Viral vs. Non-Viral Vectors for CRISPR Delivery: A 2025 Analysis of Efficiency, Safety, and Clinical Translation
This article provides a comprehensive analysis of viral and non-viral delivery vectors for CRISPR-Cas9 therapeutics, tailored for researchers and drug development professionals.
Viral vs. Non-Viral Vectors for CRISPR Delivery: A 2025 Analysis of Efficiency, Safety, and Clinical Translation
Abstract
This article provides a comprehensive analysis of viral and non-viral delivery vectors for CRISPR-Cas9 therapeutics, tailored for researchers and drug development professionals. It explores the foundational mechanisms of CRISPR delivery, compares the methodological applications and editing efficiencies of different vector systems, and addresses critical troubleshooting strategies for optimizing safety and efficacy. Drawing on the latest 2025 clinical trial data and scientific reviews, the content offers a validated, comparative perspective to guide strategic decisions in therapeutic development, from pre-clinical research to clinical application.
The CRISPR Delivery Landscape: Understanding Cargo Formats and Vector Fundamentals
The therapeutic application of the CRISPR/Cas9 system hinges on the efficient delivery of its molecular components into the nucleus of target cells. The choice of how these components are formatted—as plasmid DNA, messenger RNA (mRNA), or preassembled ribonucleoprotein (RNP) complexes—profoundly influences editing efficiency, specificity, duration of activity, and safety profile. This guide provides an objective comparison of these three core cargo formats, focusing on their performance within the broader context of viral versus non-viral delivery vectors for CRISPR-based therapeutics. Understanding the characteristics, advantages, and limitations of each format is essential for researchers to select the optimal strategy for specific experimental or therapeutic goals.
Cargo Format Definitions and Characteristics
Table 1: Core Characteristics of CRISPR/Cas9 Cargo Formats
| Feature | Plasmid DNA (pDNA) | mRNA + gRNA | Ribonucleoprotein (RNP) |
|---|---|---|---|
| Components Delivered | DNA encoding Cas9 and gRNA[s] [1] | Cas9 mRNA and separate gRNA[s] [1] | Precomplexed Cas9 protein and gRNA[s] [1] |
| Nuclear Entry | Required for transcription [1] | Not required (cytosolic translation) | Required for DNA targeting [1] |
| Onset of Activity | Delayed (requires transcription and translation) | Moderate (requires translation) | Immediate [2] |
| Duration of Activity | Prolonged (dependent on promoter and vector) | Transient (mRNA degradation) | Short (protein turnover) [3] |
| Risk of Off-Target Effects | Higher (prolonged Cas9 expression) [3] | Lower (transient expression) [1] | Lowest (short activity window) [1] [3] |
| Immunogenicity | Higher (risk of TLR9 recognition) | Moderate (risk of TLR recognition) | Lower [2] |
The cargo format directly influences the cellular processing and kinetics of the CRISPR/Cas9 system. Plasmid DNA (pDNA) delivers the genetic code for Cas9 and the guide RNA, requiring nuclear entry for transcription and subsequent translation into functional protein [1]. In contrast, the mRNA format bypasses the transcription step, allowing for direct translation of Cas9 protein in the cytoplasm, while the gRNA is delivered separately [1]. The Ribonucleoprotein (RNP) complex represents the most direct approach, involving the delivery of a preassembled, functional Cas9 protein-gRNA complex that is immediately capable of recognizing and cleaving target DNA sequences upon nuclear entry [1] [2].
Performance Comparison: Efficiency, Specificity, and Practicality
Quantitative data from peer-reviewed studies highlight the performance trade-offs between the different cargo formats.
Table 2: Experimental Performance Comparison of CRISPR Cargo Formats
| Cargo Format | Reported Editing Efficiency | Delivery Method & Cell Type | Key Experimental Findings |
|---|---|---|---|
| Plasmid DNA | Up to 20% genomic excision [2] | Polymer-based (HPAE-EB) in HEK293 cells [2] | Editing efficiency dropped when translated to primary human keratinocytes [2]. |
| mRNA + gRNA | High efficacy, specific data not quantified [1] | Bioreducible Lipid Nanoparticles (LNPs) in sensitive cells [1] | Demonstrated high genome editing efficacy and biocompatibility; suitable for transient Cas9 expression with decreased off-target events [1]. |
| RNP Complex | >40% target genomic deletion [2] | Polymer-based (HPAE-EB) in RDEB keratinocytes [2] | Outperformed plasmid DNA delivery in primary cells; minimizes off-target effects and toxicity [1] [2]. |
| RNP Complex | Efficient editing, specific data not quantified [1] | Lipid Nanoparticles (LNPs) in mouse liver and lung [1] | Achieved tissue-specific gene editing in vivo [1]. |
| RNP Complex | High number of INDEL mutations [4] | Transient delivery (DNA-free) into Chicory protoplasts [4] | Produced non-transgenic plants with no risk of unwanted plasmid DNA integration [4]. |
A critical finding from comparative studies is that the performance of a cargo format can be highly context-dependent. For instance, while plasmid DNA mediated 15-20% target genomic excision in HEK293 cells, its efficiency dropped significantly in harder-to-transfect primary human recessive dystrophic epidermolysis bullosa (RDEB) keratinocytes. In the same primary cell model, switching to RNP delivery dramatically increased the editing efficiency to over 40% target genomic deletion [2]. This underscores the importance of considering the target cell type when selecting a cargo format.
Detailed Experimental Protocols
Protocol 1: RNP Delivery via Electroporation for Ex Vivo Cell Engineering
This protocol is widely used in clinical applications, such as the FDA-approved therapy CASGEVY (CTX001) for sickle cell disease [1] [3].
- RNP Complex Assembly: Combine synthetic, HPLC-purified gRNA with purified Cas9 nuclease protein in a defined molar ratio (e.g., 6.6:1 gRNA:Cas9) in a nuclease-free duplex buffer. Incubate at room temperature for 10-20 minutes to allow for complex formation [2].
- Cell Preparation: Isolate target cells (e.g., hematopoietic stem cells, T-cells) and suspend them in an electroporation-compatible buffer.
- Electroporation: Mix the preassembled RNP complexes with the cell suspension. Electroporate using an optimized program (specific voltage, pulse length, and number of pulses vary by cell type). Using a square-wave system is often beneficial for primary cells.
- Post-Transfection Handling: Immediately after electroporation, transfer cells to pre-warmed culture medium. Assess viability and gene editing efficiency after 48-72 hours. For clinical applications, the edited cells are expanded ex vivo before being infused back into the patient [3].
Protocol 2: Polymer-Based Delivery of CRISPR Cargoes
This protocol uses a highly branched poly(β-amino ester) polymer, HPAE-EB, for in vitro delivery [2].
- Polyplex Formation:
- For DNA/mRNA: Dilute the CRISPR cargo (pDNA or mRNA) and the HPAE-EB polymer separately in 25 mM sodium acetate buffer. Mix the two solutions at a 1:1 volume ratio at optimized weight/weight (w/w) ratios (e.g., 20:1 to 60:1 polymer:DNA). Vortex the mixture for 30 seconds and incubate at room temperature for 10-30 minutes to form stable polyplexes [2].
- For RNP: The anionic nature of the RNP complex (due to the gRNA) allows it to be complexed with cationic polymers similarly to nucleic acids. Dilute the preassembled RNP and polymer separately, then mix at the determined optimal w/w ratio (e.g., 20:1 polymer:RNP) [2].
- Cell Transfection: Add the formed polyplexes to cells at 60-70% confluence. Replace the medium with fresh culture medium after 4 hours post-transfection.
- Analysis: Assess transfection efficiency (e.g., via GFP reporter expression for plasmid DNA) and gene editing outcomes (e.g., via T7E1 assay or next-generation sequencing) 48-72 hours post-transfection [2].
Cargo-Vector Integration: A Systems Perspective
The choice of cargo format is intrinsically linked to the selection of the delivery vector, forming an integrated system that dictates the overall success of CRISPR-based therapeutics.
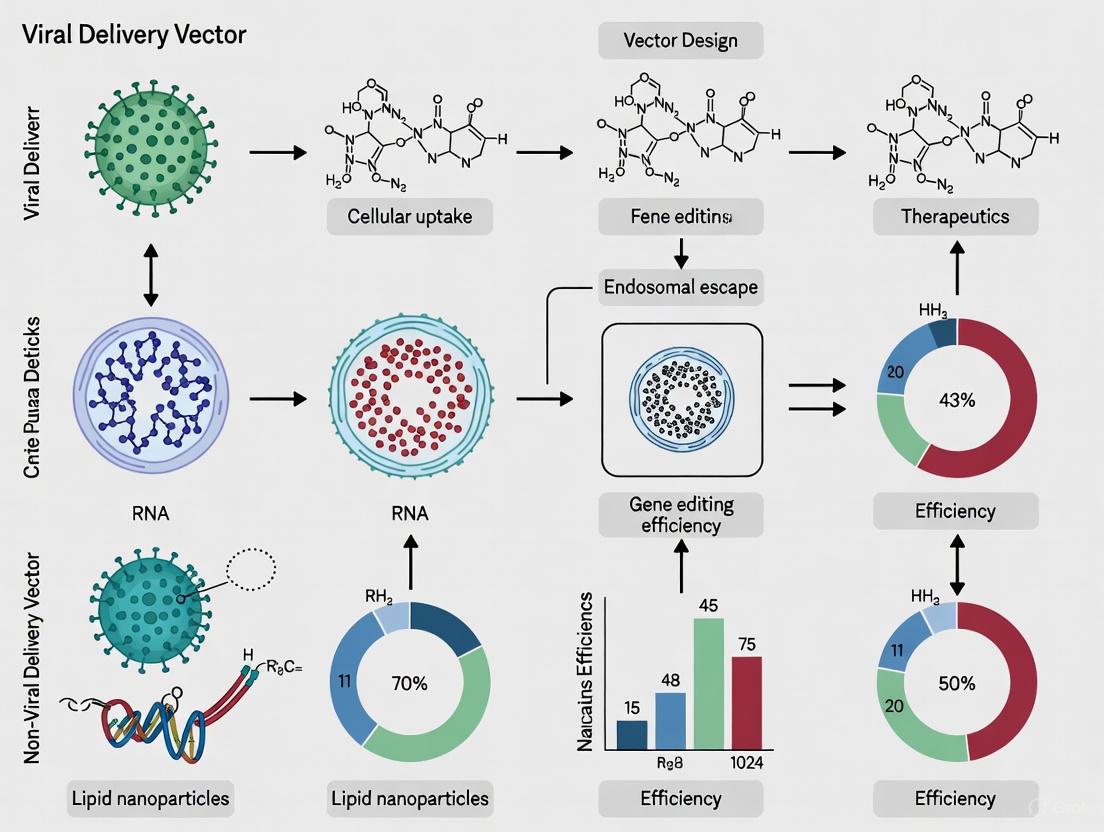
The diagram above illustrates the logical relationships between cargo formats, delivery vectors, and resulting therapeutic outcomes. Viral vectors, such as Adeno-Associated Viruses (AAVs) and Adenoviruses, are predominantly used with DNA-based cargoes (pDNA) for in vivo delivery due to their high transduction efficiency [3]. However, they pose challenges like limited packaging capacity, immunogenicity, and potential for insertional mutagenesis [5] [3]. AAVs, for instance, have a ~4.7 kb packaging limit, which can constrain the delivery of larger Cas9 orthologs [6].
Non-viral vectors, including lipid nanoparticles (LNPs), polymers, and physical methods like electroporation, offer a safer alternative with lower immunogenicity, no risk of insertional mutagenesis, and ease of large-scale production [5] [3]. They are versatile and can deliver all three cargo formats but are particularly well-suited for transient payloads like mRNA and RNP complexes [3]. Electroporation is the gold standard for ex vivo RNP delivery into immune cells and stem cells, as evidenced by its use in approved therapies and clinical trials [1] [3].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for CRISPR Cargo Research
| Reagent / Material | Function / Application | Notes |
|---|---|---|
| Highly Branched Poly(β-amino ester) (HPAE-EB) | A lead cationic polymer for non-viral delivery of DNA, mRNA, and RNP complexes in vitro [2]. | Demonstrates high buffering capacity for endosomal escape and can be functionalized to enhance uptake [2]. |
| Lipid Nanoparticles (LNPs) | A clinically advanced platform for in vivo delivery, particularly of mRNA and RNP cargoes [1] [3]. | Modular systems allow for tuning of organ specificity (e.g., via SORT technology) [3]. |
| Electroporation Systems | Physical method for transient RNP delivery into hard-to-transfect primary cells ex vivo [1] [3]. | Critical for clinical workflows (e.g., CAR-T engineering, CASGEVY) [3]. |
| HPLC-Purified Synthetic gRNA | High-purity guide RNA for RNP assembly or co-delivery with mRNA [3]. | End modifications can enhance stability and reduce cytotoxicity, improving editing outcomes [3]. |
| AAV Serotypes (e.g., AAV8, AAV9) | Recombinant AAV vectors for in vivo delivery of DNA cargoes to specific tissues like liver and CNS [6]. | Serotype determines tissue tropism; packaging capacity is limited to ~4.7 kb [6]. |
The selection of a CRISPR cargo format is a fundamental decision that balances editing efficiency, specificity, and safety. Plasmid DNA can be effective but often presents challenges with delivery efficiency in primary cells and a higher risk of off-target effects. mRNA offers a good balance of transient expression and reduced off-target potential compared to pDNA. However, the RNP format consistently demonstrates superior performance in terms of editing efficiency in sensitive primary cells, the highest specificity with minimal off-target effects, and an excellent safety profile. For ex vivo therapeutic applications, particularly in non-dividing or primary cells, RNP delivery via electroporation or advanced non-viral nanoparticles currently sets the benchmark. For in vivo applications, the choice remains context-dependent, with mRNA/LNP and DNA/AAV systems being prominent, though RNP delivery via non-viral vectors is a rapidly advancing field promising to combine the benefits of high efficiency and superior safety.
The transformative potential of CRISPR-Cas9 gene editing extends from basic biological research to clinical therapeutics, offering unprecedented capabilities for precise genomic modifications. The efficacy of this technology is fundamentally governed by two critical phases: the initial delivery of CRISPR components into target cells and the subsequent cellular machinery that repairs the induced DNA breaks. The choice of delivery vector—viral or non-viral—profoundly influences intracellular trafficking, editing efficiency, and ultimate therapeutic success. This guide provides a systematic comparison of delivery system efficiencies, detailing the journey from cellular uptake through the critical DNA repair pathways that execute the desired genetic alterations.
Cellular Uptake Mechanisms and Intracellular Processing
The mechanism by which CRISPR-Cas9 components enter a cell varies significantly depending on the delivery vector, directly impacting editing efficiency and specificity.
Table 1: Comparison of Cellular Uptake Mechanisms by Delivery Method
| Delivery Method | Primary Uptake Mechanism | Intracellular Processing | Onset of Editing Activity |
|---|---|---|---|
| Viral Vectors (AAV, LV, AdV) | Receptor-mediated endocytosis [7] [8] | Endosomal escape, capsid uncoating, genome release [8] | Moderate (requires transcription/translation for DNA delivery) [9] |
| Lipid Nanoparticles (LNPs) | Endocytosis (lipid raft-dependent) [10] | Endosomal escape via ionizable lipids, release into cytoplasm [7] [10] | Fast (direct activity of RNP or translation of mRNA) [9] |
| Electroporation | Physical membrane disruption [7] | Direct deposition into cytoplasm [7] | Very fast (especially for RNPs) [9] |
| RNP Complexes | Endocytosis (when using carriers) [10] | Endosomal escape, passive nuclear import [9] [10] | Immediate (fully functional complex) [9] |
The journey begins with cellular uptake. Viral vectors like Adeno-Associated Virus (AAV) and Lentivirus (LV) exploit receptor-mediated endocytosis, where the viral capsid binds to specific cell surface receptors and is internalized within an endosome [7] [8]. Non-viral methods, such as Lipid Nanoparticles (LNPs), also rely on endocytosis but are facilitated by the formation of a lipid bilayer around the cargo [10]. Physical methods like electroporation bypass these pathways entirely by creating transient pores in the cell membrane, allowing for direct cytoplasmic entry [7].
Once inside, the cargo must reach the nucleus. Viral vectors have evolved sophisticated mechanisms for endosomal escape and genome release [8]. For non-viral vectors, the key challenge is also endosomal escape, which for LNPs is mediated by ionizable lipids that become protonated in the acidic endosomal environment, leading to membrane disruption and cargo release into the cytoplasm [7] [10]. The final step is nuclear entry. While viral genomes can exploit active nuclear import mechanisms, large Cas9 ribonucleoproteins (RNPs) rely on passive diffusion through the nuclear pore complex or the use of nuclear localization signals (NLS), which are short amino acid sequences that tag the protein for active nuclear transport [10]. Delivery format significantly influences the timeline for editing: plasmid DNA (slowest) requires nuclear entry, transcription, and translation; mRNA (faster) bypasses transcription; and pre-assembled RNPs (fastest) are immediately active upon nuclear entry [9].
DNA Repair Pathways: NHEJ and HDR
Upon successful nuclear entry, the Cas9 nuclease introduces a double-strand break (DSB) in the target DNA. The cellular response to this break is the most critical determinant of the editing outcome, primarily mediated by two competing repair pathways [11].
1. Non-Homologous End Joining (NHEJ) NHEJ is the cell's dominant and most rapid DSB repair pathway. It functions throughout the cell cycle by directly ligating the broken DNA ends together. This process is error-prone, often resulting in small insertions or deletions (indels) at the cleavage site [12] [11]. In the context of CRISPR-Cas9, these indels can disrupt the coding sequence of a gene, leading to a functional knockout. This makes NHEJ the preferred pathway for gene disruption applications [13] [11].
2. Homology-Directed Repair (HDR) HDR is a precise, high-fidelity repair mechanism that operates primarily in the late S and G2 phases of the cell cycle. It requires a homologous DNA template—which can be supplied as an exogenous donor template—to accurately repair the break [11] [14]. This pathway allows for specific gene corrections, insertions, or nucleotide substitutions, making it essential for therapeutic applications that require precision [14]. However, HDR is inherently less efficient than NHEJ and is limited to dividing cells, presenting a significant challenge for editing non-dividing cells like neurons or cardiomyocytes [11].
Table 2: Characteristics of DNA Repair Pathways in CRISPR-Cas9 Editing
| Pathway | Repair Mechanism | Template Required | Efficiency | Primary Outcome | Main Applications |
|---|---|---|---|---|---|
| Non-Homologous End Joining (NHEJ) | Ligation of broken ends | No | High (dominant pathway) | Small insertions or deletions (indels) | Gene knockout, gene disruption [13] [11] |
| Homology-Directed Repair (HDR) | Copying from a homologous template | Yes (donor DNA) | Low (competes with NHEJ) | Precise nucleotide changes or gene insertions | Gene correction, knock-in, specific mutations [11] [14] |
The balance between NHEJ and HDR is crucial. NHEJ is the default pathway, meaning that achieving high HDR efficiency often requires strategic intervention. Common experimental strategies to enhance HDR efficiency include synchronizing cells to the S/G2 phase, using chemical inhibitors of key NHEJ proteins (e.g., Ku70/80 or DNA-PKcs), and optimizing the design and delivery of the donor DNA template [14].
Vector Efficiency and Practical Considerations
The delivery vector choice creates a complex trade-off between efficiency, payload capacity, safety, and applicability.
Table 3: Comprehensive Comparison of Viral vs. Non-Viral Delivery Systems
| Delivery System | Typical Editing Efficiency | Payload Capacity | Immunogenicity & Safety Concerns | Ideal Applications |
|---|---|---|---|---|
| Adeno-Associated Virus (AAV) | Moderate to High [9] [8] | Low (~4.7 kb) [15] [8] | Low immunogenicity; mostly episomal, low risk of insertional mutagenesis [15] [8] | In vivo gene therapy; high precision editing with compact Cas9s [15] [8] |
| Lentivirus (LV) | High [9] | High (~8 kb) | Integrates into host genome; risk of insertional mutagenesis; higher immunogenicity [7] [9] | Ex vivo editing (e.g., CAR-T cells); stable long-term expression [7] [9] |
| Adenovirus (AdV) | Moderate [12] | High (up to ~35 kb) [12] | High immunogenicity; transient expression [12] | In vivo delivery of large cargos; vaccination [12] |
| Lipid Nanoparticles (LNP) | Variable (Moderate to High for liver) [7] [10] | Moderate | Lower immunogenicity than viruses; potential toxicity at high doses [7] | In vivo mRNA/protein delivery; clinical RNAi/CRISPR therapeutics [7] [10] |
| Electroporation (RNPs) | High (ex vivo) [9] | N/A (direct delivery) | Minimal immunogenicity; no genomic integration risk; can be cytotoxic [7] [9] | Ex vivo editing of sensitive cells (e.g., HSCs, T-cells); high-precision editing [9] |
Viral Vector Strategies and Innovations:
- AAVs are favored for in vivo therapy due to their low immunogenicity and high tissue specificity. Their major limitation is a cargo capacity of <4.7 kb, which is insufficient for the standard SpCas9. Solutions include using smaller Cas orthologs (e.g., SaCas9), split-intein systems, or dual-vector approaches where Cas9 and gRNA are delivered separately [15] [8].
- Lentiviruses offer high transduction efficiency and stable long-term expression due to genome integration, but this raises safety concerns about insertional mutagenesis, limiting their use primarily to ex vivo applications [7] [9].
- Adenoviruses have a very high packaging capacity (up to 35 kb for "gutless" versions) but trigger strong immune responses, leading to transient expression and potential toxicity [12].
Non-Viral Vector Strategies and Innovations:
- Lipid Nanoparticles (LNPs) have emerged as a powerful platform, particularly for delivering mRNA and RNPs. A key innovation is the inclusion of permanently cationic lipids (e.g., DOTAP) in formulations, which enables efficient RNP encapsulation at neutral pH, preserving protein structure and function [10]. LNPs can be engineered for tissue-specific targeting.
- Electroporation is highly efficient for ex vivo delivery, especially for RNP complexes. It minimizes off-target effects due to transient activity but can reduce cell viability [7] [9].
- RNP Delivery is considered the gold standard for minimizing off-target effects and avoiding immune responses, as the pre-assembled complexes are active immediately upon nuclear entry and rapidly degraded [9] [10].
Successful CRISPR experimentation requires a suite of carefully selected reagents and tools.
Table 4: Key Research Reagent Solutions for CRISPR-Cas9 Experiments
| Reagent / Tool | Function | Key Considerations |
|---|---|---|
| Cas9 Expression Constructs | Provides the nuclease. Can be plasmid DNA, mRNA, or protein. | Plasmid: cost-effective but persistent expression increases off-target risk. mRNA: transient expression. Protein (for RNP): immediate activity, lowest off-target risk [9]. |
| Guide RNA (gRNA) | Targets Cas9 to specific genomic locus. | Can be expressed from a plasmid or synthesized in vitro. Specificity is critical to minimize off-target effects [9] [11]. |
| Donor DNA Template | Provides homology for HDR-mediated precise editing. | Can be single-stranded oligodeoxynucleotide (ssODN) or double-stranded DNA (dsDNA) donor. Design with sufficient homology arms [14]. |
| Delivery Vectors | Transports CRISPR components into cells. | Choice depends on application (in vivo vs. ex vivo), target cell type, and cargo size (see Table 3). |
| NHEJ/HDR Modulators | Small molecules or peptides that manipulate repair pathway choice. | Compounds like Scr7 (NHEJ inhibitor) or RS-1 (HDR enhancer) can be used to boost HDR efficiency relative to NHEJ [14]. |
| Cell Synchronization Agents | Chemical agents to arrest cells in S/G2 phase. | Agents like aphidicolin can increase the proportion of cells competent for HDR, thereby boosting precise editing rates [14]. |
The journey of CRISPR-Cas9 from cellular uptake to final DNA repair is a complex process where the choice of delivery vector is inextricably linked to the molecular outcome. Viral vectors like AAV offer sophisticated in vivo delivery but are constrained by packaging limits, while non-viral systems like LNPs and electroporated RNPs provide flexibility and enhanced safety for both in vivo and ex vivo applications. The ultimate genetic outcome hinges on the competition between the error-prone NHEJ and precise HDR pathways, a balance that researchers can now influence through vector selection and experimental strategy. As the field advances, the development of next-generation vectors with improved tissue specificity, reduced immunogenicity, and enhanced capacity to deliver diverse payloads will be paramount to fully realizing the therapeutic potential of precise genome editing.
The therapeutic application of CRISPR technology represents a paradigm shift in biomedical science, offering unprecedented potential for treating genetic disorders, cancers, and other intractable diseases. However, the transformative promise of CRISPR is contingent upon one critical factor: the efficient delivery of editing components to target cells. The efficiency of any CRISPR-based therapeutic is fundamentally governed by three core metrics: transfection rates (the successful delivery of CRISPR machinery into target cells), editing specificity (the precision of on-target editing without off-target effects), and duration of effect (the persistence of the therapeutic outcome). These metrics vary dramatically between the two primary delivery paradigms—viral and non-viral vectors—each with distinct advantages and limitations. This guide provides a structured comparison of these delivery systems, supported by current experimental data and methodological protocols, to inform strategic decisions in therapeutic development.
Comparative Analysis of Delivery Vector Performance
The choice of delivery vector directly influences the critical performance metrics of a CRISPR therapeutic. The table below provides a quantitative comparison of the most widely used viral and non-viral delivery systems based on current research and clinical data.
Table 1: Performance Metrics of CRISPR Delivery Vectors
| Delivery Vector | Transfection Rate/Efficiency | Editing Specificity (On-target vs. Off-target) | Duration of Effect | Primary Cargo Form |
|---|---|---|---|---|
| Adeno-Associated Virus (AAV) | High for target tissues (e.g., liver, retina) [15] | High but prolonged expression may increase off-target risk [16] | Long-term (persistent episomal expression) [15] [17] | DNA [17] |
| Lentivirus (LV) | High for dividing and non-dividing cells [17] | Lower due to random genomic integration [17] | Permanent (integration into host genome) [17] | DNA [17] |
| Lipid Nanoparticle (LNP) | Variable; high for liver cells [18] [19] | Highest (transient activity reduces off-targets) [16] | Short-term (transient expression) [18] [16] | mRNA, RNP [17] [16] |
| Virus-Like Particle (VLP) | Promising in preclinical models [20] [21] | High (RNP delivery is transient) [17] | Short-term [17] | RNP [17] |
| Spherical Nucleic Acid (SNA) | 3x higher cell entry vs. standard LNP [19] | Improved precision, reduced toxicity [19] | Data emerging (likely transient) [19] | RNP, mRNA [19] |
Key Trade-offs and Decision Factors
The data in Table 1 reveals fundamental trade-offs. Viral vectors, particularly AAV, excel at achieving high transfection rates and sustained long-term effects, which is ideal for monogenic diseases requiring permanent correction [15] [17]. However, their prolonged activity can increase the potential for off-target effects, and their limited packaging capacity restricts the size of CRISPR machinery that can be delivered [15] [16]. In contrast, non-viral vectors like LNPs offer superior safety profiles with transient activity that minimizes off-target effects and avoids genome integration [18] [16]. Their primary limitation is their transient nature, which may necessitate re-dosing, and a current tendency to accumulate primarily in the liver [18] [17]. The recent development of LNP-SNAs demonstrates how novel nanotechnologies can significantly enhance transfection rates and specificity, pointing to a future where these trade-offs may be mitigated [19].
Experimental Protocols for Assessing Efficiency Metrics
Robust experimental validation is essential for quantifying the metrics described above. Below are detailed protocols for key assays used to evaluate delivery efficiency and editing outcomes.
Protocol 1: Quantifying Transfection Rate and Efficiency
Objective: To determine the percentage of cells that have successfully internalized CRISPR cargo. Methodology: This can be assessed using a PEG-mediated transfection of a GFP reporter plasmid into isolated protoplasts, as optimized for pea and adaptable to other cell types [22].
Materials:
- Target cells (e.g., cell line, primary cells, or protoplasts)
- GFP reporter plasmid
- Polyethylene Glycol (PEG) solution (e.g., 20-40%)
- Plasmid DNA (e.g., 20 µg)
- Flow cytometer or fluorescence microscope
Procedure:
- Isolate and purify target cells or protoplasts. For plant protoplasts, this involves enzymatic digestion of the cell wall with cellulase and macerozyme [22].
- Incubate the cells with the GFP plasmid and PEG solution. Optimal conditions from one study are 20 µg of plasmid DNA with 20% PEG for 15 minutes [22].
- Wash the cells to remove excess plasmid and PEG.
- Culture the transfected cells for 24-48 hours.
- Analyze using flow cytometry or fluorescence microscopy to count the percentage of GFP-positive cells. A well-optimized protocol can achieve transfection efficiencies of approximately 59% [22].
Protocol 2: Assessing Editing Specificity and On-target Efficiency
Objective: To confirm precise on-target editing and identify potential off-target effects. Methodology: A combination of next-generation sequencing (NGS) for on-target efficiency and specialized assays for off-target detection.
Materials:
- Genomic DNA from transfected cells
- PCR reagents and primers flanking the target site
- NGS platform
- Off-target prediction software (e.g., Cas-OFFinder)
- Methods like DISCOVER-Seq or targeted amplicon sequencing for suspected off-target sites [21]
Procedure:
- Extract genomic DNA from treated and control cells.
- Amplify the target locus using PCR with specific primers.
- Sequence the amplicons using NGS. The editing efficiency is calculated as the percentage of sequencing reads containing indels or precise edits at the target site. Efficiencies can exceed 90% in some systems [22].
- Predict potential off-target sites in silico using the gRNA sequence.
- Interrogate predicted off-target sites using methods like amplicon sequencing to quantify mis-editing. Novel tools like AutoDISCO are being developed to streamline this clinically [21].
Protocol 3: Evaluating the Duration of Effect
Objective: To measure the persistence of the genomic edit and its functional consequence over time. Methodology: Long-term tracking of edited cell populations and functional biomarkers in vivo.
Materials:
- Animal disease model
- Blood collection supplies
- ELISA kits for disease-specific proteins
- Equipment for functional assessments (e.g., echocardiogram)
Procedure:
- Administer the CRISPR therapeutic to an animal model.
- Collect serial samples (e.g., blood, tissue biopsies) over an extended period (months to years).
- Quantify the persistence of editing in genomic DNA from samples using digital PCR or NGS.
- Monitor a durable functional outcome. For example, in a trial for hereditary transthyretin amyloidosis (hATTR), a single dose of an LNP-delivered CRISPR therapy led to a ~90% reduction in the disease-related TTR protein that was sustained for over two years in all participants, demonstrating a long-lasting therapeutic effect from a transiently delivered editor [18].
Visualizing the CRISPR Delivery Workflow and Trade-offs
The following diagrams map the critical decision pathways and experimental workflows for evaluating CRISPR delivery systems.
CRISPR Delivery Vector Decision Pathway
Experimental Workflow for Efficiency Assessment
The Scientist's Toolkit: Essential Reagents and Solutions
Successful execution of the aforementioned protocols requires a suite of specialized reagents. The table below lists key solutions for researchers building a CRISPR delivery workflow.
Table 2: Essential Research Reagents for CRISPR Delivery and Evaluation
| Reagent / Solution | Function | Example Use Case |
|---|---|---|
| Polyethylene Glycol (PEG) | A chemical facilitator that induces DNA uptake by disrupting the cell membrane [22]. | PEG-mediated transfection of CRISPR constructs into plant protoplasts or hard-to-transfect mammalian cells [22]. |
| Ionizable Lipids | The key functional component of LNPs, enabling encapsulation of nucleic acids and endosomal escape upon cellular entry [17]. | Formulating LNPs to deliver CRISPR mRNA or RNPs for in vivo applications, particularly to the liver [18] [17]. |
| AAV Serotypes (e.g., AAV5, AAV9) | Engineered viral capsids with distinct tropisms for different tissues (e.g., retina, liver, CNS) [15]. | Selecting the optimal serotype (e.g., AAV5 for retinal delivery in EDIT-101) for targeted in vivo CRISPR therapy [15]. |
| Alt-R HDR Enhancer | A recombinant protein that increases the efficiency of homology-directed repair (HDR) without increasing off-target effects [20]. | Enhancing the rate of precise gene insertion or correction when co-delivered with a CRISPR system and a donor DNA template [20]. |
| Cell Strainers (40 μm) | Used to filter out undigested tissue and debris after enzymatic protoplast isolation, yielding a clean single-cell suspension [22]. | Purifying viable protoplasts post-isolation for subsequent transfection experiments [22]. |
| Enzyme Solutions (Cellulase/Macerozyme) | A cocktail of enzymes that digest plant cell walls to release naked protoplasts [22]. | Isating protoplasts from plant tissues like leaves for rapid, high-throughput testing of CRISPR reagent efficiency [22]. |
The strategic selection of a delivery vector is a cornerstone of successful CRISPR therapeutic development, as it directly dictates the triad of efficiency metrics: transfection rate, editing specificity, and duration of effect. Viral vectors like AAV offer the advantage of potent and sustained editing, making them suitable for diseases requiring a one-time, permanent cure, albeit with considerations for packaging limits and potential immunogenicity. Non-viral vectors, particularly LNPs, provide an excellent safety profile with high specificity and re-dosing capability, though their effects are transient and tropism is currently limited. Emerging technologies, such as LNPs engineered for selective organ targeting (SORT) and structurally enhanced nanoparticles like SNAs, are actively breaking these historical constraints, offering a future of more precise, efficient, and versatile CRISPR delivery systems. Researchers must therefore weigh these performance trade-offs against their specific therapeutic goals, using the standardized protocols and tools outlined here, to navigate the complex and rapidly evolving landscape of CRISPR delivery.
The therapeutic application of CRISPR-Cas9 technology represents a frontier in modern medicine, offering potential cures for a range of genetic disorders. Its clinical translation, however, is contingent on the efficient and safe delivery of CRISPR components into target cells. Delivery vectors are broadly categorized into viral and non-viral systems, each with distinct profiles of advantages and limitations. For researchers and drug development professionals, the critical challenges of immunogenicity, cargo size limitations, and off-target effects often dictate the choice of delivery platform. This guide provides an objective comparison of viral and non-viral vector efficiency, synthesizing current experimental data and methodologies to inform strategic decisions in therapeutic development.
Core Challenges in CRISPR Delivery Vector Efficiency
Immunogenicity
The immune response elicited by a delivery vector can compromise both the safety and efficacy of a CRISPR therapy. Viral vectors, due to their biological origin, often pose a higher risk.
- Viral Vectors: Adeno-associated viruses (AAVs) are favored for their relatively low immunogenicity compared to other viral vectors. They are not known to cause disease in humans and typically provoke mild immune responses [23] [17]. However, pre-existing immunity in human populations remains a concern, and AAVs can still trigger dose-limiting inflammatory responses [23] [15]. In contrast, adenoviral vectors (AdVs) and lentiviral vectors (LVs) are more immunogenic. AdVs are known to cause strong immune reactions, while LVs, with an HIV-derived backbone, present significant safety implications that limit their in vivo use [17] [9].
- Non-Viral Vectors: Systems like lipid nanoparticles (LNPs) and polymeric nanoparticles generally exhibit minimal safety and immunogenicity concerns due to the absence of viral components [17] [24]. Their synthetic nature makes them less recognizable to the immune system. A key clinical advantage of LNPs, as demonstrated in trials for hereditary transthyretin amyloidosis (hATTR) and a personalized therapy for CPS1 deficiency, is the possibility of redosing without the severe immune reactions typically associated with viral vector re-administration [18].
Cargo Size Limitations
The packaging capacity of a vector is crucial for delivering the relatively large CRISPR-Cas9 system.
- Viral Vectors: The ~4.7 kb packaging capacity of AAVs is a major constraint. The commonly used Streptococcus pyogenes Cas9 (SpCas9) is approximately 4.2 kb, leaving insufficient space for additional essential elements like promoters and guide RNA(s) [23] [15]. This has spurred the development of innovative workarounds, such as:
- Non-Viral Vectors: Nanocarriers such as LNPs, gold nanoparticles (AuNPs), and extracellular vesicles (EVs) do not face the same strict size limitations as AAVs [17] [25]. They can be engineered to accommodate various forms of CRISPR cargo—plasmid DNA, mRNA, or ribonucleoprotein (RNP) complexes—without being constrained by a fixed payload size [24] [25]. This flexibility allows for the delivery of larger CRISPR systems or multiple editing components simultaneously.
Off-Target Effects
Off-target effects refer to unintended edits at genomic sites with sequences similar to the target, a key concern for therapeutic safety.
- Viral Vectors: Vectors like AAVs and LVs often lead to prolonged expression of the Cas9 nuclease because they maintain the editing machinery inside cells for an extended period (via episomal persistence or genomic integration). This sustained activity increases the window for off-target cleavage [23] [9].
- Non-Viral Vectors: Delivery of pre-assembled ribonucleoprotein (RNP) complexes is associated with the lowest off-target effects. RNP activity is transient, as the complex is rapidly degraded by cellular proteases, minimizing the time for unintended edits to occur [17] [9]. This transient nature is a primary reason why the first FDA-approved CRISPR therapy, Casgevy for sickle cell disease, utilizes RNP delivery via electroporation ex vivo [9].
Table 1: Comparative Profile of Viral and Non-Viral Delivery Vectors
| Challenge | Vector Type | Key Characteristics | Experimental Evidence & Clinical Context |
|---|---|---|---|
| Immunogenicity | Viral (AAV) | Low to moderate immunogenicity; pre-existing immunity is a concern; re-dosing is typically not possible. | Clinical trials for hATTR (NCT04601051) show manageable immune responses, but high doses can trigger inflammation [18] [15]. |
| Viral (Lentivirus) | Moderate immunogenicity; safety concerns due to genomic integration. | Primarily used ex vivo; FDA-approved for CAR-T therapies (e.g., Kymriah) but not for in vivo CRISPR delivery [17] [9]. | |
| Non-Viral (LNP) | Low immunogenicity; enables re-dosing. | Successful redosing demonstrated in a Phase I hATTR trial and a personalized CPS1 deficiency case with no serious side effects [18]. | |
| Cargo Size Limitations | Viral (AAV) | Strict ~4.7 kb limit. | Strategies to overcome this: SaCas9 (3.2 kb) showed therapeutic efficacy in mouse models; dual-AAV systems for SpCas9 are in development [15]. |
| Non-Viral (Nanocarriers) | High flexibility; no strict size limit. | LNPs successfully deliver Cas9 mRNA (>>4.7 kb) for in vivo editing in liver targets [18] [24]. | |
| Off-Target Effects | Viral (AAV/Lentivirus) | Sustained Cas9 expression; higher risk of off-target edits. | In vivo studies show persistent Cas9 expression for weeks; inducible systems can help mitigate this [23] [9]. |
| Non-Viral (RNP) | Transient activity; fastest clearance; lowest off-target risk. | NGS-based assays (GUIDE-seq) show RNP delivery reduces off-targets compared to plasmid DNA delivery [17] [26] [9]. |
Experimental Protocols for Assessing Key Challenges
Protocol for Evaluating Immunogenicity
Objective: To quantify innate and adaptive immune responses to a CRISPR delivery vector in a murine model. Methodology:
- Administration: Systemically administer the CRISPR-loaded vector (e.g., AAV8 or LNP) to mice via tail-vein injection. Include a control group receiving empty vector or buffer.
- Sample Collection: Collect blood and tissue (e.g., liver, spleen) samples at 6, 24, and 72 hours post-injection, and again at 1-2 weeks.
- Cytokine Analysis: Use a multiplex cytokine ELISA on serum to quantify pro-inflammatory cytokines (e.g., IL-6, TNF-α, IFN-γ). A significant increase indicates activation of the innate immune system.
- Immune Cell Profiling: Isolate immune cells from the spleen and liver. Use flow cytometry to characterize immune cell populations (e.g., T-cells, B-cells, macrophages, neutrophils) and their activation states.
- Antibody Detection: At later time points (e.g., 2 weeks), use an enzyme-linked immunosorbent assay (ELISA) to detect the presence of neutralizing antibodies (NAbs) against the vector (e.g., AAV capsid) or the Cas9 protein itself.
Protocol for Testing Cargo Delivery Efficiency
Objective: To assess the functional delivery of CRISPR components and subsequent editing efficiency. Methodology:
- In Vitro Transduction/Transfection: Deliver the CRISPR vector (e.g., AAV, LNP-RNP) to cultured target cells.
- Genomic DNA Extraction: Harvest cells 72-96 hours post-delivery and extract genomic DNA.
- Editing Efficiency Analysis:
- T7 Endonuclease I Assay: PCR-amplify the target genomic region. Digest the heteroduplexed PCR product with T7EI, which cleaves DNA at mismatched bases. Analyze fragments by gel electrophoresis; the ratio of cleaved to uncleaved products indicates editing efficiency.
- Next-Generation Sequencing (NGS): For a more quantitative and comprehensive measurement, amplify the target region and subject it to NGS. The percentage of reads containing insertions or deletions (indels) at the target site provides a precise measure of editing efficiency.
Protocol for Detecting Off-Target Effects
Objective: To identify and quantify unintended genomic edits genome-wide. Methodology:
- Cell Treatment: Treat cells with the CRISPR delivery system.
- Genome-Wide Profiling: Use an advanced sequencing-based method to identify potential off-target sites. GUIDE-seq is a widely adopted method:
- A short, double-stranded oligonucleotide tag is introduced into cells alongside the CRISPR system during transfection. This tag is incorporated into DSBs generated by Cas9.
- Genomic DNA is extracted and subjected to NGS. The locations of tag integration reveal potential off-target cleavage sites across the entire genome [26].
- Validation: Potential off-target sites identified by GUIDE-seq are validated by targeted amplicon sequencing to confirm and quantify the frequency of indels at those loci.
Visualization of Vector Challenges and Solutions
The following diagram illustrates the key challenges and primary strategies for both viral and non-viral CRISPR delivery systems.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents and Tools for CRISPR Delivery Research
| Item | Function/Description | Example Use Case |
|---|---|---|
| SpCas9 Plasmid | Expresses the full-length Cas9 nuclease from S. pyogenes. Used for stable, long-term editing. | Creating stable cell lines for gene knockout studies [23] [9]. |
| SaCas9 Plasmid | A compact Cas9 variant (~1 kb smaller than SpCas9). Essential for AAV-based delivery. | Packaging into a single AAV vector for in vivo gene therapy applications [15]. |
| Cas9 mRNA | In vitro transcribed mRNA for Cas9 translation. Offers transient expression. | Delivery via LNPs for in vivo editing with reduced off-target risk compared to plasmids [9]. |
| Ribonucleoprotein (RNP) | Pre-complexed Cas9 protein and sgRNA. Provides immediate, transient activity with high specificity. | Gold-standard for ex vivo editing (e.g., Casgevy); delivered via electroporation [17] [9]. |
| Lipid Nanoparticles (LNPs) | Synthetic nanocarriers for encapsulating and delivering nucleic acids (DNA, mRNA) or RNPs. | Leading platform for systemic, in vivo non-viral delivery, particularly to the liver [18] [24]. |
| AAV Serotype Library | Different AAV capsids (e.g., AAV2, AAV8, AAV9) with varying tissue tropisms. | Screening for optimal transduction efficiency in a specific target tissue (e.g., liver, muscle, CNS) [15] [9]. |
| GUIDE-seq Kit | A complete reagent set for genome-wide identification of off-target cleavage sites. | Profiling the safety and specificity of a novel gRNA or delivery method [26]. |
| T7 Endonuclease I | An enzyme that cleaves mismatched heteroduplex DNA. | A cost-effective and rapid method for initial assessment of on-target editing efficiency [25]. |
The choice between viral and non-viral delivery vectors for CRISPR therapeutics involves a critical trade-off between efficiency and safety. Viral vectors, particularly AAVs, offer high transduction efficiency and durable expression but are constrained by immunogenicity and cargo size. Non-viral vectors, especially LNPs delivering RNP or mRNA, provide superior safety, reduced immunogenicity, and transient activity but often require optimization for delivery efficiency beyond the liver. The evolving landscape, marked by the first approved therapies and advanced clinical trials, indicates a future where the selection of a delivery system will be highly tailored to the specific disease, target tissue, and desired duration of therapy. Innovations in vector engineering, such as novel AAV capsids and smart non-viral nanomaterials, continue to push the boundaries toward safer and more effective CRISPR-based medicines.
Delivery in Action: Viral and Non-Viral Vector Mechanisms and Workflows
The advancement of CRISPR-based therapeutics is intrinsically linked to the development of efficient and safe delivery vectors. Viral vectors, particularly Adeno-Associated Virus (AAV), Lentivirus (LV), and Adenovirus (Ad), have emerged as the primary vehicles for transporting CRISPR machinery into target cells. These vectors offer distinct advantages and limitations based on their structural biology, tropism, and genomic integration capabilities. The selection of an appropriate viral vector is a critical determinant in the success of gene editing experiments and therapies, influencing factors such as editing efficiency, specificity, duration of expression, and immunogenic response. This guide provides a objective comparison of these three viral vector systems, focusing on their application in CRISPR therapeutics research for scientists and drug development professionals.
Vector Characteristics and Comparative Analysis
The fundamental biological and functional characteristics of AAV, Lentivirus, and Adenovirus directly inform their suitability for specific research applications.
Core Structural and Functional Properties
Adeno-Associated Virus (AAV): AAV is a small, non-enveloped virus with a single-stranded DNA genome of approximately 4.7 kb, flanked by inverted terminal repeats (ITRs) that are essential for genome packaging and replication [27] [28]. Its icosahedral capsid, composed of VP1, VP2, and VP3 proteins, determines serotype-specific tissue tropism [27]. AAV is replication-deficient and requires helper virus functions (typically from adenovirus) for productive infection. For recombinant AAV (rAAV) production, the native
repandcapgenes are replaced with the therapeutic transgene cassette, resulting in a vector that persists primarily as episomal DNA in the host cell nucleus, enabling long-term transgene expression without integration-related risks [28].Lentivirus (LV): Lentiviruses are enveloped viruses belonging to the retrovirus family, characterized by an RNA genome that is reverse-transcribed into DNA upon host cell entry [29]. The viral core is often conical or bullet-shaped and houses the genome along with essential enzymes like reverse transcriptase and integrase [27]. A key feature of recombinant Lentiviral vectors (rLVs) is their ability to infect both dividing and non-dividing cells. Their genome integrates into the host chromosome, facilitating long-term transgene expression, which is particularly valuable for ex vivo cell engineering applications [29]. Lentiviral vectors are commonly pseudotyped with the vesicular stomatitis virus G-glycoprotein (VSV-G) to broaden cellular tropism and enhance particle stability [29] [30].
Adenovirus (Ad): Adenovirus is a non-enveloped, double-stranded DNA virus with a larger native genome (~36 kb) and an icosahedral capsid [31]. The capsid features fiber proteins that mediate initial attachment to host cell receptors. Adenoviral vectors are characterized by high transduction efficiency across a wide range of dividing and non-dividing cells and can accommodate large transgene payloads (up to approximately 37 kb in helper-dependent "gutted" vectors). They remain episomal in the nucleus and do not integrate into the host genome, leading to robust but transient transgene expression due to eliciting strong cellular immune responses against transduced cells [31].
Quantitative Comparison of Key Parameters
The table below summarizes the critical characteristics of AAV, Lentivirus, and Adenovirus vectors for direct comparison.
Table 1: Comparative Analysis of Major Viral Vector Systems
| Parameter | Adeno-Associated Virus (AAV) | Lentivirus (LV) | Adenovirus (Ad) |
|---|---|---|---|
| Genome Type | Single-stranded DNA | Single-stranded RNA (reverse transcribed to DNA) | Double-stranded DNA |
| Packaging Capacity | ~4.7 kb [27] | 8-12 kb [27] | ~8 kb (1st/2nd gen.); up to ~37 kb (helper-dependent) |
| Genomic Integration | Predominantly episomal [27] | Integrates into host genome [29] | Episomal [31] |
| Transgene Expression Duration | Long-term (months to years) [28] | Long-term (stable in dividing cells due to integration) [29] | Short-term (days to weeks) due to immune clearance |
| Typical Applications | In vivo gene therapy, CRISPR delivery to non-dividing cells (e.g., neurons, retina) [32] [33] | Ex vivo cell engineering (e.g., CAR-T, HSCs), in vivo delivery to dividing/non-dividing cells [29] | Vaccines, oncolytic therapy, transient gene expression, large gene delivery [31] |
| Primary Tropism/ Targeting | Serotype-dependent (e.g., AAV9 for CNS, AAV5 for lungs, AAV8 for liver) [27] [34] | Broad (can be pseudotyped, e.g., VSV-G for wide tropism) [29] | Broad native tropism; can be retargeted using antibody conjugates [31] |
| Immunogenicity | Relatively low; pre-existing antibodies common [29] | Moderate | High; limits repeat administration |
| Production Yield | Challenging; lower yields, issue of empty capsids [27] [35] | High production yields [27] | Very high titers achievable |
Application in CRISPR-Cas9 Delivery
The delivery of CRISPR-Cas9 components—typically the Cas nuclease and guide RNA (gRNA)—poses specific challenges and requirements that are met differently by each vector system.
Performance in CRISPR Workflows
AAV for CRISPR: AAV's small packaging capacity is its primary limitation for CRISPR delivery. A single AAV vector cannot package the coding sequence for the commonly used Streptococcus pyogenes Cas9 (SpCas9, ~4.2 kb) along with its gRNA and necessary promoters. Researchers employ strategies to overcome this, including:
- Dual AAV Systems: The Cas9 and gRNA expression cassettes are split across two separate AAV vectors [32].
- Smaller Cas Orthologs: Using smaller Cas proteins like Staphylococcus aureus Cas9 (SaCas9) or Cas13d that can fit into a single AAV particle with their gRNA [34] [33].
- All-in-one Systems: For smaller CRISPR systems, a single vector can deliver all components for applications like gene knockdown [34]. AAV is the leading platform for in vivo CRISPR delivery due to its ability to transduce non-dividing cells and mediate long-term expression from a single administration, which is crucial for therapeutic applications in tissues like the CNS and retina [33] [28].
Lentivirus for CRISPR: Lentivirus's larger cargo capacity readily accommodates both SpCas9 and single or multiple gRNAs within a single "all-in-one" vector, simplifying experimental workflows [27] [29]. Its integrating nature ensures persistent expression of CRISPR components, which is desirable for long-term gene disruption in dividing cells or for genetic screens. However, sustained Cas9 expression increases the potential for off-target effects and immune responses. Lentiviral vectors are predominantly used for ex vivo CRISPR applications, such as engineering CAR-T cells or creating stable knockout cell lines, where their ability to transduce a wide variety of cell types is advantageous [29] [30].
Adenovirus for CRISPR: Adenovirus can easily package the full SpCas9 and gRNA expression cassette, making it a straightforward tool for CRISPR delivery. It provides high transduction efficiency and very rapid transgene expression. However, its high immunogenicity and transient expression profile make it less suitable for therapeutic applications requiring long-term editing but potentially useful for transient genetic manipulations or in immuno-oncology contexts [31].
Quantitative Data and Experimental Evidence
Recent studies highlight the performance of these vectors in specific CRISPR applications.
Table 2: Experimental Data from Recent CRISPR Delivery Studies
| Vector / System | CRISPR Application | Model System | Key Performance Metric | Result | Citation |
|---|---|---|---|---|---|
| AAV.CPP.16 | Delivery of CRISPR-Cas13d to inhibit SARS-CoV-2 Rdrp gene | Mouse (intranasal) | Prophylaxis against SARS-CoV-2 infection | Significant inhibition of viral gene transcription | [34] |
| Lentivirus (IDLV) | gRNA delivery (with separate Cas9 mRNA) | 293T cells ( in vitro ) | Gene editing efficiency | Highly efficient, but induced significant anti-Cas9 IgG in vivo | [30] |
| Virus-Like Particle (RIDE) | CRISPR RNP delivery for Vegfa knockout | Mouse (subretinal) | Indel frequency in RPE | 38% indel frequency; 43% decrease in choroidal neovascularization area | [30] |
| AAV vs. LNP | General CRISPR modality delivery | N/A | Key differentiators | AAV: Sustained expression, broad tropism. LNP: Transient, good for liver targets. | [32] |
Detailed Experimental Workflows
A critical understanding of viral vector production and transduction protocols is essential for experimental success and data reproducibility.
AAV Vector Production and Purification
The most common method for research-scale AAV production is transient transfection of HEK293 cells using a three-plasmid system [27] [32] [35].
Protocol: AAV Production via HEK293 Transient Transfection
Plasmid Transfection: HEK293 cells (adherent or suspension) are co-transfected with three plasmids:
- Transfer Plasmid: Contains the transgene (e.g., Cas9 or gRNA) flanked by AAV Inverted Terminal Repeats (ITRs).
- Packaging Plasmid: Provides the AAV
repandcapgenes. Thecapgene determines the serotype. - Helper Plasmid: Supplies essential adenoviral genes (E2A, E4, VA RNA) required for AAV replication. Transfection is typically performed using polyethylenimine (PEI) or other commercial reagents [27] [35].
Harvest and Lysis: 48-72 hours post-transfection, cells and media are harvested. The cell pellet is lysed to release the packaged AAV particles.
Purification: The crude lysate is treated with nucleases to degrade unprotected nucleic acids. AAV is then purified using methods such as:
- Ultracentrifugation: Iodixanol density gradient centrifugation is a common research-scale method [27].
- Chromatography: Affinity or ion-exchange chromatography is used for higher purity and is more scalable for manufacturing. This step is critical for removing empty capsids (a key product-related impurity) [32] [35].
Formulation and QC: The purified virus is concentrated and dialyzed into a suitable buffer (e.g., PBS). Rigorous quality control is performed, including:
Diagram 1: AAV production workflow.
Lentiviral Vector Production
Lentiviral vector production also relies on transient transfection of HEK293 cells, typically with a three- or four-plasmid system designed to enhance safety by minimizing the chance of generating replication-competent viruses [27] [29].
Protocol: Third-Generation Lentivirus Production
Plasmid Transfection: HEK293T cells are co-transfected with:
- Transfer Plasmid: Contains the gene of interest (e.g., all-in-one CRISPR construct) flanked by Long Terminal Repeats (LTRs).
- Packaging Plasmid(s): Provides the gag-pol genes (structural proteins and enzymes). In third-generation systems, the
revgene is often on a separate plasmid. - Envelope Plasmid: Encodes the heterologous envelope glycoprotein, most commonly VSV-G, which confers broad tropism [27] [29].
Vector Harvest: Viral supernatant is collected 48 and 72 hours post-transfection, filtered to remove cell debris, and often concentrated via ultracentrifugation or tangential flow filtration.
Titering and QC: Functional titer is determined by transducing target cells and measuring transgene expression (e.g., by flow cytometry for a fluorescent marker) or by qPCR for vector copies integrated into the genome.
Diagram 2: Lentivirus production workflow.
The Scientist's Toolkit: Essential Research Reagents
Successful viral vector production and CRISPR application depend on key reagents and cell lines.
Table 3: Essential Reagents for Viral Vector & CRISPR Research
| Reagent / Material | Function in Workflow | Specific Examples & Notes |
|---|---|---|
| HEK293T Cells | Producer cell line for AAV and LV | Readily transfectable, derived from human embryonic kidney cells; "T" denotes expression of SV40 Large T-antigen [35]. |
| Packaging Plasmids | Provide essential viral genes in trans | AAV: Rep/Cap and Helper plasmids. LV: 2nd/3rd gen gag-pol, rev, VSV-G plasmids. Critical for safety and yield [27]. |
| Transfer Plasmid | Carries the therapeutic/editing cargo | Contains ITRs (for AAV) or LTRs (for LV) flanking the expression cassette for Cas9, gRNA, or a reporter gene [27] [32]. |
| Transfection Reagent | Introduces plasmids into producer cells | Polyethylenimine (PEI) is widely used due to its cost-effectiveness and efficiency with HEK293 cells [35]. |
| Purification Resins/Medium | Isolation and purification of viral vectors | Iodixanol for gradient ultracentrifugation; affinity resins (e.g., AVB Sepharose for AAV) for chromatography [27] [35]. |
| Target Cells/Animal Models | For functional validation of vectors | Primary cells or cell lines; disease-specific animal models (e.g., mouse models of IPF [34] or Huntington's disease [30]). |
| Titer & QC Assays | Quantification and quality assessment | qPCR (genome titer), TCID50 or flow cytometry (functional titer), SDS-PAGE/Western (purity), ELISA (empty/full capsids) [32] [35]. |
AAV, Lentivirus, and Adenovirus each occupy a distinct niche in the CRISPR delivery landscape. AAV is the vector of choice for direct in vivo gene editing applications requiring long-term expression in non-dividing cells, despite its packaging constraints. Lentivirus excels in ex vivo cell engineering and applications where stable genomic integration is beneficial. Adenovirus offers high transduction efficiency and large cargo capacity but is limited by immunogenicity. The choice of vector is not one-size-fits-all and must be tailored to the specific experimental or therapeutic goal, considering the trade-offs between payload size, persistence of expression, immunogenicity, and tropism. Emerging technologies like engineered virus-like particles (VLPs) for transient RNP delivery are showing promise in addressing limitations of current viral vectors, such as pre-existing immunity and long-term nuclease expression [30]. As the field advances, continued optimization of production workflows to increase yield and purity, coupled with sophisticated capsid and envelope engineering for precise targeting, will further solidify the role of viral vectors in enabling the next generation of CRISPR therapeutics.
The advent of CRISPR-Cas9 technology has revolutionized biomedical research and therapeutic development, offering unprecedented precision in manipulating genetic material. However, the clinical translation of CRISPR-based therapies faces a significant bottleneck: the efficient and safe delivery of genome-editing components into target cells [24]. Delivery vectors are broadly categorized into viral and non-viral systems. While viral vectors, such as adeno-associated viruses (AAVs), offer high transduction efficiency, they present considerable challenges, including immunogenicity, limited packaging capacity, and potential for insertional mutagenesis [36] [15]. These limitations have accelerated the development of non-viral delivery platforms, which offer improved safety profiles, larger payload capacity, and reduced risk of off-target effects [24] [17].
Among the diverse non-viral strategies, three platforms have emerged as frontrunners: Lipid Nanoparticles (LNPs), Electroporation, and Polymeric Nanocarriers. These "non-viral champions" are distinguished by their unique mechanisms, applications, and performance characteristics. LNPs, validated by their successful deployment in mRNA COVID-19 vaccines, excel in in vivo delivery [37]. Electroporation, a physical method, achieves high efficiency in ex vivo settings, notably in approved therapies like Casgevy for sickle cell disease [18]. Polymeric Nanocarriers, with their highly tunable chemical structures, offer versatile nucleic acid condensation and potential for sophisticated functionalization [36] [2]. This guide provides a objective, data-driven comparison of these three leading non-viral delivery systems, framing their performance within the critical context of viral versus non-viral delivery efficiency for CRISPR therapeutics.
Performance Comparison of Non-Viral Delivery Systems
The following tables summarize the key characteristics and quantitative performance metrics of the three champion non-viral delivery systems, based on current literature and experimental data.
Table 1: Key Characteristics and Applications
| Delivery System | Primary Mechanism | Best Suited Application | CRISPR Cargo Format | Key Advantages |
|---|---|---|---|---|
| Lipid Nanoparticles (LNPs) | Encapsulation and fusion with cell membranes [37] | In vivo delivery (e.g., systemic IV injection) [18] | mRNA, RNP [17] | Proven clinical success; innate liver tropism; suitable for redosing [18] |
| Electroporation | Electrical pulses create transient pores in cell membrane [17] | Ex vivo delivery (e.g., hematopoietic stem cells) [18] | RNP, mRNA [17] | High efficiency for hard-to-transfect cells; direct cytoplasmic delivery [17] |
| Polymeric Nanocarriers | Electrostatic condensation into "polyplexes" [36] [2] | In vitro and in vivo delivery (under development) | DNA, RNP, mRNA [2] | Highly tunable structure; high buffering capacity for endosomal escape [36] [2] |
Table 2: Quantitative Performance Metrics from Experimental Studies
| Delivery System | Reported Editing Efficiency | Cell Viability Post-Delivery | Throughput / Scalability | Key Challenges |
|---|---|---|---|---|
| Lipid Nanoparticles (LNPs) | ~90% protein reduction in hATTR trial [18] | Mild to moderate infusion-related reactions [18] | High scalability for clinical manufacturing [38] | Endosomal entrapment; limited targeting beyond liver [17] |
| Electroporation | High efficiency in clinical ex vivo editing [18] | Significant cytotoxicity if parameters not optimized [17] | Lower throughput, more suited for ex vivo use [17] | High cell mortality; requires specialized equipment [17] |
| Polymeric Nanocarriers | >40% genomic deletion in RDEB keratinocytes with RNP [2] | Viability maintained >80% with optimized HPAE-EB polymer [2] | Facile synthesis, but batch-to-batch variation can occur [38] | Can struggle with complexation stability and payload release [38] |
Experimental Protocols and Workflows
To ensure reproducibility and provide a practical resource, this section outlines standard experimental protocols for evaluating each of the three non-viral champion systems.
Lipid Nanoparticle (LNP) Formulation and Testing
Objective: To formulate LNPs encapsulating CRISPR-RNP and evaluate their editing efficiency in vitro.
- Step 1: LNP Formulation. Prepare lipid mixtures typically containing an ionizable cationic lipid, phospholipid, cholesterol, and PEG-lipid in ethanol [37]. The ionizable lipid is crucial for endosomal escape [37]. Mix the lipid solution with an aqueous buffer containing the CRISPR-RNP complex using rapid mixing techniques, such as microfluidics, to form uniform LNPs ~100 nm in size [38].
- Step 2: Characterization. Dilute the formed LNPs in phosphate-buffered saline (PBS). Use Dynamic Light Scattering (DLS) to measure particle size, polydispersity index (PDI), and zeta potential. Determine encapsulation efficiency using a Ribogreen assay [37].
- Step 3: In Vitro Transfection. Seed target cells (e.g., HEK293 or hepatocytes) in a 24-well plate. Add LNP formulations at various lipid-to-RNP weight ratios. Incubate for 48-72 hours [24].
- Step 4: Efficacy and Safety Assessment. Harvest cells and extract genomic DNA. Assess editing efficiency via T7E1 assay or next-generation sequencing. Evaluate cell viability using a colorimetric assay (e.g., MTT or Alamar Blue) [2].
LNP Experimental Workflow: The process for formulating and testing Lipid Nanoparticles.
Electroporation Protocol for Ribonucleoprotein (RNP) Delivery
Objective: To deliver CRISPR-RNP complexes into cells ex vivo using electroporation for high-efficiency genome editing.
- Step 1: RNP Complex Formation. Reconstitute purified Cas9 protein and synthetic sgRNA. To form the RNP complex, incubate Cas9 with sgRNA at a molar ratio of 1:6.6 (Cas9:sgRNA) for 10-20 minutes at room temperature [2].
- Step 2: Cell Preparation. Harvest the target cells (e.g., hematopoietic stem cells or T-cells) and wash with an electroporation buffer. Resuspend the cells at a high concentration (e.g., 10-20 million cells per mL) [17].
- Step 3: Electroporation. Mix the cell suspension with the pre-formed RNP complex. Transfer the mixture to an electroporation cuvette. Apply an optimized electrical pulse using a specialized electroporator (e.g., Lonza 4D-Nucleofector). The specific program (pulse voltage, length, and number) must be empirically determined for each cell type [17].
- Step 4: Post-Transfection Recovery. Immediately after electroporation, add pre-warmed culture medium and transfer the cells to a culture plate. Incubate the cells for 48-72 hours before analyzing editing efficiency and viability [17].
Polymeric Nanocarrier Polyplex Formation and Transfection
Objective: To form polyplexes using a cationic polymer for the delivery of CRISPR plasmid DNA and assess transfection performance.
- Step 1: Polymer Synthesis and Preparation. Synthesize cationic polymers like Highly Branched Poly(beta-amino ester) (HPAE-EB) as described in the literature [2]. Dissolve the polymer in sodium acetate buffer (25 mM, pH 5.2) [2].
- Step 2: Polyplex Formation. Dilute the CRISPR cargo (e.g., plasmid DNA encoding Cas9 and gRNA) in the same sodium acetate buffer. Mix the polymer and DNA solutions at a 1:1 volume ratio at pre-optimized weight/weight (w/w) ratios. Vortex the mixture for 30 seconds and incubate at room temperature for 10-30 minutes to allow polyplex formation [2].
- Step 3: Biophysical Characterization. Measure the hydrodynamic diameter and zeta potential of the polyplexes using DLS. Confirm complexation and nucleic acid protection via gel electrophoresis retardation assay [2].
- Step 4: Cell Transfection and Analysis. Add the polyplexes to cells (e.g., HEK293 or primary keratinocytes) at 60-70% confluence. Replace the medium after 4 hours. After 48 hours, analyze transfection efficiency (e.g., via GFP expression if using a reporter plasmid) and gene editing efficacy (via T7E1 assay). Evaluate cell viability 48 hours post-transfection [2].
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of non-viral CRISPR delivery requires a suite of essential reagents and materials. The following table details key components and their functions.
Table 3: Essential Reagents for Non-Viral CRISPR Delivery Research
| Reagent / Material | Function / Purpose | Examples / Notes |
|---|---|---|
| CRISPR-Cas9 RNP | The active editing machinery; pre-complexing reduces off-target effects [2] | HiFi Cas9 Nuclease; custom synthetic sgRNA or crRNA+tracrRNA [2] |
| Ionizable Cationic Lipids | Core component of LNPs; enables nucleic acid complexation and endosomal escape [37] | DLin-MC3-DMA; SM-102; ALC-0315 [37] |
| Cationic Polymers | Condense nucleic acids via electrostatic interactions to form polyplexes [36] [2] | Highly Branched Poly(β-amino ester) (HPAE-EB); Polyethylenimine (PEI) [36] [2] |
| Helper Lipids | Stabilize LNP structure and enhance performance [37] | Cholesterol (stability); DSPC (structural lipid); PEG-lipids (reduce opsonization) [37] |
| Electroporation Buffer | Environment for cells during electrical pulse; formulation is critical for viability [17] | Cell-type specific buffers; often proprietary to instrument manufacturers [17] |
| Sodium Acetate Buffer | Diluent for polymer and DNA for polyplex formation; optimal at pH ~5.2 [2] | 25 mM concentration is commonly used [2] |
The landscape of CRISPR delivery is no longer dominated solely by viral vectors. Lipid Nanoparticles, Electroporation, and Polymeric Nanocarriers have each demonstrated champion-level capabilities in specific domains. LNPs are the leading platform for in vivo therapeutic delivery, as evidenced by clinical trials. Electroporation remains the gold standard for high-efficiency ex vivo editing of challenging primary cells. Polymeric Nanocarriers offer a highly customizable and promising alternative, with ongoing research focused on improving their efficacy and specificity.
The choice between these systems is not a matter of identifying a single winner, but of matching the tool to the task. Researchers must consider the target cells (in vivo vs. ex vivo), the desired editing window (transient vs. sustained), and the specific cargo (DNA, mRNA, or RNP) when selecting a delivery platform. As these non-viral technologies continue to mature and converge—for instance, in the development of hybrid lipid-polymer systems—their collective potential to unlock the full therapeutic promise of CRISPR gene editing will only expand.
The therapeutic application of CRISPR gene editing is primarily advanced through two distinct delivery paradigms: ex vivo and in vivo editing. The fundamental distinction lies in the site where genetic modification occurs. Ex vivo editing involves harvesting cells from a patient, genetically modifying them outside the body using CRISPR, and then reinfusing the edited cells back into the patient [39]. In contrast, in vivo editing entails the direct administration of the CRISPR therapeutic agent (e.g., viral vectors, lipid nanoparticles) into the patient's body to edit the DNA of target cells in situ [39] [40].
The choice between these paradigms is a cornerstone of therapeutic design and is intrinsically linked to the broader thesis on viral versus non-viral delivery vector efficiency. This guide provides an objective comparison of these workflows, supported by experimental data and detailed protocols, to inform researchers and drug development professionals.
Ex Vivo Gene Editing: The CASGEVY Model
Clinical Workflow and Protocol
Ex vivo CRISPR therapy, exemplified by Casgevy (exagamglogene autotemcel), involves a multi-step, centralized process [39]. The following workflow diagram outlines the key stages from cell collection to patient reinfusion.
The clinical protocol for Casgevy, as established in the CLIMB-111, CLIMB-121, and CLIMB-131 trials, involves [39]:
- HSC Collection & Shipment: CD34+ hematopoietic stem and progenitor cells are collected from the patient via apheresis and shipped to a specialized manufacturing facility.
- CRISPR-Cas9 Editing: At the facility, cells are electroporated with CRISPR-Cas9 ribonucleoprotein (RNP) complexes targeting the BCL11A gene to disrupt its expression and induce fetal hemoglobin production.
- Patient Conditioning: While cells are being edited, the patient undergoes myeloablative conditioning with busulfan to clear bone marrow space for the edited cells.
- Reinfusion: The CRISPR-edited CD34+ cells are infused back into the patient.
- Engraftment: The edited cells engraft in the bone marrow and begin producing red blood cells with elevated fetal hemoglobin levels.
Key Research Reagents and Solutions
Table 1: Essential Reagents for Ex Vivo CRISPR Workflows
| Research Reagent | Function in Protocol | Example/Specification |
|---|---|---|
| CRISPR RNP Complex | The active editing machinery; Cas9 protein pre-complexed with sgRNA. | High-fidelity Cas9 (e.g., SpyFi Cas9) and sgRNA targeting the gene of interest (e.g., BCL11A). |
| CD34+ Cell Isolation Kit | To purify hematopoietic stem cells from apheresis product. | Immunomagnetic bead-based separation (e.g., CliniMACS system). |
| Electroporation System | Physical method to deliver RNP complexes into hard-to-transfect HSCs. | Neon Transfection System or Lonza 4D-Nucleofector. |
| Stem Cell Culture Media | Supports viability and potency of HSCs during the editing process. | Serum-free media supplemented with cytokines (e.g., SCF, TPO, FLT3-L). |
In Vivo Gene Editing: The Lipid Nanopipeline
Clinical Workflow and Mechanism of Action
In vivo editing simplifies the clinical pathway for the patient by directly administering the CRISPR therapy. The mechanism relies on sophisticated delivery vectors to reach and edit specific cells inside the body. The process for a systemically administered LNP-based therapy is detailed below.
A representative protocol from an ongoing clinical trial for hereditary transthyretin amyloidosis (hATTR) using Intellia Therapeutics' NTLA-2001 illustrates this paradigm [18]:
- Formulation: The CRISPR payload, consisting of mRNA for the Cas9 protein and a guide RNA targeting the TTR gene, is encapsulated in liver-tropic lipid nanoparticles (LNPs).
- Administration: A single dose of the LNP formulation is administered to the patient via intravenous infusion.
- In Vivo Action: LNPs naturally accumulate in liver cells (hepatocytes), release their payload, and the Cas9 protein is expressed. The resulting Cas9-gRNA complex enters the nucleus and creates a double-strand break in the TTR gene, knocking it out and reducing the production of the disease-causing protein.
Key Research Reagents and Solutions
Table 2: Essential Reagents for In Vivo CRISPR Workflows
| Research Reagent | Function in Protocol | Example/Specification |
|---|---|---|
| Ionizable Lipids | Critical component of LNPs; enables encapsulation, endosomal escape, and payload release. | Proprietary lipids like ALC-0315 or SM-102; SORT molecules for targeted organ delivery. |
| CRISPR mRNA & sgRNA | The genetic blueprint for the editing machinery. | Modified nucleotides for stability; codon-optimized Cas9 mRNA and target-specific sgRNA. |
| LNP Formulation System | For consistent, scalable production of CRISPR-loaded nanoparticles. | Microfluidic mixer (e.g., NanoAssemblr). |
| Animal Disease Models | For pre-clinical efficacy and safety testing of the in vivo therapy. | Transgenic mouse or non-human primate models of the target disease. |
Direct Comparison: Workflows, Efficiencies, and Applications
Quantitative Comparison of Paradigms
Table 3: Head-to-Head Comparison of Ex Vivo vs. In Vivo Delivery Paradigms
| Parameter | Ex Vivo (Casgevy model) | In Vivo (LNP model) |
|---|---|---|
| Clinical Workflow | Complex, multi-step; requires cell harvesting, manufacturing, and reinfusion. | Simplified; single intravenous infusion. |
| Manufacturing | Decentralized, patient-specific (autologous), logistically complex. | Centralized, off-the-shelf (allogeneic), scalable. |
| Delivery Control | High; editing occurs in a controlled, validated process outside the body. | Lower; dependent on biodistribution and uptake of the delivery vector. |
| Target Tissues | Limited to cells that can be extracted, manipulated, and reinfused (e.g., hematopoietic cells, T-cells). | Broad potential, but currently most efficient for liver (with LNPs) and muscle (with AAVs). |
| Therapeutic Examples | Casgevy: Sickle Cell Disease, Beta-Thalassemia [39]. CAR-T-cell therapies: Cancer immunotherapy [39]. | NTLA-2001 (Intellia): hATTR Amyloidosis, Hereditary Angioedema (HAE) [18]. CTX310/320 (CRISPR Tx): Cardiovascular disease [40]. |
| Key Delivery Vectors | Physical Methods: Electroporation (primary method for RNP delivery) [17]. Viral Vectors: Lentivirus for certain cell engineering applications. | Non-Viral: Lipid Nanoparticles (LNPs) for mRNA/sgRNA [41] [18]. Viral Vectors: Adeno-Associated Virus (AAV) for DNA templates. |
| Immunogenicity | Lower risk of immune reaction to CRISPR components due to transient RNP exposure. | Higher concern, especially with viral vectors (AAV); pre-existing immunity is a challenge. LNPs allow for potential re-dosing [18]. |
| Editing Specificity | Potentially higher; controlled conditions and transient RNP delivery reduce off-target risks [17]. | Varies with delivery; prolonged expression from viral vectors may increase off-target risk. |
| Regulatory Status | Clinically proven; first FDA/EMA-approved CRISPR therapy (Casgevy) [39]. | Late-stage clinical trials; no approved therapies yet, but promising Phase I/II data [40] [18]. |
Supporting Experimental Data and Outcomes
- Ex Vivo Efficacy: In the pivotal trials for Casgevy, patients with sickle cell disease experienced a resolution of vaso-occlusive crises. Of 44 patients with at least 16 months of follow-up, over 95% achieved this primary endpoint [39]. Patients with transfusion-dependent beta-thalassemia saw 93% (54 of 58 patients) achieve transfusion independence [39].
- In Vivo Efficacy: In the Phase I trial of NTLA-2001 for hATTR, a single intravenous infusion led to a mean reduction of over 90% in serum TTR protein levels, an effect that was sustained for over two years with no serious adverse events [18]. Similarly, a single dose of CRISPR Therapeutics' CTX310 led to peak reductions of up to 81% in LDL cholesterol and 82% in triglycerides in patients with atherosclerotic heart disease [40].
The ex vivo and in vivo CRISPR delivery paradigms represent two distinct paths to a common goal: durable genetic cures. The ex vivo approach, with its controlled manufacturing and proven clinical success, is currently the established modality for blood and immune cell disorders. The in vivo approach, with its simpler administration and "off-the-shelf" potential, holds immense promise for treating a wider array of genetic diseases, particularly those affecting internal organs like the liver.
The efficiency of both paradigms remains inextricably linked to advancements in delivery vector technology. The success of non-viral LNPs in enabling the first in vivo CRISPR therapies marks a significant shift in the field [41] [18]. Future progress hinges on developing next-generation vectors with enhanced tissue specificity, reduced immunogenicity, and greater payload capacity. As these delivery technologies mature, the choice between ex vivo and in vivo paradigms will be guided by the specific biology of the target disease, balancing logistical complexity against delivery precision to bring transformative therapies to patients.
The development of Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR)-based therapies represents a paradigm shift in treating genetic disorders. A central challenge in realizing this potential is the efficient and safe delivery of CRISPR components to target cells in vivo. The competition between viral and non-viral delivery vectors defines a critical frontier in genetic medicine [3]. Viral vectors, particularly adeno-associated viruses (AAVs), are renowned for their high transduction efficiency and sustained transgene expression, making them a strong candidate for diseases requiring long-term correction [15] [9]. However, their limited packaging capacity, risk of immunogenicity, and potential for insertional mutagenesis pose significant constraints [15] [3]. In contrast, lipid nanoparticles (LNPs) represent a leading non-viral platform. They offer a transient expression profile that minimizes off-target risks, a superior payload capacity, and a reduced immunogenic footprint, allowing for potential re-dosing [42] [18]. This case study delves into the application of LNP technology for liver-targeted therapy, using the landmark treatment for hereditary transthyretin amyloidosis (hATTR) as a primary example to objectively compare its performance against viral vector approaches.
LNP Mechanism of Action for Liver-Targeted Delivery
LNPs are sophisticated nanostructures typically composed of four key lipid components: an ionizable lipid, phospholipid, cholesterol, and a PEGylated lipid [43] [44]. Their remarkable natural tropism for the liver is not accidental but is driven by a specific biological mechanism. Upon intravenous administration, LNPs acquire apolipoprotein E (ApoE) from the bloodstream. The ApoE-coated LNP then acts as a ligand for receptors on hepatocytes, primarily the low-density lipoprotein receptor (LDLR), facilitating efficient cellular uptake via receptor-mediated endocytosis [43] [44]. Following cellular entry, the ionizable lipids within the LNP become protonated in the acidic environment of the endosome. This promotes a transition from a bilayer to a hexagonal structure, disrupting the endosomal membrane and releasing the CRISPR payload into the cytosol—a critical step known as endosomal escape [44]. For CRISPR applications, the payload (e.g., Cas9 mRNA and guide RNA) can then assemble and travel to the nucleus to perform its gene-editing function.
The following diagram illustrates this targeted delivery mechanism.
Case Study: LNP-Mediated CRISPR Therapy for hATTR
Intellia Therapeutics' phase I trial for hATTR is a pioneering example of in vivo LNP delivery for CRISPR therapy [18]. This disease is characterized by the buildup of misfolded transthyretin (TTR) protein, primarily produced in the liver, which leads to progressive neuropathy and cardiomyopathy.
The therapeutic strategy involved a single, systemic intravenous infusion of LNPs encapsulating CRISPR components. The LNP formulation was engineered for hepatic tropism, leveraging the natural ApoE-LDLR pathway described above [43] [18]. The encapsulated cargo consisted of:
- Cas9 mRNA: Providing the template for the gene-editing enzyme.
- Single-guide RNA (sgRNA): Designed to specifically target the TTR gene in hepatocytes.
The mechanism of action is gene disruption. The CRISPR-Cas9 complex introduces a double-strand break in the TTR gene, which is then repaired by the cell's error-prone non-homologous end joining (NHEJ) pathway. This process results in small insertions or deletions (indels) that effectively knock out the gene, leading to a sustained reduction in the production of the disease-causing TTR protein [18].
Key Experimental Data and Outcomes
The clinical results have demonstrated the compelling efficacy and safety profile of this LNP-based approach. The table below summarizes the key quantitative outcomes from the trial.
Table 1: Key Efficacy and Safety Data from the hATTR Clinical Trial
| Metric | Result | Significance |
|---|---|---|
| TTR Protein Reduction | ~90% average reduction in serum TTR levels [18] | Biomarker confirming potent in vivo genome editing. |
| Durability of Effect | Sustained TTR reduction over 2+ years of follow-up [18] | Suggests a durable, potentially one-time therapeutic effect. |
| Therapeutic Outcome | Disease symptom stabilization or improvement [18] | Translates biomarker success into clinical benefit for patients. |
| Dosing Regimen | Successful re-dosing reported in clinical trials [18] | Highlights a key advantage over viral vectors. |
| Common Adverse Events | Mild to moderate infusion-related reactions [18] | Manageable safety profile, distinct from viral vector immunogenicity. |
Comparative Analysis: LNP vs. Viral Vectors for Liver-Targeted CRISPR
The success of the hATTR trial provides a concrete dataset for a head-to-head comparison with viral vector systems, such as AAV. The following table contrasts the critical parameters of each platform.
Table 2: Objective Comparison of LNP and Viral Vector Delivery Systems
| Parameter | Lipid Nanoparticles (LNPs) | Adeno-Associated Virus (AAV) |
|---|---|---|
| Packaging Capacity | High (Virtually unlimited for mRNA) [42] | Limited (<4.7 kb), requiring smaller Cas9 orthologs [15] |
| Expression Kinetics | Transient (Days to weeks) [42] [9] | Long-term/Persistent (Months to years) [15] |
| Immunogenicity | Lower risk; allows for potential re-dosing [18] [3] | Higher risk; pre-existing immunity and immune responses prevent re-dosing [15] [3] |
| Risk of Insertional Mutagenesis | Very Low; functions episomally [43] | Low, but documented; potential for AAV integration [3] |
| Manufacturing & Scalability | Highly scalable and cost-effective cell-free synthesis [43] [42] | Complex and expensive biological production [9] |
| Off-Target Risk Profile | Lower risk due to transient Cas9 expression [42] [9] | Higher risk due to persistent Cas9 expression [9] |
| Tropism (Liver) | Natural, high tropism via ApoE/LDLR uptake [43] [44] | Requires selection/engineering of specific serotypes (e.g., AAV8, AAV9) [15] |
Critical Interpretation of Comparative Data
The data in Table 2 reveals a clear trade-off. LNPs excel in safety, payload delivery, and dosing flexibility. Their transient nature is a strategic advantage for CRISPR nuclease applications, as it limits the window for off-target editing and mitigates immunogenic responses, which is a significant challenge with AAVs [15] [18]. The demonstrated ability to re-dose LNP-based therapies, as seen in the hATTR trial and a personalized case for CPS1 deficiency, is a transformative feature not feasible with AAVs due to neutralizing antibody formation [18].
Conversely, AAVs provide superior longevity of transgene expression. This makes them potentially better suited for applications requiring continuous production of a therapeutic protein, such as in some gene replacement strategies. However, for CRISPR-mediated gene knockout—the mechanism used in the hATTR trial—the durable effect achieved after a single, transient LNP treatment demonstrates that long-term expression of the editing machinery is not necessary [18]. The primary limitation of AAVs for CRISPR is their constrained cargo capacity, which complicates the delivery of the commonly used Streptococcus pyogenes Cas9 (SpCas9) and requires sophisticated workarounds like dual-vector systems or the use of less characterized compact Cas enzymes [15].
The Scientist's Toolkit: Essential Reagents for LNP-Based CRISPR Delivery
Developing an LNP-based CRISPR therapy requires a suite of specialized reagents and materials. The following table details key components and their functions.
Table 3: Essential Research Reagents for LNP-CRISPR Experiments
| Reagent / Material | Function | Example & Notes |
|---|---|---|
| Ionizable Lipid | Core LNP component; enables encapsulation and endosomal escape [44] | e.g., DLin-MC3-DMA; critical for efficiency and tropism. |
| Cas9 mRNA | Template for in situ production of the Cas9 protein. | N1-methylpseudouridine-modified mRNA enhances stability and reduces immunogenicity [43]. |
| Structurally Optimized Guide RNA | Confers target specificity to the CRISPR-Cas complex. | HPLC-purified synthetic sgRNA with end modifications to enhance stability and editing fidelity [9]. |
| Microfluidic Device | Enables reproducible, scalable LNP formulation. | e.g., NanoAssemblr; ensures uniform particle size and high encapsulation efficiency [44]. |
| Animal Disease Model | For in vivo efficacy and safety testing. | e.g., Fah mutant mice for hereditary tyrosinemia type 1 [15]. |
The clinical success of LNP-mediated CRISPR therapy for hATTR provides a powerful validation of non-viral delivery platforms. The objective data reveals that LNPs hold distinct advantages over viral vectors for in vivo liver-targeted gene editing, particularly in their favorable safety profile, high packaging capacity, and re-dosing capability. While AAVs remain a valuable tool for certain long-term gene expression applications, LNPs have emerged as the superior vector for transient, potent CRISPR-mediated gene disruption. The future of this field lies in the continued optimization of LNP formulations to expand their reach beyond the liver and further improve their efficacy and specificity, solidifying their role as a cornerstone technology for the next generation of genetic medicines.
Navigating Delivery Hurdles: Strategies for Enhancing Safety and Specificity
The therapeutic application of CRISPR-Cas9 systems represents a frontier in treating genetic disorders, yet its clinical translation is significantly challenged by immunogenicity. Immune responses can be directed against both the delivery vehicle—particularly viral capsids—and the bacterial-derived Cas9 nuclease itself, potentially compromising both the safety and efficacy of treatments. Understanding and mitigating these responses is paramount for the development of successful gene therapies. This guide objectively compares the immunogenic profiles of viral and non-viral delivery vectors for CRISPR therapeutics, providing a structured analysis of the inherent challenges and the experimental strategies employed to overcome them.
The immunogenicity landscape is complex. Viral vectors, while efficient, can trigger immune reactions due to pre-existing immunity in human populations or from the initial administration. Concurrently, the Cas9 protein, being of bacterial origin, can be recognized by the human immune system as a foreign antigen, leading to cytotoxic responses that may eliminate the very cells needed for therapeutic effect. This review synthesizes current data and methodologies, providing researchers with a comparative framework to select and optimize delivery platforms.
Immunogenicity of Viral Vectors
Viral vectors, particularly Adeno-Associated Viruses (AAV), are a mainstay for in vivo gene delivery due to their high transduction efficiency and sustained transgene expression. However, their immunogenicity presents a dual challenge: pre-existing neutralizing antibodies in a large portion of the human population can render treatments ineffective, and the initial administration can elicit a robust cellular and humoral immune response that prevents re-dosing [3].
The immune response to AAV is primarily mediated by capsid-specific T cells. Following administration, the viral capsid is processed by antigen-presenting cells, leading to the activation of CD8+ cytotoxic T lymphocytes that can eliminate transduced cells [15]. This not only reduces the duration of therapeutic effect but also poses a significant safety risk. A 10-year follow-up study in AAV-treated dogs with hemophilia suggested a potential risk of vector integration near genes controlling cell growth, hinting at carcinogenic risks [3]. Furthermore, a recent clinical setback underscores this risk; Intellia Therapeutics paused two Phase 3 trials for its CRISPR-Cas therapy for transthyretin amyloidosis after a patient experienced severe (Grade 4) liver toxicity, though the delivery vector was not immediately suspected [21].
Table 1: Immune Challenges and Mitigation Strategies for Viral Vectors
| Vector Type | Primary Immune Challenges | Reported Incidence/Data | Mitigation Strategies |
|---|---|---|---|
| Adeno-Associated Virus (AAV) | Pre-existing neutralizing antibodies (NAbs), Capsid-specific T-cell response, Limited packaging capacity (~4.7 kb) constrains use of larger Cas9 variants [15] [45]. | A high percentage of the population has pre-existing NAbs; Clinical hold due to Grade 4 liver toxicity event [21]. | Serotype switching: Using less common AAV serotypes [15]. Capsid engineering: Developing engineered capsids with reduced immunogenicity [15]. Empty capsid purification: Removing empty capsids during manufacturing to reduce antigen load [15]. |
| Adenoviral (AdV) | Strong innate and adaptive immune responses, High inflammation potential [17]. | Commonly causes inflammatory responses, limiting re-administration. | Hexon modification: Engineering the viral hexon protein to evade immune recognition [17]. Immunosuppression: Using transient immunosuppressive regimens around the time of administration [17]. |
| Lentiviral (LV) | Insertional mutagenesis risk, Immune responses to viral components [17]. | Pre-clinical models show potential for genotoxicity, though newer generations are safer. | Pseudotyping: Using envelopes from other viruses (e.g., VSV-G) to alter tropism and potentially reduce immune recognition [17]. Self-inactivating (SIN) designs: Engineering the viral backbone to enhance safety [17]. |
Immunogenicity of the Cas9 Nuclease
Independent of the delivery method, the Cas9 nuclease itself is a significant source of immunogenicity. As a protein derived from bacteria (Streptococcus pyogenes and others), the human immune system can harbor pre-existing humoral and cell-mediated immunity against it. Studies have detected the presence of anti-Cas9 antibodies and Cas9-reactive T cells in a substantial number of individuals [3].
This pre-existing immunity can lead to a rapid immune response against CRISPR-Cas9-modified cells, clearing them and thus negating the therapeutic benefit. In the context of viral delivery, particularly with AAVs, the situation is exacerbated. The prolonged expression of Cas9 from the viral genome increases the window for immune system recognition and attack. In contrast, non-viral methods that deliver Cas9 as a transient mRNA or protein (Ribonucleoprotein, RNP) exhibit a shorter pharmacokinetic profile, thereby potentially reducing the risk of eliciting a strong immune response [17] [3].
Non-Viral Delivery as a Strategy to Reduce Immunogenicity
Non-viral delivery methods have gained prominence as a strategy to circumvent the immunogenic pitfalls of viral vectors. The primary advantage of platforms like Lipid Nanoparticles (LNPs) is the transient delivery of CRISPR components—as mRNA or pre-assembled Cas9-gRNA Ribonucleoprotein (RNP) complexes—which significantly reduces the duration of Cas9 exposure and minimizes the risk of persistent immune responses and off-target editing [17] [3].
Intellia Therapeutics' clinical programs provide compelling evidence for this approach. Their LNP-based in vivo CRISPR therapies for hereditary transthyretin amyloidosis (hATTR) and hereditary angioedema (HAE) have demonstrated deep and sustained reduction of disease-causing proteins with no serious side effects reported from the Cas9 protein itself [18]. Notably, the LNP platform has enabled the possibility of redosing, a significant limitation of AAVs. In their hATTR trial, three participants who received a low initial dose were safely administered a second, higher dose, demonstrating that LNPs do not trigger the same immune memory as viral vectors [18]. This was further validated in a landmark case of a personalized CRISPR treatment for an infant with CPS1 deficiency, where the patient safely received three separate LNP doses [18].
Table 2: Comparing Immunogenic Profiles of Viral and Non-Viral CRISPR Delivery
| Characteristic | Viral Vectors (e.g., AAV) | Non-Viral Vectors (e.g., LNP) |
|---|---|---|
| Cas9 Expression | Long-term, persistent expression from integrated or episomal DNA [15]. | Short-term, transient expression from mRNA or direct RNP delivery [17]. |
| Pre-existing Immunity | High prevalence of neutralizing antibodies to common viral serotypes [3]. | No pre-existing immunity to the synthetic LNP vehicle. Pre-existing immunity to Cas9 remains a consideration [3]. |
| Risk of Insertional Mutagenesis | Yes, particularly with lentivirus; AAV can integrate at CRISPR cut sites [3]. | No, non-viral systems do not integrate into the host genome [17]. |
| Inflammatory Potential | Moderate to High (dependent on vector and serotype) [17]. | Generally Low, with mild infusion-related reactions reported [18]. |
| Potential for Re-dosing | Severely limited due to adaptive immune memory against the capsid [15]. | Demonstrated to be feasible in clinical trials [18]. |
| Packaging Capacity | Limited (e.g., AAV: ~4.7 kb), often requiring complex solutions for SpCas9 [15]. | High capacity, easily packages Cas9 mRNA and sgRNA [17]. |
Experimental Protocols for Assessing Immunogenicity
Rigorous preclinical assessment is critical for evaluating the immunogenic potential of CRISPR therapeutics. The following protocols outline standard methodologies for quantifying immune responses to both viral capsids and the Cas9 nuclease.
Protocol 1: Evaluating Cellular Immune Responses to Cas9
This protocol measures T-cell activation against Cas9, a key determinant of cell-mediated immunity.
- CD8+ T-Cell Cytotoxicity Assay:
- Isolate and Load Target Cells: Harvest primary cells (e.g., hepatocytes) from a donor model (humanized mouse or non-human primate). Transduce the cells with an AAV vector expressing Cas9 and a model antigen (e.g., ovalbumin peptide SIINFEKL).
- Isolate Effector Cells: Isolate naive T cells from the same donor or a syngeneic model.
- Co-culture and Activation: Co-culture the Cas9-expressing target cells with the naive T cells for 7-10 days to allow for T-cell priming and expansion.
- Chromium Release Assay: Label fresh, Cas9-expressing target cells with Chromium-51 (⁵¹Cr). Incubate these labeled target cells with the activated T cells at various effector-to-target (E:T) ratios.
- Measurement: After 4-6 hours, measure the amount of ⁵¹Cr released into the supernatant. Specific lysis is calculated as:
(Experimental Release – Spontaneous Release) / (Maximum Release – Spontaneous Release) * 100. A high percentage of specific lysis indicates a strong CD8+ T-cell response against Cas9.
Protocol 2: Assessing Humoral Immunity to Viral Capsids
This protocol quantifies the levels of neutralizing antibodies (NAbs) against AAV capsids, which can inhibit transduction.
- AAV Neutralizing Antibody Assay:
- Serum Collection: Collect serum from the test subject (e.g., human patient or animal model).
- Prepare AAV Reporter Vector: Generate an AAV vector containing a reporter gene, such as Green Fluorescent Protein (GFP) or luciferase.
- Serum-Vector Incubation: Dilute the serum and incubate it with a fixed titer of the AAV reporter vector for 1 hour at 37°C.
- Cell Infection: Add the serum-vector mixture to a permissive cell line (e.g., HEK293T cells). Include controls with no serum and with serum from naive subjects.
- Quantification: After 48-72 hours, measure reporter gene expression (e.g., via flow cytometry for GFP or luminescence reading). The NAb titer is defined as the highest serum dilution that reduces reporter gene expression by 50% or more compared to the naive serum control.
The Scientist's Toolkit: Key Reagents for Immunogenicity Research
Table 3: Essential Research Reagents for Immunogenicity Studies
| Reagent / Tool | Function in Immunogenicity Research |
|---|---|
| HPLC-purified, modified sgRNA | Reduces innate immune activation by the RNA component and minimizes cytotoxicity, leading to cleaner experimental outcomes [3]. |
| Cas9 Ribonucleoprotein (RNP) | The pre-complexed form of Cas9 protein and sgRNA; enables transient editing, reduces off-target effects, and is the preferred cargo for LNP and electroporation-based delivery [17]. |
| Anti-CRISPR (Acr) Proteins | Used in experimental settings to rapidly inactivate Cas9 activity after editing, which can help dissect the duration of Cas9 expression from immune outcomes [21]. |
| Selective Organ Targeting (SORT) LNPs | A advanced class of LNPs engineered through the inclusion of a SORT molecule to target specific tissues beyond the liver (e.g., lung, spleen), enabling tissue-specific immunogenicity profiling [17]. |
| Cytokine ELISA Kits | Essential for quantifying the levels of pro-inflammatory cytokines (e.g., IFN-γ, IL-6) in serum or supernatant following administration of CRISPR therapeutics. |
| Immune Cell Isolation Kits | For the positive or negative selection of specific immune cell populations (e.g., CD8+ T cells, B cells) from peripheral blood or tissues for downstream functional assays. |
Visualizing Immune Pathways and Experimental Workflows
Immune Activation Pathways in CRISPR Therapy
This diagram illustrates the key pathways through which viral vectors and the Cas9 nuclease activate the adaptive immune system.
Assessing Cas9-Specific T-Cell Responses
This flowchart details the experimental workflow for a cytotoxicity assay to evaluate T-cell responses against the Cas9 nuclease.
The choice between viral and non-viral delivery vectors for CRISPR therapeutics involves a direct trade-off between the efficiency and durability of editing and the risk of immunogenicity. Viral vectors, particularly AAVs, offer potent and long-lasting effects but are significantly constrained by pre-existing and treatment-induced immune responses. Non-viral vectors, especially LNPs, present a compelling alternative with a superior safety profile, reduced immunogenicity, and the unique clinical advantage of re-dosing.
Future progress will be driven by continued innovation in both camps. For viral vectors, this includes the development of novel engineered capsids with reduced immunogenicity and the use of immunosuppressive regimens. For non-viral methods, the focus will be on enhancing delivery efficiency to a broader range of tissues and further optimizing the LNP formulations. The ongoing clinical trials for both approaches will yield critical long-term data on immune responses in humans. Ultimately, the specific therapeutic application—the target tissue, required duration of editing, and patient population—will determine the optimal delivery strategy, making both viral and non-viral platforms crucial tools in the expanding CRISPR therapeutic arsenal.
The therapeutic application of CRISPR-Cas systems represents a groundbreaking advancement in genetic medicine, with the potential to permanently correct disease-causing mutations [46]. However, a significant bottleneck impedes clinical translation: the efficient packaging and delivery of the often-large CRISPR components into target cells [47] [41]. The CRISPR machinery consists primarily of the Cas nuclease and a guide RNA (gRNA), which together form a complex that can be challenging to deliver due to its substantial molecular size and negative charge [41] [46]. This challenge is particularly acute for viral vectors, which are favored for their high delivery efficiency but operate under strict packaging constraints [15]. This guide objectively compares the leading strategies developed to overcome these cargo limitations, providing researchers with a clear framework for selecting the optimal delivery system for their therapeutic goals.
The Cargo Challenge: Understanding Size Constraints in CRISPR Delivery
The CRISPR system can be delivered in three primary biological formats, each with distinct implications for cargo size: plasmid DNA (pDNA), messenger RNA (mRNA), or as a pre-assembled ribonucleoprotein (RNP) complex [48]. The most commonly used Cas9 protein from Streptococcus pyogenes (SpCas9) has a coding sequence of approximately 4.2 kb, which alone nearly fills the capacity of the widely used adeno-associated virus (AAV) vectors, limited to about 4.7 kb [48] [15]. When the sequences for the gRNA and regulatory elements are added, the payload easily exceeds this limit.
The table below summarizes the cargo capacities of the most common delivery vehicles, illustrating the core of the packaging challenge.
| Delivery Vehicle | Cargo Capacity | Compatible CRISPR Cargo Formats |
|---|---|---|
| Adeno-Associated Virus (AAV) | ~4.7 kb [17] [48] [15] | DNA, gRNA [41] |
| Lentivirus (LV) | ~10 kb [17] [49] | DNA [17] |
| Adenovirus (AdV) | ~36 kb [17] | DNA [17] |
| Lipid Nanoparticle (LNP) | Flexible, no strict genetic limit [17] [41] | pDNA, mRNA, RNP [17] [41] |
| Virus-Like Particle (VLP) | Limited, but can be engineered [17] | Protein, RNP [17] |
Comparative Analysis of Strategic Solutions
Researchers have developed multiple innovative strategies to bypass these cargo limitations. The following table provides a high-level comparison of the primary approaches, which are detailed in subsequent sections.
| Strategy | Key Principle | Best-Suited For | Notable Advantages | Key Limitations |
|---|---|---|---|---|
| Compact Cas Orthologs [48] [15] | Using naturally smaller Cas proteins (e.g., SaCas9, Cas12f) | All-in-one AAV delivery; in vivo therapies [15] | Simpler system; single vector administration [15] | May have different PAM requirements; potentially lower efficiency [48] |
| Dual-Vector Systems [15] | Splitting CRISPR components across two AAV vectors | Delivering full-length SpCas9 and gRNA [15] | Uses well-characterized, highly efficient SpCas9 [15] | Lower co-transduction efficiency; more complex manufacturing [15] |
| LNPs for RNP/mRNA [17] [41] | Lipid-based encapsulation of mRNA or pre-formed RNP | Transient editing; therapies requiring redosing [18] [19] | High cargo flexibility; low immunogenicity; suitable for redosing [18] [17] | Can struggle with endosomal escape; requires further optimization for tissue targeting [17] [19] |
| Advanced Nanostructures [19] | Structural engineering of nanoparticles (e.g., SNA) to enhance delivery | Boosting efficiency in hard-to-transfect cells [19] | Can triple gene-editing efficiency; reduced cellular toxicity [19] | Emerging technology; requires further in vivo validation [19] |
Strategy 1: Employing Compact Cas Orthologs
One of the most straightforward strategies is the use of naturally occurring or engineered compact Cas proteins. By replacing SpCas9 with smaller variants, the entire CRISPR system can be packaged within a single AAV vector.
- Established Compact Nucleases: Staphylococcus aureus Cas9 (SaCas9, ~1,000 amino acids) is a well-established alternative that fits comfortably within AAV's capacity [48] [15]. Newer, hypercompact systems like Cas12f (also known as Cas14, ~500-700 amino acids) offer even greater packaging flexibility [48] [15].
- Experimental and Ancestral Systems: Research is exploring putative ancestors of Cas proteins, such as IscB and TnpB, which are ultra-compact and show promise for AAV delivery with reduced immunogenicity [15].
- Therapeutic Evidence: In a preclinical study for retinitis pigmentosa, subretinal delivery of an rAAV8 vector encoding the compact CasMINI_v3.1/ge4.1 achieved transduction efficiencies of over 70% in retinal cells and led to a significant improvement in photoreceptor function [15].
Strategy 2: Dual rAAV Vector Systems
For applications where SpCas9 is indispensable, a dual AAV vector system is a widely adopted solution. This approach involves splitting the CRISPR components—typically with Cas9 on one vector and the gRNA on another—across two separately packaged AAVs [15]. The success of this strategy hinges on the co-transduction of the same cell by both vectors, which then rely on the cell's machinery to reassemble the functional CRISPR system.
Strategy 3: Non-Viral Delivery of RNP and mRNA
Lipid Nanoparticles (LNPs) represent a powerful non-viral alternative that completely bypasses the genetic payload constraints of viral vectors. LNPs can encapsulate not only DNA but also Cas9 mRNA or the pre-assembled RNP complex [17] [41].
- Clinical Validation: The first personalized in vivo CRISPR treatment for CPS1 deficiency was successfully delivered using LNPs, with the patient safely receiving multiple doses, demonstrating the platform's re-dosing capability [18].
- Performance Advantages: A head-to-head comparison in cellular cultures showed that a new type of nanostructure, lipid nanoparticle spherical nucleic acids (LNP-SNAs), entered cells up to three times more effectively than standard LNPs and boosted gene-editing efficiency threefold while reducing toxicity [19].
- Mechanistic Workflow: The following diagram illustrates the typical experimental workflow for developing and testing an LNP-based CRISPR delivery system, from cargo formulation to functional assessment.
Key Experimental Workflows and Protocols
A critical step in evaluating any delivery strategy is the quantitative assessment of its editing outcomes. A robust protocol for this involves using a fluorescent reporter system, such as enhanced Green Fluorescent Protein (eGFP), to distinguish between different DNA repair pathways [50].
- Protocol Principle: Cells stably expressing eGFP are transfected with CRISPR reagents designed to target and disrupt the eGFP gene. Successful Non-Homologous End Joining (NHEJ) leads to gene knockout and a loss of green fluorescence. If a donor template for Homology-Directed Repair (HDR) is co-delivered, it can introduce a specific mutation that shifts fluorescence from green to blue (BFP) [50].
- Measurement and Analysis: The cells are then analyzed using Fluorescence-Activated Cell Sorting (FACS). The ratio of non-fluorescent (NHEJ) or blue (HDR) cells to the total transfected population provides a quantitative measure of editing efficiency [50]. This protocol is adaptable for high-throughput screening of different delivery systems or CRISPR construct designs.
The logical workflow and key decision points for such a fluorescent reporter assay are mapped below.
The Scientist's Toolkit: Essential Reagents for CRISPR Delivery Research
The following table catalogs key reagents and materials essential for executing experiments in CRISPR delivery, particularly those focused on overcoming cargo limits.
| Research Reagent / Material | Function in Experimentation |
|---|---|
| Ionizable Cationic Lipids [17] [48] | Core component of LNPs; enables cargo encapsulation and facilitates endosomal escape through pH-dependent charge shift. |
| Compact Cas Orthologs (e.g., SaCas9, CjCas9) [48] [15] | Smaller Cas proteins used to fit CRISPR systems within the limited packaging capacity of single AAV vectors. |
| MS2 Aptamer-Modified sgRNA [46] | Engineered sgRNA used in modular loading strategies (e.g., for EV or VLP delivery) to recruit fusion proteins for cargo packaging. |
| UV-Cleavable Linker Domains (e.g., PhoCl) [46] | Molecular tool used in advanced delivery platforms to enable controlled release of CRISPR cargo inside the target cell upon light activation. |
| Fluorescent Reporters (e.g., eGFP) [50] | A critical tool for rapidly screening and quantifying gene editing outcomes (e.g., knockout via NHEJ or precise mutation via HDR) in a cell population. |
| Selective Organ Targeting (SORT) Molecules [17] | Molecules incorporated into LNPs to direct them to specific tissues beyond the liver, such as the lungs or spleen. |
The quest to overcome the cargo limits of CRISPR delivery has driven the development of a diverse and innovative toolkit. The choice between viral and non-viral vectors is no longer a simple binary but a strategic decision based on the specific therapeutic needs.
- For applications demanding long-term, sustained expression and where a compact Cas nuclease is available or sufficient, single-AAV vectors offer an elegant solution.
- When the use of larger, high-fidelity nucleases like SpCas9 is non-negotiable, dual-AAV systems provide a viable, though more complex, pathway.
- For therapies that prioritize safety, re-dosing capability, and maximal cargo flexibility, LNP-based delivery of mRNA or RNP complexes is emerging as the leading platform, a position strengthened by recent clinical successes and advancements in nanostructure engineering like LNP-SNAs.
The future of CRISPR therapeutics will likely see increased convergence of these strategies, combining the targeting precision of viral vectors with the safety and cargo flexibility of non-viral systems. As these delivery platforms mature, the potential of CRISPR to treat a vast array of genetic diseases moves closer to realization.
The efficacy of CRISPR-based therapeutics is fundamentally constrained by the ability to deliver gene-editing machinery precisely to target cells. The central challenge lies in engineering vectors that can navigate biological barriers to achieve high specificity and efficiency while minimizing off-target effects and immunogenicity. The ongoing debate between viral and non-viral delivery systems centers on balancing cargo capacity, targeting precision, manufacturing complexity, and safety profiles. This guide objectively compares the performance of emerging vector engineering strategies, providing experimental data and methodologies that enable researchers to select optimal systems for specific therapeutic applications.
Vector Systems: A Comparative Analysis
Viral vs. Non-Viral Delivery Platforms
Table 1: Performance Comparison of Major CRISPR Delivery Vectors
| Delivery Method | Specificity Engineering Approach | Max Cargo Capacity | Editing Efficiency | Primary Safety Concerns | Optimal Application Context |
|---|---|---|---|---|---|
| AAV Vectors | Serotype selection (AAV9 for CNS [9]); Capsid engineering [9] | ~4.7 kb [9] [17] | Moderate [9] | Limited immunogenicity [9]; Pre-existing immunity | In vivo delivery to well-characterized tissues [9] |
| Lentiviral Vectors | Pseudotyping with engineered envelopes [17] | ~10 kb [7] | High [9] | Insertional mutagenesis [9] [7] | Ex vivo editing (e.g., CAR-T [9]); Integrase-deficient for CNS [9] |
| Adenoviral Vectors | Modification of fiber proteins for cell targeting [17] | ~36 kb [17] | Moderate [9] | High immunogenicity [9] | Large cargo delivery; Vaccines [7] |
| Lipid Nanoparticles (LNPs) | Selective Organ Targeting (SORT) molecules [17] | Limited by encapsulation efficiency | Variable (cell-type dependent) [9] | Low immunogenicity [9]; Endosomal entrapment [17] | Systemic in vivo delivery (liver-tropic [18]); Redosable regimens [18] |
| Virus-Like Particles (VLPs) | Engineering of empty viral capsids [17] | Similar to AAV [17] | High (transient) | Minimal safety concerns (non-integrating) [17] | Transient editing with reduced off-target risk [17] |
Quantitative Assessment of Delivery Efficiency
Table 2: Experimental Performance Metrics Across Vector Platforms
| Vector Type | In Vivo Transduction Efficiency (% Target Cells) | Duration of Expression | Cell-Type Specificity Index (Target:Non-Target) | Clinical Trial Phase (Representative Example) |
|---|---|---|---|---|
| AAV9 | 40-70% (CNS) [9] | Long-term (years) | Moderate (serotype-dependent) | Phase 1/2 (EBT-101 for HIV) [9] |
| Lentivirus | 60-90% (ex vivo) [9] | Persistent (integration) | High (with pseudotyping) | FDA-approved (CAR-T, Zynteglo) [9] |
| LNPs | 30-60% (hepatocytes) [18] | Transient (days) | High (with SORT engineering) | Phase 3 (Intellia's hATTR treatment) [18] |
| RNPs (Electroporation) | 70-95% (ex vivo) [9] | Immediate (hours) | N/A (direct delivery) | FDA-approved (Casgevy for SCD) [9] |
Engineering Strategies for Enhanced Specificity
Viral Vector Engineering Approaches
Capsid and Envelope Modification: For AAV vectors, tissue specificity is primarily achieved through serotype selection (e.g., AAV9 for crossing the blood-brain barrier [9]) and capsid engineering. Directed evolution approaches generate novel capsid variants with improved targeting capabilities by creating mutant libraries and screening for enhanced tissue tropism in vivo [9]. Lentiviral vectors achieve specificity through pseudotyping - incorporating envelope glycoproteins from other viruses (e.g., VSV-G, Rabies-G) to alter cellular tropism [17].
Payload Optimization: The limited cargo capacity of AAVs (~4.7 kb) necessitates innovative solutions for delivering CRISPR components. Successful strategies include:
- Using compact Cas9 orthologs (e.g., SaCas9) that fit within size constraints [9]
- Dual-vector systems where Cas9 and gRNA are delivered separately [9]
- Split-Cas9 systems where the nuclease is divided across two vectors [9]
- Single-vector systems in Cre-dependent Cas9 mouse lines that bypass packaging limitations [51]
Non-Viral Vector Engineering Approaches
Lipid Nanoparticle (LNP) Optimization: LNPs demonstrate natural tropism for liver tissues but can be engineered for broader applicability. The Selective Organ Targeting (SORT) platform incorporates additional molecules that alter LNP surface properties, enabling targeted delivery to lungs, spleen, and specific cell types within these organs [17]. This approach represents a significant advancement beyond first-generation LNPs.
Cell-Penetrating Peptides (CPPs): Peptide-based delivery systems offer potential for enhanced specificity through incorporation of tissue-specific homing domains. These systems leverage natural cell-penetrating capabilities while minimizing immunogenic responses and can be engineered for endosomal escape, a critical barrier for non-viral delivery [52].
Experimental Protocols for Specificity Assessment
Protocol 1: Single-Vector System for Neuronal Targeting
Objective: Achieve cell-type-specific CRISPR editing and tool delivery in the nervous system using a single AAV vector [51].
Methodology:
- Vector Design: Clone Cre-dependent transgene (e.g., GCaMP8f, ChRonos, mCherry) into pX552 vector containing gRNA scaffold [51]
- gRNA Selection: Identify target exon shared across all splice variants using NCBI Gene database. Input coding sequence into CRISPOR tool to identify optimal gRNA sequences adjacent to SpCas9 PAM sites [51]
- Animal Model: Cross Cre-dependent Cas9 mouse lines (e.g., Rosa26-LSL-Cas9) with appropriate Cre-driver lines for cell-type specificity [51]
- Stereotactic Injection: Deliver single AAV vector expressing both gRNA and Cre-dependent transgene into target brain regions [51]
- Validation: Assess editing efficiency via sequencing and functional readouts (e.g., calcium imaging, axonal tracing) [51]
Key Advantage: This approach ensures complete overlap between edited cells and transgene expression, overcoming the variable co-transduction efficiency of dual-vector systems [51].
Protocol 2: LNP-Mediated Systemic Delivery for Liver Editing
Objective: Achieve in vivo genome editing through systemic administration of LNP-formulated CRISPR components [18].
Methodology:
- Formulation Optimization: Encapsulate CRISPR mRNA or RNPs in ionizable lipid nanoparticles with optimized lipid:RNA ratios [18]
- Dosing Regimen: Administer via intravenous injection; consider multiple doses (as demonstrated in hATTR and CPS1 deficiency trials) [18]
- Efficiency Assessment: Quantify protein reduction in serum (e.g., TTR levels for hATTR) as biomarker for editing efficiency [18]
- Safety Monitoring: Track infusion-related reactions and liver enzymes; assess off-target effects via GUIDE-seq or similar methods [18]
Key Advantage: LNPs enable redosable in vivo editing without the immunogenic concerns associated with viral vectors, as demonstrated in clinical trials where patients received multiple doses [18].
Visualizing Experimental Workflows
Single-Vector Neuronal Targeting Workflow
LNP Systemic Delivery Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Vector Engineering and Specificity Assessment
| Reagent/Solution | Function | Application Context | Key Considerations |
|---|---|---|---|
| pX552 Vector | AAV backbone with gRNA scaffold for single-vector systems [51] | Neuronal targeting studies | Enables co-expression of gRNA and Cre-dependent transgenes |
| CRISPOR Tool | Web-based gRNA design and selection [51] | All CRISPR targeting applications | Identifies optimal gRNA sequences with minimal off-target potential |
| SORT Molecules | Lipid nanoparticles engineered with targeting molecules [17] | Tissue-specific LNP delivery | Enables redirection of LNPs from liver to lungs, spleen, etc. |
| Ionizable Lipids | Primary component of LNPs for nucleic acid encapsulation [17] | LNP formulation | Critical for endosomal escape and cargo release |
| Cre-Driver Mouse Lines | Provide cell-type-specific Cre recombinase expression [51] | In vivo specificity studies | Must be crossed with Cre-dependent Cas9 lines |
| Rosa26-LSL-Cas9 Mice | Express Cas9 in Cre-dependent manner [51] | In vivo editing with single-vector systems | Bypasses AAV cargo limitations |
| GCaMP8f | Genetically encoded calcium indicator [51] | Functional validation of edited neurons | Enables recording of calcium transients via photometry |
| ChRonos | Channelrhodopsin for optogenetic manipulation [51] | Functional validation of edited neurons | Allows precise control of neuronal activity |
The engineering of tissue and cell-type-specific vectors for CRISPR delivery continues to evolve with both viral and non-viral systems demonstrating distinct advantages. Viral vectors, particularly AAVs with engineered capsids, offer refined targeting capabilities for well-characterized tissues, while emerging non-viral approaches like SORT-LNPs provide unprecedented opportunities for systemic delivery with reduced immunogenicity. The single-vector strategy for neuronal applications represents a significant methodological advancement that ensures complete overlap between editing and reporter expression. As clinical validation progresses—exemplified by the successful redosing of LNP-based therapies—the selection of optimal delivery systems will increasingly depend on specific application requirements including target tissue, cargo size, desired expression duration, and safety profile. The continued refinement of these engineering approaches promises to expand the therapeutic landscape for CRISPR-based interventions across diverse genetic disorders.
The clinical translation of CRISPR-based therapies is revolutionizing the treatment of genetic disorders, yet this promise is tempered by persistent concerns about genomic safety. Beyond the well-documented issue of off-target mutations at sites with sequence similarity to the intended target, recent studies have uncovered a more pressing challenge: large structural variations (SVs) including chromosomal translocations and megabase-scale deletions [53]. These undervalued genomic alterations raise substantial safety concerns for clinical applications, particularly as CRISPR therapies progress from ex vivo to in vivo applications [26] [53]. The choice between viral and non-viral delivery vectors significantly influences these genomic risks, creating a critical trade-off between editing efficiency and genomic integrity that researchers must carefully navigate.
The therapeutic benefit-risk calculus for any CRISPR intervention must weigh the potential for curative outcomes against the possibility of genotoxic side effects [26]. This balance becomes particularly crucial when considering that not all genomic off-target events carry equal pathological weight, with alterations in tumor suppressor genes or proto-oncogenes representing worst-case scenarios [53]. This article provides a comprehensive comparison of how different delivery systems modulate these genomic risks, synthesizing recent findings on structural variations and off-target effects to inform therapeutic development strategies.
Understanding CRISPR-Induced Genomic Alterations: Mechanisms and Detection
Spectrum of Unintended Genomic Outcomes
CRISPR-Cas9 systems induce double-strand breaks (DSBs) that activate cellular DNA repair pathways, primarily non-homologous end joining (NHEJ) and homology-directed repair (HDR) [24]. While designed to create precise genetic modifications, this process can generate a spectrum of unintended consequences:
- Simple indels: Small insertions or deletions at the target site resulting from error-prone NHEJ repair [24]
- Large-scale deletions: Kilobase- to megabase-scale deletions at the on-target site [53]
- Chromosomal rearrangements: Including translocations between homologous or heterologous chromosomes [53]
- Chromothripsis: Catastrophic chromosomal shattering and reassembly [53]
The following table summarizes the types and significance of major CRISPR-induced genomic alterations:
Table 1: Types of CRISPR-Induced Genomic Alterations
| Alteration Type | Scale | Primary Detection Methods | Clinical Significance |
|---|---|---|---|
| Simple indels | 1-100 bp | Amplicon sequencing, NGS | Can disrupt gene function; well-characterized risk |
| Large deletions | 1 kb - several Mb | CAST-Seq, LAM-HTGTS, long-read sequencing | May delete critical regulatory elements or multiple genes |
| Chromosomal translocations | Variable | CAST-Seq, LAM-HTGTS, cytogenetics | Can create novel fusion genes with oncogenic potential |
| Chromosomal arm losses | >10 Mb | Karyotyping, FISH, sequencing | Severe genomic instability, cell death or transformation |
Detection Methodologies for Comprehensive Risk Assessment
Accurate assessment of genomic alterations requires sophisticated methodologies that overcome the limitations of conventional short-read sequencing. The following experimental protocols represent state-of-the-art approaches for detecting CRISPR-induced genotoxicity:
CIRCLE-Seq Protocol: An in vitro screen for genome-wide CRISPR-Cas9 nuclease off-targets [26]
- Isolate genomic DNA from target cells and fragment by sonication
- Circulate DNA fragments using circligase enzyme
- Perform Cas9 cleavage on circularized DNA
- Liberate cleaved fragments through enzymatic digestion
- Prepare sequencing libraries from cleaved fragments for NGS
- Bioinformatics analysis to identify potential off-target sites
CHANGE-Seq Protocol: Reveals genetic and epigenetic effects on CRISPR-Cas9 genome-wide activity [26]
- Extract genomic DNA and incubate with Cas9-gRNA complex in vitro
- Repair Cas9-induced breaks with a biotinylated nucleotide
- Shear DNA and capture biotinylated fragments
- Prepare sequencing libraries for high-throughput sequencing
- Map cleavage sites across the genome
CAST-Seq Protocol: Designed to detect chromosomal rearrangements and structural variations [53]
- Edit cells with CRISPR-Cas9 system
- Extract genomic DNA after 72 hours
- Perform PCR amplification using target-specific and genome-wide primers
- Prepare sequencing libraries and perform NGS
- Bioinformatics pipeline to identify chimeric sequences indicating SVs
Diagram 1: CRISPR DNA Repair Pathways and Outcomes. This diagram illustrates how double-strand breaks induced by CRISPR-Cas9 are processed through different DNA repair pathways, leading to varying genomic outcomes and risk profiles.
Delivery Vector Comparison: Viral vs. Non-Viral Systems
Viral Vector Systems
Viral vectors remain the most efficient delivery vehicles for in vivo CRISPR therapies, with recombinant adeno-associated viruses (rAAVs) dominating clinical applications due to their favorable safety profile and tissue specificity [15].
Table 2: Viral Delivery Systems for CRISPR Therapeutics
| Vector Type | Packaging Capacity | Integration Status | Key Advantages | Genomic Risk Concerns |
|---|---|---|---|---|
| Adeno-Associated Virus (AAV) | <4.7 kb | Primarily non-integrating | Low immunogenicity, high tissue specificity [15] | Limited payload, requires compact editors, potential for SVs from prolonged expression [15] [53] |
| Adenoviral Vectors (AdV) | Up to 36 kb | Non-integrating | Large cargo capacity, broad tropism [17] | High immunogenicity, inflammatory responses [17] |
| Lentiviral Vectors (LV) | ~8 kb | Integrating | Stable long-term expression, broad tropism [17] | Insertional mutagenesis, persistent off-target activity [17] |
Non-Viral Delivery Systems
Non-viral vectors have gained significant traction due to their improved safety profiles and transient delivery of CRISPR components, potentially reducing off-target effects [24] [25].
Table 3: Non-Viral Delivery Systems for CRISPR Therapeutics
| Vector Type | CRISPR Cargo Format | Key Advantages | Genomic Risk Profile |
|---|---|---|---|
| Lipid Nanoparticles (LNPs) | mRNA/gRNA or RNP | Clinical validation, targeted delivery, redosing capability [18] [54] | Reduced off-target risk from transient expression, lower SV frequency [24] |
| Polymeric Nanoparticles | DNA, mRNA, or RNP | Tunable properties, biocompatibility [24] | Moderate efficiency, endosomal escape challenges [24] |
| Gold Nanoparticles | RNP preferred | Excellent biocompatibility, surface functionalization [24] [25] | Limited in vivo application data, primarily research use [25] |
| Cell-Penetrating Peptides | RNP preferred | Direct nuclear delivery, minimal toxicity [17] | Low delivery efficiency, serum stability issues [17] |
Quantitative Risk Assessment: Comparative Data Analysis
Structural Variation Frequencies Across Delivery Platforms
Recent studies have quantified the frequency and types of structural variations associated with different CRISPR delivery approaches:
Table 4: Quantitative Comparison of Structural Variation Risks
| Delivery Method | Editing Context | Large Deletion Frequency | Translocation Events | Key Risk Modifiers |
|---|---|---|---|---|
| rAAV with SaCas9 | In vivo mouse liver editing | 5-15% of edited alleles [15] | Not detected | Use of DNA-PKcs inhibitors increased megabase deletions >100-fold [53] |
| LNP with mRNA | In vivo non-human primate | <2% of edited alleles [54] | Rare | Transient expression reduced SV risk; redosing possible without increased SVs [18] |
| Electroporation (RNP) | Ex vivo HSC editing | 2-9% of edited alleles [53] | 0.5-2% of cells | Cell-type specific; higher in HSCs versus primary lymphocytes [53] |
| Adenoviral Vector | In vitro cell lines | 8-12% of edited alleles [17] | 1-3% of cells | Prolonged expression correlated with increased rearrangement frequency [17] |
Off-Target Editing Profiles by Delivery Modality
The format of CRISPR cargo significantly influences off-target editing rates, independent of delivery vehicle:
Table 5: Off-Target Activity by CRISPR Cargo Format
| Cargo Format | Time to Peak Activity | Duration of Activity | Relative Off-Target Rate | Advantages for Risk Mitigation |
|---|---|---|---|---|
| Plasmid DNA | 24-48 hours | 5-7 days | High (5-10× baseline) | Low cost, stable storage [25] [17] |
| mRNA/gRNA | 6-12 hours | 2-3 days | Medium (2-4× baseline) | No nuclear entry requirement, transient [25] |
| Ribonucleoprotein (RNP) | 1-4 hours | 24-48 hours | Low (1-2× baseline) | Immediate activity, rapid degradation, highest precision [25] [17] |
Risk Mitigation Strategies and Experimental Design
The Scientist's Toolkit: Essential Reagents and Methods
Table 6: Research Reagent Solutions for Genomic Risk Assessment
| Reagent/Method | Primary Function | Key Applications | Considerations for Use |
|---|---|---|---|
| HiFi Cas9 | High-fidelity nuclease with reduced off-target activity [53] | Therapeutic applications requiring high specificity | 20-40% reduced on-target efficiency tradeoff [53] |
| CAST-Seq Kit | Detection of chromosomal translocations and rearrangements [53] | Preclinical safety assessment, vector comparison | Requires bioinformatics expertise, validated for multiple cell types |
| CIRCLE-Seq | In vitro genome-wide off-target profiling [26] | gRNA screening, early-stage risk assessment | Biochemical method may not capture cellular context |
| DNA-PKcs Inhibitors | Enhance HDR efficiency by suppressing NHEJ [53] | Precision editing applications | Dramatically increases SV risk (up to 1000×) [53] |
| Next-generation LNPs | Organ-selective CRISPR delivery [18] [54] | Targeted in vivo applications, redosing possible | Liver-tropic variants most advanced; other tissues in development |
| Compact Cas Orthologs | Fit within AAV packaging limits [15] | AAV-mediated in vivo delivery | Varied PAM requirements, potentially reduced editing efficiency |
Pathway to Clinical Safety: Integrated Risk Assessment Framework
Diagram 2: Integrated Genomic Risk Assessment Workflow. This framework outlines a systematic approach for evaluating genomic risks throughout therapeutic development, from delivery system selection to clinical decision points.
The landscape of CRISPR therapeutic development requires careful navigation between editing efficiency and genomic safety. Viral vectors, particularly rAAVs, offer high delivery efficiency and tissue specificity but present challenges including payload limitations and potential for prolonged expression that may increase structural variation risks [15] [53]. Non-viral systems, especially LNPs, provide transient delivery compatible with redosing and demonstrate favorable genomic risk profiles, though with initially lower editing efficiency in some tissues [24] [18] [54].
Recent findings on structural variations represent a paradigm shift in safety assessment, revealing that large-scale genomic alterations rather than point mutations may pose the most significant clinical risk [53]. These findings underscore the necessity of advanced detection methods that complement traditional amplicon sequencing, particularly when using NHEJ-inhibiting compounds that can dramatically increase SV frequency [53].
The future of safe CRISPR therapeutics lies in the continued development of precision editing tools with inherent safety features—including high-fidelity nucleases, optimized delivery systems that limit exposure duration, and comprehensive risk assessment protocols that adequately capture the full spectrum of genomic alterations. As the field progresses toward increasingly sophisticated clinical applications, this balanced approach to managing genomic risks will be essential for realizing the full therapeutic potential of CRISPR-based medicines.
Head-to-Head: A Data-Driven Comparison of Vector Performance
The therapeutic application of CRISPR-Cas systems represents a monumental advance in molecular biology, offering unprecedented capabilities for precise genomic modification across diverse organisms [55]. The fundamental efficiency and safety of these editing outcomes are inextricably linked to the delivery vector employed to transport CRISPR components into target cells. The central challenge lies in balancing high on-target editing rates—the desired therapeutic effect—against minimizing off-target effects, which pose potential genotoxic risks [56]. This comparison guide provides a structured, data-driven analysis of how viral and non-viral delivery systems directly influence these critical parameters, offering researchers a framework for selecting optimal delivery strategies based on empirical evidence.
The CRISPR-Cas mechanism relies on creating double-strand breaks (DSBs) at predefined genomic locations, which are subsequently repaired by endogenous cellular mechanisms, primarily non-homologous end joining (NHEJ) or homology-directed repair (HDR) [57] [55]. The delivery vector directly impacts multiple facets of this process: the kinetics and concentration of editing components present in the cell, the duration of nuclease activity, and the potential for immune activation that could compromise efficacy or safety. Understanding these vector-specific properties is essential for designing therapeutic strategies with favorable risk-benefit profiles.
Quantitative Efficiency Comparison of Delivery Platforms
The selection of a delivery platform involves critical trade-offs between editing efficiency, specificity, cargo flexibility, and persistence. The table below provides a direct comparison of these parameters across major delivery systems.
Table 1: Direct Performance Comparison of CRISPR Delivery Vectors
| Parameter | AAV (Viral) | Lentivirus (Viral) | LNP (Non-Viral) | Electroporation (Non-Viral) |
|---|---|---|---|---|
| Primary Use Case | In vivo gene delivery to post-mitotic tissues (CNS, eye, liver) [58] | Ex vivo cell therapy (CAR-T, HSCs) [58] | In vivo gene editing (liver-tropic) [18] [59] | Ex vivo editing of hard-to-transfect cells (hPSCs, immune cells) [57] |
| Typical On-target Efficiency | High (>80% protein reduction in liver targets) [18] | High (efficient integration in dividing cells) [7] | High (86-90% protein reduction in clinical trials) [18] | Variable (cell-type dependent, often >70% in optimized conditions) [57] |
| Off-target Risk Profile | Moderate (sustained expression may increase risk) [56] | Moderate (integration concerns) [7] | Lower (transient expression reduces risk) [57] [58] | Lower (especially with RNP delivery) [57] |
| Cargo Flexibility | Limited (~4.7 kb strict capacity) [58] | Moderate (~10 kb capacity) [58] | High (virtually unlimited for mRNA/protein) [58] | High (flexible for RNP, mRNA, DNA) [57] |
| Expression Kinetics | Slow onset (days), long-term persistence (months-years) [58] | Slow onset, permanent integration [58] | Rapid onset (hours), transient (days) [57] | Rapid onset (hours), transient (days) [57] |
| Immunogenicity | High (pre-existing antibodies, prevents re-dosing) [58] | Low (mostly used ex vivo) [58] | Low (re-dosable, minimal anti-vector immunity) [58] | N/A (ex vivo application) |
| Key Safety Concerns | Immune reactions, hepatotoxicity at high doses | Insertional mutagenesis (theoretical) [7] | Infusion reactions, lipid component toxicity [18] | Cell toxicity, reduced viability [57] |
Recent clinical data underscores these comparative profiles. Intellia Therapeutics' phase I trial for hereditary transthyretin amyloidosis (hATTR) using LNP-delivered CRISPR demonstrated both high efficacy (~90% reduction in TTR protein) and a favorable safety profile with no serious side effects reported [18]. Similarly, their hereditary angioedema (HAE) trial showed an 86% reduction in kallikrein protein with eight of eleven participants in the high-dose group being attack-free during the observation period [18]. These results highlight the therapeutic potential of non-viral delivery when targeted to appropriate tissues.
Experimental Protocols for Efficiency Assessment
Measuring On-target Editing Efficiency
Digital Droplet PCR (ddPCR) and Next-Generation Sequencing (NGS) Workflow: For precise quantification of editing efficiency at the target locus, researchers employ a combination of molecular techniques. Following delivery of CRISPR components via the test vector (e.g., LNP infusion or AAV transduction), genomic DNA is extracted from target cells or tissues at specified timepoints (e.g., 48-72 hours for initial assessment, and weeks to months for persistence studies). For ddPCR, specific probe sets are designed to distinguish between edited and wild-type alleles, providing absolute quantification without the need for standard curves. For deeper characterization, NGS amplicon sequencing of the target region is performed. The region flanking the CRISPR target site is PCR-amplified with barcoded primers, followed by library preparation and high-depth sequencing (>100,000x coverage). Bioinformatic analysis pipelines (e.g., CRISPResso2) then align sequences to the reference genome and quantify the percentage of reads containing insertions, deletions, or precise edits relative to the total read count [56]. This dual-method approach provides both rapid quantification (ddPCR) and comprehensive characterization of the editing spectrum (NGS).
Comprehensive Off-target Profiling
GUIDE-seq and CIRCLE-seq Methodologies: Identifying potential off-target sites requires sophisticated predictive and biochemical approaches. The GUIDE-seq (Genome-wide Unbiased Identification of DSBs Enabled by Sequencing) method involves co-delivering a synthetic double-stranded oligodeoxynucleotide tag along with the CRISPR-Cas9 components. When a DSB occurs, this tag integrates into the break site, serving as a molecular marker. After genomic DNA extraction and shearing, tag-specific enrichment and sequencing identify integration sites genome-wide, providing a comprehensive map of actual off-target events in living cells [56].
For a more predictive approach without cellular delivery, CIRCLE-seq (Circularization for In Vitro Reporting of Cleavage Effects by Sequencing) employs purified genomic DNA that is fragmented, circularized, and amplified. The resulting circular library is incubated with the CRISPR-Cas9 ribonucleoprotein complex, which cleaves its target sites, linearizing the circles. Subsequent sequencing identifies these cleaved fragments, providing a highly sensitive in vitro profile of potential off-target sites without the constraints of cellular delivery [56]. Combining these methods offers both predictive power and confirmation of actual cellular events, creating a robust safety profile for therapeutic candidates.
Table 2: Essential Research Reagents for Efficiency Assessment
| Research Reagent | Function/Application | Key Characteristics |
|---|---|---|
| CRISPR-Cas9 RNP Complex | Direct delivery of editing machinery; minimizes off-targets [57] | Precomplexed Cas9 protein and sgRNA; rapid nuclear localization |
| Lipid Nanoparticles (LNPs) | In vivo delivery vehicle to liver cells [18] [59] | Ionizable lipids, PEG-lipids, cholesterol, phospholipid composition |
| Adeno-Associated Virus (AAV) | In vivo delivery to non-dividing cells [7] [58] | Multiple serotypes (AAV9, AAVrh74); ~4.7 kb cargo capacity |
| Lentiviral Vectors | Ex vivo delivery for integrating therapies [7] | Self-inactivating (SIN) design; ~10 kb capacity; integrates into genome |
| Neon Transfection System | Electroporation for hard-to-transfect cells [57] | Microscale electroporation in capillaries; optimized for stem cells |
| ddPCR Supermix | Absolute quantification of editing efficiency [56] | Droplet-based digital PCR; no standard curve needed; high precision |
| NGS Library Prep Kits | Amplicon sequencing for on/off-target analysis [56] | Barcoded primers; high-fidelity enzymes; low bias amplification |
Visualizing Delivery and Assessment Workflows
The following diagrams illustrate the fundamental relationships and experimental workflows discussed in this guide, highlighting the critical decision points in delivery vector selection and efficiency assessment.
Diagram 1: CRISPR Delivery Vector Selection Logic
Diagram 2: Editing Efficiency and Safety Assessment Workflow
The direct comparison of editing rates and off-target profiles reveals a nuanced landscape for CRISPR delivery vector selection. Viral vectors, particularly AAV, offer the advantage of potent, long-lasting editing in non-dividing tissues but present challenges related to immunogenicity and cargo constraints. Lentiviral systems remain indispensable for ex vivo applications requiring stable genomic integration, such as CAR-T therapies, despite theoretical concerns about insertional mutagenesis. Non-viral platforms, especially LNPs, have demonstrated remarkable clinical efficacy for liver-targeted therapies with favorable safety profiles and the unique advantage of re-dosability [18] [58]. Electroporation of RNP complexes provides the most direct control over editing kinetics, minimizing off-target risks while enabling manipulation of challenging primary cell types.
The evolving regulatory landscape further influences this calculus. As agencies increasingly treat delivery vehicles as "platforms," developers with well-characterized vectors may benefit from streamlined pathways for new payloads [58]. The critical path forward requires matching vector capabilities to therapeutic objectives: AAV for durable expression in static tissues, lentivirus for engineered cell therapies, and LNPs for transient editing applications where control over nuclease activity is paramount. As the field advances, hybrid approaches and next-generation vectors will likely blur these distinctions, but the fundamental principles of efficiency, specificity, and safety profiled in this guide will remain essential for therapeutic development.
The therapeutic application of CRISPR-Cas genome editing represents a paradigm shift in treating genetic disorders, with the choice of delivery vector—viral or non-viral—profoundly influencing both efficacy and safety outcomes. As CRISPR technologies advance toward clinical translation, comprehensive safety profiling of these delivery platforms has become imperative. The immunogenicity, genotoxicity, and long-term risks associated with CRISPR therapeutics are inextricably linked to vector selection and design. Viral vectors, particularly recombinant adeno-associated viruses (rAAVs), offer efficient delivery and sustained expression but face challenges related to pre-existing immunity, limited packaging capacity, and persistent nuclease activity that may amplify genotoxic risks [15] [60]. Non-viral platforms, especially lipid nanoparticles (LNPs), provide transient editing activity, reduced immunogenicity concerns, and dose titration capability, though they often exhibit lower delivery efficiency to non-hepatic tissues [18] [24]. This analysis systematically compares the safety profiles of these divergent delivery strategies, providing researchers with critical insights for platform selection and optimization.
Immunogenicity Profiles: Viral versus Non-Viral Delivery Platforms
Immune Recognition Mechanisms
The immunogenicity of CRISPR therapeutics stems from multiple components: the bacterial-derived Cas nuclease, the delivery vector itself, and the nucleic acid components. Viral vectors, particularly rAAVs, trigger both innate and adaptive immune responses. Pre-existing immunity to rAAV serotypes is widespread in human populations due to natural exposure, leading to neutralization of therapeutic vectors and impaired transduction efficiency [60]. Additionally, rAAV-mediated delivery typically results in persistent Cas9 expression, prolonging antigen exposure and potentially driving robust T-cell and B-cell activation [61].
Non-viral delivery systems, particularly LNPs, exhibit markedly different immunogenicity profiles. LNPs primarily stimulate innate immune responses through interactions with pattern recognition receptors, but generally do not elicit pre-existing vector-specific immunity [18] [24]. The transient nature of CRISPR delivery via LNPs limits the duration of immune exposure, reducing the likelihood of sustained adaptive immune responses against Cas9. Clinical evidence from Intellia Therapeutics' trials demonstrates that LNP-delivered CRISPR systems enable re-dosing—an option largely precluded with viral vectors due to neutralizing antibody development [18].
Table 1: Comparative Immunogenicity Profiles of CRISPR Delivery Vectors
| Immune Parameter | Viral Vectors (rAAV) | Non-Viral Vectors (LNPs) |
|---|---|---|
| Pre-existing Immunity | High prevalence of neutralizing antibodies (varies by serotype) [60] | Minimal to no pre-existing immunity [18] |
| Cas9-Specific T-cell Response | Robust CD8+ T-cell activation; hepatocyte apoptosis observed in pre-immunized models [60] | Diminished T-cell activation due to transient expression [24] |
| Antibody Generation | High-titer, persistent anti-Cas9 antibodies [61] | Reduced antibody responses [18] |
| Innate Immune Activation | Moderate; TLR-mediated responses [60] | Moderate; primarily through nucleic acid sensors [24] |
| Re-dosing Potential | Limited by adaptive immune memory [15] | Feasible, as demonstrated in clinical trials [18] |
| Mitigation Strategies | Serotype switching, capsid engineering, immunosuppression [15] | Nucleic acid modifications, optimized formulation [24] |
Pre-existing Immunity to CRISPR Components
Pre-existing immunity to Cas proteins presents a significant challenge, particularly for viral delivery systems that enable prolonged expression. Seroprevalence studies indicate anti-SpCas9 antibodies in 2.5%-95% and anti-SaCas9 antibodies in 4.8%-95% of healthy populations, with variations attributable to geographical factors and assay sensitivity [60]. T-cell responses against Cas9 are even more prevalent, detectable in 57%-95% of healthy donors [60]. This pre-existing cellular immunity poses dual risks: accelerated clearance of edited cells and potential immunopathological reactions.
The clinical significance of pre-existing immunity was demonstrated in a murine study where animals pre-immunized against SaCas9 exhibited hepatocyte apoptosis and failed genome editing following AAV-CRISPR administration [60]. Conversely, LNP-mediated delivery in the landmark case of an infant with CPS1 deficiency allowed multiple therapeutic doses without serious adverse effects, highlighting the tolerability advantage of non-viral platforms [18].
Diagram 1: Immunogenicity Pathways of Viral versus Non-Viral CRISPR Delivery Systems. Viral vectors promote persistent Cas9 expression that activates pre-existing immunity, leading to potential immunotoxicity and clearance of edited cells. Non-viral systems enable transient expression that limits adaptive immune activation, supporting therapeutic tolerance and re-dosing capability.
Genotoxicity Assessment: Structural Variations and Off-Target Effects
On-Target Genotoxic Events
A concerning genotoxicity profile has emerged for CRISPR systems that extends beyond simple off-target edits to include significant on-target structural variations. Conventional short-read sequencing initially underestimated these risks, but advanced genomic techniques have revealed that CRISPR editing can induce kilobase- to megabase-scale deletions, chromosomal translocations, and complex rearrangements [53]. These structural variations (SVs) pose substantial safety concerns, particularly when affecting tumor suppressor genes or oncogenic regulatory elements.
The mechanism underlying these large-scale deletions involves the processing of double-strand breaks (DSBs) by alternative DNA repair pathways. When multiple DSBs occur simultaneously—whether at on-target sites, off-target sites, or a combination—erroneous repair can generate extensive genomic rearrangements [53]. Notably, the use of DNA-PKcs inhibitors to enhance homology-directed repair (HDR), a common strategy for improving editing precision, has been shown to exacerbate these genotoxic outcomes, increasing the frequency of megabase-scale deletions and chromosomal arm losses by up to a thousand-fold [53].
Table 2: Genotoxicity Profiles Across CRISPR Editing Platforms
| Genotoxicity Parameter | CRISPR-Cas9 Nuclease | Base Editors | Prime Editors |
|---|---|---|---|
| Double-Strand Break Formation | High (primary mechanism) [11] | Minimal [15] | Minimal [15] |
| Large Deletions (>1 kb) | Frequent; up to megabase scale [53] | Rare [15] | Rare [15] |
| Chromosomal Translocations | Documented in multiple studies [53] | Not reported | Not reported |
| Off-Target Indels | Common; varies with guide design [53] | Reduced frequency [15] | Lowest reported frequency [15] |
| On-Target Structural Variations | Kilobase- to megabase-scale deletions reported [53] | Minimal evidence | Minimal evidence |
| Therapeutic Examples | Casgevy (SCD, TDT), EDIT-101 (LCA10) [15] | Nme2-ABE8e (hereditary tyrosinemia) [15] | Preclinical development [15] |
Delivery Vector Influence on Genotoxicity
The choice of delivery vector indirectly influences genotoxicity profiles by modulating the duration and intensity of nuclease exposure. Viral vectors, particularly rAAVs, sustain Cas9 expression for extended periods, potentially increasing the cumulative risk of off-target activity and complex genomic rearrangements over time [15]. Additionally, the DNA repair template provided in rAAV-based HDR strategies can itself integrate randomly at off-target sites, creating unintended knock-in events [53].
Non-viral delivery typically results in transient Cas9 expression, theoretically narrowing the window for genotoxic events but requiring higher initial editing efficiency. The LNP delivery platform used in Intellia's hATTR trial demonstrated a favorable safety profile with no reported genotoxic adverse events, suggesting that controlled, transient expression may mitigate some SV risks [18]. However, comprehensive analysis using advanced SV detection methods like CAST-Seq and LAM-HTGTS is necessary for definitive comparative assessment [53].
Diagram 2: Genotoxicity Pathways in CRISPR Genome Editing. Double-strand breaks initiated by CRISPR nucleases are processed through competing DNA repair pathways. Error-prone repair mechanisms like MMEJ can generate significant structural variations, while therapeutic interventions to enhance HDR efficiency may unexpectedly exacerbate these genotoxic outcomes.
Experimental Approaches for Safety Assessment
Standardized Methodologies for Risk Evaluation
Comprehensive safety assessment of CRISPR therapeutics requires orthogonal experimental approaches to evaluate both immunogenicity and genotoxicity. For immunogenicity assessment, standardized protocols include:
T-cell Activation Assays: Peripheral blood mononuclear cells (PBMCs) from healthy donors are cultured with Cas9 protein or peptides, with T-cell activation measured via ELISpot (IFN-γ secretion) or flow cytometry (CD69/CD137 expression) [60]. Positive controls include anti-CD3/anti-CD28 stimulation, while negative controls use irrelevant proteins.
Humoral Immunity Profiling: ELISA-based detection of anti-Cas9 antibodies in human serum samples using recombinant Cas9 proteins as capture antigens. Threshold for positivity is typically established as signal exceeding mean + 3SD of naive controls [60].
In Vivo Immunogenicity Models: C57BL/6 mice receive intramuscular or intravenous CRISPR administration with subsequent analysis of cytokine production, lymphocyte infiltration in tissues, and antigen-specific memory formation [61].
For genotoxicity assessment, advanced genomic methods are essential:
CAST-Seq (Circularization for In Vitro Translocation Sequencing): This method identifies chromosomal translocations and large deletions by ligating sequencing adapters to breakpoint junctions followed by PCR amplification and next-generation sequencing [53]. The protocol involves: (1) extraction of genomic DNA 72 hours post-editing; (2) fragmentation and size selection; (3) adapter ligation; (4) nested PCR with target-specific primers; (5) library preparation and sequencing.
LAM-HTGTS (Linear Amplification-Mediated High-Throughput Genome-Wide Translocation Sequencing): This approach comprehensively maps translocation breakpoints genome-wide through linear amplification using biotinylated primers followed by capture and sequencing [53].
Long-Read Sequencing: Oxford Nanopore or PacBio platforms enable detection of large structural variations that escape conventional short-read sequencing, particularly important for assessing on-target genomic integrity [53].
The Scientist's Toolkit: Essential Reagents for CRISPR Safety Assessment
Table 3: Key Research Reagents for CRISPR Safety Evaluation
| Reagent/Category | Specific Examples | Research Application | Safety Context |
|---|---|---|---|
| Cas9 Variants | SpCas9, SaCas9, HiFi Cas9 [53] [60] | Editing efficiency and specificity assessment | HiFi variants reduce off-target effects but may not prevent on-target SVs |
| Immunogenicity Assays | IFN-γ ELISpot kits, HLA tetramers [60] | T-cell response measurement | Detects pre-existing and therapy-induced cellular immunity |
| Structural Variation Detection | CAST-Seq, LAM-HTGTS kits [53] | Chromosomal rearrangement analysis | Identifies large-scale deletions and translocations missed by amplicon sequencing |
| DNA Repair Modulators | DNA-PKcs inhibitors (AZD7648), 53BP1 inhibitors [53] | HDR efficiency enhancement | DNA-PKcs inhibition increases SV risk; 53BP1 inhibition may be safer |
| Control gRNAs | Predicted high-specificity and low-specificity guides [53] | Off-target risk assessment | Benchmarking against test guides establishes baseline genotoxicity |
| Vector Systems | rAAV serotypes (AAV5, AAV8, AAV9), LNPs [15] [18] | Delivery efficiency comparison | rAAV enables sustained expression; LNPs allow transient activity and re-dosing |
Risk Mitigation Strategies and Future Directions
Engineering Solutions for Enhanced Safety
Innovative engineering approaches are emerging to address the immunogenicity and genotoxicity challenges in CRISPR therapeutics. For viral vectors, strategies include:
Capsid Engineering: Development of synthetic AAV capsids with reduced seroprevalence and enhanced tropism for target tissues [15]. These engineered capsids evade pre-existing immunity while maintaining transduction efficiency.
Compact CRISPR Systems: Utilization of smaller Cas orthologs (CjCas9, SaCas9, Cas12f) and putative ancestors (IscB, TnpB) that fit within AAV packaging constraints while potentially exhibiting reduced immunogenicity [15].
Epitope Masking: Structure-guided mutagenesis of immunodominant Cas9 T-cell epitopes to reduce MHC presentation without compromising enzymatic activity [61].
For genotoxicity mitigation, approaches include:
Editor Selection: Preference for base editors or prime editors that minimize DSB formation when precise editing is required [15]. These systems demonstrate substantially reduced structural variation rates in preclinical models.
Dual rAAV Systems: Split-intein approaches that deliver large CRISPR constructs via dual AAV vectors, reducing the genotoxic burden associated with oversized packaging [15].
Conditional Activation: Self-inactivating CRISPR systems and regulatory circuits that limit editing duration, particularly important for viral delivery platforms [24].
Clinical Translation and Regulatory Considerations
The regulatory landscape for CRISPR therapeutics is evolving alongside the technology. The FDA and EMA now require comprehensive assessment of both on-target and off-target effects, including evaluation of structural genomic integrity [53]. Clinical protocols must incorporate:
Patient Screening: Assessment of pre-existing immunity to both delivery vector and CRISPR components prior to treatment enrollment [60].
Long-Term Monitoring: Extended follow-up periods to detect delayed immune responses or oncogenic transformation resulting from genotoxic events [62].
Risk-Benefit Analysis: Context-dependent safety thresholds, recognizing that life-threatening conditions may justify higher risk tolerance, particularly when targeting non-oncogenic pathways [11].
The recent clinical successes of both viral-delivered (EDIT-101) and non-viral delivered (Intellia's hATTR program) CRISPR therapies demonstrate that safety risks can be managed through thoughtful vector selection and engineering [15] [18]. As the field advances, personalized approaches considering individual immune status and genetic background will further enhance the safety profile of these transformative therapeutics.
The therapeutic application of CRISPR gene editing represents a paradigm shift in treating genetic disorders, with the first approved therapies already demonstrating remarkable clinical success. However, a significant bottleneck remains: the efficient, safe, and scalable delivery of CRISPR components to target cells. The choice between viral and non-viral delivery systems involves critical trade-offs between efficiency, payload capacity, manufacturing complexity, and safety profiles that directly impact clinical translation and commercial viability. Viral vectors, particularly adeno-associated viruses (AAV), offer high transduction efficiency and sustained expression but face limitations in packaging capacity and scalable manufacturing. Non-viral systems, especially lipid nanoparticles (LNPs), provide transient editing with reduced immunogenicity and greater packaging flexibility, enabling more complex CRISPR systems while leveraging manufacturing platforms proven during the COVID-19 pandemic. This guide objectively compares the manufacturing and scalability considerations for both approaches, providing researchers and drug development professionals with critical data for platform selection.
Technical Comparison of Delivery Platforms
Fundamental Characteristics and Manufacturing Workflows
Table 1: Core Characteristics of Viral vs. Non-Viral CRISPR Delivery Systems
| Parameter | Viral Vectors (AAV) | Non-Viral Vectors (LNP) |
|---|---|---|
| Packaging Capacity | Limited (~4.7 kb) [15] [17] | Higher capacity, flexible packaging [17] |
| Editing Duration | Long-term, sustained expression [15] | Transient, reduced off-target risk [17] |
| Manufacturing Platform | Cell-based (HEK293, Sf9); complex purification [15] [63] | Chemical synthesis; scalable modular assembly [18] [17] |
| Immunogenicity | Pre-existing immunity concerns; immune responses to capsid [17] [63] | Lower immunogenicity; allows redosing [18] [17] |
| Tropism/Targeting | Natural tropism; engineered capsids for specificity [15] [63] | Organ-specific targeting (e.g., liver); SORT molecules for tissue specificity [18] [17] |
| Regulatory Precedent | Established gene therapy pathway [17] | mRNA vaccine-established safety profile [17] |
| Key Scalability Challenge | Viral vector production consistency; empty capsids [15] [63] | LNP formulation stability; endosomal escape efficiency [17] |
The manufacturing workflows for both platforms involve distinct processes and challenges. AAV production requires cellular bioreactor systems (using HEK293 cells or baculovirus/Sf9 systems) followed by complex purification steps to remove empty capsids and cellular contaminants [15] [63]. In contrast, LNP manufacturing employs bottom-up chemical assembly through rapid mixing of lipids with CRISPR cargo (mRNA, ribonucleoprotein) in microfluidic devices, creating nanoparticles through self-assembly [17]. This fundamental difference in production methodology significantly impacts scalability, cost structure, and quality control requirements.
Quantitative Performance Data from Clinical Applications
Table 2: Clinical Performance Comparison in Selected Trials
| Therapeutic Application | Delivery System | Editing Efficiency | Clinical Outcomes | Manufacturing Implications |
|---|---|---|---|---|
| hATTR (Intellia) [18] | LNP (systemic) | ~90% reduction in TTR protein | Sustained response at 2 years; redosing possible | Single-dose administration; scalable LNP production |
| Hereditary Angioedema [18] | LNP (systemic) | 86% reduction in kallikrein | 8/11 patients attack-free (16 weeks) | Consistent batch manufacturing |
| LCA10 (EDIT-101) [15] | AAV5 (subretinal) | Improved photoreceptor function | Favorable safety; limited efficacy | Local administration; complex intraocular manufacturing |
| Personalized CPS1 Deficiency [18] | LNP (systemic) | Symptom improvement after 3 doses | Multiple safe redoses | Rapid development (6 months) |
| Sickle Cell Disease (Casgevy) [11] [63] | Ex vivo (electroporation) | N/A (ex vivo) | 96.7% elimination of vaso-occlusive crises | Complex autologous manufacturing |
Recent clinical data demonstrates that LNP-mediated in vivo delivery achieves therapeutic-level editing (85-90% protein reduction) in hepatic targets like hATTR and HAE [18]. The ability to safely administer multiple doses - as demonstrated in the personalized CPS1 deficiency case and Intellia's hATTR trial - represents a significant advantage over AAV systems, where immune responses typically prevent redosing [18]. For AAV systems, the subretinal delivery of EDIT-101 for LCA10 demonstrated good safety but highlighted the challenges of achieving sufficient editing efficiency in human trials, contributing to the discontinuation of further enrollment [15].
Manufacturing Processes and Scalability Assessment
Viral Vector Manufacturing Complexities
AAV manufacturing faces substantial scalability challenges due to biological production constraints. The process requires sophisticated cell culture systems and is limited by:
- Plasmid Complexity: Triple transfection systems require GMP-grade plasmid production for rep, cap, and vector genome [63]
- Empty Capsid Ratio: Consistent production of fully-packaged vectors is challenging; empty capsids must be removed via sophisticated chromatography [63]
- Product-Related Impurities: Host cell proteins and DNA necessitate multiple purification steps, reducing yields [15] [63]
- Analytical Characterization: Comprehensive quality control includes titering, potency, full/empty capsid ratio, and vector genome integrity [63]
Recent engineering advances include optimized capsids with enhanced tissue specificity and reduced immunogenicity, and self-complementary AAV designs that improve transduction efficiency but further reduce packaging capacity [63]. For CRISPR applications, the limited ~4.7 kb payload capacity necessitates creative solutions such as dual-vector systems or compact editors like SaCas9 and CasMINI, which introduce additional manufacturing complexity [15] [63].
Non-Viral Manufacturing Advantages and Limitations
LNP manufacturing benefits from established scalable platforms refined for mRNA vaccines, with distinct advantages for CRISPR delivery:
- Modular Production: Lipids and CRISPR cargo are produced separately then combined in microfluidic mixers, simplifying quality control [17]
- Flexible Payloads: LNPs efficiently deliver multiple cargo types (mRNA, guide RNA, RNP) without size constraints of AAV [17]
- Rapid Formulation: Process from components to finished product requires days rather than weeks [18] [17]
- Thermal Stability: LNPs generally demonstrate better stability than viral vectors
The primary technical challenge remains endosomal escape efficiency - only a small fraction of LNPs successfully release their cargo into the cytoplasm [17] [13]. Additionally, while liver-targeted delivery is efficient, targeting other tissues requires further development of SORT (Selective ORgan Targeting) molecules [17].
Experimental Protocols and Workflows
Protocol: AAV-CRISPR Vector Production and Quality Control
This protocol outlines the production of recombinant AAV vectors for CRISPR delivery based on current Good Manufacturing Practice (cGMP) standards [15] [63]:
Materials and Reagents:
- HEK293 cell line (suspension or adherent)
- Three plasmid system: Rep/Cap, Adenoviral Helper, CRISPR Transfer Vector
- Polyethylenimine (PEI) transfection reagent
- Benzonase for host DNA digestion
- Iodixanol gradient solutions
- Anion exchange chromatography resins
- Empty capsid separation matrix (e.g., POROS CaptureSelect)
Methodology:
- Cell Expansion: Culture HEK293 cells in appropriate bioreactor system to target density
- Triple Transfection: Co-transfect with three plasmid system at optimized ratios
- Harvest: Collect cells and media 72 hours post-transfection
- Clarification: Remove cell debris via filtration and centrifugation
- Nuclease Treatment: Incubate with Benzonase to degrade unprotected nucleic acids
- Purification: Initial concentration via tangential flow filtration followed by iodixanol gradient ultracentrifugation
- Empty Capsid Removal: Apply anion exchange chromatography to separate full and empty capsids
- Formulation: Exchange buffer to final formulation via dialysis or diafiltration
- Sterile Filtration: 0.22 μm filtration and fill into final containers
Quality Control Assays:
- Titer Determination: qPCR for vector genome titer, ELISA for capsid titer
- Potency: Transduction assay in permissive cell line
- Purity: SDS-PAGE, silver staining, host cell protein ELISA
- Safety: Sterility, endotoxin, replication-competent AAV testing
Protocol: LNP-CRISPR Formulation and Characterization
This protocol describes LNP formulation for CRISPR ribonucleoprotein (RNP) or mRNA delivery based on current clinical approaches [18] [17]:
Materials and Reagents:
- Ionizable cationic lipid (e.g., DLin-MC3-DMA, SM-102)
- Helper lipids (DSPC, cholesterol, PEG-lipid)
- CRISPR cargo (purified RNP complex or mRNA)
- Microfluidic mixing device (e.g., NanoAssemblr, staggered herringbone mixer)
- Tangential flow filtration system
- Dynamic light scattering instrument
Methodology:
- Lipid Preparation: Dissolve lipid mixture in ethanol at precise molar ratios
- Aqueous Phase Preparation: Dilute CRISPR cargo in citrate buffer (pH 4.0)
- Microfluidic Mixing: Rapidly mix organic and aqueous phases at optimized flow rate ratios (typically 3:1 aqueous:organic)
- Buffer Exchange: Dialyze against PBS or formulation buffer to remove ethanol
- Concentration: Concentrate via tangential flow filtration to target concentration
- Sterile Filtration: 0.22 μm filtration under aseptic conditions
Quality Control Assays:
- Particle Size: Dynamic light scattering (target 70-100 nm)
- Polydispersity Index: <0.2 indicates monodisperse population
- Encapsulation Efficiency: Ribogreen assay for nucleic acid cargo
- Potency: In vitro editing assay in target cells
- Sterility: Membrane filtration and microbiological testing
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for CRISPR Delivery Studies
| Reagent Category | Specific Examples | Research Application | Manufacturing Consideration |
|---|---|---|---|
| Compact Cas Proteins | SaCas9, CjCas9, CasMINI, Cas12f [15] | Enables AAV packaging with gRNA | Smaller size facilitates all-in-one AAV vectors |
| Ionizable Lipids | DLin-MC3-DMA, SM-102, ALC-0315 [17] | LNP formulation; enables endosomal escape | Scalable chemical synthesis; regulatory approval history |
| AAV Serotypes | AAV2, AAV5, AAV8, AAV9, AAVrh.10 [15] [63] | Tissue-specific targeting | Different purification challenges; varying yields |
| Chemical Modifications | Pseudouridine (mRNA), 2'-O-methyl (gRNA) [17] | Enhances stability and reduces immunogenicity | Additional manufacturing steps; quality control complexity |
| SORT Molecules | Tissue-specific targeting ligands [17] | Enhances LNP delivery beyond liver | Additional characterization requirements |
| Purification Tags | HIS-tag, FLAG-tag on Cas proteins [63] | Facilitates RNP complex purification | Potential immunogenicity concerns for clinical use |
| Analytical Standards | NISTmAb, reference materials [63] | Quality control standardization | Critical for manufacturing consistency |
The choice between viral and non-viral delivery systems for CRISPR therapeutics involves multidimensional considerations beyond simple efficiency metrics. AAV vectors provide superior transduction efficiency and sustained expression but face significant manufacturing constraints related to packaging capacity, production scalability, and immunogenicity that limit their application for larger CRISPR systems or repeat dosing. LNP systems offer manufacturing advantages with proven scalability, flexible packaging, and redosing capability, but require optimization for tissue-specific delivery beyond the liver and improved endosomal escape efficiency.
For research applications requiring persistent editing in easily transduced cells, AAV systems remain valuable despite manufacturing complexities. For clinical translation where scalable production, redosing flexibility, and delivery of larger CRISPR payloads (base editors, prime editors) are priorities, LNP platforms present compelling advantages. The recent clinical success of LNP-delivered CRISPR therapeutics for hepatic targets demonstrates this platform's viability for in vivo genome editing. Future advancements in vector engineering, including targeted AAV capsids and tissue-specific LNPs, will continue to narrow the performance gap while manufacturing innovations will address current scalability limitations across both platforms.
The year 2025 marks a pivotal moment for CRISPR-based therapeutics, characterized by a dynamic interplay between groundbreaking clinical successes and evolving market forces. The field has moved from promise to reality with the first regulatory approvals of CRISPR medicines, validating the technology's therapeutic potential while also highlighting the critical challenges that remain. The central thesis framing current development strategies is the comparative efficiency and safety of viral versus non-viral delivery systems for in vivo and ex vivo applications. As of early 2025, the CRISPR medicine landscape monitors approximately 250 clinical trials involving gene-editing therapeutic candidates, with more than 150 trials currently active [64]. This robust pipeline is navigating a complex environment where scientific progress is increasingly influenced by commercial considerations, including tightened venture capital investment and significant shifts in government research funding [18].
The choice of delivery vector—whether viral or non-viral—is no longer merely a technical experimental parameter but a core strategic decision that dictates regulatory pathway, manufacturing complexity, scalability, and ultimately, commercial viability. This analysis provides a comprehensive regulatory and commercial outlook by examining approved therapies and the ongoing clinical trials of 2025, with a specific focus on how delivery system selection is shaping the future of CRISPR medicine.
Approved CRISPR Therapies: Delivery Paradigms and Regulatory Precedents
Casgevy (exagamglogene autotemcel)
Casgevy, developed through collaboration between CRISPR Therapeutics and Vertex Pharmaceuticals, represents the historic first approval of a CRISPR-based therapy, validating the entire field [65]. This ex vivo therapy treats sickle cell disease (SCD) and transfusion-dependent beta thalassemia (TBT) by editing a patient's own hematopoietic stem cells to produce fetal hemoglobin [66].
- Delivery Mechanism: Casgevy utilizes ex vivo electroporation of ribonucleoprotein (RNP) complexes [9]. This non-viral approach involves extracting patient CD34+ hematopoietic stem cells, editing them outside the body using preassembled Cas9 protein and guide RNA complexes, and then reinfusing the modified cells back into the patient.
- Regulatory and Commercial Significance: The approval pathway for Casgevy established critical precedents for ex vivo cell therapies using non-viral delivery. The RNP delivery method was advantageous from a regulatory perspective due to its transient activity, which minimizes off-target effects and reduces the risk of persistent immunogenicity [9] [17]. From a commercial standpoint, the ex vivo approach bypasses the complex biodistribution and targeting challenges associated with in vivo delivery, though it introduces significant logistical and cost challenges related to cell processing and personalized manufacturing.
Comparative Analysis of Delivery Systems in Approved Therapies
Table 1: Delivery System Comparison in Approved CRISPR Therapies
| Therapy | Indication | Delivery Method | Delivery Format | Regulatory Status | Key Advantage |
|---|---|---|---|---|---|
| Casgevy | SCD, TBT | Ex vivo electroporation | RNP | Approved in US, EU, UK | Transient editing, minimal off-target effects |
| Exa-cel | SCD, β-thalassemia | Ex vivo electroporation | RNP | Approved [66] | Avoids viral vector immunogenicity |
The exclusive use of non-viral RNP delivery in approved therapies highlights the regulatory comfort with this approach's safety profile, particularly the reduced risk of insertional mutagenesis and controllable editing window. The ex vivo paradigm has proven commercially viable for serious monogenic disorders despite its complexity and high cost, with companies making progress on reimbursement arrangements with state Medicaid programs and national health systems [18].
2025 Clinical Trial Landscape: Viral vs. Non-Viral Delivery Trends
Analysis of Current Clinical Trials by Delivery System
The 2025 clinical trial landscape reveals a diversified approach to delivery systems, with both viral and non-viral vectors advancing through clinical stages. The choice of delivery system increasingly correlates with specific therapeutic areas and administration routes.
Table 2: 2025 Clinical Trial Trends by Delivery System and Therapeutic Area
| Delivery System | Therapeutic Area | Representative Therapies | Phase | Key Developments |
|---|---|---|---|---|
| LNP (mRNA) | Hereditary Amyloidosis | NTLA-2001 (Intellia) [18] | Phase III | ~90% protein reduction sustained at 2 years |
| LNP (mRNA) | Hereditary Angioedema | NTLA-2002 (Intellia) [18] | Phase I/II | 86% kallikrein reduction, 8/11 patients attack-free |
| AAV | Duchenne Muscular Dystrophy | HG-302 (HuidaGene) [67] | Phase I | Uses compact hfCas12Max for single AAV delivery |
| LNP (Base Editing) | Hypercholesterolemia | VERVE-102 (Verve) [67] | Phase Ib | GalNAc-LNP delivery showing promising early safety |
| Ex Vivo RNP | Autoimmune Diseases | CTX112 (CRISPR Tx) [66] | Phase I | Allogeneic CAR-T for autoimmune applications |
| Bacteriophage | Bacterial Infections | SNIPR Biome, Locus Biosciences [18] | Phase I/II | CRISPR-enhanced phages against E. coli and UTIs |
In Vivo Non-Viral Delivery Advances
Lipid Nanoparticles (LNPs) have emerged as the leading platform for in vivo CRISPR delivery, particularly for liver-targeted diseases. The 2025 landscape shows remarkable progress:
- Redosability: Intellia Therapeutics reported the first-ever redosing of an in vivo CRISPR therapy in their hATTR trial, with participants safely receiving a second infusion at higher doses [18]. This addresses a historical limitation of viral vectors, which typically trigger immune responses that prevent redosing.
- Liver Tropism: LNPs naturally accumulate in the liver, making them ideal for diseases where therapeutic proteins are produced in hepatocytes. Programs targeting ANGPTL3 (CTX310), Lp(a) (CTX320), AGT (CTX340), and ALAS1 (CTX450) all exploit this natural targeting [66].
- Personalized Medicine Applications: In a landmark case, researchers developed a personalized in vivo CRISPR treatment for an infant with CPS1 deficiency using LNP delivery in just six months, setting a regulatory precedent for rapid approval of bespoke therapies [18].
Viral Vector Evolution in Clinical Trials
Adeno-Associated Viruses (AAVs) continue to play important roles in clinical development, particularly for tissues beyond the liver:
- Capsid Engineering: Advances in AAV capsid evolution are enabling better targeting of specific tissues, with clinical candidates like HG-302 for Duchenne Muscular Dystrophy using engineered Cas12Max nucleases that fit within AAV cargo constraints [9] [67].
- Safety Refinements: The field is addressing immunogenicity concerns through improved capsid designs and empty capsid removal techniques, though manufacturing complexity remains a challenge compared to LNP platforms.
Emerging Delivery Platforms
Bacteriophage delivery represents a novel approach advancing through clinical trials in 2025. Companies including SNIPR Biome and Locus Biosciences are testing CRISPR-enhanced phages against dangerous bacterial infections like E. coli and urinary tract infections, showing positive results in early trials [18] [64]. This approach leverages the natural specificity of phages for bacterial targets, using CRISPR to enhance their antibacterial potency.
Experimental Protocols and Methodology
LNP Formulation and In Vivo Delivery Protocol
The following methodology is representative of approaches used in current clinical trials for liver-targeted LNP delivery:
Materials Required:
- Ionizable lipids (e.g., DLin-MC3-DMA) for encapsulation efficiency
- Helper lipids (cholesterol, DSPC) for membrane stability
- PEG-lipids for nanoparticle stealth properties
- Cas9 mRNA and sgRNA targeting the gene of interest
- Microfluidic mixer for precise LNP formation
Procedure:
- Prepare lipid mixture in ethanol phase at precise molar ratios (typically 50:10:38.5:1.5 ionizable lipid:DSPC:cholesterol:PEG-lipid)
- Prepare aqueous phase containing Cas9 mRNA and sgRNA in citrate buffer (pH 4.0)
- Combine phases using microfluidic mixing at controlled flow rate ratios (typically 3:1 aqueous:ethanol)
- Dialyze against PBS (pH 7.4) to remove ethanol and establish neutral pH
- Characterize LNPs for size (70-100 nm ideal), polydispersity (<0.2), and encapsulation efficiency (>90%)
- Administer via intravenous injection at dosage 0.5-3.0 mg RNA/kg body weight
- Assess editing efficiency via plasma protein reduction (e.g., TTR, ANGPLT3) at 2-week intervals [18] [68]
Ex Vivo RNP Electroporation Protocol
This protocol mirrors the approach used in approved therapies like Casgevy and current ex vivo trials:
Materials Required:
- Patient-derived CD34+ hematopoietic stem cells or T cells
- Recombinant Cas9 protein with nuclear localization signals
- In vitro transcribed sgRNA or synthetic sgRNA for higher purity
- Electroporation system (e.g., Lonza 4D-Nucleofector)
- Cell culture media with cytokines for maintenance post-editing
Procedure:
- Isolate and activate target cells (typically 1-10 million cells per condition)
- Precomplex Cas9 protein and sgRNA at 3:1 molar ratio in PBS to form RNP complexes (incubate 10-20 minutes at room temperature)
- Mix cell suspension with RNP complexes in electroporation cuvettes
- Electroporate using optimized program (e.g., pulse code DZ-113 for hematopoietic cells)
- Immediately transfer cells to recovery media with Rho-kinase inhibitor (Y-27632) to enhance viability
- Culture cells for 48-72 hours before assessing editing efficiency (T7E1 assay or NGS)
- Expand edited cells or administer directly to patient after quality control checks [9] [17]
Technical and Commercial Challenges in Delivery System Implementation
Manufacturing and Scalability Considerations
The translation from clinical success to commercial viability heavily depends on manufacturing scalability:
- LNP Production: While LNP manufacturing benefits from established infrastructure (thanks to COVID-19 vaccine development), scaling to commercial volumes while maintaining batch-to-batch consistency presents challenges, particularly for complex organ-targeted formulations beyond the liver [68].
- Viral Vector Production: AAV and lentiviral vector manufacturing remains complex and expensive, with limited global capacity creating supply chain vulnerabilities. The requirement for cell-based production systems introduces more variables than synthetic LNP formation [9].
- Ex Vivo Processing: Therapies like Casgevy require sophisticated cell processing facilities and logistics chains, limiting treatment centers to major medical institutions and impacting patient access [18].
Vector-Related Toxicity and Immunogenicity
Delivery system safety profiles continue to evolve through clinical experience:
- LNP-Related Toxicities: Mild-to-moderate infusion-related reactions are commonly observed with LNP administration, though these are generally manageable with premedication [18]. The potential for complement activation-related pseudoallergy (CARPA) remains a consideration in susceptible populations.
- AAV Immune Responses: While AAVs generally exhibit lower immunogenicity than other viral vectors, pre-existing immunity in patient populations and the development of neutralizing antibodies post-administration can limit efficacy, particularly for redosing [9] [17].
- Insertional Mutagenesis Risks: Lentiviral vectors carry theoretical risks of insertional mutagenesis, though improved designs and manufacturing have substantially mitigated this concern. Integration-deficient lentiviral vectors (IDLVs) are being developed to further reduce this risk [9].
Decision Framework for Delivery System Selection
The choice between viral and non-viral delivery systems involves multiple technical, regulatory, and commercial considerations. The following workflow outlines the key decision points:
Diagram: CRISPR Delivery System Selection Workflow
Essential Research Reagents and Solutions
The following toolkit represents critical materials required for implementing the delivery systems discussed in this review:
Table 3: Research Reagent Solutions for CRISPR Delivery Studies
| Reagent/Solution | Function | Example Applications | Key Considerations |
|---|---|---|---|
| Ionizable Lipids | LNP self-assembly and endosomal escape | In vivo liver targeting [68] | Optimized pKa for endosomal release; liver tropism |
| Cationic Polymers | Nucleic acid complexation and protection | Polyplex formation for DNA delivery [17] | Molecular weight and charge density affect toxicity |
| Electroporation Systems | Temporary membrane permeabilization | Ex vivo RNP delivery to hematopoietic cells [9] | Cell-type specific optimization of voltage and pulse length |
| AAV Serotypes | Tissue-specific transduction | CNS, muscle, and retinal targeting [9] [17] | Pre-existing immunity screening; tissue tropism matching |
| Cas9 Variants | Size-optimized for viral packaging | AAV delivery with SaCas9 [9] | Balancing size constraints with editing efficiency |
| Cell-Penetrating Peptides | Enhanced cellular uptake | RNP delivery to difficult-to-transfect cells [17] | Sequence optimization to minimize cytotoxicity |
| Inducible Systems | Temporal control of editing | Tetracycline/doxycycline-inducible Cas9 [9] | Leakiness minimization; rapid induction kinetics |
The regulatory and commercial landscape for CRISPR therapeutics in 2025 reflects a field in transition from initial proof-of-concept to mature therapeutic platform. The comparative analysis of viral and non-viral delivery systems reveals a nuanced picture where each approach finds its strategic niche based on therapeutic indication, target tissue, and commercial considerations.
Non-viral delivery, particularly LNP-based platforms, has gained substantial momentum for in vivo applications, driven by favorable safety profiles, redosing capability, and manufacturing scalability. The clinical success of liver-targeted LNP programs has established a clear pathway for additional indications, with the personalized CRISPR treatment for CPS1 deficiency demonstrating unprecedented regulatory flexibility for bespoke therapies [18].
Viral vectors, particularly AAVs, maintain important roles for tissues beyond the liver and for applications requiring more persistent expression. Continued innovation in capsid engineering and manufacturing is addressing immunogenicity and scalability challenges.
The commercial environment presents both opportunities and constraints, with market forces pushing companies to narrow their pipelines and focus on getting products to market quickly [18]. This commercial pressure, combined with concerning trends in government research funding, may impact the diversity of future therapeutic approaches.
As the field progresses, the delivery system selection will continue to be the critical determinant of both clinical success and commercial viability, with the optimal choice dependent on a complex interplay of biological, regulatory, and economic factors that extend far beyond simple editing efficiency metrics.
Conclusion
The choice between viral and non-viral delivery vectors is not a matter of declaring a single winner, but rather of strategic selection based on the specific therapeutic application. Viral vectors, particularly AAVs, offer high transduction efficiency and持久 expression but are constrained by immunogenicity and cargo size. Non-viral methods, especially LNPs, have emerged as powerful, safer alternatives for transient delivery with reduced immunogenicity, proven by recent in vivo clinical successes. Future directions will focus on developing next-generation, cell-specific non-viral platforms, overcoming cargo limitations with engineered Cas variants, and establishing more sensitive assays to quantify complex genomic rearrangements. The ongoing clinical progress, including the landmark approval of CASGEVY and promising in vivo trials, underscores that efficient and safe delivery remains the critical gateway to unlocking the full therapeutic potential of CRISPR across a broader spectrum of diseases.
References
- 1. CRISPR/Cas9 Delivery Systems to Enhance Gene Editing ... [https://www.mdpi.com/1422-0067/26/9/4420]
- 2. Non-viral delivery of CRISPR–Cas9 complexes for targeted ... [https://www.nature.com/articles/s41434-021-00282-6]
- 3. Viral or Nonviral: Which Is Better for CRISPR-Based ... [https://www.genengnews.com/topics/genome-editing/viral-or-nonviral-which-is-better-for-crispr-based-therapies/]
- 4. A comparison of three different delivery methods for ... [https://www.frontiersin.org/journals/plant-science/articles/10.3389/fpls.2023.1111110/full]
- 5. Non-viral delivery systems for CRISPR/Cas9-based genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5944364/]
- 6. Adeno-Associated Viral (AAV) Vector Guide [https://www.addgene.org/guides/aav/]
- 7. Viral and Non-Viral Systems to Deliver Gene Therapeutics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11242246/]
- 8. Viral Vectors for the in Vivo Delivery of CRISPR Components [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.895713/full]
- 9. CRISPR This Way: Choosing Between Delivery System [https://en.vectorbuilder.com/resources/vector-academy/lessons/crispr-delivery-systems.html]
- 10. Systemic nanoparticle delivery of CRISPR-Cas9 ... [https://www.nature.com/articles/s41467-020-17029-3]
- 11. Advancing CRISPR genome editing into gene therapy clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12094669/]
- 12. Unlocking Genome Editing: Advances and Obstacles in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11595195/]
- 13. Overcoming the Delivery Challenges in CRISPR/Cas9 ... [https://www.medsci.org/v22p3625.htm]
- 14. CRISPR-Cas9-mediated homology-directed repair for ... [https://www.sciencedirect.com/science/article/pii/S2162253124002312]
- 15. innovations and challenges in rAAV vector-based CRISPR ... [https://www.nature.com/articles/s41434-025-00573-2]
- 16. Unlocking mRNA-driven CRISPR-Cas9 gene therapy via ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12594903/]
- 17. CRISPR Delivery Methods: Cargo, Vehicles, and Challenges [https://www.synthego.com/blog/delivery-crispr-cas9/]
- 18. CRISPR Clinical Trials: A 2025 Update [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 19. Scientists just made CRISPR three times more effective [https://www.sciencedaily.com/releases/2025/09/250907024543.htm]
- 20. CMN Weekly (10 October 2025) [https://crisprmedicinenews.com/news/cmn-weekly-10-october-2025-your-weekly-crispr-medicine-news/]
- 21. CMN Weekly (31 October 2025) [https://crisprmedicinenews.com/news/cmn-weekly-31-october-2025-your-weekly-crispr-medicine-news/]
- 22. Efficient protoplast isolation and transfection for CRISPR ... [https://link.springer.com/article/10.1007/s11240-025-03198-w]
- 23. Challenges and Opportunities in the Application of CRISPR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12503735/]
- 24. CRISPR-Cas9 Gene Therapy: Non-Viral Delivery and Stimuli ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11820414/]
- 25. CRISPR/Cas9 gene editing strategy for cancer therapy [https://www.sciencedirect.com/science/article/abs/pii/S0141813025089469]
- 26. Measurement and clinical interpretation of CRISPR off- ... [https://www.nature.com/articles/s41588-025-02428-3]
- 27. AAV vs Lentivirus Resources - BioInnovatise [https://bioinnovatise.com/articles/aav-vs-lentivirus-which-viral-vector-is-right-for-my-research/]
- 28. Adeno-Associated Virus Vectors in Retinal Gene Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12292589/]
- 29. AAV Vs. Lentiviral Vectors - Life in the Lab [https://www.thermofisher.com/blog/life-in-the-lab/aav-vs-lv/]
- 30. Customizable virus-like particles deliver CRISPR–Cas9 ... [https://www.nature.com/articles/s41565-024-01851-7]
- 31. In-vivo-targeted gene delivery using adenovirus-antibody ... [https://www.sciencedirect.com/science/article/pii/S2329050125000920]
- 32. AAV Vector Design Service for In Vivo Genome Editing [https://www.creative-biolabs.com/gene-therapy/aav-vector-design-service-in-vivo-genome-editing.htm]
- 33. Trends and challenges of AAV-delivered gene editing ... [https://www.sciencedirect.com/science/article/pii/S2162253125001891]
- 34. Cross-species tropism of AAV.CPP.16 in the respiratory tract ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12208343/]
- 35. Advancing AAV production with high-throughput screening ... [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/3254/advancing-aav-production-with-highthroughput-screening-and-transcriptomics]
- 36. Emerging non-viral vectors for gene delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10433663/]
- 37. Nanodelivery of nucleic acids [https://www.nature.com/articles/s43586-022-00104-y]
- 38. Comparison of Lipid Nanoparticles vs Polymer Carriers [https://eureka.patsnap.com/report-comparison-of-lipid-nanoparticles-vs-polymer-carriers]
- 39. CRISPR Technologies for In Vivo and Ex Vivo Gene Editing [https://www.ncbi.nlm.nih.gov/books/NBK609557/]
- 40. Can CRISPR Build on Casgevy's Success With Its In Vivo ... [https://finance.yahoo.com/news/crispr-build-casgevys-success-vivo-125500765.html]
- 41. Viral and nonviral nanocarriers for in vivo CRISPR-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12341846/]
- 42. /Cas9 CRISPR Systems to Enhance Gene Editing Delivery ... Efficiency [https://pmc.ncbi.nlm.nih.gov/articles/PMC12072885/]
- 43. Delivering the Message: Translating mRNA Therapy for Liver ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12361847/]
- 44. Versatility of LNPs across different administration routes for ... [https://pubs.rsc.org/en/content/articlehtml/2025/tb/d5tb00575b]
- 45. Viral Vector vs CRISPR Resources [https://bioinnovatise.com/articles/viral-vector-vs-crispr/]
- 46. A modular strategy for extracellular vesicle-mediated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12639036/]
- 47. Delivery Strategies of the CRISPR-Cas9 Gene-Editing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5723556/]
- 48. CRISPR/Cas Systems: Biological Formats and Delivery ... [https://www.yeasenbio.com/blogs/enzyme/crispr-cas-systems-biological-formats-and-delivery-strategies-for-genome-editing]
- 49. Optimizing CRISPR delivery for drug discovery [https://www.drugdiscoverynews.com/optimizing-crispr-delivery-for-drug-discovery-16487]
- 50. Protocol to rapidly screen CRISPR-Cas9 gene editing ... [https://www.sciencedirect.com/science/article/pii/S2666166725003569]
- 51. Cell-Specific Single Viral Vector CRISPR/Cas9 Editing and ... [https://www.eneuro.org/content/11/7/ENEURO.0438-23.2024]
- 52. Tissue-Specific Delivery of CRISPR Therapeutics [https://pmc.ncbi.nlm.nih.gov/articles/PMC7583726/]
- 53. The hidden risks of CRISPR/Cas: structural variations and ... [https://www.nature.com/articles/s41467-025-62606-z]
- 54. Press Release [https://ir.crisprtx.com/news-releases/news-release-details/crispr-therapeutics-provides-business-update-and-reports-third-6]
- 55. Precision gene editing: The power of CRISPR-Cas in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590234/]
- 56. Off-target effects in CRISPR-Cas genome editing for ... [https://www.sciencedirect.com/science/article/pii/S2162253125001908]
- 57. Recent Advances in CRISPR/Cas9 Delivery Approaches for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10661828/]
- 58. Viral vs. Non-Viral Gene Delivery: A Critical Choice for ... [https://www.drugdiscoverynews.com/viral-vs-non-viral-gene-delivery-a-critical-choice-for-gene-therapy-developers-16819]
- 59. In Vivo [https://crisprtx.com/focus-areas/in-vivo]
- 60. Immunogenicity of CRISPR therapeutics—Critical ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2023.1138596/full]
- 61. Peeling back the layers of immunogenicity in Cas9-based ... [https://www.sciencedirect.com/science/article/pii/S1525001625005350]
- 62. Non-clinical safety considerations on genome editing using ... [https://www.sciencedirect.com/science/article/pii/S2352304225002740]
- 63. Engineering adeno-associated viral vectors for CRISPR ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961225002339]
- 64. Overview CRISPR Clinical Trials 2025 - Learn | Innovate [https://crisprmedicinenews.com/clinical-trials/]
- 65. Casgevy [https://crisprtx.com/therapies]
- 66. Pipeline [https://crisprtx.com/pipeline]
- 67. CRISPR Clinical Trials to Follow [https://www.synthego.com/blog/crispr-clinical-trials/]
- 68. CRISPR/Cas9 Delivery Systems to Enhance Gene Editing ... [https://pubmed.ncbi.nlm.nih.gov/40362657/]