexin V/PI staining)
Cancer Stem Cell Properties:
- Perform sphere formation assays under non-adherent conditions
- Evaluate self-renewal through serial sphere formation
- Assess differentiation capacity
Invasion and Metastasis:
- Conduct Transwell invasion assays
- Evaluate epithelial-mesenchymal transition (EMT) markers (E-cadherin, vimentin)
- Measure SOX2 expression (stemness marker)
In Vivo Validation:
- Establish xenograft or orthotopic models
- Treat with SOX9 inhibitors ± radiotherapy
- Monitor tumor growth, metastasis, and survival
Troubleshooting:
- Issue: Off-target effects of SOX9 inhibition Solution: Use multiple inhibition approaches (pharmacological, genetic); include rescue experiments
- Issue: Poor nanocarrier delivery efficiency Solution: Optimize ligand density; test different nanocarrier formulations
Frequently Asked Questions (FAQs)
SOX9 Biology and Experimental Design
Q1: Why does SOX9 appear to have contradictory roles—promoting regeneration in some contexts but driving fibrosis and cancer in others?
A: SOX9 exhibits context-dependent functionality determined by multiple factors:
- Temporal regulation: Transient SOX9 activation promotes regeneration, while persistent expression drives pathology [31] [86]
- Cellular microenvironment: SOX9 interacts with different partner factors (β-catenin, SF1, Sox5/6) that determine transcriptional outcomes [2]
- Tissue-specific programs: SOX9 regulates distinct gene networks in various tissues—chondrogenesis genes in cartilage, EMT regulators in epithelium [2] [52]
- Dosage effects: Heterozygous vs. homozygous inactivation produces different phenotypes in mouse models [52]
Q2: What are the key considerations when selecting SOX9 inhibition strategies for experimental or therapeutic purposes?
A: Strategy selection should consider:
- Specificity: Small molecules vs. genetic approaches (siRNA, CRISPR) offer different specificity levels
- Delivery method: Nanocarriers improve tissue-specific delivery, crucial for minimizing side effects [25]
- Temporal control: Inducible systems allow precise timing of inhibition relative to injury/therapy
- Compensation mechanisms: Consider potential redundancy with other SOXE proteins (Sox8, Sox10) [2]
- Toxicity monitoring: Particularly for intestinal regeneration impairment [25]
Technical Troubleshooting
Q3: How can I resolve inconsistent results in SOX9 localization studies?
A: Inconsistent SOX9 localization typically stems from:
- Sample processing: Optimize fixation and antigen retrieval methods
- Subcellular fractionation: Validate fractionation efficiency using compartment-specific markers
- Activity markers: Distinguish between total SOX9 and active SOX9 using phosphorylation status (PKA-phosphorylated SOX9 is nuclear and active) [2]
- Context interpretation: Nuclear SOX9 indicates active transcription, while cytoplasmic may represent inactive or regulated pools
Q4: What approaches can validate the specificity of SOX9 inhibitors in cellular models?
A: Employ a multi-pronged validation strategy:
- Genetic confirmation: Use SOX9 knockdown/knockout as comparator
- Rescue experiments: Express SOX9 resistant to inhibition (if possible)
- Target engagement assays: CETSA, cellular thermal shift assays
- Transcriptomic validation: RNA-seq to verify expected signature changes
- Off-target screening: Assess related transcription factors (other SOX proteins)
Data Interpretation and Translation
Q5: How can I determine whether SOX9 is functioning as an oncogene or tumor suppressor in my experimental system?
A: Evaluate these key parameters:
- Expression correlation: Compare SOX9 levels with differentiation markers (inverse correlation suggests oncogene) [52]
- Genetic alteration status: Assess SOX9 mutations (loss-of-function suggests tumor suppressor) [52]
- Functional studies: Conduct both gain and loss-of-function experiments
- Clinical correlation: Analyze human tumor databases for SOX9 expression-survival correlations
- Pathway analysis: Determine if SOX9 activates or represses Wnt/β-catenin signaling in your context [85] [52]
Q6: What strategies can mitigate the side effects of SOX9 inhibition on tissue repair mechanisms?
A: Several approaches can minimize adverse effects:
- Tissue-specific delivery: Nanocarriers with ligands targeting specific cell types [25]
- Timing optimization: Transient inhibition with careful scheduling around injury events
- Combinatorial approaches: SOX9 inhibition paired with protective factors for normal tissues
- Compensatory pathway activation: Co-administration of factors that support regeneration
- Monitoring regimens: Establish sensitive biomarkers for tissue repair impairment
The investigation of SOX9-dependent pathways requires sophisticated methodological approaches that account for its contextual functions across tissues. This technical support document provides standardized frameworks for evaluating SOX9 biology while addressing the practical challenges faced by researchers. By implementing these protocols, troubleshooting guides, and analytical tools, scientists can advance our understanding of SOX9's dual roles in regeneration and disease, ultimately facilitating the development of targeted therapeutic strategies that maximize beneficial outcomes while minimizing adverse effects on tissue repair mechanisms.
FAQ: SOX9 Inhibition in Cancer Therapeutics
Q1: What is the primary therapeutic challenge associated with targeting SOX9 in cancer? SOX9 presents a "double-edged sword" or "janus-faced" role, creating a significant challenge for therapeutic targeting. On one hand, inhibiting SOX9 can combat tumor immune escape and reverse chemoresistance in various cancers. On the other hand, SOX9 is essential for maintaining macrophage function, contributing to cartilage formation, and supporting tissue regeneration and repair. This dual function means that inhibiting SOX9 for cancer treatment could potentially impair normal tissue repair mechanisms [1].
Q2: How does SOX9 contribute to chemotherapy resistance in colorectal cancer? In colorectal cancer, SOX9 promotes resistance to oxaliplatin by activating a specific DNA damage repair pathway. It forms a complex with MMS22L, a protein required for repairing stalled replication forks and DNA double-strand breaks. SOX9 regulates MMS22L expression and promotes its nuclear translocation upon oxaliplatin treatment, enhancing the cancer cell's ability to repair chemotherapy-induced DNA damage and survive treatment [87].
Q3: What is the relationship between SOX9 and Cancer Stem Cells (CSCs) in therapy resistance? SOX9 is a key marker and regulator of cancer stem-like cells (CSCs) in multiple digestive system cancers, including pancreatic cancer and hepatocellular carcinoma. It promotes essential CSC properties like self-renewal, tumor initiation, and division. Since CSCs are inherently resistant to conventional anti-cancer therapies, the overexpression of SOX9 in these cells contributes significantly to radioresistance and chemoresistance. Inhibition of SOX9 is proposed as a strategy to eradicate CSCs and overcome this resistance [25].
Q4: Are there targeted strategies to overcome SOX9-mediated PARP inhibitor resistance? Recent research has identified a promising strategy to overcome SOX9-mediated PARP inhibitor resistance in ovarian cancer. The deubiquitinating enzyme USP28 stabilizes the SOX9 protein by preventing its degradation. Using the specific USP28 inhibitor AZ1 promotes the breakdown of SOX9, impairs DNA damage repair capabilities, and re-sensitizes ovarian cancer cells to PARP inhibitors like olaparib. This suggests that combining USP28 inhibitors with PARPi could be an effective clinical strategy [33].
Troubleshooting Guide: Common Experimental Issues in SOX9 Research
Problem 1: Inconsistent Results in SOX9 Knockdown Experiments
- Potential Cause: Incomplete or transient SOX9 knockdown leading to variable phenotypic effects.
- Solution:
- Validate knockdown efficiency using multiple methods (Western blot, qRT-PCR).
- Use stable, inducible knockdown or knockout cell lines (e.g., with lentiviral shRNA or CRISPR-Cas9 systems).
- Employ multiple distinct shRNAs or sgRNAs to rule off-target effects. The sequence
CCGGCTCCACCTTCACCTACATGAACTCGAGTTCATGTAGGTGAAGGTGGAGTTTTTGhas been used successfully in prior studies [87].
Problem 2: Failure to Recapitulate SOX9-Mediated Drug Resistance In Vitro
- Potential Cause: The cellular model lacks the appropriate context, such as the SOX9-MMS22L axis or other co-factors.
- Solution:
- Confirm the endogenous expression levels of both SOX9 and MMS22L in your cell line.
- Mimic clinical scenarios by generating resistant cell lines through long-term, low-dose exposure to the chemotherapeutic drug (e.g., oxaliplatin) [87].
- Assess the nuclear translocation of MMS22L upon drug treatment in your model, as this is a key mechanistic step [87].
Problem 3: High Toxicity in Normal Tissues During SOX9 Inhibition In Vivo
- Potential Cause: SOX9's critical role in reserve intestinal stem cells (rISCs) and tissue repair is being broadly inhibited.
- Solution:
- Investigate targeted delivery systems for SOX9 inhibitors, such as drug-loaded nanocarriers conjugated with ligands specific to cancer stem cells, to minimize off-target effects [25].
- Explore the timing of therapy; for instance, using SOX9 inhibitors concurrently with radiotherapy but administering SOX9 inducers after high-dose RT completion to protect normal intestinal crypts and promote regeneration [25].
Table 1: SOX9 Expression and Correlation with Clinical Outcomes in Human Cancers
| Cancer Type | SOX9 Expression vs. Normal | Correlation with Prognosis | Associated Therapy Resistance |
|---|---|---|---|
| Colorectal Cancer (CRC) | Higher [87] | Poor overall survival [87] | Oxaliplatin resistance [87] |
| Ovarian Cancer | Higher [33] | Poor prognosis, lymph node metastasis [33] | Cisplatin resistance, PARP inhibitor (Olaparib) resistance [33] |
| Various Solid Tumors | Frequently overexpressed [1] | Advanced tumor stage, worse survival [1] | General chemoresistance and malignant potential [1] |
Table 2: Key Experimental Findings on SOX9 and Therapy Resistance
| Experimental Context | Key Finding | Proposed Mechanism |
|---|---|---|
| CRC + Oxaliplatin [87] | SOX9 knockdown increases oxaliplatin sensitivity. | SOX9 complexes with MMS22L to promote DNA double-strand break repair. |
| Ovarian Cancer + PARP Inhibitor [33] | USP28 inhibition sensitizes cells to Olaparib. | USP28 stabilizes SOX9; inhibition leads to SOX9 degradation, impairing DNA repair. |
| GI Cancer + Radiotherapy [25] | SOX9 knockout intestinal crypts undergo apoptosis post-RT. | SOX9 is required for the regeneration and radioresistance of reserve intestinal stem cells. |
Detailed Experimental Protocols
Protocol 1: Evaluating SOX9's Role in Chemoresistance via the SOX9-MMS22L Axis
This protocol is adapted from research on oxaliplatin resistance in colorectal cancer [87].
1. Cell Line Preparation:
- Cell Lines: Use human colorectal cancer cell lines (e.g., HCT116, RKO, SW480).
- Culture: Maintain cells in DMEM supplemented with 10% FBS and 1% penicillin-streptomycin at 37°C with 5% CO2.
2. Genetic Modulation:
- Overexpression: Transfect cells with a CMV-MCS-3FLAG-SV40-Neomycin lentiviral vector expressing full-length human SOX9.
- Knockdown: Infect cells with a U6-MCS-Ubiquitin-cherry-IRES-puromycin shSOX9 lentiviral vector. A validated shRNA sequence is:
- Forward:
5′-CCGGCTCCACCTTCACCTACATGAACTCGAGTTCATGTAGGTGAAGGTGGAGTTTTTG-3′ - Reverse:
5′-GATCCAAAAACTCCACCTTCACCTACATGA ACTCGAGTTCATGTAGGTGAAGGTGGAG-3′
- Forward:
- Selection: Select stably transduced cells using 4 μg/ml puromycin.
3. Drug Sensitivity Assay:
- Treat modulated cells and control cells with a range of oxaliplatin concentrations.
- Assess cell viability after 48-72 hours using assays like MTT or CellTiter-Glo.
- Calculate IC50 values to quantify changes in drug sensitivity.
4. Mechanistic Validation:
- Immunofluorescence: After oxaliplatin treatment, fix cells and stain for MMS22L and a nuclear marker (e.g., DAPI). Confirm SOX9-dependent nuclear translocation of MMS22L.
- Western Blotting: Analyze protein lysates for key DNA damage repair markers, such as γH2AX (a marker of DNA double-strand breaks). SOX9 overexpression should correlate with faster resolution of γH2AX foci post-damage.
- Co-Immunoprecipitation (Co-IP): Lyse cells and immunoprecipitate SOX9 using a specific antibody. Probe the immunoprecipitate for MMS22L to confirm direct interaction [87].
Protocol 2: Assessing SOX9 Inhibition in PARP Inhibitor Resistance
This protocol is based on recent findings in ovarian cancer [33].
1. Generating PARPi-Resistant Cells:
- Use parental ovarian cancer cell lines (e.g., SKOV3).
- Culture cells in progressively increasing concentrations of olaparib over several months to generate a resistant sublime (e.g., SKOV3/Ola).
2. Targeting the USP28-SOX9 Axis:
- Treat both parental and resistant cells with the USP28-specific inhibitor (AZ1), a PARPi (olaparib), or a combination.
- Perform dose-response curves to determine if AZ1 re-sensitizes resistant cells to olaparib.
3. Measuring DNA Damage and Repair:
- Immunofluorescence for DNA Damage Foci: Stain treated cells for γH2AX and RAD51. Count the number of foci per nucleus. SOX9 inhibition should result in increased and persistent γH2AX foci and reduced RAD51 foci formation after DNA damage, indicating impaired Homologous Recombination (HR) repair.
- Clonogenic Survival Assay: Plate cells at low density after drug treatment, allow them to form colonies for 1-2 weeks, then stain and count. This assay measures the long-term reproductive viability of cells after DNA damage, directly linking SOX9 function to survival.
4. Protein Stability Assay:
- Treat cells with the protein synthesis inhibitor cycloheximide (CHX) with or without the USP28 inhibitor AZ1.
- Collect protein lysates at various time points (e.g., 0, 1, 2, 4, 8 hours).
- Perform Western blotting for SOX9 to monitor its degradation rate. AZ1 should accelerate the decay of SOX9 protein.
Signaling Pathways and Mechanisms
SOX9 Regulation and Role in DNA Repair
The Dual Role of SOX9 Posing a Therapeutic Challenge
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating SOX9 in Therapy Resistance
| Reagent / Tool | Function / Application | Example Product / Identifier |
|---|---|---|
| Anti-SOX9 Antibody | Detection and quantification of SOX9 protein in tissues (IHC) and cell lysates (WB). | ABclonal, A19710 [87]; Sigma-Aldrich, AB5535 [33] |
| shSOX9 Lentiviral Particles | For stable knockdown of SOX9 gene expression in cell lines. | Sequence: CCGGCTCCACCTTCACCTACATGAACTCGAGTTCATGTAGGTGAAGGTGGAGTTTTTG [87] |
| USP28 Inhibitor (AZ1) | A specific small-molecule inhibitor used to destabilize SOX9 protein and overcome PARPi resistance. | Selleck Chemicals, S8904 [33] |
| PARP Inhibitor (Olaparib) | Induces DNA damage and selects for/researches resistance mechanisms in cancer models. | Selleck Chemicals, AZD2281 [33] |
| Anti-γH2AX Antibody | A key marker for identifying and quantifying DNA double-strand breaks via immunofluorescence or WB. | Abcam, ab81299 [33] |
| Anti-MMS22L Antibody | To study the interaction with SOX9 and its nuclear translocation in response to DNA damage. | Bioss, 17689R [87] |
The transcription factor SOX9 is a critical regulator of diverse biological processes, including cell fate determination, organ development, and tissue repair. However, its dysregulation contributes to various pathologies, particularly cancer and fibrotic diseases. This technical support document examines the context-dependent outcomes of SOX9 modulation through detailed case studies, highlighting both successful therapeutic inhibition and instances where such approaches compromise essential physiological functions. Understanding this balance is crucial for researchers developing targeted therapies, as SOX9 operates as a "double-edged sword" in biology—its inhibition can be therapeutically beneficial in some contexts while potentially disrupting vital tissue repair mechanisms in others [1].
Successful Case Studies of SOX9 Inhibition
Overcoming Chemoresistance in High-Grade Serous Ovarian Cancer
Experimental Context and Findings: In high-grade serous ovarian cancer (HGSOC), SOX9 has been identified as a key driver of chemoresistance. Research demonstrates that SOX9 expression is significantly upregulated following platinum-based chemotherapy in both cell lines and patient samples [9] [88]. Single-cell RNA sequencing of tumors from 11 HGSOC patients before and after neoadjuvant chemotherapy revealed consistent SOX9 upregulation in post-treatment cancer cells [9]. Functional experiments confirmed that epigenetic upregulation of SOX9 was sufficient to induce a stem-like transcriptional state and significant platinum resistance in vivo [9].
Key Experimental Protocols:
- SOX9 Knockout Using CRISPR/Cas9: SOX9 was knocked out in HGSOC cell lines using SOX9-targeting sgRNA and CRISPR/Cas9. The knockout significantly increased sensitivity to carboplatin treatment, as measured by colony formation assays [9].
- Induction of Chemoresistance: HGSOC cell lines were treated with carboplatin, resulting in acute SOX9 induction at both RNA and protein levels within 72 hours. SOX9 expression induced formation of a stem-like subpopulation capable of surviving chemotherapy [9].
- Transcriptional Divergence Analysis: A metric called transcriptional divergence was used to measure SOX9's association with transcriptional plasticity. This was defined as the sum of expression of the top 50% of detected genes divided by the sum of expression of the bottom 50% [9].
Mechanistic Insights: SOX9 drives chemoresistance by reprogramming the transcriptional state of naive ovarian cancer cells into a stem-like state. This population exhibits enhanced transcriptional plasticity, enabling survival under chemotherapeutic stress [9] [88]. SOX9 expression correlates with poor prognosis, with patients in the top quartile of SOX9 expression showing significantly shorter overall survival [9].
Reversing PARP Inhibitor Resistance in Ovarian Cancer
Experimental Context and Findings: Elevated SOX9 expression contributes to PARP inhibitor (PARPi) resistance in ovarian cancer. A 2025 study identified the deubiquitinating enzyme USP28 as a novel SOX9 interaction partner that stabilizes SOX9 protein levels by counteracting FBXW7-mediated ubiquitination and degradation [33].
Key Experimental Protocols:
- Co-immunoprecipitation (Co-IP): Ovarian cancer cells were lysed and SOX9 complexes were immunoprecipitated using specific antibodies. Interacting partners were identified through mass spectrometry, revealing USP28 as a novel SOX9 binding partner [33].
- Ubiquitination Assay: SOX9 ubiquitination status was assessed by treating cells with MG132 proteasome inhibitor, followed by immunoprecipitation and western blotting with ubiquitin antibodies to detect polyubiquitinated SOX9 [33].
- Chromatin Immunoprecipitation Sequencing (ChIP-Seq): SOX9 binding sites were genome-widely mapped, revealing direct binding to promoters of DNA damage repair genes including SMARCA4, UIMC1, and SLX4 [33].
Therapeutic Intervention: The USP28-specific inhibitor AZ1 successfully promoted SOX9 degradation and sensitized ovarian cancer cells to olaparib treatment both in vitro and in vivo, suggesting a promising combination strategy to overcome PARPi resistance [33].
Overcoming Temozolomide Resistance in Glioblastoma
Experimental Context and Findings: In glioblastoma (GBM), SOX9 is regulated by super-enhancers (SEs) and contributes to temozolomide (TMZ) resistance. SE inhibitors THZ2 (targeting CDK7) and JQ1 (targeting BRD4) demonstrated synergistic antitumor effects when combined with TMZ [89].
Key Experimental Protocols:
- Establishment of TMZ-Resistant Cell Lines: GBM cells were exposed to progressively increasing TMZ concentrations over 14-day intervals to develop resistant lines [89].
- Super-Enhancer Inhibition: TMZ-resistant GBM cells were treated with THZ2 or JQ1. THZ2 particularly reversed TMZ resistance by suppressing SE-driven SOX9 expression [89].
- CUT&RUN Assay: Protein-DNA interactions were examined to confirm SOX9, CDK7, and BRD4 binding to histone H3K27ac-marked enhancer regions [89].
Problematic SOX9 Inhibition: Compromised Tissue Repair and Regeneration
Disrupted Cartilage Repair and Osteoarthritis Progression
Experimental Context and Findings: In contrast to cancer contexts, SOX9 activation proves beneficial in cartilage maintenance and osteoarthritis (OA) treatment. CRISPR-dCas9-mediated SOX9 activation in mesenchymal stromal cells (MSCs) enhanced chondrogenic potential and attenuated OA progression in mouse models [14].
Key Experimental Protocols:
- CRISPR-dCas9 SOX9 Activation: Lentiviral vectors expressing dSpCas9-VP64 were used to activate SOX9 in bone marrow stromal cells. Five different sgRNAs were designed and screened for optimal SOX9 activation [14].
- Chondrogenic Differentiation: CD45− BMSCs were treated with chondrocyte differentiation medium, during which SOX9 upregulation was monitored as a key indicator of successful chondrogenesis [14].
- In Vivo OA Model: Surgically-induced OA mice received intraarticular injections of SOX9-activated MSCs. Cartilage degradation and pain measurements were tracked, showing significant improvement compared to controls [14].
Mechanistic Insights: SOX9-activated MSCs promoted expression of factors beneficial to cartilage integrity, inhibited catabolic enzymes in osteoarthritic joints, and suppressed immune cell activation. Modified cells survived in cartilaginous tissues, suggesting potential for long-term tissue maintenance [14].
Impaired Intrahepatic Bile Duct Morphogenesis
Experimental Context and Findings: Sox9 plays a critical role in intrahepatic bile duct (IHBD) development, particularly in the formation of peripheral ductules. Conditional knockout of Sox9 in hepatoblasts resulted in significantly fewer ductules and disrupted branching morphogenesis in adult livers [90].
Key Experimental Protocols:
- Conditional Knockout Mouse Model: Sox9-floxed mice were crossed with Albumin-Cre mice to generate Sox9 conditional knockouts with recombination beginning at E10.5 [90].
- Whole-Tissue 3D Imaging: iDISCO+ and light sheet microscopy enabled comprehensive visualization of IHBD architecture in control and Sox9cKO livers [90].
- Sholl Analysis: This quantitative method, typically used for neuronal branching, was adapted to quantify IHBD branching complexity by counting intersections at spherical intervals from the hilum [90].
Mechanistic Insights: Sox9 inhibits Activin A to promote biliary maturation and branching morphogenesis. Inhibition of Activin A in early postnatal development partially rescued IHBD morphogenesis in Sox9-deficient mice, indicating this pathway's central role [90].
Reduced Amyloid Plaque Clearance in Alzheimer's Disease
Experimental Context and Findings: SOX9 activation in astrocytes enhanced clearance of amyloid-β plaques in Alzheimer's disease mouse models. Sox9 overexpression triggered astrocytes to ingest more amyloid plaques, clearing them from the brain and preserving cognitive function [15].
Key Experimental Protocols:
- Sox9 Genetic Manipulation: Sox9 expression was either increased or removed in Alzheimer's mouse models that had already developed cognitive impairment and amyloid plaques [15].
- Cognitive Function Tracking: Mice were monitored for six months using object recognition and environmental familiarity tests to assess cognitive abilities [15].
- Plaque Quantification: Brain tissues were analyzed post-sacrifice to measure amyloid plaque accumulation [15].
Key Finding: Sox9 knockout accelerated plaque formation and reduced astrocyte complexity, while Sox9 overexpression promoted plaque clearance and maintained cognitive function, highlighting its protective role in neurodegenerative contexts [15].
Table 1: Comparative Outcomes of SOX9 Modulation Across Disease Contexts
| Disease Context | SOX9 Modulation | Primary Outcome | Key Metrics | Molecular Mechanism |
|---|---|---|---|---|
| Ovarian Cancer (HGSOC) | Inhibition | Improved chemosensitivity | ↓ IC50 to carboplatin; ↑ overall survival in low-SOX9 patients | Reprogramming of stem-like transcriptional state; reduced transcriptional divergence [9] |
| Ovarian Cancer (PARPi resistance) | Inhibition via USP28 targeting | Restored olaparib sensitivity | ↓ SOX9 protein stability; ↑ ubiquitin-mediated degradation | Disruption of SOX9-USP28 interaction; impaired DNA damage repair [33] |
| Glioblastoma | Inhibition via SE targeting | Reversed TMZ resistance | Synergistic effect with TMZ (Combination Index <1) | Suppression of SE-driven SOX9 expression; reduced H3K27ac binding [89] |
| Osteoarthritis | Activation | Attenuated cartilage degradation | Significant pain reduction; improved cartilage integrity | Enhanced chondrogenic potential of MSCs; suppressed inflammatory response [14] |
| Intrahepatic Bile Duct Development | Loss of Function | Disrupted branching morphogenesis | ↓ Distal branching (AUC 0.50-1.00); ↑ Sholl decay coefficient | Failed inhibition of Activin A; impaired ductule formation [90] |
| Alzheimer's Disease | Activation | Enhanced plaque clearance | Significant plaque reduction; preserved cognitive function | Increased astrocyte phagocytic activity; maintained cell complexity [15] |
Table 2: Experimental Models and Reagents for SOX9 Research
| Experimental Approach | Key Reagents/Tools | Function/Application | Considerations for Use |
|---|---|---|---|
| CRISPR/Cas9 Knockout | SOX9-targeting sgRNA, Cas9 protein | Complete SOX9 ablation; study of loss-of-function phenotypes | Potential compensatory effects; complete knockout may not reflect partial inhibition |
| CRISPR-dCas9 Modulation | dSpCas9-VP64 (activation), dSaCas9-KRAB (repression) | Precise transcriptional control without DNA cleavage | Enables fine-tuning of SOX9 expression to desired levels [14] |
| Super-Enhancer Inhibition | THZ2 (CDK7 inhibitor), JQ1 (BRD4 inhibitor) | Target SE-driven SOX9 expression | Synergistic effects with conventional chemotherapeutics [89] |
| Protein Stabilization Inhibition | AZ1 (USP28 inhibitor) | Promote SOX9 degradation via ubiquitin-proteasome pathway | Effective in combination with PARP inhibitors [33] |
| Conditional Knockout Mice | Sox9-floxed mice, Tissue-specific Cre lines | Tissue-specific Sox9 deletion; study of developmental roles | Timing of recombination critical for phenotype observation [90] |
| 3D Tissue Imaging | iDISCO+, Light sheet microscopy | Comprehensive morphological analysis of complex structures | Specialized equipment required; complex sample preparation [90] |
Signaling Pathways and Experimental Workflows
Diagram 1: Context-Dependent SOX9 Signaling in Disease. This diagram illustrates the opposing roles of SOX9 in cancer versus tissue repair contexts, highlighting why inhibition strategies require careful consideration of biological context.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for SOX9 Investigation
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| SOX9 Modulators | THZ2 (CDK7 inhibitor), JQ1 (BRD4 inhibitor) | Target super-enhancer driven SOX9 expression | Exhibit synergistic effects with conventional chemotherapeutics [89] |
| SOX9 Stabilization Inhibitors | AZ1 (USP28 inhibitor) | Promote SOX9 degradation via ubiquitin-proteasome pathway | Particularly effective in combination with PARP inhibitors [33] |
| CRISPR Tools | SOX9-targeting sgRNA, dSpCas9-VP64, dSaCas9-KRAB | Genetic knockout or transcriptional modulation | CRISPRa/i enables fine-tuning without complete knockout [14] |
| Animal Models | Sox9-floxed mice, Tissue-specific Cre lines (Albumin-Cre) | Tissue-specific Sox9 deletion studies | Timing of recombination critical for phenotype observation [90] |
| Analytical Tools | Sholl analysis, Transcriptional divergence metrics | Quantitative morphological and transcriptional analysis | Sholl analysis adapted from neuroscience to quantify branching complexity [90] |
| Imaging Reagents | iDISCO+, Light sheet microscopy | 3D tissue morphology visualization | Enables comprehensive analysis of complex structures like bile ducts [90] |
Frequently Asked Questions (FAQs): Troubleshooting SOX9 Research
Q1: Why does SOX9 inhibition show such context-dependent effects, being beneficial in cancer but problematic in tissue repair? SOX9 exhibits "janus-faced" functionality, acting as a "double-edged sword" in biology [1]. In cancer contexts, SOX9 promotes stem-like properties, transcriptional plasticity, and therapy resistance [9] [88]. In contrast, in tissue repair contexts, it drives essential differentiation and morphogenetic programs—chondrogenesis in cartilage, branching morphogenesis in bile ducts, and phagocytic activation in astrocytes [14] [90] [15]. The differential outcome depends on the cellular context, specific interacting partners, and downstream target genes.
Q2: What are the key considerations when designing SOX9-targeting experiments to avoid compromising tissue repair mechanisms?
- Tissue-Specificity: Utilize conditional knockout models or tissue-targeted delivery systems to limit off-target effects [90].
- Dosage Optimization: Consider partial rather than complete inhibition, as demonstrated by CRISPRa/i approaches that fine-tune expression levels [14].
- Temporal Control: Time interventions to avoid critical developmental or repair windows where SOX9 function is essential [90].
- Combination Therapies: Pair SOX9 inhibition with complementary approaches (e.g., USP28 inhibitors with PARPi) to allow lower doses of each agent [33].
Q3: What experimental metrics most reliably capture SOX9's functional impact in different disease models?
- Cancer Models: Transcriptional divergence measurements, stem cell marker expression, therapy resistance assays, and DNA damage repair capacity [9] [33].
- Tissue Repair Models: Morphological analyses (e.g., Sholl analysis for branching complexity), functional recovery assessments, and specific differentiation markers [14] [90] [15].
- Across Contexts: Comprehensive omics approaches (ChIP-Seq, scRNA-Seq) to identify SOX9 target genes and affected pathways in specific biological contexts [33] [9].
Q4: How can researchers navigate the challenge of SOX9's dual roles when developing therapeutic strategies?
- Context-Specific Biomarkers: Identify and monitor biomarkers that indicate whether SOX9 is functioning in pro-disease versus pro-repair pathways.
- Combinatorial Approaches: Develop strategies that inhibit SOX9 in diseased tissue while sparing or even activating it in repair contexts.
- Temporal Regulation: Design interventions that account for the temporal dynamics of SOX9 function in different biological processes.
- Advanced Delivery Systems: Utilize nanoparticle, viral, or other targeted delivery systems to achieve tissue-specific modulation.
Q5: What are the most promising emerging technologies for SOX9 research and therapeutic targeting?
- CRISPR-dCas9 Modulation: Enables precise transcriptional control without DNA cleavage, allowing fine-tuning of SOX9 expression levels [14].
- Super-Enhancer Targeting: Specific inhibitors (THZ2, JQ1) that disrupt the regulatory architecture driving pathological SOX9 expression [89].
- Protein Stabilization Manipulation: Targeting upstream regulators like USP28 that control SOX9 protein stability rather than directly inhibiting its expression [33].
- Advanced Imaging: iDISCO+ and light-sheet microscopy for comprehensive 3D morphological analysis of SOX9-dependent structures [90].
- Single-Cell Multi-omics: Combined transcriptomic and epigenomic analyses at single-cell resolution to dissect SOX9's cell-type-specific functions [9].
FAQ: Core Concepts and Dual Functionality of SOX9
What is the fundamental biological role of SOX9, and why is it considered a "double-edged sword" in therapeutic targeting? SOX9 is a transcription factor crucial for multiple developmental processes, including chondrogenesis (cartilage formation), sex determination, and embryogenesis [1] [91]. Its function is context-dependent, acting as a "double-edged sword" or a "janus-faced regulator" [1]. In cancer, SOX9 often acts as an oncogene, promoting tumor progression, chemoresistance, and immune escape [1] [65]. Conversely, in specific tissues like colon epithelium, it can function as a tumor suppressor, and in adult homeostasis, it is vital for tissue regeneration and repair, such as in cartilage and lung epithelium [1] [92] [57]. This duality means that inhibiting SOX9 for cancer therapy could inadvertently impair essential tissue repair mechanisms.
How do mutations in SOX9 cause Campomelic Dysplasia (CD), and what does this teach us about SOX9 inhibition? Campomelic Dysplasia (CD) is a severe skeletal malformation syndrome caused by heterozygous mutations in the SOX9 gene [91] [93]. While it was initially thought to result primarily from SOX9 haploinsufficiency (where one functional gene copy is insufficient), recent evidence identifies a novel molecular mechanism. Specific distal truncating mutations that leave the DNA-binding and dimerization domains intact can exert a dominant-negative effect [93]. This means the mutant SOX9 protein interferes with the function of the normal protein produced by the healthy allele, leading to a more severe impact on SOX9 function and a pronounced effect on bone development [93]. This demonstrates that the functional threshold for SOX9 is critical and that even partial disruption of its activity can have profound consequences.
FAQ: Experimental Models & Assessing SOX9 Function
What are the key in vivo models for studying SOX9's role in tissue repair and disease? Researchers use several robust mouse models to dissect SOX9 function in different contexts, each providing unique insights as summarized in the table below.
Table 1: Key In Vivo Models for SOX9 Research
| Model System | Key Genetic Features/Interventions | Primary Research Applications | Key Readouts & Phenotypes |
|---|---|---|---|
| Conditional Knockout (e.g., in colon) | Apc inactivation alone vs. combined Apc and Sox9 inactivation [92] |
Studying SOX9's tumor suppressor role in colorectal cancer (CRC) [92] | Increased tumor invasiveness, EMT, SOX2 upregulation, and metastasis [92] |
| Cell-Type Specific Knockout (e.g., in lung) | Sox9flox/flox;SftpcCre−ERT2 mice [57] |
Defining SOX9's role in alveolar type 2 epithelial (AEC2) stem cells during lung injury and repair [57] | Impaired epithelial regeneration, worsened lung injury score, dysregulated inflammatory response [57] |
| Lineage Tracing Model | Sox9-CreERT2 Ai9 mice [57] |
Fate mapping of Sox9-positive progenitor cells to track their contribution to tissue repair [57] | Proliferation and differentiation of labeled Sox9+ cells into alveolar epithelial cells post-injury [57] |
| CRISPR/dCas9 Engineered MSC | Simultaneous dCas9-SOX9 activation and dCas9-RelA inhibition in Mesenchymal Stromal Cells (MSCs) [56] | Cell-based therapy optimization for osteoarthritis; enhancing chondrogenic potential and immunomodulation [56] | Enhanced cartilage integrity, reduced joint catabolism, pain relief, and survival of transplanted cells in cartilage [56] |
What methodologies are critical for analyzing SOX9 expression and function in experimental samples? A combination of molecular and histological techniques is essential for a comprehensive analysis.
- Immunohistochemistry (IHC) & Semi-Quantitative Scoring: A standard method for assessing SOX9 protein levels and localization in tissue sections, often using a polyclonal rabbit anti-SOX9 antibody [65]. A robust scoring system multiplies the staining intensity (0=negative, 1=weak, 2=medium, 3=strong) by the proportion of positive cells (0-5 scale). A final score above 10 is typically classified as "high SOX9 expression," which correlates with poorer survival in cancers like intrahepatic cholangiocarcinoma [65].
- Gene Expression Analysis: RNA isolation followed by RT-qPCR is used to quantify SOX9 transcript levels. Key steps include using TRIzol reagent for RNA extraction, SYBR Green kits for cDNA amplification, and normalizing to a reference gene like
Actb[57]. - Functional Assays: In vitro knockdown via siRNA or shRNA is a primary method for establishing SOX9's functional role. For instance, silencing SOX9 in cholangiocarcinoma cells with siRNA (e.g., Dharmacon M-021507-00) increases gemcitabine-induced apoptosis and inhibits multidrug resistance genes [65]. Cell viability can be assessed using MTT assays [65].
The following diagram illustrates the core workflow for investigating SOX9 in a tissue repair context, from model establishment to key analytical pathways.
FAQ: Troubleshooting SOX9 Inhibition in Research
What are the potential side effects of systemic SOX9 inhibition, particularly on tissue repair mechanisms? Evidence from multiple models indicates that SOX9 inhibition can significantly impair the regenerative capacity of various tissues, posing a major challenge for its therapeutic application.
- Impaired Lung Regeneration: In chemical-induced acute lung injury, the specific deletion of Sox9 in AEC2 cells (
Sox9flox/flox;SftpcCre−ERT2model) results in a deficient repair response. These mice show reduced cell proliferation in damaged alveolar regions and dysregulated inflammatory responses, hindering epithelial regeneration [57]. - Compromised Intestinal Regeneration: SOX9 is required for the function of radioresistant reserve intestinal stem cells (rISCs). SOX9 knockout intestinal crypts lose their regeneration capacity after radiation injury and undergo apoptosis, indicating that SOX9 is vital for protecting and regenerating the intestinal epithelium [25].
- Loss of Tumor Suppressor Function: In colorectal cancer, SOX9 can exhibit tumor-suppressive activity. Its loss promotes epithelial-mesenchymal transition (EMT), induces the stem cell factor SOX2, and drives tumor invasion and metastasis [92].
How can researchers design experiments to mitigate the side effects of SOX9-targeted therapies? The key is to move away from systemic inhibition and toward targeted strategies.
- Tissue-Specific Delivery: For cancer therapy, investigate nanocarriers conjugated with ligands that target SOX9 inhibitors specifically to cancer stem cells (CSCs), minimizing exposure to normal repair-prone tissues [25].
- Context-Dependent Strategy: The approach must be tailored to the disease. In gastrointestinal cancer radiotherapy, the strategy would be to use SOX9 inhibitors concurrently with radiation to sensitize tumors, but then administer SOX9 inducers post-radiation to protect normal intestinal tissue and promote crypt regeneration [25].
- Combinatorial Gene Regulation: As demonstrated in osteoarthritis, using CRISPR-dCas9 to simultaneously fine-tune multiple pathways—such as activating SOX9 while inhibiting the inflammatory factor RelA in mesenchymal stromal cells—can enhance regenerative potential while suppressing damaging processes, offering a more sophisticated therapeutic profile than simple inhibition [56].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for SOX9-Focused Research
| Reagent / Material | Function / Application | Example Specifications / Notes |
|---|---|---|
| siRNA / shRNA | Knockdown of SOX9 expression to study loss-of-function in vitro and in vivo. | e.g., ON-TARGETplus Human SOX9 siRNA (Dharmacon, M-021507-00) [65] |
| Anti-SOX9 Antibody | Detection and localization of SOX9 protein via IHC, IF, and Western Blot. | e.g., Polyclonal rabbit anti-SOX9 (Sigma-Aldrich, HPA001758) at 1:100 dilution for IHC [65] |
| Conditional KO Mice | In vivo study of cell-type-specific SOX9 function in development, disease, and repair. | e.g., Sox9flox/flox mice crossed with cell-specific Cre drivers (e.g., SftpcCre-ERT2 for lung) [57] |
| Lineage Tracing Mice | Fate mapping of SOX9-expressing cells and their progeny over time. | e.g., Sox9-CreERT2 mice crossed with Ai9 (tdTomato) reporter mice [57] |
| CRISPR/dCas9 System | Precise transcriptional activation or inhibition of SOX9 without altering DNA sequence. | Used to simultaneously activate SOX9 and inhibit RelA in MSCs for enhanced therapy [56] |
| Tamoxifen | Inducer of Cre-ERT2 recombinase activity for temporal control of genetic manipulation in mice. | Administered via intraperitoneal injection (e.g., 100 mg/kg for 5 days) to activate Cre in inducible models [57] |
Conclusion
SOX9 inhibition represents a paradigm of precision oncology's fundamental challenge: effectively targeting pathological processes while preserving physiological repair. The evidence clearly demonstrates that while SOX9 suppression holds immense promise for overcoming therapy resistance in cancers, it unavoidably compromises critical regeneration mechanisms in intestine, skin, cartilage, and vasculature. Future success in this field requires developing sophisticated targeting approaches—whether temporal, spatial, or combinatorial—that maximize the therapeutic window. Critical research directions include developing inducible systems, tissue-specific delivery platforms, and combinatorial regimens with SOX9 inducers post-anticancer therapy. For drug development professionals, comprehensive preclinical assessment of tissue repair endpoints must become standard in the development pathway of SOX9 inhibitors to ensure these promising therapies do not exchange disease control for unacceptable tissue damage.
References
- 1. Frontiers | SOX9: a novel janus-faced regulator in immunity and its promise as a therapeutic target [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1700812/full]
- 2. The versatile functions of Sox9 in development, stem cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4326072/]
- 3. Frontiers | SOX9: a key transcriptional regulator in organ fibrosis [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1507282/full]
- 4. The pioneer factor SOX9 competes for epigenetic factors to ... [https://www.nature.com/articles/s41556-023-01184-y]
- 5. Transcription Factor Sox9 - an overview [https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/transcription-factor-sox9]
- 6. Sox9-expressing cells promote regeneration after radiation-induced lung injury via the PI3K/AKT pathway | Stem Cell Research & Therapy | Full Text [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-021-02465-9]
- 7. Knockdown of SOX9 alleviates tracheal fibrosis through the Wnt/β-catenin signaling pathway - PubMed [https://pubmed.ncbi.nlm.nih.gov/36192639/]
- 8. Aberrant cell state plasticity mediated by developmental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10058311/]
- 9. SOX9 drives a stem-like transcriptional state and platinum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483608/]
- 10. SOX9 in organogenesis: shared and unique transcriptional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9482574/]
- 11. SOX9: an important factor in regulating breast cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360010/]
- 12. Downregulation of SOX suppresses breast cancer cell 9 ... proliferation [https://pmc.ncbi.nlm.nih.gov/articles/PMC8114479/]
- 13. The effects of lncRNA MALAT1 on proliferation , invasion and... [https://molmed.biomedcentral.com/articles/10.1186/s10020-018-0050-5]
- 14. CRISPR-mediated Sox9 activation and RelA inhibition ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11405173/]
- 15. Scientists Find a Way to Help the Brain Clear Alzheimer's ... [https://scitechdaily.com/scientists-find-a-way-to-help-the-brain-clear-alzheimers-plaques-naturally/]
- 16. SOX9 Maintains Reserve Stem Cells and Preserves ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4709179/]
- 17. SOX9 maintains reserve stem cells and preserves ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/26170137/]
- 18. SOX9 inactivation affects the proliferation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8194236/]
- 19. SOX9 is an intestine crypt transcription factor, is regulated by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2172132/]
- 20. Sox9 Is Crucial for Mesenchymal Stem Cells to Enhance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8611311/]
- 21. Sox9 and Rbpj differentially regulate endothelial to ... [https://www.nature.com/articles/s41467-021-22717-9]
- 22. The role of NF-κB-SOX9 signalling pathway in osteoarthritis [https://www.sciencedirect.com/science/article/pii/S2405844024132227]
- 23. Histone hypo-acetylation of Sox9 mediates nicotine ... [https://pubmed.ncbi.nlm.nih.gov/29631619/]
- 24. SOX9 in cartilage development and disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6956855/]
- 25. Inhibition of SOX9 may be an effective target for increasing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5451632/]
- 26. Sox9 Accelerates Vascular Aging by Regulating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10826924/]
- 27. SOX9 mediates the phenotypic transformation of vascular ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1592594/full]
- 28. Distinct roles of SOX9 in self-renewal of progenitors and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11303482/]
- 29. Endothelial-Mesenchymal Transition in Regenerative Medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC4838799/]
- 30. SOX9 Stem-Cell Factor: Clinical and Functional Relevance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6463569/]
- 31. A SOX9 switch from regeneration to fibrosis [https://www.nature.com/articles/s41580-024-00720-4]
- 32. SOX9 is a novel cancer stem cell marker surrogated by ... [https://www.nature.com/articles/srep30489]
- 33. USP28 promotes PARP inhibitor resistance by enhancing ... [https://www.nature.com/articles/s41419-025-07647-4]
- 34. RNAi vs. CRISPR: Guide to Selecting the Best Gene ... [https://www.synthego.com/blog/rnai-vs-crispr-guide/]
- 35. Optimized Lipid Nanoparticle-Mediated mRNA Co-Delivery of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12554278/]
- 36. Experimental Methods for the Biological Evaluation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9959606/]
- 37. Nanocarrier‐Based Systems for Targeted Delivery [https://pmc.ncbi.nlm.nih.gov/articles/PMC12371215/]
- 38. Recent insights and applications of nanocarriers-based ... [https://www.sciencedirect.com/science/article/abs/pii/S1040842825000344]
- 39. Enhanced drug delivery with nanocarriers - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11380656/]
- 40. SOX9 is an atypical intestinal tumor suppressor controlling ... [https://www.oncotarget.com/article/10573/text/]
- 41. Peer review in Sox9 prevents retinal degeneration and is ... [https://elifesciences.org/articles/102337/peer-reviews]
- 42. What are SOX9 inhibitors and how do they work? [https://synapse.patsnap.com/article/what-are-sox9-inhibitors-and-how-do-they-work]
- 43. Cell Culture Troubleshooting [https://www.sigmaaldrich.com/US/en/applications/cell-culture-and-cell-culture-analysis/cell-culture-troubleshooting?srsltid=AfmBOorPdU89MgtRYqr_tZCugboYXpuU2KsZ2NO-pqFQIlCwqM9eCl1v]
- 44. In Vitro Research Reproducibility: Keeping Up High Standards [https://pmc.ncbi.nlm.nih.gov/articles/PMC6916005/]
- 45. Assessment of In Vivo Analgesic, Anti-Inflammatory and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623095/]
- 46. A zebrafish model of intestinal epithelial damage reveals ... [https://www.sciencedirect.com/science/article/pii/S193302192500042X]
- 47. Gut microbiome dysbiosis accelerates osteoarthritis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12232632/]
- 48. USP18 deubiquitinates and stabilizes SOX9 to promote the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12081856/]
- 49. Sox9 Is Crucial for Mesenchymal Stem Cells to Enhance ... [https://www.ijstemcell.com/journal/view.html?doi=10.15283/ijsc21078]
- 50. The local and circulating SOX9 as a potential biomarker for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7292907/]
- 51. Knockdown of SOX9 Inhibits the Proliferation, Invasion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7840816/]
- 52. SOX9 suppresses colon cancer via inhibiting epithelial- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12126244/]
- 53. A multifaceted strategy for intra- and extracellular nucleic ... [https://www.nature.com/articles/s41467-025-63194-8]
- 54. Chronological Changes in the Expression and Localization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10379325/]
- 55. Tankyrase inhibition preserves osteoarthritic cartilage by ... [https://www.nature.com/articles/s41467-019-12910-2]
- 56. CRISPR-mediated Sox9 activation and RelA inhibition ... [https://www.sciencedirect.com/science/article/pii/S1525001624003988]
- 57. Promoting epithelial regeneration in chemically induced acute ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-04124-1]
- 58. Sox9 Inhibits Wnt Signaling by Promoting β-Catenin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2631972/]
- 59. Inhibiting synovial inflammation and promoting cartilage ... [https://www.sciencedirect.com/science/article/pii/S2590006425003527]
- 60. Cancer stem cell surface markers on normal stem cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5498139/]
- 61. Cancer stem cell surface markers on normal stem cells [https://www.bmbreports.org/view.html?uid=1153&vmd=Full]
- 62. Biology of stem cell paradox: a double-edged sword ... [https://cancerci.biomedcentral.com/articles/10.1186/s12935-025-03981-x]
- 63. Enhanced disc regeneration through CRISPR/Cas9-mediated ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04600-2]
- 64. Histone hypo-acetylation of Sox9 mediates nicotine-induced ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-018-0853-x]
- 65. SOX9 expression decreases survival of patients with ... [https://www.nature.com/articles/s41416-018-0338-9]
- 66. Promoting epithelial regeneration in chemically induced ... [https://pubmed.ncbi.nlm.nih.gov/39849583/]
- 67. Sox9+ messenger cells orchestrate large-scale skeletal ... [https://elifesciences.org/articles/40715]
- 68. SOX9: a key transcriptional regulator in organ fibrosis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11835943/]
- 69. Setd4-expressing cells drive regenerative recovery in ... [https://www.sciencedirect.com/science/article/abs/pii/S0168827825025644]
- 70. Sox9 regulates alternative splicing and pancreatic beta cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10796970/]
- 71. Alternative Pathway Diagnostics - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC9851998/]
- 72. SOX9 keeps growth plates and articular cartilage healthy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7923381/]
- 73. Regulation and function of SOX9 during cartilage ... [https://www.sciencedirect.com/science/article/abs/pii/S1044579X20300961]
- 74. Chondrocyte fatty acid oxidation drives osteoarthritis via ... [https://www.nature.com/articles/s41467-025-60037-4]
- 75. A kinome-wide screen identifies a CDKL5-SOX9 regulatory ... [https://www.nature.com/articles/s41467-020-15638-6]
- 76. Evaluation of QSAR models for tissue-specific predictive ... [https://www.sciencedirect.com/science/article/abs/pii/S2468111324000318]
- 77. Drug toxicity prediction based on genotype-phenotype ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12597050/]
- 78. The basics of preclinical drug development for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2697630/]
- 79. Epigenetic Regulation of SOX9 by the NF-κB Signaling ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3775871/]
- 80. The Sox transcriptional factors: Functions during intestinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5326606/]
- 81. Expression and Functional Role of Sox9 in Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3548846/]
- 82. Upregulation of SOX9 inhibits the growth of human and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2662541/]
- 83. Inhibition of SOX9 may be an effective target for increasing ... [https://atm.amegroups.org/article/view/14162/html]
- 84. SOX9 inactivation affects the proliferation and differentiation of ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-021-02422-6]
- 85. Role of Sox9 in BPD and its effects on the Wnt/β-catenin ... [https://www.nature.com/articles/s41420-023-01795-2]
- 86. Sox9 Activation Highlights a Cellular Pathway of Renal ... [https://www.sciencedirect.com/science/article/pii/S2211124715007949]
- 87. The SOX9-MMS22L Axis Promotes Oxaliplatin Resistance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8191464/]
- 88. Targeting SOX9 May Help Overcome Ovarian Cancer ... [https://breakthroughsforphysicians.nm.org/obgyn-research-article-transcription-factor-ovarian-cancer]
- 89. Super-enhancer inhibitors THZ2 and JQ1 reverse ... [https://www.oaepublish.com/articles/cdr.2025.105]
- 90. Sox9 inhibits Activin A to promote biliary maturation and ... [https://www.nature.com/articles/s41467-025-56813-x]
- 91. Understanding the role of SOX9 in acquired diseases: lessons from development - PubMed [https://pubmed.ncbi.nlm.nih.gov/21237710/]
- 92. SOX9 suppresses colon cancer via inhibiting epithelial ... [https://pubmed.ncbi.nlm.nih.gov/40179020]
- 93. Dominant-negative SOX9 mutations in campomelic dysplasia - PubMed [https://pubmed.ncbi.nlm.nih.gov/31389106/]