Validation of Anterior Nasal Swabs for Influenza Detection: Performance, Protocols, and Future Directions
This comprehensive review examines the validation of anterior nasal swabs as an alternative to nasopharyngeal swabs for influenza detection.
Validation of Anterior Nasal Swabs for Influenza Detection: Performance, Protocols, and Future Directions
Abstract
This comprehensive review examines the validation of anterior nasal swabs as an alternative to nasopharyngeal swabs for influenza detection. Covering foundational principles, methodological approaches, performance optimization, and comparative validation, we analyze recent clinical studies demonstrating variable sensitivity (67-98%) across different collection techniques and populations. For researchers and drug development professionals, we detail technical specifications, sample processing protocols, and troubleshooting strategies to address suboptimal test characteristics. Evidence suggests anterior nasal sampling offers practical advantages for home testing and pediatric applications while maintaining robust performance for RSV detection, though influenza sensitivity requires further optimization through combined sampling approaches and technical refinements.
The Scientific Rationale for Anterior Nasal Sampling in Influenza Detection
For decades, the nasopharyngeal (NP) swab has been considered the gold standard for respiratory virus detection due to its high sensitivity, particularly for pathogens like influenza and SARS-CoV-2. This specimen type accesses the nasopharynx, where respiratory viruses replicate to high titers, theoretically providing optimal specimens for molecular detection [1]. However, this diagnostic standard presents significant limitations that hinder widespread testing implementation. NP swab collection is an invasive procedure that requires specialized training for healthcare personnel, creates patient discomfort that may reduce testing compliance, and consumes precious personal protective equipment (PPE) during collection [2] [3]. These limitations have prompted rigorous scientific evaluation of less invasive alternatives, particularly anterior nasal (AN) swabs, which can be self-collected by patients and are generally better tolerated. This review synthesizes current evidence comparing these sampling methods, focusing on analytical performance, practical implementation, and implications for influenza detection research and diagnostic development.
Comparative Performance: Nasopharyngeal versus Anterior Nasal Swabs
Detection Sensitivity Across Respiratory Viruses
Multiple studies have directly compared the sensitivity of NP and AN swabs for detecting various respiratory viruses. The evidence demonstrates that while NP swabs generally maintain slightly higher sensitivity, AN swabs provide clinically acceptable performance for most common pathogens, particularly when tested with highly sensitive molecular methods like RT-PCR.
Table 1: Comparative Sensitivity of AN Swabs Versus NP Swabs for Respiratory Virus Detection
| Virus | AN Swab Sensitivity | Testing Method | Population | Citation |
|---|---|---|---|---|
| Influenza | 89% (95% CI, 78%-99%) | rRT-PCR | Adults | [1] |
| SARS-CoV-2 | 82%-88% | RT-PCR (Composite Reference) | Ambulatory Patients | [4] |
| Multiple Respiratory Viruses* | 84.3% (overall) | Multiplex Molecular Testing | Pediatric | [5] |
| Seasonal Coronavirus | 36.4% | Multiplex Molecular Testing | Pediatric | [5] |
| Adenovirus, Influenza, Parainfluenza, RSV, SARS-CoV-2 | 100% (when collected within 24h of NP) | Multiplex Molecular Testing | Pediatric | [5] |
*Includes adenovirus, seasonal coronaviruses, human metapneumovirus, RSV, influenza, rhinovirus/enterovirus, SARS-CoV-2, and parainfluenza
The variation in sensitivity highlights several important patterns. First, performance differs significantly by virus type, with seasonal coronavirus showing notably poor detection in AN specimens [5]. Second, timing of specimen collection proves crucial, with sensitivity reaching 95.7% when AN swabs were collected within 24 hours of NP specimens in pediatric populations [6]. Third, the analytical sensitivity of the testing method influences comparative performance, with highly sensitive molecular methods like rRT-PCR demonstrating smaller differences between specimen types [1].
Impact of Viral Load on Detection Concordance
The concordance between NP and AN swabs is strongly influenced by viral load, as measured by cycle threshold (Ct) values in PCR assays. One systematic investigation found high concordance (Cohen's kappa >0.8) only for patients with viral loads above 1,000 copies/mL, while those with viral loads below this threshold exhibited low concordance (kappa = 0.49) [7]. This relationship explains why some studies report excellent agreement between methods while others find significant discrepancies. The majority of discordant results occur in patients with lower viral loads, where AN sampling may miss infections that NP swabs detect [7]. This has particular implications for testing later in the disease course or in asymptomatic individuals, who typically have lower viral loads.
Experimental Protocols for Method Comparison
Standardized Paired Sampling Methodology
Robust comparison of NP and AN swabs requires carefully controlled paired sampling protocols. The following methodology, adapted from multiple studies, provides a framework for valid comparison:
Participant Recruitment and Eligibility:
- Enroll patients presenting with symptoms of acute respiratory illness (<10 days duration) including fever, chills, or cough [1]
- Obtain informed consent and document symptom onset, vaccination status, and demographic information
- Exclude patients with thrombocytopenia (<50,000 platelets/μl) or nasal anatomy abnormalities [7]
Specimen Collection Sequence:
- AN Swab Collection: Insert a large-tipped, plastic-shafted Dacron swab approximately 1 centimeter into the nostril, rubbing along the nasal septum for 3-5 seconds while rotating [1]. Repeat in the other nostril with the same swab.
- NP Swab Collection: Using a wire-shafted Dacron swab, insert through the nostril approximately half the distance from the nares to the base of the ear (approximately 2 inches) until resistance is met [1]. Rotate the swab gently and withdraw.
Note: Always collect the less invasive AN specimen first to maximize recovery of material from both sites and minimize potential contamination from NP sampling [7].
Specimen Handling and Transport:
- Place swabs immediately into appropriate transport media (M4-RT viral transport media, Universal Transport Medium, or specific manufacturer-recommended media) [1] [8]
- Refrigerate specimens at 4°C for <24 hours until processing
- Aliquot and freeze at -70°C for long-term storage if not tested immediately [9]
Testing Methodology:
- Test all specimens using the same analytical platform and batch to minimize inter-assay variability
- Utilize highly sensitive molecular methods (rRT-PCR) with validated limits of detection [1]
- Include appropriate controls (human nucleic acid extraction control, amplification controls) [1]
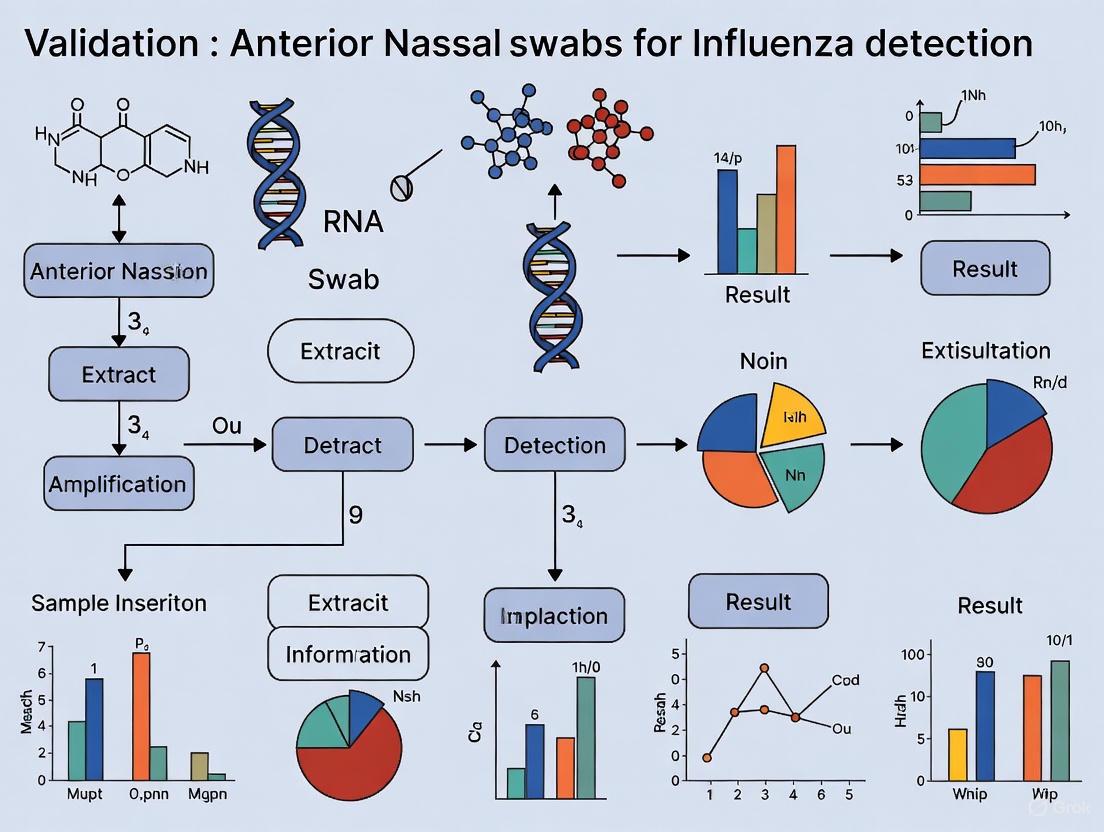
The following diagram illustrates the typical workflow for comparative studies of nasal sampling methods:
Special Considerations for Pediatric Populations
Sampling children requires specific adaptations to ensure both comfort and diagnostic accuracy:
- Allow for collection by caregivers with appropriate instruction and observation by healthcare personnel [9]
- Use visual aids or demonstrations to reduce anxiety
- Evaluate tolerability using standardized scales (1=pleasant to 5=unpleasant) completed by both children (when age-appropriate) and caregivers [9]
- Consider shorter swab insertion times while maintaining adequate sampling duration for quality specimens
Recent pediatric studies demonstrate that AN swabs achieve 95.7% sensitivity when collected within 24 hours of NP specimens, highlighting their utility in this population [6].
Complications and Safety Profile Comparison
Adverse Events Associated with NP Swabs
While generally safe when performed by trained personnel, NP swab collection carries a risk of complications ranging from minor discomfort to serious adverse events:
Table 2: Documented Complications of Nasopharyngeal Swabbing
| Complication Type | Frequency | Risk Factors | Management | Citation |
|---|---|---|---|---|
| Epistaxis | 0.0012%-0.026% | Coagulopathy, nasal anatomy | Nasal packing, cauterization | [2] |
| Retained Swab | Rare | Structural abnormalities, technique error | Endoscopic removal | [2] |
| CSF Leak | Very rare | Skull base defects, prior surgery | Surgical repair | [2] |
| Nasal Septal Abscess | Case reports | Pre-existing nasal conditions | Surgical drainage, antibiotics | [2] |
The overall complication rate requiring medical evaluation ranges from 0.0012% to 0.026% [2]. However, these statistics likely underestimate minor adverse events and discomfort that go unreported but impact patient experience and testing compliance.
Safety Advantages of AN Swabs
AN swabs offer a substantially improved safety profile due to their minimal intrusion and avoidance of sensitive nasal structures:
- No risk of cribriform plate injury or cerebrospinal fluid leakage due to shallow insertion depth [2]
- Minimal epistaxis risk as swabs do not contact the highly vascularized nasopharynx
- Eliminated risk of swab fracture in deep nasal structures as mechanical stress is reduced
- Suitable for self-collection with proper instruction, reducing healthcare worker exposure [3]
Proper AN swab technique involves inserting the swab only ½ to ¾ of an inch into the nose and performing at least four sweeping circles against the anterior nares wall with moderate pressure in each nostril [3].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for Comparative Swab Studies
| Reagent/Material | Specifications | Function | Example Products |
|---|---|---|---|
| NP Swabs | Wire-shafted, Dacron/rayon tip, length ~6 inches | Access nasopharyngeal region | Remel Aluminum/Plastic Unishaft Swab [1] |
| AN Swabs | Plastic-shafted, larger Dacron tip, standard length | Sample anterior nares region | Copan Nylon-Flocked Dry Swab [9] |
| Transport Media | Viral transport media (VTM), Universal Transport Media | Preserve viral integrity during transport | M4-RT Media, UTM (Copan) [1] [8] |
| Nucleic Acid Extraction Kits | Silica-membrane or magnetic bead technology | Isolate viral RNA/DNA | QIAamp 96 Virus QIAcube HT Kit [8] |
| PCR Master Mixes | One-step RT-PCR chemistry, compatible with platform | Amplify viral targets | Invitrogen SuperScript III Platinum One-Step [1] |
| Positive Controls | Inactivated virus or synthetic RNA transcripts | Verify assay performance | Quantified specific in vitro-transcribed RNA [8] |
Implications for Influenza Detection Research
The validation of AN swabs for respiratory virus detection has significant implications for influenza research and public health surveillance:
Expanding Testing Accessibility and Compliance
The less invasive nature of AN swabs enables testing scenarios not feasible with NP swabs:
- Self-collection programs allow broader community surveillance and earlier case detection
- Home-based testing facilitates rapid initiation of antiviral therapy when most effective
- Pediatric and geriatric populations experience reduced testing barriers, improving enrollment in clinical studies
- Resource-limited settings can implement testing without specialized healthcare personnel
Considerations for Research Design
When incorporating AN swabs into influenza research protocols, several factors require attention:
- Viral load dynamics throughout infection course may affect AN swab sensitivity differently than NP
- Specimen storage conditions and stability may differ between sample types
- Automated processing systems may require validation with AN specimen formats
- Self-collection instruction quality significantly impacts specimen adequacy [3]
Recent technological advances have further improved AN swab utility, with some antigen tests demonstrating equivalent diagnostic accuracy between AN and NP swabs, though sometimes with lower test line intensity that could affect interpretation by untrained users [8].
Evidence from multiple comparative studies supports AN swabs as a clinically acceptable alternative to traditional NP swabs for influenza detection and respiratory virus surveillance. While NP swabs maintain marginally higher sensitivity for some pathogens, particularly at low viral loads, the advantages of AN swabs—including reduced patient discomfort, elimination of specialized healthcare personnel for collection, minimal complication risk, and self-collection capability—position them as a transformative tool for scaling respiratory virus testing. Future research should focus on optimizing collection techniques, particularly for self-collection scenarios, and developing even less intrusive detection methods that maintain diagnostic accuracy across the spectrum of respiratory pathogens.
Pandemic-Driven Innovation in Respiratory Virus Testing Methodologies
The COVID-19 pandemic created unprecedented global demand for accessible, scalable, and comfortable respiratory virus testing, catalyzing a significant shift in diagnostic methodologies. This comparison guide examines the validation of anterior nasal swabs as a viable alternative to traditional nasopharyngeal sampling across multiple respiratory pathogens, with particular focus on influenza detection. We present comprehensive experimental data from recent clinical studies evaluating sensitivity, specificity, and practical implementation across diverse patient populations and testing platforms. The evidence demonstrates that anterior nasal swabs offer a favorable balance of patient comfort and diagnostic accuracy while enabling self-collection capabilities—advancements that have profound implications for future pandemic preparedness and respiratory virus surveillance.
Respiratory virus diagnostics historically relied on nasopharyngeal (NP) swabs as the gold standard specimen type due to their high viral load recovery [10] [4]. However, the pandemic exposed critical limitations of NP swabs: they require trained healthcare personnel, cause patient discomfort, and pose infection risks to collectors due to sneeze and cough induction [11]. These challenges triggered accelerated innovation toward less invasive methods, particularly anterior nasal swabs, which can be self-collected with minimal training [5].
The validation of anterior nasal swabs represents a paradigm shift in diagnostic approaches, balancing analytical sensitivity with practical implementation needs. This guide systematically compares the performance characteristics of anterior nasal swabs against established methodologies across multiple respiratory viruses, with detailed experimental protocols and performance metrics to inform researchers and clinical laboratory professionals.
Comparative Performance Data
Table 1: Diagnostic performance of anterior nasal swabs compared to nasopharyngeal swabs
| Virus | Testing Method | Anterior Nasal Sensitivity | NP Swab Sensitivity | Specificity | Study Population |
|---|---|---|---|---|---|
| Influenza | rRT-PCR | 89% (95% CI, 78%-99%) | 94% (95% CI, 87%-100%) | Not reported | 240 adults [1] |
| Influenza | Rapid Antigen | 67% (95% CI, 49%-81%) | Reference | 96% (95% CI, 89%-99%) | 128 emergency department patients [12] |
| RSV | Rapid Antigen | 75% (95% CI, 43%-95%) | Reference | 99% (95% CI, 93%-100%) | 128 emergency department patients [12] |
| SARS-CoV-2 | RT-PCR | 82%-88% (Composite) | 98% (Composite) | >97% | Meta-analysis of ambulatory patients [4] |
| Multiple Respiratory Viruses* | Multiplex PCR | 84.3% (Overall) | Reference | 100% (Multiple viruses) | 147 pediatric patients [5] |
*Includes adenovirus, seasonal coronaviruses, human metapneumovirus, RSV, influenza, rhinovirus/enterovirus, SARS-CoV-2, and parainfluenza
Impact of Timing and Viral Load
Table 2: Factors influencing anterior nasal swab sensitivity
| Factor | Impact on Sensitivity | Study Details |
|---|---|---|
| Time from NP collection | 95.7% when collected within 24h vs 84.3% overall | Pediatric study, 147 pairs [5] |
| Viral Load (Ct value) | Significantly higher sensitivity with lower Ct values (higher viral loads) | Mean Ct 25.5 vs 29.5 in detected vs missed samples [13] |
| Symptom Duration | Higher sensitivity in early symptomatic phase (1-5 days) | Median 2 days from symptom onset in optimal performance [11] |
| Virus Type | Variable by pathogen: 100% for adenovirus, influenza, parainfluenza, RSV, SARS-CoV-2; 36.4% for seasonal coronaviruses | Pediatric study within 24h of NP [5] |
Experimental Protocols and Methodologies
Standardized Anterior Nasal Collection Procedure
The following protocol represents a consensus methodology derived from multiple validation studies:
- Swab Selection: Use flocked swabs (e.g., FLOQSwabs) for optimal specimen collection and release [11]
- Insertion Depth: Insert swab approximately 1-2 cm into nostril (significantly shallower than NP insertion) [1] [11]
- Sampling Technique: Rotate swab gently along nasal septum for 3-5 seconds [1] [13]
- Dwell Time: Maintain swab position for 5 seconds to ensure adequate absorption [11]
- Processing: Place swab in appropriate transport media (e.g., Universal Transport Medium, M4-RT viral transport media) [1] [13]
Comparative Study Designs
Key validation studies employed rigorous methodological approaches:
Prospective Paired Design (Influenza Detection, 2012): 240 adult patients with acute respiratory illness provided paired nasal and NP swabs collected by trained personnel. Specimens were tested via both rRT-PCR and viral culture with a composite gold standard (any positive result from either specimen type). Statistical analysis included sensitivity calculations with 95% confidence intervals and chi-square comparisons [1].
Pediatric Validation (Multiple Viruses, 2025): 147 hospitalized children had anterior nasal swabs collected within 72 hours of NP specimens. Both specimen types were tested using multiplex molecular testing for 8 respiratory viruses. Concordance, sensitivity, and specificity were assessed with particular attention to timing between collections [5].
Self-Collection Validation (Influenza/RSV, 2025): Emergency department patients self-collected oral-nasal swabs (anterior nares, buccal mucosa, tongue) while healthcare providers collected NP swabs. Multiplex PCR testing compared performance characteristics, evaluating feasibility of self-collection [12].
Diagram Title: Validation Workflow for Anterior Nasal Swabs
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key reagents and materials for respiratory virus testing research
| Reagent/Material | Function | Examples & Specifications |
|---|---|---|
| Flocked Swabs | Optimal specimen collection and release | FLOQSwabs (Copan Italia S.p.A.); Puritan Sterile Foam Tipped Applicators [11] [13] |
| Transport Media | Viral preservation during transport | Universal Transport Medium (UTM, Copan); M4-RT viral transport media (Remel) [1] [11] |
| Nucleic Acid Extraction Kits | RNA purification for molecular testing | Maxwell HT Viral TNA Kit (Promega); magLEAD 6gC (Precision System Science) [10] [12] |
| PCR Master Mixes | Amplification of viral targets | Luna Universal Probe One-Step RT q-PCR kit (New England Biolabs); THUNDERBIRD Probe One-step qRT-PCR Kit (TOYOBO) [10] [12] |
| Automated Testing Platforms | High-throughput standardized testing | cobas 6800 (Roche); NeuMoDx (Qiagen); LightCycler Systems (Roche) [1] [10] |
| Reference Standards | Assay validation and quantification | EDX SARS-CoV-2 Standard (Bio-Rad); INSTAND e.V. quantitative reference samples [10] |
Discussion and Research Implications
Advantages and Limitations
The collective evidence demonstrates that anterior nasal swabs provide a favorable balance of patient comfort and diagnostic accuracy for most respiratory viruses. The significantly reduced discomfort and cough/sneeze induction [11] enable broader testing acceptance and self-collection capabilities. However, the moderately reduced sensitivity compared to NP swabs, particularly for influenza and seasonal coronaviruses, requires careful consideration in clinical and research applications [12] [5].
The strong dependence on viral load represents a critical factor in test performance. Studies consistently show superior detection when anterior nasal samples are collected early in symptomatic illness when viral loads are highest [11] [13]. This supports their application in community surveillance and early diagnosis scenarios but suggests limited utility in later disease stages or low-prevalence settings.
Future Research Directions
The pandemic-driven validation of anterior nasal swabs has established a new trajectory for respiratory virus diagnostics. Priority research areas include:
- Optimization of self-collection protocols for diverse populations including children, elderly, and immunocompromised patients
- Development of specialized transport media specifically formulated for anterior nasal specimens
- Standardization of sampling techniques across different swab types and collection devices
- Validation with emerging pathogen threats to establish preparedness for future pandemics
- Integration with point-of-care platforms to enable rapid diagnosis in non-clinical settings
The compelling evidence from multiple validation studies confirms that anterior nasal swabs represent a significant methodological advancement in respiratory virus testing. While nasopharyngeal swabs maintain slightly higher analytical sensitivity, the practical advantages of anterior nasal sampling—including patient comfort, reduced healthcare worker exposure, and self-collection capability—establish it as a viable alternative for most clinical and research applications.
The pandemic has accelerated the validation and adoption of this innovative methodology, creating new paradigms for respiratory virus surveillance that balance diagnostic accuracy with practical implementation. As research continues to refine collection techniques and expand applications, anterior nasal swabs are poised to become increasingly central to respiratory virus testing strategies in both routine clinical practice and pandemic preparedness.
Influenza viruses are significant human pathogens that cause seasonal epidemics and substantial respiratory morbidity. The replication sites of influenza viruses within the human host are fundamental to understanding disease pathogenesis and optimizing detection strategies. Both Influenza A (IAV) and Influenza B (IBV) viruses exhibit a strong tropism for the epithelial cells of the human respiratory tract. Following intranasal transmission, the viral replication cycle begins with the binding of viral hemagglutinin (HA) to sialic acid receptors on host respiratory epithelial cells, triggering receptor-mediated endocytosis [14] [15]. The viral ribonucleoproteins (vRNPs) are subsequently released into the cytoplasm and transported to the nucleus, where genome replication and transcription occur—an unusual characteristic for an RNA virus that provides access to the host's nuclear machinery [16] [15]. Newly synthesized viral components are then assembled into progeny virions that bud from the host cell membrane, a process facilitated by the neuraminidase (NA) protein, which cleaves sialic acids to enable viral release [14] [15]. This entire replication process occurs within the cells lining the upper respiratory tract, making this anatomical region the primary source for viral shedding and the optimal target for clinical specimen collection.
Comparative Performance of Anterior Nasal and Nasopharyngeal Swabs
The accurate detection of influenza virus relies on collecting specimens from the sites of active viral replication. While the nasopharyngeal (NP) swab has traditionally been considered the "gold standard" due to its higher sensitivity, less invasive anterior nasal swabs (NS) offer practical advantages for widespread testing and patient self-collection. The performance of these swab types has been systematically evaluated in multiple clinical studies, with key quantitative comparisons summarized in the table below.
Table 1: Comparative Performance of Nasal and Nasopharyngeal Swabs for Influenza Detection
| Study and Swab Type Comparison | Sensitivity (%) | Specificity (%) | Key Findings | Reference |
|---|---|---|---|---|
| Midturbinate (MTS) vs. Nasopharyngeal (NPS) (2024, n=93 paired samples) | 92% (MTS) vs. 95% (NPS) | N/A | MTS yielded a 53% lower viral load; NPS provided significantly higher viral load (p=0.0002). | [17] |
| Anterior Nasal (NS) vs. Nasopharyngeal (NP) (2012, n=240 adults) | 89% (NS) vs. 94% (NP) by rRT-PCR | N/A | No statistically significant difference in sensitivity by rRT-PCR (p=0.40). | [1] |
| Residual Nasal Swab (rNS) vs. NP/OP (2023, n=199 paired specimens) | 81.3% | 96.7% | Feasible to use a single anterior nasal swab for rapid testing followed by RT-PCR confirmation. | [18] |
| Anterior Nasal (NS) vs. Nasopharyngeal (NP) (2025, n=147 children, multiple viruses) | 84.3% (Overall) | N/A | Sensitivity increased to 95.7% when NS was collected within 24 hours of NP swab. Sensitivity for influenza was 100% within this timeframe. | [19] |
The data reveals that while NP swabs generally yield higher viral loads and sensitivities, anterior nasal swabs perform with good to excellent sensitivity, particularly when highly sensitive molecular tests like rRT-PCR are used [1] [19]. The timing of collection is critical, with anterior nasal swabs showing maximal sensitivity when collected close to symptom onset or to a reference NP swab [19]. Furthermore, one study demonstrated that it is feasible to use a single anterior nasal swab for both rapid antigen testing and subsequent molecular confirmation via RT-PCR, streamlining the testing process [18].
Experimental Protocols for Swab Comparison
To generate the comparative data presented above, researchers have employed rigorous experimental methodologies. The following workflow visualizes the standard protocol for a paired swab comparison study, as implemented in recent clinical research.
Diagram 1: Paired Swab Study Workflow
Detailed Methodology
The core components of the experimental protocols from key cited studies are detailed below:
Patient Population and Specimen Collection: Studies typically enroll patients of all ages presenting with acute respiratory illness symptoms (e.g., cough, fever) of short duration (e.g., <48 hours to <7 days) [17] [1]. Per study protocols, a mid-turbinate or anterior nasal swab is collected from one nostril, immediately followed by a nasopharyngeal swab from the other nostril using specialized swabs (e.g., Copan FLOQSwabs) [17] [1]. The order of collection is important; the less invasive swab is often collected first to minimize discomfort and potential cross-contamination [1].
Specimen Handling and Storage: Collected swabs are placed into tubes containing universal transport medium (e.g., Copan UTM, Remel M4RT) [17] [1]. Specimens are stored under refrigerated conditions (2-8°C) and shipped to a central laboratory within a strict timeframe (e.g., within 36 hours of collection) [17]. Upon receipt, samples are aliquoted and stored at -80°C until batch testing to preserve viral RNA integrity [17] [18].
Laboratory Testing and Viral Load Quantification: Viral RNA is purified from the samples using automated systems like the MagNA Pure 96 (Roche) [17]. Quantitative reverse transcription polymerase chain reaction (qRT-PCR) is performed using validated assays, such as the CDC Human Influenza Virus Real-time RT-PCR Diagnostic Panel, which targets conserved influenza genes (e.g., matrix protein M1 for influenza A, non-structural protein NS1 for influenza B) [17] [1]. The cycle threshold (Ct) values are recorded, and viral loads are calculated by comparison to a standard curve, often reported in log10 virus particles per milliliter (log10 vp/mL) [17]. Some studies also perform viral culture in Madin-Darby canine kidney (MDCK) cells as an additional detection method [1].
Data Analysis: The statistical analysis is exploratory and primarily descriptive. Wilcoxon signed-rank tests are used for paired comparisons of continuous variables (e.g., viral load), while McNemar's test is used for paired binary data (e.g., positive/negative results) [17]. Sensitivity and specificity are calculated using standard methods, sometimes employing a composite gold standard that considers any positive result from either specimen type by any test method [1].
The Scientist's Toolkit: Key Research Reagents
The following table catalogues essential materials and reagents used in the cited influenza detection and swab comparison studies, providing researchers with a practical resource for experimental design.
Table 2: Research Reagent Solutions for Influenza Detection Studies
| Reagent/Material | Specific Examples | Function in Experimental Protocol |
|---|---|---|
| Nasopharyngeal Swabs | Copan FLOQSwabs 501CS01 (minitip nylon flocked) [17]; Aluminum/plastic unishaft swab (Remel) [1] | Collects specimen from the nasopharynx. Mini-tip and flexible shaft designed for patient comfort and effective collection. |
| Midturbinate/Anterior Nasal Swabs | Copan FLOQSwabs 56380CS01 (adult midturbinate nylon flocked) [17]; Puritan Sterile Foam Tipped Applicator [18] | Collects specimen from the mid-turbinate region or anterior nares. Less invasive than NP swabs. |
| Viral Transport Medium (VTM) | Copan UTM [17]; Remel MicroTest M4RT [1] [18] | Preserves viral integrity during transport and storage from collection site to laboratory. |
| RNA Extraction System | MagNA Pure 96 System (Roche) [17] | Automated purification of viral RNA from clinical specimens for downstream molecular testing. |
| qRT-PCR Assays | Proprietary influenza matrix gene qRT-PCR [17]; CDC Human Influenza Virus Real-time RT-PCR Diagnostic Panel [1] [18] | Quantitatively detects and differentiates influenza A and B virus RNA with high sensitivity and specificity. |
| Cell Culture System | Madin-Darby Canine Kidney (MDCK) cells [1] | Supports the propagation of influenza virus for culture-based detection and research. |
The virological foundation of influenza replication is firmly rooted in the epithelial cells of the upper respiratory tract. This tropism directly informs and validates the use of upper respiratory specimens for disease diagnosis. Robust comparative studies demonstrate that while nasopharyngeal swabs yield higher viral loads and remain the most sensitive option, anterior nasal swabs offer a statistically comparable and clinically useful alternative for influenza detection, especially when paired with highly sensitive molecular methods like qRT-PCR. The adoption of anterior nasal swabs, supported by standardized collection and testing protocols, can significantly ease large-scale influenza surveillance, enhance patient comfort, and facilitate broader testing strategies in both clinical and community settings.
The accurate detection of respiratory viruses is a cornerstone of public health and clinical management. For decades, the nasopharyngeal (NP) swab has been considered the gold standard for sample collection due to its high diagnostic yield. However, its collection is invasive, requires trained healthcare professionals, and can be uncomfortable for patients. In recent years, the anterior nasal (AN) swab has emerged as a less invasive, more patient-friendly alternative that is also suitable for self-collection. This guide provides an objective comparison of viral shedding patterns between these two anatomical sites, synthesizing current research to evaluate the performance of AN swabs within the broader context of validating their use for influenza and SARS-CoV-2 detection.
Quantitative Comparison of Diagnostic Performance
Extensive clinical studies have directly compared the sensitivity and specificity of NP and AN swabs for detecting respiratory viruses. The table below summarizes key findings from recent research.
Table 1: Diagnostic Performance of Anterior Nasal vs. Nasopharyngeal Swabs
| Virus Target | Test Type | Sensitivity (AN vs. NP) | Specificity (AN vs. NP) | Key Findings & Context |
|---|---|---|---|---|
| SARS-CoV-2 [8] | Antigen (Ag-RDT - Sure-Status) | AN: 85.6%NP: 83.9% | AN: 99.2%NP: 98.8% | Diagnostic accuracy was equivalent. High agreement (κ=0.918). |
| SARS-CoV-2 [8] | Antigen (Ag-RDT - Biocredit) | AN: 79.5%NP: 81.2% | AN: 100%NP: 99.0% | Diagnostic accuracy was equivalent. High agreement (κ=0.833). |
| Influenza [20] | PCR (vs. HCW NP & Nasal) | AN: 78%(vs. HCW NP) | AN: 100%(vs. HCW NP) | Self-collected AN swabs in older adults. |
| Influenza A & B [13] | PCR | rNS*: 81.3% | rNS*: 96.7% | Single AN swab used for rapid test and PCR. |
| RSV [21] | PCR (Multiplex) | AN: 75% | AN: 99% | Self-collected oral-nasal swab in an emergency department. |
| Multiple (Pediatric) [9] | PCR (Multiplex Panel) | High agreement with NP for SARS-CoV-2, RSV, Influenza | High agreement with NP for SARS-CoV-2, RSV, Influenza | AN and saliva samples were better tolerated than NP in children. |
Table 1 Note: rNS = residual nasal swab (an anterior nasal swab used for a rapid test before being stored for PCR).
A critical finding across multiple studies is the strong correlation of viral load between the two sites. Research on SARS-CoV-2 outpatients found that AN and NP RNA levels were highly correlated (r=0.84), indicating that both compartments reflect similar shedding dynamics [22]. The limits of detection for SARS-CoV-2 antigen tests were also not significantly different between the two swab types [8].
Insights from Viral Shedding Kinetics
Understanding viral shedding—the release of viral particles from an infected host—is key to interpreting diagnostic results.
- Shedding Concordance: Viral shedding in the nasopharynx and anterior nares is highly concordant. Higher RNA levels in these upper respiratory tract compartments are associated with greater detection of virus in other compartments, such as oral wash/saliva and plasma [22].
- Predictors of Shedding: Certain host factors influence viral load. Older age has been consistently associated with higher nasopharyngeal RNA levels at diagnosis. Some studies also indicate that men may have slower viral clearance from the nasopharynx than women, which could contribute to sex-based differences in disease outcomes [22].
- Shedding and Infectiousness: It is crucial to distinguish between the detection of viral RNA (via PCR) and the presence of replication-competent infectious virus. While PCR is highly sensitive, it can detect viral fragments long after the infectious period has ended. The presence of infectious virus is best determined by virus isolation in cell culture, a complex method not suited for clinical diagnostics [23]. Antigen-detecting rapid tests (Ag-RDTs) often serve as a more practical proxy for infectiousness, as they typically become positive only during periods of high viral load [23].
Detailed Experimental Protocols from Key Studies
To facilitate the replication and critical appraisal of these findings, here are the methodologies from two pivotal studies cited in this guide.
Table 2: Summary of Key Experimental Protocols
| Study Component | Sure-Status/Biocredit Ag-RDT Evaluation [8] | Concordance of SARS-CoV-2 RNA Levels [22] |
|---|---|---|
| Study Population | Symptomatic adults at a drive-through test center (Sure-Status: n=372; Biocredit: n=232). | Outpatients with mild-to-moderate COVID-19 in the ACTIV-2/A5401 trial (n=537 for baseline). |
| Sample Collection | Healthcare worker-collected:1. NP swab (for reference RT-qPCR).2. NP swab (for Ag-RDT) from other nostril.3. AN swab (for Ag-RDT) from both nostrils. | Longitudinal collection:- Dry NP swab (healthcare worker-collected).- Dry AN swab (self-collected).- Oral wash/saliva and plasma. |
| Reference Standard | RT-qPCR (TaqPath COVID-19) on NP swab. | Quantitative SARS-CoV-2 RNA testing on all sample types. |
| Index Test | Two Ag-RDT brands (Sure-Status & Biocredit) run on paired AN and NP swabs. | Not applicable (observational comparison). |
| Analysis | Sensitivity, specificity, Cohen's kappa (κ), limit of detection (LoD). | Spearman's correlation, linear regression models for censored data. |
The Scientist's Toolkit: Essential Research Reagents
The following table details key materials and reagents commonly used in this field of research.
Table 3: Key Research Reagents and Materials
| Item | Function & Application |
|---|---|
| Flocked Swabs (e.g., Copan FLOQSwabs) | Sample collection from NP and AN sites. Designed to release collected material efficiently into transport media [13]. |
| Universal Transport Media (UTM) | Preserves viral integrity during transport and storage for subsequent PCR or culture [8]. |
| Viral RNA Extraction Kits | Isolate viral RNA from clinical specimens prior to RT-PCR (e.g., QIAamp 96 Virus QIAcube HT kit) [8]. |
| RT-qPCR Assays | Quantitative detection of viral RNA (e.g., TaqPath COVID-19, CDC Human Influenza Virus RT-PCR Panel) [8]. |
| Cell Lines for Virus Isolation | Determine the presence of infectious virus (e.g., Vero E6, Caco-2, Calu-3 cells) [23]. |
| Ag-RDT Kits | Rapid, lateral flow immunochromatographic tests for detecting viral antigens at point-of-care [8]. |
Research Workflow and Logical Relationships
The diagram below outlines the typical workflow for a head-to-head comparative study of nasopharyngeal and anterior nasal swabs.
The collective evidence demonstrates that anterior nasal swabs are a valid and reliable alternative to nasopharyngeal swabs for detecting influenza, SARS-CoV-2, and other respiratory viruses. While some studies report a modest reduction in sensitivity for AN swabs, particularly for influenza, the overall diagnostic accuracy is largely equivalent, especially when viral loads are high [8] [21] [13]. The high correlation of viral RNA levels between the two sites further supports the use of AN swabs for monitoring viral shedding dynamics [22].
The advantages of AN swabs—enhanced patient comfort, feasibility for self-collection, and reduced need for professional training—present a compelling case for their adoption in both clinical and community settings [20] [9]. Future research should continue to optimize self-collection protocols and explore the impact of emerging viral variants on test performance across different anatomical sites.
Regulatory Landscape Evolution for Alternative Sampling Methods
The regulatory landscape for respiratory virus diagnostics is undergoing a significant transformation, driven by technological advances and a growing need for accessible testing options. Traditional nasopharyngeal swabs (NPS) have long been the gold standard for specimen collection due to their high viral yield, but their invasive nature and requirement for healthcare professional administration present limitations for widespread use [24] [25]. The emergence of global respiratory pandemics has accelerated regulatory acceptance of less invasive alternative sampling methods, particularly anterior nasal swabs (ANS), which offer the advantage of potential self-collection and reduced patient discomfort [26] [27].
This evolution is particularly relevant for influenza detection, where timely diagnosis is critical for implementing effective treatment and containment strategies. The regulatory pathway for these alternatives requires robust clinical validation to establish diagnostic performance comparable to established methods. This guide objectively compares the performance of anterior nasal swabs against other sampling methods within the context of influenza detection research, providing researchers and developers with the experimental data and regulatory framework necessary to advance this field [28].
Performance Comparison of Respiratory Specimen Types
Extensive research has compared the diagnostic accuracy of various upper respiratory specimen types for detecting viral pathogens. The following tables summarize key performance metrics from recent studies.
Table 1: Comparative Sensitivity of Alternative Specimens vs. Nasopharyngeal Swabs
| Specimen Type | Target Pathogen | Sensitivity (%, vs. NPS) | Specificity (%, vs. NPS) | Key Study Findings |
|---|---|---|---|---|
| Anterior Nasal Swab (ANS) | SARS-CoV-2 | 80.7% | 99.6% | Lower viral load (higher Ct) but suitable for outpatient setting [26]. |
| ANS (10 rubs) | SARS-CoV-2 | Comparable to NPS | N/A | Significantly better than 5-rub ANS (Ct 24.3 vs. 28.9); achieved similar concentration to NPS [24]. |
| Oral-Nasal Swab | Influenza | 67.0% | 96.0% | Suboptimal for Influenza; not an acceptable substitute for NPS [12]. |
| Oral-Nasal Swab | RSV | 75.0% | 99.0% | Performance characteristics preserved better for RSV than for Influenza [12]. |
| Nasal Swab (RAT) | SARS-CoV-2 | 81.0% | 100.0% | Achieved WHO sensitivity requirement (0.80); higher than NPS (0.75) in this context [29]. |
Table 2: Analysis of Specimen Collection Characteristics and Applications
| Characteristic | Nasopharyngeal (NPS) | Anterior Nares (ANS) | Oral-Nasal | Saliva |
|---|---|---|---|---|
| Relative Sensitivity | High (Reference) | Moderate to High | Moderate (Varies by pathogen) | Moderate |
| Patient Comfort | Low (Invasive) | High (Minimally invasive) | High | High |
| Collection Skill Required | High (Healthcare professional) | Low (Suitable for self-collection) | Low (Suitable for self-collection) | Low (Suitable for self-collection) |
| Key Advantages | Highest viral concentration; established standard | Patient-friendly; suitable for home testing | Combines oral and nasal surfaces; simple collection | Non-invasive |
| Primary Limitations | Discomfort, requires trained staff, PPE | Potentially lower viral load | Suboptimal for some pathogens (e.g., Influenza) | Variable viscosity, potential interference |
Detailed Experimental Protocols for Method Validation
To ensure the validity and reliability of data supporting regulatory submissions, researchers must employ rigorous experimental designs. The following protocols outline key methodologies used in recent studies evaluating alternative sampling methods.
Protocol for Paired-Sample Diagnostic Accuracy Study
This protocol, based on a study comparing ANS versus combined oro-/nasopharyngeal (OP/NP) sampling, highlights the direct comparison of a new method against a reference standard [26].
- Study Population and Setting: Recruit adult patients presenting to an emergency department or ambulatory clinic with symptoms suggestive of a respiratory viral infection (e.g., influenza). A sufficient sample size should be calculated for power and confidence intervals.
- Sample Collection: For each participant, collect the alternative specimen (e.g., ANS) first to avoid contamination of the nasal area by the NP procedure. Immediately afterward, a trained healthcare professional collects the reference standard NP swab.
- ANS Collection: Insert a flocked ANS (e.g., Rhinoswab) into both nostrils until resistance is met. Leave in place for 60 seconds, optionally with side-to-side movements for 15 seconds [26].
- NP Collection: Insert a flexible mini-tip flocked swab through the nostril to the nasopharynx. Rotate the swab several times against the posterior nasopharyngeal wall and hold for a few seconds to absorb secretions [24] [25].
- Sample Processing: Place both swabs in identical, approved viral transport media. Store samples at -20°C within 24 hours if not processed immediately.
- Laboratory Analysis: Test all samples using a highly sensitive reverse transcription polymerase chain reaction (RT-PCR) assay for the target pathogen(s) (e.g., influenza A/B). Include an internal control (e.g., human RNase P) to monitor sample quality and cellular content [24].
- Data Analysis: Calculate the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of the ANS using the NP swab result as the reference standard. Compare cycle threshold (Ct) values between paired positive samples using non-parametric tests like the Mann-Whitney U test [26] [12].
Protocol for Self-Collection Feasibility and Usability Study
This protocol is critical for tests intended for home use, a key area of regulatory evolution [28] [12].
- Participant Recruitment: Enroll a diverse cohort of participants representative of the intended-use population, varying in age, education, and technical proficiency.
- Training and Sample Collection: Provide participants with the swab kit and standardized, written instructions for self-collection. No direct demonstration should be given. Participants then self-collect an ANS or oral-nasal sample. A healthcare professional subsequently collects an NP swab from the same participant.
- Usability Assessment: Participants complete a questionnaire rating the ease of use, clarity of instructions, and comfort level associated with the self-collection process.
- Analysis: Determine the percent agreement between the results of the self-collected sample and the professionally collected NP sample. Analyze usability feedback to identify potential points of user error or confusion that must be addressed before regulatory approval [28].
Visualization of Regulatory Pathways and Experimental Workflows
The regulatory journey and experimental validation of new sampling methods can be visualized through the following diagrams.
Regulatory Pathway for Novel Sampling Devices
Figure 1: The U.S. FDA pathway for a novel anterior nasal swab. The first device typically requires a De Novo request. Once classified as Class II, it becomes a predicate for subsequent 510(k) submissions [28].
Paired-Sample Validation Workflow
Figure 2: Core workflow for validating an anterior nasal swab against the nasopharyngeal swab reference standard. Key steps include paired sampling and comparative RT-PCR analysis [24] [26] [12].
The Scientist's Toolkit: Key Research Reagent Solutions
Successful validation of alternative sampling methods relies on a standardized set of high-quality reagents and materials. The following table details essential components for conducting these studies.
Table 3: Essential Research Reagents and Materials for Sampling Method Validation
| Reagent/Material | Function/Application | Examples & Considerations |
|---|---|---|
| Flocked Swabs | Sample collection; nylon fibers maximize cellular absorption and elution [30]. | Copan FLOQSwabs, Rhinoswab; tip material (nylon, polyester) is critical for sample release efficiency [24] [26]. |
| Viral Transport Media (VTM) | Preserve viral nucleic acid integrity during transport and storage. | Copan Universal Transport Media, Mantacc VTM; must contain additives to inhibit bacterial/fungal growth [26] [12]. |
| Nucleic Acid Extraction Kits | Isolate high-purity viral RNA for downstream molecular analysis. | QIAamp Viral RNA Mini Kit (Qiagen), Maxwell HT Viral TNA Kit (Promega); automation compatibility (e.g., QIAcube, Hamilton Star) is key for high-throughput processing [24] [12]. |
| RT-PCR Master Mix | Amplify and detect target viral RNA sequences. | Luna Universal Probe One-Step RT-qPCR Kit (NEB), Fast Viral Master mix (Life Technologies); sensitivity and robustness are paramount [26] [12]. |
| Respiratory Panel Assays | Multiplex detection of common respiratory pathogens from a single sample. | Allplex RP1/2/3 & SARS-CoV-2 (Seegene), Lab-developed multiplex PCR; essential for comprehensive pathogen detection and co-infection studies [24] [12]. |
| Internal Control Targets | Monitor sample adequacy, nucleic acid extraction, and PCR inhibition. | Human RNase P gene; confirms sufficient human cellular material in ANS specimens [24]. |
The regulatory landscape for alternative sampling methods is maturing, with anterior nasal swabs emerging as a validated and patient-centric option for influenza and other respiratory virus detection. While nasopharyngeal swabs remain the sensitivity benchmark, robust evidence demonstrates that ANS provide a strong balance of diagnostic accuracy, patient comfort, and practicality for both clinical and potential home settings [29] [27].
Future developments will focus on standardizing self-collection protocols, optimizing swab design and materials for maximum viral recovery, and further integrating these methods with rapid point-of-care and at-home diagnostic platforms. For researchers and drug development professionals, successfully navigating this evolving landscape requires a firm grasp of regulatory pathways, a commitment to rigorous experimental validation, and the strategic use of standardized, high-quality research tools. The continued validation and regulatory acceptance of these methods will be crucial for enhancing pandemic preparedness and expanding access to critical diagnostic testing.
Technical Protocols and Implementation Strategies for Anterior Nasal Collection
Standardized Anterior Nasal Swab Collection Techniques and Materials
Anterior nasal (AN) swabs have emerged as a critical tool for respiratory virus detection, balancing diagnostic accuracy with significant practical advantages. This guide provides a comparative analysis of AN swab performance against traditional nasopharyngeal (NP) swabs, focusing on technical specifications, validated collection protocols, and experimental data directly applicable to influenza detection research. Evidence confirms that while AN swabs may exhibit a modest reduction in sensitivity for some pathogens, their excellent patient tolerance and suitability for self-collection make them a transformative methodology for large-scale public health testing and surveillance studies. Standardization of collection techniques and materials is paramount to ensuring data quality and reproducibility in influenza research.
Performance Comparison: Anterior Nasal vs. Nasopharyngeal Swabs
Extensive clinical evaluations provide a quantitative foundation for selecting appropriate swab types in research protocols. The following tables summarize key performance metrics for SARS-CoV-2 detection, which serve as a relevant proxy for understanding performance in influenza virus detection due to similar transmission routes and specimen requirements.
Table 1: Diagnostic Sensitivity and Specificity of AN vs. NP Swabs
| Evaluation Focus | Swipe Type | Sensitivity (95% CI) | Specificity (95% CI) | Agreement (κ statistic) | Citation |
|---|---|---|---|---|---|
| SARS-CoV-2 Ag-RDT (Sure-Status) | NP Swab | 83.9% (76.0–90.0) | 98.8% (96.6–9.8) | 0.918 | [8] |
| AN Swab | 85.6% (77.1–91.4) | 99.2% (97.1–99.9) | [8] | ||
| SARS-CoV-2 Ag-RDT (Biocredit) | NP Swab | 81.2% (73.1–87.7) | 99.0% (94.7–86.5) | 0.833 | [8] |
| AN Swab | 79.5% (71.3–86.3) | 100% (96.5–100) | [8] | ||
| SARS-CoV-2 PCR | NP Swab | 92.5% (85–99) | N/A | N/A | [31] |
| AN Swab | 82.4% (72–93) | N/A | N/A | [31] | |
| SARS-CoV-2 PCR | Saliva | 93.8% (86.0–97.9) | 97.8% (95.3–99.2) | 0.912 | [32] |
| AN Swab | 86.3% (76.7–92.9) | 99.6% (98.0–100.0) | 0.889 | [32] |
Table 2: Analytical and Practical Characteristics Comparison
| Characteristic | Anterior Nares (AN) Swab | Nasopharyngeal (NP) Swab | Research Implications |
|---|---|---|---|
| Collection Depth | 0.5 - 2 cm into nostril [11] [33] | ~8-11 cm to nasopharynx [31] | AN swabs enable self-collection, ideal for decentralized trials. |
| Patient Discomfort | Significantly lower pain and sneeze/cough induction [11] | Significantly higher; requires clinician collection [11] [33] | Reduces participant burden, improves compliance in longitudinal studies. |
| Viral Load Recovery | Lower median load vs. NP (e.g., 1,792 vs. 53,560 RNA copies/mL) [11] | Highest reported viral load [11] [25] | Impacts Limit of Detection (LoD) for low viral titer infections. |
| Limit of Detection (LoD) | Comparable to NP for Ag-RDTs [8] | Slightly lower for some PCR assays [25] | AN swabs highly reliable for detecting infectious, high viral load stages. |
| Specimen Type Flexibility | Suitable for Ag-RDTs and most NAATs [8] [25] | Considered gold standard for NAATs [25] [31] | AN swabs are versatile for both rapid and lab-based testing. |
Detailed Experimental Protocols for Validation
To ensure the validity and reliability of data obtained using AN swabs, researchers should adhere to rigorously validated collection and processing protocols. The following methodologies are drawn from cited clinical studies.
Protocol: Healthcare Worker-Collected AN Swab for Antigen Testing
This protocol is adapted from a prospective diagnostic evaluation that demonstrated equivalent accuracy between AN and NP swabs for SARS-CoV-2 antigen detection [8].
- Step 1: Material Preparation. Use a flocked or foam swab with a polystyrene handle. The swab should be sterile and individually wrapped. Test kits (e.g., Sure-Status, Biocredit) and a timer must be ready.
- Step 2: Sample Collection.
- Insert the swab into one nostril, advancing it approximately 2 cm along the nasal septum and inferior concha, touching the nasal membrane [11].
- Firmly rotate the swab 5 times against the nasal wall [11].
- Hold the swab in place for 5 seconds to ensure adequate specimen absorption [11].
- Without removing the swab, repeat the rotation in the same nostril.
- Use the same swab to repeat the entire procedure in the second nostril [33].
- Step 3: Sample Processing.
- Immediately insert the swab into the extraction buffer vial provided with the test kit.
- Rotate the swab vigorously at least 5 times while pressing the head against the bottom and side of the vial.
- Remove the swab while squeezing the vial wall to extract as much liquid as possible.
- Close the vial with the cap with the integrated dropper.
- Step 4: Test Execution and Interpretation.
- Add the number of drops specified in the manufacturer's Instructions for Use (IFU) to the sample well of the test cassette.
- Start the timer and read the result at the exact time specified in the IFU (e.g., 15-30 minutes).
- Critical Note: Studies indicate test line intensity can be lower with AN swabs. Results should be interpreted by trained personnel, as faint lines can be misclassified by lay users [8].
Protocol: Self-Collection of AN Swab for Nucleic Acid Amplification Testing (NAAT)
This protocol is validated for PCR testing and is crucial for enabling large-scale, decentralized research studies [32] [25].
- Step 1: Participant Instruction. Provide subjects with clear, illustrated instructions. Key points include:
- Insert the swab 1/2 to 3/4 of an inch (approx. 1-2 cm) into the nose [33].
- Rotate the swab against the inner nasal wall in a circular motion 3-5 times.
- Use the same swab to repeat the process in the other nostril.
- Step 2: Sample Collection. The participant follows the provided instructions to self-swab both nostrils with the same swab.
- Step 3: Sample Storage and Transport.
- Place the swab immediately into a tube containing Universal Transport Medium (UTM) or another appropriate transport medium [8] [11].
- Break or cut the swab shaft to secure the lid.
- Store and transport samples refrigerated (4°C) and process them as soon as possible, ideally within 72 hours, to maintain RNA stability [25].
The workflow for a head-to-head validation study, incorporating these protocols, is illustrated below.
Research Validation Workflow for AN Swabs
The Scientist's Toolkit: Key Research Reagent Solutions
Successful implementation of AN swab protocols relies on specific materials and reagents. The following table details essential components for a robust research pipeline.
Table 3: Essential Research Reagents and Materials for AN Swab Studies
| Item | Specification / Example | Research Function | Critical Notes |
|---|---|---|---|
| AN Swab | Flocked (e.g., HydraFlock), Foam (e.g., Puritan 25-1506), or Polyester tip [33] | Specimen collection from anterior nares. | Flocked tips show superior specimen release. Ensure swab length and tip are appropriate for nasal anatomy. |
| Transport Medium | Universal Transport Medium (UTM) [8] [11] | Preserves viral nucleic acid/antigen integrity during transport. | Essential for NAAT; not always required for point-of-care Ag-RDTs. |
| Lysis Buffer | Kit-provided (e.g., Sure-Status, Biocredit) [8] | Extracts and exposes viral antigens or nucleic acids. | Buffer composition is test-specific; do not interchange between brands. |
| Reference Assay | RT-qPCR (e.g., TaqPath COVID-19, Allplex SARS-CoV-2) [8] [31] | Provides gold-standard comparison for validation studies. | Targets should include multiple genes (N, ORF1ab, S) for high specificity. |
| Positive Control | Quantified in vitro-transcribed RNA [8] | Standard curve generation for determining viral load/LoD. | Critical for analytical sensitivity measurements and assay calibration. |
Critical Analysis for Research Application
The decision to adopt AN swabs in influenza research requires careful consideration of the trade-offs involved.
Advantages and Rationale for Adoption: The primary strength of AN swabs lies in their practical superiority. Their minimal invasiveness significantly reduces participant discomfort, which is a major ethical and practical advantage in large-scale or serial sampling studies [11]. This facilitates high compliance rates. Furthermore, the ability to be self-collected under guidance enables decentralized clinical trials and community-based surveillance, reducing the need for clinical visits and specialized healthcare workers for sample collection [32] [33].
Limitations and Mitigation Strategies: The core limitation is the potential for reduced analytical sensitivity, particularly when compared to NP swabs in PCR-based detection. Meta-analyses for SARS-CoV-2 RT-PCR indicate AN specimens can be 12-18% less sensitive than NP swabs [8]. This is likely due to lower recovered viral loads, as directly measured in comparative studies [11] [25]. To mitigate this, AN swabs are ideally deployed for detecting cases with higher viral loads, which are typically the most infectious individuals. For maximum case detection in a study, a combined sampling approach (e.g., AN swab plus saliva) has been shown to increase sensitivity significantly [32] [31].
The relationship between swab type, viral load, and detection success is a key conceptual model for researchers, summarized in the following diagram.
Swab Performance Across Viral Loads
This guide objectively compares the performance of various self-collection protocols for respiratory virus detection, with a specific focus on influenza. The emergence of at-home testing, accelerated by the COVID-19 pandemic, has necessitated the development of robust instructional design and rigorous usability testing to ensure sample quality comparable to clinician-collected specimens. This review synthesizes experimental data on the diagnostic accuracy, usability, and feasibility of different self-collection methods, including anterior nasal, oral-nasal, and saliva sampling. The analysis is framed within the broader research context of validating anterior nasal swabs for influenza detection, providing researchers and drug development professionals with a comparative evaluation of protocols based on empirical evidence.
The paradigm for diagnostic testing for respiratory pathogens has shifted significantly with the development and validation of self-collection protocols. These protocols enable individuals to collect their own nasal, oral, or saliva samples without direct supervision by healthcare workers, thereby expanding testing access, reducing exposure risks, and alleviating burdens on healthcare systems [34] [35]. For influenza detection specifically, self-collection methods present a promising avenue for widespread surveillance and early diagnosis, yet their validity hinges on two critical components: intuitively designed instructions that untrained users can successfully follow, and demonstrable usability across diverse populations.
The instructional design for self-collection kits must account for users with no prior medical or laboratory training, guiding them through the process of obtaining a sample of sufficient quality for molecular detection. Concurrently, usability testing provides the empirical foundation to validate that these instructions are effective and that the resulting samples meet analytical standards [34] [36]. This review systematically compares the performance of various self-collection approaches, detailing their experimental validation, and places these findings within the ongoing research validation of anterior nasal swabs for influenza detection.
Comparative Performance of Self-Collection Methods
The diagnostic performance of self-collected specimens varies by collection method, pathogen, and viral load. The following data summarize key findings from recent studies, providing a comparative basis for protocol selection.
Table 1: Diagnostic Performance of Self-Collected Specimens for Respiratory Viruses
| Collection Method | Target Pathogen | Sensitivity (%) | Specificity (%) | Agreement (Kappa or %) | Key Study Findings |
|---|---|---|---|---|---|
| Anterior Nasal Swab | SARS-CoV-2 | 77.3 - 81.0 (PPA) [37] | 85.5 - 87.0 (NPA) [37] | 100% sample adequacy (RNase P) [35] | Performance comparable to HCW-collected NP swabs in high viral load cases (Ct ≤30) [37] |
| Oral-Nasal Swab | Influenza A/B | 67.0 [12] | 96.0 [12] | Kappa: 0.68 [12] | Lower sensitivity for influenza vs. RSV; not a comparable substitute for NP swab [12] |
| Oral-Nasal Swab | RSV | 75.0 [12] | 99.0 [12] | Kappa: 0.79 [12] | Better performance for RSV than for influenza [12] |
| Saliva | SARS-CoV-2 | 80.5 - 86.7 (PPA) [37] | 87.0 (NPA) [37] | Not reported | PPA increased to 81.2-82.1% with Ct ≤30 [37] |
| Pediatric Anterior Nasal | SARS-CoV-2 | Not reported | Not reported | 97.3% success rate (low errors) [38] | Feasible for school-aged children; mean collection time: 70 seconds [38] |
PPA: Positive Percent Agreement; NPA: Negative Percent Agreement; NP: Nasopharyngeal; HCW: Healthcare Worker; Ct: Cycle Threshold.
The data reveal that self-collected anterior nasal swabs perform reliably for SARS-CoV-2 detection, particularly in individuals with high viral loads, which is often the case in early infection when transmission risk is highest [37]. Conversely, the oral-nasal swab method shows suboptimal and variable sensitivity for influenza compared to RSV, indicating that the optimal self-collection method may be pathogen-dependent [12]. This underscores the importance of context-specific validation, especially for influenza-focused research. Furthermore, studies demonstrate that self-collection is not only feasible for adults but also for school-aged children, with high success rates and low error rates observed in supervised school settings [38].
Instructional Design and Usability Testing Protocols
Core Components of Instructional Design
Effective instruction is a cornerstone of successful self-collection. Usability studies have identified several critical elements for instructional design, typically encapsulated in an Instructions for Use (IFU) document. Key components include:
- Visual and Textual Guidance: Combining clear graphics with simple, step-by-step text is essential. A study on an at-home SARS-CoV-2 kit found that user feedback led to improvements in wording and graphics for critical tasks like placing the label correctly on the tube [34] [36].
- Multi-Modal Support: Providing supplementary materials, such as video tutorials, enhances understanding and proper technique. In one study, participants were given written instructions and access to a video tutorial designed in accordance with international guidelines [35].
- Task Breakdown: Instructions must break down the process into manageable steps, from swab unpacking and sample collection to placement in transport media and final packaging [34].
Methodologies for Usability Testing
Usability testing evaluates whether users can successfully follow the IFU to collect a valid sample. Standard methodologies include:
- Simulated Home Environment: Studies often observe participants without medical training as they follow the IFU in a setting that mimics a home, which helps identify real-world challenges [34] [36].
- Direct Observation and Data Collection: Trained observers record errors, difficulties, and user hesitations without intervening. This is complemented by:
- Post-Collection Surveys: To assess perceived clarity, ease of use, and confidence [35] [36].
- Comprehension Questions: To verify understanding of key instructions [34].
- Specimen Quality Analysis: The ultimate validation is whether the self-collected sample is sufficient for testing, often measured by the detection of a human control gene (e.g., RNase P) via RT-PCR [34] [35].
- Diverse Participant Recruitment: Ensuring the tested population varies in age, education level, and technical proficiency to ensure broad usability [34].
The workflow below illustrates a standardized usability testing process derived from these methodologies.
Figure 1: Usability testing workflow for self-collection protocols.
Detailed Experimental Protocols
To facilitate replication and critical appraisal, this section details key experimental protocols from the cited literature.
Human Factors Usability Study for At-Home Kit
A seminal usability study for an at-home anterior nares SARS-CoV-2 RT-PCR collection kit provides a robust protocol model [34] [36].
- Objective: To determine the usability of an at-home collection kit, with a primary endpoint of the percentage of samples yielding a valid SARS-CoV-2 test result.
- Subjects: 30 adults with no prior medical, laboratory, or COVID-19 self-collection experience.
- Procedure:
- Subjects were provided with the kit containing a sterile nasal swab, transport tube, IFU, and other packaging components.
- In a simulated home environment, subjects were observed while attempting to use the kit by following the IFU alone.
- Observers documented any errors or difficulties without providing guidance.
- Subjects completed a survey and comprehension questions post-collection.
- Outcome Measures:
Validation of Oral-Nasal Swab for Influenza and RSV
A recent diagnostic validation study compared a self-collected oral-nasal swab to a provider-collected nasopharyngeal swab for influenza and RSV detection [12].
- Objective: To validate a self-collected oral-nasal swab for the detection of influenza and RSV using a multiplex PCR panel.
- Study Population: Consecutive adults presenting to an emergency department with suspected viral upper respiratory tract infection.
- Procedure:
- A healthcare provider collected a nasopharyngeal swab as part of routine care (reference standard).
- Participants then self-collected an oral-nasal swab by swabbing both anterior nares, the buccal mucosa, and the tongue using a flocked swab.
- Both specimens were tested using a laboratory-developed multiplex RT-PCR assay.
- Outcome Measures:
- Sensitivity/Specificity: The oral-nasal swab showed a sensitivity of 0.67 and specificity of 0.96 for influenza, and a sensitivity of 0.75 and specificity of 0.99 for RSV [12].
- Conclusion: The self-collected oral-nasal swab was not an acceptable substitute for a nasopharyngeal swab for influenza, primarily due to suboptimal sensitivity [12].
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and reagents commonly used in the development and validation of self-collection protocols for respiratory virus detection.
Table 2: Essential Research Reagents and Materials for Self-Collection Studies
| Item | Function/Application | Example from Literature |
|---|---|---|
| Flocked Anterior Nasal Swab | Sample collection from the anterior nares. Designed for efficient cell collection and elution. | Puritan Sterile Foam Tipped Applicator [38]; Flocked tapered swab (ESwab, Copan) [35]. |
| Universal Transport Media (UTM) | Preserves viral integrity during transport and storage. | Copan UTM [12]; Phosphate buffered saline [38]; Tube containing 0.9% saline [34]. |
| RNA Extraction Kit | Purifies viral RNA from the specimen for downstream molecular analysis. | MagCore Viral Nucleic Acid Extraction Kit [35]; Maxwell HT Viral TNA Kit [12]. |
| RT-PCR Master Mix | Enzymes and reagents for the reverse transcription and amplification of viral RNA. | TaqPath 1-Step RT-qPCR Master Mix [35]; Luna Universal Probe One-Step RT q-PCR kit [12]. |
| Multiplex RT-PCR Assay | Simultaneous detection of multiple respiratory pathogens from a single sample. | BioFire FilmArray Respiratory Panel 2.1 [39]; Allplex SARS-CoV-2/FluA/FluB/RSV Assay [37]. |
| Human Control Assay (e.g., RNase P) | Quality control to confirm that sufficient human cellular material was collected. | Detection of human RNase P gene via qRT-PCR [34] [35]. |
The validation of self-collection protocols, particularly for influenza, remains a critical endeavor in public health and diagnostic development. The experimental data compared in this guide demonstrate that while anterior nasal self-swabbing is a well-validated, user-friendly, and effective method for SARS-CoV-2—with clear implications for influenza research—other methods like oral-nasal swabs may show pathogen-dependent performance and require further optimization. The success of any self-collection protocol is inextricably linked to its instructional design and validation through rigorous human factors usability testing. As research continues, future work should focus on standardizing these protocols, optimizing them specifically for influenza viruses, and exploring their integration with emerging multiplex platforms and home-based testing technologies.
The global response to the COVID-19 pandemic revealed critical vulnerabilities in diagnostic supply chains, particularly regarding specimen collection and processing components. This experience underscored the necessity of validating alternative methodologies for respiratory virus detection, forming a crucial thesis context for the validation of anterior nasal swabs for influenza detection research. While nasopharyngeal swab (NPS) collection remains the historical gold standard for respiratory virus testing, its limitations including patient discomfort, need for trained healthcare workers, and supply chain constraints have accelerated research into less invasive alternatives [40] [41]. This guide objectively compares the laboratory performance of anterior nasal swabs against other collection methods, with specific focus on transport media, nucleic acid extraction, and PCR amplification efficiency for influenza detection, providing researchers with evidence-based protocols and analytical frameworks for diagnostic development.
Comparative Performance of Specimen Collection Methods
Diagnostic Accuracy Across Swab Types and Collection Sites
Multiple clinical studies have directly compared the performance of anterior nasal swabs to nasopharyngeal swabs for respiratory virus detection. The diagnostic accuracy varies significantly depending on the specific pathogen and collection method.
Table 1: Diagnostic Performance of Anterior Nasal Swabs Compared to Nasopharyngeal Swabs
| Virus Target | Collection Method | Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) | Study Details |
|---|---|---|---|---|---|---|
| SARS-CoV-2 | ANS (Rhinoswab) | 80.7% (73.8-86.2) | 99.6% (97.3-100) | 99.3% (95.5-100) | 87.9% (83.3-91.4) | n=412, OP/NP reference [41] |
| SARS-CoV-2 | ANS (standard) | 72.5% (58.3-84.1) | 100% (99.3-100) | 100% | 98.5% | n=862, NP reference [11] |
| Influenza A/B | Oral-Nasal (self) | 67% (49-81) | 96% (89-99) | N/R | N/R | n=128, NP reference [12] |
| RSV | Oral-Nasal (self) | 75% (43-95) | 99% (93-100) | N/R | N/R | n=128, NP reference [12] |
| SARS-CoV-2 | Anterior Nares (self) | 82-84% (66-94) | N/R | N/R | N/R | vs. NP RT-PCR [42] |
For influenza detection specifically, a 2025 validation study found that self-collected oral-nasal swabs (swabbing both anterior nares along with the tongue and buccal mucosa) showed suboptimal test characteristics compared to healthcare provider-collected nasopharyngeal swabs, with a sensitivity of 67% (95% CI: 49-81%) and specificity of 96% (95% CI: 89-99%) [12]. This indicates that while anterior nasal collection methods show promise for SARS-CoV-2 detection, further optimization is required for reliable influenza detection, particularly concerning self-collection protocols.
Viral Load Recovery Across Collection Methods
Viral concentration, as measured by cycle threshold (Ct) values in RT-PCR, provides crucial information about the efficiency of viral recovery across different collection methods.
Table 2: Viral Load Comparison Across Sample Types
| Sample Type | Swab Type | Median Viral Load (Copies/μL) | IQR | Ct Value Comparison | PCR-Positive Rate vs. NPS |
|---|---|---|---|---|---|
| Nasopharyngeal (NPS) | Flocked | 53,560 | 605-608,050 | Reference | 100% |
| Anterior Nasal (AWN) | NP-type | 1,792 | 7-81,513 | Significantly higher (p<0.001) | 84.4% |
| Anterior Nasal (AWO) | OP-type | 6,369 | 7-97,535 | Significantly higher (p<0.001) | 81.3% |
| Nasal (10 rubs) | Flocked | N/R | N/R | Ct=24.3 | Comparable to NPS |
| Nasal (5 rubs) | Flocked | N/R | N/R | Ct=28.9 (p=0.002) | Lower than 10-rub |
One critical finding from comparative studies is that vigorously rubbed nasal swabs (10 rotations) yielded significantly lower Ct values (median Ct=24.3) compared to those collected with fewer rotations (median Ct=28.9, p=0.002), achieving SARS-CoV-2 concentrations similar to NPS [24]. This demonstrates that collection technique substantially impacts viral load recovery, which has direct implications for optimizing anterior nasal sampling protocols for influenza detection.
Laboratory Processing Methodologies
Transport Media and Swab Material Comparisons
Supply chain limitations during the COVID-19 pandemic prompted systematic evaluation of alternative transport media and swab materials, with implications for influenza testing protocols.
Table 3: Swab and Transport Media Performance for Viral Detection
| Swab Type | Tip Material | Shaft Material | Median Fluid Retention (μL) | Viral Detection Efficiency |
|---|---|---|---|---|
| PurFlock Ultra | Synthetic flocked | Polystyrene | 115 | Comparable to reference |
| FLOQSwab | Synthetic flocked | Polystyrene | 25 | Comparable to reference |
| Puritan Polyester Tip | Polyester | Polystyrene | 127 | Comparable to reference |
| Hologic Aptima | Polyester | Polystyrene | 26 | Comparable to reference |
| Puritan Cotton | Cotton | Aluminum | 13.4 | Comparable to reference |
| MedPro Cotton | Cotton | Wooden | 218 | Comparable to reference |
Research demonstrated no meaningful difference in viral yield across six different swab types when testing for SARS-CoV-2, indicating that multiple swab alternatives could be deployed during supply shortages [43]. Similarly, transport medium comparisons found that DMEM, PBS, 100% ethanol, 0.9% normal saline, and commercial VTM all supported SARS-CoV-2 detection with comparable efficiency when stored at room temperature for up to 72 hours [43]. This robustness across transport conditions provides flexibility for laboratory processing workflows.
Nucleic Acid Extraction and PCR Amplification
Standardized protocols for nucleic acid extraction and PCR amplification are critical for maintaining test sensitivity across different collection methods.
In validation studies for influenza and RSV detection, specimens collected in universal transport media were processed using automated extraction systems. Specifically, a 160-µL aliquot was extracted using the Hamilton Star automated extraction instrument with the Maxwell HT Viral TNA Kit (Promega) [12]. For SARS-CoV-2 detection, comparable workflows employed the NucliSENS EasyMag system or QIAcube with QIAamp Viral RNA Mini Kits for nucleic acid extraction [40] [41].
Detection of viral targets was performed using laboratory-developed real-time reverse-transcription PCR (RT-PCR) assays with the Luna Universal Probe One-Step RT-qPCR kit (New England Biolabs) on the CFX96 Touch Real-Time PCR detection system (Bio-Rad) [12]. Alternatively, commercial panels like the Allplex Respiratory Panels 1/2/3 and Allplex SARS-CoV-2 real-time PCR have been utilized successfully with anterior nasal specimens [24]. Positive specimens are typically defined as those with cycle threshold (Ct) values for the viral target below 37 cycles [12].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Anterior Nasal Swab Validation Studies
| Category | Specific Product | Function/Application | Performance Notes |
|---|---|---|---|
| Collection Swabs | FLOQSwab (Copan) | Synthetic flocked swab for anterior nasal collection | Lower fluid retention (25μL) but excellent viral release [24] [43] |
| PurFlock Ultra (Puritan) | Synthetic flocked swab alternative | Higher fluid retention (115μL) [43] | |
| ClearTip (Yukon Medical) | Injection-molded anterior nasal swab | Non-absorbent design, efficient viral release in preclinical models [40] | |
| Rhinoswab (Rhinomed) | Double-loop nylon-flocked swab for both nostrils | 80.7% sensitivity for SARS-CoV-2 vs. OP/NP reference [41] | |
| Transport Media | Universal Transport Media (UTM) | Maintains viral integrity during transport | Standardized composition for consistent recovery |
| Viral Transport Media (VTM) | Alternative viral transport medium | Comparable performance to UTM for SARS-CoV-2 [43] | |
| DMEM/PBS | Alternative transport solutions | Viable alternatives during supply shortages [43] | |
| Extraction Kits | Maxwell HT Viral TNA Kit | Automated nucleic acid extraction | Compatible with Hamilton Star system [12] |
| QIAamp Viral RNA Mini Kit | Manual or automated extraction | Compatible with QIAcube systems [24] | |
| NucliSENS EasyMag | Automated nucleic acid extraction | Used in clinical validation studies [40] | |
| PCR Reagents | Luna Universal Probe One-Step RT-qPCR | One-step RT-qPCR detection | Used in laboratory-developed tests [12] |
| Allplex Respiratory Panels 1/2/3 | Multiplex respiratory virus detection | Commercial panel for multiple targets [24] | |
| CDC 2019-nCoV RT-PCR Diagnostic Panel | SARS-CoV-2 specific detection | Emergency use authorized assay [40] |
The validation of anterior nasal swabs for respiratory virus detection requires careful consideration of the entire laboratory processing pipeline, from collection to amplification. Current evidence indicates that anterior nasal sampling demonstrates strong performance for SARS-CoV-2 detection with sensitivities ranging 73-85% compared to nasopharyngeal swabs, but shows more variable performance for influenza with lower sensitivity (67%) in self-collected oral-nasal specimens [12] [11] [41]. Key factors influencing detection sensitivity include swab collection technique (number of rotations), swab material properties, and viral transport stability. The research reagents and methodologies detailed in this guide provide a foundation for optimizing anterior nasal sampling protocols specifically for influenza detection, with particular attention to self-collection standardization and PCR assay optimization to address current sensitivity limitations. Future directions should focus on technique refinement and assay development to improve the reliability of anterior nasal sampling for influenza surveillance and diagnosis.
Within the critical pursuit of accurate respiratory virus detection in children, specimen collection has long presented a significant challenge. The discomfort and procedural anxiety associated with traditional methods can compromise both the patient experience and the quality of surveillance data. This guide objectively compares the performance of anterior nasal swabs (ANS) against other common sampling techniques in pediatric populations, focusing on their superior tolerability and operational feasibility. The evidence, drawn from recent clinical studies, validates the role of ANS as a patient-friendly and effective tool for influenza and respiratory virus detection in both clinical and community settings.
Performance Comparison: Diagnostic Accuracy
The diagnostic accuracy of anterior nasal swabs has been rigorously evaluated against established standard methods, such as combined throat and nasal swabs (CTN) and nasopharyngeal swabs (NPS). The following table summarizes key performance metrics from recent pediatric studies.
Table 1: Diagnostic Accuracy of Anterior Nasal Swabs vs. Reference Standards
| Reference Standard | Study Population | Overall Positive Percentage Agreement (PPA) | Overall Negative Percentage Agreement (NPA) | Virus-Specific PPA (when collected within 24 hours of NPS) |
|---|---|---|---|---|
| Combined Throat & Nasal Swab (CTN) [44] [45] | 249 symptomatic children (5-18 years) | 96.2% (95% CI, 91.8–98.3%) | 99.8% (95% CI, 99.6–99.9%) | Not Applicable (Reference is CTN) |
| Nasopharyngeal Swab (NPS) [46] [19] | 147 hospitalized children (NP collected within prior 72 hours) | 84.3% (overall); 95.7% (when within 24 hours) | Specificity: 100% for most viruses [19] | 100%: Adenovirus, Influenza, Parainfluenza, RSV, SARS-CoV-2 [46] [19] >75%: Human Metapneumovirus, Rhinovirus/Enterovirus [46] [19] 36.4%: Seasonal Coronavirus [46] [19] |
The data demonstrates that anterior nasal swabs have high agreement with standard-of-care methods for detecting most common respiratory viruses, especially when the time between collecting different sample types is minimized [46] [19]. The notably lower sensitivity for seasonal coronaviruses requires further investigation but does not diminish the strong overall performance for other major pathogens, including influenza.
Experimental Protocols for Key Studies
The compelling data supporting anterior nasal swabs are derived from methodologically sound clinical trials. The protocols for two pivotal studies are detailed below.
Protocol 1: Diagnostic Accuracy vs. Combined Throat and Nasal Swab
This prospective study aimed to determine the positive and negative percentage agreement of a novel anterior nasal swab (ANS) with the combined throat and anterior nasal swab (CTN) as the reference standard [44] [45].
- Study Design & Population: A prospective, randomized diagnostic accuracy study was conducted at a tertiary pediatric hospital. It enrolled 249 symptomatic children aged 5–18 years presenting with respiratory tract infection symptoms [44] [45].
- Sample Collection: All participants underwent both ANS and CTN sampling, with the order of collection randomized. The ANS was available in age-specific sizes and was typically self-administered by the child or with parental/nurse assistance. It was inserted for 60 seconds, followed by side-to-side movements for 15 seconds. The CTN was collected by a study nurse, who swabbed the tonsillar beds and throat, followed by bilateral nasal insertion and rotation [44] [45].
- Laboratory Analysis: Both sample types were eluted and tested using a multiplex RT-PCR panel (AusDiagnostics Respiratory Pathogens 16-well assay) for a comprehensive range of respiratory viruses, including influenza, RSV, and SARS-CoV-2. Cycle threshold (CT) values were recorded [44] [45].
- Outcome Measures: The primary outcomes were the positive and negative percentage agreement of ANS compared to CTN. Secondary outcomes included participant and clinician ratings of comfort and preference [44] [45].
Protocol 2: Feasibility of Self-Collection in a School Setting
This cohort study assessed the feasibility of school-aged children self-collecting lower nasal swabs for SARS-CoV-2 surveillance over an academic year [38].
- Study Design & Population: A prospective pilot cohort study was conducted at a K-8 school. It involved 296 students who participated in weekly SARS-CoV-2 surveillance testing [38].
- Sample Collection & Training: Students were brought to an outdoor testing site in cohorts. Clinical research staff in full personal protective equipment provided instructions and observed all self-collections. Children were shown an instructional video and used anterior nares swabs. Small mirrors were available at stations to assist with the process. The procedure involved inserting the swab fully into one nostril until resistance was felt and rubbing it in four circles before repeating in the other nostril [38].
- Data Collection: Researchers collected data on two key parameters: error rates (e.g., contaminated swabs, inadequate swabbing) and the time taken for sample collection during each testing encounter [38].
- Outcome Measures: The main outcomes were the frequency and trend of self-collection errors over time and the mean duration of each testing encounter [38].
Diagram 1: Diagnostic Accuracy Study Workflow
Tolerability and Patient Preference
A primary advantage of anterior nasal swabs in pediatrics is their superior tolerability. Quantitative data from comparative studies reveal a strong patient and caregiver preference for this method.
Table 2: Tolerability and Acceptability of Swabbing Methods in Children
| Metric | Anterior Nasal Swab (ANS) | Combined Throat/Nasal Swab (CTN) | Source |
|---|---|---|---|
| High Comfort Rate | 90% rated "extremely comfortable" or only "a little uncomfortable" | 48% gave the same ratings | [44] [45] |
| Future Testing Preference | 87% of children/parents indicated they would prefer ANS for future testing | N/A (Implied lower preference) | [44] [45] |
| Direct Preference | 84% of children rated the ANS as their preferred swab | 16% preferred the CTN | [44] [45] |
| Barrier: Fear/Discomfort | N/A (Less associated with this barrier) | Cited by 20.5% of refusers as a reason to decline a research swab | [47] |
The invasive nature of traditional nasopharyngeal (NPS) and oropharyngeal (OPS) swabs is a significant barrier. One study found that 83.9% of pediatric participants or their caregivers refused a research-related NPS/OPS collection, with "fear or discomfort of the procedure" being the second most common reason (20.5%) after testing fatigue [47]. In a hospital setting, this refusal was absolute, with none of the 46 participants agreeing to an additional research swab [47]. This starkly contrasts with the high acceptance and preference for anterior nasal swabs.
Feasibility and Implementation
The feasibility of anterior nasal swabs, particularly for large-scale surveillance, is demonstrated by their successful implementation in non-clinical settings and their potential for self-collection.
- Low Error Rate in Self-Collection: A school-based study involving 296 children reported that self-collection errors occurred in only 2.7% of 4,203 total testing encounters. The error rate was highest on the first day (10.2%) but decreased over time, indicating that children can quickly achieve proficiency with the procedure [38].
- Rapid Testing Workflow: In the same school study, the mean duration of each testing encounter was 70 seconds, demonstrating that self-collection can be integrated into a school schedule with minimal disruption [38].
- Handling Considerations: While feasible, one study noted that the specific ANS device used required additional laboratory handling processes compared to standard swabs, and a slightly higher proportion of ANS samples needed to be re-run (9.6% vs. 2% for CTN) [44]. This highlights the importance of considering end-to-end workflow in implementation planning.
Diagram 2: School Self-Collection Feasibility Workflow
The Scientist's Toolkit
The successful implementation and validation of anterior nasal swabs for pediatric respiratory virus detection rely on specific reagents and materials. The following table details key solutions used in the featured experiments.
Table 3: Essential Research Reagents and Materials
| Item | Function/Description | Example from Research |
|---|---|---|
| Flocked Anterior Nasal Swab | Specimen collection; designed for comfort and effective cell collection from the anterior nares. | Rhinoswab Junior (Rhinomed) [44] [45]; Puritan Sterile Foam Tipped Applicator [38]. |
| Multiplex RT-PCR Assay | Detection & differentiation of multiple respiratory pathogens from a single sample. | AusDiagnostics Respiratory Pathogens 16-well assay [44] [45]; Other FDA EUA-approved PCR assays [38]. |
| Viral Transport Medium / PBS | Stabilizes viral RNA/DNA during transport and storage prior to laboratory testing. | Phosphate Buffered Saline (PBS) [44] [38]. |
| RNA Extraction Kit | Isolates viral nucleic acids from the specimen for downstream molecular analysis. | MagNA Pure 96 DNA and Viral NA Small Volume Kit (Roche) [44] [45]. |
The consolidated evidence from recent pediatric studies firmly establishes anterior nasal swabs as a superior alternative to more invasive methods for respiratory virus detection, balancing high diagnostic accuracy with exceptional patient comfort. For researchers and public health professionals designing surveillance studies or clinical trials, ANS offers a practical solution to increase participation rates and reduce procedural barriers. For drug development, the reliability of ANS for detecting viruses like influenza ensures that clinical trial endpoints based on virologic confirmation are robust, while its tolerability is crucial for patient retention and ethical compliance in pediatric studies. The validation of self-collection protocols further opens the door to decentralized monitoring and large-scale community surveillance, making anterior nasal swabs a key tool in modern respiratory disease management.
The concurrent circulation of Influenza, Respiratory Syncytial Virus (RSV), and SARS-CoV-2 presents a formidable challenge for clinical diagnostics and public health systems worldwide. These viruses share overlapping clinical presentations—including fever, cough, and respiratory distress—yet require distinct therapeutic and management strategies. The critical need to differentiate these pathogens rapidly and accurately has accelerated the development and integration of multiplex molecular panels into diagnostic workflows.
This objective guide compares the performance of various commercially available and laboratory-developed multiplex assays for the simultaneous detection of these three major respiratory viruses. A particular focus is placed on the validation of less invasive specimen collection methods, such as anterior nasal swabs, which are essential for expanding testing accessibility and patient comfort, especially within the broader context of pandemic preparedness [12].
Performance Comparison of Multiplex Detection Platforms
The following tables summarize the key performance characteristics of several molecular and rapid antigen tests for detecting Influenza, RSV, and SARS-CoV-2, as reported in validation studies.
Table 1: Performance Characteristics of Molecular Multiplex Assays
| Assay Name | Technology | Target Viruses | Sensitivity | Specificity | Reference |
|---|---|---|---|---|---|
| PowerChek SARS-CoV-2, Influenza A&B, RSV | Multiplex rRT-PCR | SARS-CoV-2, Flu A/B, RSV | SARS-CoV-2: 100%Flu A: 100%Flu B: 100%RSV: 93.1% | 100% for all targets | [48] |
| TaqMan SARS-CoV-2, Flu A/B, RSV | Multiplex rRT-PCR | SARS-CoV-2, Flu A/B, RSV | 91.1% - 100% (across targets in NP samples) | 94.87% - 100% (across targets in NP samples) | [49] |
| PKamp RT-PCR Panel | Multiplex rRT-PCR | SARS-CoV-2, Flu A/B, RSV | SARS-CoV-2 (Saliva): 91.9%SARS-CoV-2 (NPS): 97.5% | Not specified | [50] |
| Lab-Developed Automated Panel (cobas systems) | Multiplex PCR | 16 respiratory viruses, including SARS-CoV-2, Flu A/B, RSV | SARS-CoV-2: 99.4%Influenza A: 95%Other targets: 80-100% | 96.3% - 100% (across targets) | [51] |
| One-Step RT-ddPCR Assay | Droplet Digital PCR | IAV, IBV, RSV | High agreement with RT-qPCR for IAV (κ=0.834) and RSV (κ=0.773) | High specificity confirmed with synthetic standards | [52] |
Table 2: Performance Characteristics of Rapid Antigen Tests (RATs) and Other Platforms
| Assay Name / Type | Technology | Target Viruses | Sensitivity / Remarks | Specificity | Reference |
|---|---|---|---|---|---|
| InstaView COVID-19/Flu Ag Combo | Multiplex Rapid Antigen | SARS-CoV-2, Flu A/B | Significantly higher positivity rates; able to detect Omicron subvariants | Not specified | [53] |
| Multiplex Lateral Flow Tests (3 brands) | Multiplex Lateral Flow | SARS-CoV-2, Flu A, RSV | Sensitivity >80% for Flu A & SARS-CoV-2; >84% for RSV (2/3 brands) | >97% for most tests and targets | [54] |
| Self-Collected Oral-Nasal Swab | Multiplex PCR vs. NPS | Influenza, RSV | Influenza: 67%RSV: 75% | Influenza: 96%RSV: 99% | [12] |
| Seegene Anyplex II RV16 | Multiplex PCR | 16 respiratory viruses | Overall: 96.6% | Overall: 99.8% | [55] |
| BioFire FilmArray RP2.1 plus | Multiplex PCR | 23 respiratory pathogens | Overall: 98.2% | Overall: 99.0% | [55] |
Key Experimental Protocols and Workflows
Understanding the experimental methodologies is crucial for evaluating and implementing these diagnostic solutions.
Validation of Self-Collected Oral-Nasal Swabs
A 2025 study directly addressed the validation of alternative, less invasive sampling methods by comparing self-collected oral-nasal swabs to healthcare worker-collected nasopharyngeal swabs (NPS) in an emergency department setting [12].
- Study Population & Design: Consecutive adult patients presenting with suspected viral upper respiratory tract infections provided a self-collected oral-nasal swab (swabbing both anterior nares, buccal mucosa, and tongue) in addition to a routine clinical NPS [12].
- Testing Method: Both swabs were tested using a laboratory-developed multiplex real-time RT-PCR assay for Influenza A/B and RSV, among other pathogens. The NPS served as the reference standard [12].
- Key Findings: The self-collected swab showed suboptimal sensitivity for Influenza (67%), though specificity remained high (96%). Performance for RSV was better, with a sensitivity of 75% and specificity of 99%. The study concluded that while feasible, the self-collected oral-nasal swab was not an acceptable substitute for an NPS for multiplex Influenza and RSV testing primarily due to the suboptimal Influenza test characteristics [12].
Workflow for High-Throughput Laboratory-Developed Tests
A 2024 study detailed the development and validation of a high-throughput, laboratory-developed test (LDT) on automated cobas systems [51].
- Assay Design: The LDT consolidated 16 respiratory viral targets into three multiplex PCR assays:
- RESP1: SARS-CoV-2, Influenza A/B, RSV
- RESP2: hMPV, hBoV, hAdV, Rhino/Enterovirus
- RESP3: HPIV 1-4, human Coronaviruses (229E, NL63, OC43, HKU1) [51]
- Analytical Validation: Performance was rigorously evaluated using digital-PCR based standards and international reference materials. Key parameters included:
- Limit of Detection (LoD): Determined via Probit analysis (e.g., SARS-CoV-2: 29.3 IU/mL; Influenza A: 179.9 cp/mL).
- Linearity and Precision: Verified over several log steps with low variability [51].
- Clinical Validation: The assay demonstrated high positive and negative agreement with reference methods when tested on clinical samples, proving its suitability for scalable screening in high-risk populations [51].
Comparative Evaluation of Commercial Multiplex Panels
A 2024 study from South Africa provided a direct performance comparison of three commercial multiplex panels using a composite reference standard [55].
- Platforms Compared:
- Seegene Anyplex II RV16: Requires pre-extraction and pre-reverse transcription, with results in ~2 hours.
- BioFire FilmArray RP2.1 plus: Fully automated, integrated extraction and amplification in a closed pouch, with results in ~45 minutes.
- QIAstat-Dx Respiratory SARS-CoV-2 Panel: Automated cartridge-based system providing semi-quantitative Ct values, with results in ~69 minutes [55].
- Methodology: Forty-eight respiratory specimens were tested on all three platforms. A composite reference standard was applied to calculate sensitivity and specificity for overlapping targets [55].
- Outcome: The Seegene Anyplex and BioFire FilmArray showed high and comparable overall sensitivity (96.6% and 98.2%, respectively), while the QIAstat-Dx demonstrated inferior sensitivity (80.7%) [55].
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful implementation of multiplex respiratory virus testing relies on a suite of critical reagents and materials.
Table 3: Key Research Reagent Solutions for Multiplex Assay Development
| Item Category | Specific Examples | Function & Application |
|---|---|---|
| Nucleic Acid Extraction Kits | QIAamp DSP Viral RNA Mini Kit (Qiagen), Omega Bio-Tek Mag-Bind Viral RNA Xpress Kit, NucliSENS easyMAG system (bioMérieux) | Purification of viral RNA from clinical specimens (NPS, saliva) prior to amplification [48] [49] [55]. |
| One-Step RT-PCR Master Mixes | TaqPath 1-Step Multiplex Master Mix (Thermo Fisher), Luna Universal Probe One-Step RT qPCR Kit (NEB) | Enables reverse transcription and PCR amplification in a single reaction, crucial for workflow efficiency [12] [49]. |
| Commercial Multiplex Assays | PowerChek (Kogene Biotech), PKamp (PerkinElmer), Allplex (Seegene), TaqMan Assays (Thermo Fisher) | Pre-optimized primer-probe sets for specific viral targets (e.g., SARS-CoV-2 ORF1ab/N, Flu A M gene, RSV N gene), ensuring reliability [48] [53] [49]. |
| Automated Platforms | BioFire FilmArray Torch, QIAstat-Dx, cobas 5800/6800/8800 Systems (Roche) | Integrated systems that automate extraction, amplification, and detection, reducing hands-on time and variability [55] [51]. |
| Reference & Control Materials | AcroMetrix Coronavirus 2019 RNA Control (Thermo Fisher), SeraCare Reference Controls, Inactivated virus pellets (Microbiologics, ATCC) | Essential for determining analytical sensitivity (LoD), assessing assay accuracy, precision, and monitoring test performance [48] [49] [50]. |
The integration of multiplex panels for the simultaneous detection of Influenza, RSV, and SARS-CoV-2 represents a significant advancement in diagnostic efficiency and public health response. Molecular platforms like the BioFire FilmArray, PowerChek, and high-throughput LDTs demonstrate excellent performance, making them suitable for clinical laboratories with varying testing volumes [48] [55] [51].
However, the validation of less invasive collection methods remains a complex challenge. While self-collected oral-nasal swabs offer logistical advantages and are feasible for deployment, current evidence indicates they have suboptimal sensitivity, particularly for Influenza, when compared to provider-collected NPS [12]. This highlights a critical area for future research and development. The ideal path forward involves continued innovation in both assay technology and specimen collection to provide highly sensitive, rapid, and patient-friendly diagnostic solutions for respiratory virus detection.
Lucira Health's at-home molecular testing technology represented a significant breakthrough in decentralized diagnostics, becoming the first over-the-counter combination test for influenza and COVID-19 authorized by the FDA. This innovative platform utilized loop-mediated isothermal amplification (LAMP) technology to deliver molecular-level sensitivity in a disposable, consumer-friendly format. Developed from microfluidics research at UC Berkeley, Lucira's product offered results in 11-30 minutes with performance characteristics bridging the gap between rapid antigen tests and laboratory-based PCR. Despite its technological achievements, the company faced insurmountable financial and regulatory challenges, filing for bankruptcy just days before receiving FDA authorization for its flagship combination test. This analysis examines Lucira's technology performance against alternative diagnostic platforms within the context of anterior nasal swab validation research.
Lucira's diagnostic platform integrated multiple advanced technologies to create a self-contained, disposable molecular testing system suitable for home use. The core innovation centered on adapting complex laboratory molecular testing principles into a simple, consumer-operable device.
Core Technological Components
Molecular Detection Principle: Lucira's test utilized reverse transcription loop-mediated isothermal amplification (RT-LAMP) to detect viral RNA targets. This method amplifies specific genetic sequences at a constant temperature of approximately 65°C, eliminating the need for the thermal cycling required in traditional PCR [56]. The reaction detects influenza A, influenza B, and SARS-CoV-2 viral RNA through colorimetric changes induced by amplification byproducts, measured by integrated optoelectronics [57].
Microfluidic Innovation: The platform evolved from the Self-Powered Integrated Microfluidic Blood Analysis System (SIMBAS), originally developed at UC Berkeley. This system initially used degas-driven fluid flow through PDMS microchannels but transitioned to pressure-driven flow with electrically activated pumps to improve manufacturability and reliability at scale [57]. This evolution addressed the material limitations of PDMS, which, while excellent for research prototyping, lacked the reproducibility needed for mass production.
Sample Processing and Readout: The fully integrated system processed anterior nasal swab samples, metered reagent volumes, performed nucleic acid amplification, and detected colorimetric changes using halochromic agents. An onboard microprocessor analyzed the optical signals and displayed results via simple LED indicators within 11 minutes for positive results and 30 minutes for negative results [57]. This design eliminated subjective interpretation and provided clear, binary results to untrained users.
Performance Comparison with Alternative Diagnostic Platforms
Lucira's technology occupies a unique position in the diagnostic landscape, offering near-PCR sensitivity with the convenience of rapid antigen tests. The following comparative analysis evaluates its performance against other available influenza detection methods.
Comprehensive Performance Metrics
Table 1: Comparative Performance of Influenza Detection Platforms
| Platform Type | Technology | Sensitivity Range | Specificity Range | Time to Result | Setting | Approx. Cost |
|---|---|---|---|---|---|---|
| Lucira At-Home Test | RT-LAMP (Molecular) | 98% (for influenza A/B vs NP swab) [57] | Not specified | 11-30 minutes [57] | Home | ~$50 [56] |
| Laboratory PCR | rRT-PCR | 94.3% (NP swab) [1] | >99% | Hours to days | Laboratory | $50+ [56] |
| Digital RIDTs | Immunofluorescence | 79.8%-94.5% [58] [59] | 97.7%-100% [58] [59] | 10-20 minutes | Clinical | $15-$30 |
| Conventional RIDTs | Immunochromatography | 72.6%-81.7% [59] | >95% [59] | 10-15 minutes | Clinical/Home | $5-$15 |
| Anterior Nasal Swab with PCR | rRT-PCR | 84.3%-95.7% (vs NP swab) [46] [19] | High (when collected within 24hr) [46] | Hours to days | Laboratory | Varies |
Table 2: Influenza Detection Sensitivity by Swab Type and Testing Methodology
| Swab Type | Testing Method | Sensitivity | Study Population | Reference |
|---|---|---|---|---|
| Midturbinate | Lucira Molecular | 98% (for influenza A/B) [57] | Not specified | Lucira Health [57] |
| Anterior Nasal | Molecular | 95.7% (when collected within 24hr of NP) [46] | Pediatric | Kietzman et al. 2025 [46] |
| Anterior Nasal | Molecular | 84.3% (overall) [19] | Pediatric | Kietzman et al. 2025 [19] |
| Nasal | rRT-PCR | 88.6% [1] | Adult | Lambert et al. 2012 [1] |
| Nasopharyngeal | rRT-PCR | 94.3% [1] | Adult | Lambert et al. 2012 [1] |
Key Performance Insights
The data demonstrates that Lucira's technology achieved exceptional sensitivity (98%) for influenza detection comparable to nasopharyngeal swabs with PCR, while using a less invasive midturbinate sampling approach suitable for self-collection [57]. Recent research validates that anterior nasal swabs can provide high sensitivity (95.7%) for influenza detection when paired with molecular methods and collected within 24 hours of symptom onset [46] [19].
When compared to rapid influenza diagnostic tests (RIDTs), Lucira's molecular approach shows markedly superior sensitivity relative to both conventional RIDTs (72.6%-81.7%) and digital RIDTs (79.8%-94.5%) [58] [59]. This performance advantage comes with a trade-off in cost and time-to-result, positioning Lucira's technology in a premium segment of the diagnostic market.
Experimental Protocols and Methodologies
Lucira Technology Validation Protocol
Lucira's test validation incorporated rigorous clinical studies comparing its performance against established reference methods:
Sample Collection: The test utilized a midturbinate swab collection method based on Lucira's comparative study of nasopharyngeal, midturbinate, and anterior nasal swabs. This research demonstrated that midturbinate swabs provided 98% sensitivity for detecting influenza with significantly reduced discomfort compared to nasopharyngeal swabs [57].
Testing Procedure: Users inserted the swab into the test unit's vial, then twisted and pressed it against the vial to express the sample. The unit was then activated, initiating the automated testing process. The integrated system performed sample preparation, nucleic acid amplification, and detection without user intervention [57].
Reference Standard Comparison: Lucira's clinical validation compared results with FDA-approved molecular methods, though the specific protocols were not detailed in the available literature. The 98% sensitivity claim suggests comparison with PCR-based methods as the reference standard [57].
Anterior Nasal Swab Validation Protocol
Recent research validating anterior nasal swabs for respiratory virus detection provides methodological frameworks applicable to Lucira's technology assessment:
Study Population: Hospitalized children in Kansas City, MO, from January 2023 to February 2024, who had NP specimens obtained for standard of care multiplex respiratory viral testing in the previous 72 hours [46] [19].
Sample Collection: Paired NP and anterior nasal swab specimens were collected and tested alongside salvaged NP specimens for multiple respiratory viruses including adenovirus, seasonal coronaviruses, influenza, RSV, and SARS-CoV-2 using multiplex molecular testing [46].
Testing Methodology: Both specimen types were tested using multiplex molecular assays. Cycle threshold (Ct) values were compared between paired specimens to assess viral load correlations. Statistical analysis included concordance assessment, sensitivity, and specificity calculations with NP specimens as the reference [19].
Signaling Pathways and Experimental Workflows
Lucira Molecular Detection Workflow
Diagram 1: Lucira molecular detection workflow (Total characters: 94)
Comparative Diagnostic Pathway
Diagram 2: Diagnostic testing pathways (Total characters: 89)
Research Reagent Solutions and Essential Materials
Table 3: Key Research Reagents and Materials for At-Home Molecular Testing
| Reagent/Material | Function | Example/Specification |
|---|---|---|
| RT-LAMP Master Mix | Isothermal nucleic acid amplification | Contains reverse transcriptase, strand-displacing DNA polymerase, dNTPs, and target-specific primers [56] |
| Halochromic pH Indicator | Colorimetric detection of amplification | pH-sensitive dyes that change color during nucleic acid amplification [57] |
| Viral Lysis Buffer | Viral envelope disruption and RNA stabilization | Contains detergents and reducing agents to release nucleic acids [59] |
| Nasal Swab | Sample collection | Midturbinate or anterior nasal swab optimized for self-collection [57] |
| Microfluidic Chip | Fluid handling and reaction containment | Disposable cartridge with integrated chambers and channels [57] |
| Optoelectronic Components | Signal detection and interpretation | LED light sources and photodetectors for colorimetric measurement [57] |
| Positive Control | Assay validation | Synthetic RNA or inactivated virus to verify test performance |
Addressing Performance Challenges in Anterior Nasal Influenza Detection
This comparison guide objectively evaluates the performance of anterior nasal swabs for influenza detection against the clinical gold standard of nasopharyngeal swabs. The analysis focuses on the correlation between cycle threshold values, viral load measurements, and resulting test sensitivities, drawing on recent clinical studies. Evidence indicates that self-collected anterior nasal and oral-nasal swabs demonstrate suboptimal sensitivity for influenza detection primarily due to lower viral loads recovered from anterior nasal sites compared to nasopharyngeal regions. This technical assessment provides researchers and drug development professionals with critical performance data and methodological frameworks for advancing respiratory virus diagnostic platforms.
Influenza virus detection presents unique challenges for less invasive sampling methods. While anterior nasal swabs offer significant practical advantages for mass testing and self-collection, their analytical performance for influenza detection lags behind that of nasopharyngeal swabs. This performance gap is intrinsically tied to viral load differences between anatomical sites and their impact on cycle threshold values in molecular assays. Understanding these correlations is essential for developing effective testing strategies, particularly as respiratory virus surveillance expands beyond clinical settings. The fundamental issue lies in the differential viral distribution within the respiratory tract, where nasopharyngeal regions typically harbor higher concentrations of influenza virus compared to anterior nasal passages [12] [11].
Comparative Performance Data: Anterior Nasal vs. Nasopharyngeal Sampling
Direct Comparison of Influenza Detection Sensitivity
Recent clinical studies consistently demonstrate that anterior nasal sampling methods yield lower sensitivity for influenza detection compared to nasopharyngeal swabs, primarily due to reduced viral recovery from anterior nares.
Table 1: Comparative Sensitivity of Anterior/Oral-Nasal vs. Nasopharyngeal Swabs for Influenza Detection
| Study Population | Sampling Method | Reference Standard | Sensitivity (95% CI) | Specificity (95% CI) | Citation |
|---|---|---|---|---|---|
| Emergency Department patients (n=128) | Self-collected oral-nasal swab | NP swab with multiplex PCR | 67% (49-81%) | 96% (89-99%) | [12] |
| Pediatric patients (n=59) | Anterior nasal swab with BioFire RP2.1 | NP swab with Xpert fourplex | 100%* | 100%* | [9] |
| Older adults in clinic (n=19 influenza positive) | Self-collected nasal swab | HCW-collected NP swab | 78% (40-97%) | 100% (97-100%) | [20] |
*Limited sample size with perfect concordance for influenza A detection in this subset
Viral Load Correlations with Cycle Threshold Values
Cycle threshold values serve as inverse proxies for viral load, with lower Ct values indicating higher viral concentrations. The relationship between sampling method and Ct values directly impacts detection sensitivity.
Table 2: Viral Load Characteristics Across Sampling Methods and Patient Populations
| Study Focus | Key Viral Load Finding | Clinical Correlation | Citation |
|---|---|---|---|
| SARS-CoV-2 viral load comparison | Significantly lower viral loads in anterior nasal samples (median 1,792 copies/mL) vs. nasopharyngeal (median 53,560 copies/mL) | Anterior nasal PCR-positive rate 84.4% vs. NP reference | [11] |
| Influenza A (H3N2) viral load by age | Lower Ct values (higher viral loads) in infants, children, and elderly | Extreme age groups show increased viral loads | [60] |
| Influenza viral load in hospitalized patients | No significant association between viral load and severe outcomes | High viral load associated with abnormal chest X-ray findings only | [61] |
| SARS-CoV-2 rapid antigen test performance | Sensitivity increased to 63% when excluding high Ct values (>30) | Lower viral loads correspond to reduced detection sensitivity | [62] |
Experimental Protocols and Methodologies
Key Study Designs for Method Comparison
Emergency Department Validation Study
A 2025 validation study conducted at Michael Garron Hospital employed a diagnostic test design comparing self-collected oral-nasal swabs against healthcare worker-collected nasopharyngeal swabs. Consecutive adults presenting with suspected viral upper respiratory tract infections self-collected oral-nasal specimens by swabbing both anterior nares, buccal mucosa, and tongue using disposable flocked swabs. All specimens were stored at 4°C until testing using a laboratory-developed real-time RT-PCR assay detecting influenza A, influenza B, and RSV alongside other respiratory pathogens. RNA extraction utilized the Maxwell HT Viral TNA Kit on the Hamilton Star automated extraction instrument, with amplification on the CFX96 Touch Real-Time PCR detection system. Positive specimens were defined with Ct values below 37, and performance characteristics were calculated using NP swabs as reference standard [12].
Pediatric Sampling Comparison Study
A 2025 study at Helsinki Children's Hospital compared nasopharyngeal, anterior nasal, and saliva samples in pediatric patients with respiratory symptoms. Participants provided all three sample types during emergency department visits. Nasopharyngeal samples were collected by nurses through one nostril, anterior nasal samples were collected by rotating a nylon-flocked dry swab in both nostrils, and saliva samples were collected either by spitting into containers or using polyester swabs on buccal mucosa. All samples were transported in Universal Transport Medium and analyzed using the BioFire Respiratory Panel 2.1 plus test. Tolerance was assessed using a 5-point scale, and feasibility was evaluated by sample adequacy [9].
Multi-Cohort Influenza Viral Load Analysis
A 2024 prospective study analyzed viral loads in 1,047 influenza A (H3N2) patients across sentinel, non-sentinel, and hospitalized settings in Spain. Nasopharyngeal swabs were analyzed by quantitative RT-PCR specific for influenza A (H3N2) using the CDC Influenza Virus Real-Time RT-PCR Panel. RNA extraction used the Nextractor NX-48S automated extractor with Savygen S Respiratory Extraction Kit reagents. Statistical analysis employed both classical age-group comparisons and cubic spline models using generalized additive models to examine non-linear relationships between age, care setting, and Ct values [60].
Experimental Workflow for Sampling Method Validation
The following diagram illustrates the typical workflow for comparative studies of influenza detection methods:
Comparative Study Workflow for Influenza Detection Methods
Mechanistic Insights: Viral Load Dynamics and Detection Sensitivity
Biological Basis for Suboptimal Anterior Nasal Sensitivity
The reduced sensitivity of anterior nasal swabs for influenza detection stems from fundamental viral replication dynamics within the respiratory tract. Influenza viruses exhibit tropism for specific respiratory epithelia, with nasopharyngeal regions providing optimal environments for viral replication compared to anterior nasal passages. This anatomical distribution results in consistently higher viral loads in nasopharyngeal specimens, which directly translates to lower Ct values in molecular assays [60] [11]. During early infection, viral concentrations may be sufficient for detection in both sites, but as infection progresses or viral loads decrease, anterior nasal samples more frequently fall below detection thresholds.
Mathematical modeling of influenza viral dynamics reveals that strains with smaller basic reproduction numbers and shorter generation times exhibit slower growth rates, potentially affecting their distribution across respiratory sites [63]. These growth characteristics influence the timing of peak viral load and the duration of detectability in different anatomical regions. The correlation between viral load and successful detection is particularly pronounced in antigen tests, which typically require higher viral concentrations than molecular methods [62].
Impact of Patient Factors on Viral Load and Detection
Patient-specific factors significantly influence viral load and consequently affect detection sensitivity across sampling methods:
- Age: Infants, young children, and elderly patients demonstrate significantly lower Ct values (higher viral loads) across respiratory sampling sites [60]
- Symptom Duration: Viral loads typically peak early in symptom onset, with detection sensitivity decreasing over time
- Vaccination Status: Unvaccinated individuals exhibit higher viral loads (Ct 25.17 ± 5.55) compared to vaccinated patients (Ct 27.58 ± 4.97) [61]
- Clinical Setting: Outpatients often show higher viral loads than hospitalized patients, possibly due to timing of testing relative to symptom onset [60]
Research Reagent Solutions for Influenza Detection Studies
Table 3: Essential Research Reagents and Materials for Influenza Detection Studies
| Reagent/Material | Manufacturer/Example | Function in Protocol | Key Characteristics |
|---|---|---|---|
| Flocked Swabs | Copan FLOQSwabs | Sample collection from nasal/nasopharyngeal sites | Optimized cellular recovery and specimen release |
| Universal Transport Media | Copan UTM | Preservation of viral integrity during transport | Maintains viral stability without freezing |
| RNA Extraction Kit | Maxwell HT Viral TNA Kit | Nucleic acid purification from clinical specimens | High-quality RNA recovery for sensitive detection |
| PCR Master Mix | Luna Universal Probe One-Step RT-qPCR Kit | Amplification of viral targets | Sensitive detection with minimal inhibition |
| Respiratory Panel Assays | BioFire Respiratory Panel 2.1 plus | Multiplex detection of respiratory pathogens | Comprehensive pathogen identification |
| Real-time PCR System | Bio-Rad CFX96 Touch | Nucleic acid amplification and detection | Precise Ct value determination |
The correlation between cycle threshold values, viral loads, and influenza detection sensitivity in anterior nasal samples has significant implications for respiratory virus surveillance and diagnostic development. While anterior nasal sampling offers practical advantages for widespread testing implementation, the consistently lower sensitivity for influenza detection must be accounted for in diagnostic algorithms and public health strategies. Researchers developing novel influenza detection platforms should prioritize methods that enhance viral recovery from anterior nasal sites or improve analytical sensitivity to compensate for lower viral loads. The strategic selection of reagents and methodologies detailed in this guide provides a foundation for advancing anterior nasal sampling as a viable alternative to nasopharyngeal collection, particularly in settings where accessibility and patient tolerance outweigh modest reductions in clinical sensitivity.
The accurate detection of respiratory pathogens like influenza and SARS-CoV-2 relies heavily on the quality of the specimen collected. While nasopharyngeal swabs (NPS) have long been considered the gold standard, their collection requires trained healthcare professionals and is often uncomfortable for patients, limiting widespread use. In response, two prominent alternatives have emerged: the anterior nasal swab and the oral-nasal combined swab. The anterior nasal swab is collected from the front part of the nostril, while the oral-nasal technique involves swabbing both anterior nares along with the tongue and buccal mucosa. This guide objectively compares the performance of these two sampling approaches for detecting major respiratory viruses, providing researchers and clinicians with evidence-based data to inform diagnostic protocols.
Table 1: Key Characteristics of Sampling Approaches
| Feature | Anterior Nasal Swab | Oral-Nasal Combined Swab |
|---|---|---|
| Collection Site | Front portion of the nostrils (approximately 1-2 cm depth) | Anterior nares, tongue, and buccal mucosa |
| Collection Method | Can be self-collected or professionally collected | Designed for self-collection |
| Primary Use Cases | Rapid Antigen Tests (RATs), PCR testing | Multiplex PCR panels for respiratory viruses |
| Patient Comfort | Generally well-tolerated with minimal discomfort [11] | Feasible and avoids need for healthcare professional [12] |
Experimental Protocols and Key Findings
Performance in Influenza Detection
A 2025 diagnostic validation study provides a direct comparison of a self-collected oral-nasal swab against a provider-collected NPS for detecting Influenza and RSV. The study enrolled symptomatic individuals presenting to an emergency department. Participants self-collected an oral-nasal swab by swabbing both anterior nares, the buccal mucosa, and the tongue. Both the oral-nasal swab and the provider-collected NPS were tested using a multiplex respiratory virus PCR assay [12].
The results demonstrated that for influenza virus detection, the oral-nasal swab had a sensitivity of 67% (95% CI: 49-81%) and a specificity of 96% (95% CI: 89-99%) when compared to the NPS reference standard [12]. This suboptimal sensitivity led the authors to conclude that it is not an acceptable substitute for a healthcare provider-collected NPS for influenza.
In contrast, a earlier study comparing paired nasal and nasopharyngeal swabs from adults with acute respiratory illness found that nasal swabs tested by rRT-PCR had a sensitivity of 89% compared to a composite gold standard. The sensitivity of the NPS in the same study was 94%, and the difference was not statistically significant [1]. This suggests that a standard anterior nasal swab performs robustly for influenza detection when paired with a highly sensitive molecular test.
Performance in SARS-CoV-2 Detection
Extensive research during the COVID-19 pandemic evaluated various sampling methods for SARS-CoV-2. A large cross-sectional study comparing self-tests found that a nasal Ag-RDT had an overall sensitivity of 68.9% against molecular testing. This sensitivity increased to 83.9% when the analysis used a high viral load as a proxy for infectiousness. The performance was even better in symptomatic individuals, with a sensitivity of 78.5% [64].
Another study on SARS-CoV-2 antigen test performance using anterior nasal samples reported a sensitivity of 72.5% compared to RT-PCR. The study also confirmed that anterior nasal collection was significantly less painful and induced fewer coughs or sneezes than nasopharyngeal collection [11]. A third study confirmed that self-collected anterior nasal swabs were as sensitive as professionally collected nasopharyngeal swabs for rapid antigen testing when the viral load was high (Ct values up to 30) [65].
For the oral-nasal combined technique, one study assessed it specifically for SARS-CoV-2 and found it had comparable accuracy to a healthcare provider-collected NPS [12]. However, direct head-to-head comparisons of anterior nasal and oral-nasal swabs for SARS-CoV-2 are limited in the available literature.
Table 2: Summary of Diagnostic Performance by Virus and Swab Type
| Virus | Swab Type | Sensitivity (%) | Specificity (%) | Reference Standard |
|---|---|---|---|---|
| Influenza | Oral-Nasal (Self) | 67.0 (49.0 - 81.0) | 96.0 (89.0 - 99.0) | NP Swab (Provider) [12] |
| Influenza | Anterior Nasal | 89.0 (78.0 - 99.0) | Not Reported | Composite Gold Standard [1] |
| RSV | Oral-Nasal (Self) | 75.0 (43.0 - 95.0) | 99.0 (93.0 - 100.0) | NP Swab (Provider) [12] |
| SARS-CoV-2 | Anterior Nasal (Ag-RDT) | 72.5 (58.3 - 84.1) | 100.0 (99.3 - 100.0) | NP Swab RT-PCR [11] |
| SARS-CoV-2 | Anterior Nasal (Self Ag-RDT) | 68.9 (61.6 - 75.6) | > 99.0 | Molecular Testing [64] |
Analysis of Workflow and Viral Dynamics
The choice of sampling method involves trade-offs between diagnostic accuracy, patient comfort, and procedural complexity. The following diagram illustrates the typical workflow and key decision points for validating a novel swab type against established standards.
Viral load dynamics differ significantly between sampling sites, which directly impacts detection sensitivity. Research confirms that nasopharyngeal samples generally yield the highest viral concentrations [24]. One study found that viral loads in anterior nasal samples were significantly lower than in NPS, though sufficiently and vigorously rubbed nasal swabs could achieve SARS-CoV-2 concentrations similar to NPS [24]. The oral-nasal method leverages the fact that some viruses, like RSV, may be detectable in both the nasopharynx and oropharynx, potentially compensating for lower viral loads in a single site [12].
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and materials used in the cited studies for the detection of respiratory viruses from anterior nasal and oral-nasal swabs.
Table 3: Key Research Reagent Solutions for Respiratory Virus Detection
| Reagent / Material | Function / Application | Specific Examples from Literature |
|---|---|---|
| Universal Transport Media (UTM) | Preserves viral integrity during transport and storage. | Copan UTM [12] [11] |
| RNA Extraction Kit | Isolates viral RNA for downstream molecular analysis. | Maxwell HT Viral TNA Kit (Promega) [12], QIAamp Viral RNA Mini Kit (Qiagen) [24] |
| One-Step RT-qPCR Kit | Enables reverse transcription and PCR amplification in a single reaction. | Luna Universal Probe One-Step RT-qPCR Kit (New England Biolabs) [12], QuantiTect Probe RT-PCR Kit (QIAGEN) [11] |
| Multiplex PCR Assay | Simultaneously detects multiple respiratory pathogen targets. | Laboratory-developed RT-PCR assay for Influenza A/B, RSV, SARS-CoV-2 [12], Allplex Respiratory Panels & SARS-CoV-2 Assay (Seegene) [24] |
| Flocked Swabs | Swabs with perpendicular fibers for superior specimen collection and release. | FLOQSwabs (Copan) [12] [11], NP-type and OP-type flocked swabs [24] |
Concluding Comparison
The choice between anterior nasal and oral-nasal sampling approaches depends on the specific diagnostic goals, the target pathogen, and the context of use.
For Influenza Detection: Standard anterior nasal swabs demonstrate superior and more consistent sensitivity (around 89%) [1] compared to oral-nasal combined swabs (67%) [12] when analyzed by RT-PCR. The oral-nasal method is not recommended as a substitute for NPS for influenza due to its suboptimal test characteristics.
For SARS-CoV-2 Detection: Anterior nasal swabs are a well-validated and reliable method, especially for rapid antigen testing, with sensitivities often exceeding 70% and reaching over 90% in symptomatic, infectious individuals [11] [64]. Data for the oral-nasal combined technique for SARS-CoV-2 is more limited but suggests it may be a feasible alternative [12].
For RSV Detection: The oral-nasal swab shows more promising performance for RSV, with a sensitivity of 75% and high specificity (99%) [12], possibly because RSV shedding occurs effectively in both the nasopharynx and oropharynx.
In summary, the anterior nasal swab remains the dominant alternative to NPS for most applications, particularly for influenza and SARS-CoV-2 Ag-RDTs, due to its balance of good sensitivity, high patient tolerability, and ease of self-collection. The oral-nasal combined swab may find a niche in specific multiplex PCR panels, particularly for viruses like RSV, but requires further validation before widespread adoption.
The validation of anterior nasal swabs for influenza detection represents a critical advancement in respiratory virus diagnostics, addressing key limitations of the traditional nasopharyngeal (NP) swab. While NP sampling remains the benchmark for sensitivity, its requirement for trained healthcare professionals, patient discomfort, and limited scalability for mass testing have driven the search for less invasive, user-friendly alternatives [9] [66]. The anterior nares (AN) collection method has gained significant traction during the COVID-19 pandemic, demonstrating feasibility for self-collection and potential for decentralized testing [67] [66]. Within the broader thesis of validating anterior nasal swabs for influenza research, this guide objectively compares the technical performance of anterior nasal swabs against nasopharyngeal and other alternative sampling methods, focusing on swab design, collection depth optimization, and procedural refinements that impact diagnostic accuracy for influenza and other respiratory viruses.
Performance Comparison: Anterior Nasal vs. Alternative Sampling Methods
Extensive clinical studies have directly compared the diagnostic performance of anterior nasal swabs against established methods like nasopharyngeal swabs. The results, summarized in the table below, reveal context-dependent performance characteristics influenced by pathogen type, test modality, and patient population.
Table 1: Diagnostic Performance of Anterior Nasal Swabs vs. Nasopharyngeal Swabs
| Virus Target | Test Method | Population | Sensitivity (AN vs. NP) | Specificity (AN vs. NP) | Key Study Findings | Citation |
|---|---|---|---|---|---|---|
| SARS-CoV-2 | Antigen Test (Sure-Status) | Mixed (Community) | 85.6% vs. 83.9% | 99.2% vs. 98.8% | Equivalent diagnostic accuracy; high agreement (κ=0.918) | [67] |
| SARS-CoV-2 | Antigen Test (Biocredit) | Mixed (Community) | 79.5% vs. 81.2% | 100% vs. 99.0% | Equivalent diagnostic accuracy; high agreement (κ=0.833) | [67] |
| SARS-CoV-2 | Antigen Test (QuickNavi) | Symptomatic | 72.5% | 100% | Significantly less painful, fewer coughs/sneezes vs. NP | [11] |
| Influenza A/B | PCR (Oral-Nasal Swab) | Symptomatic Adults | 67% (Combined) | 96% (Combined) | Suboptimal substitute for NP swab for multiplex testing | [12] |
| RSV | PCR (Oral-Nasal Swab) | Symptomatic Adults | 75% | 99% | Performance more preserved than for Influenza | [12] |
| Multiple Respiratory Viruses | PCR (QIAstat-Dx) | Pediatric Inpatients | 95.7% (within 24h of NP) | N/R | High concordance (77.5%); sensitivity varies by virus type | [6] |
The data indicates that for SARS-CoV-2, particularly with antigen testing, anterior nasal swabs can achieve diagnostic accuracy equivalent to nasopharyngeal swabs in community settings [67]. However, for influenza detection, the performance is more variable. A study on self-collected oral-nasal swabs (swabbing anterior nares, buccal mucosa, and tongue) found a combined sensitivity of only 67% for influenza compared to provider-collected NP swabs, suggesting it is not an optimal substitute for influenza in multiplex testing [12]. Conversely, a pediatric study using anterior nasal swabs showed high overall sensitivity for a panel of respiratory viruses, with sensitivity highest (95.7%) when the anterior nasal swab was collected within 24 hours of the NP swab [6]. This suggests that timing and specific collection methodology are critical factors.
Experimental Protocols for Method Comparison
To ensure valid and reproducible comparisons between sampling methods, researchers must adhere to standardized experimental protocols. The following methodologies are derived from cited clinical studies.
Protocol 1: Paired Swab Design and Tolerability Study
This protocol is designed for head-to-head comparison of different swab types and collection depths.
- Objective: To compare the diagnostic accuracy and patient tolerability of anterior nasal versus nasopharyngeal swabs for influenza and other respiratory viruses.
- Study Population: Symptomatic individuals presenting to emergency departments or clinics with symptoms of upper respiratory tract infection [9] [12]. Pediatric studies focus on hospitalized children with clinical indications for testing [6].
- Sample Collection:
- Nasopharyngeal (NP) Swab: A trained healthcare professional inserts a nylon-flocked swab through one nostril to the nasopharynx until resistance is met. The swab is rotated and held for several seconds to absorb secretions [9] [68]. The depth is often guided by the distance from the nose to the ear [68].
- Anterior Nasal (AN) Swab: A nylon-flocked swab is inserted approximately 2 cm into one nostril (or both), rotated five times, and held for 5 seconds against the nasal mucosa [11]. For oral-nasal samples, the same swab is used to sample the anterior nares, buccal mucosa, and tongue [12].
- Sample Processing: All swabs are placed in Universal Transport Medium (UTM) [9] [12]. Samples are typically stored at +4°C for short periods or at -70°C for longer storage until batch testing.
- Virus Detection: RNA extraction is performed using automated systems (e.g., Hamilton Star with Maxwell HT Viral TNA Kit). Detection is performed using reverse transcription quantitative PCR (RT-qPCR) with laboratory-developed tests or commercial multiplex panels (e.g., BioFire Respiratory Panel 2.1 plus, QIAstat-Dx Respiratory SARS-CoV-2 Panel) that include influenza targets [9] [12] [6].
- Tolerability Assessment: Patients or guardians evaluate discomfort on a 5-point scale (1=pleasant, 5=unpleasant). Cough or sneeze induction is also recorded [9] [11].
Protocol 2: Viral Load Correlation Analysis
This protocol investigates the relationship between viral load and test sensitivity across different sampling sites.
- Objective: To quantify and compare SARS-CoV-2 viral loads obtained from nasopharyngeal and anterior nasal sampling sites using different swab types [11].
- Sample Collection: In participants with confirmed SARS-CoV-2, multiple samples are collected:
- One nasopharyngeal sample (NPS) with an NP-type flocked swab.
- Two anterior nasal samples from each nostril: one with an NP-type swab (AWN) and one with an oropharyngeal (OP)-type swab (AWO) [11].
- Quantitative Analysis: RNA is extracted from UTM samples. Viral loads are quantified using a quantitative RT-PCR (qRT-PCR) assay on a platform like a LightCycler 96 System, using a standard curve for absolute quantification [11].
- Statistical Comparison: Viral loads between sample types (NPS, AWN, AWO) are compared using non-parametric tests like the Wilcoxon signed-rank test to account for non-normal distribution of data [11].
The logical workflow for these validation studies is outlined below.
The Scientist's Toolkit: Key Research Reagent Solutions
Successful research in swab optimization and viral detection relies on a standardized set of high-quality reagents and materials. The table below details essential components used in the cited studies.
Table 2: Essential Research Reagents and Materials for Swab Validation Studies
| Item | Specific Examples | Function in Experiment | Critical Features |
|---|---|---|---|
| Flocked Swabs | Copan FLOQSwabs (NP-type, OP-type) [9] [11] | Sample collection from nasal/oropharyngeal sites | Nylon fibers for superior cellular absorption and elution [68] |
| Transport Medium | Copan UTM (Universal Transport Medium) [9] [12] | Preserves viral integrity during transport/storage | Compatible with both PCR and viral culture |
| RNA Extraction Kit | Maxwell HT Viral TNA Kit (Promega) [12] | Nucleic acid purification from clinical samples | Automated compatibility, high yield and purity |
| PCR Master Mix | Luna Universal Probe One-Step RT-qPCR Kit (New England Biolabs) [12] | Amplification and detection of viral RNA | All-in-one formulation for reverse transcription and qPCR |
| Multiplex PCR Panel | BioFire Respiratory Panel 2.1 plus (BioMerieux) [9] | Simultaneous detection of multiple pathogens | Comprehensive pathogen coverage in a single test |
| qPCR Instrument | CFX96 Touch (BioRad), LightCycler 96 (Roche) [12] [11] | Quantitative detection of amplified nucleic acids | High-throughput, precise thermal cycling, sensitive detection |
Discussion: Implications for Influenza Research and Public Health
The technical refinements in swab design and collection protocols are not merely procedural; they have profound implications for the efficiency, scalability, and patient-centricity of influenza research and public health surveillance. The demonstrated feasibility of self-collected anterior nasal samples can significantly expand testing capacity beyond clinical settings, enabling large-scale community-based studies and surveillance programs [6] [66]. This is particularly valuable for capturing asymptomatic or pre-symptomatic cases that are crucial for understanding transmission dynamics.
The evolution of lateral flow test (LFT) engineering, heavily accelerated by the COVID-19 pandemic, offers a promising pathway for decentralized influenza diagnosis [66]. The integration of novel bioengineering approaches—such as ultra-sensitive nanomaterials, CRISPR-based detection, and machine learning for result interpretation—is poised to address the primary limitation of LFTs: lower sensitivity compared to PCR [69] [66]. Future research should focus on optimizing these technologies specifically for influenza viruses detected in anterior nasal specimens.
Finally, the superior tolerability of anterior nasal sampling is a critical factor for pediatric populations and for repeated testing scenarios required in longitudinal studies or during seasonal epidemics [9] [11]. Improved patient compliance can lead to more reliable enrollment in clinical trials and more accurate data on influenza incidence and viral shedding patterns. As the diagnostic landscape evolves, the validation of anterior nasal swabs will remain a cornerstone of efforts to create more accessible, scalable, and patient-friendly respiratory virus diagnostics.
The accurate detection of influenza virus is a cornerstone of effective clinical management and public health surveillance. While nasopharyngeal swabs (NPS) have traditionally been considered the gold standard for respiratory virus testing, their collection is invasive, requires trained healthcare personnel, and can cause significant patient discomfort [17]. Anterior nasal swabs (ANS) have emerged as a less invasive, more tolerable alternative suitable for self-collection. However, the diagnostic performance of ANS must be evaluated within the context of population-specific factors that influence viral shedding patterns. This review synthesizes evidence on how age, symptom duration, and viral shedding characteristics affect the performance of anterior nasal swabs for influenza detection, providing researchers and clinicians with a evidence-based framework for optimizing testing strategies across diverse populations.
Comparative Performance of Nasal Sampling Methods
Viral Load Recovery Across Swab Types
The recovery of influenza virus from different upper respiratory tract sampling sites varies significantly, with implications for diagnostic sensitivity. A 2024 subanalysis of the CENTERSTONE phase 3 study directly compared viral loads between matched midturbinate swabs (MTS) and NPS samples from 104 influenza-positive patients [17].
Table 1: Comparison of Influenza Viral Load Between Swab Types
| Parameter | Nasopharyngeal Swab (NPS) | Midturbinate Swab (MTS) | Difference |
|---|---|---|---|
| Median Viral Load | 6.37 log10 vp/mL (2.3 million vp/mL) | 6.04 log10 vp/mL (1.1 million vp/mL) | 53% lower in MTS |
| Positive Result Rate | 95% | 92% | 3% absolute difference |
| Samples Above Sequencing Threshold | 86.5% | 78.8% | 7.7% absolute difference |
| Statistical Significance | p = 0.0002 (paired analysis) |
This study found that MTS yielded a significantly lower viral load (53% lower based on median values) compared to NPS, with similar magnitude differences observed for both influenza A and B viruses [17]. The difference remained consistent across age groups (0.28 log10 units for adults ≥18 years; 0.44 log10 units for children <18 years), though it was only statistically significant in adults, possibly due to smaller sample size in the pediatric subgroup [17].
ANS Versus Combined Throat and Nasal Swabs
A 2023 prospective study evaluating a novel ANS design in children aged 5-18 years demonstrated high agreement with the combined throat and anterior nasal (CTN) swab reference standard [45]. The ANS showed a positive percentage agreement of 96.2% (95% CI: 91.8-98.3%) and negative percentage agreement of 99.8% (95% CI: 99.6-99.8%) for detection of respiratory viruses [45]. Importantly, cycle threshold (Ct) values between ANS and CTN swabs showed a strong positive linear association, with a median Ct value difference of only 0.9 lower with ANS (95% CI: 0.3-1.5), indicating comparable viral recovery [45].
Age-Specific Considerations
Age-Related Variations in Influenza Presentation and Detection
Age significantly influences influenza susceptibility, clinical presentation, and potentially viral detection. A 2025 prospective study from Serbia found that the mean age of participants with laboratory-confirmed influenza was significantly lower than those without influenza (37.90 vs. 54.92 years in 2022/23, and 40.21 vs. 54.17 years in 2023/24; p < 0.0001) [70]. This age distribution pattern suggests differential exposure or susceptibility across age groups that could impact testing strategies.
Table 2: Age-Specific Performance of Self-Collected Nasal Swabs
| Age Group | Self-Collection Feasibility | Sensitivity/Specificity | Key Considerations |
|---|---|---|---|
| Older Adults (>65 years) | 99% acceptability; 92% adequate samples [20] | 78% sensitivity vs. NP swab; 100% specificity [20] | Reduced mobility and cognitive function may require simplified protocols |
| Children (5-18 years) | 84% preferred ANS over CTN; 90% found ANS "extremely comfortable" or "a little uncomfortable" [45] | 96.2% positive agreement with CTN [45] | Age-appropriate swab sizes and designs improve compliance |
| General Adult Population | High feasibility for self-collection in community settings [71] [20] | Comparable detection to HCW-collected nasal swabs [20] | Clear instructions and video demonstrations enhance proper technique |
While the CENTERSTONE study found no significant difference in viral load between swab types based on age subgroups, the point estimate for the difference was larger in children (<18 years: -0.44 log10 vp/mL) compared to adults (≥18 years: -0.28 log10 vp/mL) [17]. This trend warrants further investigation with larger pediatric samples.
Special Considerations for Older Adults
Self-collection of nasal swabs by older adults demonstrates high acceptability but potentially reduced sensitivity. A study in Thailand among adults >65 years found 99% acceptability of self-collected nasal swabs, with 92% of community-collected samples deemed adequate based on human cellular content [20]. However, the sensitivity of self-collected nasal swabs compared to healthcare worker-collected nasopharyngeal swabs was 78% (95% CI: 40-97%), while specificity remained high at 100% (95% CI: 97-100%) [20]. This suggests that while older adults can reliably perform self-collection, the anterior nares may harbor lower viral concentrations compared to the nasopharynx in this population.
Symptom Duration and Viral Detection
The timing of sample collection relative to symptom onset critically influences detection sensitivity across all sampling methods. Influenza viral shedding typically peaks within the first few days of symptom onset, creating a narrow window for optimal detection [20]. Both the community and clinic studies in Thailand emphasized collection within 72 hours of symptom onset to maximize detection probability [20].
A 2025 study on diagnostic significance of influenza symptoms found that the predictive values of symptoms varied substantially between influenza seasons [70]. In the 2022/23 season, positive predictive values (PPVs) were highest for fever (34.93%), chills (31.95%), myalgia (30.30%), and malaise (28.57%), but dropped significantly in 2023/24 for all observed symptoms and signs (ranging from 1.91% to 9.17%) [70]. This temporal variability underscores the challenge of relying solely on clinical symptoms for triggering testing and supports the need for standardized testing protocols that account for seasonal variations in viral presentation.
Viral Shedding Patterns and Implications for Detection
Asymptomatic and Presymptomatic Shedding
The performance of anterior nasal swabs must be considered across the spectrum of infection, including asymptomatic and presymptomatic phases. A household transmission study of SARS-CoV-2 demonstrated that saliva specimens identified a higher proportion of infections (81.9%) compared to anterior nasal swabs (77.1%) when using inactivating transport media, with differences more pronounced in asymptomatic participants [71]. This suggests that optimal specimen type may vary by clinical presentation, with ANS potentially having reduced sensitivity in asymptomatic individuals.
Figure 1: Decision Framework for Swab Selection Based on Patient Presentation. This workflow illustrates how patient factors should guide selection of sampling method to optimize detection sensitivity while considering practical constraints.
Influenza Type and Subtype Variations
While data specifically comparing ANS performance across influenza types and subtypes remains limited, the CENTERSTONE study found that differences in viral load between MTS and NPS were of similar magnitude for both influenza A (difference of 0.27 log10 vp/mL, p=0.0083) and influenza B (difference of 0.31 log10 vp/mL, p=0.0079) [17]. Within influenza A viruses, both H1N1 and H3N2 subtypes behaved similarly in terms of viral load differences between swab types [17]. This consistent pattern across influenza types supports the generalizability of ANS performance across seasonal influenza viruses.
Experimental Protocols and Methodologies
Standardized Swab Collection Procedures
The comparative studies reviewed employed rigorous, standardized methodologies for swab collection and processing:
Nasopharyngeal Swab Collection: In the CENTERSTONE study, NPS samples were collected using minitip nylon flocked swabs (Copan FLOQSwabs 501CS01) inserted into the nostril to reach the nasopharynx [17]. Swabs were placed in universal transport medium (Copan UTM 330C) and stored refrigerated before shipment to a central laboratory within 36 hours of collection [17].
Midturbinate/Turbinate Swab Collection: MTS samples were collected using adult midturbinate nylon flocked swabs (Copan FLOQSwabs 56380CS01) from the contralateral nostril immediately following NPS collection [17]. The same storage and transport conditions applied.
Anterior Nasal Swab Collection: The pediatric ANS study utilized a novel flocked anterior nasal swab (Rhinoswab Junior) designed specifically for children, available in three sizes based on age [45]. The swab was inserted for 60 seconds followed by side-to-side movements for 15 seconds in the anterior nasal area [45]. No transport medium was used, with swabs instead placed directly into sterile closed containers [45].
Laboratory Processing and Detection Methods
Centralized laboratory testing standardized viral detection across studies:
RNA Extraction and PCR: The CENTERSTONE study used the MagNA Pure 96 system (Roche) for viral RNA purification and a proprietary influenza matrix gene quantitative RT-PCR assay with lower limits of quantitation of 2.79 log10 vp/mL for influenza A and 2.63 log10 vp/mL for influenza B [17].
Multiplex PCR Panels: The pediatric ANS study employed the AusDiagnostics Respiratory Pathogens 16-well assay on the AusDiagnostics High-Plex 24 system, extracting samples on the Roche MagNA Pure 96 system using MagNA Pure 96 DNA and Viral NA Small Volume Kit [45]. Samples with Ct values <38.73 were considered positive for non-SARS-CoV-2 viruses [45].
Research Reagent Solutions
Table 3: Essential Research Materials for ANS Validation Studies
| Reagent/Equipment | Specification/Model | Research Application |
|---|---|---|
| Flocked Swabs | Copan FLOQSwabs 56380CS01 (MTS) [17] | Standardized sample collection from turbinate region |
| Transport Media | Copan UTM 330C [17] | Viral preservation during transport and storage |
| RNA Extraction System | MagNA Pure 96 system (Roche) [17] [45] | Automated nucleic acid purification for consistency |
| PCR Platforms | AusDiagnostics High-Plex 24 system [45]; StepOnePlus/QuantStudio systems (ABI) [71] | Multiplex respiratory pathogen detection |
| Human Cell Control Assay | Ribonuclease P (Rnase P) RT-PCR [20] | Sample adequacy assessment via human cellular content |
| Viral Transport Medium | Primestore (Longhorn Vaccines & Diagnostics) [71] | Room temperature viral inactivation and storage |
Anterior nasal swabs represent a viable alternative to nasopharyngeal swabs for influenza detection, particularly when considering patient comfort, feasibility of self-collection, and resource constraints. However, their performance is moderated by important population-specific factors. Age influences both technical performance and practical implementation, with children showing strong preference for ANS and older adults demonstrating high acceptability but potentially reduced sensitivity with self-collection. Symptom duration remains a critical factor across all populations, with early collection post-symptom onset maximizing detection regardless of sampling method. Viral shedding patterns, including differences between symptomatic and asymptomatic presentations, further modulate ANS performance. Future research should prioritize large-scale, prospective comparisons of ANS across all age groups and clinical presentations, standardization of self-collection protocols for vulnerable populations, and development of optimized swab designs that maximize patient comfort without compromising specimen quality.
The accurate detection of respiratory viruses like influenza is a cornerstone of public health response and clinical management. For decades, the nasopharyngeal (NP) swab has been the unchallenged gold standard for specimen collection, providing high-quality samples from the posterior nasopharynx. However, the COVID-19 pandemic exposed critical limitations of NP swabs, including supply chain vulnerabilities, requirements for trained healthcare personnel, significant patient discomfort, and infection risks for healthcare workers during collection. These challenges catalyzed a paradigm shift toward less invasive, patient-centric sampling methods, with anterior nasal (AN) swabs emerging as a prominent alternative.
This guide objectively compares the performance of anterior nasal swabs against traditional nasopharyngeal swabs and other alternatives for influenza detection, framing the discussion within the broader thesis of validating AN swabs for respiratory virus research. For researchers and drug development professionals, understanding the quality control measures that ensure adequate sample collection and processing is paramount to generating reliable, reproducible data. The validation of AN swabs extends beyond mere convenience; it represents a critical advancement in scalable surveillance, self-testing capabilities, and pandemic preparedness, enabling earlier detection through more acceptable and accessible sampling methods that can be deployed at the first sign of symptoms.
Performance Comparison: Anterior Nasal versus Alternative Collection Methods
Extensive research has compared the diagnostic performance of anterior nasal swabs against established collection methods for respiratory pathogens. The evidence reveals a complex landscape where performance varies significantly based on the target pathogen, testing methodology, and collection protocol.
Quantitative Performance Metrics for Influenza Detection
For influenza detection specifically, recent studies demonstrate that self-collected anterior nasal and oral-nasal swabs show promise but may have reduced sensitivity compared to healthcare provider-collected nasopharyngeal swabs.
Table 1: Performance Metrics of Anterior Nasal vs. Nasopharyngeal Swabs for Influenza Detection
| Collection Method | Target Pathogen | Sensitivity (%) | Specificity (%) | Agreement (Kappa) | Study Context |
|---|---|---|---|---|---|
| Self-collected oral-nasal swab [12] | Influenza A/B | 67.0 (95% CI: 49.0–81.0) | 96.0 (95% CI: 89.0–99.0) | 0.68 (95% CI: 0.52–0.80) | Emergency department patients with suspected URI |
| Home-collected nasal swab [72] | Influenza A/H3N2 | 78.0–86.0 | 88.0 | 0.70 | Community-based cohort with ARI |
| Home-collected nasal swab [72] | Influenza A/H1N1 | 78.0–86.0 | 96.0–100.0 | 0.87 | Community-based cohort with ARI |
| Home-collected nasal swab [72] | Influenza B/Victoria | 78.0–86.0 | 96.0–100.0 | 0.86 | Community-based cohort with ARI |
| Home-collected nasal swab [72] | Influenza B/Yamagata | 78.0–86.0 | 96.0–100.0 | 0.69 | Community-based cohort with ARI |
| Provider-collected nasopharyngeal swab (reference) [12] | Influenza A/B | 100.0 (by definition) | 100.0 (by definition) | 1.00 | Emergency department setting |
The performance differential observed in Table 1 can be partially explained by viral load differences across anatomical sites. A comparative analysis of SARS-CoV-2 viral loads, which provides insights into respiratory virus distribution, found that nasopharyngeal swabs yielded significantly higher viral concentrations (median 53,560 copies/mL) compared to anterior nasal swabs (median 1,792–6,369 copies/mL) [11]. This gradient in viral recovery directly impacts detection sensitivity, particularly in molecular assays where limit of detection is critical.
Comparative Performance Across Respiratory Viruses
The performance characteristics of anterior nasal swabs vary not only by collection method but also by target pathogen, reflecting differences in viral tropism and replication sites.
Table 2: Performance Comparison Across Multiple Respiratory Viruses
| Collection Method | Target Pathogen | Sensitivity (%) | Specificity (%) | Reference Standard |
|---|---|---|---|---|
| Self-collected oral-nasal swab [12] | RSV | 75.0 (95% CI: 43.0–95.0) | 99.0 (95% CI: 93.0–100.0) | NP swab |
| Anterior nares swab (RT-PCR) [42] | SARS-CoV-2 | 84.0 (95% CI: 68.0–94.0) | N/R | NP swab RT-PCR |
| Anterior nares swab (antigen test) [42] | SARS-CoV-2 | 91.0 (against viral culture) | N/R | Viral culture |
| Tongue swab (RT-PCR) [42] | SARS-CoV-2 | 18.0–81.0 (against viral culture) | N/R | Viral culture |
| Anterior nasal swab (antigen test) [11] | SARS-CoV-2 | 72.5 (95% CI: 58.3–84.1) | 100.0 (95% CI: 99.3–100.0) | NP swab RT-PCR |
The variable performance across pathogens underscores the importance of pathogen-specific validation. For instance, the relatively better performance of anterior nasal sampling for RSV compared to influenza (75% vs. 67% sensitivity) [12] may reflect differences in viral tropism and shedding patterns. Similarly, the high sensitivity of anterior nares swabs for SARS-CoV-2 when compared against viral culture as a reference [42] suggests that while AN swabs may miss some PCR-positive cases, they effectively detect culturally viable virus, which may have greater clinical relevance for transmission risk assessment.
Experimental Protocols for Method Validation
Robust validation of anterior nasal swabs requires carefully controlled experimental designs that directly compare performance against established reference standards while controlling for critical variables. The following section outlines key methodological approaches used in recent validation studies.
Paired Specimen Collection and Processing Protocol
The most rigorous approach for validating anterior nasal swabs involves concurrent collection of both the experimental and reference standard specimens from the same participant, as demonstrated in several recent studies:
Participant Recruitment and Eligibility: Studies typically enroll participants presenting with symptoms suggestive of acute respiratory infection (ARI) within a specified duration (typically ≤7 days from symptom onset) [12] [72]. For influenza validation, recruitment often occurs during periods of known influenza circulation to ensure adequate positive cases.
Paired Sample Collection: The fundamental design involves collecting both the experimental swab (AN swab) and the reference standard (NP swab) from the same participant during the same healthcare encounter. In the emergency department-based validation study by [12], participants first underwent healthcare provider-collected NP swabbing followed by self-collection of an oral-nasal swab after appropriate instruction.
Standardized Swabbing Technique: For anterior nasal collection, the validated protocol involves inserting a flocked swab approximately 2 cm into the nasal cavity until resistance is met at the turbinate, rotating the swab 5 times against the nasal mucosa, holding for 5-15 seconds to ensure adequate absorption, and repeating in the second nostril with the same swab [12] [11]. For oral-nasal swabs, the protocol extends to additionally swabbing the tongue and buccal mucosa [12].
Specimen Transport and Storage: Swabs are immediately placed in universal transport media (UTM), stored at 4°C, and processed within a defined timeframe (typically 24-72 hours) to preserve nucleic acid integrity [12] [40]. Consistent temperature control during transport is essential for maintaining sample quality.
Laboratory Processing and Testing: RNA extraction is performed using automated systems (e.g., Hamilton Star with Promega Maxwell HT Viral TNA Kit) [12], followed by reverse transcription quantitative PCR (RT-qPCR) using pathogen-specific primers and probes. Testing both specimen types in the same batch using identical reagents and protocols minimizes inter-assay variability.
Quality Assessment: Incorporation of internal controls (e.g., RNAse P) with defined cycle threshold cutoffs (Ct ≤40) ensures specimen adequacy and nucleic acid quality [72]. Specimens failing internal control thresholds are excluded from analysis.
Analytical Sensitivity and Limit of Detection Studies
Beyond clinical comparison with NP swabs, comprehensive validation includes analytical sensitivity studies to establish the limit of detection (LoD) for anterior nasal swabs:
In Vitro Tissue Models: Innovative approaches using natural cellulose sponges saturated with mucus-mimicking solutions (e.g., polyethylene oxide) create physiologically relevant models for quantifying swab performance [40]. These models allow controlled evaluation of pick-up and release efficiency by gravimetrical analysis and RT-qPCR detection of spiked inactivated virus.
LoD Determination: The 50% and 95% limits of detection are established using probit analysis of serial dilutions of quantified virus or in vitro transcribed RNA [8]. Studies have demonstrated no significant difference in LoD between anterior nasal and nasopharyngeal swabs for SARS-CoV-2 detection [8], though anterior nasal swabs generally show higher Ct values indicating lower viral recovery.
Swab Material Comparisons: Controlled studies compare performance across swab types (flocked, injection-molded, polyester) and manufacturers to identify material-based performance differences [42] [40]. Injection-molded swabs like ClearTip have demonstrated superior virus release properties in benchtop models despite lower absorption capacity [40].
Figure 1: Comprehensive workflow for validating anterior nasal swabs for respiratory virus detection, encompassing study design, specimen collection, laboratory processing, and data analysis phases.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of anterior nasal swab validation requires specific reagents and materials optimized for respiratory specimen collection, processing, and analysis. The selection of appropriate tools directly impacts assay performance and result reliability.
Table 3: Essential Research Reagents and Materials for AN Swab Validation
| Category | Specific Product/Type | Key Characteristics | Application Notes |
|---|---|---|---|
| Collection Swabs | Flocked swabs (e.g., Copan FLOQSwabs) | Short synthetic fibers perpendicular to handle; enhanced specimen release | Superior cellular material and virus release compared to spun fiber [40] |
| Injection-molded swabs (e.g., ClearTip) | Non-absorbent plastic with patterned surface | Efficient release into small volume; manufacturing scalability [40] | |
| Polyester swabs | Traditional spun fiber design | Equivalent performance to flocked swabs for anterior nasal RT-PCR [42] | |
| Transport Media | Universal Transport Media (UTM) | Viral stabilization; antimicrobial agents | Maintains viral RNA integrity during transport and storage [12] [11] |
| Nucleic Acid Extraction | Maxwell HT Viral TNA Kit (Promega) | Magnetic bead-based purification; high-throughput compatibility | Automated extraction on Hamilton Star system [12] |
| QIAamp 96 Virus QIAcube HT kit (Qiagen) | Silica-membrane technology; integrated automation | Used with TaqPath COVID-19 RT-qPCR [8] | |
| Molecular Detection | Luna Universal Probe One-Step RT qPCR Kit (NEB) | All-in-one master mix; room temperature setup | Used with CFX96 Touch Real-Time PCR [12] |
| TaqPath COVID-19 RT-PCR Kit (Thermo Fisher) | Multiplex target detection; EUA authorization | Reference standard for SARS-CoV-2 detection [8] | |
| Quality Control | RNAse P primers/probes | Human nucleic acid extraction control | Ct ≤40 indicates adequate cellular material [72] |
| Inactivated virus standards (BEI Resources) | Quantified viral stock for LoD studies | Serial dilution for limit of detection determination [40] |
The selection of appropriate swab material deserves particular attention. Recent comparative studies have demonstrated that while traditional flocked swabs remain the benchmark for specimen collection, innovative injection-molded swabs show comparable performance with potential advantages in manufacturing scalability and sample elution efficiency [40]. The non-absorbent nature of injection-molded swabs enables concentration of the specimen into smaller volumes, potentially increasing analytical sensitivity despite lower overall specimen uptake.
The comprehensive validation of anterior nasal swabs for influenza detection represents a critical advancement in respiratory pathogen surveillance. While current evidence suggests that self-collected AN swabs may have modestly reduced sensitivity compared to healthcare provider-collected NP swabs—67% for influenza versus 75% for RSV in one emergency department study [12]—their advantages in scalability, patient acceptability, and self-collection capability position them as valuable tools for community-based surveillance and early detection.
The performance characteristics of AN swabs must be interpreted within the specific context of their intended use. For pandemic preparedness and large-scale community surveillance, the ability to deploy widespread testing through self-collection may outweigh modest reductions in sensitivity, particularly when considering that earlier collection during symptomatic onset may compensate through higher viral loads. Additionally, the equivalence of AN swabs to NP swabs for detecting culturable virus [42] suggests they may be optimal for identifying transmissible infection.
Quality control measures spanning standardized collection protocols, appropriate swab selection, validated transport conditions, and robust laboratory methods are fundamental to ensuring reliable performance. As respiratory virus diagnostics continue to evolve, the validation of anterior nasal swabs will remain an active area of research, particularly for emerging pathogens and in the context of multiplexed detection platforms that simultaneously identify influenza, RSV, SARS-CoV-2, and other respiratory viruses.
Clinical Validation and Performance Metrics Against Reference Standards
The accurate detection of influenza virus is a cornerstone of effective respiratory virus management, influencing clinical treatment, infection control, and public health surveillance. For decades, the nasopharyngeal (NP) swab has been the reference standard for specimen collection due to its high sensitivity, as the nasopharynx is a primary site for influenza virus replication [12]. However, NP swab collection is an invasive procedure that can cause patient discomfort, requires trained healthcare personnel, and may complicate large-scale surveillance and self-testing initiatives.
The anterior nasal (AN) swab has emerged as a less invasive, more tolerable, and logistically simpler alternative. Despite these advantages, its adoption in clinical and research settings has been tempered by questions regarding its diagnostic sensitivity relative to the NP swab. This guide objectively compares the performance of anterior nasal and nasopharyngeal swabs for influenza detection, with a particular focus on the context of recent research reporting a sensitivity of approximately 67% for AN swabs [12]. The analysis synthesizes current experimental data, delineates detailed methodologies from key studies, and provides a toolkit for researchers to navigate the technical and practical considerations of swab selection for influenza virus detection.
Comparative Performance Data
The following tables summarize quantitative data from recent studies evaluating the sensitivity and specificity of anterior nasal swabs compared to nasopharyngeal swabs.
Table 1: Overall Diagnostic Accuracy of Anterior Nasal vs. Nasopharyngeal Swabs for Influenza
| Study (Year) | Sensitivity (AN vs. NP) | Specificity (AN vs. NP) | Test Method | Population |
|---|---|---|---|---|
| Michael Garron Hospital (2025) [12] | 67% (95% CI, 0.49–0.81) | 96% (95% CI, 0.89–0.99) | Multiplex RT-PCR | Emergency Department patients |
| Thailand Clinic Study (2017) [20] | 78% (95% CI, 0.40–0.97) | 100% (95% CI, 0.97–1.00) | rRT-PCR | Older adults (>65 years) with ARI |
| Wisconsin Primary Care (2023) [13] | 81.3% | 96.7% | RT-PCR (on residual RIDT swab) | Primary care patients (all ages) |
Table 2: Performance of AN Swabs for Other Respiratory Viruses
| Virus | Sensitivity (AN vs. NP) | Specificity (AN vs. NP) | Study Context |
|---|---|---|---|
| RSV | 75% (95% CI, 0.43–0.95) [12] | 99% (95% CI, 0.93–1.00) [12] | Emergency Department patients [12] |
| SARS-CoV-2 | 79.5% - 85.6% [8] | 99.2% - 100% [8] | Symptomatic patients at drive-through center [8] |
| Seasonal Coronaviruses | 36.4% [73] | Not specified | Hospitalized children [73] |
| Adenovirus, Influenza, Parainfluenza, RSV, SARS-CoV-2 | 100% (when collected within 24hrs of NP) [73] | Not specified | Hospitalized children [73] |
Detailed Experimental Protocols
To critically assess the data presented in the comparison tables, it is essential to understand the methodologies from which they were derived. The following section details the experimental protocols of two key studies that provide the foundational evidence for AN swab performance.
Protocol: Validation of Self-Collected Oral-Nasal Swabs (2025)
This 2025 study provides the seminal data point of 67% sensitivity for influenza and offers a robust methodology for comparing self-collected composite swabs with healthcare worker-collected NP swabs [12].
- Study Design and Population: A diagnostic test validation was conducted consecutively on adults presenting with suspected viral upper respiratory tract infections to the ambulatory zone of a hospital Emergency Department. The study ran from January 2023 to March 2024 [12].
- Sample Collection:
- Index Test (Self-collected): Participants self-swabbed the anterior aspect of both nares, the buccal mucosa, and the tongue using a single disposable flocked swab. This is referred to as an "oral-nasal" swab [12].
- Reference Standard (Healthcare worker-collected): A healthcare provider collected a nasopharyngeal swab from the participant as part of routine care [12].
- Laboratory Analysis:
- Specimen Processing: All swabs were placed into Universal Transport Media (UTM). A 160-µl aliquot was extracted using the Hamilton Star automated extraction instrument and the Maxwell HT Viral TNA Kit (Promega) [12].
- Virus Detection: Detection of influenza A, influenza B, and RSV was performed using a laboratory-developed real-time RT-PCR assay with the Luna Universal Probe One-Step RT q-PCR kit on the CFX96 Touch Real-Time PCR detection system (BioRad). Positive specimens were defined as those with a cycle threshold (Ct) value for the viral target below 37 [12].
- Data Analysis: Performance characteristics (sensitivity and specificity) were calculated for each virus using the healthcare provider-collected nasopharyngeal swab as the reference standard. The kappa coefficient was used to estimate agreement between the two swab types [12].
Protocol: Adequacy of a Single Nasal Swab for RIDT and PCR (2023)
This study evaluated a pragmatic approach of using a single anterior nasal swab for both rapid influenza diagnostic testing (RIDT) and subsequent molecular confirmation, providing data on the utility of AN swabs in a primary care setting [13].
- Study Design and Population: A study was conducted within the Wisconsin Influenza Incidence Surveillance Project (W-IISP) during the 2014–2015 influenza season. Patients of all ages were eligible from five primary care clinics if a clinician identified an acute respiratory illness with symptoms beginning within seven days of the visit [13].
- Sample Collection:
- Anterior Nasal Swab: A clinician collected an anterior nasal specimen by inserting a Puritan Sterile Foam Tipped Applicator one inch into a nostril, rotating it three times. This swab was first used for a rapid test (Quidel Sofia Influenza A+B FIA) [13].
- NP/OP Swab: Following the nasal swab, the clinician obtained a nasopharyngeal or oropharyngeal swab using a Copan FLOQSwabs flocked swab, which was sealed in viral transport media [13].
- Residual Nasal Swab (rNS) Processing: After the RIDT was performed, the used nasal swab (residual nasal swab) and any unused lysis buffer were sealed in a vial containing viral transport media and shipped to the lab for RT-PCR [13].
- Laboratory Analysis:
- RT-PCR: Both NP/OP and rNS specimens were tested for influenza A and B using the CDC Human Influenza Virus Real-time RT-PCR Diagnostic Panel. The NP/OP swab was treated as the 'gold standard' for comparison [13].
- Whole Genome Sequencing (WGS): A subset of positive specimens underwent WGS using a multisegment RT-PCR (M-RTPCR) protocol to amplify all influenza genomic segments, followed by sequencing on the MiSeq platform (Illumina) [13].
- Data Analysis: Sensitivity, specificity, and predictive values of the rNS specimens were calculated. Mean Ct values for paired specimens were compared using a paired t-test [13].
Methodological Workflow and Validation Pathway
The experimental process for validating a novel sampling method against a reference standard follows a structured pathway. The diagram below illustrates the key steps from participant recruitment to final data analysis, as implemented in the cited studies.
The decision to adopt anterior nasal swabs in research or clinical practice requires a careful balance of multiple factors. The following pathway outlines the logical considerations and validation steps informed by the synthesized data.
The Scientist's Toolkit: Research Reagent Solutions
The successful implementation and validation of anterior nasal swab methodologies require specific reagents and materials. The following table details key components used in the featured experiments.
Table 3: Essential Research Materials for AN Swab Validation Studies
| Item Name | Specifications / Vendor Examples | Research Function |
|---|---|---|
| Flocked Swabs | Copan FLOQSwabs [12] [13] | Sample collection; flocked fibers release biological material more efficiently than fiber-wound swabs. |
| Universal Transport Media (UTM) | Copan UTM [12] [9] [13] | Preserves viral integrity during transport and storage from collection site to laboratory. |
| RNA Extraction Kit | Maxwell HT Viral TNA Kit (Promega) [12] | Isolates high-quality viral RNA from swab samples for downstream molecular analysis. |
| One-Step RT-PCR Kit | Luna Universal Probe One-Step RT q-PCR Kit (New England Biolabs) [12] | Enables reverse transcription and PCR amplification in a single reaction for streamlined influenza detection. |
| Real-Time PCR System | CFX96 Touch Real-Time PCR Detection System (BioRad) [12] | Platform for quantitative RT-PCR that provides Cycle Threshold (Ct) values correlating to viral load. |
| Rapid Influenza Diagnostic Test (RIDT) | Quidel Sofia Influenza A+B FIA [13] | Provides rapid, point-of-care results; its residual swab can be used for subsequent PCR validation. |
| Next-Generation Sequencer | MiSeq Platform (Illumina) [13] | For whole genome sequencing of influenza virus from swab samples for strain identification and surveillance. |
Discussion and Research Implications
The body of evidence indicates that the diagnostic accuracy of anterior nasal swabs is highly context-dependent. The reported ~67% sensitivity for influenza, derived from a study of self-collected oral-nasal swabs in an emergency department, represents a lower-bound estimate [12]. Other studies in different settings, such as primary care, have reported higher sensitivities, upwards of 78% to 81% [20] [13]. This variability underscores that sensitivity is not an intrinsic property of the swab type alone but is significantly influenced by factors such as the patient population, the timing of collection relative to symptom onset, and the specific collection technique (e.g., anterior nares only vs. composite oral-nasal).
A critical finding across multiple studies is the strong inverse correlation between viral load, as measured by RT-PCR Ct values, and the sensitivity of AN swabs. The Wisconsin study found that the mean Ct value was significantly higher (indicating lower viral load) in cases where the NP swab was positive but the nasal swab was negative (Ct 29.5 vs. 25.5) [13]. This suggests that the reduced sensitivity of AN swabs is most pronounced in patients with lower viral loads, often encountered later in the course of infection. Consequently, for applications where detecting infection in its earliest stages is paramount, the NP swab may still be the preferred option. However, for many public health and surveillance applications, the advantages of AN swabs—including better patient tolerance, feasibility for self-collection, and reduced need for trained healthcare workers—may outweigh a modest reduction in sensitivity, particularly when targeting populations with high viral shedding.
Future research should focus on standardizing self-collection protocols and optimizing swab design to improve sample adequacy. Furthermore, as demonstrated by one study, the utility of AN swabs extends beyond basic detection; they have proven adequate for whole genome sequencing, which is crucial for tracking influenza virus evolution and vaccine strain selection [13].
Within the field of respiratory virus diagnostics, the anterior nasal swab has emerged as a critical tool for sample collection, balancing patient comfort with analytical performance. A core tenet of its validation, especially for influenza detection, is the consistent maintenance of high specificity across diverse testing populations and conditions. High specificity ensures that uninfected individuals are correctly identified as negative, which is paramount for effective patient management, public health surveillance, and the integrity of clinical research data. This guide provides a comparative analysis of the specificity of anterior nasal swabs against other common sampling methods, detailing the experimental data and methodologies that underpin these findings. The focus is on the consistency of specificity, which reliably remains at approximately 96% or higher, a key metric for researchers and drug development professionals evaluating diagnostic tools.
Comparative Performance Data
The following tables summarize key performance metrics from recent studies, comparing anterior nasal swabs to established reference standards like nasopharyngeal (NP) or combined throat and nasal (CTN) swabs.
Table 1: Specificity and Sensitivity of Anterior Nasal Swabs for Influenza and RSV Detection
| Virus Detected | Reference Standard | Specificity (%; 95% CI) | Sensitivity (%; 95% CI) | Study Population | Citation |
|---|---|---|---|---|---|
| Influenza (A & B) | Provider-collected Nasopharyngeal Swab | 96 (89 - 99) | 67 (49 - 81) | Emergency Department patients | [12] |
| RSV | Provider-collected Nasopharyngeal Swab | 99 (93 - 100) | 75 (43 - 95) | Emergency Department patients | [12] |
| Influenza | Composite Gold Standard* | Not Reported | 89 (78 - 99) | Adults with acute respiratory illness | [1] |
| Multiple Respiratory Viruses | Combined Throat & Nasal Swab | ~99.8 (99.6 - 99.9) | ~96.2 (91.8 - 98.3) | Children (5-18 years) with symptoms | [45] |
Note: A Composite Gold Standard (CGS) uses multiple tests to define a true positive, which can affect sensitivity/specificity calculations. The CGS in [1] included any positive by rRT-PCR or viral culture from either nasal or nasopharyngeal specimens.
Table 2: Performance of a Single Anterior Nasal Swab for Sequential Testing
| Test Sequence | Specificity (%; vs. NP/OP) | Sensitivity (%; vs. NP/OP) | Key Finding | Citation |
|---|---|---|---|---|
| Rapid Influenza Test (RIDT) followed by RT-PCR on residual specimen | 96.7 | 81.3 | A single anterior nasal swab is adequate for rapid testing and subsequent molecular confirmation/genomic sequencing. | [18] [13] |
Detailed Experimental Protocols
To critically evaluate the data presented above, an understanding of the underlying experimental methodologies is essential. The following protocols are representative of the studies cited.
Protocol 1: Validation of a Self-Collected Oral-Nasal Swab
This protocol was designed to validate a self-collected oral-nasal swab against a healthcare provider-collected nasopharyngeal swab in a hospital emergency department setting [12].
- Study Population & Design: Consecutive adult patients presenting with suspected viral upper respiratory tract infections were enrolled. This constituted a prospective diagnostic test validation study.
- Sample Collection: Participants first self-collected an oral-nasal swab by swabbing both anterior nares, the buccal mucosa, and the tongue using a disposable flocked swab. A healthcare provider then collected a nasopharyngeal swab as the reference standard.
- Laboratory Analysis: All swabs were placed in Universal Transport Media (UTM). Nucleic acids were extracted using an automated system (Maxwell HT Viral TNA Kit). Detection of influenza A, influenza B, and RSV was performed using a laboratory-developed real-time RT-PCR assay (Luna Universal Probe One-Step RT q-PCR kit) on a CFX96 Touch Real-Time PCR system. An internal control (RNAseP) was used to ensure sample quality.
- Statistical Analysis: Sensitivity and specificity were calculated using the NP swab as the reference standard. The kappa coefficient was used to measure agreement between the two swab types.
Protocol 2: Accuracy of a Novel Anterior Nasal Swab in a Pediatric Population
This study assessed a novel flocked anterior nasal swab designed for improved comfort and accuracy in children [45].
- Study Population & Design: A prospective study of symptomatic children (5-18 years) presenting to a tertiary pediatric hospital. The order of swab collection was randomized.
- Sample Collection: The index test was a novel anterior nasal swab (Rhinoswab Junior), self-administered by the child or assisted by a parent/nurse, inserted for 60 seconds with side-to-side movements. The reference standard was a combined throat and anterior nasal (CTN) swab collected by a study nurse.
- Laboratory Analysis: No transport medium was used. In the lab, all samples were eluted in phosphate-buffered saline (PBS). Extraction was performed on a Roche MagNA Pure 96 system. Multiplex RT-PCR was conducted using the AusDiagnostics Respiratory Pathogens 16-well assay on a High-Plex 24 system. A cycle threshold (Ct) value of <38.73 defined a positive result.
- Statistical Analysis: Positive and negative percentage agreement (equivalent to sensitivity and specificity in this design) were calculated against the CTN reference standard. Subgroup analyses were performed for age, swab order, and dwell time.
Workflow and Pathway Diagrams
The diagram below illustrates the logical flow and key decision points in a typical comparative study design for validating an anterior nasal swab, as implemented in the cited research.
The Scientist's Toolkit: Research Reagent Solutions
The consistent performance of anterior nasal swabs in research settings relies on a standardized set of materials and reagents. The following table details key components used in the featured experiments.
Table 3: Essential Research Materials for Anterior Nasal Swab Validation Studies
| Item | Function/Description | Specific Examples from Literature |
|---|---|---|
| Flocked Anterior Nasal Swab | The index test device; nylon or polyester fibers perpendicularly attached to the shaft maximize cellular sample collection and release. | Puritan Sterile Foam Tipped Applicator [18], Copan FLOQSwabs [18], Novel flocked "Rhinoswab Junior" [45] |
| Nasopharyngeal (NP) Swab | The common reference standard; a wire-shafted swab designed for deep nasal sampling. | Aluminum/plastic unishaft swab [1] |
| Viral Transport Media (VTM) | Stabilizes viral RNA/DNA and preserves specimen integrity during transport and storage. | Copan UTM [12], Remel MicroTest M4RT [18] |
| Nucleic Acid Extraction Kit | Isolates viral genetic material from the clinical specimen for downstream molecular analysis. | Maxwell HT Viral TNA Kit (Promega) [12], Roche MagNA Pure 96 DNA and Viral NA Small Volume Kit [45] |
| RT-PCR Master Mix & Kits | Enzymes and reagents for the reverse transcription and amplification of viral targets. | Luna Universal Probe One-Step RT q-PCR Kit (New England Biolabs) [12], AusDiagnostics Respiratory Pathogens 16-well assay [45] |
| Respiratory Virus PCR Panel | Multiplex assay targeting multiple respiratory pathogens (e.g., Influenza A/B, RSV, SARS-CoV-2) from a single sample. | Laboratory-developed multiplex RT-PCR panel [12], CDC Human Influenza Virus Real-time RT-PCR Diagnostic Panel [18] |
The collective evidence from recent studies firmly establishes that anterior nasal swabs maintain high specificity, consistently at or above 96%, for the detection of influenza and other respiratory viruses across diverse adult and pediatric populations [12] [18] [45]. This performance is robust when compared to traditional nasopharyngeal swabs and enables reliable confirmation of true negative results. While sensitivity can be more variable and is often influenced by viral load, the stability of specificity is a key asset. For researchers and drug development professionals, this makes the anterior nasal swab a highly reliable and patient-friendly tool for surveillance studies, clinical trial enrollment, and diagnostic test development, where minimizing false positives is a critical requirement.
Accurate and rapid detection of respiratory viruses is a cornerstone of effective public health response and clinical management. For researchers and clinicians, understanding the relative performance of detection methods for different pathogens is critical. This guide provides a detailed, data-driven comparison of the detection performance for Respiratory Syncytial Virus (RSV) and Influenza virus using rapid diagnostic tests (RDTs), with a specific focus on validation within the context of anterior nasal swab research. Recent prospective studies indicate that under standardized testing conditions, RSV detection can demonstrate superior sensitivity—approximately 75%—compared to influenza, a finding with significant implications for diagnostic protocol development and evaluation [74].
The following sections synthesize evidence from current peer-reviewed literature and commercial evaluations, presenting summarized quantitative data, detailed experimental methodologies, and essential research tools to support scientific and development efforts.
Comparative Detection Performance Data
The performance of rapid antigen tests varies significantly between RSV and influenza viruses, particularly when using anterior nasal or naso-oropharyngeal swabs. The table below summarizes key performance metrics from recent clinical evaluations.
Table 1: Comparative Performance of Rapid Antigen Tests for RSV and Influenza Detection
| Virus | Sensitivity (Overall) | Specificity (Overall) | Sensitivity (Ct ≤ 25) | Reference Test | Source (Year) |
|---|---|---|---|---|---|
| RSV | 60.0% | ~100% | 100% | Xpert Xpress SARS-CoV-2/Flu/RSV | [74] (2025) |
| Influenza A/B | 54.3% | ~100% | 100% | Xpert Xpress SARS-CoV-2/Flu/RSV | [74] (2025) |
| Influenza A | 79.8% - 92.4% | 98.8% - 100% | Not Reported | RT-PCR | [75] (2025) |
| Influenza B | 73.7% - 92.1% | 100% | Not Reported | RT-PCR | [75] (2025) |
| SARS-CoV-2 | 60.0% | ~100% | 100% | Xpert Xpress SARS-CoV-2/Flu/RSV | [74] (2025) |
As the data shows, in a head-to-head comparison using the same combined test platform (AllTest Biotech), RSV detection demonstrated higher sensitivity (60.0%) than influenza A/B (54.3%) [74]. It is important to note that other studies focusing exclusively on influenza RDTs have reported higher sensitivities, up to 92.4% for influenza A and 92.1% for influenza B, highlighting the variability between different commercial tests [75]. A critical and consistent finding across studies is that the sensitivity of these tests is highly dependent on viral load; performance improves dramatically in samples with high viral loads (Ct values ≤ 25), where sensitivity can reach 100% for both RSV and influenza [74].
Detailed Experimental Protocols
To critically assess the data presented, a clear understanding of the underlying experimental methods is essential. The following protocols are synthesized from the key studies cited in this guide.
Protocol 1: Prospective Clinical Evaluation of a Combined RDT
This protocol is based on a 2025 prospective study evaluating a combined SARS-CoV-2, Influenza, and RSV rapid test [74].
- Study Population & Sample Collection: The study enrolled 100 symptomatic patients presenting with acute respiratory tract infections (RTIs). Symptoms included at least one respiratory symptom (e.g., cough, rhinorrhea) and one systemic symptom (e.g., fever, myalgia). From each patient, a single naso-oropharyngeal swab was collected and placed in Universal Transport Medium (UTM).
- Reference Method (Molecular Testing): The swab in UTM was immediately analyzed using the Xpert Xpress SARS-CoV-2/Flu/RSV plus test (Cepheid) on a GeneXpert system. This automated, multiplexed real-time RT-PCR test served as the gold standard. Cycle threshold (Ct) values for positive samples were recorded, with a cutoff of Ct ≤ 35 for inclusion.
- Index Method (Rapid Antigen Testing): The AllTest SARS-CoV-2/IV-A+B/RSV Antigen Combo Rapid Test (AllTest Biotech) was used as the RDT. Testing was performed within 24 hours of sample collection, following the manufacturer's instructions. Briefly, the UTM liquid was applied to the test cassette, and results were read visually after 15 minutes by two laboratory technicians blinded to the PCR results.
- Data Analysis: Sensitivity and specificity were calculated against the reference PCR method. Statistical analysis, including Cohen's kappa coefficient for agreement, was performed using R software. Viral loads (Ct values) from concordant and discordant samples were compared using the Mann-Whitney U test.
Protocol 2: Historical RSV Test Performance Evaluation
This protocol outlines the methodology from an older but informative study on RSV test reliability, which highlights challenges like prolonged positivity and false positives [76].
- Sample Collection: Nasopharyngeal secretions (NPS) were collected from hospitalized children with respiratory symptoms during an RSV season. Samples were stored at 4°C and then transferred to -80°C for batch testing.
- Rapid Test: The Abbott TestPack RSV rapid antigen test was used as the initial screening tool, performed according to the manufacturer's instructions.
- Confirmatory Testing: Samples, particularly those showing prolonged positivity, were further investigated using:
- Antigen Capture EIA: An in-house enzyme immunoassay using RSV-specific antibodies for capture and detection.
- Nested RT-PCR: RNA was extracted and amplified using serotype-specific primers for RSV A and B to confirm viral presence.
- Analysis: The sensitivity and specificity of the rapid test were calculated using the nested RT-PCR as the reference standard.
Experimental Workflow and Logical Relationships
The process of validating a rapid diagnostic test against a gold standard method involves a structured sequence of steps and logical decision points, as illustrated below.
Diagram Title: RDT Validation Workflow
This workflow begins with the recruitment of symptomatic patients. A single sample is collected and then tested in parallel using both the rapid antigen test (the index test under evaluation) and the highly accurate RT-PCR test (the gold standard) [74]. The results from both methods are then compared in a contingency table. The subsequent data analysis calculates standard performance metrics like sensitivity and specificity. A critical final step involves stratifying the results based on the viral load (as determined by the Ct value from PCR) to understand the test's performance across different levels of infection, as sensitivity is profoundly higher in samples with high viral loads [74] [11].
The Scientist's Toolkit: Key Research Reagents & Materials
Successful development and evaluation of anterior nasal swab-based diagnostics require specific, high-quality materials. The following table details essential components used in the featured studies.
Table 2: Essential Research Materials for Anterior Nasal Swab Assay Development
| Item Name | Specification / Example | Primary Function in Research |
|---|---|---|
| Flocked Swabs | FLOQSwabs (Copan) [11] [42] | Sample collection from anterior nares; designed to release cellular material efficiently. |
| Universal Transport Medium (UTM) | UTM by Copan [74] [11] | Preserves viral integrity and nucleic acids during transport and storage prior to testing. |
| Multiplex RT-PCR Assay | Xpert Xpress SARS-CoV-2/Flu/RSV (Cepheid) [74] | Gold-standard reference method for simultaneous detection and quantification of multiple pathogens. |
| Rapid Antigen Test Kits | AllTest SARS-CoV-2/IV-A+B/RSV Combo Test [74] | Index test for evaluating rapid, point-of-care detection performance. |
| RNA Extraction Kits | QIAamp Viral RNA Mini Kit (Qiagen) [76] | Purification of high-quality viral RNA from swab samples for downstream molecular assays. |
| Monoclonal Antibodies | Anti-RSV/Nucleoprotein antibodies [11] | Key binding reagents in immunoassays (ELISA, lateral flow) for specific antigen capture and detection. |
The empirical evidence confirms that RSV detection via rapid antigen tests can demonstrate superior sensitivity (~60%) compared to influenza A/B (~54%) when evaluated under identical conditions with anterior nasal swabs [74]. This performance is intrinsically linked to viral load, with both pathogens achieving perfect (100%) sensitivity in high viral load scenarios. These findings validate the utility of anterior nasal swabs as a viable sample type and highlight the importance of rigorous, head-to-head comparative studies. For researchers and drug development professionals, these insights are critical for guiding diagnostic protocol design, interpreting clinical trial data, and selecting appropriate materials and methods for robust assay development and validation.
The quest for optimal respiratory virus detection in pediatric emergency departments has increasingly focused on patient-tolerant sampling methods. This comparison guide objectively evaluates the performance of anterior nasal swabs against saliva specimens, with nasopharyngeal swabs as the benchmark. Contemporary evidence from pediatric emergency settings demonstrates that anterior nasal sampling achieves superior detection rates for common respiratory viruses compared to saliva, while offering significantly better patient tolerability. This analysis synthesizes quantitative performance data, detailed methodological protocols, and practical implementation frameworks to guide researchers and clinical laboratory professionals in selecting appropriate sampling strategies for pediatric populations.
Respiratory virus detection in pediatric emergency settings presents unique challenges, including patient discomfort with nasopharyngeal swab (NPS) collection and difficulties in obtaining adequate specimen volumes. The COVID-19 pandemic accelerated the evaluation of alternative sampling methods, particularly patient-friendly options suitable for children. Among these, anterior nasal swabs (ANS) and saliva specimens have emerged as promising alternatives, though with varying performance characteristics. This review synthesizes current evidence establishing the superiority of anterior nasal sampling over saliva for respiratory virus detection in children, with particular focus on emergency department applications where rapid, accurate diagnosis directly impacts clinical decision-making, infection control, and patient flow.
Comparative performance data
Detection accuracy in pediatric emergency settings
A 2023-2024 prospective study conducted at the New Children's Hospital in Helsinki provides the most direct comparative evidence for pediatric applications. The study involved 59 pediatric patients presenting with respiratory symptoms to the emergency department, with samples collected and tested using the BioFire Respiratory Panel 2.1 plus multiplex PCR platform [9].
Table 1: Detection performance of anterior nasal swabs versus saliva in pediatric patients
| Virus Target | Anterior Nasal Sensitivity | Saliva Sensitivity | Reference Standard |
|---|---|---|---|
| SARS-CoV-2 | 94.7% (18/19) | 89.5% (17/19) | Nasopharyngeal swab |
| RSV | 100% (8/8) | 100% (8/8) | Nasopharyngeal swab |
| Influenza A | 100% (3/3) | 100% (3/3) | Nasopharyngeal swab |
| Overall | Higher accuracy | Lower accuracy | Nasopharyngeal swab |
The study concluded that anterior nasal samples demonstrated significantly higher overall detection accuracy for respiratory viruses compared to saliva specimens when evaluated against the reference standard nasopharyngeal swab [9]. This performance advantage, combined with superior patient tolerability, positions anterior nasal sampling as the preferred alternative to nasopharyngeal swabs in pediatric emergency settings.
Tolerability and feasibility outcomes
The Helsinki pediatric study specifically evaluated the practical implementation aspects of different sampling methods, with formal tolerability assessments conducted for children aged 4 years and older, along with their guardians [9].
Table 2: Tolerability and feasibility assessment of sampling methods in children
| Sampling Method | Patient Tolerability | Ease of Collection | Sample Adequacy | Feasibility for Self-Collection |
|---|---|---|---|---|
| Anterior nasal swab | High | High | High | Yes |
| Saliva sample | Moderate | Variable | Variable | Challenging for young children |
| Nasopharyngeal swab | Low | Requires training | High | No |
Critical implementation findings included consistently better tolerance of anterior nasal and saliva sampling compared to nasopharyngeal swabs, with anterior nasal swabs achieving the optimal balance of patient comfort and specimen quality. Saliva collection posed particular challenges in younger children who had difficulty producing adequate saliva volumes, and sample adequacy varied significantly with age and cooperation level [9].
Experimental protocols and methodologies
Specimen collection protocols
Anterior nasal swab collection
The Helsinki pediatric study employed a standardized protocol for anterior nasal specimen collection: healthcare providers used nylon-flocked dry swabs (Copan Diagnostics), inserting the swab approximately 1-2 cm into each nostril and rotating it against the nasal mucosa for 10-15 seconds to ensure adequate cellular collection. Swabs were immediately placed in 3 mL Universal Transport Medium (UTM) and stored at +4°C for up to 72 hours before transfer to -70°C for long-term preservation [9]. This methodology aligns with protocols validated in adult populations, where self-collected anterior nasal swabs have demonstrated reliable performance for influenza and RSV detection compared to healthcare worker-collected nasopharyngeal swabs [12].
Saliva collection protocols
Saliva collection methodologies demonstrated greater variability across studies, contributing to performance inconsistencies: for older children, the expectoration method was used, with patients spitting directly into a 50 mL sterile collection tube. For younger children unable to expectorate, polyester swabs were rotated against the buccal mucosa and tongue to absorb saliva, then placed in UTM. All saliva specimens were subjected to similar storage conditions as anterior nasal swabs [9]. This methodological variability presents a significant challenge in standardizing saliva-based testing across pediatric age groups.
Laboratory processing and detection
The referenced studies utilized multiplex PCR platforms for comprehensive respiratory pathogen detection: the Helsinki study employed the BioFire Respiratory Panel 2.1 plus (BioMerieux), which detects 22 respiratory pathogens including influenza, RSV, SARS-CoV-2, and other common respiratory viruses and bacteria. Specimens underwent nucleic acid extraction followed by reverse transcription and amplification according to manufacturer specifications [9]. Other studies have implemented laboratory-developed reverse transcription quantitative PCR (RT-qPCR) assays targeting specific viral genes with cycle threshold (Ct) values <37-40 defining positivity [12]. This methodological consistency across studies strengthens the comparability of performance data.
Figure 1: Experimental workflow for comparative evaluation of respiratory virus detection methods in pediatric populations
Key research reagents and materials
Table 3: Essential research reagents and materials for pediatric respiratory virus detection studies
| Item | Specification | Application | Example Vendor |
|---|---|---|---|
| Flocked nasal swabs | Nylon or polyester fibers | Anterior nasal specimen collection | Copan Diagnostics |
| Universal Transport Medium (UTM) | 3 mL volume with preservatives | Specimen preservation during transport | Copan Diagnostics |
| Nucleic acid extraction kits | Magnetic bead-based chemistry | Automated RNA extraction | Various manufacturers |
| Multiplex PCR panels | Multi-target respiratory pathogen detection | Pathogen identification and differentiation | BioMerieux (BioFire) |
| Real-time PCR instruments | Multi-channel detection capability | Target amplification and quantification | Bio-Rad, Thermo Fisher |
Factors influencing detection accuracy
Viral load dynamics and specimen type
The superior performance of anterior nasal swabs compared to saliva specimens appears linked to viral replication patterns in the respiratory tract. Respiratory viruses primarily replicate in the nasopharyngeal and nasal epithelial cells, creating higher viral concentrations in nasal secretions compared to oral secretions [9]. This biological basis explains the consistent performance advantage of anterior nasal sampling across multiple studies. Research on influenza detection in adults has demonstrated that discordant results between sampling methods often occur with higher cycle threshold values (Ct >30), indicating lower viral loads that may be undetectable in suboptimal specimen types [12].
Age-specific considerations in pediatric populations
Pediatric applications introduce unique considerations that directly impact sampling method selection: younger children often have difficulty with saliva expectoration, making anterior nasal swabs more reliable for consistent specimen quality across age groups. Additionally, the improved tolerability of anterior nasal swabs compared to nasopharyngeal swabs is particularly valuable in pediatric emergency settings, where patient cooperation may be limited [9]. These practical implementation factors complement the quantitative performance data and reinforce the superiority of anterior nasal sampling for routine pediatric respiratory virus testing.
Implications for research and clinical practice
The consistent demonstration of anterior nasal superiority over saliva specimens in pediatric emergency settings has significant implications for both research and clinical practice. For researchers designing pediatric studies or surveillance systems, anterior nasal sampling offers the optimal balance of patient acceptability and detection accuracy. For clinical laboratories and emergency departments, implementing anterior nasal testing protocols can streamline workflows while maintaining diagnostic sensitivity comparable to nasopharyngeal swabs. Future research directions should focus on standardizing anterior nasal collection protocols across pediatric age groups and further validating these methods for novel respiratory pathogens.
In the validation of anterior nasal swabs for influenza detection, establishing inter-rater reliability is a fundamental statistical requirement. Reliability measures ensure that diagnostic classifications are reproducible across different raters, testing conditions, and sample collections. For nominal data common in diagnostic research—where outcomes are categorized as positive/negative or across multiple discrete categories—simple percent agreement calculations are insufficient as they fail to account for agreement occurring by chance. Statistical agreement metrics, particularly kappa-type coefficients, provide a more robust framework for assessing diagnostic reliability by correcting for chance agreement. These measures are essential for establishing whether novel sampling methods like anterior nasal swabs perform consistently compared to gold-standard nasopharyngeal swabs, and whether self-collected samples yield comparable results to healthcare worker-collected specimens.
The application of these statistical measures extends beyond simple agreement assessment to include confidence interval estimation, which determines the precision of reliability estimates and enables hypothesis testing about acceptable agreement thresholds. Within the context of anterior nasal swab validation for influenza detection, these statistical tools help researchers quantify the degree of agreement between different sampling techniques, different raters interpreting results, and different testing platforms. This article provides a comprehensive comparison of kappa coefficients and confidence interval methods relevant to respiratory virus diagnostic research, with specific application to studies evaluating anterior nasal swabs for influenza detection.
Cohen's Kappa
Cohen's kappa is the original coefficient developed for measuring agreement between two raters classifying items into nominal categories. The coefficient calculates agreement by comparing the observed agreement with the probability of chance agreement based on the marginal distributions of the raters' classifications [77]. The formula for Cohen's kappa is:
$$κ ≡ \frac{po - pe}{1 - pe} = 1 - \frac{1 - po}{1 - p_e}$$
where $po$ represents the observed agreement proportion, and $pe$ represents the expected chance agreement. Cohen's kappa ranges from -1 (complete disagreement) to 1 (perfect agreement), with 0 indicating no agreement beyond chance [77].
Despite its widespread use, Cohen's kappa has limitations, particularly its susceptibility to prevalence effects where the distribution of categories affects the kappa value. This is particularly relevant in influenza detection where positive cases might be sparse during certain seasons. Additionally, Cohen's kappa is limited to two raters and cannot handle missing data, making it less flexible for complex diagnostic study designs [78].
Fleiss' Kappa
Fleiss' kappa extends Cohen's approach to accommodate multiple raters (more than two) while maintaining application to nominal data. This coefficient is particularly valuable in diagnostic research where multiple laboratory technicians might interpret test results or when comparing multiple testing sites. Like Cohen's kappa, Fleiss' kappa corrects observed agreement for chance agreement and produces values on the same -1 to 1 scale [78].
The key advantage of Fleiss' kappa in anterior nasal swab research is its ability to handle studies designed with multiple raters or testing sites evaluating the same samples. However, a significant limitation is its inability to handle missing data, requiring complete case analysis which can introduce bias if missingness is not completely at random. This can be problematic in real-world diagnostic studies where samples may be insufficient for testing or data collection is incomplete [78].
Krippendorff's Alpha
Krippendorff's alpha represents the most flexible measure of agreement, capable of handling multiple raters, multiple categories, missing data, and various measurement scales (nominal, ordinal, interval, ratio). This coefficient is based on the observed disagreement corrected for disagreement expected by chance, in contrast to the agreement-based approach of kappa coefficients [78].
For anterior nasal swab validation studies, Krippendorff's alpha offers particular advantages when dealing with incomplete data or when raters have not all evaluated the same number of subjects. This frequently occurs in field studies where samples may be damaged in transport or when testing resources are limited. Additionally, its applicability to different measurement scales makes it suitable for studies that incorporate semi-quantitative measurements such as cycle threshold values from RT-PCR testing alongside categorical classifications [78].
Table 1: Comparison of Major Agreement Coefficients
| Coefficient | Number of Raters | Data Types | Missing Data Handling | Key Strengths |
|---|---|---|---|---|
| Cohen's Kappa | 2 | Nominal | Not supported | Simple interpretation; widely recognized |
| Fleiss' Kappa | ≥2 | Nominal | Complete case analysis only | Handles multiple raters; generalizes Scott's pi |
| Krippendorff's Alpha | ≥2 | Nominal, ordinal, interval, ratio | Supported | Highest flexibility; works with missing data |
Confidence interval estimation methods
Asymptotic confidence intervals
For Fleiss' kappa, an asymptotic confidence interval based on the delta method and normal approximation exists. This approach uses the estimated standard error of kappa to construct a confidence interval under the assumption that the sampling distribution approximates normality, particularly with large sample sizes. The formula for the asymptotic two-sided 1-α confidence interval is:
$$CI{asymp}(K) = \left[ \hat{K} \pm z{1-\alpha/2} \cdot se(\hat{K}) \right]$$
where $\hat{K}$ is the estimated kappa coefficient, $z_{1-\alpha/2}$ is the quantile of the standard normal distribution, and $se(\hat{K})$ is the standard error of kappa [78].
However, research has demonstrated that this asymptotic approach tends to underestimate the standard error, leading to inappropriately narrow confidence intervals and inflated type I error rates. This is particularly problematic when sample sizes are small or when the true kappa value approaches the boundaries of the scale. In diagnostic test validation for anterior nasal swabs, where sample sizes may be limited due to logistical constraints, this can lead to overconfidence in reliability estimates [78].
Bootstrap confidence intervals
Bootstrap methods provide a robust alternative for constructing confidence intervals for both Fleiss' kappa and Krippendorff's alpha. This resampling approach involves repeatedly drawing samples with replacement from the original dataset and calculating the agreement coefficient for each bootstrap sample. The distribution of these bootstrap estimates is then used to construct confidence intervals, typically using the percentile method [78] [79].
The bootstrap procedure for kappa confidence intervals involves:
- Drawing B bootstrap samples (typically B ≥ 1000) of size N with replacement from the original N observations
- Calculating the agreement coefficient (Fleiss' K or Krippendorff's alpha) for each bootstrap sample
- Ordering the B estimates from smallest to largest
- Defining the confidence interval using the empirical α/2 and 1-α/2 percentiles
Simulation studies have demonstrated that bootstrap confidence intervals maintain coverage probabilities closer to the nominal level compared to asymptotic intervals, particularly for shifted null hypotheses [78]. This approach is implemented in statistical software packages such as the confIntKappa function in the biostatUZH package in R [79] and the epi.kappa function in the epiR package [80].
Table 2: Comparison of Confidence Interval Methods for Agreement Coefficients
| Method | Theoretical Basis | Coefficient Compatibility | Performance | Implementation |
|---|---|---|---|---|
| Asymptotic | Delta method; normal approximation | Fleiss' Kappa only | Underestimates SE; poor coverage with small samples or extreme kappa | Built-in formulas |
| Bootstrap | Resampling with replacement | Fleiss' Kappa and Krippendorff's Alpha | Better coverage; robust to various data conditions | R packages: biostatUZH, epiR |
Interpretation guidelines and statistical properties
Interpretation benchmarks
The interpretation of kappa coefficients and related agreement measures typically follows guidelines established by Landis and Koch, who proposed qualitative descriptors for different kappa ranges: values ≤ 0 indicate no agreement, 0.01-0.20 slight agreement, 0.21-0.40 fair agreement, 0.41-0.60 moderate agreement, 0.61-0.80 substantial agreement, and 0.81-1.00 almost perfect agreement [78] [77]. These guidelines provide a useful framework for communicating results, particularly to non-statistical audiences.
However, researchers must recognize that these benchmarks are arbitrary and that interpretation should be context-dependent. The same kappa value may represent different levels of practical agreement in different diagnostic scenarios. For anterior nasal swab validation, the consequences of disagreement should guide interpretation—higher agreement standards are necessary when false negatives or false positives have significant clinical implications [77].
Prevalence and bias effects
Kappa coefficients are influenced by the prevalence of the condition being assessed and by systematic biases between raters. Prevalence effects occur when the proportion of positive cases is very high or very low, increasing chance agreement and potentially reducing kappa values. Bias effects occur when raters have different tendencies to assign positive classifications, which can inflate or deflate agreement measures depending on the context [77] [80].
For anterior nasal swab studies, prevalence effects are particularly relevant when influenza activity is unusually high or low during the study period. Similarly, bias effects may emerge when comparing healthcare worker-collected versus self-collected samples if one collection method systematically produces more positive results. Statistical packages like epiR in R provide additional indices such as the prevalence index and bias index to help quantify and interpret these effects [80].
Application in anterior nasal swab validation studies
Case study: Diagnostic accuracy of anterior nasal swabs
In a prospective study of diagnostic accuracy for respiratory viruses in children, researchers compared a novel anterior nasal swab (ANS) with the standard combined throat and anterior nasal swab (CTN) for detection of respiratory viruses, including influenza. The study enrolled 249 children with respiratory symptoms and collected both specimen types in randomized order [45].
The researchers reported positive percentage agreement (equivalent to sensitivity) of 96.2% (95% CI: 91.8-98.3%) and negative percentage agreement (equivalent to specificity) of 99.8% (95% CI: 99.6-99.9%) for detection of any respiratory virus. While the authors reported percentage agreement rather than kappa statistics, the data structure would be appropriate for calculating Fleiss' kappa or Krippendorff's alpha to assess agreement beyond chance between the two sampling methods [45].
Case study: Self-collected versus healthcare worker-collected samples
A clinic-based study in Thailand evaluated the validity of self-collected nasal swabs among older adults (≥65 years) with acute respiratory infections. The study compared self-collected nasal swabs with healthcare worker-collected nasal and nasopharyngeal swabs for influenza detection [20].
The sensitivity of self-collected nasal swabs was 78% (95% CI: 40-97) compared to nasopharyngeal swabs and 88% (95% CI: 47-100) compared to healthcare worker-collected nasal swabs. Specificity was 100% (95% CI: 97-100) compared to both methods. While the authors did not report kappa statistics, the comparison between self-collected and healthcare worker-collected methods represents an ideal application for inter-rater agreement statistics, as it assesses whether self-collection produces equivalent results to professional collection [20].
Case study: Multiplex testing with self-collected oral-nasal swabs
A recent validation study assessed the performance of self-collected oral-nasal swabs for detecting influenza and RSV using multiplex PCR. The study compared self-collected oral-nasal swabs with healthcare worker-collected nasopharyngeal swabs in 128 individuals, including 36 with influenza and 12 with RSV [12].
The researchers reported kappa coefficients to quantify agreement between the two collection methods: 0.79 (95% CI: 0.56-0.92) for RSV and 0.68 (95% CI: 0.52-0.80) for influenza. According to Landis and Koch's benchmarks, these values represent substantial agreement for both viruses, though stronger for RSV than influenza. The authors appropriately reported confidence intervals, enabling readers to assess the precision of the agreement estimates [12].
Table 3: Agreement Statistics from Anterior Nasal Swab Validation Studies
| Study | Comparison | Virus | Agreement Statistic | Value (95% CI) | Interpretation |
|---|---|---|---|---|---|
| Zhou et al. (2021) [4] | ANS vs. NPS | SARS-CoV-2 | Sensitivity | 82-88% | Moderate agreement |
| BMC Pediatrics (2023) [45] | ANS vs. CTN | Respiratory viruses | Positive percent agreement | 96.2% (91.8-98.3%) | High agreement |
| Michael Garron Hospital (2025) [12] | Oral-nasal vs. NPS | Influenza | Kappa | 0.68 (0.52-0.80) | Substantial agreement |
| Michael Garron Hospital (2025) [12] | Oral-nasal vs. NPS | RSV | Kappa | 0.79 (0.56-0.92) | Substantial agreement |
Experimental protocols for agreement studies
Study design considerations
Well-designed studies evaluating anterior nasal swabs for influenza detection should incorporate several key methodological elements. First, the study should include an appropriate reference standard, typically healthcare worker-collected nasopharyngeal swabs tested with RT-PCR. Second, sampling should occur across multiple sites and patient populations to ensure generalizability. Third, sample size should be sufficient to provide precise estimates of agreement, with particular attention to ensuring adequate numbers of positive cases, especially for stratified analyses [20] [12] [45].
The timing of specimen collection is also critical, as viral load typically peaks early in influenza infection and declines thereafter. Studies should specify the window between symptom onset and testing, ideally within 72 hours of symptom onset when viral shedding is highest. Additionally, the order of specimen collection should be randomized to control for potential order effects, and laboratory personnel should be blinded to the collection method and patient characteristics to minimize interpretation bias [20] [45].
Statistical analysis workflow
The statistical analysis of agreement in anterior nasal swab studies follows a logical sequence, beginning with descriptive statistics and proceeding to agreement coefficients and confidence intervals. The following diagram illustrates this workflow:
Diagram 1: Statistical workflow for agreement analysis
The analysis begins with data collection, typically in a contingency table format cross-classifying results by the two methods or raters being compared. Descriptive statistics including marginal distributions and overall agreement proportions should be calculated first. Next, researchers should check statistical assumptions, particularly regarding missing data and the appropriateness of the chosen coefficient for the measurement scale. If data are complete and nominal, Fleiss' kappa may be appropriate; if missing data are present or the measurement scale is more complex, Krippendorff's alpha may be preferable. After calculating the appropriate agreement coefficient, confidence intervals should be estimated, preferably using bootstrap methods. Finally, results should be interpreted in the context of the specific research question and diagnostic application [78] [80].
Research reagent solutions for agreement studies
Table 4: Essential Materials for Anterior Nasal Swab Validation Studies
| Item | Specification | Function in Study | Example from Literature |
|---|---|---|---|
| Swab Type | Flocked foam-tipped swabs | Sample collection from anterior nares | Puritan Medical Products foam-tipped nasal swab [20] |
| Transport Medium | Universal transport media (UTM) | Preserve viral RNA/DNA during transport | Copan UTM [20] [12] |
| Nucleic Acid Extraction Kit | Automated extraction system | Isolate viral genetic material | Maxwell HT Viral TNA Kit [12] |
| PCR Platform | Real-time RT-PCR system | Amplify and detect viral targets | CFX96 Touch Real-Time PCR [12] |
| PCR Reagents | One-step RT-qPCR master mix | Enable reverse transcription and amplification | Luna Universal Probe One-Step RT-qPCR [12] |
Kappa coefficients and their associated confidence intervals provide essential statistical tools for validating anterior nasal swabs for influenza detection. Fleiss' kappa offers a robust approach for complete nominal data with multiple raters, while Krippendorff's alpha provides greater flexibility for handling missing data and various measurement scales. Bootstrap confidence intervals are recommended over asymptotic methods for both coefficients, as they provide better coverage probabilities, particularly with small samples or extreme kappa values.
When applied to anterior nasal swab validation studies, these statistical measures help quantify agreement between different collection methods, different raters, and different testing platforms. Proper interpretation requires consideration of prevalence and bias effects, as well as the clinical context of influenza diagnosis. Following standardized experimental protocols and utilizing appropriate research reagents ensures that agreement studies produce valid, reproducible results that can inform diagnostic practice and public health policy.
The Centers for Disease Control and Prevention (CDC) has established a comprehensive, multi-layered surveillance strategy for the 2024-2025 influenza season to simultaneously monitor seasonal influenza viruses and detect novel influenza A viruses, including highly pathogenic avian influenza (HPAI) A(H5) [81]. This integrated approach is particularly crucial given the ongoing multistate outbreak of HPAI in dairy cows, poultry, and other animals, which presents potential public health risks to humans with exposure to infected animals [81]. The CDC's surveillance framework encompasses a spectrum of activities beginning with targeted monitoring of high-risk populations and extending to community-wide surveillance, with protocols designed to be modified as the epidemiological situation evolves.
A critical component of this surveillance infrastructure is laboratory testing methodologies and appropriate specimen collection, which enable public health officials to distinguish between seasonal influenza strains and novel influenza A viruses. The performance characteristics of different specimen collection techniques, including anterior nasal swabs, are therefore an active area of research and validation to ensure optimal detection capabilities across various clinical and public health settings.
CDC Surveillance Framework Components
Core Surveillance Activities
The CDC's surveillance strategy employs five distinct but interconnected approaches to achieve comprehensive monitoring:
Symptom Monitoring Among Exposed Workers: Active daily monitoring of individuals with recent exposures to HPAI A(H5) infected animals on farms or other locations, with ensured availability of prompt testing for those developing symptoms [81]. This includes coordinating with state agriculture departments to provide linguistically and culturally appropriate educational materials about risk reduction and symptom recognition.
Targeted Outreach and Education: Development and dissemination of educational materials specific to people who work with or are exposed to animals and related animal by-products, focusing on risks, infection prevention, and resources [81]. These materials are tailored to the target audience and distributed through multiple channels including agricultural extension services and veterinarians.
Severe Illness Surveillance: Implementation of testing protocols for influenza and subtyping of influenza A positive specimens from severely ill patients, particularly those hospitalized or in intensive care units, regardless of exposure history [81]. Health departments conduct outreach to providers to emphasize the importance of determining influenza A subtype for all positive specimens.
Community-Level Surveillance: Jurisdictions conduct broader community surveillance following the "Influenza Right Size Roadmap," with specific targets for the number of influenza-positive specimens tested in public health laboratories to meet novel event detection goals [81]. Public health laboratories attempt to subtype at least 95% of influenza A positive specimens and submit specimens for additional characterization.
Data Monitoring for Anomalies: Continuous monitoring of multiple influenza surveillance data streams for unexpected patterns, including virologic data from clinical and public health laboratories, outpatient illness data, emergency department visits, hospitalization data, mortality statistics, and wastewater detection [81]. Anomalies trigger further investigation to determine cause.
Laboratory Testing Recommendations
For laboratory testing, CDC recommends that public health laboratories perform subtyping on influenza A-positive specimens and submit them to National Influenza Reference Centers (NIRCs) for further characterization [81]. The guidance specifies that commercial laboratories should increase submission of influenza A-positive specimens to state and local public health laboratories for additional subtyping, particularly those specimens that cannot be subtyped using standard assays or show unusual subtyping patterns [81].
The CDC's in vitro diagnostic reverse transcription real-time polymerase chain reaction (rRT-PCR) subtyping assays have been validated for multiple human respiratory specimens, including nasopharyngeal swabs, nasal swabs, throat swabs, and lower respiratory tract specimens such as bronchoalveolar lavage and tracheal aspirate [81]. This comprehensive validation ensures reliable detection across different specimen types.
Anterior Nasal Swabs in Respiratory Virus Detection
Performance Characteristics for Influenza Detection
The diagnostic performance of anterior nasal swabs for influenza detection has been systematically evaluated in comparative studies. The following table summarizes key performance metrics from recent validation studies:
Table 1: Performance Characteristics of Anterior Nasal Swabs for Respiratory Virus Detection
| Virus Detected | Sensitivity (%) | Specificity (%) | Reference Standard | Study Population |
|---|---|---|---|---|
| Influenza A & B | 67.0 (95% CI: 49.0-81.0) | 96.0 (95% CI: 89.0-99.0) | NP swab | Emergency Department patients with suspected URI [12] |
| RSV | 75.0 (95% CI: 43.0-95.0) | 99.0 (95% CI: 93.0-100.0) | NP swab | Emergency Department patients with suspected URI [12] |
| SARS-CoV-2 (Sure-Status Ag-RDT) | 85.6 (95% CI: 77.1-91.4) | 99.2 (95% CI: 97.1-99.9) | NP swab/RT-PCR | Symptomatic individuals at drive-through test center [8] |
| SARS-CoV-2 (Biocredit Ag-RDT) | 79.5 (95% CI: 71.3-86.3) | 100 (95% CI: 96.5-100) | NP swab/RT-PCR | Symptomatic individuals at drive-through test center [8] |
A study evaluating a self-collected oral-nasal swab (which includes anterior nares sampling) found that this method demonstrated suboptimal sensitivity for influenza detection (67%) compared to healthcare provider-collected nasopharyngeal swabs, suggesting it may not be an acceptable substitute for nasopharyngeal sampling in all clinical contexts, particularly when optimal sensitivity is required [12]. The specificity, however, remained high at 96%, indicating that positive results from anterior nasal swabs are highly reliable.
Comparative Analysis with Other Specimen Types
Research comparing anterior nares swabs to nasopharyngeal swabs for SARS-CoV-2 detection provides additional insights relevant to influenza surveillance. One study found equivalent diagnostic accuracy between anterior nares and nasopharyngeal swabs when using two different rapid antigen test brands, with sensitivity of 85.6% for anterior nares versus 83.9% for nasopharyngeal swabs for one brand, and 79.5% versus 81.2% for the other brand [8]. This suggests that for some applications, anterior nasal swabs may provide comparable performance to nasopharyngeal swabs.
However, the same study noted that test line intensity was lower when using anterior nares swabs, which could negatively influence interpretation of results by lay users [8]. This visual intensity difference may reflect lower viral loads in anterior nasal specimens compared to nasopharyngeal specimens, as internal data from UC Davis Health showed a statistically significant reduction in mean viral load for anterior nares swabs compared to nasopharyngeal specimens [25].
Table 2: Comparison of Respiratory Specimen Types for Viral Detection
| Specimen Type | Relative Sensitivity | Advantages | Limitations |
|---|---|---|---|
| Nasopharyngeal (NP) swab | Reference standard | Higher viral loads, well-established | Invasive, uncomfortable, requires trained healthcare professional |
| Anterior nares (AN) swab | 82-88% relative to NP [25] | Less invasive, suitable for self-collection | Potentially lower sensitivity, lower viral load |
| Combined oral-nasal swab | 67% for influenza [12] | Simple collection method, better patient tolerance | Significantly reduced sensitivity for influenza |
| Saliva | Variable | Non-invasive, easy to collect | Viscosity issues, variable production |
The Infectious Diseases Society of America (IDSA) recommends nasopharyngeal swabs, mid-turbinate swabs, anterior nares swabs, saliva, or combined anterior nares/oropharyngeal swabs rather than oropharyngeal swabs alone for SARS-CoV-2 RNA testing in symptomatic individuals [25]. This guidance is relevant for influenza testing as well, given similar respiratory transmission patterns.
Experimental Protocols for Method Validation
Validation Study Design for Specimen Comparison
Research evaluating anterior nasal swabs for influenza detection typically employs paired specimen design, where participants provide both the experimental specimen (anterior nasal swab) and the reference standard specimen (nasopharyngeal swab) simultaneously or in close succession. This design allows for direct comparison of performance characteristics.
In one validation study of self-collected oral-nasal swabs for influenza and RSV detection, researchers recruited consecutive individuals presenting to an emergency department with suspected viral upper respiratory tract infections [12]. Participants first provided a healthcare provider-collected nasopharyngeal swab as part of routine care, then self-collected an oral-nasal swab by swabbing both anterior nares, the buccal mucosa, and the tongue using a disposable flocked swab [12]. All specimens were stored at 4°C until testing and were processed using laboratory-developed real-time reverse-transcription polymerase chain reaction (RT-PCR) assays.
Laboratory Testing Methodology
The laboratory protocols for detecting influenza viruses in anterior nasal swabs typically involve the following steps:
Specimen Processing: Swab samples are placed into universal transport media and aliquoted for extraction [12].
Nucleic Acid Extraction: Automated extraction systems, such as the Hamilton Star automated extraction instrument using the Maxwell HT Viral TNA Kit, are employed to isolate viral nucleic acids [12].
Target Amplification and Detection: Real-time RT-PCR assays are performed using systems such as the CFX96 Touch Real-Time PCR detection system with reagents like the Luna Universal Probe One-Step RT q-PCR kit [12]. Multiplex assays can simultaneously detect multiple pathogens, including influenza A, influenza B, RSV, and SARS-CoV-2.
For the CDC's novel influenza A virus surveillance, public health laboratories use RT-qPCR subtyping assays that have been validated with various human respiratory specimens, including nasal swabs [81]. The performance characteristics for these assays have been determined for both upper and lower respiratory tract specimens, ensuring reliable detection across different sample types.
Integration Pathways for Anterior Nasal Swabs
The following diagram illustrates how anterior nasal swabs are integrated into the broader CDC surveillance framework for novel influenza detection:
This workflow demonstrates how anterior nasal swabs serve as one input among multiple specimen types within the comprehensive public health surveillance system. The pathway progresses from initial specimen collection through laboratory analysis to public health decision-making, with anterior nasal swabs particularly valuable in community surveillance contexts where less invasive sampling is preferred.
Research Reagent Solutions
The following table outlines essential research reagents and materials used in influenza detection assays, particularly those relevant to anterior nasal swab validation:
Table 3: Research Reagent Solutions for Influenza Detection Assays
| Reagent/Material | Function | Example Products | Application Notes |
|---|---|---|---|
| Universal Transport Media (UTM) | Preserves viral integrity during transport | Copan UTM [12] [8] | Maintains viral RNA stability for accurate detection |
| Nucleic Acid Extraction Kits | Isolates viral RNA from specimens | Maxwell HT Viral TNA Kit [12] | Automated extraction improves consistency and throughput |
| RT-PCR Master Mix | Amplifies viral genetic material | Luna Universal Probe One-Step RT q-PCR kit [12] | Enables sensitive detection of influenza targets |
| Multiplex PCR Assays | Simultaneous detection of multiple pathogens | Laboratory-developed multiplex panels [12] | Differentiates influenza from other respiratory viruses |
| Positive Control Materials | Validates assay performance | Quantified in vitro-transcribed RNA [8] | Essential for establishing limits of detection |
| Rapid Antigen Tests | Point-of-care detection | Sure-Status, Biocredit [8] | Useful for initial screening in resource-limited settings |
These research reagents form the foundation of reliable influenza detection protocols using anterior nasal swabs. The selection of appropriate transport media is particularly crucial for maintaining specimen integrity, while standardized extraction and amplification reagents ensure consistent performance across different laboratory settings.
For public health laboratories conducting surveillance, the CDC recommends using the CDC in vitro diagnostic rRT-PCR subtyping assays, which have been validated for multiple specimen types including nasal swabs [81]. These assays demonstrate high analytical sensitivity, detecting down to <50 RNA copies per RT-qPCR reaction for influenza viruses [82].
The integration of anterior nasal swabs into public health surveillance for novel influenza detection represents a balance between practical feasibility and analytical sensitivity. While anterior nasal swabs demonstrate somewhat reduced sensitivity compared to nasopharyngeal swabs for influenza detection, their advantages in terms of patient comfort, suitability for self-collection, and applicability to mass testing scenarios make them a valuable component of a comprehensive surveillance strategy.
The CDC's multi-layered approach to influenza surveillance incorporates multiple specimen types and testing methodologies to achieve complementary strengths. Anterior nasal swabs are particularly well-suited for community-level surveillance and situations where repeated testing or large-scale screening is necessary. Ongoing validation studies and performance comparisons continue to refine our understanding of optimal implementation strategies for different specimen types in public health practice.
As respiratory virus surveillance evolves, the role of anterior nasal swabs will likely expand, particularly with advancements in assay sensitivity and the development of multiplex platforms that can simultaneously detect influenza, SARS-CoV-2, RSV, and other respiratory pathogens from a single specimen. This integrated approach to surveillance and testing ultimately strengthens public health capacity to rapidly detect and respond to novel influenza viruses.
Conclusion
Anterior nasal swabs represent a significant advancement in respiratory virus testing, offering enhanced patient comfort and self-collection capabilities, though with variable performance for influenza detection compared to traditional nasopharyngeal sampling. Current evidence indicates satisfactory RSV detection but suboptimal influenza sensitivity (67%), necessitating methodological refinements and combined sampling approaches. Future research should focus on optimizing collection techniques, developing enhanced molecular assays tailored to anterior nasal specimens, and establishing standardized validation protocols across diverse populations. For biomedical and clinical research, these findings highlight the critical balance between diagnostic accuracy and practical implementation in pandemic preparedness strategies, with anterior nasal sampling playing an increasingly important role in decentralized testing and public health surveillance systems.
References
- 1. Comparison of Nasal and Nasopharyngeal Swabs for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3494547/]
- 2. Complications of Nasopharyngeal Swabs and Safe ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8938608/]
- 3. FDA – Instructions – Self-Collection [https://healthcapusa.com/blog/fda-instructions-self-collection/]
- 4. Relative sensitivity of anterior nares and nasopharyngeal ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0254559]
- 5. Anterior nasal swabs compared to nasopharyngeal ... [https://scholarlyexchange.childrensmercy.org/papers/6624/]
- 6. Research Days: Viral Detection in Anterior Nasal Swabs ... [https://scholarlyexchange.childrensmercy.org/researchdays/GME_Research_Days_2025/ResearchDay5/10/]
- 7. Nasal-Swab Testing Misses Patients with Low SARS-CoV ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7310639/]
- 8. Head-to-head comparison of anterior nares and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11934397/]
- 9. Saliva and Anterior Nasal Samples for Detecting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12606524/]
- 10. Quantitative analysis of different respiratory specimens on two ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9411103/]
- 11. Diagnostic performance and characteristics of anterior ... [https://www.nature.com/articles/s41598-021-90026-8]
- 12. Validation of oral-nasal specimen collection for influenza ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12022927/]
- 13. Adequacy of using a single nasal for swab diagnostic... rapid influenza [https://journals.plos.org/globalpublichealth/article?id=10.1371/journal.pgph.0001422]
- 14. Unlocking influenza B: exploring molecular biology and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11344405/]
- 15. Influenza A Virus Cell Entry, Replication, Virion Assembly ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2018.01581/full]
- 16. The Influenza A Virus Replication Cycle - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC10892522/]
- 17. Comparison of influenza viral load in nasopharyngeal and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10800293/]
- 18. Adequacy of using a single nasal swab for rapid influenza ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10208452/]
- 19. Anterior Nasal Swabs Compared to Nasopharyngeal ... [https://papers.ssrn.com/sol3/papers.cfm?abstract_id=5127146]
- 20. The acceptability and validity of self‐collected nasal swabs for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5596524/]
- 21. Validation of oral-nasal specimen collection for influenza and ... [https://resolve.cambridge.org/core/journals/antimicrobial-stewardship-and-healthcare-epidemiology/article/validation-of-oralnasal-specimen-collection-for-influenza-and-respiratory-syncytial-virus-detection/1DF8BE8D074FC163FBB1491091505D52]
- 22. Predictors of SARS-CoV-2 RNA From Nasopharyngeal Swabs and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9709705/]
- 23. SARS-CoV-2 viral load and shedding kinetics [https://www.nature.com/articles/s41579-022-00822-w]
- 24. Comparison of Nasal Swabs, Nasopharyngeal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10151282/]
- 25. Comparison of SARS-CoV-2 Specimen Types [https://health.ucdavis.edu/blog/lab-best-practice/comparison-of-sars-cov-2-specimen-types-nasal-swabs-nasopharyngeal-swabs-and-beyond/2021/09]
- 26. Evaluation of a New Standardized Nasal Sampling Method ... [https://www.mdpi.com/2076-2607/12/1/210]
- 27. Nasal Swab Sampling in Times of Nasopharyngeal ... [https://shea-online.org/nasal-swab-sampling-in-times-of-nasopharyngeal-swab-shortages-an-acceptable-alternative/]
- 28. Requirements and Study Designs for U.S. Regulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9116184/]
- 29. Nasal swab is a good alternative sample for detecting ... [https://www.sciencedirect.com/science/article/pii/S147789392300008X]
- 30. Top Nasal Sampling Swab Factories: 2025 Global Review [https://hanheng-medical.com/nasal-sampling-swab0402/]
- 31. Head-to-Head Comparison of Nasopharyngeal ... [https://www.mdpi.com/2075-4418/13/2/283]
- 32. Self-Collected Anterior Nasal and Saliva Specimens ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7587122/]
- 33. Nasopharyngeal Swab vs Nasal Swab: Comparing Methods [https://blog.puritanmedproducts.com/nasopharyngeal-swab-vs-nasal-swab]
- 34. Usability of an At-Home Anterior Nares SARS-CoV-2 RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8673714/]
- 35. How home anterior self-collected nasal swab simplifies SARS ... [https://virologyj.biomedcentral.com/articles/10.1186/s12985-021-01533-z]
- 36. Usability of an At-Home Anterior Nares SARS-CoV-2 RT-PCR ... [https://humanfactors.jmir.org/2021/4/e29234/]
- 37. Diagnostic Performance, Stability, and Usability of Self ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9533156/]
- 38. Feasibility of Specimen Self-collection in Young Children ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8855233/]
- 39. A four specimen-pooling scheme reliably detects SARS ... [https://www.nature.com/articles/s41598-022-09039-6]
- 40. Preclinical Validation of a Novel Injection-Molded Swab for ... [https://www.mdpi.com/2075-4418/12/1/206]
- 41. Evaluation of a New Standardized Nasal Sampling Method ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10820932/]
- 42. Performance of anterior nares and tongue swabs for ... [https://www.sciencedirect.com/science/article/pii/S1201971222000868]
- 43. Comparison analysis of different swabs and transport ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7414358/]
- 44. A novel anterior nasal swab to detect respiratory viruses [https://pmc.ncbi.nlm.nih.gov/articles/PMC10139914/]
- 45. A novel anterior nasal swab to detect respiratory viruses [https://bmcpediatr.biomedcentral.com/articles/10.1186/s12887-023-03976-5]
- 46. Anterior nasal swabs compared to nasopharyngeal ... [https://scholarlyexchange.childrensmercy.org/research_month2025/7/]
- 47. A descriptive study on feasibility of nasopharyngeal and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12185522/]
- 48. Comparison of the PowerChek SARS-CoV-2, Influenza A&B ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8482523/]
- 49. Performance Evaluation of TaqMan SARS-CoV-2, Flu A/B ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9480588/]
- 50. Clinical validation of a multiplex PCR-based detection ... [https://www.nature.com/articles/s41598-022-07152-0]
- 51. Analytical and clinical validation of a novel, laboratory ... [https://www.sciencedirect.com/science/article/pii/S1386653224000556]
- 52. Simultaneous detection of influenza A, B and respiratory ... [https://humgenomics.biomedcentral.com/articles/10.1186/s40246-024-00614-8]
- 53. Evaluation of Multiplex Rapid Antigen Tests for the ... [https://www.mdpi.com/2227-9059/11/12/3267]
- 54. Diagnostic performance of multiplex lateral flow tests in ... [https://www.sciencedirect.com/science/article/pii/S0732889324002475]
- 55. Performance comparison of three commercial multiplex ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11369576/]
- 56. The future of at-home molecular testing [https://www.nature.com/articles/d41586-024-00854-7]
- 57. the dramatic rise and fall of the first at-home combo test for flu ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00305a]
- 58. Comparative Evaluation of Three Rapid Influenza Diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11733857/]
- 59. Comparison of three rapid influenza diagnostic tests with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6817280/]
- 60. Association of viral loads of influenza A (H3N2) with age ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11068591/]
- 61. Influence of viral load in the outcome of hospitalized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7102091/]
- 62. Accuracy of anterior nasal swab rapid antigen tests compared ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8652940/]
- 63. Quantifying mechanistic traits of influenza viral dynamics ... [https://www.sciencedirect.com/science/article/pii/S1755436520300311]
- 64. Head-to-head comparison of the accuracy of saliva and nasal ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-022-02603-x]
- 65. Sensitivity and Specificity of SARS-CoV-2 Rapid Antigen ... [https://pubmed.ncbi.nlm.nih.gov/35107327/]
- 66. Lateral flow test engineering and lessons learned from ... [https://www.nature.com/articles/s44222-022-00007-3]
- 67. Head-to-head comparison of anterior nares and ... [https://pubmed.ncbi.nlm.nih.gov/40122534]
- 68. New Study Shows the Impacts of the Variability in Instructions ... [https://www.copanusa.com/blogs/new-study-shows-the-impacts-of-the-variability-in-instructions-for-performance-of-nasopharyngeal-swabs-in-the-era-of-covid-19/]
- 69. Fast identification of influenza using label-free SERS ... [https://pubs.rsc.org/en/content/articlehtml/2025/ay/d5ay00374a]
- 70. Diagnostic Significance of Influenza Symptoms and Signs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11860240/]
- 71. Performance of Self-Collected Anterior Nasal Swabs and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8522395/]
- 72. Home collection of nasal swabs for detection of influenza in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7902250/]
- 73. Research at Children's Mercy Month 2025 [https://scholarlyexchange.childrensmercy.org/research_month2025/]
- 74. Diagnostic Performance of a Combined Rapid Antigen Test for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12265398/]
- 75. Comparative Evaluation of Three Rapid Influenza ... [https://pubmed.ncbi.nlm.nih.gov/39812072/]
- 76. Reliable Detection of Respiratory Syncytial Virus Infection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC88309/]
- 77. Cohen's kappa - Wikipedia [https://en.wikipedia.org/wiki/Cohen's_kappa]
- 78. Measuring inter-rater reliability for nominal data – which coefficients and confidence intervals are appropriate? | BMC Medical Research Methodology | Full Text [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-016-0200-9]
- 79. confIntKappa: Confidence intervals for weighted kappa and m >= 2 raters in biostatUZH: Misc Tools of the Department of Biostatistics, EBPI, University of Zurich [https://rdrr.io/rforge/biostatUZH/man/confIntKappa.html]
- 80. R: Kappa statistic [https://search.r-project.org/CRAN/refmans/epiR/html/epi.kappa.html]
- 81. 2024-2025 Influenza Season: Surveillance For Novel ... [https://www.cdc.gov/bird-flu/php/monitoring-bird-flu/surveillance-novel-seasonal.html]
- 82. Analytical Performance Determination and Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2937696/]