Beyond PICADAR: Addressing Diagnostic Gaps and False Negatives in Primary Ciliary Dyskinesia
This article examines the significant limitations of the PICADAR predictive tool in identifying Primary Ciliary Dyskinesia (PCD), particularly its concerning false-negative rates in patients without classic laterality defects or hallmark...
Beyond PICADAR: Addressing Diagnostic Gaps and False Negatives in Primary Ciliary Dyskinesia
Abstract
This article examines the significant limitations of the PICADAR predictive tool in identifying Primary Ciliary Dyskinesia (PCD), particularly its concerning false-negative rates in patients without classic laterality defects or hallmark ultrastructural abnormalities. Recent evidence reveals PICADAR's sensitivity can be as low as 59-61% in these subgroups, potentially delaying diagnosis and treatment. We explore the pathophysiological and genetic basis for these limitations, evaluate complementary diagnostic methodologies including advanced genetic testing and high-speed video microscopy, and propose optimized, integrated diagnostic algorithms. For researchers and drug development professionals, this synthesis provides critical insights for developing next-generation diagnostic strategies and designing more inclusive clinical trials that account for PCD's full phenotypic spectrum.
Unmasking PICADAR's Blind Spots: The Evidence for Limited Sensitivity
FAQs: Core Performance and Limitations of PICADAR
Recent large-scale studies indicate that the PICADAR tool has significant limitations in sensitivity. A 2025 study of 269 individuals with genetically confirmed PCD found that PICADAR had an overall sensitivity of only 75% when using the recommended cutoff score of ≥5 points. This means the tool would miss approximately one in four true PCD cases [1].
A critical design limitation is that the tool's algorithm begins by excluding all individuals who do not report a daily wet cough. The same 2025 study found that 7% of genetically confirmed PCD patients did not have this symptom and would have been automatically ruled out by PICADAR without further assessment [1].
Q2: How does PICADAR performance vary across different PCD patient subgroups?
PICADAR demonstrates markedly different sensitivity across patient subgroups, with particularly poor performance in certain populations. The table below summarizes the key disparities identified in recent research [1]:
| Subgroup Characteristic | Sensitivity | Median PICADAR Score (IQR) |
|---|---|---|
| Overall PCD Population | 75% (202/269) | 7 (5–9) |
| Patients with laterality defects (e.g., situs inversus) | 95% | 10 (8–11) |
| Patients with situs solitus (normal organ arrangement) | 61% | 6 (4–8) |
| Patients with hallmark ultrastructural defects | 83% | Information missing |
| Patients without hallmark ultrastructural defects | 59% | Information missing |
This data reveals that PICADAR's sensitivity drops substantially in patients without laterality defects or in those with normal ciliary ultrastructure, missing nearly 40% of true PCD cases in these subgroups [1].
Q3: What is the recommended diagnostic workflow when using PICADAR in research?
The following workflow integrates PICADAR into a comprehensive diagnostic strategy while accounting for its known limitations:
Q4: What alternative or complementary screening approaches are available?
Given PICADAR's limitations, a multi-modal screening approach is recommended:
- Nasal Nitric Oxide (nNO) Measurement: Serves as a valuable screening tool, though certain genetic variants can show normal or elevated nNO values, limiting its use as a standalone test [2] [3].
- High-Speed Video Microscopy Analysis (HSVA): Can detect abnormal ciliary beat patterns even when other tests are normal, making it particularly valuable for identifying non-classic PCD presentations [4].
- Clinical Questionnaires: The American Thoracic Society clinical screening questionnaire (ATS-CSQ) represents an alternative, though it also has recognized sensitivity limitations [5].
Essential Research Reagents and Materials for Definitive PCD Diagnosis
Since PICADAR is only a screening tool, definitive PCD diagnosis requires specialized tests available at reference centers. The table below details key reagents and materials used in confirmatory investigations [6]:
| Research Reagent / Solution | Function in PCD Diagnosis |
|---|---|
| Nasal Epithelial Cells | Obtained via nasal brushing for ciliary functional and structural analysis. |
| Culture Media for Air-Liquid Interface (ALI) | Supports differentiation and growth of ciliated epithelial cells from biopsy samples. |
| Glutaraldehyde Fixative | Used for preparing ciliary samples for structural analysis by Transmission Electron Microscopy (TEM). |
| Antibodies for Immunofluorescence (IF) | Target specific ciliary proteins (e.g., DNAH5, GAS8) to detect defects in protein localization. |
| DNA Sequencing Kits (PCD Gene Panel) | Used in genetic testing to identify biallelic mutations in known PCD-causing genes (≥40 genes). |
| Chemiluminescence Analyzer | Essential for measuring low Nasal Nitric Oxide (nNO) levels, a hallmark of PCD. |
Experimental Protocol: Validating PICADAR Performance in Research Cohorts
Methodology for Assessing PICADAR Sensitivity and Specificity
Objective: To evaluate the real-world performance of PICADAR in identifying patients with Primary Ciliary Dyskinesia, particularly across genetic and phenotypic subgroups.
Study Population:
- Recruit patients with clinically suspected PCD or genetically confirmed PCD diagnosis.
- Ensure inclusion of diverse subgroups: patients with and without laterality defects, various genetic mutations, and different ultrastructural defects.
- Collect complete clinical histories for PICADAR parameter assessment [1] [5].
Data Collection:
- PICADAR Scoring: Calculate PICADAR scores for all participants based on seven clinical parameters:
- Full-term gestation (+1 point)
- Neonatal chest symptoms (+2 points)
- Neonatal intensive care unit admission (+1 point)
- Chronic rhinitis (+1 point)
- Ear symptoms (+1 point)
- Situs inversus (+2 points)
- Congenital cardiac defect (+2 points) [6]
- Reference Standard Testing: Perform definitive PCD diagnostic testing:
Statistical Analysis:
- Calculate overall sensitivity and specificity of PICADAR using a ≥5 cutoff point.
- Perform subgroup analyses stratifying by presence of laterality defects and ultrastructural abnormalities.
- Use statistical tests (e.g., chi-square) to compare sensitivity across subgroups [1].
Implementation Considerations:
- Account for potential recall bias, particularly for neonatal events in adult patients.
- Ensure blinding of personnel performing reference standard tests to PICADAR results.
- Collaborate with specialized PCD centers for access to advanced diagnostic techniques [3].
Frequently Asked Questions (FAQs)
FAQ 1: What defines a "high-risk phenotype" in the context of PCD and situs solitus? A high-risk phenotype for PCD, in this context, refers to a patient who has a classic clinical presentation of PCD but possesses two key features that can lead to a false-negative diagnostic result: situs solitus (the normal arrangement of thoracic and abdominal organs) and normal ciliary ultrastructure upon transmission electron microscopy (TEM) analysis [4] [7]. This specific combination is high-risk because it is frequently missed by standard diagnostic algorithms like PICADAR and some diagnostic guidelines, leaving the patient undiagnosed [4].
FAQ 2: Why does the PICADAR clinical score produce false negatives in this specific patient group? The PICADAR tool uses clinical features to identify patients requiring further testing for PCD. It has high sensitivity but lower specificity [4]. A core clinical feature included in some scoring systems is situs inversus (a mirror-image arrangement of organs), which is a strong indicator of PCD. Patients with situs solitus lack this major red flag. Consequently, when a patient has situs solitus and normal ultrastructure, their clinical score may fall below the threshold for positive screening, or they may not be referred for the full battery of necessary tests, leading to a false-negative result [4].
FAQ 3: What is the recommended diagnostic pathway for a suspected high-risk phenotype? The European Respiratory Society (ERS) guidelines recommend a multi-modal approach [4]. If clinical history is strong, do not exclude PCD based on a single normal test. The pathway should include:
- Nasal Nitric Oxide (nNO): Should not be used in isolation to exclude PCD, as false negatives are known to occur [4].
- High-Speed Video Analysis (HSVA): Essential for detecting abnormal ciliary beat pattern and frequency, even when ultrastructure is normal [4].
- Genetic Testing: To identify mutations in PCD-associated genes known to cause disease with normal ultrastructure (e.g., DNAH11, GAS8, HYDIN) [4] [7]. The ERS suggests that both nNO and HSVA should be entirely normal before deciding further investigation is not warranted [4].
FAQ 4: Which genetic mutations are commonly associated with this phenotype? Mutations in several genes are linked to PCD with normal ultrastructure. Key genes include:
- DNAH11: A frequently identified mutation in patients with situs solitus and normal TEM [4] [7].
- CCDC103, DNAH9, RSPH1: Identified in patients with a strong clinical history and normal nNO or HSVA, but confirmed PCD via genetics [4].
- GAS8, HYDIN: Genes for which HSVA is particularly critical for diagnosis, as TEM is typically normal [4].
Troubleshooting Guides
Guide 1: Investigating a Patient with Strong Clinical History but Normal nNO and TEM
Problem: A patient exhibits a strong clinical history of PCD (e.g., neonatal respiratory distress, perennial wet cough, chronic otitis media, bronchiectasis) but has situs solitus, normal nNO levels, and normal ciliary ultrastructure on TEM. The initial diagnosis is negative for PCD.
Solution: This is a classic scenario for a false-negative diagnosis. The following actions are recommended:
| Step | Action | Rationale |
|---|---|---|
| 1 | Review HSVA | Ensure that High-Speed Video Analysis has been performed by an experienced accredited center. An abnormal ciliary beat pattern is a key indicator of PCD, even with normal nNO and TEM [4]. |
| 2 | Initiate Genetic Testing | Proceed with next-generation sequencing (NGS) of a known PCD gene panel. Focus on genes associated with normal ultrastructure (e.g., DNAH11, GAS8, HYDIN) [4]. |
| 3 | Correlate Genotype with Phenotype | Ensure that identified genetic variants are pathogenic and compatible with the clinical and functional (HSVA) phenotype. This step is crucial to avoid false-positive genetic results [4]. |
Expected Outcome: A confirmed PCD diagnosis based on a combination of clinical history, abnormal HSVA, and/or identification of biallelic pathogenic mutations in a PCD-associated gene.
Guide 2: Validating Pathogenicity of Genetic Variants of Unknown Significance (VUS)
Problem: Genetic testing has identified biallelic variants of unknown significance (VUS) in a PCD-associated gene in a patient with situs solitus and normal TEM. It is unclear if this is a true PCD diagnosis.
Solution: Pathogenicity must be confirmed through functional and clinical correlation.
| Step | Action | Rationale |
|---|---|---|
| 1 | Functional Studies | Perform immunofluorescence (IF) microscopy to assess the localization and expression of the corresponding protein and other ciliary components. Altered protein localization can support pathogenicity. |
| 2 | Clinical Correlation | Re-evaluate the HSVA and clinical phenotype. Does the ciliary beat pattern defect match what has been previously reported for mutations in this gene? [4] |
| 3 | Segregation Analysis | Test the parents and other family members for the VUS. Finding the variants in trans in an affected individual strongly supports pathogenicity. |
Expected Outcome: Confirmation that the genotype is the cause of the patient's ciliary phenotype, allowing for a definitive diagnosis.
Summarized Data Tables
Table 1: Diagnostic Test Profiles in PCD High-Risk Phenotypes
This table summarizes the expected results of standard PCD diagnostic tests in patients with situs solitus and specific genetic mutations.
| Gene / Mutation | Situs Status | nNO Level | HSVA (Beat Pattern) | Ciliary Ultrastructure (TEM) |
|---|---|---|---|---|
| DNAH11 [4] | Situs Solitus | Low / Normal | Abnormal | Normal |
| RSPH1 [4] | Situs Solitus | Low / Normal | Abnormal | May show subtle defects (e.g., microtubule disorganization) |
| HYDIN [4] | Situs Solitus | Low | Abnormal | Normal |
| GAS8 [4] | Situs Solitus | Low / Normal | Abnormal | Normal |
| CCDC103 [4] | Situs Solitus | Low / Normal | Abnormal | Normal |
| DNAH9 [4] | Situs Solitus | Low / Normal | Abnormal | Normal |
Table 2: Key Genetic Mutations and Associated Cardiac/Renal Anomalies in Situs Solitus
This table links specific genes to the risk of concurrent congenital heart defects (CHD) and congenital anomalies of the kidney and urinary tract (CAKUT), which can be part of a broader ciliopathy phenotype.
| Gene | Chromosome | Proposed Impact / Function | Associated Anomalies (Beyond PCD) |
|---|---|---|---|
| BMP2 [8] | 20p12.3 | Bone morphogenetic protein signaling; crucial for cardiac and skeletal development. | Isolated dextrocardia with situs solitus, short stature, skeletal anomalies. |
| ZFPM2 [9] | 8q23.1 | Ventricular septum morphogenesis. | Cardiac malformations (e.g., TOF, TGA). |
| FOXF1 [9] | 16q24.1 | Endocardial cushion development; regulation of Smoothened signaling. | VACTERL association, cardiac and renal defects. |
| ZIC3 [9] | Xq26.3 | Determination of left/right asymmetry. | Heterotaxy, VACTERL association, CHD. |
| NODAL [9] | 10q22.1 | Determination of left/right asymmetry. | Laterality defects, CHD. |
| GATA4 [9] | 8p23.1 | Cardiac morphogenesis. | Atrioventricular septal defects (AVSD). |
Experimental Protocols
Protocol 1: Comprehensive Diagnostic Workflow for High-Risk PCD Phenotypes
Objective: To systematically diagnose Primary Ciliary Dyskinesia in patients with a strong clinical history but situs solitus and normal or inconclusive initial test results.
Materials: See "Research Reagent Solutions" below. Methodology:
- Clinical Assessment & PICADAR Scoring: Calculate the patient's PICADAR score. Note that a score below the threshold does not rule out PCD in high-risk phenotypes [4].
- Nasal Nitric Oxide (nNO) Measurement: Perform nNO testing according to ATS/ERS standards. A low nNO is supportive, but a normal level cannot rule out PCD [4].
- Ciliary Biopsy and Culture: Obtain a nasal or bronchial brush biopsy. A portion of the sample should be analyzed immediately (for HSVA and initial TEM), and a portion should be cultured to differentiate primary from secondary ciliary dyskinesia.
- High-Speed Video Analysis (HSVA): Record ciliary beat pattern and frequency from freshly harvested ciliated cells. Analysis must be performed by an expert in an accredited center [4].
- Transmission Electron Microscopy (TEM): Process ciliated cells to analyze the internal 9+2 microtubule structure and dynein arms. Document any abnormalities or confirm normal ultrastructure.
- Genetic Analysis: Extract genomic DNA from peripheral blood. Perform whole exome sequencing or targeted NGS using a comprehensive PCD gene panel.
- Data Integration and Diagnosis: Correlate all findings. A definitive diagnosis of PCD is confirmed by either:
- An abnormal HSVA with a known pathogenic mutation, or
- An abnormal HSVA with diagnostic TEM findings, or
- In cases of normal TEM, an abnormal HSVA with biallelic pathogenic mutations in a PCD gene [4].
Protocol 2: Functional Validation of VUS using Immunofluorescence (IF)
Objective: To determine the impact of a genetic VUS on ciliary protein localization.
Materials: Cultured ciliated epithelial cells from the patient, primary antibodies against the protein of interest and a ciliary marker (e.g., acetylated α-tubulin), fluorescently-labeled secondary antibodies, confocal microscope. Methodology:
- Cell Culture and Ciliogenesis: Differentiate airway epithelial cells at an air-liquid interface (ALI) to produce a ciliated culture.
- Cell Fixation and Staining: Fix cells and permeabilize using standard IF protocols.
- Antibody Incubation: Incubate with primary antibodies, followed by appropriate secondary antibodies.
- Confocal Microscopy: Image the cilia using a confocal microscope.
- Analysis: Compare the localization and intensity of the protein of interest in patient cells versus healthy control cells. Absence or mislocalization of the protein supports the pathogenicity of the VUS.
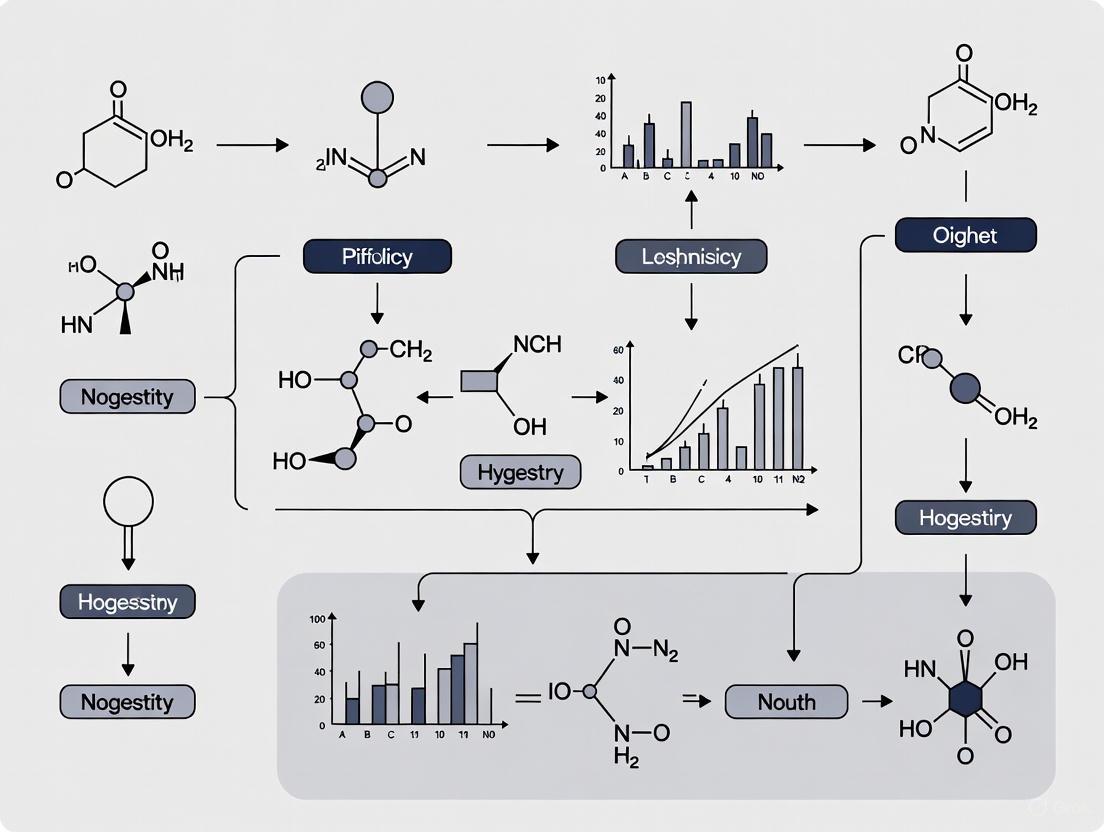
Signaling Pathways and Diagnostic Workflow
Ciliary Function and PCD Diagnostic Pathway
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function / Application in PCD Research |
|---|---|
| Air-Liquid Interface (ALI) Culture System | Differentiates primary human airway epithelial cells to generate a ciliated cell culture model for in vitro functional studies (HSVA, IF, TEM). |
| High-Speed Video Microscope | Essential equipment for capturing ciliary beat frequency and pattern at high frame rates (>500 fps) for HSVA, a critical diagnostic tool. |
| Transmission Electron Microscope | Used to visualize the internal ultrastructure of cilia, including the 9+2 microtubule arrangement and outer/inner dynein arms. |
| Next-Generation Sequencing (NGS) Gene Panel | A targeted panel of known PCD-associated genes used to identify pathogenic mutations, especially in cases with normal TEM. |
| Anti-Acetylated α-Tubulin Antibody | A standard immunofluorescence marker that stains the ciliary axoneme, used to visualize the location and structure of cilia. |
| Anti-DNAH11 / GAS8 / etc. Antibodies | Gene-specific antibodies used in immunofluorescence to determine if a genetic mutation causes mislocalization or absence of the corresponding protein. |
| Nasal Nitric Oxide (nNO) Analyzer | A device that measures the concentration of nitric oxide in nasal air, which is typically low in most forms of PCD. |
Frequently Asked Questions
Q1: If the daily wet cough criterion has such notable limitations, why is it so commonly used in initial screenings? The daily wet cough criterion serves as a highly specific, though poorly sensitive, initial filter. It is easily ascertainable in clinical and research settings and effectively identifies a classic PCD phenotype. However, over-reliance on this single symptom misses a significant subset of patients, as chronic wet cough is not universally present. Many individuals, particularly older children and adults, may present with a dry or intermittent cough despite having a confirmed PCD diagnosis [4].
Q2: In a research context, what specific patient populations are most at risk of being missed by this criterion? Research cohorts focusing solely on daily wet cough are likely to be biased and miss key demographic and genotypic subgroups, including:
- Patients with specific genetic variants: Individuals with mutations in genes like DNAH9 or RSPH1 often have milder respiratory symptoms and may not exhibit a daily wet cough [4].
- Older patients and adults: As individuals age, the clinical presentation can evolve, and the classic daily wet cough may become less prominent.
- Patients with effective airway clearance regimens: Subjects enrolled in rigorous physiotherapy or airway clearance studies may not report a daily wet cough, despite having the underlying ciliary defect.
Q3: What is the most robust alternative or complementary screening method for identifying research subjects? The PICADAR (PrImary CiliAry DyskinesiA Rule) tool is a validated predictive score that outperforms simple symptom checklists. It incorporates seven key clinical features to calculate a risk score, demonstrating high sensitivity (0.97) for identifying patients who require further diagnostic testing. Using a cutoff score of 4, PICADAR correctly identifies 97% of true PCD cases while maintaining reasonable specificity (0.48), ensuring research resources are allocated efficiently [4].
Q4: How do major society guidelines, like those from the ERS and ATS, differ in their approach to initial patient selection? The European Respiratory Society (ERS) and American Thoracic Society (ATS) guidelines offer different approaches, highlighting the lack of a single, perfect standard.
| Guideline Body | Recommended Screening Approach | Reported Sensitivity | Reported Specificity |
|---|---|---|---|
| European Respiratory Society (ERS) [4] | Flexible: "patients with several typical features" or use of the PICADAR tool. | 0.97 (for PICADAR) | 0.48 (for PICADAR) |
| American Thoracic Society (ATS) [4] | A four-point clinical symptoms score (possessing 2 of 4 features). | 0.80 | 0.72 |
The ATS approach, while specific, may miss up to 20% of PCD patients at the screening stage. The ERS's flexible approach and use of PICADAR aim for higher sensitivity to minimize false negatives [4].
Q5: For a research study aiming to enroll all comers with suspected PCD, what is the recommended diagnostic workflow to overcome the limitations of initial criteria? A tiered, multi-modal diagnostic protocol is essential. No single test is sufficient due to the genetic and phenotypic heterogeneity of PCD. The following workflow, which integrates initial screening with advanced confirmation, is recommended to minimize both false positives and false negatives.
The Scientist's Toolkit: Key Diagnostic & Research Reagents
The following table details essential materials and assays used in advanced PCD research and diagnostics.
| Research Reagent / Tool | Primary Function in PCD Investigation |
|---|---|
| High-Speed Video Microscopy (HSVA) | Visualizes and quantifies ciliary beat frequency and pattern in real-time. Critical for detecting functional defects in patients with normal ultrastructure (e.g., DNAH11 mutations) [4]. |
| Transmission Electron Microscopy (TEM) | Provides ultrastructural analysis of ciliary axonemes. Identifies hallmark defects (e.g., absent dynein arms) based on the BEAT-PCD TEM criteria (Class I/II alterations) [10]. |
| Next-Generation Sequencing (NGS) Panels | Genetic screening for pathogenic variants in over 50 known PCD-related genes. Essential for confirming diagnosis and correlating genotype with phenotypic data [4] [10]. |
| Nasal Nitric Oxide (nNO) | Measures nasal NO levels, which are characteristically very low in most PCD patients. Used as a rapid, non-invasive screening test, though it can yield false negatives [4]. |
| Immunofluorescence (IF) Labeling | Uses fluorescent antibodies to visualize and localize specific ciliary proteins. Helps confirm the pathogenic effect of genetic variants of uncertain significance (VUS) by showing mislocalization of proteins [4]. |
Experimental Protocols for Key Assays
Protocol 1: High-Speed Video Microscopy (HSVA) Analysis
- Sample Collection: Nasal epithelial tissue is collected via cytological brushing of the inferior turbinate.
- Sample Preparation: The sample is immediately placed in culture medium and analyzed within 24 hours to maintain ciliary vitality.
- Data Acquisition: Ciliary motion is recorded using a high-speed camera (≥500 frames per second) mounted on a phase-contrast microscope.
- Analysis: Recordings are analyzed manually and/or with specialized software for ciliary beat frequency and, critically, beat pattern. Dyskinetic, stiff, or circular patterns are indicative of PCD [4].
Protocol 2: Transmission Electron Microscopy (TEM) for BEAT-PCD Criteria
- Fixation: The ciliated biopsy is fixed in 3% glutaraldehyde for a minimum of 3 hours at 4°C.
- Processing: The sample is washed in a phosphate buffer, post-fixed in osmium tetroxide, dehydrated, and embedded in resin.
- Sectioning & Staining: Ultrathin sections (60-90 nm) are cut and stained with heavy metals (e.g., uranyl acetate and lead citrate).
- Imaging & Classification: A minimum of 100 ciliary cross-sections are imaged and classified according to the international BEAT-PCD TEM criteria [10]:
- Class I (Hallmark Defects): >50% of axonemes with Outer Dynein Arm (ODA) defects ± Inner Dynein Arm (IDA) defects.
- Class II (Supportive Defects): Includes central complex defects, microtubular disorganization with IDA present, or ODA defects in 25-50% of cross-sections. These require additional supportive evidence for a definitive diagnosis.
Quantitative Data on Diagnostic Tool Performance
The limitations of single-criterion screening and the relative performance of various diagnostic tools are summarized in the table below.
| Diagnostic Tool / Criterion | Utility & Strengths | Limitations & False Negative Rates |
|---|---|---|
| Daily Wet Cough Criterion | High specificity; easy to administer. | Low sensitivity; misses atypical and milder phenotypes. |
| PICADAR (Score ≥4) | High sensitivity (0.97); validated clinical score. | Moderate specificity (0.48); may refer some non-PCD patients [4]. |
| Nasal Nitric Oxide (nNO) | Excellent screening tool; high specificity in classic PCD. | False negatives occur in genes like RSPH1 and DNAH9 [4]. |
| High-Speed Video Analysis (HSVA) | Detects functional defects; identifies TEM/genetic false negatives. | Requires significant expertise; result can be subjective [4]. |
| Transmission Electron Microscopy (TEM) | Gold standard for ultrastructural defects; high specificity. | ~20-30% false negative rate; normal ultrastructure in some genetic forms [4]. |
| Genetic Testing | Provides definitive diagnosis; identifies all biallelic pathogenic variants. | Inconclusive with Variants of Unknown Significance (VUS); ~10% of genes unknown [10]. |
Genetic and Ultrastructural Diversity Underlying Diagnostic Escapes
Frequently Asked Questions (FAQs): Troubleshooting Diagnostic Challenges
1. Our clinical screening using the PICADAR tool failed to identify a patient who was later genetically confirmed to have PCD. What are the known limitations of this predictive rule?
The PICADAR tool has demonstrated significant limitations in sensitivity, particularly in specific patient subgroups. Recent validation studies found its overall sensitivity to be approximately 75% in a genetically confirmed PCD cohort. Performance varies substantially based on patient characteristics [11]:
- Situs solitus (normal organ arrangement): Sensitivity drops to 61%
- Absence of hallmark ciliary ultrastructural defects: Sensitivity drops to 59%
- Lack of daily wet cough: The tool's initial question excludes these patients from further scoring, yet 7% of genetically confirmed PCD patients do not report this symptom [11].
Recommended Action: Do not rely on PICADAR as the sole factor for initiating a PCD diagnostic work-up. For patients with a strong clinical history but low PICADAR scores, proceed to specialist testing [4] [11].
2. What is the recommended diagnostic pathway when genetic and ultrastructural results are discordant (e.g., pathogenic mutations found but TEM appears normal)?
Discordance between genetic and ultrastructural findings is a common diagnostic escape scenario, occurring in 20–30% of true PCD cases [4]. This is frequently associated with mutations in genes such as DNAH11 and HYDIN.
Recommended Action: Follow a multi-method diagnostic approach as per European Respiratory Society (ERS) guidelines. If genetic testing identifies biallelic pathogenic mutations in a PCD-associated gene, the diagnosis is confirmed even with normal TEM. Furthermore, an abnormal high-speed video analysis (HSVA) showing a dyskinetic ciliary beat pattern can indicate that PCD is "highly likely," and a PCD treatment plan should be initiated while awaiting confirmatory tests [4].
3. How can we mitigate the risk of false-positive genetic results in PCD diagnosis?
A significant pitfall in genetic testing is the misinterpretation of variants of unknown significance (VUS). It is not uncommon for individuals without PCD to have biallelic VUS in PCD-related genes, which severely reduces the specificity of genetic testing [4].
Recommended Action: Always ensure the genetic findings are compatible with the clinical and ciliary phenotype. Correlate the genotype with results from HSVA, TEM, and/or immunofluorescence labeling. A genotype is only considered confirmatory if the mutations are known to be pathogenic and match the observed phenotype [4].
Troubleshooting Guides for Key Experimental Challenges
Guide 1: Overcoming Limitations of Clinical Prediction Tools
Problem: A clinical prediction score (e.g., the 4-point ATS score or PICADAR) is being used for referral, leading to missed diagnoses.
Solution: Implement a multi-parameter and sensitive screening strategy.
Step 1: Broaden Clinical Suspicion Move beyond a rigid scoring system. Consider a flexible approach for any patient presenting with "several typical features" of PCD, such as neonatal respiratory distress at term, daily wet cough, persistent rhinitis, and unexplained bronchiectasis [4] [12].
Step 2: Utilize Nasal Nitric Oxide (nNO) as a Triage Tool Use nNO measurement as a sensitive, though not specific, screening test. A diagnostically low nNO value warrants further investigation, even if other screens are normal [4].
Step 3: Integrate High-Speed Video Analysis (HSVA) HSVA can detect ciliary beat pattern abnormalities in patients with normal nNO and TEM. The ERS guideline suggests that both nNO and HSVA should be entirely normal before ruling out the need for further PCD testing [4].
Table: Comparison of PCD Diagnostic Predictive Tools
| Tool Name | Sensitivity | Specificity | Key Limitations |
|---|---|---|---|
| PICADAR | 75% (Overall); 61% (Situs Solitus) [11] | 75% [12] | Low sensitivity in patients without laterality defects or hallmark ultrastructural defects; excludes patients without daily wet cough [11]. |
| ATS 4-Feature Score | 80% [4] | 72% [4] | May miss 20% of PCD patients; designed to select only the most likely cases for diagnostic services [4]. |
Guide 2: Validating Pathogenicity of Genetic Variants
Problem: Genetic testing has identified biallelic variants of unknown significance (VUS), and their clinical relevance is uncertain.
Solution: A functional and correlative validation workflow is essential.
Step 1: Phenotypic Correlation with HSVA If possible, obtain a ciliary biopsy and perform HSVA. A clearly abnormal, dyskinetic ciliary beat pattern supports the pathogenicity of the VUS [4] [13].
Step 2: Ultrastructural Correlation with TEM Analyze the ciliary ultrastructure. Certain genetic mutations are linked to specific TEM defects (e.g., outer dynein arm缺失), while others (e.g., DNAH11) yield normal TEM. The observed structure should be consistent with the known genotype-phenotype association [4].
Step 3: Employ Immunofluorescence (IF) Labeling Use antibodies against proteins encoded by the gene harboring the VUS. A marked reduction or absence of protein localization in the ciliary axoneme provides strong functional evidence for variant pathogenicity [4].
Step 4: Check for Compensatory Mutations Be aware that in some cases, a second-site mutation (compensatory evolution) can restore fitness without reversing the resistance phenotype, complicating genotype-phenotype maps [13].
Guide 3: Implementing a Multi-Modal Diagnostic Workflow to Capture All Cases
Problem: Reliance on a single "gold standard" test is resulting in diagnostic escapes.
Solution: Adopt a holistic diagnostic algorithm that leverages the complementary strengths of multiple techniques to account for genetic and ultrastructural diversity. The following workflow integrates the key methods for a comprehensive assessment.
Integrated Diagnostic Workflow for PCD
The Scientist's Toolkit: Key Research Reagents & Materials
Table: Essential Reagents for Investigating Diagnostic Escapes in PCD
| Reagent / Material | Primary Function | Application in Troubleshooting |
|---|---|---|
| High-Speed Video Microscope (HSVM) | To visualize and quantify ciliary beat frequency and pattern in real-time. | Detecting ciliary dyskinesia in patients with normal nNO and TEM (e.g., DNAH11 mutations) [4]. |
| Nasal Nitric Oxide (nNO) Analyzer | To measure the level of nasal NO, which is characteristically low in most PCD patients. | Initial, non-invasive screening and triage of patients for further testing [4] [12]. |
| Transmission Electron Microscope (TEM) | To visualize the internal ultrastructure of cilia (e.g., dynein arms, microtubules). | Identifying hallmark structural defects (e.g., ODA/IDA缺失) and correlating with genetic findings [4] [14]. |
| PCD Gene Panel (NGS-based) | To sequence known and candidate PCD genes for pathogenic mutations. | Genetic confirmation of disease, especially in cases with ambiguous or discordant functional results [4] [13]. |
| Ciliary Protein Antibodies | For immunofluorescence (IF) microscopy to localize specific proteins within the ciliary axoneme. | Validating the functional impact of VUS by showing loss of protein localization [4]. |
| Air-Liquid Interface (ALI) Cell Culture System | To differentiate and culture human bronchial epithelial cells, regenerating ciliated epithelium. | Re-differentiating ciliated cells from biopsy samples for repeat HSVA or TEM, eliminating secondary dyskinesia [4] [12]. |
Enhanced Diagnostic Frameworks: Integrating Tools Beyond Clinical Scores
Diagnostic Algorithms & Quantitative Performance Gaps
Diagnostic Criteria and Workflow Comparison
| Feature | ERS Guideline (2017) | ATS Guideline (2018) | Performance Gap |
|---|---|---|---|
| Core Approach | Categorizes results into four diagnostic groups [15] | Binary diagnostic outcome [15] | ERS allows for diagnostic uncertainty; ATS provides definitive classification [15] |
| Final Diagnostic Categories | 1. PCD positive2. PCD highly likely3. PCD highly unlikely4. Inconclusive [15] | 1. PCD diagnosed2. PCD not diagnosed [15] | 15% of patients receive conflicting diagnoses between guidelines [15] |
| nNO Measurement | Recommended for patients >6 years (velum closure); suggested for children <6 years (tidal breathing) [16] | Used as a primary initial test [15] | Techniques and interpretation may vary, contributing to diagnostic discordance |
| Genetic Analysis | Considered a confirmatory test (PCD positive if biallelic pathogenic variants) [15] | Part of the primary diagnostic panel (>12 genes) [15] | Differences in gene panels and variant interpretation can affect outcomes |
| TEM Role | Confirmatory for hallmark defects; further testing recommended if normal ultrastructure but strong clinical history [16] | Used in the diagnostic pathway [15] | Specimen quality and expertise can impact results inconsistently |
| HSVM Role | Recommended for ciliary beat pattern analysis, preferably after cell culture [16] | Not explicitly defined in the studied algorithm [15] | ERS utilizes dynamic ciliary function assessment more centrally |
| Immunofluorescence | Not included in the original 2017 algorithm [15] | Not included in the 2018 algorithm [15] | Added in modified algorithms (e.g., PCD-UNIBE) to improve accuracy [15] |
Quantitative Concordance Data
A 2021 clinical study directly compared the ERS and ATS algorithms, revealing significant diagnostic discrepancies [15].
Table 1.2: Diagnostic Algorithm Concordance in a Clinical Cohort (n=54) [15]
| Diagnostic Outcome | Number of Patients | Percentage of Cohort |
|---|---|---|
| All Algorithms Concordant (PCD Positive or Negative) | 46 | 85% |
| PCD Diagnosed by ATS only | 5 | 9% |
| PCD Diagnosed by ERS only | 1 | 2% |
| PCD Diagnosed by ERS and PCD-UNIBE only | 1 | 2% |
| PCD Diagnosed by PCD-UNIBE only | 1 | 2% |
Statistical agreement was substantial between ERS and ATS (κ=0.72, 95% CI 0.53–0.92) and between ATS and PCD-UNIBE (κ=0.73, 95% CI 0.53–0.92), and almost perfect between ERS and PCD-UNIBE (κ=0.92, 95% CI 0.80–1.00) [15].
FAQs: Addressing Key Experimental Challenges
My study population includes patients with strong clinical symptoms but normal PICADAR scores. How should I proceed?
Proceed with full diagnostic testing. The PICADAR tool has limited sensitivity, particularly in specific subpopulations. A 2025 study found that 7% of genetically confirmed PCD patients did not report a daily wet cough, which alone rules out PCD according to PICADAR [1]. The overall sensitivity of PICADAR was 75%, but it dropped to 61% in patients with situs solitus (normal organ placement) and to 59% in those without hallmark ultrastructural defects on TEM [1]. Relying solely on PICADAR will miss these cases.
What is the most critical step to reduce inter-laboratory variability in PCD diagnostic results?
Standardized cell culture and expert central review. The ERS guideline strongly recommends repeating High-Speed Video Microscopy Analysis (HSVA) after air-liquid interface (ALI) culture to differentiate primary ciliary dyskinesia from secondary, acquired defects [16]. Furthermore, techniques like immunofluorescence staining and transmission electron microscopy should only be performed in experienced, specialist centres due to significant batch-to-batch variability and the profound impact of expertise on interpretation [17].
How do I resolve a conflicting diagnosis where ERS criteria classify a case as "PCD highly likely" but ATS criteria result in "PCD not diagnosed"?
This occurs in about 9% of cases [15]. Follow these steps:
- Re-review all primary data, focusing on the quality and concordance of each test.
- Incorporate immunofluorescence (IF) staining. IF can detect the absence of specific ciliary proteins, providing functional evidence for a genetic finding or clarifying a case with normal ultrastructure [17]. This was a key differentiator in the PCD-UNIBE algorithm [15].
- Consider expanded genetic testing. Next-generation sequencing panels may identify variants in genes not covered in initial tests, especially for patients with normal ultrastructure [16].
- Refer to a specialized multidisciplinary board for a final consensus diagnosis [15].
Are there any newly proposed international standards to overcome these inconsistencies?
Yes. In September 2025, the ERS and ATS published new joint international guidelines to create a unified diagnostic approach. These new guidelines strongly recommend a combination of tests—including nasal nitric oxide, genetic testing, TEM, HSVM, and immunofluorescence—emphasizing that no single test is sufficient to confirm or exclude PCD [17]. This unified guideline aims to resolve the discrepancies of the past.
Experimental Protocols for Diagnostic Testing
Protocol: High-Speed Videomicroscopy (HSVM) with ALI Culture
Objective: To assess ciliary beat frequency and pattern, distinguishing primary from secondary dyskinesia.
Methodology Details:
- Nasal Brushing: Obtain nasal epithelial cells using minimally invasive interdental brushes [15].
- Initial HSVM: Record ciliary motion from fresh cells immediately after brushing. Use an inverted microscope with a high-speed camera (e.g., 300 fps). Analyze ciliary beat pattern (CBP), frequency, amplitude, and coordination [15].
- ALI Culture: Culture the harvested cells at an air-liquid interface to promote ciliary differentiation and eliminate secondary inflammatory effects [15].
- Post-Culture HSVM: Repeat the HSVM analysis on the cultured cells. The persistence of an abnormal CBP after culture is indicative of PCD [16] [15].
Troubleshooting Tip: If ciliary beating is immotile or dyskinetic in fresh cells but normalizes after culture, this suggests a secondary, reversible cause rather than PCD.
Protocol: Diagnostic Immunofluorescence (IF) Staining
Objective: To detect the absence or mislocalization of ciliary proteins, confirming defects suggested by genetics or HSVM.
Methodology Details:
- Sample Preparation: Use ciliated epithelial cells, preferably from ALI culture, fixed on slides [15].
- Antibody Staining: Apply a panel of antibodies targeting key ciliary proteins. A standard panel should include DNAH5, GAS8, and RSPH9. Expand the panel based on HSVM findings or genetic results (e.g., stain for DNAH11 in cases of stiff, low-amplitude beating) [15].
- Imaging and Analysis: Use fluorescence microscopy to visualize antibody binding. Compare against healthy control samples. The absence of specific protein signals is a strong indicator of PCD [17].
Troubleshooting Tip: Include a positive control (e.g., antibody against acetylated tubulin) to confirm the presence of cilia in the sample. Batch-to-batch variability of antibodies is a known issue, so validate new batches with known positive and negative controls [17].
Diagnostic Pathway Visualization
PCD Diagnostic Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 5.1: Essential Materials for PCD Diagnostic Research
| Item | Function / Application | Key Considerations |
|---|---|---|
| Chemiluminescence nNO Analyzer | Measures nasal nitric oxide flow; a key screening tool. | Use velum closure technique for patients >6 years; tidal breathing for younger children [16] [17]. |
| High-Speed CMOS Camera (>200 fps) | Records ciliary motion for HSVM analysis. | Essential for detailed assessment of ciliary beat pattern, not just frequency [16] [15]. |
| Air-Liquid Interface (ALI) Culture System | Differentiates primary from secondary ciliary dyskinesia. | Culturing cells is superior to analysis of fresh cells alone [16] [15]. |
| Antibody Panel for IF | Detects absence/mislocalization of ciliary proteins. | Standard panel: DNAH5, GAS8, RSPH9. Expand based on phenotype (e.g., DNAH11, RSPH1) [15]. Validate batches [17]. |
| Transmission Electron Microscope | Visualizes ultrastructural defects in ciliary axoneme. | Follows BEAT-PCD TEM criteria for standardized reporting [15]. |
| Next-Generation Sequencing Panel | Identifies pathogenic variants in >50 known PCD genes. | Crucial for confirming diagnosis, especially in cases with normal TEM [16] [17]. |
The Role of High-Speed Video Microscopy in Detecting Atypical Cases
FAQs: High-Speed Video Microscopy in PCD Diagnostics
Q1: How does High-Speed Video Microscopy Analysis (HSVA) address the limitations of PICADAR and other clinical prediction scores in research?
Clinical prediction scores like PICADAR are used to identify patients who should undergo definitive testing for Primary Ciliary Dyskinesia (PCD). While PICADAR has a high sensitivity (approximately 0.97), its specificity is lower (approximately 0.48), meaning it correctly identifies most true cases but also flags many individuals who do not have PCD [4]. In a research context focused on overcoming false negatives, HSVA is crucial because it can detect PCD cases with normal ultrastructure (false negatives from Transmission Electron Microscopy) and atypical beat patterns that may be missed by screening algorithms alone [4] [18]. It serves as a functional first-line test to capture these atypical cases.
Q2: What are the key PCD genotypes that HSVA can detect which might be missed by transmission electron microscopy (TEM)?
A significant number of PCD cases (approximately 20-30%) have normal ciliary ultrastructure when examined by TEM [4] [19]. HSVA is particularly valuable for identifying these atypical cases. Key genotypes include:
- DNAH11: Patients typically have a hyperkinetic and irregular ciliary beat pattern [20] [18].
- HYDIN, CCDC164, DNAH9, and GAS8: These genotypes can also present with PCD despite normal TEM findings, and their ciliary function is best assessed via HSVA [21] [18].
- RSPH1 and RSPH4A: These mutations can lead to unexpected beat patterns that may be non-diagnostic without functional analysis [21].
Q3: What are the primary causes of false-positive and false-negative results in HSVA, and how can they be mitigated in a research protocol?
False positives often result from secondary dyskinesias caused by factors like infection, smoking, or sample processing damage, which can alter the ciliary beat pattern [18]. False negatives can occur because defects in at least six known PCD-associated genes (e.g., HYDIN, CCDC164) can result in normal or non-diagnostic HSVA results [21]. Mitigation strategies:
- Cell Culture: The European Respiratory Society (ERS) guidelines strongly recommend regrowing ciliary samples at the air-liquid interface to eliminate secondary dyskinesias, though this is a weeks-long process [21].
- Repeat Testing: Diagnosis should be confirmed by repeating HSVA at least twice at different times and showing identical aberrations [18].
- Multi-Modal Diagnosis: HSVA should not be used alone. Findings should be corroborated with other methods like genetic testing, immunofluorescence microscopy (IFM), or nasal nitric oxide (nNO) measurement [4] [21] [18].
Troubleshooting Guides for HSVA Experiments
Guide 1: Addressing Non-Diagnostic or Inconclusive Video Footage
Problem: Recorded video clips show insufficient ciliary movement, excessive mucus, or contamination with blood cells. Solutions:
- Cause A: Poor Sample Quality. Ensure the patient has been on a two-week course of oral amoxicillin-clavulanic acid (terminated 2 days before the procedure) to eradicate biofilms that interfere with cilia function [20].
- Cause B: Epithelial Injury. Nasal brushing should be quick (approximately 2 seconds) to avoid severe epithelial injury and consequent epistaxis, which leads to contamination with red blood cells [20].
- Cause C: Mucus Overlay. Ask the patient to blow their nose thoroughly before brushing to diminish the overlay of mucous material on the epithelial cell strips [20].
Guide 2: Managing Discrepancies Between HSVA and Genetic Results
Problem: A research subject has a strong clinical phenotype and low nNO, but HSVA results are normal, and genetic testing reveals variants of unknown significance (VUS). Solutions:
- Action 1: Correlate Genotype with Phenotype. It is essential to ensure that the genotype is compatible with the ciliary phenotype using HSVA, TEM, and/or immunofluorescence labeling [4]. Not all biallelic VUS are pathogenic.
- Action 2: Utilize IFM. Immunofluorescence microscopy can reveal proteins that are absent from the cilia's axial filament, providing functional evidence to support or refute the genetic findings [19].
- Action 3: Consider Extended Analysis. Remember that normal HSVA does not exclude PCD. Proceed to further testing, including TEM and extended genetic panels, as the specificity of genetic testing is reduced when variants are of unknown significance [4] [21].
Quantitative Data on PCD Diagnostic Modalities
Table 1: Performance Characteristics of Key PCD Diagnostic Tools
| Diagnostic Method | Reported Sensitivity | Reported Specificity | Key Limitations |
|---|---|---|---|
| High-Speed Video Analysis (HSVA) | 100% (in expert hands) [20] | 96% (in expert hands) [20] | Non-standardized; requires expertise; false negatives possible for specific genotypes [21] |
| Transmission Electron Microscopy (TEM) | ~70% [19] [18] | High (when abnormal) | Misses ~30% of PCD cases with normal ultrastructure [20] [19] |
| Genetic Testing | ~70-80% [19] | High (for known pathogenic variants) | Up to 30% of cases have negative or ambiguous results; variants of unknown significance are common [4] [19] |
| Clinical Score (PICADAR) | 0.97 [4] | 0.48 [4] | A screening tool, not a diagnostic; needs validation in primary care [4] |
Experimental Protocol: HSVA for Atypical PCD Case Identification
This protocol is designed for research settings focused on validating PCD diagnoses where first-line tests are inconclusive.
Step 1: Patient Identification and Sample Collection
- Identify Subjects: Use a flexible clinical approach or the PICADAR tool (cutoff ≥4 points) to select patients with a high pre-test probability of PCD for research inclusion [4].
- Brush Biopsy: Using a 0.6 mm interdental brush, brush the inferior turbinate of both nostrils for approximately 2 seconds to collect epithelial cell strips [20].
- Sample Preservation: Immediately place the harvested cell strips into a 1.5 mL microcentrifuge tube containing Dulbecco’s Modified Eagle Medium (DMEM) [20].
Step 2: Sample Transport and Preparation
- Transport: Fix the tube in a polystyrene box with a cold pack (4-8°C). Do not freeze the specimen. Analysis must be performed within 24 hours [20].
- Preparation for Imaging: Warm the sample to 37°C to mimic in vivo conditions. Pipette two drops into a glass-bottom dish or cuvette for microscopy [20].
Step 3: High-Speed Video Recording
- Microscopy Setup: Use a differential-interference microscope with an oil immersion lens (100x magnification) and a high-speed video camera capable of recording at least 200 frames per second [20].
- Recording: Search for cell clusters with low mucus and no red blood cells. Record video sequences of cilia from the side and top views. Record multiple representative regions of interest [20].
Step 4: Video Analysis for Ciliary Beat Frequency (CBF) and Pattern (CBP)
- CBF Analysis: Play videos back frame-by-frame. Count 10 consecutive beats and record the number of frames elapsed. Calculate CBF using the formula: CBF (Hz) = (10 * Frame Rate) / X, where X is the number of frames for 10 beats [20]. Compare to age-specific reference values.
- CBP Analysis: Two independent, experienced operators should qualitatively assess the waveform for abnormalities such as dyskinesia, circular movement, or reduced amplitude [20] [18]. The diagnosis of PCD is "highly likely" with a repeatedly dyskinetic beat pattern, even if genetics and TEM are normal [4].
The following workflow diagram summarizes the key experimental and decision-making steps for using HSVA in a research setting focused on atypical PCD cases.
Research Reagent Solutions for HSVA
Table 2: Essential Materials for HSVA Experiments
| Item | Function / Application in Protocol |
|---|---|
| Interdental Brush (0.6 mm) | Harvesting respiratory epithelial cells from the inferior turbinate via brushing [20]. |
| Dulbecco's Modified Eagle Medium (DMEM) | Cell-nourishing medium for sample preservation during storage and transport; maintains cell viability [20]. |
| Glass-Bottom Dish or Cuvette | Holds the sample during microscopy, providing an optimal surface for high-resolution imaging [20]. |
| Differential-Interference Microscope | Provides high-contrast images of unstained, living ciliated cells by enhancing interference patterns [20]. |
| High-Speed Video Camera (≥200 fps) | Captures the rapid motion of cilia, allowing for detailed frame-by-frame analysis of beat pattern and frequency [20]. |
| Antibiotics (e.g., Amoxicillin-clavulanic acid) | Administered prior to brushing to eradicate biofilms that can interfere with and obscure true cilia function [20]. |
Genetic Panel Testing and Whole Genome Sequencing as First-Line Tools
Diagnostic Performance & Quantitative Data
The table below summarizes the performance metrics of traditional predictive tools versus modern genetic sequencing techniques in diagnosing Primary Ciliary Dyskinesia (PCD).
Table 1: Performance Comparison of PCD Diagnostic Tools
| Diagnostic Tool | Reported Sensitivity | Reported Specificity | Key Limitations / Advantages |
|---|---|---|---|
| PICADAR (Clinical Score) | 75% (Overall); 61% (Situs Solitus); 59% (Normal Ultrastructure) [11] | 75% (for cutoff score of 5) [12] | Low sensitivity in patients without laterality defects or hallmark TEM findings [11]. |
| Nasal Nitric Oxide (nNO) | Varies; less specific in young children (AUC 0.75) [22] | Varies; improves with genetic testing (AUC 0.97) [22] | Requires patient cooperation; results are non-specific and must be combined with other tests [4] [22]. |
| Transmission Electron Microscopy (TEM) | ~70-80% (20-30% false-negative rate) [4] [23] | High for hallmark defects | Normal ultrastructure does not rule out PCD; identifies ~70% of cases [4] [5] [23]. |
| Whole-Exome Sequencing (WES) | 94% diagnostic yield in highly suspicious cohort [22] | High when biallelic pathogenic variants are identified | Can establish alternative diagnoses; accuracy improves with trio-based testing [22] [24]. |
Troubleshooting Guides & FAQs
FAQ 1: Our research cohort is screened with PICADAR, but we suspect we are missing genetically confirmed PCD cases. What is the primary pitfall?
Challenge: The PICADAR tool has a critical design limitation for research populations. Its initial question regarding "daily wet cough" automatically rules out PCD in individuals without this symptom. A recent study found that 7% of genetically confirmed PCD patients did not report a daily wet cough and would have been excluded from further testing by PICADAR alone [11]. Furthermore, its sensitivity plummets to ~60% in patients with normal organ arrangement (situs solitus) or those without hallmark ultrastructural defects on TEM [11].
Solution: Do not use PICADAR as a standalone enrollment criterion for research. It should be supplemented with other clinical features like unexplained neonatal respiratory distress in term infants, persistent rhinitis, or a history of recurrent otitis media. For definitive cohort building, proceed directly to genetic testing in cases with strong clinical suspicion, even if the PICADAR score is low [4] [11].
FAQ 2: When designing a genetic study for PCD, what are the key practical considerations for choosing between Whole Genome Sequencing (WGS) and Whole Exome Sequencing (WES)?
Challenge: Choosing the most efficient and cost-effective genetic testing strategy.
Solution: The choice depends on the research objectives, budget, and existing genetic knowledge of the cohort.
Table 2: WES vs. WGS at a Glance
| Feature | Whole Exome Sequencing (WES) | Whole Genome Sequencing (WGS) |
|---|---|---|
| Target Region | Protein-coding exons (~1-2% of genome) [24] | Entire genome, including non-coding regions [24] |
| Data Volume | ~10 GB per sample [24] | ~120 GB per sample (12x larger) [24] |
| Variant Load | ~50,000 variants per sample [24] | ~3 million variants per sample (60x more) [24] |
| Best For | Identifying pathogenic variants in known coding regions [22] | Discovering novel non-coding variants, structural variants (SVs), and copy number variants (CNVs) [24] |
| Cost & Analysis | Lower cost; faster analysis (e.g., ~2 hours) [24] | Higher cost (2-5x WES); computationally intensive (e.g., ~24 hours analysis) [24] |
| Key Limitation | May miss non-coding and structural variants [24] | Many variants in non-coding regions are of unknown significance; interpretation is challenging [24] |
For most diagnostic-oriented research, WES is an excellent first-line tool due to its high diagnostic yield (94%) and lower cost [22]. WGS is recommended when research aims to discover novel non-coding variants or structural defects, or when a patient has a strong clinical phenotype but previous genetic tests are negative [24].
FAQ 3: A significant number of genetic variants from our NGS data are classified as "Variants of Uncertain Significance" (VUS). How can we mitigate this in our analysis?
Challenge: Interpreting VUS, especially in non-coding regions identified by WGS, is a major hurdle [24].
Solution:
- Utilize Trio-Based Sequencing: Sequencing the proband and both parents allows for precise determination of de novo mutations and inheritance patterns, dramatically improving the identification of pathogenic variants [24].
- Implement Ensemble Genotyping: Using multiple variant-calling algorithms on the same dataset and integrating the results can reduce false positives by over 98% while retaining >95% of true positives, leading to more reliable variant sets for interpretation [25].
- Correlate with Functional Phenotypes: Whenever possible, correlate genetic findings with ciliary phenotype data from High-Speed Video Microscopy Analysis (HSVA) or TEM. A VUS in a PCD gene combined with an abnormal ciliary beat pattern strongly supports pathogenicity [4].
- Incorporate Transcriptome Analysis (RNA-seq): Using RNA sequencing in parallel can confirm the functional impact of a variant on splicing or gene expression, which was essential for diagnosis in 18% of cases in one study [24].
Experimental Protocols
Protocol 1: Implementing Untargeted Whole-Exome Sequencing for PCD Diagnosis
This protocol is adapted from a prospective clinical study that demonstrated a 94% diagnostic yield [22].
1. Patient Selection & Sample Preparation:
- Cohort: Include patients with a high clinical suspicion of PCD. Key criteria include: term-born with chronic sinopulmonary symptoms since early childhood, plus one or more of: unexplained bronchiectasis, situs inversus/heterotaxy, or history of unexplained neonatal respiratory distress [22].
- Controls: Include family members (trio-based design is ideal) for segregation analysis [24].
- DNA Extraction: Extract genomic DNA from whole blood using standard kits (e.g., FlexiGene DNA Kit) [5].
2. Exome Sequencing & Bioinformatic Analysis:
- Library Preparation: Use an exome enrichment kit (e.g., SureSelect Human All Exon kit) [22].
- Sequencing: Perform sequencing on a platform such as an Illumina HiSeq2500 to generate high-quality 125-bp paired-end reads [22].
- Alignment & Variant Calling: Align reads to the human reference genome (e.g., GRCh37/hg19) using a standard aligner (e.g., BWA). Call variants using a pipeline like GATK. Ensure minimum coverage of 50x across the exome [22].
- Variant Filtering & Prioritization:
- Focus on non-synonymous, splice-site, and loss-of-function (stop-gain, frameshift) variants.
- Filter against population frequency databases (e.g., gnomAD) to remove common polymorphisms.
- Prioritize rare (e.g., MAF <0.1%) biallelic variants in known PCD-related genes. A list of over 50 causative genes is available in current reviews [23].
3. Validation & Interpretation:
- Confirmation: Confirm putative pathogenic variants using an orthogonal method like Sanger sequencing [25].
- Segregation Analysis: Check that biallelic variants are in trans (on different parental alleles).
- Pathogenicity Assessment: Classify variants according to ACMG/AMP guidelines. Correlate the genotype with the clinical phenotype and any available functional ciliary data (e.g., HSVA, TEM) [4] [5].
Protocol 2: A Multipronged Approach to Overcome PICADAR False Negatives
This workflow integrates multiple diagnostic tools to comprehensively identify PCD cases that would be missed by clinical prediction rules alone [4] [22] [11].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for PCD Genetic Research
| Item | Function / Application | Example Product / Note |
|---|---|---|
| DNA Extraction Kit | High-quality genomic DNA extraction from whole blood or cells. | FlexiGene DNA Kit (Qiagen) [5] |
| Exome Enrichment Kit | Captures and enriches exonic regions from genomic DNA for sequencing. | SureSelect Human All Exon Kit (Agilent) [22] |
| Whole Genome Sequencing Service | Provides comprehensive sequencing of the entire genome. | Services from Illumina, Complete Genomics [25] |
| Variant Annotation Database | Annotates identified variants with population frequency and functional impact. | dbSNP, snpEff with Ensembl transcript model [25] |
| PCD Gene Panel | A curated list of genes known to cause PCD for targeted analysis. | Over 50 genes (e.g., DNAH11, DNAH5, CCDC39, CCDC40) [23] |
| Bioinformatics Pipeline | For alignment, variant calling, and filtering of NGS data. | BWA for alignment, GATK for variant calling [22] |
Immunofluorescence and TEM in the Era of Genomic Medicine
In the diagnosis of complex genetic disorders like Primary Ciliary Dyskinesia (PCD), genomic medicine has provided powerful tools such as PICADAR (Primary Ciliary Dyskinesia Aided Diagnosis), a validated clinical tool that uses symptoms and clinical history to calculate a probability for PCD. However, even the most sophisticated genetic screening can yield false negatives due to novel pathogenic variants, genes not included in testing panels, or complex genetic interactions that escape detection.
This technical support center establishes how the integrated application of immunofluorescence (IF) and transmission electron microscopy (TEM) can overcome these diagnostic limitations. When PICADAR suggests a high probability of PCD yet genetic tests are inconclusive, these morphological and ultrastructural techniques provide a critical pathway to a definitive diagnosis. The following guides and protocols are designed to help researchers and clinicians validate findings, troubleshoot diagnostic challenges, and characterize novel disease mechanisms at the subcellular level.
Troubleshooting Guides & FAQs
This section addresses specific experimental challenges encountered when correlating immunofluorescence and TEM data, particularly in the context of PCD diagnosis and research.
Troubleshooting Common Problems
Problem: Inconclusive TEM results despite strong clinical suspicion of PCD.
- Potential Cause: Secondary ciliary dyskinesia due to infection or inflammation, which can cause transient ultrastructural defects that mimic PCD.
- Solution:
- Repeat Biopsy: Collect a new nasal brush or biopsy after the patient has recovered from acute respiratory infection.
- Air-Liquid Interface (ALI) Culture: Culture the ciliated epithelium to allow regeneration of cilia in a controlled, infection-free environment. Repeat TEM on the cultured cells [26] [27].
- Correlative IF: Perform immunofluorescence testing on the same sample. The absence of a specific ciliary protein (e.g., DNAH5) by IF confirms a true primary defect, whereas secondary defects typically show normal protein presence [26].
Problem: Poor or absent immunofluorescence signal in samples with good morphology.
- Potential Cause: Antigen masking or destruction due to over-fixation, especially with high concentrations of glutaraldehyde.
- Solution:
- Optimize Fixation: Use a combination of low concentrations of paraformaldehyde (e.g., 2-4%) and glutaraldehyde (e.g., 0.1-0.5%) to balance morphology and antigen preservation [28].
- Use Tokuyasu Cryosectioning: For TEM correlation, prepare samples using the Tokuyasu method (slight fixation, sucrose infusion, cryosectioning). This method is renowned for superior preservation of antigenicity [29] [28].
- Anticide Selection: Validate antibodies specifically for use on TEM samples or cryosections. Not all antibodies suitable for light microscopy work well for EM-level immunolabeling [28].
Problem: Discrepancy between IF and genetic results.
- Potential Cause: Mislocalization, rather than absence, of a ciliary protein. Some genetic mutations allow protein synthesis but disrupt its transport and incorporation into the ciliary axoneme.
- Solution:
- High-Resolution IF: Use super-resolution or confocal microscopy to precisely localize the protein within the cell. Look for accumulation in the cell body instead of the cilia.
- TEM Correlation: Use TEM to identify the specific ultrastructural defect (e.g., missing dynein arms). Correlate this Class 1 defect with the IF pattern to build a conclusive diagnostic case [27].
Frequently Asked Questions (FAQs)
Q1: What constitutes a definitive PCD diagnosis by TEM, and how does it relate to IF findings?
A: According to the international BEAT PCD TEM consensus guideline, a definitive diagnosis can be made by identifying "Class 1" defects [27]. These hallmark defects are highly specific for PCD and include:
- Outer Dynein Arm (ODA) Defect: Absence from the majority of doublets in >50% of axonemes.
- Combined ODA and Inner Dynein Arm (IDA) Defect: Absence of both structures.
- Microtubular Disorganization with IDA Defect: Disordered microtubule arrangement coupled with missing IDAs.
IF findings directly complement these observations. For example, the absence of DNAH5 (an ODA protein) by IF correlates with ODA defects on TEM, providing molecular validation for the ultrastructural observation [26] [27].
Q2: Our research aims to discover novel PCD genes. How can IF/TEM guide genetic analysis?
A: IF and TEM are powerful for phenotyping patients with inconclusive genetic results. The workflow is as follows:
- Phenotype First: Use TEM to categorize the patient's defect (e.g., ODA defect, IDA defect, central pair apparatus defect).
- Molecular Phenotyping: Use a targeted IF antibody panel (e.g., against DNAH5 for ODAs, DNALI1 for IDAs, RSPH4A for radial spokes) to pinpoint the missing protein complex [26].
- Prioritize Genetic Analysis: This phenotypic data allows you to prioritize sequencing of genes known to be associated with that specific defect, or to focus the search for novel genes within pathways governing that particular ciliary complex.
Q3: What is the recommended sample preparation workflow for combined IF and TEM analysis?
A: The optimal workflow that preserves both antigenicity for IF and ultrastructure for TEM involves the following key steps [29] [28]:
Q4: What are the specific advantages of using the Tokuyasu method for immuno-TEM?
A: The Tokuyasu cryosectioning method offers several distinct advantages for correlative microscopy [29] [28]:
- Superior Antigen Preservation: Because embedding in plastic resin is avoided, more antigenic sites remain accessible to antibodies.
- Versatility: The same cryosection can be used for initial IF screening and subsequent high-resolution TEM imaging, ensuring perfect correlation.
- Robust Multiple Labeling: It facilitates reliable double- or triple-labeling experiments with different-sized gold particles, allowing for the study of multiple proteins simultaneously.
Experimental Protocols & Diagnostic Criteria
Detailed Protocol: Immunofluorescence for PCD Diagnosis
This protocol is adapted from studies validating IF as a diagnostic tool for PCD [26].
1. Sample Preparation:
- Collect ciliated epithelial cells via nasal brushing.
- Cytospin onto glass slides and air dry.
2. Fixation:
- Fix cells in ice-cold methanol for 10 minutes at -20°C.
- Alternatively, use 4% PFA for 10 minutes at room temperature, followed by permeabilization with 0.1% Triton X-100 for 5 minutes.
3. Immunostaining:
- Block with 3% BSA in PBS for 30 minutes.
- Incubate with primary antibody cocktail (e.g., anti-acetylated tubulin and anti-DNAH5) in a humidified chamber for 1 hour at room temperature or overnight at 4°C.
- Wash 3x with PBS.
- Incubate with appropriate fluorescent secondary antibodies (e.g., Alexa Fluor 488, 568) for 45 minutes at room temperature, protected from light.
- Wash 3x with PBS.
- Mount with antifade mounting medium containing DAPI.
4. Imaging and Analysis:
- Image using a fluorescence or confocal microscope with a 63x or 100x oil immersion objective.
- Score a minimum of 10 well-ciliated cells. The protein of interest (e.g., DNAH5) is considered "absent" if there is a consistent lack of colocalization with the ciliary marker (acetylated tubulin) along the axoneme in >70% of evaluated cilia.
Diagnostic Criteria: Interpreting TEM Results
The following table summarizes the key ultrastructural defects as defined by the international BEAT PCD TEM consensus guideline [27].
Table 1: TEM Diagnostic Criteria for Primary Ciliary Dyskinesia (PCD)
| Defect Class | Ultrastructural Finding | Diagnostic Implication | Common Associated Genes |
|---|---|---|---|
| Class 1 (Diagnostic) | Outer Dynein Arm (ODA) defect | Definitive for PCD | DNAH5, DNAI1, CCDC114 |
| ODA + Inner Dynein Arm (IDA) defect | Definitive for PCD | DNAAF1, DNAAF3, CCDC103 | |
| Microtubular disorganization with IDA defect | Definitive for PCD | CCDC39, CCDC40 | |
| Class 2 (Supportive) | Central apparatus defect (e.g., missing central pair) | Highly indicative of PCD, requires supporting evidence | RSPH4A, RSPH9 |
| Isolated IDA defect | Highly indicative of PCD, requires supporting evidence | Genes not well defined | |
| Mislocalization of basal bodies | Highly indicative of PCD, requires supporting evidence | CCNO | |
| Non-Diagnostic | Secondary defects (e.g., compound cilia, disorientation) | Not diagnostic for PCD; caused by infection/inflammation | N/A |
The Scientist's Toolkit: Research Reagent Solutions
Successful integration of IF and TEM relies on a carefully selected toolkit of reagents and materials. The table below details essential items for experiments focused on ciliary structure and function.
Table 2: Essential Research Reagents and Materials for Immunofluorescence and TEM Studies
| Item | Function/Application | Examples & Notes |
|---|---|---|
| Anti-DNAH5 Antibody | IF marker for outer dynein arms; absence indicates ODA defects [26]. | Validated for use on cryosections and nasal brushings. |
| Anti-Acetylated Tubulin Antibody | IF marker for the ciliary axoneme; used as a reference for cilia structure and to normalize other signals [26]. | Stains the stable microtubules of the ciliary shaft. |
| Anti-RSPH4A Antibody | IF marker for the radial spoke head complex; absence indicates central apparatus defects [26]. | Useful for diagnosing a specific subclass of PCD. |
| Protein A-Conjugated Colloidal Gold | Post-embedding immunogold labeling for TEM; allows localization of specific proteins at ultrastructural resolution [28]. | Available in different sizes (e.g., 5nm, 10nm, 15nm) for multiple labeling. |
| Tokuyasu Cryosectioning Setup | Sample preparation methodology that optimally preserves both antigenicity for IF and ultrastructure for TEM [29] [28]. | Requires ultramicrotome with cryo-attachment, sucrose for infiltration. |
| Glutaraldehyde (EM Grade) | Cross-linking fixative that provides excellent preservation of ultrastructural details for TEM. | Typically used at low concentrations (0.1-0.5%) in combination with PFA for immuno-EM. |
| Uranyl Acetate & Lead Citrate | Heavy metal stains for TEM; provide contrast to cellular structures by binding to lipids, proteins, and nucleic acids [27]. | Standard post-staining reagents for visualizing ciliary components. |
Integrated Diagnostic Workflow: From PICADAR to Confirmation
The following diagram illustrates the complete diagnostic and research pathway, integrating clinical assessment, genomics, and morphological techniques to conclusively overcome PICADAR false negatives.
This workflow demonstrates that when genetic testing is inconclusive, IF and TEM provide a powerful, complementary pathway not only to a definitive diagnosis but also to the discovery of new disease mechanisms and genes. By systematically applying these techniques, researchers and clinicians can effectively overcome the limitations of genetic screening alone.
Strategies for Diagnostic Improvement in Clinical and Research Settings
Developing Phenotype-Expanded Predictive Models
Understanding the Diagnostic Challenge: The Limitations of PICADAR
What is the primary weakness of the PICADAR score, and why is research into expanded models needed?
The Primary Ciliary Dyskinesia Rule (PICADAR) is a diagnostic predictive tool recommended by the European Respiratory Society to assess the likelihood of a Primary Ciliary Dyskinesia (PCD) diagnosis. However, a 2025 study has demonstrated that it has limited sensitivity, failing to identify a significant number of true PCD cases [11].
The core limitation is its reliance on specific clinical features. The tool's initial question rules out PCD in all individuals without a daily wet cough [11]. In the study, this single criterion excluded 7% of genetically confirmed PCD patients from further diagnostic work-up. The overall sensitivity of the score was 75%, meaning one in four confirmed PCD patients was not identified by the tool [11].
The performance is particularly poor in key patient subgroups, as shown in the table below [11].
Table 1: PICADAR Sensitivity in Key Patient Subgroups
| Patient Subgroup | Sensitivity | Median PICADAR Score |
|---|---|---|
| Overall | 75% | 7 |
| With Laterality Defects | 95% | 10 |
| With Situs Solitus (normal arrangement) | 61% | 6 |
| With Hallmark Ultrastructural Defects | 83% | - |
| Without Hallmark Ultrastructural Defects | 59% | - |
This evidence confirms that PICADAR should not be the sole factor used to initiate a PCD diagnostic work-up. Research into phenotype-expanded models is crucial to capture the full spectrum of the disease, especially for patients with normal body composition and normal ciliary ultrastructure [11].
Troubleshooting Guides & FAQs for Predictive Model Development
FAQ: Our model is performing well on one cohort but fails to generalize to others. What strategies can improve stability?
A common challenge in multi-omics predictive modeling is a lack of generalizability across different study cohorts. This often stems from cohort-specific technical variations or biological differences not captured by the model.
- Solution: Implement Cohort-Wise Cross-Validation. Instead of a simple random split of your dataset, design your validation strategy to test the model on each independent cohort separately. This provides a more realistic estimate of how your model will perform on entirely new data from a different source [30].
- Solution: Utilize Multi-Omics Integration. For complex regression tasks like predicting biomarker levels, using multi-omics data (e.g., combining transcriptomics and methylomics) can improve performance, stability, and generalizability compared to models based on a single type of data. Visible neural networks that elegantly combine these data types at the gene level have shown promise in this area [30].
- Solution: Employ Interpretable ("Visible") Neural Networks. Using neural networks that incorporate prior biological knowledge (e.g., gene and pathway annotations) not only makes the model's decisions interpretable but can also enhance its ability to learn robust, biologically-grounded patterns that generalize better to new data [30].
FAQ: We suspect our model's interpretations are unreliable and change with each training run. How can we ensure consistency?
The reliability of model interpretations is critical for generating biological insights. Instability can indicate issues with model configuration or training.
- Troubleshooting Step: Assess Interpretation Robustness. Recent research has found that interpretations from complex models can be strongly affected by different random weight initializations. To diagnose this, you should train your model multiple times with different random seeds and then quantify the consistency of the resulting interpretations (e.g., the top important genes or features) [30].
- Best Practice: Leverage Biological Knowledge. To guard against spurious interpretations, use biologically informed neural network architectures. For instance, in a multi-omics context, you can structure your network so that individual DNA methylation sites and gene expression data are connected through a shared gene layer based on genomic annotations. This built-in structure guides the model toward biologically plausible relationships [30].
- Best Practice: Perform Cohort-Wise Consistency Checks. In a multi-cohort setting, check if the same genes and pathways are consistently identified as important across the different independent cohorts. This cross-validation of interpretations strengthens the credibility of the findings [30].
FAQ: Our bioinformatics pipeline for data preprocessing keeps failing or producing errors. What are the common issues and fixes?
Errors in bioinformatics pipelines can derail research progress. Common failure points include data quality, tool compatibility, and computational resources [31].
- Common Challenge: Data Quality Issues. Low-quality raw data (e.g., from sequencing platforms) can lead to erroneous results downstream.
- Actionable Fix: Use quality control tools like FastQC and Trimmomatic to identify and remove contaminants or low-quality reads before proceeding with alignment and analysis [31].
- Common Challenge: Tool Compatibility. Conflicts between software versions or missing dependencies can disrupt the entire workflow.
- Actionable Fix: Use a workflow management system like Nextflow or Snakemake to manage software environments. Regularly update tools and use version control systems like Git to ensure reproducibility [31].
- Common Challenge: Computational Bottlenecks. Insufficient memory or processing power can cause pipelines to slow down or crash, especially with large datasets.
- Actionable Fix: Optimize parameters for tools like aligners or variant callers. For large-scale analyses, consider migrating the pipeline to a cloud computing platform (e.g., AWS, Google Cloud) that offers scalable resources [31].
Experimental Protocols for Model Development and Validation
Protocol: Building a Biologically Interpretable Multi-Omics Neural Network
This protocol outlines the methodology for creating interpretable predictive models for multi-omics data using "visible" neural networks, as demonstrated in recent research [30].
1. Input Data and Preprocessing:
- Data Types: Collect genome-wide RNA expression data (e.g., from blood) and CpG methylation data.
- Preprocessing: Follow standardized procedures for data gathering and processing across all cohorts to minimize batch effects. For the methylation data, annotate CpG sites using a tool like the Genomic Regions Enrichment of Annotations Tool (GREAT), connecting each site to its closest gene based on genomic distance [30].
2. Network Architecture Design (Visible Neural Networks):
- Gene-Level Layer:
- Create a methylation gene layer where all CpGs annotated to a specific gene are connected to a single neuron representing that gene's methylation.
- For the gene expression input, connect each gene's expression measurement directly to its corresponding gene-level neuron.
- Pathway-Level Layers (Optional):
- To model higher-order biological interactions, add hierarchical layers based on prior knowledge from databases like KEGG.
- Group genes into functional pathways (e.g., 321 pathways), then into mid-level groups (e.g., 44 groups like "endocrine system"), and finally into global-level groups (e.g., 6 groups like "organismal systems") [30].
- Implement "skip connections" from the gene layer directly to the output to ensure all genes contribute to the prediction, even those not annotated in the pathway databases [30].
- Output Layer: Use a single node with a sigmoid activation function for classification tasks (e.g., disease yes/no) or a ReLu activation for regression tasks (e.g., predicting age or biomarker levels) [30].
3. Model Training and Validation:
- Validation Strategy: Employ a cohort-wise cross-validation setting. Iteratively train the model on data from several cohorts and validate it on a held-out cohort to rigorously test generalizability [30].
- Initialization: For regression tasks, initialize the bias of the final output neuron to the mean value of the prediction outcome in the training set to improve training stability [30].
This workflow is summarized in the following diagram:
Protocol: Validating Predictive Models for Complex Traits
This protocol describes the process for developing and validating a prediction model, using the example of Near-Infrared Spectroscopy (NIRS) for phenotyping grain content, a methodology that can be adapted for other predictive applications [32].
1. Model Development (Calibration):
- Sample Selection: Use a large set of samples (e.g., 150+ genotypes) with a wide range of the trait you wish to predict.
- Reference Data: For each sample, obtain a precise laboratory measurement of the trait (e.g., grain protein content via the micro-Kjeldahl method). This is your reference ("ground truth") data.
- Mathematical Pretreatments: Employ various mathematical pretreatments on the predictor data (e.g., NIRS spectra) under a modified partial least squares (mPLS) regression model.
- Model Selection: Identify the optimal mathematical model based on statistical indicators: the lowest standard error of cross-validation (SECV), the highest coefficient of determination (RSQ), and the lowest standard error of calibration (SEC) [32].
2. Model Validation:
- Statistical Validation: Use a paired t-test to compare the model's predictions against the reference values from the laboratory method. A high coefficient of determination (R² between 0.90 and 0.97) between predicted and reference values indicates a highly accurate and effective model [32].
- Application Testing: Further validate the model by applying it to a new, independent dataset (e.g., a mapping population). Use the model's predictions to conduct downstream analyses, such as identifying genomic regions associated with the trait, which tests the model's practical utility [32].
Table 2: Essential Computational Tools for Predictive Model Development
| Tool or Resource | Function | Use Case / Explanation |
|---|---|---|
| Visible Neural Networks (VNN) [30] | Creates interpretable predictive models by incorporating biological knowledge into the network architecture. | Explains model decisions and reveals biological mechanisms, unlike "black box" models. |
| Genomics 2 Proteins (G2P) Portal [33] | Maps genetic variants and functional annotations onto protein sequences and 3D structures. | Integrates genetic, functional, and structural data to help interpret the impact of gene variants. |
| Workflow Management Systems (Nextflow, Snakemake) [31] | Streamlines pipeline execution, manages software environments, and provides error logs for debugging. | Essential for reproducible, scalable, and efficient bioinformatics analysis. |
| TiDeTree (BEAST 2 Platform) [33] | Infers time-scaled phylogenies and estimates population dynamic parameters from genetic lineage tracing data. | Useful for analyzing cellular processes like development and differentiation at a single-cell level. |
| Quality Control Tools (FastQC, MultiQC) [31] | Performs quality checks on raw sequencing data to identify errors, contaminants, or quality issues. | Critical first step in any bioinformatics pipeline to ensure downstream analysis accuracy. |
| Version Control (Git) [31] | Tracks all changes to code and scripts, ensuring full reproducibility of the analysis. | Manages code history and collaboration, a foundational best practice in computational research. |
| Cohort-Wise Cross-Validation [30] | A validation technique where a model is trained on several cohorts and tested on a held-out cohort. | Rigorously tests a model's generalizability and robustness beyond a single dataset. |
Optimizing Referral Pathways Despite Negative Screening Results
Troubleshooting Guide: Addressing PICADAR False Negatives
Frequently Asked Questions
Q1: What clinical factors might explain a false negative PICADAR result in a patient with strong PCD symptoms? A false negative PICADAR result (score <5) in a symptomatic patient can occur due to several factors. Consider patients with atypical presentations, such as those without neonatal respiratory distress or with milder upper airway symptoms. Some genetic variants of PCD may not manifest the classic clinical features included in the PICADAR scoring system. Additionally, incomplete patient history or undocumented neonatal events can lead to underestimation of the PICADAR score. For patients with persistent wet cough but scores below the threshold, consider advanced diagnostic testing regardless of the PICADAR result [12] [34].
Q2: What specialized diagnostic tests should be pursued after a negative PICADAR result when clinical suspicion remains high? When clinical suspicion for PCD persists despite a negative PICADAR screening, pursue these confirmatory diagnostic tests through specialized PCD centers: Nasal Nitric Oxide (nNO) measurement - levels ≤30 nL·min⁻¹ strongly suggest PCD; Transmission Electron Microscopy (TEM) to identify hallmark ciliary ultrastructural defects; High-Speed Video Microscopy Analysis (HSVMA) to assess ciliary beat pattern and frequency; Genetic testing for known PCD-associated mutations [12] [2]. These tests require specialized equipment and expertise but provide definitive diagnostic information.
Q3: How can referral pathways be optimized to reduce delays for patients requiring specialized PCD testing? Implement a structured referral system using the FOCUS-PDCA (Find, Organize, Clarify, Understand, Select, Plan, Do, Check, Act) methodology, which has proven effective in reducing referral delays in specialized care settings. Key strategies include: developing comprehensive electronic referral systems with clear accessibility; creating standardized referral criteria and forms; implementing rapid response protocols with triage systems categorized by urgency level; establishing clear communication channels with referring providers; and conducting regular tracking and analysis of referral patterns [35] [36] [37]. One oncology center reduced average patient acceptance time from 4.3 to 1.3 days using this approach [35].
Q4: What technological solutions can improve the accuracy and efficiency of PCD referral pathways? Electronic health record (EHR) integration allows seamless referral submission and tracking. Consider implementing referral management platforms that provide visibility into referral status, enable secure communication between providers, and track outcomes. Artificial intelligence (AI) enhanced screening strategies can improve diagnostic accuracy and reduce specialist workload - one study demonstrated that AI-assisted screening reduced radiologist workload by 54.5% while maintaining high sensitivity [38] [36]. These technologies facilitate coordination between primary, secondary, and tertiary care levels.
Q5: How should researchers design studies to investigate PICADAR false negatives and refine predictive models? Employ retrospective cohort designs analyzing patients with definitive PCD diagnoses despite negative PICADAR screens. Collect comprehensive clinical data beyond the seven PICADAR parameters, including additional neonatal history, detailed family history, and imaging findings. Use multivariate logistic regression to identify independent predictors of false negatives. External validation across multiple centers ensures generalizability. Consider simulation optimization methods, which have been successfully applied to patient referral problems in hospital-collaboration environments [39] [12].
PICADAR Performance Metrics and Validation Data
Table 1: PICADAR Diagnostic Performance Across Validation Studies
| Metric | Derivation Group (n=641) | External Validation Group (n=187) | Optimal Cut-off |
|---|---|---|---|
| Sensitivity | 0.90 | 0.90 (estimated) | ≥5 points |
| Specificity | 0.75 | 0.75 (estimated) | ≥5 points |
| Area Under Curve (AUC) | 0.91 | 0.87 | - |
| PCD Prevalence in Referred Population | 12% (75/641) | 50% (93/187) | - |
| Positive Predictive Value | 0.36 | 0.78 (at 50% prevalence) | - |
| Negative Predictive Value | 0.98 | 0.88 (at 50% prevalence) | - |
Table 2: PICADAR Scoring System Components and Point Values
| Clinical Parameter | Point Value | Notes |
|---|---|---|
| Full-term gestation | 1 | Excludes preterm infants |
| Neonatal chest symptoms | 2 | Respiratory distress at term birth |
| Neonatal intensive care admission | 2 | For respiratory support |
| Chronic rhinitis | 1 | Persistent symptoms >3 months |
| Ear symptoms | 1 | Recurrent otitis media or glue ear |
| Situs inversus | 4 | Complete mirror-image arrangement |
| Congenital cardiac defect | 2 | Associated with heterotaxy |
| Total Possible Score | 13 | Cut-off ≥5 for PCD prediction |
Experimental Protocols for PICADAR Validation Studies
Protocol 1: Diagnostic Accuracy Study Design
Patient Population: Consecutively recruit patients referred for PCD testing to avoid spectrum bias. Include patients with persistent wet cough across all age groups.
Data Collection: Use standardized proforma completed through clinical interview prior to diagnostic testing. Collect data on all seven PICADAR parameters plus additional clinical features.
Reference Standard Testing: Apply composite diagnostic criteria including at least two abnormal specialized tests ("hallmark" TEM, "hallmark" ciliary beat pattern, or nNO ≤30 nL·min⁻¹). In cases with strong clinical phenotype, diagnosis may be based on a single definitive test plus characteristic history.
Statistical Analysis: Perform logistic regression to identify significant predictors. Calculate sensitivity, specificity, positive and negative predictive values. Assess model discrimination using Area Under the Receiver Operating Characteristic Curve (AUC) and calibration with Hosmer-Lemeshow goodness-of-fit test [12].
Protocol 2: External Validation Methodology
Site Selection: Recruit multiple PCD diagnostic centers with different patient populations to assess generalizability.
Standardized Implementation: Apply identical PICADAR scoring criteria across all sites. Train staff in consistent data collection methods.
Blinded Assessment: Ensure those applying PICADAR criteria are blinded to results of definitive diagnostic testing.
Analysis: Test diagnostic performance in each validation cohort separately. Assess transportability of the prediction rule across different healthcare settings and patient demographics [12].
Research Reagent Solutions for PCD Diagnostic Studies
Table 3: Essential Materials for PCD Diagnostic Research
| Reagent/Equipment | Function/Application | Specifications |
|---|---|---|
| Nasal Nitric Oxide Analyzer | nNO measurement for PCD screening | Chemiluminescence analyzer capable of detecting nNO ≤30 nL·min⁻¹ |
| Transmission Electron Microscope | Ultrastructural analysis of ciliary defects | High-resolution TEM for identifying dynein arm defects, microtubular disorganization |
| High-Speed Video Microscope | Ciliary beat pattern analysis | Capable of recording at ≥500 frames per second with analysis software |
| Cell Culture Media | Ciliary epithelial cell culture | DMEM/F12 with antibiotics and fetal bovine serum for air-liquid interface culture |
| Genetic Sequencing Panel | PCD-associated gene mutation detection | Next-generation sequencing panel covering known PCD genes (DNAH5, DNAI1, CCDC39, etc.) |
| Immunofluorescence Antibodies | Protein localization in cilia | Antibodies against dynein proteins, tubulin, and other ciliary components |
Workflow Diagrams for Referral Pathway Optimization
Diagram 1: Enhanced Referral Pathway for Negative PICADAR
Diagram 2: System Optimization Using FOCUS-PDCA
Leveraging Genetic Findings to Recalibrate Clinical Suspicion
Troubleshooting Guides
Guide 1: Resolving a Negative PICADAR Score in a Symptomatic Patient
Problem: A patient presents with strong clinical features suggestive of Primary Ciliary Dyskinesia (PCD), such as chronic wet cough and neonatal respiratory distress, but scores below the predictive threshold on the PICADAR clinical scoring tool, potentially delaying definitive diagnosis and appropriate management [40].
Investigation & Solution:
Step 1: Re-evaluate Clinical Inputs
- Action: Double-check the accuracy and completeness of all data entered into the PICADAR calculator. Confirm the presence and documentation of key features like neonatal respiratory distress, which is a high-score item [40].
- Expected Outcome: Ensure the score was not artificially low due to incomplete data entry or subjective interpretation of symptoms.
Step 2: Initiate Advanced Genetic Testing
- Action: Proceed with comprehensive genetic testing, as a negative PICADAR does not rule out PCD. A significant proportion of genetically confirmed PCD patients have an incomplete genetic diagnosis after standard testing [41].
- Methodology:
- Initial Test: Order a next-generation sequencing (NGS) panel of known PCD genes [41].
- If Inconclusive: For patients with only a single heterozygous pathogenic variant, pursue end-to-end gene sequencing of key PCD genes (e.g., DNAH11). This method sequences non-coding intronic regions, unlike standard tests that focus on exons [41].
- Validation: For identified intronic variants, perform cDNA analysis from nasal brushings to confirm the variant causes aberrant splicing [41].
- Expected Outcome: Identification of pathogenic non-coding variants that explain the PCD phenotype despite the low PICADAR score. This can increase the genetic diagnostic yield for PCD from approximately 46.8% to over 50% [41].
Step 3: Integrate Findings into Clinical Profile
- Action: Use the positive genetic finding to recalibrate the clinical suspicion for PCD. This genetic evidence overrides the negative PICADAR score and justifies a definitive diagnosis.
- Expected Outcome: The patient receives a confirmed PCD diagnosis, enabling access to appropriate care, genetic counseling, and potential future therapies.
Guide 2: Interpreting a Variant of Uncertain Significance (VUS) in a Patient with a High PICADAR Score
Problem: A patient with a high PICADAR score undergoes genetic testing, but the result returns a VUS, leaving the diagnosis unresolved and creating uncertainty for clinical management and family counseling [41].
Investigation & Solution:
Step 1: Functional Validation
- Action: Do not base a clinical diagnosis solely on a VUS. Seek functional studies to determine the variant's pathogenicity.
- Methodology: The gold standard is cDNA analysis from patient-derived cells (e.g., nasal epithelial cells) to assess if the variant disrupts RNA splicing or expression [41]. Alternative approaches include developing patient-derived organoid models to study ciliary function [41].
- Expected Outcome: Biochemical evidence that upgrades the VUS to "Likely Pathogenic" or confirms it as "Benign."
Step 2: Leverage Genomic Databases
- Action: Inquire if the testing laboratory has shared the VUS data or can check international PCD-specific genomic databases such as ClinGen and CiliaVar [41].
- Expected Outcome: Discovery of identical variants in other, unrelated PCD patients, which provides strong evidence for pathogenicity and allows for variant reclassification.
Step 3: Correlate with Phenotype
- Action: If functional studies are not possible, closely correlate the genotype with the patient's clinical phenotype and results from other diagnostic tests (e.g., electron microscopy, nasal nitric oxide).
- Expected Outcome: A strong, classic PCD phenotype in the presence of a VUS in a known PCD gene may support a clinical diagnosis while awaiting more definitive evidence.
Frequently Asked Questions (FAQs)
Q1: Our research involves patients with clinical PCD but no definitive genetic diagnosis. What is the most effective genetic approach to identify novel variants? A: For research aimed at discovering novel variants, especially non-coding ones, end-to-end gene sequencing of known PCD genes is the most effective method. This approach sequences both exons and introns. A 2025 study using this method on 17 PCD genes in undiagnosed patients found new pathogenic variants in 38% of cases, the majority of which were intronic splice-altering variants that standard panels miss [41].
Q2: Why is the turnaround time for Whole Genome Sequencing (WGS) longer than for a targeted gene panel? A: Targeted panels use high-throughput assays focused on a predefined set of genes, streamlining analysis. In contrast, WGS performs sequencing on the entire genome, which requires significantly more time for data generation, complex interpretation across all genes, and comprehensive reporting [42].
Q3: What is the critical difference between a CLIA-approved lab and a research lab for genetic testing? A: CLIA-approved labs are certified under the Clinical Laboratory Improvement Amendments, requiring strict quality controls, proficiency testing, and personnel standards to ensure results are reliable for clinical diagnosis. Research labs are generally exempt from these standards; their results are intended for discovery and cannot be used for clinical patient management [42].
Q4: A patient has a known pathogenic variant in one PCD gene allele, but we cannot find a second variant. What could explain this? A: The second pathogenic variant may reside in a non-coding region (like an intron) not covered by your initial test [41]. Another possibility is that the condition has a more complex genetic basis, such as a multigenic contribution, or that the phenotype is caused by a mutation in a novel PCD gene not included on the testing panel.
Q5: How can we ensure consistency in genetic testing for a multi-site clinical trial? A: Using a centralized genetic testing provider is essential. This ensures every sample is processed and analyzed in a single laboratory using identical assay methods, interpretation guidelines, and reporting standards. This practice avoids inter-lab classification discrepancies and reduces logistical complexity at clinical sites [42].
Data Presentation
Table 1: Impact of End-to-End Gene Sequencing on PCD Diagnostic Yield
Data derived from a 2025 study sequencing 17 PCD genes in 42 patients with an incomplete genetic diagnosis [41].
| Metric | Initial Yield (Standard Genetic Testing) | Final Yield (After End-to-End Sequencing) | Net Gain |
|---|---|---|---|
| Overall Genetic Diagnosis | 46.8% | 50.0% | +3.2 percentage points |
| Selected Cohort with Incomplete Diagnosis | 0% (by definition) | 38% (16/42 patients) | +16 patients diagnosed |
| Pathogenic Non-Coding Variants Identified | N/A | 12 intronic variants (10 predicted splice-altering) | N/A |
Table 2: Key Methodologies for Resolving PCD Genetic Diagnoses
Summary of experimental protocols for overcoming false negatives.
| Method | Key Procedure | Application in PCD | Critical Consideration |
|---|---|---|---|
| End-to-End Gene Sequencing | Sequences entire genomic region of a gene, including exons and introns [41]. | Identifying deep intronic variants that disrupt splicing [41]. | More costly and complex to interpret than targeted panels. |
| cDNA Analysis | RNA is extracted from patient cells (nasal brushing), reverse-transcribed to cDNA, and sequenced [41]. | Functional validation of splicing defects caused by intronic variants [41]. | Requires freshly collected cells with viable RNA; not always feasible. |
| Centralized Genetic Testing | All study/trial samples are processed and analyzed at a single, high-volume CLIA lab [42]. | Ensuring consistent variant classification and reporting across a patient cohort [42]. | Avoids discrepancies between different laboratories' methodologies. |
Diagnostic Workflow Visualization
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for PCD Genetic Research
| Research Reagent / Tool | Function in Research | Example/Note |
|---|---|---|
| Next-Generation Sequencing (NGS) Platform | High-throughput sequencing of targeted PCD gene panels, whole exomes, or whole genomes [43]. | Enables the initial screening for pathogenic mutations in coding regions. |
| End-to-End Gene Sequencing Assay | Comprehensive sequencing of entire gene loci, including introns and exons, to identify deep intronic and structural variants [41]. | Critical for resolving cases with a single identified variant or strong phenotype with negative panel results. |
| RNA Extraction Kit | Isolates high-quality RNA from patient-derived cells (e.g., nasal brushings) for downstream cDNA synthesis [41]. | Quality of starting RNA is crucial for successful cDNA analysis. |
| cDNA Synthesis Kit | Reverse transcribes RNA into complementary DNA (cDNA) for splicing analysis and functional validation of variants [41]. | Used to confirm whether an intronic variant causes aberrant mRNA splicing. |
| PCD-Specific Genomic Databases | International repositories for sharing and comparing genetic variants linked to PCD phenotypes [41]. | ClinGen and CiliaVar are key resources for variant interpretation and reclassification. |
| Automated Nucleic Acid Extraction System | Standardizes and automates the DNA/RNA extraction process, improving efficiency and reducing human error in sample preparation [43]. | Essential for handling large sample volumes in research studies or clinical trials. |
Resource-Adapted Approaches for Diverse Healthcare Settings
Troubleshooting Guides and FAQs: Navigating PICADAR False Negatives in PCD Research
Frequently Asked Questions
Q1: What is the primary limitation of the PICADAR tool in PCD diagnosis? The PICADAR tool has limited sensitivity, particularly in specific patient subgroups. It uses an initial question about "daily wet cough" to rule out PCD; individuals without this symptom are automatically considered negative. Overall, its sensitivity is approximately 75%, meaning it misses about a quarter of true PCD cases. Sensitivity drops significantly to 61% in patients without laterality defects (situs solitus) and to 59% in patients whose PCD is not associated with hallmark ciliary ultrastructural defects [11].
Q2: Why should PICADAR not be used as the sole screening tool? Relying solely on PICADAR risks a substantial number of false-negative results, leading to missed diagnoses and delayed treatment. Expert guidelines and recent research emphasize that a combination of diagnostic methods is essential. No single test, including PICADAR, nasal nitric oxide (nNO), or high-speed video analysis (HSVA), is perfect on its own. A comprehensive diagnostic work-up should proceed if clinical suspicion is high, even if a PICADAR score is low [11] [4].
Q3: Which patient populations are most at risk for a false-negative PICADAR result? The following patient groups are at the highest risk of being missed by PICADAR [11]:
- Patients who do not report a daily wet cough.
- Patients with situs solitus (normal organ arrangement) rather than situs inversus.
- Patients whose PCD is caused by genetic mutations that do not result in hallmark defects on transmission electron microscopy (TEM).
Q4: What is the recommended diagnostic pathway when PICADAR is negative but clinical suspicion for PCD remains high? A negative PICADAR score should not terminate the diagnostic process if clinical history is suggestive of PCD. The European Respiratory Society (ERS) guidelines recommend further investigation with a combination of tools. The flow below outlines this diagnostic pathway.
The table below summarizes the sensitivity of the PICADAR tool across different patient populations, highlighting its limitations [11].
| Patient Population | Sensitivity | Median PICADAR Score (IQR) | Key Risk Factor for False Negatives |
|---|---|---|---|
| Overall PCD Cohort | 75% (202/269) | 7 (5 - 9) | Initial 'no daily wet cough' rule excludes 7% of patients |
| With Laterality Defects | 95% | 10 (8 - 11) | Lower overall score due to fewer points from laterality |
| Without Laterality Defects (Situs Solitus) | 61% | 6 (4 - 8) | Absence of points for situs inversus |
| With Hallmark Ultrastructural Defects | 83% | Not Specified | Genetic mutations affecting ciliary beat pattern without structural defects |
| Without Hallmark Ultrastructural Defects | 59% | Not Specified |
Experimental Protocol: A Comprehensive Approach to Overcome PICADAR Limitations
This protocol outlines a multi-modal diagnostic strategy to mitigate the risk of false negatives when screening for Primary Ciliary Dyskinesia (PCD).
1. Objective To establish a robust, resource-adapted diagnostic workflow for PCD that minimizes false-negative results by integrating PICADAR with other diagnostic modalities, particularly in cases of high clinical suspicion.
2. Materials and Equipment
- PICADAR Tool: The validated 7-question predictive tool.
- nNO Analyzer: Equipment for measuring nasal nitric oxide.
- High-Speed Video Microscope: For ciliary beat frequency and pattern analysis.
- Cell Culture Incubator: For ciliary re-differentiation following air-liquid interface culture.
- Transmission Electron Microscope (TEM): For visualizing ciliary ultrastructure.
- Genetic Sequencing Platform: For next-generation sequencing of known PCD-associated genes.
3. Methodology
Step 1: Initial Clinical Assessment and PICADAR Scoring
- Administer the PICADAR tool to all patients with clinical features suggestive of PCD (e.g., lifelong wet cough, neonatal respiratory distress, chronic rhinosinusitis, otitis media).
- Troubleshooting Tip: Do not discontinue the diagnostic pathway based on a low PICADAR score alone. A strong clinical history warrants further investigation [4].
Step 2: Secondary Functional Testing
- Perform nasal nitric oxide (nNO) measurement. Note that nNO can also be normal in some PCD cases, so a normal result does not rule out PCD [4].
- Perform high-speed video analysis (HSVA) of ciliary beat frequency and pattern on a fresh nasal brush or biopsy sample.
- Troubleshooting Tip: If HSVA is abnormal, it provides strong evidence for PCD, even if subsequent genetic tests or TEM are normal. Conversely, a normal HSVA does not completely rule out PCD, but makes it less likely [4].
Step 3: Confirmatory Cellular and Genetic Testing
- If functional tests (nNO or HSVA) are abnormal, proceed to confirmatory testing.
- Culture respiratory epithelial cells at an air-liquid interface to allow ciliary re-differentiation. This step is crucial for clearing secondary damage and obtaining a reliable result for both HSVA and TEM.
- Perform transmission electron microscopy (TEM) on the cultured cells to assess ciliary ultrastructure.
- Initiate genetic testing via a targeted PCD gene panel or whole-exome sequencing.
Step 4: Data Integration and Diagnosis
- Correlate all findings—clinical history, PICADAR score, nNO, HSVA, TEM, and genetics. A definitive PCD diagnosis is made based on a characteristic clinical phenotype plus either biallelic pathogenic mutations in a PCD gene or a definitive ciliary ultrastructural defect on TEM [4].
- Troubleshooting Tip: In cases of conflicting results (e.g., abnormal HSVA with normal genetics and TEM), the patient should be considered "highly likely" to have PCD and managed accordingly, while acknowledging the limitations of current diagnostic technology [4].
Research Reagent Solutions for PCD Diagnostic Research
The table below lists key materials and their applications in establishing a PCD diagnostics research pipeline.
| Research Reagent / Material | Function in PCD Research |
|---|---|
| Air-Liquid Interface (ALI) Culture Media | Supports the differentiation of ciliated respiratory epithelial cells from patient biopsies, essential for obtaining primary cilia free of secondary infection-related damage for functional and structural analysis. |
| Transmission Electron Microscopy (TEM) Reagents | A suite of chemicals (e.g., glutaraldehyde, osmium tetroxide) for fixing, staining, and processing ciliated cell samples to visualize the 9+2 microtubular arrangement and other ultrastructural defects. |
| Targeted PCD Gene Panel | A curated set of primers or probes for next-generation sequencing of over 50 known PCD-associated genes, enabling efficient and comprehensive genetic diagnosis. |
| High-Speed Video Analysis (HSVA) Software | Specialized software for capturing and quantitatively analyzing ciliary beat frequency and pattern from high-frame-rate video recordings of ciliary motion. |
| Anti-Acetylated Tubulin Antibody | An immunofluorescence reagent used to label ciliary axonemes, allowing for visualization of cilia presence, length, and organization in patient cell samples. |
Evaluating Diagnostic Accuracy and Future Directions
Primary Ciliary Dyskinesia (PCD) is a rare, genetically heterogeneous, inherited ciliopathy characterized by impaired mucociliary clearance. This leads to recurrent respiratory tract infections, chronic rhinosinusitis, otitis media, bronchiectasis, and laterality defects in approximately half of patients [44]. A significant challenge in managing PCD is the frequent delay in diagnosis, often due to its nonspecific clinical presentation and the limited availability of specialized testing [44]. Accurate and early diagnostic tools are therefore critical for initiating appropriate care and improving long-term patient outcomes.
This technical support guide focuses on the performance and limitations of the Primary Ciliary Dyskinesia Rule (PICADAR), a diagnostic predictive tool, in the context of emerging research and technologies. It is structured to help researchers and clinicians troubleshoot diagnostic challenges, particularly the issue of false negatives, by providing a comparative analysis and detailed experimental methodologies.
Performance Analysis: PICADAR vs. Alternative Diagnostic Modalities
What is PICADAR and how is it used?
The Primary Ciliary Dyskinesia Rule (PICADAR) is a clinical predictive tool designed to assess the likelihood of PCD before proceeding with more complex, costly, or invasive confirmatory tests [11] [4]. It was developed to help identify patients who should be referred for definitive PCD diagnostic testing. The tool uses an initial screening question followed by a points-based scoring system for patients who pass the initial screen [11].
- Initial Screening Question: The tool first asks, "Does the patient have a daily wet cough?" If the answer is no, PICADAR rules the patient negative for PCD, and no further scoring is performed [11].
- Scoring System: For patients with a daily wet cough, seven additional questions related to clinical history are used to calculate a score. A score of ≥5 points is recommended as the threshold to suggest a high likelihood of PCD and warrant further diagnostic investigation [11] [4].
What are the documented limitations and false-negative rates of PICADAR?
Recent research has highlighted significant limitations in PICADAR's sensitivity, making it an imperfect screening tool. A 2025 study by Omran et al. evaluated PICADAR in 269 individuals with genetically confirmed PCD and found its performance to be suboptimal, especially in specific patient subgroups [11].
Key Limitations and False-Negative Concerns:
- Initial Screen Exclusion: The study found that 7% (18/269) of genetically confirmed PCD patients reported no daily wet cough. These individuals were ruled out by the initial question and never reached the scoring stage, representing a direct source of false negatives [11].
- Overall Sensitivity: The overall sensitivity of PICADAR (proportion of true PCD patients scoring ≥5) was only 75% [11]. This means one in four confirmed PCD patients would be missed by the tool.
- Performance in Subgroups: The sensitivity varies dramatically based on patient phenotype:
- Patients with laterality defects (e.g., situs inversus): Sensitivity was high at 95% [11].
- Patients with situs solitus (normal organ arrangement): Sensitivity dropped drastically to 61% [11].
- Patients without hallmark ultrastructural defects on electron microscopy: Sensitivity was also low, at 59% [11].
The conclusion from this research is that PICADAR should not be the sole factor in deciding to initiate a PCD diagnostic work-up, particularly for patients without laterality defects or with normal ciliary ultrastructure [11].
How does PICADAR compare to other diagnostic criteria and tools?
The North American Criteria Defined Clinical Features (NA-CDCF) is another clinical tool used to identify patients for PCD testing. The following table provides a structured comparison of PICADAR, NA-CDCF, and key confirmatory diagnostic tests based on current literature.
Table 1: Comparative Performance of PCD Diagnostic Tools and Tests
| Metric | PICADAR Score | NA-CDCF Criteria | Nasal Nitric Oxide (nNO) | High-Speed Video Microscopy Analysis (HSVA) |
|---|---|---|---|---|
| Purpose & Type | Clinical predictive rule | Clinical feature checklist | Confirmatory/Supportive test | Confirmatory/Supportive test |
| How it Works | 7-item questionnaire with points [11] | Presence of ≥2 of 4 clinical features [4] | Measures level of nNO, which is typically low in PCD [4] | Analyzes ciliary beat pattern and frequency [44] [4] |
| Reported Sensitivity | 75% (overall); 61% (situs solitus) [11] | ~80% [4] | High, but not 100% (risk of false negatives) [4] | High accuracy for diagnosis [4] |
| Reported Specificity | 48% (at cutoff ≥5) [4] | 72% [4] | High, but not 100% [44] | High, but can be falsely positive [4] |
| Key Advantage | Simple, quick, objective score | Simple, based on major clinical features | Non-invasive, quick result | Provides functional assessment, can detect cases with normal ultrastructure [4] |
| Key Limitation | Low sensitivity in key subgroups; reliant on daily wet cough [11] | Misses ~20% of PCD patients (false negatives) [4] | Can be normal in some PCD cases (e.g., with DNAH11 mutations) [44] [4] | Requires specialized equipment and expertise [44] |
What emerging tools and AI platforms could influence future PCD diagnosis?
While direct applications of AI for PCD diagnosis are not yet mature, the field of AI-driven drug discovery and disease modeling is advancing rapidly. These technologies represent the frontier of diagnostic innovation and could potentially be adapted for complex rare diseases like PCD in the future.
Table 2: Overview of Emerging AI Platforms with Potential Diagnostic Utility
| Platform / Tool | AI Approach | Primary Application | Potential Future Relevance for PCD |
|---|---|---|---|
| PDGrapher [45] | Graph Neural Network | Identifies genes and drug combinations to reverse diseased cells to a healthy state. | Could model ciliary dysfunction and predict therapeutic targets to correct ciliary beating. |
| Digital Twins / Virtual Patients [46] | Quantitative Systems Pharmacology (QSP) | Creates simulated patients to run clinical trial simulations and test interventions. | Could be used to simulate individual patient ciliary function and predict response to treatments. |
| Generative AI & Model Compression [47] | Generative Models, Compression Algorithms | Generates novel molecular structures and optimizes AI models for smaller devices. | Could aid in rapid genetic variant interpretation or enable portable diagnostic aids. |
| Atomwise, Insilico Medicine [48] [49] | Deep Learning, Generative Chemistry | Accelerates target identification and drug candidate design. | Could help identify novel PCD gene functions or therapies aimed at specific genetic defects. |
Troubleshooting Guides & FAQs: Addressing PICADAR False Negatives
FAQ 1: A patient with a strong clinical phenotype for PCD was ruled out by PICADAR's initial "daily wet cough" question. What should I do?
Answer: This scenario highlights a critical flaw in relying solely on PICADAR. A 2025 study confirmed that 7% of genetically proven PCD patients do not have a daily wet cough [11]. If the clinical suspicion for PCD remains high based on other features (e.g., neonatal respiratory distress in a term infant, laterality defect, persistent non-seasonal rhinitis, or recurrent otitis media), you should proceed with further diagnostic testing and not consider PCD ruled out [44] [4]. Adhere to guideline recommendations that suggest further investigation is warranted in patients with several typical PCD features, irrespective of a single predictive tool's result [4].
FAQ 2: How can I validate a PCD diagnosis in a patient with a high PICADAR score but normal electron microscopy (TEM) results?
Answer: A normal TEM result does not exclude PCD, as approximately 20-30% of true PCD cases have normal ciliary ultrastructure [4]. In this situation, a multi-step diagnostic process is essential.
- Functional Analysis: Perform High-Speed Video Microscopy Analysis (HSVA) to assess ciliary beat pattern. An abnormal, dyskinetic beat pattern strongly supports a PCD diagnosis even with normal TEM [44] [4].
- Genetic Testing: Initiate extensive genetic testing, including a PCD gene panel. Mutations in genes like DNAH11, GAS8, and HYDIN are known to cause PCD with normal ultrastructure [44] [4].
- Immunofluorescence (IF): Use IF staining with antibodies against specific ciliary proteins (e.g., DNAH5) to identify mislocalized proteins, which can indicate a defect even when structure appears normal [44]. The European Respiratory Society guidelines state that repeatedly abnormal HSVA with a compatible clinical history makes PCD "highly likely," and treatment should be initiated while awaiting genetic confirmation [4].
FAQ 3: Our lab is developing a new predictive model for PCD. What are the key patient subgroups to include to avoid the pitfalls of PICADAR?
Answer: To build a more robust model than PICADAR, ensure your training and validation datasets are enriched for the following subgroups that are known to cause false negatives in existing tools [11]:
- PCD patients with situs solitus (normal organ arrangement).
- PCD patients without hallmark ultrastructural defects (e.g., those with normal TEM or isolated inner dynein arm defects).
- PCD patients who lack a daily wet cough from infancy.
- PCD patients with mutations in genes not associated with classic ODA/IDA defects (e.g., DNAH11, CCDC39, CCDC40, RSPH genes).
Including these phenotypes will force the model to learn from a wider spectrum of the disease's genetic and clinical diversity, improving overall sensitivity.
Experimental Protocols for Validating PCD Diagnostic Findings
Protocol 1: Multi-Modal Diagnostic Workflow for Suspected PCD
This protocol outlines a comprehensive diagnostic pathway that mitigates the risk of false negatives from any single test.
Objective: To confirm or exclude a diagnosis of PCD in a patient with suggestive clinical features, using a sequential, multi-modal approach. Background: No single test for PCD has perfect sensitivity and specificity. A combination of tests is required for an accurate diagnosis, especially in cases with atypical presentations or conflicting initial results [44] [4].
Materials: * See "Research Reagent Solutions" section below. Procedure: 1. Initial Clinical Assessment: Apply clinical tools like PICADAR or NA-CDCF with the understanding of their limitations. Record full clinical history including neonatal history, laterality, and chronic symptoms. 2. First-Line Objective Tests: Perform nNO measurement and HSVA. * Interpretation: If both nNO and HSVA are unequivocally normal, PCD is unlikely. If either is abnormal/suggestive, proceed to step 3 [4]. 3. Confirmatory Testing: Initiate TEM and genetic testing concurrently. * Interpretation: A definitive pathogenic mutation in a PCD-associated gene confirms the diagnosis. A hallmark ultrastructural defect on TEM (e.g., ODA loss) also confirms the diagnosis. 4. Integrated Diagnosis (For Discordant Results): * Scenario: Abnormal HSVA + Normal TEM + No definitive genetic findings. * Action: Consider ciliary culture to exclude secondary dyskinesia. Repeat HSVA. Perform immunofluorescence staining. Classify as "highly likely PCD" per ERS guidelines and manage accordingly, while continuing to seek genetic validation [4].
Diagram Title: Comprehensive PCD Diagnostic Workflow
Protocol 2: In Silico Validation of Genetic Variants using AI-Based Pathogenicity Prediction
Objective: To utilize emerging AI tools to assist in the interpretation of Variants of Unknown Significance (VUS) found during PCD genetic testing. Background: Genetic testing often uncovers VUS. AI tools that model protein structure and function can provide supporting evidence for variant pathogenicity, helping to resolve ambiguous cases [45] [49].
Materials:
- Hardware: Computer with internet access.
- Software: Access to AI-based pathogenicity prediction tools (e.g., AlphaFold for protein structure, PDGrapher-like network analysis) [45] [49].
- Input: Genetic variant data (gene, nucleotide change, amino acid change).
Procedure:
- Data Extraction: From genetic test report, extract the VUS information: Gene name, cDNA (DNA) change, and protein (amino acid) change.
- Structural Analysis:
- Input the wild-type and mutant protein sequences into a structure prediction tool like AlphaFold [49].
- Compare the predicted 3D structures of the wild-type and mutant protein. Note any significant disruptions in protein folding, stability, or key functional domains.
- Network Analysis (Conceptual):
- Leveraging concepts from tools like PDGrapher, map the variant gene's product onto known ciliary protein interaction networks [45].
- Predict the downstream impact of the mutation on the broader network function (e.g., "Does this disruption in Gene A likely affect the assembly of Protein Complex B?").
- Evidence Integration: Combine the in silico predictions with clinical, functional (HSVA, IF), and ultrastructural (TEM) data. Strong computational evidence of pathogenicity can support the reclassification of a VUS to "Likely Pathogenic."
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents for PCD Diagnostic and Research Experiments
| Reagent / Material | Function / Application | Example Use in PCD Research |
|---|---|---|
| Anti-DNAH5 Antibody | Immunofluorescence (IF) staining to localize the outer dynein arm heavy chain protein. | Detects mislocalization or absence of DNAH5 in cilia, confirming ODA defects even in samples with suboptimal TEM [44]. |
| Anti-GAS8 Antibody | IF staining for a component of the nexin-dynein regulatory complex (NDRC). | Investigates defects associated with microtubule disorganization and inner dynein arm anomalies [44]. |
| Cell Culture Media for Ciliary Differentiation | Supports the growth and differentiation of human airway epithelial cells at an air-liquid interface (ALI). | Generates ciliated cell cultures from patient biopsies, allowing for repeated HSVA and functional studies without repeated nasal brushing [4]. |
| Nasal Nitric Oxide (nNO) Analyzer | Measures the concentration of nitric oxide in nasal air. | Used as a non-invasive, high-sensitivity screening test; low nNO is a strong indicator of PCD [44] [4]. |
| Transmission Electron Microscope (TEM) | Provides high-resolution imaging of ciliary ultrastructure. | The gold standard for identifying hallmark defects like absent outer/inner dynein arms or microtubular disorganization [44]. |
| Next-Generation Sequencing (NGS) Panels | Targets >50 known PCD-associated genes for simultaneous genetic analysis. | Identifies pathogenic mutations for confirmatory diagnosis, especially in cases with normal ultrastructure [44] [4]. |
International Validation Efforts and Real-World Implementation Data
# FAQ: Troubleshooting PICADAR False Negatives
### What are the documented limitations of the PICADAR score in international validation studies?
Recent international validation studies have revealed specific limitations in the PICADAR tool's sensitivity. A 2025 study by Omran et al. found that its performance is highly variable across different patient subgroups [11].
The table below summarizes the key performance metrics from validation efforts:
| Study / Population | Overall Sensitivity | Sensitivity in Situs Solitus (no laterality defects) | Sensitivity without Hallmark Ultrastructural Defects |
|---|---|---|---|
| Original Derivation (Behan et al., 2016) [12] | 0.90 (90%) | Information not specified | Information not specified |
| External Validation (Omran et al., 2025) [11] | 0.75 (75%) | 0.61 (61%) | 0.59 (59%) |
A critical design limitation is that PICADAR automatically rules out PCD in individuals without a persistent daily wet cough. The 2025 study found that 7% of genetically confirmed PCD patients did not report this symptom and would have been missed solely based on this initial criterion [11]. Performance is significantly higher in patients with laterality defects (e.g., situs inversus) than in those with normal organ arrangement (situs solitus) [11].
### Which patient subgroups are most at risk for a false negative PICADAR result?
Your research should be particularly vigilant for false negatives in the following patient profiles:
- Patients without a daily wet cough: These individuals are filtered out before the scoring begins [11].
- Patients with situs solitus (normal organ arrangement): The sensitivity of PICADAR drops substantially in this group [11].
- Patients with normal ciliary ultrastructure: The tool is less effective at identifying patients who have PCD caused by genetic variants that do not produce the classic "hallmark" defects visible under transmission electron microscopy (TEM) [11].
- Patients with specific genetic variants: Variants in genes such as CCDC103, DNAH9, and RSPH1 can be associated with normal nasal nitric oxide (nNO) levels and may present with atypical clinical features, potentially leading to false negatives on clinical prediction tools [4].
### What complementary diagnostic strategies can mitigate the risk of false negatives?
To overcome the limitations of PICADAR, a multi-assay diagnostic approach is essential. The European Respiratory Society (ERS) guidelines recommend that no single test is sufficient to rule out PCD [4].
The following diagnostic workflow illustrates the recommended pathway to minimize false negatives:
The cornerstone of mitigating false negatives is to never exclude a PCD diagnosis based on a single test [4]. Key strategies include:
- Combining Functional and Structural Tests: Use high-speed video microscopy analysis (HSVA) to detect abnormal ciliary beat patterns, even in patients with normal nNO or normal TEM [4].
- Incorporating Genetics: Genetic testing can provide a definitive diagnosis, especially in cases with conflicting or borderline results from other tests. Always ensure that identified genetic variants are confirmed as pathogenic and are consistent with the clinical and functional phenotype [4].
- Clinical Override: A strong clinical history, such as a sibling with confirmed PCD or a classic phenotype, should warrant further specialist testing regardless of the PICADAR score [12] [4].
### What is the detailed protocol for a multi-assay diagnostic approach as per ERS guidelines?
The following protocol outlines the key experiments in a comprehensive PCD diagnostic workup.
Experiment 1: Nasal Nitric Oxide (nNO) Measurement
- Objective: To measure nNO levels as a screening test. Low nNO is a supportive, but not definitive, indicator of PCD.
- Methodology:
- nNO is measured using a chemiluminescence analyzer during velum closure.
- The patient performs a slow exhalation against resistance from total lung capacity over 30-45 seconds.
- The procedure is repeated until three plateau values agree within 10%.
- Interpretation: nNO values ≤30 nL·min⁻¹ in children or ≤50 nL·min⁻¹ in adults are highly suggestive of PCD. Note: Some genetic variants can present with normal nNO, so a normal measurement cannot rule out PCD [4] [2].
Experiment 2: High-Speed Video Microscopy Analysis (HSVA)
- Objective: To qualitatively and quantitatively assess ciliary beat pattern and frequency.
- Methodology:
- Nasal epithelial cells are obtained via brushing biopsy.
- Ciliated edges are recorded at high frame rates (≥500 frames per second) using a high-speed video camera.
- Videos are analyzed for beat pattern, frequency, and coordination.
- Interpretation: A consistently abnormal, dyskinetic beat pattern across multiple samples is indicative of PCD. HSVA can identify patients with normal nNO and normal ultrastructure, making it critical for capturing false negatives from other tests [4].
Experiment 3: Transmission Electron Microscopy (TEM)
- Objective: To visualize the internal ultrastructure of cilia.
- Methodology:
- Ciliated samples are fixed in glutaraldehyde and processed for TEM.
- Ultrathin sections are stained and examined under the electron microscope.
- Multiple cilia are assessed for the presence of hallmark defects, such as outer dynein arm loss, inner dynein arm loss, or microtubular disorganization.
- Interpretation: The presence of a hallmark defect confirms PCD. However, a normal ultrastructure does not rule out PCD, as up to 30% of genetically confirmed cases have normal TEM [4].
Experiment 4: Genetic Analysis
- Objective: To identify biallelic pathogenic mutations in known PCD-associated genes.
- Methodology:
- Next-generation sequencing using targeted PCD gene panels, whole-exome, or whole-genome sequencing.
- Identified variants are confirmed and segregated within the family via Sanger sequencing.
- Interpretation: Finding biallelic pathogenic mutations in a PCD-associated gene is confirmatory. Caution is required with variants of unknown significance (VUS); their pathogenicity must be assessed in the context of the clinical and functional phenotype [4].
# The Scientist's Toolkit: Research Reagent Solutions
The table below details essential materials and their functions for establishing key PCD diagnostic assays.
| Research Reagent / Tool | Primary Function in PCD Diagnostics |
|---|---|
| Nasal Nitric Oxide (nNO) Analyzer | Measures nasal nitric oxide concentration; low levels are a sensitive screening biomarker for most forms of PCD [4] [2]. |
| High-Speed Video Microscope | Captures ciliary beat patterns at high frame rates to visualize and analyze ciliary motility and diagnose dyskinesia [4]. |
| Transmission Electron Microscope | Visualizes the internal ultrastructure (axoneme) of cilia to identify hallmark structural defects (e.g., missing dynein arms) [12] [4]. |
| PCD Genetic Testing Panel | Identifies pathogenic mutations in over 50 known PCD-associated genes, providing a definitive molecular diagnosis [4] [2]. |
| Air-Liquid Interface (ALI) Cell Culture | Re-differentiates ciliated epithelium in vitro to rule out secondary ciliary dyskinesia and perform functional/genetic validation [12]. |
Biomarker Discovery for Objective Disease Identification
Troubleshooting Common Biomarker Discovery Challenges
This section addresses specific experimental and analytical hurdles researchers face during biomarker discovery and validation, with a focus on improving diagnostic tools like PICADAR for Primary Ciliary Dyskinesia (PCD).
FAQ 1: How can we address the limited sensitivity of clinical prediction tools like PICADAR in specific patient subgroups?
The Challenge: The PICADAR (Primary Ciliary Dyskinesia Rule) tool demonstrates variable sensitivity, potentially missing true PCD cases. A 2025 study found its overall sensitivity is 75%, meaning one in four PCD cases is missed. Performance is worse in patients without laterality defects (61% sensitivity) or hallmark ultrastructural ciliary defects (59% sensitivity). A fundamental limitation is that it automatically excludes patients without a daily wet cough, which applies to 7% of genetically confirmed PCD cases [1] [6].
Troubleshooting Guide:
- Action: Integrate Multi-Omics Data.
- Rationale: Relying solely on clinical history scores limits sensitivity. Multi-omics approaches provide a holistic molecular view of disease, capturing heterogeneity that clinical checklists miss [50] [51].
- Methodology: Supplement clinical scoring with genomic, proteomic, and metabolomic profiling from patient samples. For PCD, this means combining PICADAR with next-generation sequencing (NGS) gene panel testing to identify pathogenic variants regardless of clinical presentation [52].
- Expected Outcome: A composite biomarker signature that improves early detection accuracy and reduces false negatives across diverse patient populations, including those with situs solitus (normal organ placement) or atypical symptoms [50] [6].
FAQ 2: How do we mitigate the risk of biased or non-generalizable biomarker panels?
The Challenge: Many biomarker algorithms are trained on limited demographic groups, reducing their accuracy and generalizability in underrepresented populations. This is a known issue with digital biomarkers and can equally apply to molecular signatures [53].
Troubleshooting Guide:
- Action: Implement Rigorous, Prospective Validation.
- Rationale: A biomarker's credibility is established through demonstrated reproducible performance in independent test cohorts that reflect the intended-use patient population [54].
- Methodology:
- Define Intended Use: Clearly outline the test's purpose, patient population, and clinical context early in development [54].
- Ensure Diverse Cohorts: Actively recruit patients from diverse ethnic, geographic, and clinical backgrounds (e.g., PCD patients with and without laterality defects) to ensure the biomarker is relevant across the disease spectrum [1] [54].
- Conduct Analytical Validation: Establish performance characteristics (e.g., sensitivity, specificity, reproducibility) suitable for the test's intended use, progressing from Research Use Only (RUO) to full clinical validation [54].
- Expected Outcome: A robust, reliable biomarker with documented performance metrics, suitable for regulatory submission and broad clinical adoption [54].
FAQ 3: What strategies can bridge the gap between biomarker discovery and clinical implementation?
The Challenge: The number of clinically validated biomarkers approved by regulatory bodies remains modest despite significant discovery efforts. Challenges include data heterogeneity, inconsistent standardization, and high implementation costs [50] [55].
Troubleshooting Guide:
- Action: Adopt an Integrated Framework Prioritizing Interpretability and Standardization.
- Rationale: Successful translation requires systematically addressing barriers from data generation to clinical adoption [50].
- Methodology:
- Multi-Modal Data Fusion: Combine data from multiple sources (e.g., clinical scores, genomic data, digital biomarkers from wearables) to create a multidimensional health profile [50] [53].
- Standardized Governance Protocols: Implement standardized protocols for biomarker validation, data collection, and analysis to enhance reproducibility and reliability across studies [50] [54].
- Interpretability Enhancement: Use artificial intelligence (AI) tools that provide interpretable results, helping clinicians understand the model's predictions and building trust for clinical adoption [50].
- Expected Outcome: A streamlined pathway for translating biomarker discoveries into clinically actionable diagnostic tests, ultimately improving patient outcomes through precision medicine [50] [51].
Quantitative Data on Predictive Tool Performance
The table below summarizes key performance data from recent studies on the PICADAR tool, highlighting its limitations and the need for complementary biomarker-based approaches.
Table 1: Performance Metrics of the PICADAR Tool in Genetically Confirmed PCD Cohorts
| Patient Subgroup | Sensitivity | Median PICADAR Score (IQR) | Key Limitation |
|---|---|---|---|
| Overall PCD Population | 75% (202/269) [1] | 7 (IQR: 5–9) [1] | Fails to identify 25% of true PCD cases [1]. |
| PCD with Laterality Defects | 95% [1] [6] | 10 (IQR: 8–11) [1] | High sensitivity, but this subgroup is not the majority [52]. |
| PCD with Situs Solitus (normal organ placement) | 61% [1] [6] | 6 (IQR: 4–8) [1] | Poor performance in a large subgroup, leading to high false negatives [1]. |
| PCD without Hallmark Ultrastructural Defects | 59% [1] | Information Not Available | High risk of missed diagnosis in genetically confirmed cases [1]. |
| PCD without Daily Wet Cough | 0% (Automatically ruled out) [1] | Not Applicable | Excludes ~7% of genetically confirmed PCD patients at the first step [1]. |
Experimental Workflows for Biomarker Validation
Overcoming the limitations of tools like PICADAR requires a systematic, phased approach to biomarker development. The following workflow diagrams and protocols outline this process.
Workflow: Diagnostic Pathway Integrating Biomarkers to Overcome PICADAR Limitations
Workflow: Phased Biomarker Validation Pathway
Experimental Protocol: Executing the Phased Validation Pathway
Biomarker Discovery & RUO Validation:
- Objective: Transition a discovered biomarker into a test method.
- Methodology: Develop an assay on a suitable analytical platform (e.g., NGS panel, immunoassay). Perform initial, small-scale validation to demonstrate reproducible performance in independent datasets.
- Considerations: This is a relatively low-cost phase to decide whether to proceed further. The chosen technology impacts future market accessibility [54].
Retrospective Clinical Validation:
- Objective: Gather additional evidence on biomarker performance using archived clinical samples.
- Methodology: Acquire a representative sample cohort (e.g., banked serum or DNA from PCD patients and controls) that reflects the intended-use population. Analyze samples using the RUO assay.
- Considerations: This stage helps identify weaknesses in test delivery and provides valuable evidence to de-risk subsequent interventional studies [54].
Analytical Validation for Investigational Use:
- Objective: Validate the biomarker for use in informing patient treatment decisions within a clinical trial.
- Methodology: Conduct one or more clinical studies where the biomarker guides patient management. Establish rigorous performance limits (sensitivity, specificity, turnaround time).
- Considerations: Testing must comply with regulations like FDA IDE (US) or IVDR (EU). Patient risk must be carefully managed [54].
Validation for Marketing Approval:
- Objective: Generate evidence to support regulatory approval for commercial use.
- Methodology: Conduct robust analytical and clinical validation studies. The scale and scope are expanded to include process validation, stability studies, and rigorous clinical performance evaluation, often through an interventional study for novel biomarkers.
- Considerations: The level of evidence required is tied to the device's safety classification. Early engagement with regulatory authorities is recommended [54].
The Scientist's Toolkit: Essential Research Reagents & Solutions
This table details key reagents and materials required for definitive PCD diagnostic testing, which serves as the gold standard for validating new biomarkers against tools like PICADAR.
Table 2: Key Reagents and Solutions for Definitive PCD Diagnostic Testing [6]
| Research Reagent / Solution | Function in PCD Diagnosis |
|---|---|
| Nasal Epithelial Cells | Obtained via nasal brushing for ciliary functional analysis (e.g., high-speed video microscopy) and structural analysis. |
| Culture Media for Air-Liquid Interface (ALI) | Supports the differentiation and growth of ciliated epithelial cells from biopsy samples for subsequent ciliary function analysis. |
| Glutaraldehyde Fixative | Used for preparing ciliary samples for structural analysis by Transmission Electron Microscopy (TEM). |
| Antibodies for Immunofluorescence (IF) | Target specific ciliary proteins (e.g., components of dynein arms) to detect defects in protein localization and assembly. |
| DNA Sequencing Kits (PCD Gene Panel) | Used in next-generation sequencing (NGS) to identify biallelic pathogenic mutations in any of the known PCD-causing genes. |
| Chemiluminescence Analyzer | Essential for measuring low Nasal Nitric Oxide (nNO) levels, a functional hallmark of PCD. |
Standardization Needs for International Diagnostic Harmonization
Primary Ciliary Dyskinesia (PCD) is a rare, genetically heterogeneous disorder affecting motile cilia, leading to chronic respiratory symptoms, laterality defects, and fertility issues. The PICADAR (Primary Ciliary Dyskinesia Rule) tool was developed as a clinical prediction rule to identify patients requiring formal PCD testing, using seven easily obtainable clinical parameters from patient history [56]. While originally demonstrating 90% sensitivity and 75% specificity at a cut-off score of 5 points in derivation studies [56], recent 2025 evidence reveals critical limitations in its sensitivity, particularly resulting in false-negative cases where true PCD patients are missed [6].
The standardization of diagnostic pathways is crucial for international harmonization, as PICADAR's performance varies significantly across patient subgroups. A 2025 analysis found the tool's sensitivity drops to 61% in patients with normal organ placement (situs solitus) compared to 95% in those with laterality defects, and to 59% in patients without hallmark ultrastructural ciliary defects [6]. Furthermore, the tool's algorithm automatically excludes patients without daily wet cough, yet 7% of genetically confirmed PCD patients lack this symptom [6]. These limitations highlight urgent standardization needs for diagnostic protocols that can reliably detect PCD across all patient populations and resource settings.
Technical Support Center: Troubleshooting PICADAR False Negatives
Frequently Asked Questions (FAQs)
Q1: What are the primary limitations of PICADAR leading to false-negative results?
- Variable Sensitivity: Overall sensitivity of PICADAR (using a ≥5 cutoff) was only 75% in a 2025 study, meaning one in four true PCD cases would be missed [6].
- Subgroup Performance Disparities: Sensitivity drops significantly in patients with situs solitus (61%) compared to those with laterality defects (95%) [6].
- Structural Defect Limitations: Sensitivity decreases to 59% in patients without hallmark ultrastructural ciliary defects [6].
- Symptom Exclusion Bias: The tool automatically excludes patients without daily wet cough, yet 7% of genetically confirmed PCD patients lack this symptom [6].
Q2: Which patient populations are most at risk for false-negative PICADAR results?
- Patients with normal organ arrangement (situs solitus) [6]
- Patients with normal ultrastructural ciliary defects [6]
- Patients without persistent daily wet cough [6]
- Adult patients where recall bias affects accurate reporting of neonatal symptoms [6]
- Patients with genetic variants affecting ciliary function without classic structural defects [4]
Q3: What complementary diagnostic approaches can mitigate PICADAR false negatives?
- High-Speed Video Analysis (HSVA): Can detect most PCD cases missed by transmission electron microscopy (TEM) and genetics [4]
- Genetic Testing with Expanded Panels: Next-generation sequencing (NGS) gene panels covering >40 PCD-associated genes [52]
- Nasal Nitric Oxide (nNO) Measurement: Low nNO is a hallmark of PCD, though it should not be used in isolation [4]
- Immunofluorescence (IF) Labeling: Detects defects in protein localization in patients with normal ultrastructure [6]
Q4: How should diagnostic protocols be standardized to address these limitations? The European Respiratory Society Guidelines recommend that both nNO and HSVA should be entirely normal before deciding further PCD investigation is not warranted [4]. Patients with strong clinical history or abnormal HSVA should proceed to further testing including TEM and genetics even with normal nNO [4].
Advanced Diagnostic Protocols
High-Speed Video Analysis (HSVA) Protocol
Purpose: To detect characteristic ciliary beat patterns and frequency abnormalities associated with PCD in cases of suspected false-negative PICADAR results.
Methodology:
- Sample Collection: Nasal epithelial cells obtained via nasal brushing from the inferior surface of the inferior turbinate [6]
- Sample Processing: Immediate analysis or culture in air-liquid interface (ALI) media to differentiate ciliated epithelial cells [6]
- Image Acquisition: Record ciliary movement using high-speed digital video microscopy (>500 frames per second) [4]
- Pattern Analysis: Assess ciliary beat frequency, pattern coordination, and waveform [4]
Interpretation Guidelines:
- Repeatedly dyskinetic cilia or abnormal beat pattern following reanalysis after culture, with normal genetics and TEM, indicates PCD is "highly likely" [4]
- HSVA can accurately diagnose most patients with normal TEM/genetics (false negatives) who require specialist PCD care [4]
- HSVA provides an accurate result on the day of testing for preliminary counseling and treatment initiation [4]
Next-Generation Sequencing Gene Panel Protocol
Purpose: To identify biallelic mutations in PCD-associated genes in patients with high clinical suspicion but negative or equivocal functional testing.
Methodology:
- Sample Collection: Blood or saliva samples for DNA extraction [52]
- Gene Panel Selection: Comprehensive panels covering 40-47 known PCD-causing genes [6]
- Sequencing: Next-generation sequencing of exons and flanking DNA with deletion/duplication analysis [52]
- Variant Interpretation: Classification of variants as pathogenic, likely pathogenic, or of uncertain significance [52]
Quality Control Considerations:
- Ensure genotype is compatible with ciliary phenotype using HSVA, TEM, and/or immunofluorescence [4]
- Correlate genetic findings with clinical phenotype to avoid false positives from variants of unknown significance [4]
- Utilize international databases (e.g., ClinVar) for variant classification [52]
Diagnostic Pathway Integration
The following diagnostic workflow integrates multiple methodologies to address PICADAR limitations and standardize PCD diagnosis across international centers:
Figure 1: Comprehensive Diagnostic Pathway for Suspected PCD Cases
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 1: Key Reagents and Solutions for Definitive PCD Diagnostic Testing
| Research Reagent / Solution | Function in PCD Diagnosis | Application Context |
|---|---|---|
| Nasal Epithelial Cells | Obtained via nasal brushing for ciliary functional and structural analysis [6] | HSVA, TEM, cell culture |
| Culture Media for Air-Liquid Interface (ALI) | Supports differentiation and growth of ciliated epithelial cells from biopsy samples [6] | Ciliary function analysis post-culture |
| Glutaraldehyde Fixative | Used for preparing ciliary samples for structural analysis by Transmission Electron Microscopy (TEM) [6] | Ultrastructural defect identification |
| Antibodies for Immunofluorescence (IF) | Target specific ciliary proteins to detect defects in protein localization [6] | Protein localization analysis |
| DNA Sequencing Kits (PCD Gene Panel) | Identify biallelic mutations in known PCD-causing genes [6] | Genetic confirmation of diagnosis |
| Chemiluminescence Analyzer | Essential for measuring low Nasal Nitric Oxide levels, a PCD hallmark [6] | nNO screening measurement |
Quantitative Assessment of Diagnostic Tool Performance
Table 2: Performance Characteristics of PCD Diagnostic Modalities
| Diagnostic Tool | Sensitivity Range | Specificity Range | Key Limitations | Role in Addressing False Negatives |
|---|---|---|---|---|
| PICADAR (≥5 cutoff) | 71-90% [56], as low as 75% in 2025 data [6] | 75-94% [56] | Lower sensitivity in situs solitus (61%) and normal ultrastructure (59%) cases [6] | Initial screening tool requiring supplementation |
| High-Speed Video Analysis (HSVA) | Detects most cases with normal TEM/genetics [4] | High when typical dyskinetic patterns observed [4] | Requires expertise and specialized equipment [4] | Identifies functional defects missed by other methods |
| Transmission Electron Microscopy (TEM) | 70-80% (identifies hallmark defects) [56] | High for hallmark defects | Normal in 20-30% of genetically confirmed PCD [4] | Structural analysis for classic defects |
| Genetic Testing (Expanded Panels) | >90% for known genes [6] | High for pathogenic variants | Variants of unknown significance complicate interpretation [4] | Molecular confirmation, especially in equivocal cases |
| Nasal Nitric Oxide (nNO) | High for classic PCD [4] | High in cooperative patients | False negatives possible, especially in CCDC103 mutations [4] | Supportive screening measure |
The limitations of PICADAR highlighted by recent 2025 research underscore the critical need for standardized, multifaceted diagnostic protocols in PCD diagnosis [6]. International harmonization requires:
- Awareness of PICADAR's variable performance across different patient subgroups, particularly its reduced sensitivity in patients with situs solitus and normal ciliary ultrastructure
- Implementation of complementary diagnostic techniques including HSVA, expanded genetic testing, and immunofluorescence to capture false-negative cases
- Standardized interpretive criteria across specialist centers to ensure consistent diagnosis and management
- Adaptation to resource settings with appropriate technology deployment, recognizing that genetic testing is becoming more accessible in diverse healthcare environments [52]
This integrated approach, utilizing the troubleshooting guides and standardized protocols outlined above, will facilitate earlier and more accurate PCD diagnosis across all patient populations, ultimately improving respiratory outcomes through timely intervention and specialized care.
Conclusion
The limitations of PICADAR underscore a critical need to evolve beyond standalone clinical prediction tools for PCD diagnosis. A substantial minority of patients, particularly those without laterality defects or classic ultrastructural findings, risk delayed diagnosis and irreversible morbidity due to PICADAR's suboptimal sensitivity. Future progress requires integrated diagnostic algorithms that combine refined clinical assessment with advanced genetic, functional, and structural analyses. For the research and drug development community, these findings highlight the importance of encompassing PCD's full genotypic and phenotypic spectrum in clinical trial design and therapeutic development. Prioritizing the creation of validated, accessible, and comprehensive diagnostic pathways will be essential for ensuring equitable and timely diagnosis for all PCD patients, ultimately improving long-term clinical outcomes.
References
- 1. Limitations of PICADAR as a diagnostic predictive tool for ... [https://www.medrxiv.org/content/10.1101/2025.09.22.25336363v1]
- 2. Primary ciliary dyskinesia: A review [https://www.sciencedirect.com/science/article/pii/S2950008725000420]
- 3. Empowering limited-resource countries: collaborating with ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1547152/full]
- 4. The Controversies and Difficulties of Diagnosing Primary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6938149/]
- 5. Challenges in Diagnosing Primary Ciliary Dyskinesia in a ... [https://www.mdpi.com/2073-4425/13/7/1252]
- 6. Reevaluating Its Role in Primary Ciliary Dyskinesia Diagnosis [https://www.molbiosci.com/posts/critical-limitations-of-picadar-reevaluating-its-role-in-primary-ciliary-dyskinesia-diagnosis]
- 7. Congenital Heart Defects and Ciliopathies Associated With ... [https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2018.00175/full]
- 8. BMP2 is a potential causative gene for isolated ... [https://www.sciencedirect.com/science/article/abs/pii/S176972122300126X]
- 9. Some Isolated Cardiac Malformations Can Be Related to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6023464/]
- 10. Challenges in Diagnosing Primary Ciliary Dyskinesia in a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9324289/]
- 11. Limitations of PICADAR as a diagnostic predictive tool for ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1691758/full]
- 12. a diagnostic predictive tool for primary ciliary dyskinesia [https://pmc.ncbi.nlm.nih.gov/articles/PMC4819882/]
- 13. Diversity and evolution of drug resistance mechanisms in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5648319/]
- 14. Ultrastructure of macromolecular assemblies contributing ... [https://www.nature.com/articles/s41467-024-45770-6]
- 15. Diagnosis of primary ciliary dyskinesia: discrepancy according ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8558472/]
- 16. ERS Task Force guideline for the diagnosis of primary ciliary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6054534/]
- 17. ERS and ATS unite for universal PCD diagnosis guideline [https://thelimbic.com/respiratory/ers-and-ats-unite-for-universal-pcd-diagnosis-guideline/]
- 18. High-speed Video Microscopy Analysis (HVMA) [https://www.medizin.uni-muenster.de/en/pcd/research/high-speed-video-microscopy-analysis-hvma.html]
- 19. Leader in PCD treatment offers HSVM and IFM… [https://www.rileychildrens.org/research/featured-research/leader-in-pcd-treatment-offers-hsvm-and-ifm-to-aid-in-disease-diagnosis]
- 20. High-speed Video Microscopy Analysis for First-line ... [https://www.jove.com/t/63292/high-speed-video-microscopy-analysis-for-first-line-diagnosis-primary]
- 21. High-Speed Videomicroscopy Analysis Presents ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6938157/]
- 22. Whole-exome sequencing accuracy in the diagnosis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7792814/]
- 23. Primary Ciliary Dyskinesia: A Clinical Review - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11171568/]
- 24. Limitations of Whole Genome Sequencing in Genetic Testing [https://3billion.io/blog/limitation-of-whole-genome-sequencing]
- 25. Reducing false positive incidental findings with ensemble ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4112476/]
- 26. Accuracy of Immunofluorescence in the Diagnosis of Primary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5519960/]
- 27. International consensus guideline for reporting transmission ... [https://publications.ersnet.org/content/erj/55/4/1900725]
- 28. An optimized protocol for immuno-electron microscopy of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9673964/]
- 29. TEM, SEM, and STEM-based immuno-CLEM workflows ... [https://www.nature.com/articles/s41598-020-79637-9]
- 30. Phenotype prediction using biologically interpretable ... [https://www.nature.com/articles/s41540-024-00405-w]
- 31. Bioinformatics Pipeline Troubleshooting [https://www.meegle.com/en_us/topics/bioinformatics-pipeline/bioinformatics-pipeline-troubleshooting]
- 32. Development of prediction models for high throughput ... [https://www.sciencedirect.com/science/article/abs/pii/S0889157525002686]
- 33. Tutorials & workshops - [BC]2 Basel Computational ... [https://www.bc2.ch/tutorials-workshops]
- 34. PICADAR A Diagnostic Predictive Tool For Primary Ciliary ... [https://www.scribd.com/document/897373060/PICADAR-a-diagnostic-predictive-tool-for-primary-ciliary-dyskinesia]
- 35. Referral Process Enhancement: Innovative Approaches and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11318818/]
- 36. Inbound vs Outbound Referrals: Optimizing Both Sides of ... [https://www.healthviewx.com/inbound-vs-outbound-referrals-optimizing-both-sides-of-the-healthcare-network/]
- 37. Factors affecting the successful implementation of the referral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8884299/]
- 38. AI enhanced diagnostic accuracy and workload reduction ... [https://www.nature.com/articles/s41746-025-01892-9]
- 39. Development of simulation optimization methods for ... [https://www.sciencedirect.com/science/article/pii/S1532046417301831]
- 40. The genetics of situs inversus without primary ciliary ... [https://www.nature.com/articles/s41598-020-60589-z]
- 41. Noncoding DNA Variants in Primary Ciliary Dyskinesia [https://pmc.ncbi.nlm.nih.gov/articles/PMC12618996/]
- 42. 8 Frequently Asked Questions About Genetic Testing in ... [https://www.worldwide.com/blog/2022/12/8-frequently-asked-questions-about-genetic-testing-in-clinical-trials/]
- 43. Key Strategies for Optimizing NGS Workflows [https://www.technologynetworks.com/genomics/articles/key-strategies-for-optimizing-ngs-workflows-395232]
- 44. Primary Ciliary Dyskinesia—Current Diagnostic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12525432/]
- 45. New AI Tool Pinpoints Genes, Drug Combos To Restore ... [https://hms.harvard.edu/news/new-ai-tool-pinpoints-genes-drug-combos-restore-health-diseased-cells]
- 46. The latest trends in drug discovery [https://www.cas.org/resources/cas-insights/2025-drug-discovery-trends]
- 47. Your Guide to Emerging Technologies and Tech Trends in ... [https://www.scalosoft.com/blog/your-guide-to-emerging-technologies-and-tech-trends-in-2025/]
- 48. Leading AI-Driven Drug Discovery Platforms [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 49. Transformative Role of Artificial Intelligence in Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406033/]
- 50. Applications and challenges of biomarker-based predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399543/]
- 51. Challenges and Future Trends in Biomarker Analysis for ... [https://blog.crownbio.com/challenges-and-future-trends-in-biomarker-analysis-for-clinical-research-whats-ahead-in-2025]
- 52. Which side are they on? Diagnosing primary ciliary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10646753/]
- 53. Unlocking the Power of Digital Biomarkers in Clinical Trials [https://acrpnet.org/2025/08/19/unlocking-the-power-of-digital-biomarkers-in-clinical-trials]
- 54. A Guide to Biomarker Validation [https://sonraianalytics.com/a-guide-to-biomarker-validation/]
- 55. Challenges in Biomarker Discovery: Combining Expert ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3548234/]
- 56. PICADAR: a diagnostic predictive tool for primary ciliary ... [https://publications.ersnet.org/content/erj/47/4/1103]